Correction: Critical Care (2023) 27:360 10.1186/s13054-023-04648-7
Following publication of the original article [1], the authors identified an errors in Figure 1. It should indicate CO = 0.80 instead of CO = 0.67 in A a) ARPDS patient on V-V ECMO and g/dl instead of mg/dl in A a), b) and c). Both the incorrect and correct Figure 1 are given hereafter.
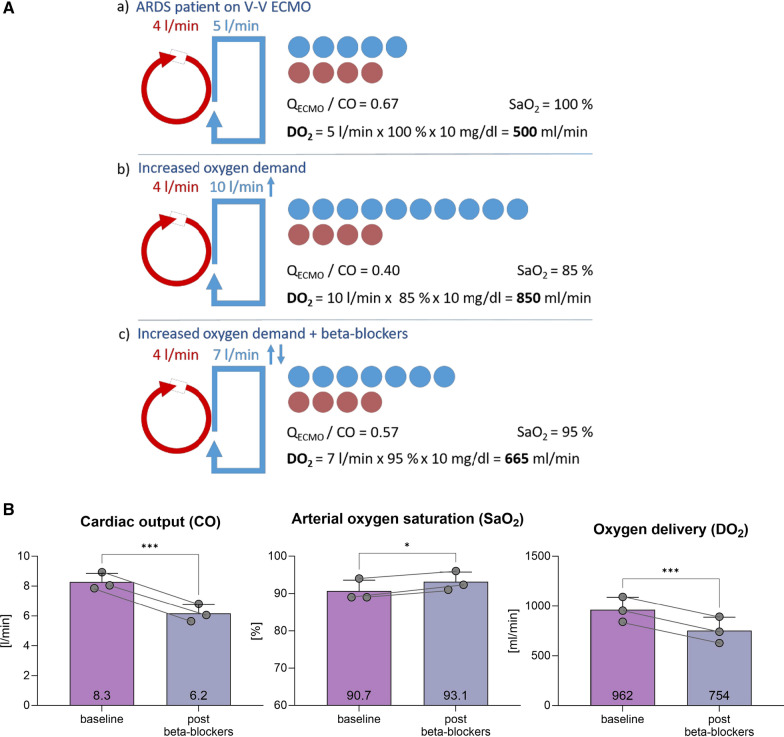
The incorrect Figure 1:
Fig. 1.
A Schematic representation of ECMO flow and cardiac output. Red indicates V-V ECMO flow, and blue indicates cardiac output. For illustrative purposes, recirculation is neglected; a Patient with ARDS and V-V ECMO support. The QECMO/CO ratio is 0.67, with saturation at 100%. DO2 is 500 ml/min. b The same patient with increased oxygen demand, for example, due to infection and fever. QECMO remains the same while CO is increased. This results in a ratio of 0.40, saturation of 85%, but a significantly increased DO2 of 850 ml/min. c Patient with increased oxygen demand treated with beta-blocker. The higher QECMO/CO ratio improved arterial oxygen saturation, but the DO2 drops to 665 ml/min. B Displays three ARDS patients undergoing V-V ECMO therapy, in whom beta-blockers were titrated based on their effects. The measurements were taken three times each after reaching a steady state
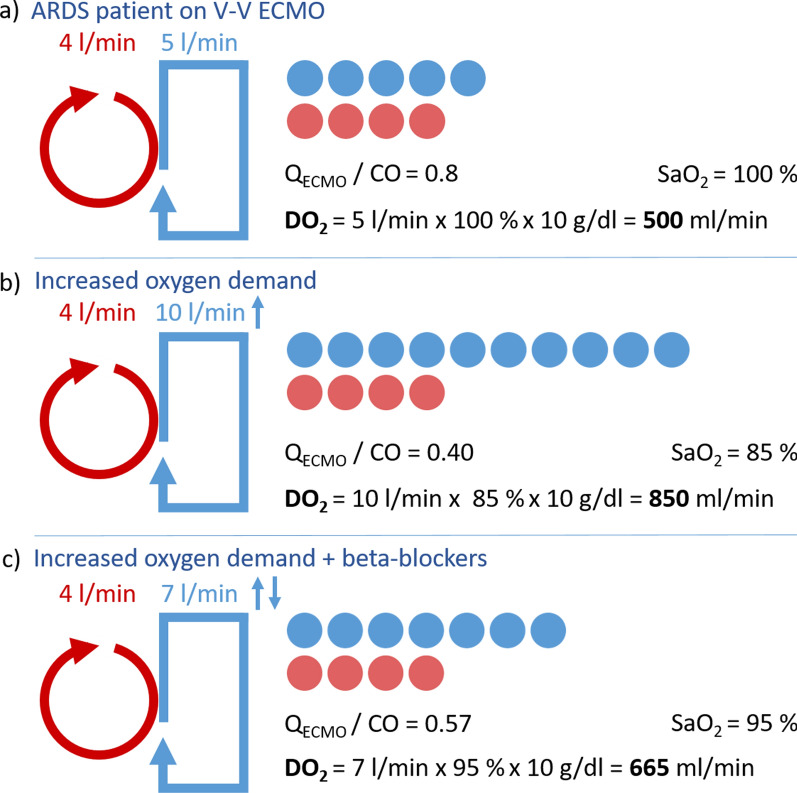
The correct Figure 1:
Fig. 1.
A Schematic representation of ECMO flow and cardiac output. Red indicates V-V ECMO flow, and blue indicates cardiac output. For illustrative purposes, recirculation is neglected; a Patient with ARDS and V-V ECMO support. The QECMO/CO ratio is 0.80, with saturation at 100%. DO2 is 500 ml/min. b The same patient with increased oxygen demand, for example, due to infection and fever. QECMO remains the same while CO is increased. This results in a ratio of 0.40, saturation of 85%, but a significantly increased DO2 of 850 ml/min. c Patient with increased oxygen demand treated with beta-blocker. The higher QECMO/CO ratio improved arterial oxygen saturation, but the DO2 drops to 665 ml/min. B Displays three ARDS patients undergoing V-V ECMO therapy, in whom beta-blockers were titrated based on their effects. The measurements were taken three times each after reaching a steady state
Figure 1 has been updated in this correction article and the original article [1] has been corrected.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Reference
- 1.Staudacher DL, Wengenmayer T, Schmidt M. Beta-blockers in refractory hypoxemia on venovenous extracorporeal membrane oxygenation: a double-edged sword. Crit Care. 2023;27:360. 10.1186/s13054-023-04648-7. [DOI] [PMC free article] [PubMed] [Google Scholar]