Abstract
Purpose
We present a case of ocular trauma following use of a virtual reality (VR) headset.
Observations
A 37-year-old female with history of a wall collision while wearing a VR headset presented with a 3-week history of floaters in the right eye. On fundoscopic exam, she was noted to have a fibrous floater in the right eye for which she underwent vitrectomy with improvement of symptoms.
Conclusions and importance
This is the first report we have found of VR headset-associated ocular injury. Given the rising use of VR in various fields, it is important to continue to track ocular incidents from the use of VR headsets to be able to recommend effective safety recommendations.
Keywords: Virtual reality (VR), Headset, Ocular trauma, Ocular injury, Floaters
1. Introduction
Virtual reality (VR) headsets are becoming more accessible to the general public with various companies having released headsets, including the Oculus Rift (owned by Facebook) and the Playstation VR (created by Sony).1 VR is not only prominent in the gaming and entertainment industries but also in other areas, including the military and medical professions.2,3 However, while the various benefits of VR have been studied, there are also adverse effects from the use of VR headsets. Reports of dermatological, neurological, and spinal injuries associated with the use of such headsets have been published.4, 5, 6 With this paper, we would like to present a case of ocular trauma associated with the use of a VR headset.
2. Case report
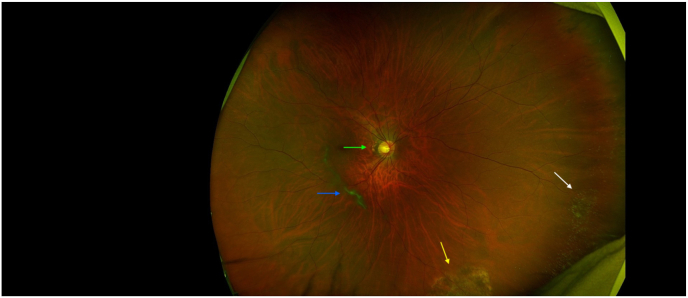
A 37-year-old female presented for evaluation of a floater in the right eye for the past 3 weeks. She was noted to have thrust herself into a brick wall one year ago while wearing an Oculus 5 (a VR gaming headset). While she reported prior instances of head injury, this was the first time she had experienced ocular sequelae following head trauma. Best-corrected visual acuity was noted to be 20/30 (OD) and 20/60-2 (OS). On dilated fundus exam of the right eye, a highly fibrous cigar-shaped floater was noted along with other vitreous opacities (Fig. 1). The vitreous of the left eye was clear without hemorrhage, cells, or pigment.
Fig. 1.
Wide-angle fundus photograph (Optos) right eye demonstrating the central cigar-shaped floater opacity (blue arrow), myopic crescent (green arrow), and inferior laser scar around lattice (yellow arrow) and nasal peripheral cystoid changes (white arrow). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
The patient was consented to undergo a vitrectomy for removal of floaters in the right eye. Due to the presence of lattice degeneration and atrophic retinal hole in the eye to be operated on, the patient was treated with laser before surgery. Patient was also found to have severe dry eyes with an initial score of 18 on the Speed 2 dry eye questionnaire, likely due to her work requiring heavy computer use and wearing contact lens for a extended period of time. This was maximized before her vitrectomy with Tranquileye compresses, BlephEx and Lipiflow treatments, and artificial tears and lid scrub as needed. Her Speed 2 score improved to a 3 before surgery.
She had the vitrectomy done 2 months after her initial visit. On postoperative day 1, visual acuity was noted to be 20/500 (OD) and dilated funduscopic exam (OD) showed a 30 % air bubble. Visual acuity improved up to 20/20 (OD) 13 days after the vitrectomy was done, with no floaters observed by the patient or on a fundoscopic exam. Her postoperative course was complicated by hypotony; her ocular pressure was 2 (OD) on postoperative day 1. To treat this, the patient was given Prolensa QD, Pred Forte every 2 hours, and atropine QD; she was also advised to sleep on her left side. Her ocular pressure increased to 6 on postoperative day 6, and to 10 on postoperative day 7.
3. Discussion/conclusion
Vitreous floaters are common as we age, due to the natural liquefaction and contraction of the vitreous gel in the posterior chamber that typically leads to a posterior vitreous detachment over time. However, other factors can contribute to the development of floaters, such as inflammatory conditions, recent eye surgery, and ocular injury.
Our patient had no history of inflammatory eye disease or recent ocular procedures. However, she was in a younger demographic and experienced recent head trauma with her collision into a wall while wearing an Oculus 5 VR headset, leading us to believe this persistent, visually significant floater was brought about by a trauma-related posterior vitreous detachment. There have also been cases of patients presenting with new onset floaters after sustaining blunt force trauma to the eye.7,8 Of note, our patient did not present with any retinal tears as the previously mentioned cases did, which was likely why she did not present to the clinic sooner. She underwent a vitrectomy for her symptoms and fundoscopic exam findings, resulting in the improvement of both.
From our literature review, we were unable to find previous reports on ocular trauma related to the use of VR headsets. With their rising ease of accessibility and the various fields they are being implemented in, it will become more important to monitor the incidence of ocular injury related to VR headsets and to consider ways in which the risk of inducing such injury can be mitigated.
CRediT authorship contribution statement
Lauren Dimalanta: Writing – original draft. Robin Ross: Writing – review & editing, Supervision, Data curation, Conceptualization.
Patient consent
The patient consented to publication of the case orally.
Claim of priority
After a literature search utilizing PubMed using the keywords “VR trauma ocular injury”, we did not find any prior reports of ocular trauma associated with the use of a VR headset and would like to present one such case.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Funding
No funding or grant support.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
None.
References
- 1.Virtual reality headset. Wikipedia. Published January 15, 2024. Accessed January 21, 2024. https://en.wikipedia.org/wiki/Virtual_reality_headset#cite_note-38.
- 2.Harris D.J., Arthur T., Kearse J., et al. Exploring the role of virtual reality in military decision training. 2023. 4. [DOI]
- 3.Mao R.Q., Lan L., Kay J., et al. Immersive virtual reality for surgical training: a systematic review. J Surg Res. 2021;268:40–58. doi: 10.1016/j.jss.2021.06.045. [DOI] [PubMed] [Google Scholar]
- 4.Moreau T., Benzaquen M., Gueissaz F. Erythema ab igne after using a virtual reality headset: a new phenomenon to know. Bern Open Reposit Inform Syst (University of Bern) 2022;36(11) doi: 10.1111/jdv.18371. [DOI] [PubMed] [Google Scholar]
- 5.Warner N., Teo J.T. Neurological injury from virtual reality mishap. BMJ Case Rep. 2021;14(10) doi: 10.1136/bcr-2021-243424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Baur D., Pfeifle C., Heyde C.E. Cervical spine injury after virtual reality gaming: a case report. J Med Case Rep. 2021;15(1) doi: 10.1186/s13256-021-02880-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiner A.J., Rao P., Williams G.A. Large traumatic retinal dialysis associated with prominent vitreous base avulsion. Ophthalmic surgery, lasers & imaging retina. 2018 doi: 10.3928/23258160-20180831-14. Published online September 1. [DOI] [PubMed] [Google Scholar]
- 8.Mandviwala M.M., Sassani P.P. Traumatic retinal detachment caused by nerf gun shot in a pediatric patient. Retin Cases Brief Rep. 2021;15(5):568–570. doi: 10.1097/icb.0000000000000853. [DOI] [PubMed] [Google Scholar]