Abstract
Background
Psychoeducation positively influences the psychological components of chronic low back pain (CLBP) in conventional treatments. The digitalization of health care has led to the discussion of virtual reality (VR) interventions. However, CLBP treatments in VR have some limitations due to full immersion. In comparison, augmented reality (AR) supplements the real world with virtual elements involving one’s own body sensory perception and can combine conventional and VR approaches.
Objective
The aim of this study was to review the state of research on the treatment of CLBP through psychoeducation, including immersive technologies, and to formulate suggestions for psychoeducation in AR for CLBP.
Methods
A scoping review following PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines was performed in August 2024 by using Livivo ZB MED, PubMed, Web of Science, American Psychological Association PsycINFO (PsycArticle), and PsyArXiv Preprints databases. A qualitative content analysis of the included studies was conducted based on 4 deductively extracted categories.
Results
We included 12 studies published between 2019 and 2024 referring to conventional and VR-based psychoeducation for CLBP treatment, but no study referred to AR. In these studies, educational programs were combined with physiotherapy, encompassing content on pain biology, psychological education, coping strategies, and relaxation techniques. The key outcomes were pain intensity, kinesiophobia, pain catastrophizing, degree of disability, quality of life, well-being, self-efficacy, depression, attrition rate, and user experience. Passive, active, and gamified strategies were used to promote intrinsic motivation from a psychological point of view. Regarding user experience from a software development perspective, user friendliness, operational support, and application challenges were recommended.
Conclusions
For the development of a framework for an AR-based psychoeducational intervention for CLBP, the combination of theories of acceptance and use of technologies with insights from health psychological behavior change theories appears to be of great importance. An example of a theory-based design of a psychoeducation intervention in AR for CLBP is proposed and discussed.
Keywords: augmented reality, virtual reality, chronic low back pain, education, pain management, intervention
Introduction
Globally, 60%-80% of adults experience low back pain, with 10% developing chronic forms, of which 85% are classified as chronic nonspecific low back pain without a clear etiology [1]. Owing to the limited efficacy and adverse effects of pharmacological approaches, there is a need for nonpharmacological alternatives [2] to improve treatment outcomes [3] and develop effective behavioral interventions [4]. Treatment guidelines recommend behavioral modification, exercise, psychoeducation [5-7], and physiotherapy for trunk muscle strengthening [8-11] to reduce pain and disability.
Educational interventions for chronic low back pain (CLBP) provide knowledge about the condition, coping strategies, and physical activity [3,12], with the objective of enhancing the quality of life and symptom management by mitigating anxiety, kinesiophobia, hyperactive pain behavior, and depression, which are risk factors for pain chronification. Additionally, psychoeducation fosters self-efficacy to break the cycle between anxiety and pain [13,14].
Many traditional interventions to boost physical activity, which is key for CLBP treatment, rely on intention theories for modifying health behavior [15]. A prominent intention theory is the Unified Theory of Acceptance and Use of Technology 2 (UTAUT 2) by Venkatesh et al [16], which examines the acceptance and use of technologies. It has gained recognition in fields such as education, e-commerce, and health research with advancing health technology [17,18]. UTAUT 2 explains the formation of intention for technology use through the constructs of performance expectancy, effort expectancy, social influence, facilitating conditions, hedonic motivation, price value, and habit. These factors may also be useful for predicting the intentions of patients with CLBP toward educational technology adoption. Furthermore, insights from theories focusing on health behavior change may prove fruitful to consider when attempting to change health behavior through the use of a new technology. For instance, Schwarzer’s Health Action Process Approach model [19], commonly used in health behavior interventions, highlights self-efficacy and outcome expectation. The Health Action Process Approach distinguishes between intention formation and implementation as well as between nonintenders, intenders, and actors, each requiring tailored interventions to promote self-efficacy, information, and support in implementation [20]. Another example is Michie’s Behavior Change Technique (BCT) taxonomy with 93 BCTs outlining strategies for successful behavior change [21].
Immersive technologies can be characterized on the Reality-Virtuality Continuum by Milgram and Kishino [22]. They demonstrate visual display technologies ranging from real to virtual environments, including augmented reality (AR) and virtual reality (VR) [23-25]. AR enables the concurrent presence and interaction of digital and physical elements within real-world environments in real time. VR, in contrast, enables complete immersion in VR and represents the extreme of Milgram’s continuum between reality and virtuality [26].
With regard to research in immersive technologies such as VR in the treatment of CLBP, VR-based treatments turned out to be promising in reducing acute, experimental, and chronic pain and can complement conventional CLBP treatments [27].
VR has proven effective in treating acute pain [24] by redirecting attention from unpleasant stimuli such as back pain to more pleasant visual, auditory, and tactile stimuli [27]. VR interventions were found to reduce pain intensity, catastrophizing symptoms, and psychological symptoms in patients with CLBP after one session through distraction, indicating the direct influence of VR on pain perception [26]. Other VR studies demonstrated the feasibility and efficacy of VR for CLBP as an alternative approach, such as VR applications with graded exposure during walking and grasping with integrated game design [28], self-administered VR therapy for CLBP at home [29], and its implementation even during COVID-19 [30]. A recent meta-analysis also showed that kinesiophobia and pain intensity in CLBP can be reduced through VR training [31].
Although there is some evidence for the safety and tolerability of VR treatment for CLBP, most studies lack methodological quality and results were limited to short-term effects. Studies on safety, acceptance, and satisfaction are lacking, including targeted investigations of the risks of spinal pain caused by VR [32]. Thus, while VR is promising in reducing CLBP symptoms, AR might offer additional benefits through the integration of physical and virtual elements, thereby reducing VR-associated discomfort. AR enables the coexistence and interaction of virtual and physical objects in real time in the real world, thus combining the advantages of VR while mitigating its limitations such as cybersickness and visual discomfort [33]. AR can enhance interaction, presence, intuitiveness, and pedagogical flexibility by enriching the real world with digital information, accommodating various learning styles, and facilitating teaching and learning [34]. Despite these presumed advantages of AR, to our knowledge, there are no empirical studies of AR-based treatment for CLBP.
In summary, pain treatment guidelines emphasize the key role of educational CLBP treatment to counteract psychological chronification and promote self-efficacy according to health behavior change models. Furthermore, when health behavior change is addressed using a new technology, a joint consideration of health psychological models with theories of acceptance from a technological perspective, like the UTAUT 2 [35], is considered useful for successful implementation. Existing studies with immersive technology [24,26-31] demonstrated positive effects for CLBP treatment in VR incorporating psychoeducational elements. However, these VR studies have methodological shortcomings and gaps regarding dimensions of user experience such as satisfaction and acceptance. Therefore, by formulating research questions using the PICO (Population, Intervention, Comparison, Outcome) framework, this scoping review aims to first examine research in patients with CLBP (P) receiving psychoeducation through immersive technology (I) compared to conventional psychoeducation (C) to improve pain relief and pain-psychological variables (O) and second on the basis of the results of the literature analysis, to develop an intervention design for AR-based psychoeducation in patients with CLBP that combines conventional methods with immersive technology based on a technology acceptance model to promote acceptance and pain management.
Methods
We investigated the research question through a scoping review and followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews [36]. This review includes studies that used psychoeducation for CLBP and chronic pain treatment: (1) conventionally, (2) with immersive technology in VR or AR, or (3) a combination of both, conventional therapy with VR or AR technology use. Only papers published in English or German in 2019-2024 were considered, wherein clinical guidelines were generally updated every 3-5 years with new evidence [37]. The exclusion criteria were as follows: (1) psychiatric patients, (2) acute back pain, (3) back pain after medical procedures, and (4) other specific pain conditions and pharmacological interventions. Scientific investigations or studies in journals or textbooks were included, regardless of the scientific methodology used. An electronic search was performed in August 2024 by using predefined English terms: (“chronic low back pain” OR “CLBP” OR “chronic pain”) AND ((“virtual reality” OR “augmented reality”) OR (“education” OR “multimodal pain therapy” OR “psychological intervention”)). Reviewer RC used Citavi to search for in vivo ZB MED and PubMed, and a manual search was conducted in the Web of Science, American Psychological Association PsycINFO, and PsyArXiv Preprints. The search was conducted in line with the Joanna Briggs Institute methodology for scoping reviews, extending the PRISMA statement [38]. In accordance with Arksey and O’Malley’s [39] recommendations for scoping reviews, we did not include a formal quality assessment of the incorporated research. The selection process was initially based on a review of titles and abstracts regarding the inclusion and exclusion criteria, followed by an assessment of the full text by a reviewer (RC) and double-checked by another reviewer (ANT). Both reviewers (RC and ANT) extracted the following information from the included studies by using Microsoft Excel, following the Joanna Briggs Institute model: (1) citation, (2) context, (3) participant characteristics, (4) study aim, (5) methodology, (6) results, (7) interventions, (8) limitations, (9) key results related to review questions, and (10) future research areas [40]. Data analysis by the first reviewer (RC) utilized a qualitative content analysis [41]. A deductive approach was used to extract relevant categories for achieving the research objective. Guidelines for the treatment of CLBP [42] as well as recommendations of the World Health Organization for digital health interventions [43] served as the basis for this. Subsequently, 4 categories were extracted to capture all the essential aspects relevant to the design of the envisaged intervention. The categories are as follows: (1) content of CLBP-specific education, (2) factors based on the psychology of learning for the intervention design, (3) technical conditions (framework) for CLBP interventions, and (4) outcome measures of the educational interventions for CLBP.
Results
Study Selection
The study selection process, as shown in Figure 1, began with a database search that yielded 11,415 results. A total of 9602 titles were screened for the following terms: education, chronic pain, chronic back pain, CLBP, VR, and AR. The title should contain a minimum of 2 of the following keywords: education, chronic pain, chronic back pain, CLBP, VR, or AR; 9291 papers were excluded due to the lack of appearance of at least 2 of the defined terms. After applying the inclusion and exclusion criteria to 311 publications, 177 studies were excluded based on the titles and 95 were excluded based on the abstracts. After reviewing the full texts of the remaining 39 publications, 27 were excluded for (1) specific applications (eg, doctor-patient communication), (2) insufficient intervention descriptions, (3) overly specific populations (eg, elite athletes, primary school students, nursing staff), (4) unspecified psychoeducation (eg, cognitive behavioral therapy [CBT], cognitive functional training), and (5) unclear differentiation between education and physiotherapy in intervention design. Finally, the scoping review analyzed 12 publications, displayed in Table 1 [44-55].
Figure 1.
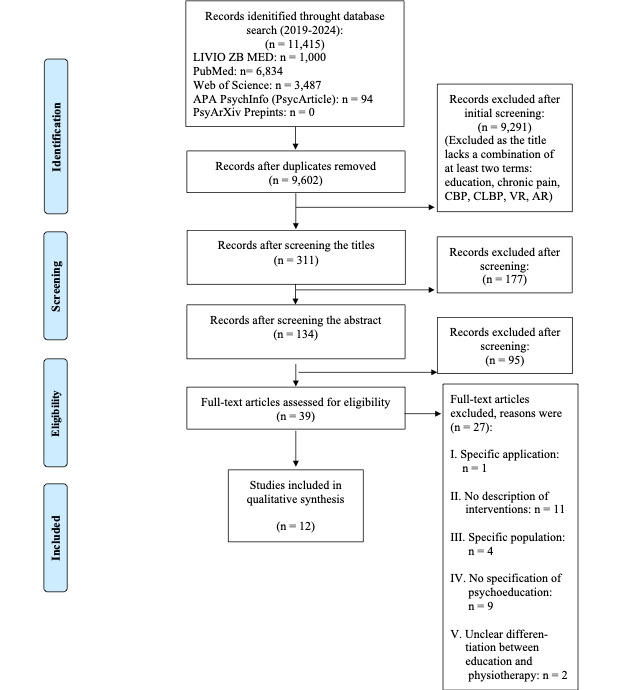
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flow diagram of the study selection process. APA: American Psychological Association; AR: augmented reality; CBP: chronic back pain; CLBP: chronic low back pain; VR: virtual reality.
Table 1.
Included studies applying psychoeducation by using conventional approaches and virtual reality approaches for the treatment of chronic low back pain [44-55].
| Author | Study title | Journal name |
| Salazar-Méndez et al [44], 2024 | Pain Neuroscience Education for Patients With Chronic Pain: A Scoping Review From Teaching-Leaning Strategies, Educational Level, and Cultural Perspective | Patient Education and Counseling |
| Ferlito et al [45], 2022 | Pain Education in the Management of Patients with Chronic Low Back Pain: A Systematic Review | Journal of Functional Morphology and Kinesiology |
| Rim et al [46], 2022 | Efficiency of Associating Therapeutic Patient Education with Rehabilitation in the Management of Chronic Low Back Pain: A Randomized Controlled Trial | Korean Journal of Family Medicine |
| Sidiq et al [47], 2024 | Effects of Pain Education on Disability, Pain, Quality of Life, and Self-Efficacy in Chronic Low Back Pain: A Randomized Controlled Trial | PLOS One |
| Tomás-Rodríguez et al [48], 2024 | Short- and Medium-Term Effects of a Single Session of Pain Neuroscience Education on Pain and Psychological Factors in Patients With Chronic Low Back Pain: A Single-Blind Randomized Clinical Trial | European Journal of Pain |
| Janik et al [49], 2024 | Middle-Term Effects of Education Program in Chronic Low Back Pain Patients to an Adherence to Physical Activity: A Randomized Controlled Trial | Patient Education and Counseling |
| Lindner et al [50], 2020 | Use of Virtual Reality as a Component of Acute and Chronic Pain Treatment | Anasthesiologie Intensivmedizin Notfallmedizin Schmerztherapie |
| Stamm et al [51], 2020 | Virtual Reality in Pain Therapy: a Requirements Analysis for Older Adults With Chronic Back Pain | Journal of NeuroEngineering and Rehabilitation |
| Stamm et al [52], 2022 | Virtual Reality Exergame for Supplementing Multimodal Pain Therapy in Older Adults With Chronic Back Pain | Virtual Reality |
| Brown et al [53], 2023 | Chronic Pain Education Delivered With a Virtual Reality Headset in Outpatient Physical Therapy Clinics: A Multisite Exploratory Trial | American Journal of Translational Research |
| McConnell et al [54], 2024 | A Multicenter Feasibility Randomized Controlled Trial Using a Virtual Reality Application of Pain Neuroscience Education for Adults With Chronic Low Back Pain | Annals of Medicine |
| de Vries et al [55], 2023 | Pain Education and Pain Management Skills in Virtual Reality in the Treatment of Chronic Low Back Pain: A Multiple Baseline Single-Case Experimental Design | Behavior Research and Therapy |
The studies originated from Italy, Spain, the Netherlands, France, Chile, India, and Tunisia (8.33% each), Germany (25%), and the United States (16.67%). The review included 9 empirical studies (1 interview study, 8 interventional studies) and 3 reviews (1 systematic, 1 scoping, and 1 narrative review). All studies were peer-reviewed, except the narrative review. The results of the analysis of the 12 publications included are presented below according to the 4 defined categories.
Contents of CLBP-Specific Education
The systematic review evaluated clinical studies from 2011 to 2021 comparing pain education/CBT with conventional physiotherapy for CLBP [45]. Thirteen studies, including 12 randomized controlled trials with 1642 participants, were analyzed. Six studies demonstrated a significant reduction in pain compared with the control group. The review concluded that due to the multimodality and heterogeneity of treatments, no definitive statement can be made regarding the efficacy of pain education or CBT in patients with CLBP [45]. Seven studies included an educational program in conjunction with physiotherapy [45-48,52-54]. Educational content varied considerably, ranging from exclusive focus on pain biology [46-49,52,53,55] to the inclusion of psychological aspects [46,52-55] and multidisciplinary approaches [49]. Most of the programs [48,55] incorporated education on pain physiology, frequently based on the book “Explain Pain” [56] by Butler and Moseley. Psychological education encompassed topics such as physical activity [45,46,49,53], fear of physical activity, emotional management [45-49,51], lifestyle modifications, daily exercises [45,49,52], pain-specific coping strategies [45,52,54], pain sensitization [47,54,55], and relaxation techniques, including stress management and mindfulness [45,49,52-55] in 6 studies, of which 5 included VR interventions. The content, duration, and physiotherapeutic integration of the individual education programs can be found in Multimedia Appendix 1.
Factors Based on Psychology of Learning for Intervention Design
This category encompasses factors of psychology of learning that are pertinent to the design of interactive interventions. Analysis of 3 studies showed that VR-based education employs passive mediation strategies such as informational videos and lectures (provided conventionally and in VR), alongside active and interactive strategies [44,50,54]. Three studies mentioned VR-based gamified approaches [50,52,55] and 2 studies [50,51] mentioned the promotion of intrinsic motivation.
Mediation Strategies
The included systematic review [44] examined the programs, cultural adaptations, and the efficacy of pain neuroscience education for chronic musculoskeletal pain, analyzing 71 studies that met our inclusion criteria and featured pain duration exceeding 3 months in adults. The analyzed studies explored pain neuroscience education in different settings by using various experimental designs, including secondary analyses of randomized controlled trials, and showed positive effects on pain and psychological variables. Despite cultural influences on pain-relevant factors, only 2 (3%) of the 71 studies culturally adapted the pain neuroscience education material. Passive teaching-learning strategies tended to yield better outcomes for pain and functionality, whereas active methods resulted in significant knowledge improvements, albeit with insufficient description. The outcomes of multimodal therapies for chronic pain depend on the individualized integration of pain-specific education, considering biopsychosocial factors, educational level, culture, and diverse learning methods and materials for conveying pain neuroscience content [44]. Interaction content is passively conveyed through videos or lectures [46-49,53], particularly VR-based 360° nature videos [53].
Gamification and Motivation Enhancement
The Pain-Neuro-Education 2.0 software utilized a VR headset with immersive footage and computer-generated images for visually and emotionally engaging educational and relaxation training for chronic pain. This included interactive emotion regulation exercises such as breathing and mindfulness exercises in natural environments [54]. The VR program Recupt was also used to convey information in an engaging manner by having the user shoot at the pain stimulus with a laser gun, among other things. In the spinal cord phase, participants focus on visual “pain gates” and breathing to metaphorically “close” them and experience relaxation-induced pain relief. The brain component elucidates the reduction in pain response through the visualization and reactivation of illuminated connections. The alarm center gameplay demonstrates how emotions, cognitions, and behaviors influence pain perception. Finally, participants envision the alarm center as a brain region that regulates pain stimuli in an aircraft cockpit [55]. The VR program ViRST provides a therapeutic, interactive user interface with task-based activities in a farm environment [52]. Patients visualize movements and exertion levels by using game-based biofeedback with progress tracking and narrative elements [51]. Exergames incorporate biofeedback such as heart rate variability via photoplethysmography to prevent overexertion in interactive scenarios [52]. Gamification can motivate and enhance therapy adherence by fulfilling the psychological needs of competence, autonomy, and relatedness through interactive knowledge transfer. It also improves user skills through playful activities [50]. In the long term, feedback should be framed positively to maintain intrinsic motivation [52]. Avatars manipulate body perception for therapeutic effects, with the Proteus effect causing users to adopt their avatar’s behavior in real life. Personalized avatars can amplify pain relief [50].
Technical Conditions (Framework) for CLBP Intervention
The technical parameters of 3 enclosed VR studies, comprising 1 needs analysis [52] and 2 feasibility studies [52,53], provide insights into the design of AR-based education and identify potential areas of focus such as user-friendliness [51,53], operational support [51-53], and various application challenges [51,53]. The needs analysis was based on semistructured interviews (n=10) in focus groups to determine the requirements of older patients with chronic back pain, physiotherapists, and psychotherapists regarding VR pain therapy in terms of overall system, hardware, and software [51]. Findings emphasize that the designed system must be user-friendly; provide personalized instructions, demonstration videos, and individual guidance; and be available for rent. Assistants should support this system. Automatic breaks were considered crucial to avoid overexertion and pain aggravation. Activity should be limited to 30 minutes followed by a 15-minute rest. The study also highlighted the importance of balancing active therapy and relaxation. For hardware, it was determined that the VR headset must be independent and removable. Software design should consider user-friendliness by integrating the game environment with the level in-game environment for individual calibration of movement restrictions, particularly in gaming activities. Finally, a spacious room and wireless head-mounted display were considered essential for safety to prevent falls.
One feasibility study also emphasized the importance of safety aspects for the usability of VR headsets. The authors indicate that 93% of the application issues were associated with handling spatial and temporal limitations [53]. The second feasibility study demonstrated that disregarding body height (insufficient arm span) was perceived as disruptive [52]. Operational support software allows therapists to intervene during instances of pain, anxiety, or improper exercise execution by using a help button or emergency assistance [51]. Incorrect exercise execution is considered disruptive [52] and often lacks adequate support personnel for error correction or clinical assistance [53].
Outcome Measures of Educational Interventions for CLBP
Of the 12 studies [44-55] reviewed, 8 [46-49,54,55] were quantitative interventional studies. Commonly evaluated outcomes in CLBP studies encompassed pain intensity [45-49,51,52,54,55], kinesiophobia [46,48,51-53,55], pain catastrophizing [48,53-55], disability [45-47,51,52,54], health-related quality of life [51,52,54], well-being [47], self-efficacy [47,54], depression [46,53], attrition rate [49,53], and VR intervention user experience [52,53]. A comprehensive table displaying the different methods used, study results, and conclusions for each of the included studies can be found in Multimedia Appendix 2. A list of the pain-specific constructs and their measurement tools assessed in the different studies can be found in Multimedia Appendix 3.
Discussion
Principal Findings
Psychoeducation is a key element for CLBP treatment. Psychoeducation provided in AR could offer more benefits than that in VR or with conventional methods by integrating physical and virtual elements. Additionally, psychoeducation in AR was assumed to be superior to VR due to reported VR-associated discomforts in CLBP treatment, such as cybersickness and visual discomfort. Therefore, we conducted a literature review in the first step to evaluate research on CLBP treatment through psychoeducation using conventional methods and immersive technologies in order to design a psychoeducational intervention in AR for CLBP. In the second step, we applied the extracted results of the literature review to a theoretical framework, in particular, the UTAUT 2, to provide a design example for AR-based psychoeducation for CLBP.
Our findings indicate that various educational programs were combined with physiotherapy [45-48,52-54]. These studies referred to conventional methods or VR-based interventions. No relevant study with AR for CLBP treatment was found. The varying educational content encompassed pain biology [46-49], psychological education on physical activity [45,46,49,53], anxiety management [45-49,51], lifestyle modifications, daily exercises [45,49,52], coping strategies [45,52,54], pain sensitization [47,54,55], and relaxation techniques [45,49,52-55]. Passive, active [44,50,54], and gamified strategies [50,52,55] were employed alongside the promotion of intrinsic motivation [50,51]. User-friendliness [51,53], operational support [51,52,54], and application challenges [52,53] were considered important for software development. The key variables of educational CLBP interventions included physiological variables such as pain intensity [45-49,51,52,54,55] and disability level [45-47,51,52,54]; psychological variables such as kinesiophobia [46,48,51,52,54,55], pain catastrophizing [48,53-55], quality of life [51,52,55], well-being [47], self-efficacy [47,54], and depression [46,53]; and technical variables such as dropout rates [49,53] and user experience [52,53].
Our results elucidate key aspects of a useful design of a psychoeducational treatment in AR for CLBP, which does not exist to date, to the best of our knowledge. Our findings point out the relevance of the interplay of technical and psychological components, in particular, the health psychological aspects incorporating psychology of learning to foster behavior change. In the next step, the findings were applied to a theoretical framework. For this, we referred to the UTAUT 2 [8,9]. UTAUT 2 encompasses constructs such as (1) performance expectancy, (2) effort expectancy, (3) social influence, (4) facilitating conditions, (5) hedonic motivation, (6) price value, and (7) habit for intention formation as well as the moderating variables age, gender, and experience [8]. Therefore, we recommend the following design suggestions for psychoeducational interventions in AR based on UTAUT 2 for the treatment of CLBP, as exemplified in Figure 2.
Figure 2.
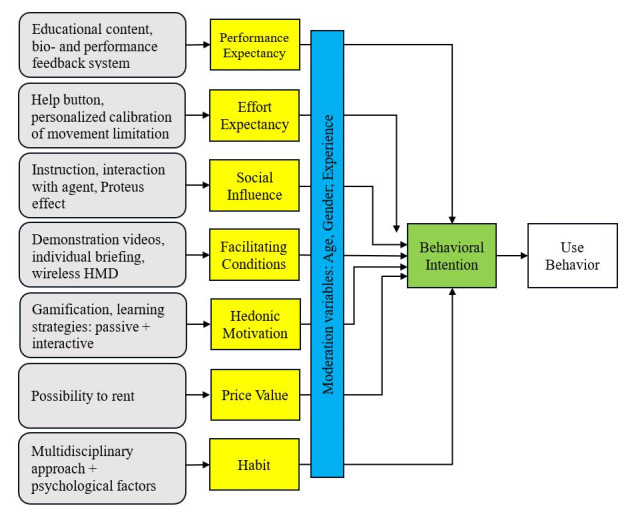
Exemplary mapping of the extracted findings from the literature review (grey) applied to the Unified Theory of Acceptance and Use of Technology to design an artificial reality–based psychoeducation for chronic low back pain. HMD: head-mounted display.
UTAUT 2 Constructs
Performance Expectancy
It is recommended to convey psychoeducational content that demonstrates how CLBP can be positively influenced through physical activity [45,46,49,53], emotion management in kinesiophobia [45-49,51], pain-specific coping strategies [45,52,54], and stress and mindfulness techniques [45,49,52-55]. This content can be conveyed through a biofeedback system and supportive agent. As many educational measures are combined with physiotherapy [45-48,52-54], the agent can provide movement exercises, educational content, and interactive stress management techniques [54], supplemented by biofeedback. The biofeedback level and multimodal feedback of avatars promote top-down and bottom-up processes and enable associative learning [50]. To avoid discrepancies between instructions and sensory feedback, facilitate rapid corrections, and enhance user-friendliness [52], the avatar should provide immediate visual-acoustic performance feedback [50]. Biofeedback and body feedback are essential interventions for behavioral modification [17]. It is recommended to combine psychoeducation with a mindfulness-based stress reduction body scan and heart rate biofeedback [51], wherein biofeedback demonstrates progress and enables gamification elements [50,52].
Effort Expectancy
Software design should incorporate a gaming environment with in-game level settings to facilitate personalized calibration of movement limitations and body size, particularly for therapeutic activities [51,52]. The system should enable therapists to intervene through a help button or emergency assistance when patients experience pain, anxiety, or perform exercises incorrectly [51]. Frequent feedback for incorrect exercise execution should be avoided, as it may be perceived as disruptive [52].
Social Influence
With regard to social influence, an AR intervention should be accompanied by an agent that conveys pain-specific knowledge through lectures as passive knowledge transfer [44] or through support in psychological interactions, such as stress management exercises [54]. An agent can monitor a patient’s body movements to integrate the phenomenon of “virtual body ownership” into the body image or utilize the analgesic effect of the Proteus effect to promote behaviors in the real world [50]. This aligns with BCT‘s recommendations for behavior change, wherein instruction, repetition, and demonstration of behavior have positive effects on physical activity that persist for up to 6 months [50,51]. Therefore, we propose to increase the intention to use by incorporating an agent in an AR intervention, with both passive and interactive roles.
Facilitating Conditions
A user-friendly system requires personalized instructions, demonstration videos, and individual briefings. For safety considerations, a spacious environment and wireless head-mounted displays are essential to mitigate the risk of falls. An assistant should be present to support the system. Automated breaks are crucial to prevent overexertion and exacerbation of pain, thereby automatically balancing the active therapy and relaxation periods. The VR headset should be designed for independent removal and application [51].
Hedonic Motivation
Passive learning strategies tend to yield superior outcomes in pain and functionality, whereas active methods can elicit significant improvements in knowledge [44]. Gamification demonstrates a motivation-enhancing effect through active and interactive patient engagement [50,52], for instance, through the interactive development of pain-specific knowledge in the Reducept program, where users enter their own brains and shoot with laser guns or connect points [55], or through movement exercises on a simulated farm [52]. A feedback system or biofeedback could be integrated, as outlined in the variable “performance expectancy” of UTAUT 2 and should be phrased positively as praise to increase motivation [51]. Praise as a social reward can occur through interaction with an agent, as described in the variable “social influence” [18]. In CBT, praise serves as positive reinforcement to promote adaptive behaviors and cognitions corresponding to positive CBT, which incorporates positive psychology and solution-focused brief therapy into a cognitive-behavioral context [57]. Gamification in an AR-based intervention enables the implementation of BCTs [17] by creating a material incentive such as within the framework of a game in an AR application [43].
Price Value
The headsets required for the interventions should be provided or loaned rather than purchased [50].
Habit
Educational programs for CLBP should incorporate a multidisciplinary approach that encompasses both physiological and psychological pain while promoting behavioral modifications such as regular physical activity [49]. Conventional recommendations for behavioral change emphasize repetition as crucial for habit formation [50]. For long-term interventions aimed at behavioral modification, theories addressing the intention-behavior gap and behavioral automaticity in physical activity should be considered, such as the Affective Reflective Theory of Physical Inactivity and Exercise [58] or the Physical Activity Adoption and Maintenance model [59].
Strengths and Limitations
This scoping review gives an overview of the most important educational content, elements of psychological training, interactive design forms, and relevant pain psychological variables for developing CLBP interventions in AR. It offers a substantiated basis for a theory-based development of a psychoeducational treatment in AR. Thus, this study provides a framework for the theory-driven extraction of hypotheses for future AR research in CLBP treatment. One limitation of this review encompasses the exclusion of certain sport science and physiotherapy databases (eg, SPORTDiscus) and the restriction to studies published in German and English, potentially omitting relevant publications. Further, the distinction between CLBP and chronic nonspecific low back pain in the included studies was often imprecise. The distinction might be relevant for the intervention design, which was neglected in our analysis.
Recommendations for Research
First, the theoretically proposed design of AR-based psychoeducation for CLBP should be realized in future research. Second, an evaluation of the feasibility and user experience is needed. Third, the therapeutic efficacy of the psychoeducational content in AR must be demonstrated in a clinical evaluation study with patients with CLBP. As no studies on the psychometric properties of measurements in AR are known, psychometric assessments must be tested for measurement equivalence.
Conclusions
For the development of a framework for an AR-based psychoeducational intervention in CLBP, the combination of theories of acceptance and use of technologies with insights from health psychological behavior change theories appears to be of great importance. An example for a theory-based design of psychoeducation in AR for CLBP is proposed and discussed. Our results offer a substantiated basis for a theory-based development of psychoeducational treatment in AR.
Acknowledgments
This work was funded in part by the Ministry for Science and Health of Rhineland-Palatinate as part of the research training group (Forschungskolleg) “Immersive Extended Reality for Physical Activity and Health” (XR-PATH). The publication was funded or supported by the Open Access Fund of Universität Trier and by the German Research Foundation (DFG).
Abbreviations
- AR
augmented reality
- BCT
behavior change technique
- CBT
cognitive behavioral therapy
- CLBP
chronic low back pain
- PICO
Population, Intervention, Comparison, Outcome
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- UTAUT 2
Unified Theory of Acceptance and Use of Technology 2
- VR
virtual reality
Contents of the education, duration, and physiotherapy involvement.
Summary of the study characteristics, results, and conclusions of the 12 included studies.
Summary of the pain-specific measuring outcomes and instruments.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews checklist.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Alsufiany M, Lohman E, Daher N, Gang G, Shallan A, Jaber H. Non-specific chronic low back pain and physical activity: A comparison of postural control and hip muscle isometric strength: A cross-sectional study. Medicine (Baltimore) 2020 Jan;99(5):e18544. doi: 10.1097/MD.0000000000018544. https://europepmc.org/abstract/MED/32000363 .00005792-202001310-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schreijenberg M, Koes BW, Lin CC. Guideline recommendations on the pharmacological management of non-specific low back pain in primary care - is there a need to change? Expert Rev Clin Pharmacol. 2019 Feb;12(2):145–157. doi: 10.1080/17512433.2019.1565992. [DOI] [PubMed] [Google Scholar]
- 3.Faucett J. Chronic low back pain: early interventions. Annu Rev Nurs Res. 1999 Jan 01;17(1):155–182. doi: 10.1891/0739-6686.17.1.155. [DOI] [PubMed] [Google Scholar]
- 4.Dobbels F, De Bleser L, Berben L, Kristanto P, Dupont L, Nevens F, Vanhaecke J, Verleden G, De Geest S. Efficacy of a medication adherence enhancing intervention in transplantation: The MAESTRO-Tx trial. J Heart Lung Transplant. 2017 May;36(5):499–508. doi: 10.1016/j.healun.2017.01.007.S1053-2498(17)30014-1 [DOI] [PubMed] [Google Scholar]
- 5.Airaksinen O, Brox JI, Cedraschi C, Hildebrandt J, Klaber-Moffett J, Kovacs F, Mannion AF, Reis S, Staal JB, Ursin H, Zanoli G, COST B13 Working Group on Guidelines for Chronic Low Back Pain Chapter 4. European guidelines for the management of chronic nonspecific low back pain. Eur Spine J. 2006 Mar;15 Suppl 2(Suppl 2):S192–300. doi: 10.1007/s00586-006-1072-1. https://europepmc.org/abstract/MED/16550448 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schäfer R, Niederer D, Levenig C, et al Effectiveness and mechanisms of a multimodal treatment for low back pain: A pragmatic matched cohort study. MedRxiv. Preprint posted online on February 2, 2023. 2023 doi: 10.1101/2022.09.28.22280380. [DOI] [Google Scholar]
- 7.Alfuth M, Lages A. Chronischer Rückenschmerz. CME. 2018 Jun 13;15(6):9–24. doi: 10.1007/s11298-018-6424-8. [DOI] [Google Scholar]
- 8.Frizziero A, Pellizzon G, Vittadini F, Bigliardi D, Costantino C. Efficacy of core stability in non-specific chronic low back pain. JFMK. 2021 Apr 22;6(2):37. doi: 10.3390/jfmk6020037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mueller J, Niederer D. Dose-response-relationship of stabilisation exercises in patients with chronic non-specific low back pain: a systematic review with meta-regression. Sci Rep. 2020 Oct 09;10(1):16921. doi: 10.1038/s41598-020-73954-9. https://doi.org/10.1038/s41598-020-73954-9 .10.1038/s41598-020-73954-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Minobes-Molina E, Nogués Maria Rosa, Giralt M, Casajuana C, de Souza Dyego Leandro Bezerra, Jerez-Roig Javier, Romeu Marta. Effectiveness of specific stabilization exercise compared with traditional trunk exercise in women with non-specific low back pain: a pilot randomized controlled trial. PeerJ. 2020;8:e10304. doi: 10.7717/peerj.10304. https://europepmc.org/abstract/MED/33312766 .10304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sutanto D, Ho RST, Poon ETC, Yang Y, Wong SHS. Effects of different trunk training methods for chronic low back pain: a meta-analysis. IJERPH. 2022 Mar 01;19(5):2863. doi: 10.3390/ijerph19052863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Isaikin AI, Nasonova TI, Mukhametzyanova AK. Emotional disorders and their therapy in chronic low back pain. RJTAO. 2022 Oct 25;14(5):90–95. doi: 10.14412/2074-2711-2022-5-90-95. [DOI] [Google Scholar]
- 13.Comachio J, Magalhães Mauricio Oliveira, Campos Carvalho E Silva Ana Paula de Moura, Marques AP. A cross-sectional study of associations between kinesiophobia, pain, disability, and quality of life in patients with chronic low back pain. Adv Rheumatol. 2018 Jun 22;58(1):8. doi: 10.1186/s42358-018-0011-2.10.1186/s42358-018-0011-2 [DOI] [PubMed] [Google Scholar]
- 14.Williams FMK, Elgaeva EE, Freidin MB, Zaytseva OO, Aulchenko YS, Tsepilov YA, Suri P. Causal effects of psychosocial factors on chronic back pain: a bidirectional Mendelian randomisation study. Eur Spine J. 2022 Jul;31(7):1906–1915. doi: 10.1007/s00586-022-07263-2. https://europepmc.org/abstract/MED/35662366 .10.1007/s00586-022-07263-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Silva-Smith AL, Hanson CL, Neubeck L, Rowat A, McHale S. Physical activity interventions framed by the health action process approach for adults with long-term conditions: a scoping review. Int J Behav Med. 2024 Dec;31(6):987–1017. doi: 10.1007/s12529-024-10305-2.10.1007/s12529-024-10305-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkatesh V, Thong JYL, Xu X. Consumer acceptance and use of information technology: extending the Unified Theory of Acceptance and Use of Technology. MIS Quarterly. 2012;36(1):157. doi: 10.2307/41410412. [DOI] [Google Scholar]
- 17.Or C. Towards an integrated model: task-technology fit in unified theory of acceptance and use of technology 2 in education contexts. JALT. 2023 Jan 20;6(1):1–2. doi: 10.37074/jalt.2023.6.1.8. [DOI] [Google Scholar]
- 18.Barbosa RAP, Martins AVS, Da Silva IPA, Costa LA, Oliveira RA, De Souza HC. Acceptance and use of a virtual learning environment (VLE): structural equations modeling of the unified theory of acceptance and use of technology. Int J Innov Educ Res. 2020 Apr 01;8(4):237–244. doi: 10.31686/ijier.vol8.iss4.2285. [DOI] [Google Scholar]
- 19.Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA) Rehabil Psychol. 2011 Aug;56(3):161–70. doi: 10.1037/a0024509.2011-14571-001 [DOI] [PubMed] [Google Scholar]
- 20.Lin J, Faust B, Ebert DD, Krämer Lena, Baumeister H. Correction: A web-based acceptance-facilitating intervention for identifying patients' acceptance, uptake, and adherence of internet- and mobile-based pain interventions: randomized controlled trial. J Med Internet Res. 2019 Feb 06;21(2):e12015. doi: 10.2196/12015. https://www.jmir.org/2019/2/e12015/ v21i2e12015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Michie S, Richardson M, Johnston M, Abraham C, Francis J, Hardeman W, Eccles MP, Cane J, Wood CE. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013 Aug;46(1):81–95. doi: 10.1007/s12160-013-9486-6. https://core.ac.uk/reader/191129821?utm_source=linkout . [DOI] [PubMed] [Google Scholar]
- 22.Milgram P, Kishino F. A taxonomy of mixed reality visual displays. IEICE Trans Inf Syst. 1994. [2024-01-13]. https://cs.gmu.edu/~zduric/cs499/Readings/r76JBo-Milgram_IEICE_1994.pdf .
- 23.Skarbez R, Smith M, Whitton MC. Revisiting Milgram and Kishino's reality-virtuality continuum. Front Virtual Real. 2021 Mar 24;2:1. doi: 10.3389/frvir.2021.647997. [DOI] [Google Scholar]
- 24.Mallari B, Spaeth EK, Goh H, Boyd BS. Virtual reality as an analgesic for acute and chronic pain in adults: a systematic review and meta-analysis. J Pain Res. 2019;12:2053–2085. doi: 10.2147/JPR.S200498. https://europepmc.org/abstract/MED/31308733 .200498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Awan A. Enhancing user experience: exploring mobile augmented reality experiences. VFAST Transactions on Software Engineering. 2024:121–132. doi: 10.21015/vtse.v12i1.1741. [DOI] [Google Scholar]
- 26.Trujillo MS, Alvarez AF, Nguyen L, Petros J. Embodiment in virtual reality for the treatment of chronic low back pain: a case series. J Pain Res. 2020;13:3131–3137. doi: 10.2147/JPR.S275312. https://europepmc.org/abstract/MED/33269003 .275312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tack C. Virtual reality and chronic low back pain. Disabil Rehabil Assist Technol. 2021 Aug;16(6):637–645. doi: 10.1080/17483107.2019.1688399. [DOI] [PubMed] [Google Scholar]
- 28.Hennessy RW, Rumble D, Christian M, Brown DA, Trost Z. A graded exposure, locomotion-enabled virtual reality app during walking and reaching for individuals with chronic low back pain: cohort gaming design. JMIR Serious Games. 2020 Aug 10;8(3):e17799. doi: 10.2196/17799. https://games.jmir.org/2020/3/e17799/ v8i3e17799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garcia LM, Darnall BD, Krishnamurthy P, Mackey IG, Sackman J, Louis RG, Maddox T, Birckhead BJ. Correction: self-administered behavioral skills-based at-home virtual reality therapy for chronic low back pain: protocol for a randomized controlled trial. JMIR Res Protoc. 2021 Feb 12;10(2):e27652. doi: 10.2196/27652. https://www.researchprotocols.org/2021/2/e27652/ v10i2e27652 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Garcia LM, Birckhead BJ, Krishnamurthy P, Sackman J, Mackey IG, Louis RG, Salmasi V, Maddox T, Darnall BD. An 8-week self-administered at-home behavioral skills-based virtual reality program for chronic low back pain: double-blind, randomized, placebo-controlled trial conducted during COVID-19. J Med Internet Res. 2021 Feb 22;23(2):e26292. doi: 10.2196/26292. https://www.jmir.org/2021/2/e26292/ v23i2e26292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li R, Li Y, Kong Y, Li H, Hu D, Fu C, Wei Q. Virtual reality-based training in chronic low back pain: systematic review and meta-analysis of randomized controlled trials. J Med Internet Res. 2024 Feb 26;26:e45406. doi: 10.2196/45406. https://www.jmir.org/2024//e45406/ v26i1e45406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nagpal AS, Raghunandan A, Tata F, Kibler D, McGeary D. Virtual reality in the management of chronic low back pain: a scoping review. Front Pain Res (Lausanne) 2022;3:856935. doi: 10.3389/fpain.2022.856935. https://europepmc.org/abstract/MED/35295809 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wu YF, Kim EY. Users’ perceptions of technological features in augmented reality (AR) and virtual reality (VR) in fashion retailing: a qualitative content analysis. Mobile Information Systems. 2022 Aug 4;2022:1–13. doi: 10.1155/2022/3080280. [DOI] [Google Scholar]
- 34.Sala N. IGI Global. Virtual reality, augmented reality, and mixed reality in education. 2020:48–73. doi: 10.4018/978-1-7998-4960-5.ch003. [DOI] [Google Scholar]
- 35.Tamilmani K, Rana NP, Wamba SF, Dwivedi R. The extended Unified Theory of Acceptance and Use of Technology (UTAUT2): A systematic literature review and theory evaluation. International Journal of Information Management. 2021 Apr;57:102269. doi: 10.1016/j.ijinfomgt.2020.102269. [DOI] [Google Scholar]
- 36.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Özge, Straus SE. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018 Oct 02;169(7):467–473. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/abs/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed .2700389 [DOI] [PubMed] [Google Scholar]
- 37.Vernooij RW, Sanabria AJ, Solà Ivan, Alonso-Coello P, Martínez García Laura. Guidance for updating clinical practice guidelines: a systematic review of methodological handbooks. Implement Sci. 2014 Jan 02;9:3. doi: 10.1186/1748-5908-9-3. https://implementationscience.biomedcentral.com/articles/10.1186/1748-5908-9-3 .1748-5908-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.von Elm E, Schreiber G, Haupt CC. [Not Available] Z Evid Fortbild Qual Gesundhwes. 2019 Jun;143:1–7. doi: 10.1016/j.zefq.2019.05.004.S1865-9217(19)30066-2 [DOI] [PubMed] [Google Scholar]
- 39.Arksey H, O'Malley L. Scoping studies: towards a methodological framework. International Journal of Social Research Methodology. 2005 Feb;8(1):19–32. doi: 10.1080/1364557032000119616. [DOI] [Google Scholar]
- 40.Khalil H, Peters MD, Tricco AC, Pollock D, Alexander L, McInerney P, Godfrey CM, Munn Z. Conducting high quality scoping reviews-challenges and solutions. J Clin Epidemiol. 2021 Feb;130:156–160. doi: 10.1016/j.jclinepi.2020.10.009.S0895-4356(20)31148-3 [DOI] [PubMed] [Google Scholar]
- 41.Mayring P, Fenzl T. Handbuch Methoden der empirischen Sozialforschung. Wiesbaden: Springer; 2019. Qualitative Inhaltsanalyse. [Google Scholar]
- 42.Nicol V, Verdaguer C, Daste C, Bisseriex H, Lefèvre-Colau Marie-Martine, Rannou F, Rören Alexandra, Facione J, Nguyen C. Chronic low back pain: a narrative review of recent international guidelines for diagnosis and conservative treatment. J Clin Med. 2023 Feb 20;12(4):1685. doi: 10.3390/jcm12041685. https://www.mdpi.com/resolver?pii=jcm12041685 .jcm12041685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.WHO Guideline Recommendations on Digital Interventions for Health System Strengthening. Geneva: World Health Organization; 2019. [PubMed] [Google Scholar]
- 44.Salazar-Méndez Joaquín, Cuyul-Vásquez Iván, Ponce-Fuentes F, Guzmán-Muñoz Eduardo, Núñez-Cortés Rodrigo, Huysmans E, Lluch-Girbés Enrique, Viscay-Sanhueza N, Fuentes J. Pain neuroscience education for patients with chronic pain: A scoping review from teaching-learning strategies, educational level, and cultural perspective. Patient Educ Couns. 2024 Jun;123:108201. doi: 10.1016/j.pec.2024.108201.S0738-3991(24)00068-5 [DOI] [PubMed] [Google Scholar]
- 45.Ferlito R, Blatti C, Lucenti L, Boscarino U, Sapienza M, Pavone V, Testa G. Pain education in the management of patients with chronic low back pain: a systematic review. JFMK. 2022 Sep 26;7(4):74. doi: 10.3390/jfmk7040074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rim M, Leila R, Aicha BT, Olfa S, Meriem H, Ines L, Najla M, Hajer R, Imen K. Efficiency of associating therapeutic patient education with rehabilitation in the management of chronic low back pain: a randomized controlled trial. Korean J Fam Med. 2022 Nov;43(6):367–373. doi: 10.4082/kjfm.21.0223. https://europepmc.org/abstract/MED/36444121 .kjfm.21.0223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Sidiq M, Muzaffar T, Janakiraman B, Masoodi S, Vasanthi RK, Ramachandran A, Bansal N, Chahal A, Kashoo FZ, Rizvi MR, Sharma A, Rai RH, Verma R, Sharma M, Alam S, Vajrala KR, Sharma J, Muthukrishnan R. Effects of pain education on disability, pain, quality of life, and self-efficacy in chronic low back pain: A randomized controlled trial. PLoS One. 2024;19(5):e0294302. doi: 10.1371/journal.pone.0294302. https://dx.plos.org/10.1371/journal.pone.0294302 .PONE-D-23-35122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tomás-Rodríguez Mª Isabel, Asensio-García María Del Rosario, García Rauf Nouni, Delicado-Miralles Miguel, Sánchez Sergio Hernández, Segura-Heras Jose Vicente. Short- and medium-term effects of a single session of pain neuroscience education on pain and psychological factors in patients with chronic low back pain. A single-blind randomized clinical trial. Eur J Pain. 2024 Nov;28(10):1841–1854. doi: 10.1002/ejp.4700. [DOI] [PubMed] [Google Scholar]
- 49.Janik F, Fabre C, Seichepine AL, Masquelier B, Barbier F, Toulotte C. Middle-term effects of education programme in chronic low back pain patients to an adherence to physical activity: A randomized controlled trial. Patient Education and Counseling. 2024 Feb;119:108081. doi: 10.1016/j.pec.2023.108081. [DOI] [PubMed] [Google Scholar]
- 50.Lindner S, Latoschik M, Rittner H. [Use of virtual reality as a component of acute and chronic pain treatment] Anasthesiol Intensivmed Notfallmed Schmerzther. 2020 Sep;55(9):549–561. doi: 10.1055/a-1022-3038. [DOI] [PubMed] [Google Scholar]
- 51.Stamm O, Dahms R, Müller-Werdan Ursula. Virtual reality in pain therapy: a requirements analysis for older adults with chronic back pain. J Neuroeng Rehabil. 2020 Sep 29;17(1):129. doi: 10.1186/s12984-020-00753-8. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-020-00753-8 .10.1186/s12984-020-00753-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stamm O, Dahms R, Reithinger N, Ruß Aaron, Müller-Werdan Ursula. Virtual reality exergame for supplementing multimodal pain therapy in older adults with chronic back pain: a randomized controlled pilot study. Virtual Real. 2022;26(4):1291–1305. doi: 10.1007/s10055-022-00629-3. https://europepmc.org/abstract/MED/35194374 .629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Brown L, DiCenso-Fleming T, Ensign T, Boyd AJ, Monaghan G, Binder DS. Chronic pain education delivered with a virtual reality headset in outpatient physical therapy clinics: a multi-site exploratory trial. Am J Transl Res. 2023;15(5):3500–3510. https://europepmc.org/abstract/MED/37303618 . [PMC free article] [PubMed] [Google Scholar]
- 54.McConnell R, Lane E, Webb G, LaPeze D, Grillo H, Fritz J. A multicenter feasibility randomized controlled trial using a virtual reality application of pain neuroscience education for adults with chronic low back pain. Ann Med. 2024 Dec;56(1):2311846. doi: 10.1080/07853890.2024.2311846. https://www.tandfonline.com/doi/10.1080/07853890.2024.2311846?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub0pubmed . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.de Vries FS, van Dongen RTM, Bertens D. Pain education and pain management skills in virtual reality in the treatment of chronic low back pain: A multiple baseline single-case experimental design. Behav Res Ther. 2023 Mar;162:104257. doi: 10.1016/j.brat.2023.104257.S0005-7967(23)00006-2 [DOI] [PubMed] [Google Scholar]
- 56.Butler D, Moseley G. 2nd ed. Australia: Noigroup Publications; 2013. Explain pain. [Google Scholar]
- 57.Bannink F, Geschwind N. Positive CBT: Individual and Group Treatment Protocols for Positive Cognitive Behavioral Therapy. Göttingen, Germany: Hogrefe; 2021. May, [Google Scholar]
- 58.Brand R, Ekkekakis P. Affective–Reflective Theory of physical inactivity and exercise. Ger J Exerc Sport Res. 2017 Nov 14;48(1):48–58. doi: 10.1007/s12662-017-0477-9. [DOI] [Google Scholar]
- 59.Jekauc D, Gürdere Ceren, Englert C, Strobach T, Bottesi G, Bray S, Brown D, Fleig L, Ghisi M, Graham J, Martinasek M, Tamulevicius N, Pfeffer I. The contribution and interplay of implicit and explicit processes on physical activity behavior: empirical testing of the physical activity adoption and maintenance (PAAM) model. BMC Public Health. 2024 May 06;24(1):1239. doi: 10.1186/s12889-024-18589-5. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-024-18589-5 .10.1186/s12889-024-18589-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Contents of the education, duration, and physiotherapy involvement.
Summary of the study characteristics, results, and conclusions of the 12 included studies.
Summary of the pain-specific measuring outcomes and instruments.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) extension for scoping reviews checklist.


