Abstract
Objectives
To investigate the attitudes of Chinese radiologists or interns towards generative pre-trained (GPT)-like technologies.
Methods
A prospective survey was distributed to 1339 Chinese radiologists or interns via an online platform from October 2023 to May 2024. The questionnaire covered respondent characteristics, opinions on using GPT-like technologies (in clinical practice, training and education, environment and regulation, and development trends), and their attitudes toward these technologies. Logistic regression was conducted to identify underlying factors associated with the attitude.
Results
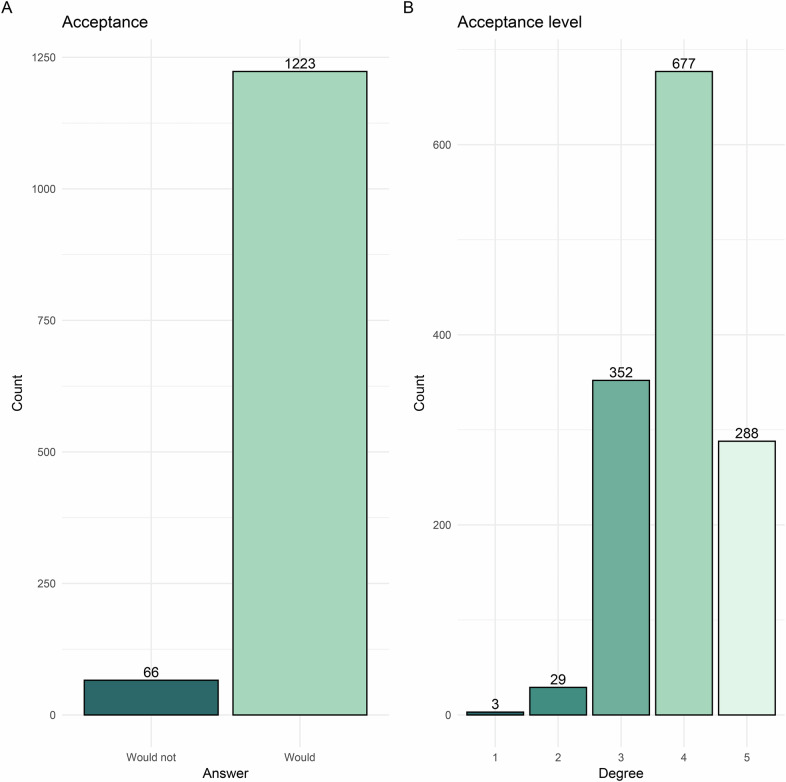
After quality control, 1289 respondents (median age, 37.0 years [IQR, 31.0–44.0 years]; 813 males) were surveyed. Most of the respondents (n = 1223, 94.9%) supported adoption of GPT-like technologies. Based on the acceptance level of GPT-like technologies, the respondents were 3 (0.2%), 29 (2.2%), 352 (27.3%), 677 (52.5%), and 228 (17.7%) from low to high acceptance degrees. Multivariable analysis revealed significant associations between positive attitudes towards GPT-like technologies and their acceptance: writing papers and language polishing (odds ratio [OR] = 1.99; p < 0.001), influence of colleagues using such technologies (OR = 1.77; p = 0.007), government regulation introduction (OR = 2.25; p < 0.001), and enhancement of decision support capabilities (OR = 2.67; p < 0.001). Sensitivity analyses confirmed these results for different acceptance thresholds (all p < 0.001).
Conclusions
Chinese radiologists or interns generally support GPT-like technologies due to their potential capabilities in clinical practice, medical education, and scientific research. They also emphasize the need for regulatory oversight and remain optimistic about their future medical applications.
Critical relevance statement
This study highlights the broad support among Chinese radiologists for GPT-like technologies, emphasizing their potential to enhance clinical decision-making, streamline medical education, and improve research efficiency, while underscoring the need for regulatory oversight.
Key Points
The impact of GPT-like technologies on the radiology field is unclear.
Most Chinese radiologists express the supportive adoption of GPT-like technologies.
GPT-like technologies’ capabilities at research and clinic prompt the attitude.
Graphical Abstract
Keywords: Radiologists, Attitude, Surveys and questionnaires, Natural language processing
Introduction
The series of ChatGPT (e.g., GPT-3.5 and GPT-4) and other tools based on large language models (LLMs) have initiated the latest wave of chatbots, impacting numerous industries. These powerful chatbots, designed to interpret, generate, and effectively converse with humans, are referred to as GPT (generative pre-trained)-like technologies, such as ChatGPT, Claude, and Google Bard. The development and refining of LLMs have also significantly impacted the field of healthcare [1]. The potential applications of GPT-like technologies in healthcare have garnered significant attention, particularly in areas such as scientific writing and medical education [2–4].
Healthcare is inundated with large amounts of free-text reports, such as radiological reports, which place a significant burden on radiologists. The inconsistencies in style and structure result in variability and complexity in radiological reports, hindering effective communication of information among various medical departments [5]. GPT-like technologies have shown great potential in structuring and correcting errors in free-text radiological reports and providing therapeutic suggestions through these reports [6–9]. Recently, positive conclusions regarding the detection of radiological findings in chest radiographs using GPT-4 with vision capabilities have demonstrated its immense potential in the department of radiology [10, 11]. Therefore, GPT-like technologies have the potential to support clinical workflow, scientific research, and educational applications in the field of radiology [3].
However, ChatGPT-like technologies have not been universally successful across all domains. Some studies indicate that, while GPT-4 demonstrated moderate agreement with human-assigned breast nodule categories, it still produced a high percentage of discordant results, potentially impacting clinical decision-making [12]. Furthermore, while GPT-like models excelled in text-based tasks, issues such as repeatability, demographic biases, and challenges in interpreting radiologic images persisted [13–15]. These limitations underscored critical areas for improvement, highlighting the need for further development before clinical implementation.
The rapid growth of interest in GPT-like technologies in healthcare raised several challenges, particularly regarding ethical concerns and potential risks building on this controversial evidence, such as misdiagnosis or missed diagnoses [2, 16, 17]. Currently, the acceptance and understanding of GPT-like technologies among radiologists are still unclear and need further investigation, which may influence the future deployment of these technologies in the field of radiology. The Zhongda Radiology Alliance, established in 2019, is a collaborative network of radiology academic centers. As of the time of our survey, it includes 264 hospitals across 31 of China’s 34 provinces. Conducting this survey within the framework of the Zhongda Radiology Alliance ensures a highly representative sample of the Chinese radiology community.
Therefore, our study aimed to conduct a comprehensive national survey to elucidate the attitudes and possible influencing factors of Chinese radiologists or interns regarding the use of GPT-like technologies in their clinical practice, medical education, and scientific research.
Materials and methods
This cross-sectional study was approved by the research ethics board and informed consent was acquired from all participants. The study was conducted in accordance with both the Declarations of Helsinki and Istanbul. This study adheres to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Survey time and procedure
The survey was conducted from October 2023 to May 2024. Questionnaires were distributed to members of the Zhongda Radiology Alliance via the survey platform Wenjuanxing (https://www.wjx.cn/) in China. The questionnaires were forwarded to radiologists or interns willing to participate through the directors of the department of radiology. Standard instructions for the questionnaire survey were provided, and appointed people were assigned to be responsible for the distribution, and quality control of the questionnaires. The questionnaires were anonymous, and all items were mandatory to complete.
Questionnaire formulation and survey respondents
The questionnaire was designed after repeated discussions and revisions by hospital management experts, senior radiology experts, and artificial intelligence (AI) algorithm experts (the questionnaire was detailed in Supplemental Materials). The questionnaire comprised three parts. Part-A: basic information included gender, age, province of workplace, hospital level, working history, professional title, scientific research pressure, experience with GPT-like technologies, familiarity with AI, and familiarity with GPT-like technologies. Part B: options on GPT-like technologies, in which the respondents rated their opinion on a Likert scale from 1 (very poor) to 5 (very good) concerning GPT-like technologies in clinical practice (10 items), training and education (9 items), environment and regulation (6 items), and development trends (5 items). Besides, Part C consisted of 2 key questions: 1. Without considering policies and costs, would you be willing to try or continue using GPT-like technologies? (would not; would); and 2. Would you be willing to try or continue using GPT-like technologies? (definitely would not; probably would not; neutral; probably would; definitely would).
All participants completed the survey anonymously without the collection of any identifiers. The respondents were radiologists with registered physician qualifications or interns majoring in radiology in mainland China. A total of 1340 respondents were members of the Zhongda Radiology Alliance from 197 hospitals. For quality control, we empirically excluded the 50 respondents who completed the questionnaire in less than 3 min (Fig. 1). The primary outcome of this study was attitudes toward the adoption of GPT-like technologies, and the secondary outcome was to explore the factors that affect the attitudes.
Fig. 1.
The process and analysis of the survey study
Statistical analysis
Results conforming to a normal distribution were expressed as mean and standard deviation, while categorical data were presented as frequencies and percentages. Results conforming to a non-normal distribution and ordered categorical data were expressed as the median and interquartile range (IQR). The Mann–Whitney U-test, or Chi-square test was performed based on the variable type. Correlations between ordered categorical variables were assessed using Spearman correlation analysis. Univariable and multivariable logistic regression was conducted to identify independent factors, presented with odds ratios (OR) and 95% confidence interval (CI). Variables with a p value < 0.1 and potential bias in the univariate logistic regression analysis were included in the multivariable analysis. The multivariable logistic regression analysis was applied to identify factors associated with radiologists’ attitudes toward the acceptance of GPT-like technologies, using the minimum value of the Akaike Information Criterion. Additionally, stratified analysis was performed as a sensitivity analysis to control the effect of confounders with potential bias.
For sensitivity analysis, we re-divided the acceptance level of GPT-like technologies into two groups: 1–3 degrees vs 4–5 degrees, and 1–4 degrees vs 5 degrees. Multivariable logistic regression analysis was performed as described above for overall items and each of the four dimensions: clinical practice, training and education, environment and regulation, and development tendency. All p values were two-sided, and significance was set at p value < 0.05. Survey data were analyzed using SPSS statistical software version 27.0 (IBM).
Results
Characteristics of the respondents
The study ultimately enrolled 1289 respondents after excluding 50 respondents due to quality control. All respondents completed the survey, and the response rate reached 96.3% without 50 unqualified questionnaires. The respondents were from 197 hospitals in 27 provinces, with a median age of 37.0 years (IQR, 31.0–44.0 years) and a median working history of 12 years (IQR, 7–21 years). Among them, 813 were males. A majority of respondents (1066, 82.7%) were from tertiary hospitals. The professional titles were distributed as follows: 438 (34.0%) were associate chief or chief radiologists, 508 (39.4%) were attending radiologists, and 343 (26.6%) were interns or residents. Notably, 125 respondents (9.7%) reported prior experience with GPT-like technologies. Respondents experiencing greater scientific research pressure (p = 0.03), having a longer working history (p = 0.04), or holding higher professional titles (p = 0.02) were more likely to try and continue using GPT-like technologies. One thousand two hundred twenty-three (94.9%) respondents expressed support for GPT-like technologies (Fig. 2A). Based on the acceptance level, the respondents were distributed as 3 (0.2%), 29 (2.2%), 352 (27.3%), 677 (52.5%), and 228 (17.7%) from low to high acceptance degrees of GPT-like technologies (Fig. 2B). Detailed characteristics of the respondents are provided in Table 1.
Fig. 2.
Bar graphs depicting respondents’ attitudes toward the adoption of GPT-like technologies based on two key questions (Supplemental Materials). A represents attitudes categorized into two categories, while B represents attitudes based on a 5-point ordinal scale. GPT, generative pre-trained
Table 1.
Characteristics of the respondents (n = 1289)
| Characteristics | Respondents (n = 1289) | Opponents (n = 66) | Supporters (n = 1223) | p value |
|---|---|---|---|---|
| Sex | 0.53 | |||
| Female | 476 (36.9) | 22 (33.3) | 454 (37.1) | |
| Male | 813 (63.1) | 44 (66.7) | 769 (62.9) | |
| Age (years)* | 37.0 (31.0–44.0) | 35.0 (29.8–40.0) | 37.0 (31.0–44.0) | 0.051† |
| Region | 0.42 | |||
| Northeast | 59 (4.6) | 3 (4.5) | 56 (4.6) | |
| North | 136 (10.6) | 9 (13.6) | 127 (10.4) | |
| East | 459 (35.6) | 15 (22.7) | 444 (36.3) | |
| Southern | 30 (2.3) | 1 (1.5) | 29 (2.4) | |
| Central | 158 (12.3) | 11 (16.7) | 147 (12) | |
| Northwest | 58 (4.5) | 3 (4.5) | 55 (4.5) | |
| Southwest | 389 (30.2) | 24 (36.4) | 365 (29.8) | |
| Hospital level | 0.13 | |||
| Tertiary | 1066 (82.7) | 50 (75.8) | 1016 (83.1) | |
| Others | 223 (17.3) | 16 (24.2) | 207 (16.9) | |
| Working history (years)* | 12.0 (7.0–21.0) | 10.0 (6.0–17.0) | 12.0 (7.0–21.0) | 0.04† |
| Professional title | 0.02† | |||
| Intern or resident | 343 (26.6) | 23 (34.8) | 320 (26.2) | |
| Attending | 508 (39.4) | 29 (43.9) | 479 (39.2) | |
| Associate chief or chief | 438 (34.0) | 14 (21.2) | 424 (34.7) | |
| Academic pressure | 0.24† | |||
| None | 269 (20.9) | 21 (31.8) | 248 (20.3) | |
| Mild | 249 (19.3) | 7 (10.6) | 242 (19.8) | |
| Moderate | 367 (28.5) | 21 (31.8) | 346 (28.3) | |
| Moderately severe | 186 (14.4) | 6 (9.1) | 180 (14.7) | |
| Severe | 218 (16.9) | 11 (16.7) | 207 (16.9) | |
| Used experience with GPT-like technologies | 0.86 | |||
| Yes | 125 (9.7) | 6 (9.1) | 119 (9.7) | |
| No | 1164 (90.3) | 60 (90.9) | 1104 (90.3) | |
| Knowledge of NLP or AI technologies | 0.27† | |||
| No understanding | 110 (8.5) | 9 (13.6) | 101 (8.3) | |
| Limited understanding | 291 (22.6) | 16 (24.2) | 275 (22.5) | |
| Basic understanding | 425 (33.0) | 19 (28.8) | 406 (33.2) | |
| Good understanding | 456 (35.4) | 22 (33.3) | 434 (35.5) | |
| Excellent understanding | 7 (0.5) | 0 (0.0) | 7 (0.6) | |
| Knowledge of GPT-like technologies | 0.29† | |||
| No understanding | 218 (16.9) | 16 (24.2) | 202 (16.5) | |
| Limited understanding | 556 (43.1) | 24 (36.4) | 532 (43.5) | |
| Basic understanding | 427 (33.1) | 25 (37.9) | 402 (32.9) | |
| Good understanding | 62 (4.8) | 0 (0.0) | 62 (5.1) | |
| Excellent understanding | 26 (2.0) | 1 (1.5) | 25 (2.0) | |
| Acceptance level of GPT-like technologies | < 0.001† | |||
| Definitely would not | 3 (0.2) | 3 (4.5) | 0 (0.0) | |
| Probably would not | 29 (2.2) | 8 (12.1) | 21 (1.7) | |
| Neutral | 352 (27.3) | 45 (68.2) | 307 (25.1) | |
| Probably would | 677 (52.5) | 10 (15.2) | 667 (54.5) | |
| Definitely would | 228 (17.7) | 0 (0.0) | 228 (18.6) |
Unless otherwise specified, data are numbers of patients, with percentages in parentheses
AI artificial intelligence, GPT generative pre-trained, NLP natural language processing
* Data are medians, with IQRs in parentheses
† p value calculated by Mann–Whitney U-test
Attitudes of the respondents toward the acceptance of GPT-like technologies
The distribution of responses to 30 questions (Q1–Q30) from Part B of the questionnaire, which pertains to the attitudes of respondents towards GPT-like technologies, is presented in Fig. 3. The majority of items showed a clear trend where most respondents chose either a positive response (4–5 degrees) or a neutral response (3 degrees), indicating overall optimistic opinions regarding the potential capabilities of GPT-like technologies. Differences in attitudes towards GPT-like technologies between the opponents and supporters were observed in most items from Part B (Supplementary Table 1). Additionally, correlation analysis showed positive correlations between a majority of items and attitudes toward GPT-like technologies (Supplementary Table 2).
Fig. 3.
The acceptance of GPT-like technologies distribution of respondents’ answers to questions 1–30 from Part B of the questionnaire. Bar graphs show a positive trend where the majority of respondents chose a positive or neutral response (3–5 degrees) at most items. Details of the questions can be found in Supplemental Materials. GPT, generative pre-trained
Univariable binary logistic regression analysis comprehensively assessed the possible factors associated with radiologists’ acceptance of GPT-like technologies. Our findings revealed that a longer working history was significantly associated with higher acceptance rates (OR = 1.03; 95% CI: 1.00, 1.06; p = 0.03), indicating that more experienced radiologists may be more willing to adopt GPT-like technologies. Furthermore, the univariable analysis showed that respondents’ positive attitudes towards GPT-like technologies were influenced by optimistic opinions in the four dimensions of clinical practice, training and education, environment and regulation, and development tendency (Table 2).
Table 2.
Binary logistic regression analysis of variables for the association with acceptance of GPT-like technologies (n = 1289)
| Factors* | Univariable analysis | Multivariable analysis | ||
|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Age (years) | 1.03 (0.99, 1.06) | 0.06 | ||
| Working history (years) | 1.03 (1.00, 1.06) | 0.03 | ||
| Q1 (Assisting in writing radiological reports) | 1.78 (1.27, 2.47) | < 0.001 | ||
| Q2 (Improving doctor-patient communication) | 1.35 (0.99, 1.83) | 0.06 | ||
| Q3 (Improving patient triage and treatment) | 1.61 (1.19, 2.17) | 0.002 | ||
| Q4 (Impact on the radiology department) | 1.70 (1.24, 2.32) | < 0.001 | ||
| Q5 (Using in emergencies) | 1.65 (1.19, 2.27) | 0.003 | ||
| Q6 (Producing misleading diagnostic results) | 1.04 (0.74, 1.47) | 0.82 | ||
| Q7 (Role in medical image diagnosis) | 1.67 (1.22, 2.30) | 0.002 | ||
| Q8 (Providing personalized treatment advice) | 1.58 (1.15, 2.17) | 0.005 | ||
| Q9 (Reducing the radiological reporting writing time) | 1.67 (1.18, 2.34) | 0.004 | ||
| Q10 (Improving efficiency in radiology emergency shifts) | 2.16 (1.56, 2.99) | < 0.001 | ||
| Q11 (Accurate medical information) | 1.87 (1.21, 2.89) | 0.005 | ||
| Q12 (Diagnostic advice in rare or complex cases) | 1.35 (1.01, 1.81) | 0.045 | ||
| Q13 (Improving radiology education effectiveness) | 1.72 (1.23, 2.38) | 0.001 | ||
| Q14 (Writing papers and language polishing) | 3.36 (2.56, 4.41) | < 0.001 | 1.99 (1.34, 2.95) | < 0.001 |
| Q15 (Designing research topics) | 2.62 (2.01, 3.42) | < 0.001 | ||
| Q16 (Designing patents) | 2.30 (1.79, 2.96) | < 0.001 | ||
| Q17 (Editing research and statistics code) | 2.65 (2.03, 3.46) | < 0.001 | ||
| Q18 (Enhancing disease understanding) | 3.99 (2.87, 5.54) | < 0.001 | ||
| Q19 (GPT-like tech training in medical education) | 2.69 (2.04, 3.56) | < 0.001 | ||
| Q20 (Leading to medical disputes) | 0.90 (0.69, 1.17) | 0.43 | ||
| Q21 (Threat to radiologists’ jobs) | 1.11 (0.85, 1.46) | 0.44 | ||
| Q22 (Privacy leak of patients) | 1.03 (0.77, 1.37) | 0.87 | ||
| Q23 (Effect of colleagues using) | 3.30 (2.47, 4.41) | < 0.001 | 1.77 (1.17, 2.68) | 0.007 |
| Q24 (Introducing regulation from the government) | 3.65 (2.66, 5.02) | < 0.001 | 2.25 (1.56, 3.22) | < 0.001 |
| Q25 (Supervising in medicine) | 1.79 (1.34, 2.35) | < 0.001 | ||
| Q26 (Widely used in hospitals in the future) | 1.74 (1.26, 2.41) | < 0.001 | ||
| Q27 (Impact on doctors’ employment) | 1.19 (0.91, 1.56) | 0.20 | ||
| Q28 (Application in the medicine in next decade) | 1.56 (1.17, 2.08) | 0.003 | ||
| Q29 (Enhancing decision support capabilities) | 5.01 (3.40, 7.36) | < 0.001 | 2.67 (1.58, 4.49) | < 0.001 |
| Q30 (Application in the medical industry) | 3.95 (2.67, 5.84) | < 0.001 | ||
Unless otherwise specified, Data in parentheses are 95% CIs. The multivariable analysis included variables with a p value < 0.1 and potential bias (used experience with GPT-like technologies, knowledge of NLP/AI technologies and GPT-like technologies)
AI artificial intelligence, CI confidence interval, GPT generative pre-trained, NLP natural language processing, OR odds ratio
* Summary of the item are shown in parentheses, the details of the items can be found in the Supplementary File
After adjusting other factors with p < 0.1, the multivariable binary logistic regression analysis identified several key questions associated with the acceptance of GPT-like technologies: Q14 (Writing papers and language polishing) (OR = 1.99; 95% CI: 1.34, 2.95; p < 0.001), Q23 (Effect of colleagues using) (OR = 1.77; 95% CI: 1.17, 2.68; p < 0.007), Q24 (Introducing regulation from the government) (OR = 2.25; 95% CI: 1.56, 3.22; p < 0.001), and Q29 (Enhancing decision support capabilities) (OR = 2.67; 95% CI: 1.58, 4.49; p < 0.001). Figure 4 displays a histogram comparing responses to these four questions between supporters and opponents of GPT-like technologies.
Fig. 4.
Bar graphs show the cumulative percentage of respondents’ answers to questions 14, 23, 24, and 29. As the response level increases to these questions, the support tendency for GPT-like technologies increases (p < 0.001). Details of questions 14, 23, 24, and 29 can be found in Supplemental Materials. GPT, generative pre-trained
To more accurately describe the acceptance of GPT-like technologies, we included two questions with 2 and 5 categories for acceptance level. The relationship between these two key questions is shown in Table 1 and Fig. 5 (p < 0.001). Sensitivity analyses were conducted to gain deeper insights into the factors associated with acceptance level. Regardless of whether the acceptance was categorized as 1–3 degrees vs 4–5 degrees or 1–4 degrees vs 5 degrees, the four items (Q14, Q23, Q24, and Q29) were still the independent factors associated with higher acceptance levels in multivariable analysis (all p < 0.001) (Table 3). Given the experience of use experience of GPT-like technologies and the level of knowledge about AI and GPT-like technologies, there may be potential bias. In the subgroup analysis, all four items (Q14, Q23, Q24, and Q29) demonstrated a significant positive association across all groups, as detailed in Table 4.
Fig. 5.
Bar graphs show the cumulative percentage between the key questions about the acceptance and acceptance level of GPT-like technologies (p < 0.001). GPT, generative pre-trained
Table 3.
Binary logistic regression analysis of variables for the association with an acceptance level of GPT-like technologies at questions 14, 23, 24, and 29 (n = 1289)
| Factors* | Acceptance level (1–3 degrees vs 4–5 degrees) | Acceptance level (1–4 degrees vs 5 degrees) | ||||||
|---|---|---|---|---|---|---|---|---|
| Univariable analysis | Multivariable analysis | Univariable analysis | Multivariable analysis | |||||
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Q14 | 5.07 (4.05, 6.35) | < 0.001 | 1.84 (1.41, 2.41) | < 0.001 | 9.27 (6.51, 13.21) | < 0.001 | 2.02 (1.35, 3.03) | < 0.001 |
| Q23 | 17.00 (12.59, 22.97) | < 0.001 | 8.47 (6.17, 11.61) | < 0.001 | 25.50 (17.58, 36.99) | < 0.001 | 12.50 (8.30, 18.84) | < 0.001 |
| Q24 | 3.94 (3.18, 4.87) | < 0.001 | 2.11 (1.61, 2.78) | < 0.001 | 5.64 (4.25, 7.47) | < 0.001 | 1.92 (1.33, 2.77) | < 0.001 |
| Q29 | 6.21 (4.86, 7.94) | < 0.001 | 2.50 (1.84, 3.41) | < 0.001 | 7.75 (5.70, 10.53) | < 0.001 | 2.11 (1.45, 3.06) | < 0.001 |
Unless otherwise specified, Data in parentheses are 95% CIs
CI confidence interval, GPT generative pre-trained, OR odds ratio
* The details of questions 14, 23, 24, and 29 can be found in the Supplementary File
Table 4.
Binary logistic regression analysis of variables for the association with acceptance of GPT-like technologies at questions 14, 23, 24, and 29 in different subgroups (n = 1289)
| Subgroup | Q14 OR (95% CI) | Q23 OR (95% CI) | Q24 OR (95% CI) | Q29 OR (95% CI) |
|---|---|---|---|---|
| Used experience with GPT-like technologies | ||||
| Yes | 3.36 (1.28, 8.82) | 2.63 (1.07, 6.49) | 3.61 (1.35, 9.66) | 6.61 (1.65, 26.55) |
| No | 3.36 (2.53, 4.47) | 3.38 (2.49, 4.60) | 3.66 (2.62, 5.12) | 4.88 (3.27, 7.29) |
| Knowledge of NLP or AI technologies | ||||
| No to limited understanding | 3.60 (2.25, 5.77) | 3.15 (1.95, 5.09) | 3.01 (1.80, 5.04) | 4.39 (2.34, 8.14) |
| Basic to excellent understanding | 3.23 (2.30, 4.52) | 3.37 (2.34, 4.85) | 4.05 (2.70, 6.07) | 5.37 (3.28, 8.81) |
| Knowledge of GPT-like technologies | ||||
| No to limited understanding | 3.62 (2.50, 5.24) | 3.28 (2.28, 4.72) | 2.94 (1.89, 4.56) | 4.92 (2.98, 8.12) |
| Basic to excellent understanding | 3.07 (2.04, 4.61) | 3.36 (2.07, 5.44) | 4.68 (2.90, 7.57) | 5.14 (2.81, 9.43) |
Unless otherwise specified, Data in parentheses are 95% CIs
AI artificial intelligence, CI confidence interval, GPT generative pre-trained, NLP natural language processing, OR odds ratio
The main factors affecting the attitude toward the acceptance of GPT-like technologies in each dimension
To further elucidate the multi-faceted views of radiologists’ attitudes toward GPT-like technologies, we conducted a multivariable logistic regression analysis to identify factors significantly associated with acceptance and different levels of acceptance across four dimensions. Table 5 shows the independent factors affecting the acceptance of GPT-like technologies in each dimension.
Table 5.
Binary logistic regression analysis of variables for the association with acceptance of GPT-like technologies based on each dimension (n = 1289)
| Factors* | Acceptance (no vs yes) | Acceptance level (1–3 degrees vs 4–5 degrees) | Acceptance level (1–4 degrees vs 5 degrees) | |||
|---|---|---|---|---|---|---|
| OR (95% CI) | p value | OR (95% CI) | p value | OR (95% CI) | p value | |
| Clinical practice | ||||||
| Q7 (Role in medical image diagnosis) | 1.27 (1.03, 1.56) | 0.02 | ||||
| Q9 (Reducing the radiology reporting writing time) | 1.49 (1.14, 1.95) | 0.003 | ||||
| Q10 (Improving efficiency in radiology emergency shifts) | 2.16 (1.56, 2.99) | < 0.001 | 1.74 (1.43, 2.11) | < 0.001 | 1.45 (1.12, 1.88) | 0.005 |
| Training and education | ||||||
| Q14 (Writing papers and language polishing) | 2.39 (1.71, 3.32) | < 0.001 | 2.94 (1.93, 4.94) | < 0.001 | ||
| Q15 (Designing research topics) | 1.53 (1.13, 2.07) | 0.005 | ||||
| Q16 (Designing patents) | 1.86 (1.37, 2.53) | < 0.001 | ||||
| Q18 (Enhancing disease understanding) | 2.36 (1.56, 3.57) | < 0.001 | 7.67 (5.58, 10.56) | < 0.001 | 5.90 (3.92, 8.90) | < 0.001 |
| Q19 (GPT-like tech training in medical education) | 1.50 (1.05, 2.14) | 0.03 | 2.02 (1.54, 2.64) | < 0.001 | 3.65 (2.41, 5.54) | < 0.001 |
| Environment and regulation | ||||||
| Q23 (Effect of colleagues using) | 2.66 (1.91, 3.70) | < 0.001 | 12.84 (9.42, 17.50) | < 0.001 | 19.19 (13.06, 28.18) | < 0.001 |
| Q24 (Introducing regulation from the government) | 2.61 (1.85, 3.68) | < 0.001 | 1.99 (1.51, 2.62) | < 0.001 | 2.41 (1.71, 3.41) | < 0.001 |
| Q25 (Supervising in medicine) | 1.50 (1.23, 1.84) | < 0.001 | ||||
| Development tendency | ||||||
| Q28 (Application in the medicine in next decade) | 1.38 (1.16, 1.65) | < 0.001 | 1.46 (1.17, 1.82) | < 0.001 | ||
| Q29 (Enhancing radiologists’ decision support capabilities) | 4.45 (2.94, 6.75) | < 0.001 | 4.21 (3.28, 5.42) | < 0.001 | 4.47 (3.21, 6.23) | < 0.001 |
| Q30 (Application in the medical industry) | 2.53 (1.69, 3.77) | < 0.001 | 5.48 (3.81, 7.89) | < 0.001 | 6.83 (4.66, 10.03) | < 0.001 |
Unless otherwise specified, Data in parentheses are 95% CIs
CI confidence interval, GPT generative pre-trained, OR odds ratio
* Summary of the item are shown in parentheses, the details of the items can be found in the Supplementary File
In the dimension of clinical practice, radiologists’ opinions on the role of GPT-like technologies in medical image diagnosis (OR = 1.27; p = 0.02) and their ability to reduce radiology report writing time (OR = 1.49; p = 0.003) were associated with higher levels of acceptance of GPT-like technologies. Notably, positive opinions on improving efficiency in radiology emergency shifts demonstrated the strongest association with the acceptance of GPT-like technologies (all p < 0.05).
Regarding training and education, enhancing disease understanding of GPT-like technologies (OR = 2.36; p < 0.001) and incorporating GPT-like technologies training in medical education (OR = 1.50; p = 0.03) were strongly related to acceptance. Besides, the capability of GPT-like technologies in writing papers and language polishing, designing research topics, and designing patents were also potential factors contributing to positive attitudes toward GPT-like technologies (all p < 0.05).
For environment and regulation, the influence of colleagues using GPT-like technologies (OR = 2.66; p < 0.001) and the introduction of government regulation for GPT-like technologies (OR = 2.61; p < 0.001) were the most significant factors for a positive attitude. Supervising in healthcare also showed significance in the analysis of acceptance level (1–3 degrees vs 4–5 degrees) (OR = 1.50; p < 0.001).
Concerning the dimension of development tendency, positive opinions on the enhancement of decision support capabilities by GPT-like technologies and their application in the medical industry were the most influential factors for respondents’ positive attitude towards trying or continuing to use the GPT-like technologies (all p < 0.001).
Discussion
GPT-like technologies have experienced rapid growth and garnered significant attention in radiology [1, 2, 4]. The advent of GPT has infused new energy into the field of radiology, but it has also raised new concerns, making radiologists’ opinions on these technologies crucial. Our study conducted a national survey of Chinese radiologists and interns at the Zhongda Radiology Alliance with a 96.3% response rate, revealing that the majority of the 1223 respondents (94.9% of 1289) from 197 hospitals in 27 provinces expressed support for trying or continuing to use GPT-like technologies. Furthermore, we identified several factors significantly associated with the acceptance of GPT-like technologies, including writing papers and language polishing, the effect of colleagues using such technologies, introducing regulation from the government, and enhancing decision support capabilities (all p < 0.001).
The Zhongda Radiology Alliance offered a unique advantage for this survey, as it spans a wide geographic area and includes a diverse range of hospitals across China. The alliance provided a high representation of the radiology community. This diversity ensured that the findings reflected the perspectives of radiologists from various settings, making the results more generalizable. The increasing demand for imaging examinations has outpaced the availability of skilled radiologists, intensifying the workload and increasing the likelihood of errors in radiology [18]. Previous studies have shown that integrating GPT-like technologies into clinical practice has the potential to structure and detect errors in radiological reports with a high cost-benefit ratio [8, 9]. In the clinical practice dimension, respondents who believed GPT-like technologies could enhance medical image diagnosis and reduce report writing time were more likely to accept them (p = 0.02–0.003). Additionally, their potential to improve efficiency during radiology emergency shifts was crucial to acceptance (all p < 0.05). Another study reported that GPT-4 achieved an accuracy of 0.88 in assessing clinical acuity in the department of emergency, compared to human accuracy of 0.86 [19]. The strong association between the belief in improved decision support (all p < 0.001) and the acceptance of GPT-like technologies underscores their critical role in clinical judgment and decision-making. Analyses of LLMs have concluded that these models can provide appropriate imaging examination suggestions and aid in surgical decision-making [6, 7, 20].
The integration of GPT-like technologies into medical education and scientific research presents a transformative opportunity for radiologists [2, 4]. In a survey study, over two-thirds of 263 medical students agreed on the need for AI to be included in medical training [21]. Focusing on the education dimension, our study demonstrated a positive association with the high acceptance level of GPT-like technologies, particularly in writing papers and language polishing, designing research topics and patents, and enhancing disease understanding (p < 0.05). Recently, the use of tools based on LLMs for polishing scientific work has become acceptable, though it raises dilemmas regarding originality and inexpressiveness [1]. These tools have also been used to assess the risk of bias in randomized clinical trials, achieving high correct assessment rates [22]. However, recent studies have also revealed limitations of GPT-like technologies in terms of general performance in radiological knowledge [23]. Indeed, respondents expressed significant concern about the accuracy of medical information provided by these technologies (p = 0.005 in univariable analysis). Training in GPT-like technologies within medical education was identified as an important factor associated with a positive attitude (all p < 0.03). However, the performance of ChatGPT-like technologies at direct imaging interpretation may not be as accurate as expected [12–15]. This could pose risks to both education and clinical practice, potentially increasing the likelihood of errors and negatively impacting patient care.
Additionally, GPT-like technologies introduce a set of challenges that must be addressed to ensure their responsible and effective use, such as medical malpractice liability, privacy, and others [16, 17]. Legal regulation is a key challenge for LLMs. Our results show that government regulations were strongly associated with tool acceptance (all p < 0.001), highlighting the need for developer-regulator collaboration. Additionally, the influence of colleagues using GPT-like technologies was a major factor in fostering a positive attitude (all p < 0.001). Future regulations for LLMs remain an unmet need and should aim to strike a balance between promoting efficiency and mitigating potential risks, with a focus on flexible, forward-looking frameworks that safeguard both societal and individual interests [24]. In our study, respondents expressed a moderately optimistic opinion about the future medical application of GPT-like technologies. A 2021 survey revealed that only 48% (501 of 1041) of radiologists had a positive attitude toward AI, which contrasts with our findings in China [25]. This discrepancy may arise from differences in survey populations or the focus on GPT-like technologies in our study. Additionally, recent AI integration in radiology may have reduced workload, enhancing radiologists’ confidence.
There were several limitations in this study. First, it is a cross-sectional study, and the participants were members of the Zhongda Radiology Alliance, which may not be representative of radiologists worldwide. None of the respondents were engaged in ultrasound diagnosis. Second, only 125 (9.7%) of the 1289 respondents had prior experience with GPT-like technologies, and most respondents may have had an inaccurate understanding of these technologies due to a lack of direct experience. Third, the survey was conducted over seven months and did not focus on a specific GPT-like tool. Thus, it is important to interpret the results with caution.
Conclusions
Our study highlights that most radiologists or interns in mainland China display a favorable attitude toward incorporating GPT-like technologies into their clinical practice and research. This favorable attitude is driven by the popularity and superior capabilities of GPT-like technologies for scientific writing and decision support. Additionally, the establishment of sound regulations emerges as a pivotal factor in the application of GPT-like technologies in radiology.
Supplementary information
Acknowledgements
We express our gratitude to the members of the Zhongda Radiology Alliance for participating in this survey.
Abbreviations
- AI
Artificial intelligence
- GPT
Generative pre-trained
- LLM
Large language model
Author contributions
T.X. and S.Z. contributed equally to the design of the work and were responsible for the data analyses and the first draft of the paper. B.Z. and Y.L were responsible for the data collection and cleaning. Z.X., Y.S., and B.C. were responsible for the statistical advice and questionnaire design. J.Z., Y.Y., Z.W. were response for the questionnaire distribution and article modification. C.L. was responsible for making the figures. T.T., Y.W., and S.J. were responsible for study supervision and quality control. All the authors read and approved the final manuscript.
Funding
This study has received funding from the National Natural Science Foundation of China (NSFC, no. 823B2040, 92359304, 82330060, 82427803, and 82371940).
Data availability
The related data can be obtained by contacting the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
The Institutional Review Board of Shanghai General Hospital approved this prospective study (Medical ethics number: 2024ZDSYLL274-P01). Written informed consent was obtained from all subjects in this study.
Consent for publication
Not applicable.
Competing interests
Y.S. is affiliated with Siemens Healthineers Ltd. The remaining authors declare that they have no competing interests.
Footnotes
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Tianyi Xia and Shijun Zhang contributed equally to this work.
Supplementary information
The online version contains supplementary material available at 10.1186/s13244-025-01908-8.
References
- 1.Thirunavukarasu AJ, Ting DSJ, Elangovan K, Gutierrez L, Tan TF, Ting DSW (2023) Large language models in medicine. Nat Med 29:1930–1940 [DOI] [PubMed] [Google Scholar]
- 2.Kataoka Y, So R (2023) Benefits, limits, and risks of GPT-4 as an AI Chatbot for medicine. N Engl J Med 388:2399 [DOI] [PubMed] [Google Scholar]
- 3.Lecler A, Duron L, Soyer P (2023) Revolutionizing radiology with GPT-based models: current applications, future possibilities and limitations of ChatGPT. Diagn Interv Imaging 104:269–274 [DOI] [PubMed] [Google Scholar]
- 4.Bhayana R (2024) Chatbots and large language models in radiology: a practical primer for clinical and research applications. Radiology 310:e232756 [DOI] [PubMed] [Google Scholar]
- 5.Schwartz LH, Panicek DM, Berk AR, Li Y, Hricak H (2011) Improving communication of diagnostic radiology findings through structured reporting. Radiology 260:174–181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bhayana R, Nanda B, Dehkharghanian T et al (2024) Large language models for automated synoptic reports and resectability categorization in pancreatic cancer. Radiology 311:e233117 [DOI] [PubMed] [Google Scholar]
- 7.Lehnen NC, Dorn F, Wiest IC et al (2024) Data extraction from free-text reports on mechanical thrombectomy in acute ischemic stroke using ChatGPT: a retrospective analysis. Radiology 311:e232741 [DOI] [PubMed] [Google Scholar]
- 8.Adams LC, Truhn D, Busch F et al (2023) Leveraging GPT-4 for post hoc transformation of free-text radiology reports into structured reporting: a multilingual feasibility study. Radiology 307:e230725 [DOI] [PubMed] [Google Scholar]
- 9.Gertz RJ, Dratsch T, Bunck AC et al (2024) Potential of GPT-4 for detecting errors in radiology reports: implications for reporting accuracy. Radiology 311:e232714 [DOI] [PubMed] [Google Scholar]
- 10.Suh PS, Shim WH, Suh CH et al (2024) Comparing diagnostic accuracy of radiologists versus GPT-4V and gemini pro vision using image inputs from diagnosis please cases. Radiology 312:e240273 [DOI] [PubMed] [Google Scholar]
- 11.Zhou Y, Ong H, Kennedy P et al (2024) Evaluating GPT-V4 (GPT-4 with vision) on detection of radiologic findings on chest radiographs. Radiology 311:e233270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cozzi A, Pinker K, Hidber A et al (2024) BI-RADS category assignments by GPT-3.5, GPT-4, and google bard: a multilanguage study. Radiology 311:e232133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayden N, Gilbert S, Poisson LM, Griffith B, Klochko C (2024) Performance of GPT-4 with vision on text- and image-based ACR diagnostic radiology in-training examination questions. Radiology 312:e240153 [DOI] [PubMed] [Google Scholar]
- 14.Santomartino SM, Zech JR, Hall K, Jeudy J, Parekh V, Yi PH (2024) Evaluating the performance and bias of natural language processing tools in labeling chest radiograph reports. Radiology 313:e232746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sun SH, Huynh K, Cortes G et al (2024) Testing the ability and limitations of ChatGPT to generate differential diagnoses from transcribed radiologic findings. Radiology 313:e232346 [DOI] [PubMed] [Google Scholar]
- 16.Mesko B, Topol EJ (2023) The imperative for regulatory oversight of large language models (or generative AI) in healthcare. NPJ Digital Med 6:120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ong JCL, Chang SY, William W et al (2024) Ethical and regulatory challenges of large language models in medicine. Lancet Digital Health 6:e428–e432 [DOI] [PubMed] [Google Scholar]
- 18.Alexander R, Waite S, Bruno MA et al (2022) Mandating limits on workload, duty, and speed in radiology. Radiology 304:274–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Williams CYK, Zack T, Miao BY et al (2024) Use of a large language model to assess clinical acuity of adults in the emergency department. JAMA Netw Open 7:e248895 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gertz RJ, Bunck AC, Lennartz S et al (2023) GPT-4 for automated determination of radiological study and protocol based on radiology request forms: a feasibility study. Radiology 307:e230877 [DOI] [PubMed] [Google Scholar]
- 21.Pinto Dos Santos D, Giese D, Brodehl S et al (2019) Medical students’ attitude towards artificial intelligence: a multicentre survey. Eur Radiol 29:1640–1646 [DOI] [PubMed] [Google Scholar]
- 22.Lai H, Ge L, Sun M et al (2024) Assessing the risk of bias in randomized clinical trials with large language models. JAMA Netw Open 7:e2412687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bhayana R, Krishna S, Bleakney RR (2023) Performance of ChatGPT on a radiology board-style examination: insights into current strengths and limitations. Radiology 307:e230582 [DOI] [PubMed] [Google Scholar]
- 24.Freyer O, Wiest IC, Kather JN, Gilbert S (2024) A future role for health applications of large language models depends on regulators enforcing safety standards. Lancet Digital Health 6:e662–e672 [DOI] [PubMed] [Google Scholar]
- 25.Huisman M, Ranschaert E, Parker W et al (2021) An international survey on AI in radiology in 1,041 radiologists and radiology residents part 1: fear of replacement, knowledge, and attitude. Eur Radiol 31:7058–7066 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The related data can be obtained by contacting the corresponding author upon reasonable request.