Abstract
Background
This study was undertaken to provide up-to-date survival data for Canadian adult in-patients following attempted resuscitation from cardiac or respiratory arrest. We hope that objective data might encourage more meaningful dialogue between physicians, patients and their families regarding resuscitation wishes.
Methods
We reviewed all records of adult cardiopulmonary arrest that occurred between Jan. 1, 1997, and Jan. 31, 1999, at the 3 main teaching hospitals in Edmonton. We then abstracted data from the full inpatient medical records to describe patient characteristics, type of arrest and survival details. The family physicians of survivors were contacted to confirm the outcomes. We included only adults admitted to hospital but not to a critical care bed.
Results
There were 247 arrests during the study period; 143 (57.9%) were witnessed, and 104 (42.1%) were unwitnessed). Of the patients whose arrests were witnessed, 48.3% (95% confidence interval [CI] 39.8%–56.8%) were able to be resuscitated, 22.4% (95% CI 15.8%–30.1%) survived to hospital discharge, and 18.9% (95% CI 12.8%–26.3%) were able to return home. Survival was highest after primary respiratory arrest and lowest after pulseless electrical activity or asystole. Of the patients with unwitnessed arrests, 21.2% (95% CI 13.8%–30.3%) were able to be resuscitated, but only 1 patient (1.0% [95% CI 0.0%–5.2%]) survived to hospital discharge and was able to return home. This patient survived an unwitnessed respiratory arrest. No patient who had an unwitnessed cardiac arrest survived to discharge. Most of the respiratory arrests were witnessed (93.1%), and most of the pulseless electrical activity or asystole arrests were unwitnessed (54.6%). We did not find age or sex to be independent predictors of survival. However, the risk of not returning home was higher among patients whose arrest occurred between 2301 and 0700 than among those whose arrest was between 0701 and 1500 (adjusted OR 3.2, 95% CI 1.0–10.1). Survival was significantly decreased after pulseless ventricular tachycardia or ventricular fibrillation arrest (adjusted OR 4.2, 95% CI 1.4–12.5) and even more so after pulseless electrical activity or asystole arrest (adjusted OR 21.0, 95% CI 6.2–71.7) than after respiratory arrest.
Interpretation
Overall, survival following cardiopulmonary resuscitation in hospital does not appear to have changed markedly in 40 years. The type of arrest is highly predictive of survival, whereas age and sex are not.
Cardiopulmonary resuscitation (CPR) was first described in 1960.1 Therapeutic advances on the one hand, and an aging population and a presumably sicker inpatient population on the other, may mean that old survival data are no longer reliable. This study was therefore undertaken to provide up-to-date survival data for the Canadian adult in-hospital population following attempted resuscitation from cardiac or respiratory arrest.
Accurate resuscitation rates are necessary in an era of increased debate regarding end-of-life directives and evidence-based treatment. Also, despite considerably different models of health care delivery, Canadians currently rely on data that is overwhelmingly from the United States. Objective data can be used to educate hospital staff, to help them from being overly fatalistic and therefore reluctant to participate in “codes” or overly optimistic and likely to blame themselves in the event of death.
Many studies have been performed to determine the effectiveness of CPR. However, there is still disagreement regarding absolute survival rates, and although it is generally accepted that patients with witnessed arrests are more likely to survive, there are surprisingly few studies that directly compare the outcomes of unwitnessed and witnessed arrests. Debate also continues regarding whether advanced age is associated with an adverse outcome. Furthermore, several American studies in the 1990s showed improved survival following resuscitation when compared with survival in previous decades. However, these studies involved patients who typically were continuously monitored and admitted for acute coronary syndromes2,3,4 and who were, according to the authors of one study, “highly selected when compared with patients who [had] received CPR in previous years.”4 It is therefore unclear whether these results can be extrapolated to the general in-hospital population in Canada. Overall, it is unclear whether resuscitation rates have changed significantly despite 40 years of therapeutic advances.
The purpose of our study was to answer this question: “If an adult is admitted to a Canadian non-critical care bed and suffers a cardiac or respiratory arrest, how likely is the patient to survive to initial resuscitation and to hospital discharge, and what are the chances of returning to live at home versus receiving assisted living or long-term care?” We also wished to determine whether survival rates differed significantly according to age, sex, type of arrest, time of arrest or whether the arrest was witnessed or not. We hope that objective data will encourage meaningful dialogue between physicians, patients and their families.
Methods
The main teaching hospitals in Edmonton are the University of Alberta Hospital, the Royal Alexandra Hospital and The Grey Nuns' Hospital. Combined they provide over 1000 active care beds for adults in addition to intensive care units, coronary care units and resuscitation teams. Whenever the overhead paging system is activated to alert hospital staff of a cardiac or respiratory arrest, an arrest record is generated. All inpatients who have a pulse after resuscitation are subsequently transferred to a critical care unit.
We examined all records of cardiac or respiratory arrest from the 3 hospitals that occurred between Jan. 1, 1997, and Jan. 31, 1999. We then retrieved the full inpatient medical records and abstracted data regarding patient characteristics, type of arrest and survival details. We included only patients who had a “true arrest” (defined as requiring one or more of manual CPR, intubation or defibrillation). For patients with more than one arrest, we included only the first episode.
We excluded patients already admitted to a “critical care unit” (defined as having continuous monitoring, one-on-one nursing or ventilators). We also excluded patients in emergency departments or operating suites, those admitted by a pediatrician, those for whom complete medical records could not be found and visitors to the hospital. We used the arrest type recorded upon arrival by the code team because the presence of people with certified training in advanced cardiac life support should have allowed for accurate identification and full resuscitation. We determined whether an arrest was witnessed or not by reviewing both the arrest record and the medical chart.
We defined initial resuscitation as the presence of a pulse following CPR. Patients with a pulse following CPR were recorded as being “able to be resuscitated.” We further reviewed the full medical record to ascertain whether the patient died in hospital or survived to be discharged and, if discharged, whether the patient was discharged home or to an assisted-living facility or nursing home. We chose a 3-month period to allow for recovery and rehabilitation. We made the distinction between survival to discharge and being discharged home in order to assess the likelihood of a patient's health deteriorating so much after an arrest that independence was lost. Survivors who had previously been residents of an assisted-living facility were considered to have been discharged home if they returned to a facility offering similar assistance. If they returned to a facility offering increased assistance we included them in the group unable to be discharged home. We contacted the family physicians of all patients discharged home or to an assisted-living facility in order to confirm the outcomes.
We calculated crude survival proportions as the number of patients surviving divided by the total population within each specified stratum. We analyzed univariable associations between hospital site and time of arrest, hospital site and survival after arrest, sex and survival, and type of arrest and survival. We also examined whether survival varied significantly by type of cardiac arrest (pulseless ventricular tacchycardia or ventricular fibrillation [pulseless VT/VF] versus pulseless electrical activity or asystole [pulseless EA/ASY]). The Pearson χ2 test and 2-sided Fisher's exact test were used.5 The variables thought to be significantly associated with survival after cardiac or respiratory arrest were initially fit into a series of logistic regression models that predicted initial survival after CPR, survival to discharge from hospital and survival to discharge home.6 These variables included age, sex, time of arrest, type of arrest, whether the arrest was witnessed or not and hospital location. We determined the final logistic regression models by backward selection of the variables, maintaining those that were significant at a p value of 0.05 or less. We left age and sex in the final models as potential confounding variables, despite their lack of statistical significance, given their inconsistent association with altered survival following cardiac arrest in previous studies and the known association between age and coronary mortality. We removed the variable coding for witnessed versus unwitnessed arrest from the final logistic regression models because of its high degree of collinearity with the variable coding for type of arrest. This implied that most of the information influencing the prediction of survival was carried by the type of arrest and that an unwitnessed arrest was likely to be a terminal rhythm such as pulseless EA/ASY. This is likely because of the natural deterioration of rhythm over time experienced by dying patients. Comparisons were deemed significant if they achieved a p value of 0.05 or less.
The Health Research Ethics Board (Biomedical Panel) at the University of Alberta approved our study protocol.
Results
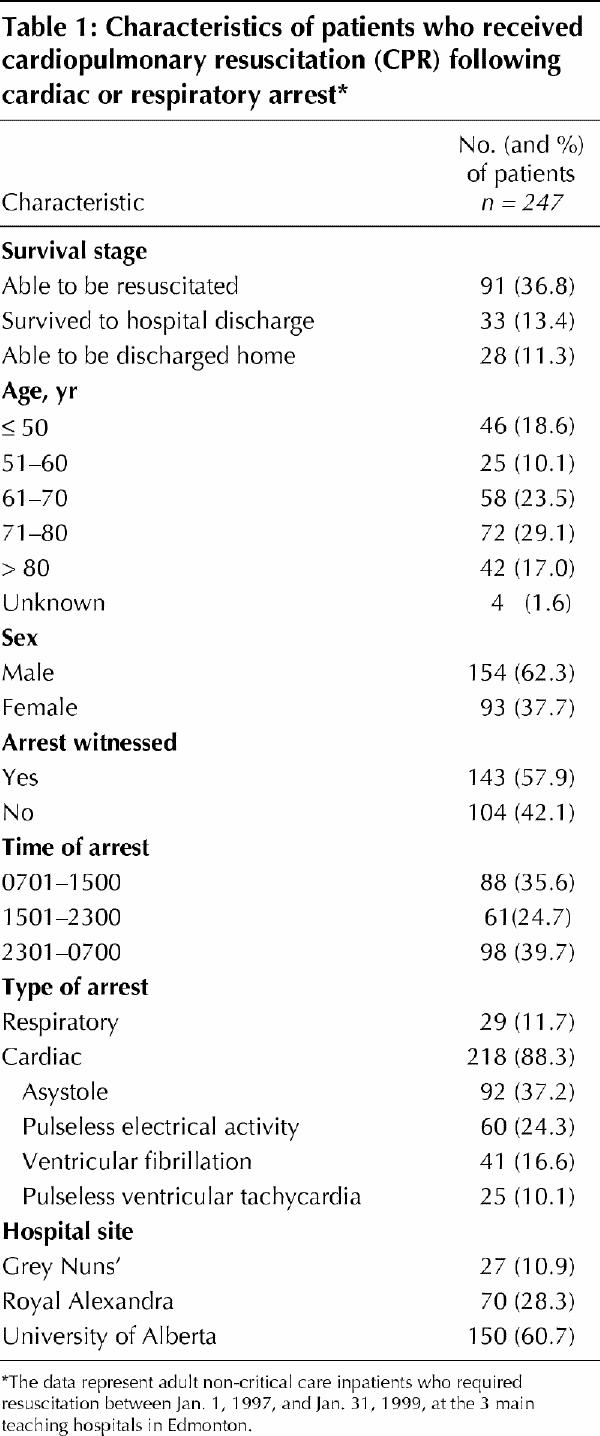
There were 299 records of in-hospital cardiac or respiratory arrest during the study period. Of these, we excluded 45 because no CPR, intubation or defibrillation was required and 7 because the full medical charts were incomplete or illegible. This left 247 arrests (Table 1). Asystole was the most frequent single arrest type (in 37.2% of cases), and pulseless EA was the second most frequent (in 24.3%).
Table 1
Of the 143 patients whose arrest was witnessed, 48.3% (95% confidence interval [CI] 39.8%–56.8%) were able to be resuscitated, 22.4% (95% CI 15.8%–30.1%) survived to hospital discharge, and 18.9% (CI 12.8%–26.3%) were discharged home (Table 2). Survival to all 3 stages was highest among patients with witnessed primary respiratory arrests (p < 0.001). After subtracting respiratory arrests from all witnessed arrests, we found that survival was lower at all stages after witnessed cardiac arrests than after all arrests combined. Of the subtypes of cardiac arrest, pulseless EA/ASY had the lowest survival of the witnessed arrest types, with 36.2% (95% CI 25.0%–48.7%) of the patients able to be resuscitated and 7.2% (95% CI 2.4%–16.1%, p < 0.001) surviving to discharge as well as to home.
Table 2
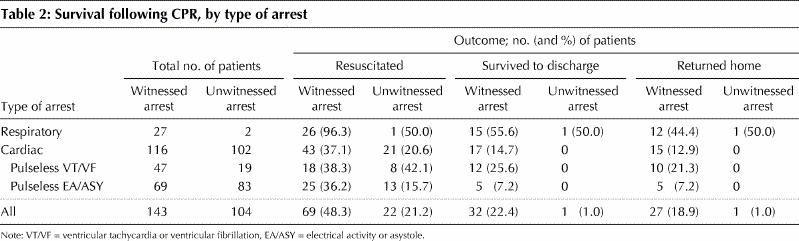
Of the 104 patients whose arrest was not witnessed, 21.2% (95% CI 13.8%–30.3%) were able to be resuscitated, but only 1 patient (1.0% [95% CI 0.0%–5.2%]) survived to discharge (Table 2). This survivor suffered an unwitnessed respiratory arrest, and estimates are that this arrest was missed by less than 2 minutes. Initial resuscitation was successful for 20.6% of the patients with an unwitnessed cardiac arrest, 42.1% of those with an unwitnessed pulseless VT/VF arrest and 15.7% of those with an unwitnessed pulseless EA/ASY arrest; however, none of these patients survived to discharge.
Overall, 36.8% of the patients were able to be resuscitated, 13.4% survived to hospital discharge and 11.3% were discharged home. Of the 33 patients who survived to discharge, all but 5 were able to return home. However, this means that 15.2% of those discharged experienced a significant enough decrease in function after their arrest that they were no longer deemed able to fully care for themselves.
We found no significant association between either age or sex and outcome (Table 3). Likewise, no association was seen between hospital site and the patient's initial resuscitation (p = 0.10), survival to hospital discharge (p = 0.89) or ability to be discharged home (p = 0.73). There was also no clear association between hospital site and time of cardiac arrest (p = 0.84). We observed a statistically significant independent association between type of arrest and survival to discharge home after adjusting for age, sex and time of initial resuscitation. The association was strongest between pulseless EA/ASY arrest (v. respiratory arrest) and not being able to return home (adjusted odds ratio [OR] 21.0, 95% CI 6.2–71.7, p < 0.001). Similarly, a weaker but statistically significant association was observed between pulseless VT/VF arrest (v. respiratory arrest) and not being able to return home (adjusted OR 4.2, 95% CI 1.4–12.5, p < 0.01).
Table 3
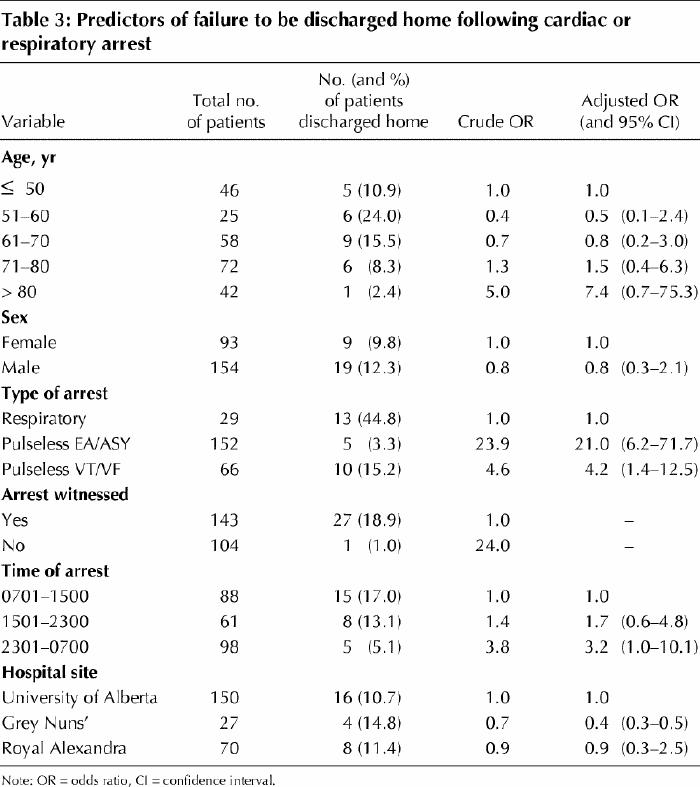
We also found that the time of arrest was an independent predictor of survival to discharge home, but not of survival to the other 2 survival stages. Patients resuscitated between 2301 and 0700 were at a significantly higher risk of not being discharged home than were those resuscitated between 0701 and 1500 (adjusted OR 3.2, 95% CI 1.0–10.1, p = 0.045) after adjusting for age, sex and type of arrest. In addition, arrests during the 2301–0700 period were more likely than arrests during the 1501–2300 period to be unwitnessed (52.0% v. 39.3%).
Interpretation
Among all the witnessed arrests, close to 1 in 2 patients were able to be resuscitated, 1 in 3 survived to 24 hours (data not shown), 1 in 4 survived to discharge, and 1 in 5 were able to return home (Table 2). Of all the discharged patients, about 1 in 7 did not return home because of decreased function following the arrest. The discrepancy between initial resuscitation and likelihood of recovering independence emphasizes the need to discuss both when deciding upon resuscitation wishes. The particularly low survival following pulseless EA/ASY arrests and unwitnessed arrests also illustrates the need to consider these eventualities separately. Although 1 in 5 patients with an unwitnessed cardiac arrest were initially resuscitated, none of them survived to discharge. However, the degree of collinearity between whether an arrest was witnessed and the type of arrest indicates that both parameters are effectively measuring a similar construct, namely the degree of “irreversibility” of the arrest, with pulseless EA/ASY being the most refractory to attempted treatment.
Our survival data do not differ greatly from those in American and Canadian studies from the 1960s to 1980s.7,8,9,10,11,12,13,14,15 In the 1990s, however, 3 American studies reported survival to discharge that was 2–3 times greater than our results.2,3,4 This difference may be because those patients typically had witnessed arrests and had single-organ cardiac disease, rather than cardiac arrest in addition to non-cardiac illness.4 Our study may be a more accurate prediction of survival in the general hospital population. If so, survival has not improved in 40 years.
Our results showed no significant association between age and outcome. The combined results of previous studies have not conclusively found a relation between age and outcome.2,3,4,7,8,11,12,13,14,15,16 Consistent with findings from other studies,17,18 our results did not show a statistically significant effect of sex on survival (Table 3). Overall, there are insufficient data to recommend refusal of resuscitation on the basis of age or sex. This study confirms that the type of arrest has a far stronger influence on outcome.
Although some researchers have argued that resuscitation is not beneficial for cardiac arrest patients,7,8 our data show that this is not the case for patients who have primary respiratory arrests. The belief that this is due to stopping an arrest in its earlier stage before full cardiorespiratory collapse occurs is supported by our finding that 93% of the respiratory arrests were witnessed, as compared with only 45% of the pulseless EA/ASY arrests. Regardless, for some patients, it may be appropriate to discuss offering ventilatory support alone instead of full CPR.
In our study, patients who had a cardiac arrest, particularly those who had a pulseless EA/ASY arrest, were significantly less likely to survive than were patients who had a primary respiratory arrest (p < 0.001). The low survival rate after pulseless EA/ASY is consistent with the findings of many studies,7,8,12,15 including the 3 from the 1990s that showed encouraging survival rates after other types of arrests.2,3,4 If we assume that pulseless EA/ASY is typically a terminal arrest, then survival following asystole may never be significantly improved upon.
Several large trials have reported an early morning peak and late night nadir for out-of-hospital arrests.19,20,21,22 The data have been less clear for in-hospital arrests, where circadian influences may be lessened. However, we observed significantly higher odds of not being able to return home for patients whose arrest occurred between 2301 and 0700, and there were more unwitnessed and pulseless EA/ASY arrests during this period. Typically, the greatest proportion of arrests in hospital occur when the least number of staff are available who might otherwise be able to witness an arrest during its early, potentially salvageable period.
Data from the 3 hospitals in our study, which encompass tertiary care, inner-city health care and community health care, should provide survival rates generalizable to most adult inpatients. However, all 3 hospitals have resuscitation teams and resources that exceed those of rural hospitals. Therefore, these results may represent a “best-case scenario,” which re-emphasizes the need to discuss the realities of resuscitation. Other limitations of our study include possible inaccuracies with charting and how competently resuscitation was performed. To examine comorbidity would require predefined standardized criteria, which are not possible with a retrospective study. Chart review is also an imperfect way to establish definitively whether arrests were unwitnessed. Despite these limitations, families must still decide on the utility of resuscitation, and therefore these crude survival data are important. Furthermore, our results are intended as objective data to facilitate informed dialogue rather than to dictate who should, or should not, be resuscitated.
In an ingenious review of television medical dramas, Diem and colleagues23 found that the initial survival rate following CPR was 75%, with 67% survival to discharge. Except for respiratory arrests, these rates are 2–6 times higher than those in any reported study. However, these figures may represent public expectations. The onus is therefore on physicians to discuss the reality and enquire about the expectations of families.
Resuscitation was never originally recommended for all patients,1 and its goal should be to “reverse premature death not prolong inevitable death.”24 The current situation is often to attempt CPR unless it is explicitly refused. Although this may be due to increased patient autonomy or litigation, it is inconsistent with an age of evidence-based treatment and resource concerns. Given the complexity and importance of resuscitation issues, vigorous debate and study are essential.
Acknowledgments
We thank Drs. David Brindley and Tom Marrie for their comments on an earlier draft of the manuscript.
Footnotes
This article has been peer reviewed.
Contributors: Dr. Brindley was a principal coauthor and contributed to the study design and data collection. Dr. Markland contributed to the data collection and Dr. Mayers to the study design. Dr. Kutsogiannis was a principal coauthor and provided statistical analysis.
Competing interests: None declared.
Correspondence to: Dr. Peter G. Brindley, Division of Critical Care Medicine, Unit 3C4, General Systems ICU, Walter C. Mackenzie Health Sciences Centre, 8440–112 St., Edmonton AB T6G 2R7; fax 780 407-3340; pebrindl@cha.ab.ca
References
- 1.Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA 1960;173:1064-7. [DOI] [PubMed]
- 2.Robinson GR, Hess D. Postdischarge survival and functional status following in-hospital cardiopulmonary resuscitation. Chest 1994;105:991-6. [DOI] [PubMed]
- 3.Rosendberg M, Wang C, Hoffman-Wilde S. Results of cardiopulmonary resuscitation. Arch Intern Med 1993;153:1370-5. [DOI] [PubMed]
- 4.Tresch DD, Heudebert G, Kutty K. Cardiopulmonary resuscitation in elderly patients hospitalized in the 1990s: a favorable outcome. J Am Geriatr Soc 1994;42:137-41. [DOI] [PubMed]
- 5.Rosner B. Fundamentals of biostatistics. Belmont: Duxbury Press; 1995.
- 6.Hosmer DW, Lemeshow S. Applied logistic regression. New York: John Wiley and Sons; 1989.
- 7.Taffet GI, Teasdale TA, Luchi RJ. In-hospital cardiopulmonary resuscitation. JAMA 1988;260:2069-72. [PubMed]
- 8.Murphy DI, Murray AM, Robinson BE. Outcomes of cardiopulmonary resuscitation in the elderly. Ann Intern Med 1989;111:199-205. [DOI] [PubMed]
- 9.Johnson AL, Tanser PH, Ulan RA, Wood TE. Results of cardiac resuscitation in 552 patients. Am J Cardiol 1967;20:831-5. [DOI] [PubMed]
- 10.Lemire JG, Johnson AL. Is cardiac resuscitation worthwhile? A decade of experience. N Engl J Med 1972;286:970-2. [DOI] [PubMed]
- 11.Tweed WA, Bristow G, Donen N, Kirk BW. Evaluation of hospital-based cardiac resuscitation 1973–1977. CMAJ 1980;122:301-4. [PMC free article] [PubMed]
- 12.Roberts D, Landolfo K, Light RB, Dobson K. Early predictors of mortality for hospitalized patients suffering cardiopulmonary arrest. Chest 1990;97:413-9. [DOI] [PubMed]
- 13.Gulati RS, Bhan GL, Horan MA. Cardiopulmonary resuscitation of the elderly. Lancet 1983;2:267-9. [DOI] [PubMed]
- 14.Bedell SE, Delbanco TL, Cook EF. Survival after cardiopulmonary resuscitation in the hospital. N Engl J Med 1983;309:569-75. [DOI] [PubMed]
- 15.Berger R, Kelley M. Survival after in-hospital cardiopulmonary arrest of non critically ill patients — a prospective study. Chest 1994;106:872-9. [DOI] [PubMed]
- 16.Tortalani AJ, Risucci DA, Rosati RJ. In-hospital cardiopulmonary resuscitation: patient arrest and resuscitation factors associated with survival. Resuscitation 1990;20:115-28. [DOI] [PubMed]
- 17.Pell JP, Sirel J, Marsden AK, Cobbe SM. Sex differences in outcome following community-based cardiopulmonary arrest. Eur Heart J 2000;21:239-44. [DOI] [PubMed]
- 18.Albert CM, McGovern BA, Newell JB, Ruskin JN. Sex difference in cardiac arrest survivors. Circulation 1996;93:1170-6. [DOI] [PubMed]
- 19.Muller JE. Circadian variation in cardiovascular events. Am J Hypertens 1999; 12(2 Pt 2):35S-42S. [DOI] [PubMed]
- 20.Willich SN, Levy D, Rocco MB, Tofler GH, Stone PH, Muller JE. Circadian variation in the incidence of sudden cardiac death in the Framingham Heart Study population. Am J Cardiol 1987;60:801-6. [DOI] [PubMed]
- 21.Muller JE, Ludner PL, Willich SN, Tofler GH, Aylmer G, Klangos I, et al. Circadian variation in the frequency of sudden cardiac death. Circulation 1987; 75:131-8. [DOI] [PubMed]
- 22.Muller JE, Stone PH, Turi ZG, Rutherford JD, Czeisler CA, Parker C, et al, and the MILIS Study Group. Circadian variation in the frequency of onset of acute myocardial infarction. N Engl J Med 1985;313:1315-22. [DOI] [PubMed]
- 23.Diem SJ, Lantos JD, Tulsky JA. Cardiopulmonary resuscitation on television. Miracles and misinformation. N Engl J Med 1996;334:1578-82. [DOI] [PubMed]
- 24.Cummins RO. Ethical aspects of emergency cardiac care. In: Cummins RO, editor. Textbook of advanced cardiac life support. Dallas: American Heart Association; 1997. p. 1-71.


