Abstract
Purpose
Complementary and alternative medicine (CAM) use is common amongst cancer patients. However, there is growing concern about its safety and efficacy. Online crowdfunding campaigns represent a unique avenue to understand the cancer patient’s perspective for using CAM or declining conventional cancer therapy (CCT).
Methods
Five hundred GoFundMe campaigns from 2012 to 2019 detailing financial need for cancer treatment were randomly selected and reviewed for endorsement of CAM use, reasons for using CAM, and reasons for declining CCT. Descriptive statistics were used to compare patient and campaign characteristics between 250 CAM users and 250 non-CAM users.
Results
Compared to non-CAM users, CAM users were more likely to be female (70% vs. 54%, p < 0.01), to report more stage IV cancer (54% vs. 12%, p < 0.01), and to have a history of delayed, missed, or misdiagnosis (10% vs. 4%, p < 0.01). Reasons for using CAM include endorsing curative/therapeutic effects 212 (85%), pain/stress reduction 137 (55%), and dissatisfaction with current or past medical treatment options 105 (42%). 87 (35%) CAM users that declined CCT reported that they wanted to try to fight off cancer using CAM first 57 (61%), that CCT was too “toxic” to the body 39 (42%), and cancer was already too advanced, so that CCT would be futile or too aggressive 25 (27%).
Conclusion
Cancer patients on GoFundMe using CAM highly value quality of life, comfort, and autonomy. Physicians should educate themselves on CAM to set realistic expectations and provide comprehensive counseling of the risks and benefits of CAM usage to patients who choose to use CAM to either augment or completely replace CCT.
Keywords: Complementary and alternative medicine, Social media, Crowdfunding, Cancer treatment, Patient perspective
Introduction
The national cost for cancer care is substantial, with expenditures totaling an estimated $125 billion in 2010 (Mariotto et al. 2010). Many cancer patients have turned to crowdfunding, the practice of soliciting monetary contributions through social media, to cover costs (Cohen et al. 2019). In addition to conventional cancer therapy (CCT) such as surgery, chemotherapy, and radiation, many cancer patients seek to crowdfund for complementary and alternative medicine (CAM) treatments as part of their medical care (Snyder and Caulfield 2019). A greater percentage of cancer patients use CAM than the general population (Anderson and Taylor 2012), with an estimated 48–84% of cancer patients reporting using CAM as part of their therapy (Johnson et al. 2018a; Richardson et al. 2000).
While there are many published studies extolling the benefits of CAM use as an adjunct to CCT (Richardson et al. 2000; Mansky and Wallerstedt 2006), there is still growing concern regarding the safety of CAM use (Snyder and Caulfield 2019), particularly when used as the sole cancer treatment. Furthermore, prior studies have found an association with CAM use and increased mortality mediated from refusal of CCT (Johnson et al. 2018a, b). Medical crowdfunding for CAM may thus represent an avenue that enables cancer patients to raise funds for unproven and potentially dangerous treatment options (Vox et al. 2018).
Considering the potential risks involved with CAM use, it is important to better characterize users and their motivations for using CAM and declining CCT. Prior studies note motivations such as pain relief, psychological well-being, and controlling the side-effects of disease or treatment (Mansky and Wallerstedt 2006; Clarke et al. 2015; Barnes et al. 2002). However, these studies have relied on surveys that may not fully capture the patient perspective. With the advent of social media and technology, individuals are now free to detail their own narratives to easily disseminate information to large audiences. These online cancer campaigns thus represent a unique avenue through which we can better understand the unfiltered patient perspective. Better understanding of CAM usage and refusal of CCT is crucial for providers to effectively counsel oncologic patients on their treatment options.
To better characterize CAM users, we examined crowdfunding campaigns for cancer treatment from GoFundMe, the largest medical crowdfunding platform. Our objective was to compare CAM users and non-CAM users to understand patients’ reasons behind CAM use and clarify their attitudes and beliefs towards CCT. We hypothesized that CAM users require substantial monetary support for their therapy and that many seek to use CAM to improve their comfort and quality of life.
Methods
Data source and selection of study cohort
Our methodology has been described previously (Cohen et al. 2019), but in brief: we identified the top 20 most prevalent cancers in the U.S. (National Cancer Institute at https://www.cancer.gov/). Each cancer and U.S. State were then queried on GoFundme.com for 1000 individual searches (50 states × 20 top cancers = 1000 batches of searches). We used web scraping and custom Python code to abstract and assemble website data for analysis to gather 37,344 total cancer campaigns. To select our study cohort, we then did a literature search and compiled a list of the top most utilized CAM methods to inform our search terms (Clarke et al. 2015). We wrote a Python code to extract out campaigns that mentioned any of the following search terms: “holistic” (n = 458), “yoga” (n = 196), “chiropract” (n = 159), “acupuncture” (n = 130), “herbal” (n = 126), “meditation” (n = 123), “hyperbaric” (n = 84), “essential oils” (n = 67), “homeopath” (n = 66), “osteopath” (n = 20), “Ayurveda” (n = 10), “energy healing” (n = 8), “tai chi” (n = 7), “fish oil” (n = 6), “botanical” (n = 6), “qigong” (n = 5), and “chakra” (n = 3). A total of 1474 campaigns were identified, and 250 campaigns were randomly selected to serve as our study cohort. Campaigns were excluded if the subject was non-human (i.e., pets with cancer), intended for non-cancer illnesses, did not explicitly mention past or current CAM use, or explicit interest in using CAM treatments in the future.
To better characterize our study cohort, 250 campaigns analyzed in our prior work that did not endorse CAM usage were also randomly selected to serve as our comparison cohort, using the randomizer tool in Stata 15 (College Station, TX).
Variables
From each campaign narrative, patient demographics and clinical characteristics were identified, including: age; primary cancer type; cancer stage (I, II–III, IV, V, or higher); cancer status (metastasis, remission/cure, hospice/end of life, active treatment, recurrence, death); history of misdiagnosis, missed diagnosis, or delayed diagnosis; and insurance status (covered, undercovered, and no insurance). We defined “covered” by any mention of having insurance coverage for medical care, excluding CAM treatments; “undercovered” by any mention of having insurance but struggling with any medical costs not covered by insurance; and “no insurance” by any mention of not having insurance.
We evaluated CAM usage of these subjects by identifying types of CAM used. For ease of descriptive analysis, CAM treatments themselves were grouped if similar. An explanation of treatment groups can be found in Appendix 1. Main reasons for using CAM were also identified and separated into categories. We also examined intent to travel out of state for CAM treatment, the timing of CAM in relation to CCT, any past CCT interventions, future CCT interventions, perceptions of CCT as “toxic”, and ideas on the efficacy of CCT in comparison to CAM. Campaign characteristics were also collected and included goal funds, actual funds raised, and number of social media shares.
Statistical analysis
Descriptive statistics were used to describe both the study cohort and comparison cohort. Patient, clinical, and campaign characteristics were stratified by CAM usage. Chi-square and Fisher’s exact tests were used to compare categorical variables, and Wilcox’s rank sum test was used to compare continuous variables. p values < 0.05 were considered statistically significant. We used the R statistical suite for analysis (https://www.r-project.org/).
Results
Five hundred total GoFundMe cancer campaigns were analyzed, with 250 campaigns that endorsed CAM use and 250 campaigns that did not endorse CAM use. There were more female subjects among the CAM users than non-CAM users (70% vs. 54% respectively, p < 0.01) (Table 1). Breast cancer was the most common cancer type among both groups, although more prominent among CAM users than non-CAM users (31% vs. 21% respectively, p < 0.01). CAM users compared to non-CAM users also tended to have a higher cancer stage (stage IV or higher 54% vs. 12%, p < 0.01), a history of misdiagnosis, or delayed diagnosis (10% vs 4%, p < 0.01), and more likely to have insurance coverage (30% vs. 12%, p < 0.01). While there was no significant difference in past CCT between CAM and non-CAM users, there was a statistically significant difference in future surgery treatment between CAM and non-CAM users (2% vs. 7%, p = 0.04). CAM users also tended to have higher fundraising goals compared to non-CAM users (median $15,000, IQR: $10,000–35,000 vs. $10,000, IQR: $5000–20,000, respectively, p < 0.001). CAM users also tended to raise more funds than non-CAM users (median $2870 IQR: $1160–7950 vs. $2145 IQR: $912–5847 respectively, p = 0.02). CAM users also had a greater number of online shares (median $247, IQR: $97–494 vs. $179, IQR: $70–436 respectively, p = 0.04).
Table 1.
Comparison of CAM users and non-CAM users
| Characteristic, n (%) | CAM users, n = 250 n (%) | Non-CAM users, n = 250 n (%) | p value |
|---|---|---|---|
| Gender | |||
| Female | 176 (70) | 135 (54) | < 0.001 |
| Male | 73 (30) | 115 (46) | |
| Cancer type | 0.007 | ||
| Breast | 77 (31) | 53 (21) | |
| Colon | 25 (10) | 13 (5) | |
| Lung | 19 (8) | 30 (12) | |
| Leukemia | 10 (4) | 32 (13) | |
| Brain | 9 (4) | 9 (4) | |
| Liver | 8 (3) | 10 (4) | |
| Pancreatic | 8 (3) | 8 (3) | |
| Stomach | 7 (3) | 8 (3) | |
| Ovarian | 7 (3) | 6 (2) | |
| Other* | 80 (32) | 81 (32) | |
| Cancer stage | |||
| I | 2 (1) | 6 (2) | < 0.001 |
| II or III | 34 (14) | 75 (30) | |
| IV or higher | 135 (54) | 30 (12) | |
| History of misdiagnosis or delayed diagnosis? | < 0.001 | ||
| Yes | 26 (10) | 9 (4) | |
| No | 47 (19) | 83 (33) | |
| Insurance status | < 0.001 | ||
| Covered | 75 (30) | 30 (12) | |
| Undercovered | 45 (18) | 50 (20) | |
| No insurance | 18 (7) | 22 (9) | |
| Past treatment | |||
| Chemotherapy only | 38 (15) | 57 (23) | 0.070 |
| Surgery only | 30 (12) | 31 (12) | 0.100 |
| Radiation + chemotherapy | 20 (8) | 12 (5) | 0.100 |
| Radiation + surgery | 9 (4) | 7(3) | 0.600 |
| Chemotherapy + surgery | 20 (8) | 26 (10) | 0.600 |
| Radiation + chemotherapy + surgery | 18 (7) | 16 (6) | 0.600 |
| Future treatment | |||
| Radiation only | 7 (3) | 6 (2) | 0.400 |
| Chemotherapy only | 19 (8) | 32 (13) | 0.400 |
| Surgery only | 5 (2) | 18 (7) | 0.040 |
| Experimental only | 8 (3) | 4 (2) | 0.100 |
| Radiation + chemotherapy | 7 (3) | 10 (4) | 0.800 |
| Goal funds | |||
| Median, IQR | 15,000 (10,000–35,000) | 10,000 (5000–20,000) | < 0.001 |
| Funds raised | |||
| Median, IQR | 2870 (1160–7950) | 2145 (912–5848) | 0.020 |
| Number of shares | |||
| Median, IQR | 247 (97–494) | 179 (70–436) | 0.040 |
*Other cancers include: bladder, cervical, kidney, non-Hodgkin lymphoma, prostate, skin (non-melanoma), melanoma, rectal, thyroid, uterine, Hodgkin lymphoma, soft tissue/muscle, and rare/non-specified cancers
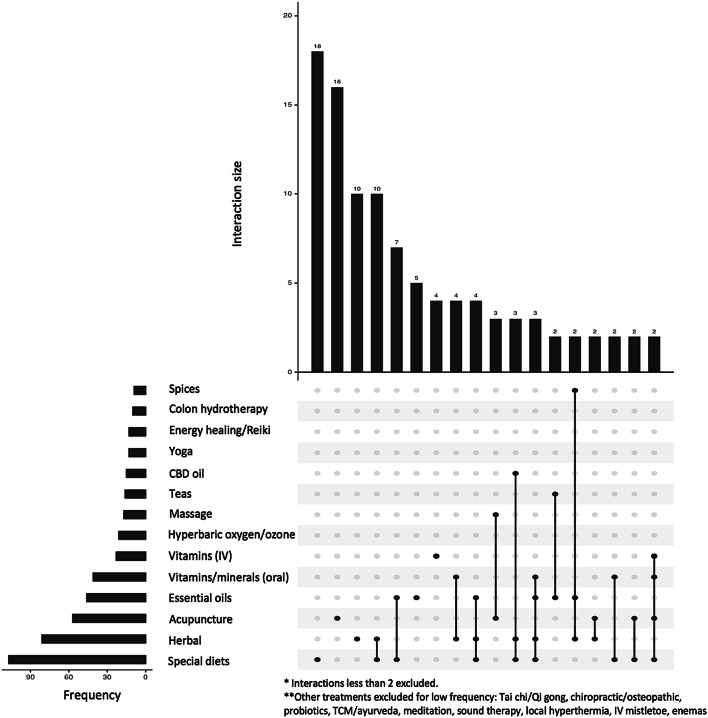
Figure 1 shows a visualization of the most frequently cited CAM treatments and their intersections (Conway et al. 2017). The top 14 most used treatments were: special diets 107( 43%), herbal 81 (33%), acupuncture 57 (23%), essential oils 46 (18%), oral vitamins and minerals 41 (16%), IV vitamins 23 (9%), hyperbaric oxygen/ozone treatments 21 (8%), massage 17 (7%), teas 16 (6%), cannabidiol oil 16 (6%), yoga 13 (5%), energy healing/Reiki 13 (5%), colon hydrotherapy 12 (5%), and spices 9 (4%). 81% of the cohort reported either already using or intending to use two or more CAM methods, while 16% reported using five or more CAM methods. Subjects either utilized CAM treatments under self-direction, under the supervision of outpatient naturopathic/holistic medicine providers, or under inpatient treatment programs at a holistic medicine center. 87 (35%) of these campaigns expressed interest or intent on traveling out of state for CAM treatment to a specific center.
Fig. 1.
Types of CAM treatments used. This figure shows a graphic representation of the different CAM treatments endorsed by subjects in the study, by frequency and interactions (Helyer et al. 2006)
Curative or therapeutic effects were cited as the top reason subjects used CAM with 212 (85%) campaigns, followed by 137 (55%) campaigns endorsing pain and stress reduction (Table 2). 105 (42%) reported using CAM due to dissatisfaction with current or past medical treatment options: 45 (18%) mentioned having no/limited viable medical options left due to the advanced nature of their cancer, 10 (4%) did not want to go through the negative side-effects of chemo or radiation, and 7 (3%) had already experienced the negative side-effects of CCT and were unwilling to tolerate any more. 63 (25%) reported using CAM for spiritual/emotional well-being and 28 (11%) reported religious beliefs as a main reason for utilizing CAM. 11 (4%) reported that financial barriers in accessing CCT were a reason for using CAM instead for cancer treatment. Only four (2%) said that CAM usage was a part of traditional cultural practices. Three (1%) mentioned a fear that CCT alone would not be enough/would not work.
Table 2.
Summary of key patient narratives
| Reason(s) for using CAM | |
| Curative or therapeutic effects | 212 (85) |
| Pain or symptom relief, stress reduction | 137 (55) |
| Dissatisfaction with current or past medical treatment options | 105 (42) |
| Spiritual/emotional well-being | 63 (25) |
| Very limited/no viable medical options left | 45 (18) |
| Religious beliefs | 28 (11) |
| Does not want to go through the negative side-effects of chemo/radiation, but still wants some treatment | 10 (4) |
| Financial reasons | 11 (4) |
| Already experienced negative side-effects of chemotherapy/radiation, cannot tolerate it anymore | 7 (2) |
| Cultural beliefs | 4 (2) |
| Fear that conventional cancer therapy alone will not be enough/won’t work | 3 (1) |
| Other/unknown | 13 (5) |
| Belief that CAM is more effective than CCT | |
| Yes | 85 (34) |
| No | 100 (40) |
| Unknown | 65 (26) |
| Intent to travel out of state for CAM treatment | |
| Yes | 87 (35) |
| No | 78 (32) |
| Unknown | 82 (33) |
| Has the patient tried CCT yet? | |
| Yes | 156 (62) |
| No | 87 (35) |
| Unknown | 7 (3) |
| Reasons for declining CCT | |
| Want to try to fight off cancer using CAM first | 57 (66) |
| Too “toxic” or “poisonous” to the body | 39 (45) |
| Cancer is too advanced already; treatment either futile or too aggressive | 25 (29) |
| Will plan on undergoing conventional cancer treatment eventually | 17 (20) |
| Financial barriers/obstacles | 9 (10) |
| Negative personal experiences previously, either with self or another loved one, in regards to using chemo/radiation | 7(8) |
| Mistrust in the medical system | 5 (6) |
| Just want to enjoy the remaining years with high QOL | 4 (5) |
In examining CAM usage in relation to CCT, 78 (31%) stated that they used only CAM as their only cancer treatment, while 165 (66%) campaigns endorsed using both CAM and CCT. Of these 165 campaigns, 5 (2%) campaigns stated that they used CAM before starting CCT, 67 (27%) stated that they started utilizing CAM after completion of CCT, and 93 (37%) stated that they use both CAM and CCT concurrently.
We also found that 85 (34%) campaigns endorsed a belief that CAM is more effective than CCT. At the time of the campaign’s publication, 156 (62%) campaigns stated that the subject had tried CCT, while 87 (35%) stated that they had not. Out of these 87 campaigns, top reasons for declining CCT include: 57 (66%) wanted to try to fight off cancer using CAM first, 39 (45%) believed that CCT was too “toxic” or “poisonous” to the body. 25 (29%) campaigns stated that their cancer was already too advanced, and CCT would be futile or too aggressive. 17 (18%) campaigns said that they would undergo CCT eventually, but had not tried CCT by the time of the campaign’s publication. 9 (10%) mentioned financial obstacles that prevented them from undergoing CCT. 7 (8%) stated that negative personal experiences, either having had CCT in the past or seeing another loved one using CCT, played the largest motivation to refuse CCT. Five (6%) stated that they did not trust the medical system or their providers to provide them with quality care.
Discussion
In this study of GoFundMe campaigns for cancer treatment, CAM users were more likely to be female, have more advanced cancer stage, and have a history of delayed, missed, or misdiagnosis. CAM users requested $5000 more in donations than non-CAM users. Nearly a third of the subjects endorsed past or future travel to a specialized CAM center for inpatient treatment, often internationally. Reasons for using CAM fell into four main categories: CCT as “toxic to the body and inferior to “natural” CAM methods; CAM as an adjunct to CCT; CAM as a last-resort option for aggressive cancer/terminal stage without medical options; and CAM as a way to prioritize quality of life in their remaining years over curative efficacy. 34.8% of CAM users declined CCT usage and endorsed CAM as their sole method of cancer treatment. The three main reasons that subjects declined CCT overlap with reasons for CAM usage: the idea that CCT is more harmful to the body than beneficial; their cancer is already too aggressive and not wanting to subject themselves to any harsh or futile treatment; and prioritizing quality of life in their remaining years.
The most compelling finding in our study is that autonomy, comfort, and quality of life are extremely important to patients when considering which cancer treatment to undertake. Considering that the risk of morbidity associated with CAM use is mediated by patients’ refusal of CCT (Anderson and Taylor 2012), it is crucial to understand why certain cancer patients are refusing CCT in lieu of CAM treatment. We found that while some subjects chose CAM and declined CCT due to a subjective judgment of “natural” treatments being superior, a larger proportion of the patient narratives demonstrate a clear understanding of the risks and benefits of declining CCT. This is consistent with the previous studies examining patient motivations behind CAM usage, particularly in the setting of oncologic disease in alleviating both the symptoms of cancer and side-effects of CCT (Mansky and Wallerstedt 2006). In one study examining patients with locally-advanced breast cancer, CAM use in patients was associated with decreased anxiety and depression, a greater sense of control over their lives, and allowed patients to feel more hopeful regarding their chances of survival (Helyer et al. 2006). These are important aspects of CAM use that are likely drivers behind CAM usage.
Patients’ motivations for using CAM and declining CCT can inform future recommendations for providers. Currently, as many as 70% of patients may not disclose CAM usage to physicians, possibly out of fear of being misunderstood (Eisenberg et al. 1998; Boon et al. 2000). Understanding patients’ preferences to use CAM may improve the patient–doctor relationship and create a more therapeutic alliance. This can improve patient satisfaction as physicians take into consideration a patient’s preference for CAM (Mazurenko et al. 2017). Considering the growth of CAM usage and awareness over the past decade, with methods such as acupuncture or chiropractic medicine now covered by many insurance plans, providers should better understand these heavily utilized practices and utilize decision-making frameworks that can address each patient’s unique needs and beliefs (Weeks et al. 2014). Physicians should approach treatment counseling by focusing on the patient’s preference for autonomy, comfort, and quality of life (Verhoef et al. 2005).
It is also paramount to educate patients on realistic expectations with CAM use. The ethics of marketing CAM therapy, often with promises of miracle cure-all effects, is a serious issue that deserves particular attention, especially as CAM use in the US continues to grow (Clarke et al. 2015; Barnes et al. 2007). Roughly $34 billion is spent annually on CAM (Herman et al. 2005) with two-thirds spent on self-directed therapy ($22 billion) and one-third on practitioner visits ($11.9 billion) (Nahin et al. 2007). This may provide economic incentive to target and even exploit cancer patients who have exhausted all other medical options. Nearly a third of CAM users in our study reported either traveling or intending to travel to a holistic center for CAM treatment, often times internationally. Considering that many CAM services are not covered by insurance policies and force patients to pay out-of-pocket upwards of tens of thousands of dollars (Eisenberg et al. 1998), it is no surprise our study found that CAM users had a higher goal funds amounts than non-CAM users. Beyond the risk of economic exploitation, there is also the concern of safety: estimated 15 million adults are at risk for potential adverse interactions involving prescription medications and herbs or high-dose vitamin supplements (Eisenberg et al. 1998). The current lack of CAM regulatory oversight may contribute to a less safe, less-efficient, and less cost-effective system (Ventola 2010). Until there is adequate regulation in place to protect patients from dishonest advertising, physicians should educate themselves on common CAM therapies to provide comprehensive counseling to patients who wish to use CAM.
The demographics of our patient population is consistent with prior literature that found CAM users more likely to be female and insured (Eisenberg et al. 1998; Subramani and Lakshmanaswamy 2017). In general, women are more likely to use CAM therapies than men (Barnes et al. 2002), with nearly 40% of women in the US reporting any recent CAM use (Upchurch et al. 2007). As breast cancer is the most frequently diagnosed cancer in women (Siegel et al. 2019), it is no surprise that 31% of CAM users in our study report breast cancer. Prior studies have found that CAM usage increases after cancer diagnosis, with breast cancer survivors the most common among cancer survivors (Saquib et al. 2011). Women represent a potentially important group to study when understanding CAM usage and trends, since women are often the managers of health care in the household (Upchurch et al. 2007) and children are also more likely to use CAM if one parent already uses CAM (Barnes et al. 2007). Our study also found that CAM users were more likely to have higher stages of cancer, which is consistent with a recent study of CAM usage (Johnson et al. 2018a). However, our study also discovered that CAM users are more likely to have a history of delayed, missed, or misdiagnosis, which is consistent with a prior study demonstrating an association between CAM use and delays in presentation and diagnosis among breast cancer patients (Mujar et al. 2017). Whether this association is due to poor access to health care leading to increasing CAM usage, or CAM use that leads to delayed presentation and diagnosis, however, is uncertain, and more studies are needed.
Our study has several limitations. The study is observational and relies on personal narratives, which may not be entirely accurate and cannot be independently verified. Fraud has been shown to exist on gofundme.com (Victor 2019), but we cannot estimate rates of fraudulent data herein. Given that the narratives are also up to subjective interpretation, our analysis of the data may also be biased. Second, our study’s sample size is limited and selecting patients manually, albeit at random, may also be prone to sample bias and thus not generalizable to other populations. Finally, we were unable to extrapolate key patient demographic data regarding race/ethnicity, education status, and income level from the campaign narratives. This information is important to establish a clearer picture of the typical CAM user, as well as identify any socio-economic factors associated with usage.
Conclusions
Our study found that CAM users are more higher cancer stage, have history of delayed, missed, or misdiagnosis, and request higher goal funds than non-CAM users.
Reasons for declining CCT include wanting to try CAM first, cancer already too aggressive or advanced, not wanting to go through side-effects of chemotherapy or radiation, and prioritizing quality of life in the remaining years. It is critical to understand the patient perspective of using CAM and/or declining CCT to provide holistic care and formulate a therapeutic patient-provider alliance, especially given the increased potential of exploitation and harm in this vulnerable patient population. Physicians should further educate themselves on CAM to set realistic expectations and provide comprehensive counseling of the risks and benefits of CAM usage to cancer patients.
Appendix 1
See Table 3.
Table 3.
Definitions of selected CAM treatments
| Term | Definition |
|---|---|
| Special diets | Specific dietary restrictions or modifications for the expressed purpose of curative or therapeutic effects, such as juicing or all-organic vegan diet |
| Herbal | Plant-based remedies derived from the leaves, flowers, or stems of plants in any form (powder, pill, serum, etc.) for medicinal purposes |
| Acupuncture | A system of Chinese integrative medicine that involves pricking the skin or tissues with needles, used to alleviate pain, and treat various physical, mental, and emotional conditions |
| Essential oils | A natural oil obtained by distillation and having the characteristic fragrance of the plant or other source from which it is extracted |
| Vitamins/minerals (oral) | Vitamins and mineral substances taken without an expressed medical indication, such as deficiency, but for overall health benefits |
| Vitamins (IV) | Direct infusion of vitamins, most typically high dose of Vitamin C, through IV to allegedly allow the nutrients to bypass the digestive system for quicker effect |
| Hyperbaric oxygen/medical ozone | Hyperbaric oxygen involves breathing pure oxygen in a pressurized room or tube. Ozone therapy involves the introduction of ozone into the body via injection |
| Energy healing/Reiki | Energy healing is a method of healing based on the belief that vital energy flows through the human body and is channeled through the practitioner to the client to help remove energy deficiencies of blockages. Reiki is a Japanese healing technique where the therapist can channel energy into the patient by means of touch to activate the natural healing processes of the body and restore physical and emotional well-being |
| Colon hydrotherapy | Irrigating the colon with water, sometimes mixed with herbs or other liquids, via the rectum using special equipment with the intention of removing non-specific toxins from the colon and intestinal tract |
| Spices | Seed, fruit, bark, or other plant substance primarily used for flavoring, coloring, or preserving food that are also used for medicinal purposes. Examples include turmeric, frankincense, and rosemary |
Compliance with ethical standards
Conflict of interest
The authors have no conflicts of interests to disclose.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Anderson JG, Taylor AG (2012) Use of complementary therapies for cancer symptom management: results of the 2007 National Health Interview Survey. J Altern Complement Med. 10.1089/acm.2011.0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnes PM, Powell-Griner E, McFann K, Nahin RL (2004) Complementary and alternative medicine use among adults: United States, 2002. Adv Data 343:1–19 [PubMed] [Google Scholar]
- Barnes PM, Bloom B, Nahin RL (2007) Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Rep 12. https://www.cdc.gov/nchs/data/nhsr/nhsr012.pdf [PubMed]
- Boon BH, Stewart M, Kennard MA et al (2000) Use of complementary/alternative medicine by breast cancer survivors in Ontario: prevalence and perceptions. Prog Mol Biol Transl Sci 18(13):2515–2521 [DOI] [PubMed] [Google Scholar]
- Clarke TC, Black LI, Stussman BJ, Barnes PM, Nahin RL (2015) Trends in the use of complementary health approaches among adults: United States, 2002–2012. Natl Health Stat Rep 79:1–16 [PMC free article] [PubMed] [Google Scholar]
- Cohen AJ, Brody H, Patino G et al (2019) Use of an online crowdfunding platform for unmet financial obligations in cancer care. JAMA Intern Med. 10.1001/jamainternmed.2019.3330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway JR, Lex A, Gehlenborg N (2017) UpSetR: an R package for the visualization of intersecting sets and their properties. Bioinformatics. 10.1093/bioinformatics/btx364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenberg DM, Davis RB, Ettner SL et al (1998) Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. J Am Med Assoc. 10.1001/jama.280.18.1569 [DOI] [PubMed] [Google Scholar]
- Helyer LK, Chin S, Chui BK et al (2006) The use of complementary and alternative medicines among patients with locally advanced breast cancer—a descriptive study. BMC Cancer 6:1–8. 10.1186/1471-2407-6-39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herman PM, Craig BM, Caspi O (2005) Is complementary and alternative medicine (CAM) cost-effective? A systematic review. BMC Med Inform Decis Mak 11:1–11. 10.1186/1472-Received [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SB, Park HS, Gross CP, Yu JB (2018a) Complementary medicine, refusal of conventional cancer therapy, and survival among patients with curable cancers. JAMA Oncol 4(10):1375–1381. 10.1001/jamaoncol.2018.2487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson SB, Park HS, Gross CP, Yu JB (2018b) Use of alternative medicine for cancer and its impact on survival. J Natl Cancer Inst 110(1):121–124. 10.1093/jnci/djx145 [DOI] [PubMed] [Google Scholar]
- Mansky PJ, Wallerstedt DB (2006) Complementary medicine in palliative care and cancer symptom management. Cancer J 12(5):425–431. 10.1097/00130404-200609000-00011 [DOI] [PubMed] [Google Scholar]
- Mariotto AB, Yabroff KR, Shao Y, Feuer EJ, Brown ML (2010) Projections of the cost of cancer care in the United States : 2010–2020. J Natl Cancer Inst 103:117–128. 10.1093/jnci/djq495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazurenko O, Collum T, Ferdinand A, Menachemi N (2017) Predictors of hospital patient satisfaction as measured by HCAHPS: a systematic review. J Healthc Manag. 10.1097/JHM-D-15-00050 [DOI] [PubMed] [Google Scholar]
- Mujar NMM, Dahlui M, Emran NA et al (2017) Complementary and alternative medicine (CAM) use and delays in presentation and diagnosis of breast cancer patients in public hospitals in Malaysia. PLoS ONE 12(4):1–12. 10.1371/journal.pone.0176394 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nahin RL, Institutes N, Barnes PM (2009) Costs of complementary and alternative medicine (CAM) and frequency of visits to CAM practitioners: United States, 2007. 18 [PubMed]
- Richardson MA, Sanders T, Palmer JL, Greisinger A, Singletary SE (2000) Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol 18(13):2505–2514. 10.1200/jco.2000.18.13.2505 [DOI] [PubMed] [Google Scholar]
- Saquib J, Madlensky L, Kealey S et al (2011) Classification of CAM use and its correlates in patients with early-stage breast cancer. Integr Cancer Ther 10(2):138–147. 10.1177/1534735410392578 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69(1):7–34. 10.3322/caac.21551 [DOI] [PubMed] [Google Scholar]
- Snyder J, Caulfield T (2019) Patients’ crowdfunding campaigns for alternative cancer treatments. Lancet Oncol 20(1):28–29. 10.1016/s1470-2045(18)30950-1 [DOI] [PubMed] [Google Scholar]
- Subramani R, Lakshmanaswamy R (2017) Complementary and alternative medicine and breast cancer, 151st edn. Elsevier Inc., Amsterdam 10.1016/bs.pmbts.2017.07.008 [Google Scholar]
- Upchurch DM, Chyu L, Greendale GA et al (2007) Complementary and alternative medicine use among american women: findings from the National Health Interview Survey, 2002. J Women’s Health 16(1):102–113. 10.1089/jwh.2006.m074 [DOI] [PubMed] [Google Scholar]
- Ventola CL (2010) Current issues regarding complementary and alternative medicine (CAM) in the United States: part 2: regulatory and safety concerns and proposed governmental policy changes with respect to dietary supplements. Pharm Ther 35(9):514–522. https://www.ncbi.nlm.nih.gov/pubmed/20975811. https://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC2957745 [PMC free article] [PubMed]
- Verhoef MJ, Balneaves LG, Boon HS, Vroegindewey A (2005) Reasons for and characteristics associated with complementary and alternative medicine use among adult cancer patients: a systematic review. Integr Cancer Ther 4(4):274–286. 10.1177/1534735405282361 [DOI] [PubMed] [Google Scholar]
- Victor D (2019) Two plead guilty in $400,000 GoFundMe fraud. New York Times 25
- Vox F, Folkers KMB, Turi A, Caplan AL (2018) Medical crowdfunding for scientifically unsupported or potentially dangerous treatments. JAMA. 10.1001/jama.2018.10264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weeks L, Balneaves LG, Paterson C, Verhoef M (2014) Decision-making about complementary and alternative medicine by cancer patients: integrative literature review. Open Med 8(2):e54 [PMC free article] [PubMed] [Google Scholar]