Abstract
Purpose
This study aimed to investigate the depression situation and the mediating role of fear of cancer recurrence (FCR) in the relationship between financial toxicity and depression in young breast cancer (BC) patient-family caregiver dyads.
Methods
A total of 196 young BC patient-family caregiver dyads at four hospitals in China were investigated. The Comprehensive scores for financial toxicity based on patient-reported outcome measures, the Hospital Anxiety and Depression Scale, and the FCR Inventory Short Form were assessed. The actor-partner interdependence mediation model using structural equation modelling in AMOS software was applied to examine the direct and indirect effects.
Results
In this study, there were 196 pairs of patients and family caregivers. The findings indicated a significant correlation between financial toxicity and FCR in both young BC patients and their family caregivers. Two significant partner effects were observed: the family caregiver’s financial toxicity significantly influenced the patient’s FCR (β=-0.450, P < 0.001), and the patient’s FCR influenced the family caregiver’s depression (β = 0.570, P < 0.001). Furthermore, financial toxicity in both young BC patients and family caregivers markedly affected both the actor and partner effects on dyadic depression, primarily through the patients’ FCR.
Conclusions
Depression in young BC patients was affected not only by themselves but also by their family caregivers. Emphasis should be placed on the interplay between financial toxicity and FCR of patients and family caregivers, with the aim of improving depression for young BC patients.
Clinical implications
The study emphasized the importance of addressing the experiences of both patient and family caregivers in clinical interventions. By demonstrating how financial toxicity and FCR are interlinked with depression in both parties, the study supports the development of we offer empirical support for developing comprehensive intervention strategies to alleviate mental distress and enhance mental health for patients and family caregivers.
Keywords: Young breast cancer patients, Depression, Financial toxicity, Fear of cancer recurrence, Actor-partner interdependence mediation model
Introduction
Breast cancer (BC) is the leading type of cancer in females [1]. Patients diagnosed at a young age constitute 15–25% of the total breast cancer cases in China [2]. Young breast cancer patients are the mainstay of their families and society, bearing enormous responsibility and facing high psychological pressure. They usually bear family and professional responsibilities and face unique socio-economic and psychological burdens at a critical stage of their lives. Compared to older adults, this increases their vulnerability to fear of cancer recurrence (FCR) and depression due to the high risk of recurrence, family responsibilities, and economic pressure [3–7]. Numerous studies have shown that paying attention to the mental health of young breast cancer patients will help improve the situation of life for patients [5, 8].
Based on the interdependent systems theory, major events such as cancer often cause more significant losses to the family or social network than to the individuals directly affected by the events themselves [9]. Consequently, as the primary family caregivers during the diagnosis and treatment phases of breast cancer patients, family caregivers experience significant psychological stress and an increased burden of care due to the impact of the disease [10, 11]. Family caregivers, while participating in treatment, not only need to provide emotional and life support for patients [12] but also face enormous economic pressure, which often leads to a series of psychological problems, such as depression and so on [13–15]. As a crucial source of support and foundation during the treatment and recovery of breast cancer patients, family caregivers’ attitudes, actions, and emotions are essential to patient outcomes and recovery [16, 17]. Therefore, it is imperative to study young cancer patients and their family caregivers as a holistic unit to understand better and address the intertwined physical and psychological health challenges they face. This approach is essential for developing comprehensive interventions to improve the overall well-being of patients and their family caregivers, ultimately enhancing treatment outcomes and quality of life.
For breast cancer patients, the process of cancer diagnosis and treatment refers to the chance of bringing significant psychological suffering to patients. Research [18] shows that depression, as a clinical condition and has associated depressive symptoms, will seriously affect the physiological function, psychological function, treatment compliance and quality of life of patients and may even be an essential factor causing the recurrence and death of breast cancer patients [19]. Research showed that the prevalence rate of young breast cancer patients during hospitalization was 17.9%, and after 12 months, the prevalence rate of depression was 8.5% [20]. As the family caregivers of breast cancer patients at the stage of disease diagnosis and treatment, they also have a substantial psychological distress and care burden [10]. While participating in treatment, breast cancer family caregivers should not only provide emotional and life support for patients but also face enormous economic pressure, which often leads to a series of psychological problems, such as depression. As an essential support and strong backing in the treatment and rehabilitation of breast cancer patients, the attitude, behaviour and emotions of family caregivers play a vital role in the treatment and recovery of patients. Negative emotions severely reduce their quality of life and affect the quality of care for patients [21]. Therefore, it is necessary to understand the depression of patients and their family caregivers.
Drawing upon the concept introduced by Zafar et al. in 2013, financial toxicity (FT) is defined as the significant financial burden and emotional distress caused to patients and their families because of the rising expense of cancer treatment [22]. Financial burden focuses on direct costs [23], and depending on the measures, the financial burden can reflect the perception and appraisal of the burden. Unlike financial burden, financial toxicity also encompasses the psychological distress from cancer-related expenses [24], reflecting the multidimensional impacts that financial challenges have on patient and family caregiver well-being. Due to the imbalance between treatment expenses and income, most survivors of malignant tumours are facing increasingly severe FT. The medical costs for cancer treatment in China continue to grow every year. Research shows that the cost of cancer treatment in China is as high as 392.462 billion yuan (1 yuan = 0.14 American dollars/0.11 British pounds) [25]. The National Cancer Center once carried out a survey targeting typical cancer patients, collecting data from 37 tertiary hospitals spread across 13 provinces and major cities in China. The data showed that among 14,594 cancer patients, the average expenditure per patient was 66,832 yuan, and the out-of-pocket expenditure was 33,948 yuan, accounting for 57.5% of household income [26]. Although China has established universal health coverage and out-of-pocket expenses have been reduced to around 35% of medical costs, the percentage of out-of-pocket expenses in private healthcare in China (78.8%) is still higher than in high-income countries such as the United States (20.9%) and the United Kingdom (53.1%) [26]. Studies have shown that families of cancer patients are more likely to experience FT [27, 28]. Prior research indicated that financial hardship was linked to more pronounced psychological symptoms, including anxiety and depression, thereby imposing heavier burdens on both patients and their family caregivers [29, 30]. However, most domestic and international scholars only analyzed the relevance between FT and depression at the patients’ level, leaving the FT in treating depression in family caregivers unclear and requiring deeper discussion.
The high cost and economic burden of cancer treatment significantly impact patients’ physical and mental health and should not be ignored. The study suggested that FT was the main reason for concerns about FCR [31]. FCR refers to the fear, worry, or anxiety about the recurrence or progression of cancer, which persists from the time of diagnosis throughout treatment and the survival period, causing considerable psychological stress to patients [32]. Young breast cancer patients usually have a higher risk of recurrence and genetic predisposition compared to elderly breast cancer patients [4, 33, 34]. Family caregivers bear the primary responsibility and financial burden for cancer patients and experience a high level of FCR [14, 35–37]. The FCR among family caregivers not only affects their mental health but is also more likely to increase harmful emotional levels in patients, such as depression [36–38]. In addition, several researchers have examined the relevance of the economic situation to FCR, suggesting that the financial situation may somewhat elevate the FCR among patients or family caregivers [39, 40]. FT encompasses both the monetary and psychological stress of cancer care, exacerbating FCR as financial stress heightens patient and family caregiver concerns about future well-being and treatment access [40]. Therefore, iit is necessary to discuss the relevance between FT, FCR, and depression in the patients-family caregiver dyad.
An increasing number of scholars encourage viewing cancer as a stressful event involving both patients and family caregivers, treating them as a dyadic unit during disease treatment, which is of significant importance for the health of the patient and the family caregiver [14, 41]. However, most current studies, both domestically and internationally, only explore the impacts of FT, FCR, and depression at the individual level of breast cancer patient-family caregiver dyads, and there is still a lack of exploration into the relationship between these variables at the dyadic level. In conclusion, this study set three sub-objectives: (1) to understand the depression situation of young breast cancer patients and their family caregivers; (2) to explore the relationship between FT and depression in young breast cancer patients and their family caregivers; (3) to explore the mediating role of FCR between FT and depression in young breast cancer patients and their family caregivers.
Methods
Participants
Between June 2020 and January 2021, researchers conducted surveys involving 212 pairs of young breast cancer patients and their family caregivers. Researchers conducted the study in four Grade-A hospitals, the highest classification in China’s healthcare system, which provide advanced oncology resources and serve as an ideal setting to access the target population of young breast cancer patients. We determined the sample size using AMOS 23.0 for APIMEM model analysis to ensure methodological rigour. Structural Equation Modeling (SEM) often requires a minimum of 5–10 participants per estimated parameter. It is generally believed that structural equations require 200 cases. SEM often requires a minimum of 5–10 participants per estimated parameter [42]. In this study, there were 14 variables, and the sample size for this study ranged from 70 to 140 dyads. We conducted a Monte Carlo simulation to confirm the adequacy of this sample size for detecting medium effect sizes with an alpha of 0.05 and a power of 0.80. The simulation further supported the requirement for at least 200 participants [43]. We also conducted a power analysis tailored to the Actor-Partner Interdependence Model with Mediation (APlMeM) framework. Utilizing the APlM Power app, designed explicitly for such models, we input parameters including an anticipated effect size of 0.3, a significance level of 0.05, and a desired power of 0.80. The analysis indicated that a sample size of approximately 150 dyads would be sufficient to detect medium effect sizes with the specified power.
The inclusion criteria for patients were: (1) female aged 18 to 40; (2) diagnosed with primary breast cancer, underwent cancer tissue resection surgery, and have less than 5 years postoperatively [44, 45]; (3) able to understand questionnaire content and oral communication; (4) willing to participate and express informed consent. The exclusion criteria were: (1) unaware of their cancer diagnosis; (2) suspected or undergone metastasis or recurrence; (3) being in weak health and unable to coordinate with this research; (4) cognitive dysfunction, psychiatric disorders, or prior psychotherapy.
The inclusion criteria for family caregivers were: (1) aged 18 years old and above; (2) able to read, comprehend, and express; and (3) voluntarily participating in this study. The exclusion criteria were: (1) physical severe illness; (2) cognitive impairment or mental illness.
In this study, researchers sent questionnaires to 205 dyads of cancer patients and family caregivers. One hundred ninety-six dyads of questionnaires were valid, yielding an effective response rate of 95.61%.
Measures
Fear of cancer recurrence inventory short form (FCRI-SF)
The FCRI-SF is an abbreviated form of the FCRI scale, consisting of seven dimensions: psychological stress, triggering factors, coping, self-awareness, functional impairment, sense of security, and severity [46]. The severity dimension exhibits a high degree of correlation with the overall FCRI score. Consequently, this FCRI-SF subscale is utilized to measure the degree of FCR in patients. It comprises nine items, each rated on a scale from 0 to 4, resulting in a maximum possible score of 36. A higher score means the patient has a more severe FCR. The critical score of this scale was 13 points [47]. Peng Li et al. [48] evaluated the reliability and validity of the Chinese version of the FCRI-SF scale by testing 207 breast cancer patients. Cronbach’s α for this study was 0.88.
Comprehensive scores for financial toxicity based on patient-reported outcome measures (COST-PROM)
This study employed the COST-PROM scale to assess FT [49]. This scale represents the world’s first specialized tool for evaluating FT in cancer patients, encompassing three dimensions: financial expenditure, financial resources, and patient social response, with 11 items in total. Utilizing the Likert 5-point scale, the total score is 44; lower scores mean more severe FT conditions. Yu Huihui et al. [50] conducted a study on the localization, reliability, and validity of the COST-PROM scale. Researchers have widely used this scale in Chinese patients and proven its reliability and validity. In this study, they reported a Cronbach’s α of 0.87.
Hospital anxiety and depression scale (HADS)
Clinicians extensively utilize HADS to examine an individual’s levels of depression and anxiety with 14 items. Each component includes seven items, each scored from 0 to 3, with a total possible score between 0 and 21 [51]. A higher score means more severe emotion in the participants. This study used the depression subscale. In this study, 8 points meet “the clinical cutoff for significant depressive symptoms [52]. The Chinese version, translated by Ye Weifei [53] and others in China, shows that HADS has good reliability and validity in the screening of anxiety and depression in patients in comprehensive hospitals, and the sensitivity and specificity of anxiety and depression emotions are both above 90%. Cronbach’sαfor this study was 0.82.
Statistical methods
We followed the methods of Lederman et al. [54] of the Actor-Partner Interdependence Mediation Model (APIMEM), an effective strategy for processing paired data. This suggests that dyad groups with intimate relationships, such as emotional cognition or behaviour, can influence each other and exhibit strong interpersonal interactions. This model can solve the problem of non-independence of data between partners to compensate for the shortcomings of traditional methods and can systematically explain the complex relationship between patients and family caregivers. Based on the binary data analysis, it can simultaneously estimate the actor partner effects of paired data. In APIMEM, the outcome variable can be predicted by its characteristics or behaviour, i.e. actor effects, or by the characteristics or behaviour of its partner, i.e. partner effects.
This study used SPSS 24.0 for descriptive statistics, Pearson correlation analysis and AMOS 23.0 for APIMEM model analysis. Researchers set the significance test at the two-tailed threshold, with P ≤ 0.05.
Results
Participants’ socio-demographic and clinical characteristics
In this study, researchers distributed questionnaires to a total of 212 pairs of breast cancer patients and their spouses, and ultimately, 196 pairs of breast cancer patient couples completed the questionnaire, yielding a response rate of 92.5%. Basic information on 196 patient-family caregiver dyads is shown in Table 1. 46 (23.5%) patients had depression, and 61 (31.1%) family caregivers had depression. The dyads were 34.83 ± 3.452 years old for patients and 39.52 ± 7.628 years old for family caregivers. 26 (13.3%) patients received breast-conserving surgery, 155 (79.1%) received chemotherapy, and 84 (42.9%) received radiotherapy.
Table 1.
Socio-demographic and clinical characteristics of patient-caregiver dyads
| Variables | Patients | Caregivers |
|---|---|---|
| (n = 196) N (%) | (n = 196) N (%) | |
| Educational level | ||
| Primary school and below | 6(3.1) | 14(7.1) |
| Junior high school | 72(36.7) | 78(39.8) |
| High school | 45(23.0) | 45(23.0) |
| University and college | 73(37.2) | 59(30.1) |
| Employment status | ||
| Employed | 180(91.8) | 184(93.9) |
| Unemployed | 16(8.2) | 12(6.1) |
| Nationality | ||
| the Han nationality | 182(92.9) | 177(90.3) |
| Other nationalities | 14(7.1) | 19(9.7) |
| Religion | ||
| No | 154(78.6) | 178(90.8) |
| Yes | 42(21.4) | 18(9.2) |
| Marital status | ||
| Married/Cohabiting partner | 192(98.0) | 187(95.4) |
| Unmarried | 1(0.5) | 2(1.0) |
| Divorced/Separated/Windowed | 3(1.5) | 7(3.6) |
| Chronic underlying diseases | ||
| No | 165(84.2) | 116(59.2) |
| Yes | 31(15.8) | 80(40.8) |
| Negative life events | ||
| No | 115(58.7) | 105(53.6) |
| Yes | 81(41.3) | 91(46.4) |
| Staging of breast diseases | ||
| I | 59(30.1) | |
| II | 88(44.9) | |
| III | 49(25.0) | |
| Breast conserving surgery | ||
| No | 170(86.7) | |
| Yes | 26(13.3) | |
| Chemotherapy | ||
| No | 41(20.9) | |
| Yes | 155(79.1) | |
| Radiotherapy | ||
| No | 112(57.1) | |
| Yes | 84(42.9) |
Correlations between FT, FCR and depression
Table 2 presents the Pearson correlations and means between FT, FCR and depression. The data revealed that patients’ FT decreased with increasing FCR levels, showing a strong negative correlation with patients (r = -0.979, P < 0.01) and family caregivers (r = -0.937, P < 0.01). Patients’ FT showed a significant association with depression in both patients (r = 0.878, P < 0.01) and family caregivers (r = -0.901, P < 0.01). Additionally, patients’ FCR was positively linked to depression levels in both the patients (r = 0.894, P < 0.01) and family caregivers (r = 0.910, P < 0.01), while it negatively correlated with the FT of family caregivers (r = -0.978, P < 0.01). Furthermore, patients’ depression demonstrated a significant negative relationship with FT (r = -0.872, P < 0.01) and a positive link with the family caregivers’ FCR (r = 0.866, P < 0.01). Similarly, family caregivers’ FT was negatively associated with both their FCR (r = -0.942, P < 0.01) and depression (r = -0.896, P < 0.01). Lastly, family caregivers’ FCR was positively related to their depression levels (r = 0.883, P < 0.01).
Table 2.
Inter-correlations, means, and SDs of the study variables for patient-caregiver dyads(N = 196 dyads)
| Patients | Caregivers | |||||
|---|---|---|---|---|---|---|
| FT | FCR | Depression | FT | FCR | Depression | |
| Patients | ||||||
| FT | 1.000 | |||||
| FCR | -0.979** | 1.000 | ||||
| Depression | -0.878** | 0.894** | 1.000 | |||
| Caregivers | ||||||
| FT | 0.992** | -0.978** | -0.872** | 1.000 | ||
| FCR | -0.937** | 0.957** | 0.866** | -0.942** | 1.000 | |
| Depression | -0.901** | 0.910** | 0.946** | -0.896** | 0.883** | 1.000 |
| Mean | 22.11 | 21.36 | 12.87 | 22.70 | 20.61 | 13.11 |
| SD | 12.750 | 6.651 | 4.931 | 12.727 | 7.102 | 4.784 |
Note. FT: financial toxicity; FCR: fear of cancer recurrence
**p < 0.01
The FT scores for patients and caregivers were 22.11 ± 12.750 and 22.70 ± 12.727, respectively, showing no statistically significant difference (t = -0.460, P = 0.646). Similarly, the FCR scores for patients and caregivers were 21.36 ± 6.651 and 20.61 ± 7.102, respectively, with no significant difference observed (t = 1.079, P = 0.281). Lastly, the depression scores for patients and caregivers were 12.87 ± 4.931 and 13.11 ± 4.784, respectively, again showing no statistically significant difference (t = -0.478, P = 0.633).
Actor–partner interdependence mediation model analysis
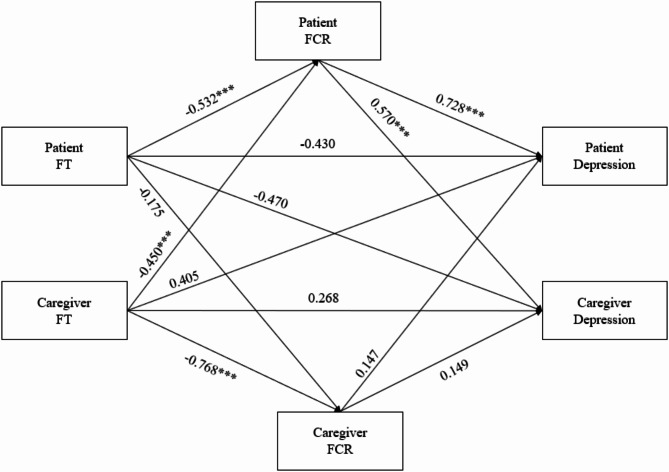
Figure 1 displays the APIMEM. The final APIMEM model examining dyadic effects of FT and FCR on depression produced a satisfactory model fit (χ2/df = 2.117, RMSEA = 0.075, CFI = 0.998, TLI = 0.994, NFI = 0.995). The results showed that the FT of patients had a negative actor effect on their own FCR (β=-0.532, P < 0.001). FCR of patients had a positive actor effect on their depression (β = 0.728, P < 0.001), and a positive partner effect on family caregivers’ depression (β = 0.570, P < 0.001). FT of family caregivers had a negative actor effect on their own FCR (β=-0.768, P < 0.001), and a negative partner effect on patients’ FCR (β=-0.450, P < 0.001).
Fig. 1.
APIMEM results of FT, FCR on depression
Note. APIMEM: Actor-partner interdependence mediation model; FT: financial toxicity; FCR: fear of cancer recurrence
Values are standardized coefficients
∗∗∗p < 0.001
A bootstrap method was applied to conduct the model, and the results showed that in the relationship between patients’ FT and their depression, their own FCR plays a partial mediating role (β=-0.150, P < 0.001, 95%CI=-0.286~-0.067), namely, the actor-actor effect of patients was established. In the relationship between family caregivers’ FT and their depression, patients’ FCR plays a partial mediating role (β=-0.096, P < 0.01, 95% CI =-0.213~-0.031), namely, the partner-partner effect of family caregivers was established. In the relationship between family caregivers’ FT and patients’ depression, patients’ FCR plays a partial mediating role (β=-0.127, P < 0.001, 95% CI =-0.258~-0.054), namely, the partner-actor effect of patients was established. In the relationship between patients’ FT and family caregivers’ depression, patients’ FCR plays a partial mediating role (β=-0.114, P < 0.01, 95% CI =-0.227~-0.040), namely, the actor-partner effect of family caregivers was established. The results of the direct effects and indirect effects of financial toxicity on depression are displayed in Table 3.
Table 3.
Standardized total effects, indirect effects, and direct effects of patients’ and caregivers’ FT on depression via FCR in the APIMEM
| Effect | Estimate | P(two-tailed) | 95%CI | ||
|---|---|---|---|---|---|
| Actor effect (individual’s FT-individual’s depression) | |||||
| Patient | Total effect | -0.326** | 0.005 | (-0.503, -0.108) | |
| Total IE | -0.160*** | 0.001 | (-0.289, -0.066) | ||
| Actor-actor simple IE | Patient FT-patient FCR-patient depression | -0.150*** | 0.000 | (-0.286, -0.067) | |
| Partner-partner simple IE | Patient FT-caregiver FCR-patient depression | -0.010 | 0.326 | (-0.085, 0.014) | |
| Direct effect | Patient FT-patient depression | -0.166 | 0.101 | (-0.360, 0.128) | |
| Caregiver | Total effect | -0.039 | 0.681 | (-0.229, 0.136) | |
| Total IE | -0.139*** | 0.000 | (-0.254, -0.063) | ||
| Actor-actor simple IE | Caregiver FT-caregiver FCR-caregiver depression | -0.043 | 0.168 | (-0.150, 0.017) | |
| Partner-partner simple IE | Caregiver FT-patient FCR-caregiver depression | -0.096** | 0.002 | (-0.213, -0.031) | |
| Direct effect | Caregiver FT-caregiver depression | 0.101 | 0.248 | (-0.079, 0.273) | |
| Partner effect (individual’s FT-partner’s depression) | |||||
| Patient | Total effect | -0.014 | 0.849 | (-0.231, 0.163) | |
| Total IE | -0.171*** | 0.000 | (-0.312, -0.076) | ||
| Actor-partner simple IE | Caregiver FT-caregiver FCR-patient depression | -0.044 | 0.232 | (-0.158, 0.029) | |
| Partner-actor simple IE | Caregiver FT-patient FCR-patient depression | -0.127*** | 0.000 | (-0.258, -0.054) | |
| Direct effect | Caregiver FT-patient depression | 0.157 | 0.114 | (-0.035, 0.334) | |
| Caregiver | Total effect | -0.300*** | 0.001 | (-0.475, -0.110) | |
| Total IE | -0.124** | 0.006 | (-0.235, -0.041) | ||
| Actor-partner simple IE | Patient FT-patient FCR-caregiver depression | -0.114** | 0.002 | (-0.227, -0.040) | |
| Partner-actor simple IE | Patient FT-caregiver FCR-caregiver depression | -0.010 | 0.302 | (-0.075, 0.012) | |
| Direct effect | Patient FT-caregiver depression | -0.176 | 0.074 | (-0.362, 0.017) | |
Note. APIMEM: Actor Partner Interdependence Mediation model; IE: indirect effect; CI: confidence interval; FT: financial toxicity; FCR: fear of cancer recurrence
Actor effect: Patient FT-Patient FCR; Caregiver FT-Caregiver FCR;
Patient FCR-Patient depression; Caregiver FCR- Caregiver depression;
Patient FT-Patient depression; Caregiver FT-Caregiver depression
Partner effect: Patient FT- Caregiver FCR; Caregiver FT- Patient FCR;
Patient FCR- Caregiver depression; Caregiver FCR- Patient depression;
Patient FT- Caregiver depression; Caregiver FT- Patient depression
Discussion
Previous limited studies primarily emphasized the actor effect between FT and depression. This study assessed the influence of FT on depression by examining the impact on individuals and their partners, as gauged by FCR. The study’s findings revealed several significant implications. FT in young breast cancer patients had an actor effect on depression through FCR. In addition, the family caregiver’s FT has a partner effect on the patient’s FCR, and the patient’s FCR has a partner effect on the family caregiver’s depression.
This study showed 46 (23.5%) patients had depression, and 61 (82.1%) family caregivers had depression. This suggests that depressive conditions are natural and occur at a higher rate among breast cancer patients and their family caregivers. The possible reason lies in the changes in role functioning after undergoing cancer diagnosis and surgical treatment, which triggers a series of fears [55]. Moreover, substantial treatment costs and worries about the family’s future can exacerbate the depressive state [55, 56]. FCR, or metastasis, may also be a significant cause of depression [55, 57].
Additionally, a comparison and analysis of the depression scores of 196 cancer patients and their family caregivers revealed significantly higher levels of depression in the family caregivers compared to the patients. Family caregivers need to provide continuous social support and daily nursing and confront the uncertainties associated with cancer patients. Consequently, this situation may lead to psychological strain and negative emotions, with depression sometimes surpassing the patients’ own experiences.
APIMEM demonstrated that FT experienced by young breast cancer patients and their family caregivers was related to their own FCR, reflecting an“actor effect” which aligned with prior research findings [31]. FT can result in individuals refusing follow-up examinations and decreasing medication adherence, significantly impacting their lifestyle, family roles, and interpersonal relationships [58] and ultimately heightening their personal FCR [55]. Furthermore, a vital discovery of this study was that the FT of family caregivers had a partner-to-partner effect on patients’ FCR. This may occur because, when confronted with FT, family caregivers might reveal their financial situation in patient interactions, which could exacerbate patients’ stress and guilt [55]. Consequently, this may lead to cost control measures that could potentially delay disease treatment and further influence FCR. However, this relationship was not found between the patient’s FT and the family caregiver’s FCR. This may be because when patients face economic pressure, they conceal it to alleviate family caregivers’ financial and psychological burden, thereby reducing their psychological distress and not affecting FCR.
This study revealed that patients’ FCR played a positive actor influence on their depression and a positive partner influence on family caregivers’ depression. When cancer patients experience FCR, they tend to pay too much attention to their physical condition, such as worrying about their health and changes in their body beyond normal levels. They use specific physical symptoms such as pain and discomfort as signals of worsening of the condition, which makes them unable to bear it psychologically and leads to depression [59]. Consequently, many patients, particularly young women, may develop apprehensions and fears about their future lives, fostering feelings of depression [3, 57, 59]. Additionally, this fear can adversely affect the family caregiver’s depressive mood [15, 35]. Upon investigation, cancer and its treatment are a collaborative process between patients and their family caregivers, with family caregivers being the primary source of emotional support throughout the entire treatment process. Binary studies on cancer indicate that the levels of pain for patients and family caregivers typically coexist, and an increase in one’s pain may ‘spill over’ and exacerbate the other’s pain [60]. The fear and uncertainty of cancer recurrence in patients may lead family caregivers to worry about their health, increase their caregiving burden and physical and mental exhaustion, and even impair their caregiving abilities, resulting in adverse psychological outcomes such as depression [61, 62]. Based on the literature review, there has been no research examining the partner effect of FCR on depression in both breast cancer patients and their family caregivers. This study serves as a valuable addition to the pertinent field.
The mediation results revealed that patients’ FT influenced their depression through FCR and played a partial mediating role. When patients face FT issues, individuals need to endure the double stress of the disease’s pain and medical costs, which exacerbates their fear and leads to more severe depression. However, this relationship was not found among the family caregivers. This may be because when family caregivers face economic difficulties or fear of disease recurrence, they rely heavily on the disease progression information provided by medical staff [63]. Family caregivers can maintain good communication with medical staff, promote information sharing, and improve psychological distress such as depression.
Additionally, this study discovered that FT could influence dyadic depression through patients’ FCR, which was the other important discovery of this research. The occurrence of such a relationship further underscores the need to survey the relationship between dyadic family caregivers’ FT, FCR, and depression. Patients and family caregivers, as the main body of the dyadic whole, are the primary source of mutual emotional support, and coping with the disease is of great significance for both parties [14]. When individuals face FT, good social support can help them show their inner thoughts about their cancer experience, encourage them to search for solutions, and reduce binary fear and depression. This result suggests that the coming survey should adopt effective measures to alleviate depression levels in both parties.
The clinical implications concerning FT in this study are significant, as they emphasize the need for healthcare systems and providers to address FT as a core component of cancer care, particularly for young breast cancer patients and their family caregivers. In clinical practice, integrating routine financial screenings and providing educational sessions on financial management resources within oncology settings could alleviate FT’s impact, supporting mental health outcomes for patients and family caregivers. Integrating financial counselling and dyadic support interventions in cancer care settings could alleviate FT, reduce FCR, and improve mental health outcomes for both patients and family caregivers.
Conclusion
FT in young breast cancer patients had an actor effect on depression through FCR. In addition, researchers identified two significant partner effects. The family caregiver’s FT has a partner effect on the patient’s FCR, and the patient’s FCR has a partner effect on the family caregiver’s depression. It is recommended that future research should concentrate on the FT, FCR and depression levels at a dyadic level.
Additional points
Limitations
Firstly, this was a cross-sectional study. It does not allow us to discern the dynamic shifts in FT, FCR, and depression among young cancer patients and family caregivers, nor can we infer causal relationships among the variables. Future longitudinal designs can delve deeper into the interplay between patients’ and family caregivers’ depression and related factors. Secondly, this study did not consider the relationship between patients and family caregivers; knowing each caregiver’s relationship to the patient (e.g., spouse, parent, sibling) could clarify how personal relationships impact psychological stress and FT, enhancing the dyadic analysis. Future research should consider this. Thirdly, researchers conducted this study in Grade-A hospitals, the highest tier in China’s healthcare system, which offers specialized oncology services. While this setting enables access to our target population, we should use broader sampling in future research to enhance generalizability. Finally, this study lacked contextual variables (social support networks, coping strategies, or pre-existing mental health conditions), socio-demographic variables (duration and stage of care) and socio-economic variables (income or health insurance status). Future research should consider these variables and control for confounding factors, as these factors may interact with financial and psychological stressors to shape dyadic health outcomes more comprehensively.
Acknowledgements
All authors would like to thank all the participants in this study.
Author contributions
Tianye Yang: Data curation, Writing-Original draft preparation.Zhu Zhu, Jianjun Shi, Lingling Tong and Jia Yang: Investigation, Data curation.Songli Mei & Hui Ren: Conceptualization, Methodology, Writing-Reviewing and Editing.
Funding
This study was supported by the 2024 Scientific Research Project of the Chinese Nursing Association (No.ZHKYQ202406), 2024 Nursing Research Fund of The First Hospital of Jilin University(No.HLKY20240101).
Data availability
The datasets generated and/or analysed during the current study are not publicly available due the protection of patient privacy, but are available from the corresponding author on reasonable request.
Declarations
Ethical approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the Public Health School of Jilin University (No.20191007).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Songli Mei, Email: meisongli@sina.com.
Hui Ren, Email: renhui2014@jlu.edu.cn.
References
- 1.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. Ca-a Cancer J Clin. 2021;71(3):209–49. [DOI] [PubMed] [Google Scholar]
- 2.Fan L, Strasser-Weippl K, Li J-J, St Louis J, Finkelstein DM, Yu K-D, Chen W-Q, Shao Z-M, Goss PE. Breast cancer in China. Lancet Oncol. 2014;15(7):E279–89. [DOI] [PubMed] [Google Scholar]
- 3.Fortin J, Leblanc M, Elgbeili G, Cordova MJ, Marin M-F, Brunet A. The mental health impacts of receiving a breast cancer diagnosis: a meta-analysis. Br J Cancer. 2021;125(11):1582–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schapira L, Zheng Y, Gelber SI, Poorvu P, Ruddy KJ, Tamimi RM, Peppercorn J, Come SE, Borges VF, Partridge AH, et al. Trajectories of fear of cancer recurrence in young breast cancer survivors. Cancer. 2022;128(2):335–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGrady ME, Willard VW, Williams AM, Brinkman TM. Psychological outcomes in adolescent and young adult Cancer survivors. J Clin Oncology: Official J Am Soc Clin Oncol. 2024;42(6):707–16. [DOI] [PubMed] [Google Scholar]
- 6.Ren H, Yang T, Yin X, Tong L, Shi J, Yang J, Zhu Z, Li H. Prediction of high-level fear of cancer recurrence in breast cancer survivors: an integrative approach utilizing random forest algorithm and visual nomogram. Eur J Oncol Nursing: Official J Eur Oncol Nurs Soc. 2024;70:102579. [DOI] [PubMed] [Google Scholar]
- 7.Iddrisu M, Aziato L, Dedey F. Psychological and physical effects of breast cancer diagnosis and treatment on young Ghanaian women: a qualitative study. BMC Psychiatry 2020, 20(1). [DOI] [PMC free article] [PubMed]
- 8.Mokhtari-Hessari P, Montazeri A. Health-related quality of life in breast cancer patients: review of reviews from 2008 to 2018. Health Qual Life Outcomes. 2020;18(1):338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Broderick. Understanding Family Process: Basics of Family Systems Theory. PsycCRITIQUES 1994, 39(12).
- 10.Fekih-Romdhane F, Henchiri H, Ridha R, Labbane R, Cheour M. Psychological distress and caregiving burden among spouses of women with breast cancer. Encephale-Revue De Psychiatrie Clinique Biol Et Therapeutique. 2019;45(2):190–2. [DOI] [PubMed] [Google Scholar]
- 11.Webb K, Sharpe L, Butow P, Dhillon H, Zachariae R, Tauber NM, O’Toole MS, Shaw J. Caregiver fear of cancer recurrence: a systematic review and meta-analysis of quantitative studies. Psycho-oncology. 2023;32(8):1173–91. [DOI] [PubMed] [Google Scholar]
- 12.Chen W, Li H, Cai J-Z, Qin N. Association between Dyadic Coping and Quality of life in breast Cancer patients and their spouses: an actor-partner interdependence mediation model. Asian Nurs Res. 2024;18(1):44–50. [DOI] [PubMed] [Google Scholar]
- 13.Grunfeld E. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. Can Med Assoc J. 2004;170(12):1795–801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li H, Sun Y, Yang T, Yin X, Zhu Z, Shi J, Tong L, Yang J, Ren H. Dyadic effects of financial toxicity and social support on the fear of cancer recurrence in breast cancer patients and caregivers: an actor–partner interdependence mediation model. BMC Nurs. 2024;23(1):378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bedaso A, Dejenu G, Duko B. Depression among caregivers of cancer patients: updated systematic review and meta-analysis. Psycho-oncology. 2022;31(11):1809–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bevan JL, Pecchioni LL. Understanding the impact of family caregiver cancer literacy on patient health outcomes. Patient Educ Couns. 2008;71(3):356–64. [DOI] [PubMed] [Google Scholar]
- 17.Nightingale CL, Sterba KR, McLouth LE, Kent EE, Dressler EV, Dest A, Snavely AC, Adonizio CS, Wojtowicz M, Neuman HB, et al. Caregiver engagement practices in National Cancer Institute Clinical Oncology Research Program settings: implications for research to advance the field. Cancer. 2021;127(4):639–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gold M, Dunn LB, Phoenix B, Paul SM, Hamolsky D, Levine JD, Miaskowski C. Co-occurrence of anxiety and depressive symptoms following breast cancer surgery and its impact on quality of life. Eur J Oncol Nurs. 2016;20:97–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang X, Wang N, Zhong L, Wang S, Zheng Y, Yang B, Zhang J, Lin Y, Wang Z. Prognostic value of depression and anxiety on breast cancer recurrence and mortality: a systematic review and meta-analysis of 282,203 patients. Mol Psychiatry. 2020;25(12):3186–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muzzatti B, Bomben F, Flaiban C, Piccinin M, Annunziata MA. Quality of life and psychological distress during cancer: a prospective observational study involving young breast cancer female patients. BMC Cancer 2020, 20(1). [DOI] [PMC free article] [PubMed]
- 21.Zhu P, Fu J-F, Wang B, Lin J, Wang Y, Fang N-N, Wang D-D. Quality of life of male spouse caregivers for breast Cancer patients in China. Asian Pac J Cancer Prev. 2014;15(10):4181–5. [DOI] [PubMed] [Google Scholar]
- 22.Zafar SY, Abernethy AP. Financial Toxicity, Part I: a new name for a growing problem. Oncology-New York. 2013;27(2):80–. [PMC free article] [PubMed] [Google Scholar]
- 23.Fernandez-Rodriguez EJ, Taboada-Taboada R, Garcia-Martin A, Sanchez-Gomez C, Saez-Gutierrez S, Rihuete-Galve MI, Fonseca-Sanchez E. Study on the additional financial burden of breast cancer disease on cancer patients and their families. Financial toxicity in cancer. Front Public Health 2024, 12. [DOI] [PMC free article] [PubMed]
- 24.Carrera PM, Kantarjian HM, Blinder VS. The Financial Burden and Distress of patients with Cancer: understanding and Stepping-Up action on the Financial toxicity of Cancer Treatment. Ca-a Cancer J Clin. 2018;68(2):153–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cai Y, Xue M, Chen W, Hu M, Miao Z, Lan L, Zheng R, Meng Q. Expenditure of hospital care on cancer in China, from 2011 to 2015. Chin J Cancer Res. 2017;29(3):253–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goss PE, Strasser-Weippl K, Lee-Bychkovsky BL, Fan L, Li J, Chavarri-Guerra Y, Liedke PER, Pramesh CS, Badovinac-Crnjevic T, Sheikine Y, et al. Challenges to effective cancer control in China, India, and Russia. Lancet Oncol. 2014;15(5):489–538. [DOI] [PubMed] [Google Scholar]
- 27.Gordon LG, Merollini KMD, Lowe A, Chan RJ. A systematic review of Financial Toxicity among Cancer survivors: we can’t pay the co-pay. Patient-Patient Centered Outcomes Res. 2017;10(3):295–309. [DOI] [PubMed] [Google Scholar]
- 28.Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: findings from a population-based national sample. Jnci-Journal Natl Cancer Inst. 2004;96(17):1322–30. [DOI] [PubMed] [Google Scholar]
- 29.Inguva S, Priyadarshini M, Shah R, Bhattacharya K. Financial toxicity and its impact on health outcomes and caregiver burden among adult cancer survivors in the USA. Future Oncol. 2022;18(13):1569–81. [DOI] [PubMed] [Google Scholar]
- 30.Chan RJ, Gordon LG, Tan CJ, Chan A, Bradford NK, Yates P, Agbejule OA, Miaskowski C. Relationships between Financial Toxicity and Symptom Burden in Cancer survivors: a systematic review. J Pain Symptom Manag. 2019;57(3):646–. [DOI] [PubMed] [Google Scholar]
- 31.Zhu Z, Xing W, Zhang X, Hu Y, So WKW. Cancer survivors’ experiences with financial toxicity: a systematic review and meta-synthesis of qualitative studies. Psycho-oncology. 2020;29(6):945–59. [DOI] [PubMed] [Google Scholar]
- 32.Chen Q, Weng Y, Wang F, Yang X, Chen W-T, Huang F. Fear of recurrence among Lung Cancer survivors. Cancer Nurs 2024. [DOI] [PubMed]
- 33.Abdulwassi HK, Amer IT, Alhibshi AH, Alnajjar AA, Bahatheq AK, Trabulsi NH, Nassif MO. Recurrence rates and long-term survival factors in young women with breast cancer. Saudi Med J. 2020;41(4):393–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gormley M, Ghazal L, Fu MR, Van Cleave JH, Knobf T, Hammer M. An Integrative Review on factors contributing to fear of Cancer Recurrence among Young adult breast Cancer survivors. Cancer Nurs. 2022;45(1):E10–26. [DOI] [PubMed] [Google Scholar]
- 35.Ağaç M, Üzar-Özçetin YS. Psychological resilience, metacognitions, and fear of recurrence among Cancer survivors and Family caregivers. Cancer Nurs. 2022;45(2):E454–62. [DOI] [PubMed] [Google Scholar]
- 36.O’Rourke L, Fisher PL, Campbell S, Wright A, Cherry MG. Factors Associated with fear of Cancer recurrence in Family caregivers of Cancer survivors: a systematic review. Front Psychol. 2021;12:625654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yang Y, Li W, Wen Y, Wang H, Sun H, Liang W, Zhang B, Humphris G. Fear of cancer recurrence in adolescent and young adult cancer survivors: a systematic review of the literature. Psycho-oncology. 2019;28(4):675–86. [DOI] [PubMed] [Google Scholar]
- 38.Mamudu L, Li J, McEligot AJ, Wood M, Rusmevichientong P, Tetteh-Bator E, Soale A-N, Fortenberry JD, Williams F. Cancer worry and its impact on self-reported depressive symptoms among adult males and females in the US: a nationwide sample study. BMC Psychiatry 2024, 24(1). [DOI] [PMC free article] [PubMed]
- 39.Kang D, Bae KR, Lim J, Kim N, Shim S, Kweon SS, Seo HJ, Cho J. Impact of objective financial burden and subjective financial distress on spiritual well-being and quality of life among working-age cancer survivors. Support Care Cancer. 2022;30(6):4917–26. [DOI] [PubMed] [Google Scholar]
- 40.Rogers SN, Monssen C, Humphris GM, Lowe D, Kanatas A. Which Head and Neck Cancer patients are most at risk of high levels of fear of Cancer recurrence. Front Psychol 2021, 12. [DOI] [PMC free article] [PubMed]
- 41.Li M, Zhang L, Li N, Luo X, Chen J, Zhang Y, Xiong C, Zhao M, Guo Z, Yan J. Effects of couple-based dyadic interventions on breast cancer patients and their intimate partners: a systematic review and meta-analysis. J Adv Nurs. 2023;79(9):3192–213. [DOI] [PubMed] [Google Scholar]
- 42.Liu N. The sample size estimation in quantitative nursing research. Chin J Nurs 2010.
- 43.Ledermann T, Rudaz M, Wu Q, Cui M. Determine power and sample size for the simple and mediation actor-Partner Interdependence Model. Fam Relat. 2022;71(4):1452–69. [Google Scholar]
- 44.Avis NE, Crawford S, Manuel J. Quality of life among younger women with breast cancer. J Clin Oncol. 2005;23(15):3322–30. [DOI] [PubMed] [Google Scholar]
- 45.Costanzo ES, Lutgendorf SK, Mattes ML, Trehan S, Robinson CB, Tewfik F, Roman SL. Adjusting to life after treatment: distress and quality of life following treatment for breast cancer. Br J Cancer. 2007;97(12):1625–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Simard S, Savard J. Fear of Cancer Recurrence Inventory: development and initial validation of a multidimensional measure of fear of cancer recurrence. Support Care Cancer. 2009;17(3):241–51. [DOI] [PubMed] [Google Scholar]
- 47.Simard S, Savard J. Screening and comorbidity of clinical levels of fear of cancer recurrence. J Cancer Surviv. 2015;9(3):481–91. [DOI] [PubMed] [Google Scholar]
- 48.Peng L, Huang W, Zhang W, Xu Y, Lu F, Zhong L, Chen X, Xu S, Chen W, Li M. Psychometric properties of the short form of the fear of Cancer Recurrence Inventory (FCRI) in Chinese breast Cancer survivors. Front Psychiatry 2019, 10. [DOI] [PMC free article] [PubMed]
- 49.de Souza JA, Yap BJ, Hlubocky FJ, Wroblewski K, Ratain MJ, Cella D, Daugherty CK. The development of a financial toxicity patient-reported outcome in Cancer the COST measure. Cancer. 2014;120(20):3245–53. [DOI] [PubMed] [Google Scholar]
- 50.Yu HH, Bi X, Liu YY. Reliability and validity of the Chinese version on Comprehensive scores for Financial Toxicity based on the patient-reported outcome measures (in Chinese). Chin J Epidemiol. 2017;38(8):1118–20. [DOI] [PubMed] [Google Scholar]
- 51.Zigmond AS, Snaith RP. THE HOSPITAL ANXIETY AND DEPRESSION SCALE. Acta Psychiatrica Scandinavica. 1983;67(6):361–70. [DOI] [PubMed] [Google Scholar]
- 52.Alves ML, Vieira JE, Silva Telles Mathias LA, Gozzani JL. Preoperative coping mechanisms have no predictive value for postoperative pain in breast cancer. Revista Brasileira De Psiquiatria. 2013;35(4):364–8. [DOI] [PubMed] [Google Scholar]
- 53.Ye W. Application and evaluation of comprehensive hospital anxiety and depression scale in patients of comprehensive hospitals (in Chinese). Chin J Behav Med. 1993;000(003):17–9. [Google Scholar]
- 54.Ledermann T, Macho S, Kenny DA. Assessing mediation in Dyadic Data using the actor-Partner Interdependence Model. Struct Equation Modeling-a Multidisciplinary J. 2011;18(4):595–612. [Google Scholar]
- 55.Chan RJ, Gordon LG, Tan CJ, Chan A, Bradford NK, Yates P, Agbejule OA, Miaskowski C. Relationships between Financial Toxicity and Symptom Burden in Cancer survivors: a systematic review. J Pain Symptom Manag. 2019;57(3):646–e660641. [DOI] [PubMed] [Google Scholar]
- 56.Kang D, Bae KR, Lim J, Kim N, Shim S, Kweon SS, Seo HJ, Cho J. Impact of objective financial burden and subjective financial distress on spiritual well-being and quality of life among working-age cancer survivors. Supportive care cancer: Official J Multinational Association Supportive Care Cancer. 2022;30(6):4917–26. [DOI] [PubMed] [Google Scholar]
- 57.Yang Y, Sun H, Luo X, Li W, Yang F, Xu W, Ding K, Zhou J, Liu W, Garg S, et al. Network connectivity between fear of cancer recurrence, anxiety, and depression in breast cancer patients. J Affect Disord. 2022;309:358–67. [DOI] [PubMed] [Google Scholar]
- 58.Thom B, Benedict C. The impact of Financial Toxicity on Psychological Well-Being, coping Self-Efficacy, and cost-coping behaviors in young adults with Cancer. J Adolesc Young Adult Oncol. 2019;8(3):236–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Liu J, Peh CX, Simard S, Griva K, Mahendran R. Beyond the fear that lingers: the interaction between fear of cancer recurrence and rumination in relation to depression and anxiety symptoms. J Psychosom Res. 2018;111:120–6. [DOI] [PubMed] [Google Scholar]
- 60.Hagedoorn M, Sanderman R, Bolks HN, Tuinstra J, Coyne JC. Distress in couples coping with cancer: a meta-analysis and critical review of role and gender effects. Psychol Bull. 2008;134(1):1–30. [DOI] [PubMed] [Google Scholar]
- 61.Shi Y, Dai J, Kuai B, Su X, Yang R, Gong S, Guo Y. Impact of fear of recurrence in patients with cancer on caregivers’ psychological health: a meta-analysis. Asia Pac J Oncol Nurs. 2023;10(10):100299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Shen Z, Zhang L, Shi S, Ruan C, Dan L, Li C. The relationship between uncertainty and fear of disease progression among newly diagnosed cancer patients: the mediating role of intolerance of uncertainty. BMC Psychiatry 2024, 24(1). [DOI] [PMC free article] [PubMed]
- 63.Yao H, Hou Y, Zhang X, Zhang Q. Extrinsic emotional regulation experienced by lung cancer patients and their family caregivers during progression-free survival. Eur J Cancer Care 2022, 31(6). [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analysed during the current study are not publicly available due the protection of patient privacy, but are available from the corresponding author on reasonable request.