Abstract
Purpose
The COVID-19 pandemic has disrupted healthcare access and telemedicine has been widely deployed. The aim of this study is to assess the impact of this health crisis on treatment consumption and telemedicine development in outpatients treated by oral anti-cancer agents and followed by the Oncoral hospital/community multidisciplinary program where continuity care is maintained by a pharmacist/nurse pair.
Methods
A prospective monocentric study was conducted among cancer patients who received Oncoral telephone follow-up during the 1st lockdown in France using a 56-item questionnaire which covered sociodemographic data, patient medication management, and telehealth.
Results
178 patients received Oncoral follow-up during the 1st lockdown and 67.4% responded to the questionnaire. During lockdown, 9.2% of patients took medication or CAM for fatigue, 6.7% for mood alteration, 10.8% for sleep disorder, 11.7% for stress and anxiety, and 12.5% to get more energy. Homeopathy consumption was triggered by the pandemic. Habits about getting drugs from the pharmacy changed significantly (p < 0.001), while other treatment habits did not. 83% of patients were satisfied by the telephone follow-up established, 69% would be in favor of repeating this in case of a new epidemic wave. Those most in favor of using telemedicine seemed to be the youngest (p < 0.001), with several dependent children (p < 0.007), high school degree or higher education (p = 0.023), and in work (p < 0.001).
Conclusion
Health system reorganization enables to limit the impact of the crisis on patients’ drug use in oncology care. Telemedicine is a promising public health tool.
Keywords: Oral anti-cancer agent, Pharmacist, Oncoral, Telemedicine, COVID-19
Introduction
The COVID-19 pandemic (Coronavirus Disease 19) had a sudden and profound impact on healthcare access throughout the world, starting January 2020 (Slimano et al. 2020). Specific measures were taken, including strict lockdowns (Contreras et al. 2020; Clement et al. 2021; Minichsdorfer et al. 2021; Edge et al. 2021). Cancer patients were identified as being at high risk of COVID-19, with severe complications and high mortality due to their age, comorbidities, polymedication, and treatments liable to impair immunity (Dai et al. 2020; Pourroy et al. 2020; Lee et al. 2020; Jansen and Amesz 2021). What was at stake for these patients was not to allow lockdown to delay treatment, with exacerbated risk of progression leading to a 6–13% increase in risk of death for 4 weeks’ delay in treatment (Hanna et al. 2020; Gualdi et al. 2021). This vulnerable population requires protection without jeopardizing cancer treatment and the continuity of care. This led to a huge growth in telemedicine, enabling remote management by telephone or connected platforms (Elbeddini et al. 2020; Jansen and Amesz 2021; Alwhaibi et al. 2021; Fiske et al. 2021; DGOS_Michel.C and DGOS_Michel.C 2022a, b).
The European Society for Medical Oncology (ESMO) recommended transferring patients on oral drugs to tele-oncology services for consultations and prescription renewals, and to use the telephone and online platforms as aids for managing symptoms and adverse effects, including dose adjustment and referral to support care. Efficient scheduling of appointments and encouragement to implement telemedicine limited time in hospital and optimized cancer care pathway (Shirke et al. 2020; Leung et al. 2020; ESMO 2023). Throughout the world, health professionals mobilized and adapted so as to ensure effective care, enabling patients to maintain treatment and contact without jeopardy to their health or at least with minimal impact (Paterson et al. 2020). Drug management was also affected during this period. Supply times were longer with unforeseen shortages (Alexander et al. 2020; Edge et al. 2021). Patients hoarded treatments massively at home for cardiovascular diseases and diabetes, and the number of anxiolytic and sleeping pill prescriptions soared (Clement et al. 2021; Alwhaibi et al. 2021; Elbeddini et al. 2020; Fiske et al. 2021).
In this context, pharmacy teams, in the community and in hospital, were called upon to secure the supply and use of oral anti-cancer drugs. Within the multidisciplinary community/hospital Oncoral care pathway, pharmaco-therapeutic follow-up of outpatients receiving oral anti-cancer treatment was to be continued, while adhering to measures to limit patients’ traveling and COVID-19 risk. Thus, whenever possible during the first lockdown in France, telephone interviews replaced the follow-up consultations that were traditionally conducted face-to-face in the hospital. This prospective study aimed to assess the impact of the COVID-19 health crisis on medical drug consumption and management, and on adoption of telemedicine (telephone follow-up, Information Technology (IT) resources available, and influence of sociodemographic factors) in outpatients treated by oral anti-cancer agents and followed in the Oncoral program during lockdown.
Material and methods
Population and study design
This study was conducted on adult patients beginning oral anti-cancer treatment in the Lyon Sud University Hospital (Hospices Civils de Lyon, France) and followed by the Oncoral outpatient pathway.Oncoral is a multidisciplinary program for patients receiving oral anti-cancer agents in which the hospital team works alongside community health professionals, including the community pharmacist, general practitioner, and home nurse. After the initial consultation with the hospital oncologist, the patient attends regular interviews with a clinical pharmacist specializing in oncology and a nurse (Prely et al. 2021; Collomb et al. 2022). Between interviews a telephone platform is available for patients to answer any questions on symptoms, adverse effects, or drug use. The program began in the Lyon Sud University Hospital (Hospices Civils de Lyon, France) in 2014. Prior to the pandemic all the interviews were face to face.
During lockdown, interviews at the hospital were replaced by telephone contact, to avoid patients having to travel from home to the hospital and thus limit their COVID-19 risk. The study population comprised all patients receiving Oncoral follow-up by telephone during the first French lockdown from March 16 to May 11, 2020. This non-interventional study, including human subjects, was approved by the data protection commission and was registered with ClinicalTrials.gov under n° NCT05069662. All participants provided written informed consent to processing of their personal data, in line with the Declaration of Helsinki. This study was registered with the French national data protection commission as authorized by the Hospices Civils de Lyon (n° 15-122).
Data collection
Data covering the topics listed in Table 1 were sourced from a questionnaire, computerized medical records, and records of interventions. The questionnaire was designed by 3 Oncoral pharmacists and comprised 54 closed and 2 open questions. The closed questions were either bimodal (“yes/no”) or categorical (Not at all/A little/Quite/A lot or 0–4 numerical scale). Where possible, the questionnaire was administered by pharmacist by telephone. If this was not feasible, it was done by face-to-face interview during a pre-scheduled consultation with the hospital oncologist, or by mail. Anonymized data were recorded on Excel.
Table 1.
Study data collected by topic and method
| Topic | Detail | Method of data collection |
|---|---|---|
| Sociodemographic data | Age, gender, family situation, educational level, socio-occupational category, household monthly income | Computerized records or interview |
| Type of cancer | Hematologic cancer and solid tumour | Computerized records |
| Drug habits before, during and after lockdown | Medication management, habits about getting drugs from the pharmacy, omission rate | Questionnaire |
| Chronic treatment drugs and complementary and alternative medicationsa taken | Focus on medications or CAM taken for fatigue, mood alteration, sleep disorder, stress and anxiety, getting more energy | Questionnaire |
| COVID-related lifestyle factors | Hygiene and diet, distancing measures, healthcare access logistics | Questionnaire |
| Access to online equipment | IT resources available, ease with using IT | Questionnaire |
| Perception of telephone follow-up | Involvement and quality of the interview | Questionnaire |
| Pharmacist and/or nurse interventions during Oncoral follow-up | Interventions included management of Patient-Reported Outcomes and adverse effects, advice on taking prescribed or non-prescribed medications or CAM, prevention of drug interactions, and community/hospital coordination. Standard ratings were applied, based on French Clinical Pharmacology Society (SFPC) guidelines (Allenet et al. 2006) | Oncoral data |
aCAM by definition included all approaches not recognized by conventional medicine: homeopathy, acupuncture, chiropractic, phytotherapy, and massage therapy (Gaboury et al. 2016). The questionnaire specifically focused on homeopathy and phytotherapy
Follow-up parameters and statistics
Descriptive analysis was conducted with mean, median values (with IQR), and counts (with proportions). Significant change over time (before, during, and after lockdown) was assessed on p-values using R software, version 4.2.1, and the mixcat and lme4 packages, with the significance threshold set at p < 0.05. Two models were used to estimate p-values: a cumulative mixed-effects logistic model for single-choice questions, treating responses as multinomial variables; and a mixed-effects logistic regression model for multiple-choice questions, with each possible response treated as a binary variable. P-values were computed using a likelihood ratio test between models with and without the time component (before lockdown, during, and after) among predictors.
For description of the population, χ2 or Fisher tests were used to compare categorical variables and the Wilcoxon–Mann–Whitney test was used to compare continuous variables.
Results
Population characteristics
178 patients receiving oral anti-cancer drugs had telephone follow-up during the first lockdown, 120 of whom (67.4%) responded to the questionnaire and only 1 patient was lost to follow-up.
The demographics of the patients who reported being at ease or not with telemedicine are shown in Table 2. Mean age was 70.5 ± 12.5 years (range 34–94 years) and patients were mostly retired (75%). Sex ratio was 1. Patients were being treated for a range of cancers. Seventy-eight patients (65%) were treated for hematologic cancer (53% multiple myeloma, 17% chronic lymphoid leukemia) and 42 for solid tumor (72% breast, 19% prostate, 5% melanoma, 5% digestive, 3% lung). 82% lived with at least one other person. 88% had children. Patients were locked down with their spouse and/or children, except for 18 (15%) locked down alone. 36% had a low educational level (junior high school diploma, or none). 39% spent more than an hour traveling to hospital (including 7% more than 2 h).
Table 2.
Patients’ sociodemographic data, online habits (equipment and daily screen time), means of travel, and ease with the telemedicine
| Variable | Ease with telemedicine | ||||
|---|---|---|---|---|---|
| N | Overall, N = 114 | No, N = 55 | Yes, N = 59 | p-value | |
| Sex, n (%) | 114 | 0.58 | |||
| Female | 55 (48) | 28 (51) | 27 (46) | ||
| Male | 59 (52) | 27 (49) | 32 (54) | ||
| Age, Median (IQR) | 114 | 73 (65–79) | 76 (70–82) | 69 (58–74) | < 0.001 |
| Live alone, n (%) | 114 | 0.17 | |||
| No | 93 (82) | 42 (76) | 51 (86) | ||
| Yes | 21 (18) | 13 (24) | 8 (14) | ||
| Child, n (%) | 114 | 0.67 | |||
| No | 14 (12) | 6 (11) | 8 (14) | ||
| Yes | 100 (88) | 49 (89) | 51 (86) | ||
| Number of dependent children, n (%) | 102 | 0.007 | |||
| 0 | 81 (79) | 42 (88) | 39 (72) | ||
| 1 | 8 (7.8) | 4 (8.3) | 4 (7.4) | ||
| 2 | 10 (9.8) | 0 (0) | 10 (19) | ||
| 3 | 2 (2.0) | 1 (2.1) | 1 (1.9) | ||
| 4 | 1 (1.0) | 1 (2.1) | 0 (0) | ||
| Unknown | 12 | 7 | 5 | ||
| Household income (€), n (%) | 109 | 0.65 | |||
| No household income | 1 (0.9) | 0 (0) | 1 (1.9) | ||
| 380–609 | 2 (1.8) | 1 (1.8) | 1 (1.9) | ||
| 610–759 | 2 (1.8) | 1 (1.8) | 1 (1.9) | ||
| 760–1069 | 2 (1.8) | 1 (1.8) | 1 (1.9) | ||
| 1070–1369 | 8 (7.3) | 6 (11) | 2 (3.7) | ||
| 1370–1829 | 11 (10) | 7 (13) | 4 (7.4) | ||
| 1830–2289 | 15 (14) | 6 (11) | 9 (17) | ||
| 2290–3049 | 13 (12) | 5 (9.1) | 8 (15) | ||
| 3050–4569 | 18 (17) | 7 (13) | 11 (20) | ||
| ≥ 4570 | 3 (2.8) | 1 (1.8) | 2 (3.7) | ||
| No answer | 34 (31) | 20 (36) | 14 (26) | ||
| Unknown | 5 | 0 | 5 | ||
| Education level, n (%) | 111 | 0.023 | |||
| No diploma or school certificate | 41 (37) | 27 (51) | 14 (24) | ||
| Bachelor's degree | 29 (26) | 13 (25) | 16 (28) | ||
| 2 years of higher education after bachelor’s degree | 21 (19) | 6 (11) | 15 (26) | ||
| 3 years of higher education after bachelor’s degree | 6 (5.4) | 3 (5.7) | 3 (5.2) | ||
| More than 5 years of higher education after bachelor’s degree | 14 (13) | 4 (7.5) | 10 (17) | ||
| Unknown | 3 | 2 | 1 | ||
| Professional situation, n (%) | 114 | < 0.001 | |||
| Work stoppage | 13 (11) | 3 (5.5) | 10 (17) | ||
| No stable employment (CDD, interim) | 1 (0.9) | 0 (0) | 1 (1.7) | ||
| Part-time job | 1 (0.9) | 0 (0) | 1 (1.7) | ||
| Full-time job | 10 (8.8) | 0 (0) | 10 (17) | ||
| Retired | 85 (75) | 51 (93) | 34 (58) | ||
| Jobless | 4 (3.5) | 1 (1.8) | 3 (5.1) | ||
| Socio-professional category, n (%) | 114 | < 0.001 | |||
| Farmer, owner | 1 (0.9) | 0 (0) | 1 (1.7) | ||
| Other activities or jobless | 8 (7.0) | 2 (3.6) | 6 (10) | ||
| Managers and Professional | 9 (7.9) | 2 (3.6) | 7 (12) | ||
| Employee | 12 (11) | 1 (1.8) | 11 (19) | ||
| Retired | 84 (73.6) | 50 (91) | 34 (58) | ||
| Online equipment (smartphone, tablet or computer), n (%) | 114 | < 0.001 | |||
| No | 24 (21) | 22 (40) | 2 (3.4) | ||
| Yes | 90 (79) | 33 (60) | 57 (97) | ||
| Regularly use of smartphone, tablet, or computer, n (%) | 109 | < 0.001 | |||
| No | 39 (36) | 32 (64) | 7 (12) | ||
| Yes | 70 (64) | 18 (36) | 52 (88) | ||
| Unknown | 5 | 5 | 0 | ||
| Travel time between home and hospital, n (%) | 113 | 0.091 | |||
| > 2 h | 8 (7.1) | 7 (13) | 1 (1.7) | ||
| Between 1 and 2 h | 36 (32) | 14 (26) | 22 (37) | ||
| Between 30 min and 1 h | 40 (35) | 21 (39) | 19 (32) | ||
| Less than 30 min | 29 (26) | 12 (22) | 17 (29) | ||
| Unknown | 1 | 1 | 0 | ||
No patients contracted COVID-19 during the first lockdown. When asked, 61% (n = 73) believed themselves more likely to contract COVID-19 because of their cancer and 32% because of their treatment.
Ownership and usage of online equipment
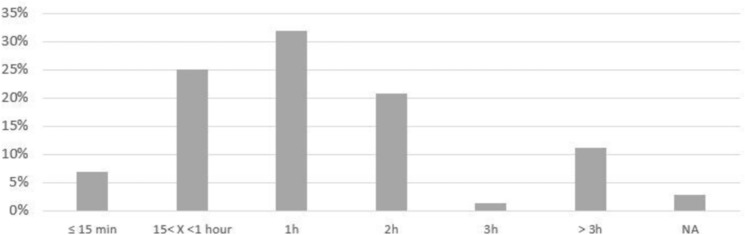
The majority of patients (79%) had access to equipment to enable them to get online (smartphone, tablet, or computer) and that was recent enough to use for telemedicine. Most (67%) were satisfied with their internet connection. 64% regularly used their devices with about a third using them for less than an hour a day, a third (32%) for 1 h a day and a third for 2 h or more. Patients most likely to own online equipment tended to be younger (mean age 69 years) than those who did not (mean age 76 years).
Changes in treatment habits with lockdown
Some treatment habits remained unchanged during lockdown. 47% of patients (n = 56) received daily help from their family for managing treatment: preparing the drugs, being reminded, and moral support. Lockdown did not significantly affect these habits (p = 0.64). There was also no significant change in the rate of omitting to take the oral anti-cancer treatment: however, 8% (n = 9) of patients encountered treatment interruptions, concerning anti-cancer drugs (procarbazine, venetoclax) in 2 cases, for less than a week. Patients reported no change in the time needed for prescription filling in the pharmacy (about 15 min).
There was, however, a change in the habits of patients and their families for getting drugs from the pharmacy (p < 0.001), with alternatives implemented, such as drug delivery by the pharmacist to the patient’s helpers, home delivery, or postal delivery.
During lockdown, 9.2% of patients took medication or CAM (homeopathy, phytotherapy) for fatigue, 6.7% for mood alteration, 10.8% for sleep disorder, 11.7% for stress and anxiety, and 12.5% to get more energy. In some cases, this was exclusively during lockdown (Table 3). The drugs and/or CAM were prescribed or recommended by the patient’s general practitioner (GP) in 45% of cases, by the oncologist in 19%, and by the pharmacist in 19% (83% of which by the community pharmacist). Before/during/after comparison showed that this consumption was triggered by the pandemic and maintained over time in the case of anti-fatigue drugs (before/during: p < 0.001 then before/after: p = 0.023), and homeopathy for mood alteration (p = 0.002 then p = 0.002), insomnia (p = 0.001 then p = 0.001), and to get more energy (p = 0.023 then p = 0.023) (Table 4).
Table 3.
Number of patients taking drugs or CAM for specific symptoms during lockdown
| Fatigue | Mood alteration | Sleep | Stress/anxiety | Energy | |
|---|---|---|---|---|---|
| Number of patients’ users during lockdown (n = , % overall population) | 11 (9.2%) | 8 (6.7%) | 13 (10.8%) | 14 (11.7%) | 15 (12.5%) |
| Among this patients, comparison of number of patients’ users before and after lockdown | |||||
| Number of patients’ users before (n) | 6 | 6 | 10 | 12 | 9 |
| Number of patients’ users after (n) | 6 | 7 | 11 | 14 | 11 |
| Number of patients’ users only during lockdown (n) | 4 | 0 | 1 | 0 | 4 |
Table 4.
Changes in medication use for different symptoms (p values) over time
| Symptoms | No | Homeopathy | Drug | Phytotherapy |
|---|---|---|---|---|
| Before, during, and after lockdown | ||||
| Fatigue | 0.003 | 0.4 | 0.003 | > 0.9 |
| Mood alteration | 0.7 | 0.005 | 0.7 | |
| Sleep | 0.4 | 0.002 | 0.7 | 0.4 |
| Stress/anxiety | 0.3 | > 0.9 | 0.12 | |
| Energy | 0.023 | 0.036 | < 0.001 | > 0.9 |
| Before and during lockdown | ||||
| Fatigue | < 0.001 | 0.025 | < 0.001 | > 0.9 |
| Mood alteration | > 0.9 | 0.002 | 0.4 | |
| Sleep | > 0.9 | 0.001 | 0.4 | > 0.9 |
| Stress/anxiety | 0.5 | > 0.9 | > 0.9 | 0.023 |
| Energy | 0.005 | 0.023 | < 0.001 | > 0.9 |
| Before and after lockdown | ||||
| Fatigue | 0.4 | > 0.9 | 0.023 | > 0.9 |
| Mood alteration | 0.5 | 0.002 | > 0.9 | |
| Sleep | 0.2 | 0.001 | 0.4 | 0.031 |
| Stress/anxiety | 0.016 | > 0.9 | 0.007 | > 0.9 |
| Energy | 0.4 | 0.023 | > 0.9 | > 0.9 |
Empty cells: no estimation due to identical distribution for a given drug/symptom pair across at least two time periods
Perception of telephone follow-up and telemedicine
All patients had telephone follow-up during lockdown. 83% were satisfied and 69% would be in favor of repeating this in case of a new epidemic wave. 71% felt well involved in the exchanges with the hospital telephone follow-up team (Fig. 1).
Fig. 1.
Mean daily screen time for patients regularly using online equipment
Thirty-eight patients had previously already had a teleconsultation. Fifty-five (46%) did not feel at ease with using telemedicine via an app. 18% (n = 22) thought a tutorial could help in using the app, and 25% (n = 30) would ask to be accompanied. Those in favor of using telemedicine were the youngest (median age, 69 years, compared to the overall median age of 76; p < 0.001), with several dependent children (p < 0.007), with high school degree or higher education (p = 0.023), and in work (p < 0.001) (Table 2).
48% (n = 57) of patients found that teleconsultation did not match the quality of face-to-face accompaniment, and 9% (n = 11) had doubts about the confidentiality of the exchanges.
Teleconsultation does not require travel. Means of travel to the hospital for face-to-face oncology consultation comprised: 53% (n = 63) transport covered by national health insurance, either taxi (46%, n = 55) or ambulance (7%, n = 8); 29% (n = 35) their own vehicle or 11% (n = 13) by car with accompaniment; 5% (n = 6) public transport; and 3% (n = 3) with no data. Home-to-hospital travel time was ≥ 1 h for 39% of patients (n = 47).
Interest of Oncoral remote follow-up and interventions
During lockdown, follow-up enabled 61 Oncoral interventions by the pharmacist and nurse, for 42 patients. 51% (n = 31) were during an incoming call from the patient or family, 38% (n = 23) during an outgoing call from the team, and 11% (n = 7) during a scheduled interview. The mean number of interventions was 1.45 ± 0.8 per patient.
Reasons for intervention concerned continuity of care and community/hospital coordination (34%, n = 21), management of Patient-Reported Outcomes and adverse effects (23%, n = 14), non-adherence (20%, n = 12), advice on a new drug or CAM with risk of interaction with the oral anti-cancer agent (15%, n = 9), or contraindications or dose adjustment (3%, n = 2). The Oncoral team involved the oncologist in 25 interventions (41%): in 36% of cases for management of adverse effects (skin rash, edema, etc.) and in 32% for community/hospital coordination (e.g., prescription validity, preparation for surgery, etc.) The community pharmacist was involved in 20% of cases, mainly to coordinate drug ordering with the patient or family member coming to the pharmacy (83%).
Discussion
The organization of cancer care was strongly impacted by the COVID-19 pandemic. Screening, diagnosis and treatment initiation sometimes had to be deferred, which might even jeopardize prognosis (Australia 2020; Sutherland et al. 2020). Outpatient follow-up was disturbed and care-teams had to adapt to ensure optimal management with remote accompaniment of treatment (Elbeddini et al. 2020; Dhawan et al. 2020). Thus, in the Oncoral multidisciplinary community/hospital follow-up of outpatients receiving oral anti-cancer drugs, the usual in-hospital face-to-face interviews conducted by the pharmacist and the nurse were replaced by remote interviews. As well as the scheduled interviews and help to care-givers, patients could interact on demand with the pharmacist and the nurse by phone or secure messaging.
Patient adherence to treatment changed during the pandemic: those under tacrolimus or opioids were more adherent than others, while those taking contraceptives or anti-psychotics were more at risk of treatment interruption (Clement et al. 2021). In the present study, patients reported that lockdown did not affect their treatment omissions with oral anti-cancer drugs. Interruptions were very rare in the study population, despite shortages in the early phase of the pandemic (Elbeddini et al. 2020; Clement et al. 2021). The Oncoral team’s follow-up was able to be maintained, limiting the impact of the crisis on patients’ drug use (Bassan et al. 2014).
Cancer patients are exposed to episodes of stress and anxiety, and the epidemic was expected to have a psychological impact on them (Nikbakhsh et al. 2014; Pitman et al. 2018; Naser et al. 2021). Before the pandemic, in the USA Hawkins et al. reported two-fold higher use of treatments for anxiety (16.8% versus 8.6%) and depression (14.1% versus 7.8%) in cancer patients compared to the general population. Some cancers are associated with elevated use of psychotropic drugs: patients with prostate cancer consume lower drugs, including psychotropic drugs, than those with cancer of the ovaries or uterus or with low life expectancy (Hawkins et al. 2017). Risk of depression can be higher for patients who had experienced lockdown as reported in a German study (Fiske et al. 2021). The present study highlighted significant progression in the use of homeopathy for sleep disorder, mood alteration and energy gain and this change seemed to be triggered by the onset of the pandemic. Therefore, close follow-up by first-line care providers is of great importance.
Patients could call on the Oncoral pharmacist and/or nurse for advice during lockdown, ensuring the safety of drug treatment. Pharmaceutic interventions concerned community/hospital coordination (e.g., defective prescription, difficulty in ordering, etc.) and management of adverse effects (e.g., digestive disorder requiring associate symptomatic treatment, skin rash requiring the oncologist’s medical opinion, etc.). The pharmacist/nurse pair played a central role in the link-up between the hospital professionals and the private-sector community professionals, to optimize global care. For example, over the same period in 2019, there were 429 Oncoral interventions involving 173 patients. These interventions highlighted the need for continuous follow-up, and telemedicine made a major contribution to this during the crisis, in agreement with previous studies (Contreras et al. 2020; Mann et al. 2020; O’Hara et al. 2020).
Telemedicine is a promising public health tool, developed particularly for patients with chronic disease (2009, LOI n° 2009–879; Finnane et al. 2017; Hanlon et al. 2017). In oncology, connected digital tools can optimize follow-up, improve patient-caregiver communication, reduce delay in managing Patient-Reported Outcomes and adverse effects, and develop educational programs with specific accompaniment (Odeh et al. 2015b; Basch et al. 2016; Mir 2020). This is why, in the present study, patients were asked about resources to enable home monitoring via connected equipment. More than three-quarters had Internet access via a computer, smartphone, or tablet, which almost half of these used regularly. These results in the Oncoral population confirm the findings of Kempf et al., in a population followed in medical oncology departments, with a median age of 68 years, which found a similar proportion of outpatients with functioning Internet access and an age effect, whereby Internet use decreased with increasing age, and an impact of socioeconomic context (Kempf et al. 2016). One common hindrance in telemedicine is advanced patient age, older patients having less IT equipment and computer literacy; this was apparent in the present study, patients at ease with the telemedicine being significantly younger. Nevertheless, the 80% rate of satisfaction with telephone follow-up shows that practices are evolving and holds out hope for elderly patients to be able to take advantage of e-medicine programs; opening up telemedicine to older patients would greatly increase its use (Badawy and Radovic 2020; O’Hara et al. 2020; Omboni et al. 2022). And indeed, elderly persons are increasingly using digital tools in fields apart from health: news, recipes, games, etc. (Amelis 2021). Tele-oncology can improve cancer care coordination by enabling early detection and prompt treatment of adverse events, improving access, and promoting education; time and cost savings are to be expected (Shirke et al. 2020).
During the COVID-19 pandemic, telephone follow-up contributed to continuity of care and limiting viral exposure; none of the study patients reported contracting the infection during lockdown. Subsequent development of telemedicine could use a secure videoconference system (Edge et al. 2021). Without replacing hospital consultations, telemedicine could reduce the need for patient travel: for 30% of patients, to home-to-hospital trip was longer than 1 h; dedicated medical transport costs could be reduced, with their impact on social and geographic inequality, which is a major concern (Assurance Maladie 2013; Institut National du Cancer 2021). Videoconferences can also serve as a teaching aid, by projecting educational documents and running workshops enabling the patient to be actively involved in management, e.g., patients could present the medications they have at home and discuss indications and dosages with the pharmacist. For the Oncoral team, radical improvements could be made to the digital solutions that are being developed to enable remote workshops. Patients confirmed that tutorials could help them in setting up these services, and the Oncoral team is therefore now providing patients, in the first interview, with a document explaining telemedicine. Although satisfied with telephone follow-up, patients reported preferring face-to-face accompaniment, which the literature confirms: they highlight their hesitations in using IT equipment and their doubts that the quality of care is as good and as personalized (Cox et al. 2017; Sansom-Daly and Bradford 2020). The present study confirmed that age and social conditions, such as the number of dependent children, educational level, and socio-occupational category, have an impact on the ease with which patients can take part in telemedicine. IT equipment may be lacking for the most socially vulnerable, and telemedicine risks becoming an aggravating factor in unequal access to therapeutic innovation. This is a point on which health professionals developing telemedicine need to be vigilant, to make sure that telemedicine is a means of facilitating access to innovation for all, and not yet another source of inequality.
The study limitations include its single-center design and outcomes are therefore dependent of care team; however, such multidisciplinary community/hospital care pathway are scarce and have to be more common. The small sample size, the heterogeneity of treatments, and diseases may preclude demonstrating some statistical significances, but it is one of the strengths of Oncoral program: real-world data from patients with all types of cancers.
Conclusion
The COVID-19 pandemic greatly changed care access during lockdown. However, the health system was reorganized so as to limit impact. Telemedicine played a major role. Its development needs to be associated to assessment of its clinical utility, accessibility, and use for accompanying outpatients, who are ever more numerous, while respecting a strict legal framework and taking care not to exacerbate inequalities in access to innovation and new means of organizing healthcare.
Author contributions
V Larbre, AG Caffin, M Maire, F Ranchon and C Rioufol contributed to the design of the study and writing of the manuscript. P. Reymond and Y. Ladjouzi contributed to data collection. N. Romain-Scelle and D. Maucort-Boulch contributed to statistical analysis. All authors reviewed and approved the manuscript.
Funding
There were no sources of funding associated with this manuscript.
Declarations
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Alexander M, Jupp J, Chazan G et al (2020) Global oncology pharmacy response to COVID-19 pandemic: Medication access and safety. J Oncol Pharm Pract 26:1225–1229. 10.1177/1078155220927450 [DOI] [PubMed] [Google Scholar]
- Allenet B, Bedouch P, Rose F-X (2006) Standardisation et Valorisation des activités de Pharmacie Clinique ACT-IP. http://www.actip.sfpc.eu/actip/index/ficheip. Accessed 24 Mar 2022
- Alwhaibi A, Alrwaished A, Binobydaan SM et al (2021) Role of pharmacist during COVID-19 pandemic: a retrospective study focused on critically ill COVID-19 patients. Saudi Pharm J 29:1050–1055. 10.1016/j.jsps.2021.07.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amelis (2021) Quels sont les avantages et usages d’Internet pour les personnes âgées ? In: Institut Amelis. https://institut.amelis-services.com/bien-vieillir/vie-sociale-fetes/internet-chez-les-seniors/. Accessed 18 Feb 2023
- Assurance Maladie (2013) Guide de prise en charge des frais de transport de patients. https://sante.gouv.fr/IMG/pdf/Guide_de_prise_en_charge_des_frais_de_transport_de_patients.pdf
- Australia C (2020) Review of the impact of COVID-19 on medical services and procedures in Australia utilising MBS data: Skin, breast and colorectal cancers, and telehealth services. https://www.canceraustralia.gov.au/publications-and-resources/cancer-australia-publications/review-impact-covid-19-medical-services-and-procedures-australia-utilising-mbs-data-skin-breast-and. Accessed 29 Dec 2021
- Badawy SM, Radovic A (2020) Digital approaches to remote pediatric health care delivery during the COVID-19 Pandemic: existing evidence and a call for further research. JMIR Pediatr Parent 3:e200449. 10.2196/20049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Basch E, Deal AM, Kris MG et al (2016) Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol 34:557–565. 10.1200/JCO.2015.63.0830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bassan F, Peter F, Houbre B et al (2014) Adherence to oral antineoplastic agents by cancer patients: definition and literature review. Eur J Cancer Care 23:22–35. 10.1111/ecc.12124 [DOI] [PubMed] [Google Scholar]
- Clement J, Jacobi M, Greenwood BN (2021) Patient access to chronic medications during the Covid-19 pandemic: evidence from a comprehensive dataset of US insurance claims. PLoS ONE 16:e0249453. 10.1371/journal.pone.0249453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collomb B, Dubromel A, Caffin AG et al (2022) Assessment of patient reported outcomes (PROs) in outpatients taking oral anticancer drugs included in the real-life Oncoral program. Cancers (basel) 14:660. 10.3390/cancers14030660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contreras CM, Metzger GA, Beane JD et al (2020) Telemedicine: patient-provider clinical engagement during the COVID-19 pandemic and beyond. J Gastrointest Surg 24:1692–1697. 10.1007/s11605-020-04623-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cox A, Lucas G, Marcu A et al (2017) Cancer survivors’ experience with telehealth: a systematic review and thematic synthesis. J Med Internet Res 19:e6575. 10.2196/jmir.6575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai M, Liu D, Liu M et al (2020) Patients with cancer appear more vulnerable to SARS-CoV-2: a multicenter study during the COVID-19 outbreak. Cancer Discov 10:783–791. 10.1158/2159-8290.CD-20-0422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- DGOS_Michel.C, DGOS_Michel.C (2022a) La télésurveillance : ETAPES. In: Ministère de la Santé et de la Prévention. https://solidarites-sante.gouv.fr/soins-et-maladies/prises-en-charge-specialisees/telesante-pour-l-acces-de-tous-a-des-soins-a-distance/article/la-telesurveillance-etapes. Accessed 4 Dec 2022a
- DGOS_Michel.C, DGOS_Michel.C (2022b) La télésanté. In: Ministère de la Santé et de la Prévention. https://solidarites-sante.gouv.fr/soins-et-maladies/prises-en-charge-specialisees/telesante-pour-l-acces-de-tous-a-des-soins-a-distance/article/la-telesante. Accessed 4 Dec 2022b
- Dhawan N, Prommer E, Sinclair CT, Subbiah IM (2020) Development of a patient-centered framework for oncology clinicians to address uncertainty in cancer care during the COVID-19 pandemic. Curr Treat Options Oncol 21:99. 10.1007/s11864-020-00795-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edge R, Meyers J, Tiernan G et al (2021) Cancer care disruption and reorganisation during the COVID-19 pandemic in Australia: a patient, carer and healthcare worker perspective. PLoS ONE 16:e0257420. 10.1371/journal.pone.0257420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbeddini A, Prabaharan T, Almasalkhi S, Tran C (2020) Pharmacists and COVID-19. J Pharm Policy Pract 13:36. 10.1186/s40545-020-00241-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- ESMO Cancer Patient Management During the COVID-19 Pandemic. https://www.esmo.org/guidelines/cancer-patient-management-during-the-covid-19-pandemic. Accessed 26 Apr 2023
- Finnane A, Dallest K, Janda M, Soyer HP (2017) Teledermatology for the diagnosis and management of skin cancer: a systematic review. JAMA Dermatol 153:319–327. 10.1001/jamadermatol.2016.4361 [DOI] [PubMed] [Google Scholar]
- Fiske A, Schneider A, McLennan S et al (2021) Impact of COVID-19 on patient health and self-care practices: a mixed-methods survey with German patients. BMJ Open 11:e051167. 10.1136/bmjopen-2021-051167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaboury I, Johnson N, Robin C et al (2016) Médecines alternatives et complémentaires. Can Fam Physician 62:e767–e771 [PMC free article] [PubMed] [Google Scholar]
- Gualdi G, Porreca A, Amoruso GF et al (2021) The effect of the COVID-19 lockdown on melanoma Diagnosis in Italy. Clin Dermatol 39:911–919. 10.1016/j.clindermatol.2021.05.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanlon P, Daines L, Campbell C et al (2017) Telehealth interventions to support self-management of long-term conditions: a systematic metareview of diabetes, heart failure, asthma, chronic obstructive pulmonary disease, and cancer. J Med Internet Res 19:e172. 10.2196/jmir.6688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanna TP, King WD, Thibodeau S et al (2020) Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 371:m4087. 10.1136/bmj.m4087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins NA, Soman A, Buchanan Lunsford N et al (2017) Use of medications for treating anxiety and depression in cancer survivors in the United States. J Clin Oncol 35:78–85. 10.1200/JCO.2016.67.7690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institut National du Cancer (2021) Le Plan cancer, 2014–2019. Institut National du Cancer [Google Scholar]
- Jansen C, Amesz B (2021) Every day counts Covid19. In: Ventura. https://www.efpia.eu/media/602636/every-day-counts-covid19-addendum.pdf. Accessed 27 Feb 2022
- Kempf E, Prévost A, Rousseau B et al (2016) Les patients ambulatoires atteints de cancer sont-ils prêts pour la télémédecine ? Bull Cancer 103:841–848. 10.1016/j.bulcan.2016.06.004 [DOI] [PubMed] [Google Scholar]
- Lee LYW, Cazier J-B, Starkey T et al (2020) COVID-19 prevalence and mortality in patients with cancer and the effect of primary tumour subtype and patient demographics: a prospective cohort study. Lancet Oncol 21:1309–1316. 10.1016/S1470-2045(20)30442-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung MST, Lin SG, Chow J, Harky A (2020) COVID-19 and Oncology: Service transformation during pandemic. Cancer Med 9:7161–7171. 10.1002/cam4.3384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loi (2009) Loi n° 2009–879. https://www.legifrance.gouv.fr/loda/id/JORFTEXT000020879475
- Mann DM, Chen J, Chunara R et al (2020) COVID-19 transforms health care through telemedicine: Evidence from the field. J Am Med Inform Assoc 27:1132–1135. 10.1093/jamia/ocaa072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Minichsdorfer C, Jeryczynski G, Krall C et al (2021) Impact of COVID-19 lockdown on routine oncology versus emergency care at a high volume cancer centre. Eur J Clin Investig 51:e13623. 10.1111/eci.13623 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mir O (2020) The Capri Program proves clinical and economic efficiency for personalized remote monitoring of patients treated with oral anticancer drugs. ASCO [Google Scholar]
- Naser AY, Hameed AN, Mustafa N et al (2021) Depression and anxiety in patients with cancer: a cross-sectional study. Front Psychol 12:585534. 10.3389/fpsyg.2021.585534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nikbakhsh N, Moudi S, Abbasian S, Khafri S (2014) Prevalence of depression and anxiety among cancer patients. Casp J Intern Med 5:167–170 [PMC free article] [PubMed] [Google Scholar]
- O’Hara VM, Johnston SV, Browne NT (2020) The paediatric weight management office visit via telemedicine: pre- to post-COVID-19 pandemic. Pediatr Obes 15:e12694. 10.1111/ijpo.12694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Odeh B, Kayyali R et al (2015) Optimizing cancer care through mobile health - PubMed. Support Care Cancer 23:2183–2188. 10.1007/s00520-015-2627-7 [DOI] [PubMed] [Google Scholar]
- Omboni S, Padwal RS, Alessa T et al (2022) The worldwide impact of telemedicine during COVID-19: current evidence and recommendations for the future. Connected Health 1:7–35. 10.20517/ch.2021.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paterson C, Bacon R, Dwyer R et al (2020) The role of telehealth during the COVID-19 pandemic across the interdisciplinary cancer team: implications for practice. Semin Oncol Nurs 36:151090. 10.1016/j.soncn.2020.151090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pitman A, Suleman S, Hyde N, Hodgkiss A (2018) Depression and anxiety in patients with cancer. BMJ 361:k1415. 10.1136/bmj.k1415 [DOI] [PubMed] [Google Scholar]
- Pourroy B, Tournamille JF, Bardin C et al (2020) Providing oncology pharmacy services during the coronavirus pandemic: French Society for Oncology Pharmacy (Société Francaise de Pharmacie Oncologique [SFPO]) Guidelines. JCO Oncol Pract. 10.1200/OP.20.00295 [DOI] [PubMed] [Google Scholar]
- Prely H, Herledan C, Caffin AG et al (2021) Real-life drug-drug and herb-drug interactions in outpatients taking oral anticancer drugs: comparison with databases. J Cancer Res Clin Oncol. 10.1007/s00432-021-03645-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sansom-Daly UM, Bradford N (2020) Grappling with the “human” problem hiding behind the technology: telehealth during and beyond COVID-19. Psychooncology 29:1404–1408. 10.1002/pon.5462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shirke MM, Shaikh SA, Harky A (2020) Implications of Telemedicine in oncology during the COVID-19 pandemic. Acta Biomed 91:e2020022. 10.23750/abm.v91i3.9849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slimano F, Baudouin A, Zerbit J et al (2020) Cancer, immune suppression and Coronavirus Disease-19 (COVID-19): need to manage drug safety (French Society for Oncology Pharmacy [SFPO] guidelines). Cancer Treat Rev. 10.1016/j.ctrv.2020.102063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland K, Chessman J, Zhao J (2020) Impact of COVID-19 on healthcare activity in NSW Australia. PHRP. 10.17061/phrp3042030 [DOI] [PubMed] [Google Scholar]