Abstract
Objective
This study aimed to evaluate the therapeutic effects of minimally invasive lateral, posterior, and posterolateral sacroiliac joint fusion for low back pain through a meta-analysis.
Methods
The PubMed, Web of Science, Embase, Cochrane Library, and ClinicalTrials.gov databases were comprehensively searched for studies up to 31 August 2024. Relevant studies using lateral, posterior, and posterolateral approaches were identified. Pooled outcomes and publication bias were assessed. The study was registered with PROSPERO (registration No. CRD42023451047)
Results
A total of 48 studies were included: 32 focused on the lateral approach, 10 on the posterior approach, four on the posterolateral approach, and two compared the lateral and posterolateral approaches. The pooled effect analysis showed statistically significant improvements in the visual analog scale (VAS) scores for all three approaches at 6 and 12 months postoperatively. Although no between-approach comparisons were conducted, the pooled improvements in VAS scores at 6 and 12 months postoperatively were numerically similar across all three approaches, as were the pooled fusion rates. The pooled complication rate for the lateral approach was 9.2%, numerically higher than 1% for the posterior approach. The pooled revision rate for the lateral approach was 2.4%, also numerically higher than 0.6% for the posterior approach.
Conclusions
Although pain relief and fusion rates were similar across all approaches, the lateral approach might be associated with a higher risk of total complications and revision surgery.
Keywords: Minimally invasive sacroiliac joint fusion, surgical approach, pain relief, total complication rate, revision rate
Introduction
Low back pain is very common in today’s society and often seriously affects patients’ quality of life. Some causes of low back pain are related to sacroiliac joint diseases, which need to be confirmed by physical examinations, such as a pelvic compression separation test and Patrick’s test. 1 Sacroiliac joint diseases may be treated conservatively and/or surgically. Conservative treatment includes medication, physiotherapy, acupuncture, and local blocking. If conservative treatment is ineffective, sacroiliac joint fusion may be considered.2–4 Minimally invasive sacroiliac joint fusion has the advantages of less blood loss and a shorter operation time than open fusion, 5 and includes three surgical approaches: lateral, posterior and posterolateral. There are currently few comparative studies of the three surgical approaches in minimally invasive sacroiliac joint fusion, and most meta-analyses have not provided separate analyses for each. The purpose of the present study was to conduct a systematic review and meta-analysis evaluating the therapeutic effects of minimally invasive lateral, posterior, and posterolateral sacroiliac joint fusion on low back pain of sacroiliac joint origin.
Materials and methods
This study followed the Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) 2020 guidelines, 6 and was registered on PROSPERO under registration No. CRD42023451047.
Search strategy
The PubMed, Web of Science, Embase, Cochrane Library, and ClinicalTrials.gov databases were searched for articles related to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin, published up to 31 August 2024. The Medical Subject Heading (MeSH) search terms included sacroiliac joint/surgery and minimally invasive surgical procedures. These keywords and their corresponding free words, together with Boolean operators, were used to create search formulas. The detailed search strategy is provided in Supplemental materials. After removal of duplicates, titles and abstracts were independently screened by two independent reviewers (KX and YLL), with any disagreements resolved by a third reviewer (SHX), followed by full-text review of remaining articles by two independent reviewers (KX and YLL), according to the inclusion and exclusion criteria. In addition, the references of the screened articles were read as an alternative way to identify articles suitable for this meta-analysis. The final selected articles were classified according to the surgical approaches: lateral, posterior, and posterolateral.
Inclusion and exclusion criteria
The inclusion criteria comprised: (1) studies on low back pain of sacroiliac joint origin; (2) studies on minimally invasive sacroiliac joint fusion for low back pain; (3) studies with a follow-up period of more than 6 months; (4) studies published in English; and (5) quantitative studies.
The exclusion criteria comprised: (1) studies including patients with neoplastic disease; (2) studies including patients with acute traumatic diseases; (3) review articles; (4) animal studies; (5) studies with incomplete data; (6) studies on revisional surgery of the sacroiliac joint; (7) studies including patients with infectious diseases; (8) studies with a sample size less than 10; and/or (9) studies with overlapping data.
Assessment of studies
The methodological quality of included studies was assessed independently by two authors (SHX and YLL). Cohort studies, a type of observational study design for evaluating the association between exposure and outcomes, with participants divided into exposed and non-exposed groups, were evaluated for quality using the Newcastle-Ottawa Scale, with a maximum of 9 points. 7 Each cohort study was assessed based on eight items, which were divided into three categories: selection, comparability and outcome. All cohort studies mentioned in the present manuscript were comparative studies, not single-arm studies. The Cochrane Collaboration’s tool was used to assess the quality of randomized controlled trials (RCTs), 8 focusing on seven key evaluation criteria, including random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, completeness of outcome data, selective reporting, and identification of potential sources of bias. For case series and prospective multicenter single-arm studies, quality evaluation was conducted using the Joanna Briggs Institute critical appraisal tool, 9 which comprises 10 questions assessing the internal validity and risk of bias. A case series was defined as a descriptive study design that focuses on the characteristics, clinical presentations, treatment responses, and outcomes of patients, without including a control group.
Data extraction
The following data were extracted from the included articles: (1) demographic parameters, including study type, approach, sample size (minimally invasive sacroiliac joint fusion, MISIJF), sex, age, internal implant name, comparison group, follow-up time and prior lumbar fusion proportion; (2) visual analog scale (VAS) score for low back pain preoperatively, and at 6 and 12 months postoperatively; and (3) the total complication rate, revision rate, and fusion rate during the follow-up period. The total complication rate included any intraoperative and postoperative complication. Fusion was defined as bone bridging within the sacroiliac joint and absence of screw loosening on the radiographic image. For both RCTs and cohort studies, only participants who received minimally invasive sacroiliac joint fusion were analyzed. All the parameters were confirmed by two authors (KX and YLL), and in case of disagreement, the two authors negotiated to reach a consensus.
Outcomes
Improvement of VAS score was defined as the mean difference in low back pain scores before and after surgery. The VAS score improvements were calculated at 6 and 12 months postoperatively and pooled estimates for different surgical approaches are presented. Additionally, the pooled total complication rate, pooled revision rate, and pooled fusion rate were calculated and reported for the various surgical techniques.
Certainty of evidence
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to evaluate the certainty of evidence for the meta-analysis. Using the GRADE approach, the study design was first considered, followed by examination of various factors for potentially downgrading or upgrading the quality of a body of evidence, which was finally classified into one of four levels: very low, low, moderate or high. 10 GRADE was used to assess the quality of evidence for each pooled effect estimate.
Statistical analyses
Meta-analysis, sensitivity analysis and publication bias testing (Egger’s test) were performed using Stata 14 (2015) statistical software (StataCorp LLC, College Station, TX, USA). If the number of studies included in the meta-analysis exceeded 10, a publication bias assessment was conducted. Data are presented as mean and SD, with results of individual studies and syntheses displayed utilizing forest plots. When calculating the pooled parameter, P (Q test) <0.1 or I2 > 50% was considered to indicate heterogeneity. A leave-one-out sensitivity analysis was conducted to identify potential sources of heterogeneity. Specifically, one study was removed at a time and the meta-analysis was re-run to assess the impact of each study on the overall results. After exploring potential factors contributing to the heterogeneity in the identified study, the study may be excluded. However, caution should be exercised when excluding studies in meta-analyses with a small number of included studies. If no heterogeneity was present, a fixed-effect model was used to combine effect sizes; if heterogeneity existed, a random-effect model was applied.
Results
Search results
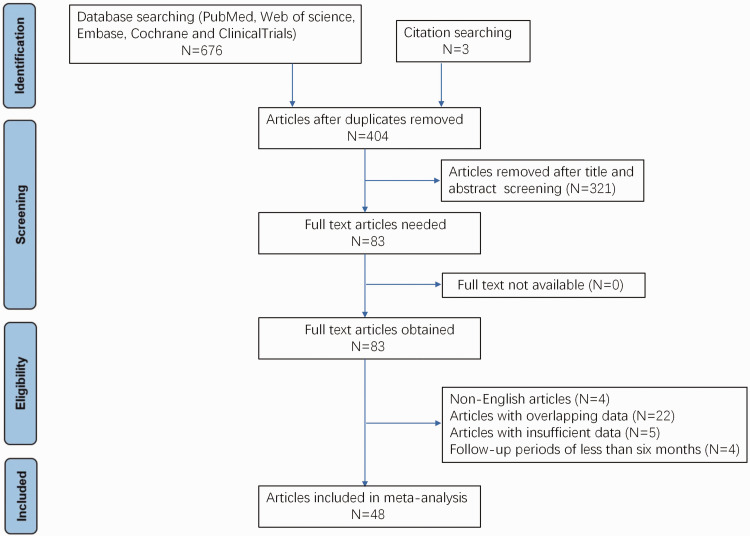
A total of 679 articles were identified using the search strategy. After screening and assessing eligible articles, 48 articles were ultimately included in the meta-analysis.4,5,11–56 The selection process is detailed in Figure 1.
Figure 1.
PRISMA flowchart of articles investigating different approaches to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin included in the meta-analysis.
Characteristics of included studies
A total of 32 studies investigated the lateral approach, 10 investigated the posterior approach, four investigated the posterolateral approach, and two compared the lateral and posterolateral approaches (the studies by Claus et al. 11 and Cahueque et al. 12 ). The included literature contained three RCTs,20,25,27 all of which focused on the lateral approach. In two of the RCTs,20,25 the control group received conservative treatment, and in the RCT by Randers et al., 27 the control group underwent sham surgery. The remaining study types included six cohort studies,4,5,11,12,31,33 a total of 33 case series,13–19,22,23,26,28–30,32,34–37,39,41,42,44,45,47–56 and six prospective multicenter single-arm studies.21,24,38,40,43,46 All included studies are summarized in Table 1.
Table 1.
Characteristics of the 48 articles investigating different approaches to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin included in the meta-analysis.
| First author | Year | Study type | Internal implant name | Approach | Age, years | Sample size, MISIJF | Female, % | Follow-up, months | Comparison group | Prior lumbar fusion, % |
|---|---|---|---|---|---|---|---|---|---|---|
| Khurana 13 | 2009 | Case series | HMA | Lateral | NR | 15 | NR | 17 | NA | NR |
| Mason 14 | 2013 | Case series | HMA | Lateral | 57 | 55 | 83.6 | 36.2 | NA | NR |
| Soliman 15 | 2022 | Case series | iFuse | Lateral | NR | 33 | 73 | 12 | NA | NR |
| Bornemann 16 | 2017 | Case series | iFuse | Lateral | 54.9 | 24 | 91.7 | 24 | NA | NR |
| Bricard 17 | 2024 | Case series | iFuse | Lateral | 59 | 54 | 75.9 | 24 | NA | 100 |
| Claus 11 | 2020 | Cohort study | iFuse | Lateral | 55.7 | 82 | 73.2 | 12 | Rialto | 61.0 |
| Cleveland 18 | 2019 | Case series | iFuse | Lateral | 51 | 50 | 76 | 14 | NA | NR |
| Cummings 19 | 2013 | Case series | iFuse | Lateral | 64 | 18 | 67 | 12 | NA | 61.1 |
| Dengler 20 | 2019 | RCT | iFuse | Lateral | 49.4 | 52 | 73.1 | 24 | CM | NR |
| Duhon 21 | 2016 | PMSAS | iFuse | Lateral | 50.9 | 172 | 69.8 | 24 | NA | 44.2 |
| Gaetani 22 | 2013 | Case series | iFuse | Lateral | 53.2 | 10 | 100 | 10 | NA | NR |
| Hermans 23 | 2022 | Case series | iFuse | Lateral | 45.6 | 29 | 86.3 | 12 | NA | 10.3 |
| Ledonio 5 | 2014 | Cohort study | iFuse | Lateral | 47.9 | 22 | 77.3 | 15 | Open surgery | NR |
| Patel 24 | 2021 | PMSAS | iFuse | Lateral | 53 | 51 | 76 | 24 | NA | NR |
| Polly 25 | 2016 | RCT | iFuse | Lateral | 50.2 | 102 | 73.5 | 6 | CM | 39.2 |
| Rainov 26 | 2019 | Case series | iFuse | Lateral | 58 | 160 | 67.5 | 12 | NA | 63.8 |
| Randers 27 | 2024 | RCT | iFuse | Lateral | 45.3 | 32 | 91 | 6 | Sham surgery | NR |
| Rudolf 28 | 2014 | Case series | iFuse | Lateral | 58 | 17 | 77 | 60 | NA | 47.1 |
| Sachs 29 | 2016 | Case series | iFuse | Lateral | 57.5 | 107 | NR | 44.4 | NA | 36.4 |
| Schmidt 30 | 2020 | Case series | iFuse | Lateral | 50 | 19 | 21 | 58 | NA | NR |
| Vanaclocha 4 | 2017 | Cohort study | iFuse | Lateral | 48 | 27 | 70.4 | 41 | CM/denervation | 7.4 |
| Smith 31 | 2013 | Cohort study | iFuse | Lateral | 57.4 | 114 | 71.9 | 24 | Open surgery | 47.4 |
| Kancherla 32 | 2017 | Case series | iFuse/ Samba | Lateral | 52.7 | 45 | 68.9 | 32.6 | NA | NR |
| Cahueque 12 | 2023 | Cohort study | Sacrix | Lateral | 62.9 | 22 | 27 | 12 | Posterolateral | 59 |
| Agarwal 33 | 2024 | Cohort study | SI-LOK | Lateral | 55 | 33 | 78.8 | 12 | iFuse | NR |
| Chaves 34 | 2022 | Case series | SI-LOK | Lateral | 66 | 36 | 61.1 | 13.3 | NA | 38.9 |
| Jedi 35 | 2023 | Case series | SI-LOK | Lateral | 32 | 85 | 56 | 6 | NA | NR |
| Mohit 36 | 2020 | Case series | SI-LOK | Lateral | 68.8 | 44 | 61.7 | 24 | NA | 87.2 |
| Rappoport 37 | 2021 | Case series | SI-LOK | Lateral | 55.2 | 32 | 62.5 | 24 | NA | NR |
| Cross 38 | 2018 | PMSAS | SImmetry | Lateral | 60.1 | 19 | 79 | 24 | NA | NR |
| Kube 39 | 2016 | Case series | SImmetry | Lateral | 47.2 | 18 | 56 | 12 | NA | 22.2 |
| Kucharzyk 40 | 2022 | PMSAS | SImmetry | Lateral | 60.5 | 250 | 70.8 | 12 | NA | 36.8 |
| Kasapovic 41 | 2022 | Case series | Torpedo | Lateral | 59 | 15 | 66.7 | 6 | NA | NR |
| Abbasi 42 | 2021 | Case series | Zyga/Corelink/LnK | Lateral | 54 | 62 | NR | 12 | NA | NR |
| Davies 43 | 2024 | PMSAS | Catamaran | Posterior | 58.9 | 33 | 76 | 12 | NA | 18 |
| Endres 44 | 2013 | Case series | DIANA | Posterior | 60.9 | 19 | 73.7 | 13.2 | NA | 100 |
| Fuchs 45 | 2018 | Case series | DIANA | Posterior | NR | 171 | 67 | 24 | NA | NR |
| Calodney 46 | 2024 | PMSAS | LinQ | Posterior | 59 | 117 | 70.1 | 12 | NA | NR |
| Moghim 47 | 2024 | Case series | LinQ | Posterior | 65.5 | 43 | 60.4 | 12 | NA | NR |
| Sayed 48 | 2021 | Case series | LinQ | Posterior | 68 | 50 | 52 | 20 | NA | NR |
| Kaye 49 | 2024 | Case series | LinQ/PsiF | Posterior | 53.4 | 53 | 88.7 | 36 | NA | NR |
| Deer 50 | 2021 | Case series | LinQ™ | Posterior | 69.8 | 111 | 54.1 | 9.7 | NA | NR |
| Lynch 51 | 2022 | Case series | PsiF™ | Posterior | 63 | 57 | NR | 6 | NA | NR |
| Wise 52 | 2008 | Case series | Threaded cages | Posterior | 53.1 | 13 | 92.3 | 29.4 | NA | NR |
| Cross 3rd 53 | 2024 | Case series | Integrity-SI | Posterolateral | 58 | 75 | 60 | 14.2 | NA | NR |
| Anton 54 | 2023 | Case series | Rialto | Posterolateral | 58.6 | 118 | 68.6 | 18.8 | NA | 50.8 |
| Claus 11 | 2020 | Cohort study | Rialto | Posterolateral | 58.4 | 74 | 73 | 12 | iFuse | 64.9 |
| Rajpal 55 | 2019 | Case series | Rialto | Posterolateral | 62.2 | 24 | 87.5 | 19 | NA | 62.5 |
| Cahueque 12 | 2023 | Cohort study | Sacrix | Posterolateral | 62.3 | 23 | 48 | 12 | Lateral | 52 |
| Raikar 56 | 2023 | Case series | Sacrix | Posterolateral | 61.5 | 19 | 89.5 | 16.2 | NA | 57.9 |
NR, not reported; NA, not applicable; RCT, randomized controlled trial; MISIJF, minimally invasive sacroiliac joint fusion; PMSAS, prospective multicenter single-arm study; CM, conservative management.
Methodological quality of included studies and GRADE assessment
Bias assessments for the case series and prospective multicenter single-arm studies, cohort studies, and RCTs are provided in Supplemental Tables S1, S2, and S3, respectively. Each pooled effect estimate included case series studies, which are considered very low-quality evidence in GRADE assessment, with no potential for upgrading the quality of evidence of case series studies. Therefore, the quality of all pooled effect estimates was rated as very low. Tables summarizing the findings for the lateral approach, posterior approach, and posterolateral approach are provided in Supplemental Tables S4, S5, and S6, respectively.
Outcomes of the meta-analysis
VAS score improvement at 6 months postoperatively
Nine studies on the lateral approach,11,15,16,21,26,27,36,37,39 three studies on the posterior approach,43,46,47 and three studies on the posterolateral approach,11,53,54 reported preoperative and 6-month postoperative VAS scores for low back pain, with pooled mean differences of 4.3 (95% confidence interval [CI] 3.6, 5.0; I2 = 92.2%, Q test P value <0.001), 4.8 (95% CI 3.6, 6.0; I2 = 86.1%, Q test P value = 0.001), and 3.0 (95% CI 1.6, 4.4; I2 = 89.9%, Q test P value <0.001), respectively (Figure 2). Following the leave-one-out analysis, no studies were excluded. In these studies, significant pain reduction was consistently observed.
Figure 2.
Forest plot of pooled VAS score improvements at 6 months postoperatively for three approaches to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin. VAS, visual analog scale; N, number; CI, confidence interval; Pre-mean, mean preoperative low back pain; Pre-SD, standard deviation of preoperative low back pain; Post-mean, mean postoperative low back pain; Post-SD, standard deviation of postoperative low back pain; MD, mean difference.
VAS score improvement at 12 months postoperatively
Fifteen studies on the lateral approach,11,12,15,16,19,21,23,26,28,31,34,36–39 two on the posterior approach,46,47 and four on the posterolateral approach,11,12,53,54 reported preoperative and 12-month postoperative VAS scores for low back pain, with pooled mean differences of 5.0 (95% CI 4.5, 5.4; I2 = 85.3%, Q test P value <0.001), 4.9 (95% CI 3.6, 6.2; I2 = 82.5%, Q test P value = 0.017), and 3.8 (95% CI 1.9, 5.7; I2 = 96.5%, Q test P value = 0.001), respectively (Supplemental Figure S1). Leave-one-out analysis revealed no source of heterogeneity for all approaches. No publication bias was identified in the lateral approach studies.
Significant postoperative reduction in pain was consistently observed in these studies. Thus, the impact of preoperative pain scores on VAS score improvement at 12 months postoperatively was analyzed. For studies with preoperative VAS scores ≥8, the pooled mean difference in postoperative scores was 5.18 (95% CI 4.72, 5.64), which was numerically higher than that for studies with preoperative VAS scores <8, at 3.94 (95% CI 2.88, 5.00; Supplemental Figure S2).
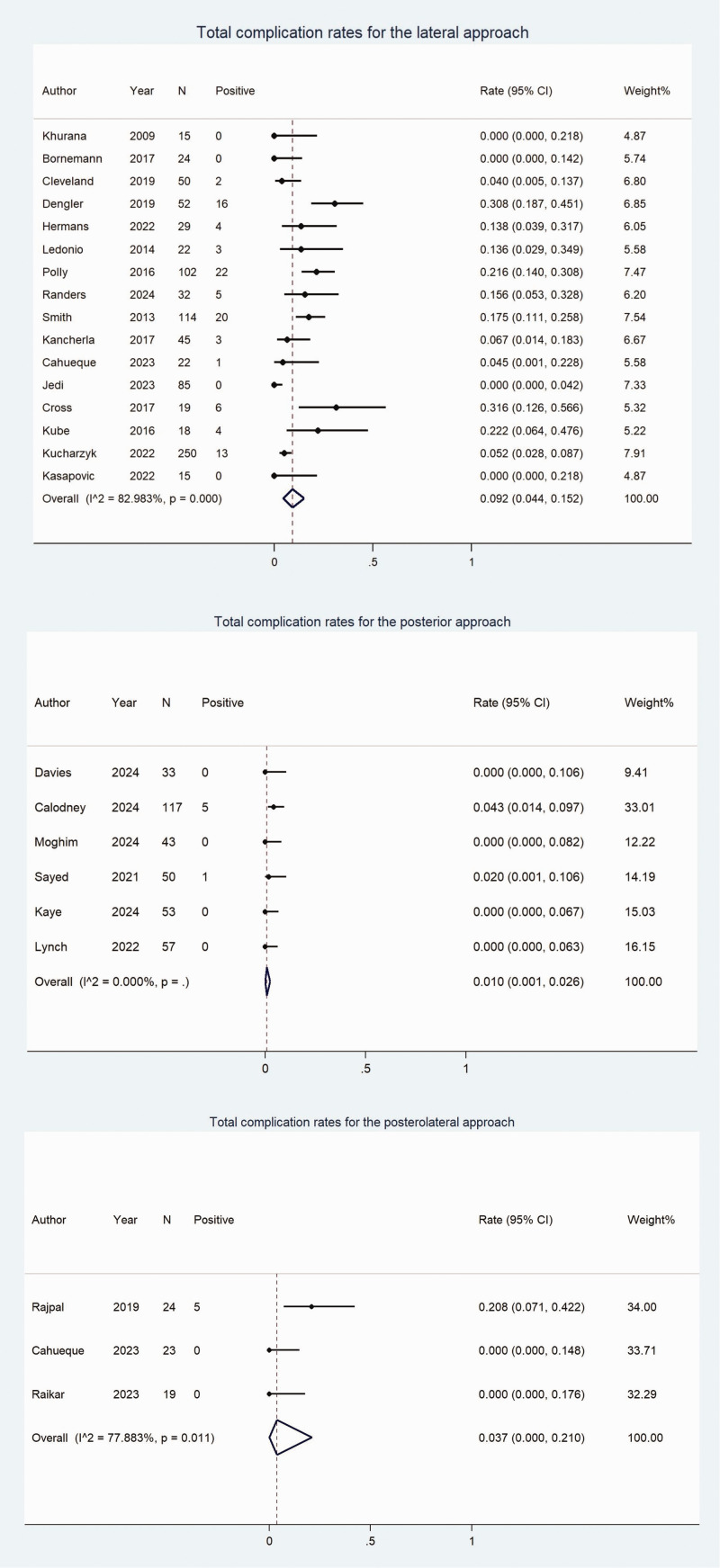
Total complication rate
Sixteen studies on the lateral approach,5,12,13,16,18,,20,23,25,27,31,32, 35,38–41 six on the posterior approach,43,46–49,51 and three on the posterolateral approach,12,55,56 reported total complication rates, with pooled total complication rates of 9.2% (95% CI 4.4%, 15.2%; I2 = 83.0%, Q test P value <0.001), 1% (95% CI 0.1%, 2.6%; I2 = 22.1%, Q test P value = 0.267), and 3.7% (95% CI 0.0%, 21.0%; I2 = 77.9%, Q test P value = 0.011), respectively (Figure 3). Leave-one-out analysis revealed no source of heterogeneity for the lateral and posterolateral approaches. No publication bias was detected in the lateral approach studies.
Figure 3.
Forest plot of pooled total complication rates for three approaches to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin. N, number; CI, confidence interval.
Revision rate
Twenty-eight studies on the lateral approach,4,5,11–14,16–21,23–27,29,31–35, 37,39–42 seven on the posterior approach,43,45–48,51,52 and five on the posterolateral approach,12,53–56 reported revision rates, with pooled revision rates of 2.4% (95% CI 1.3%, 3.9%; I2 = 49.6%, Q test P value = 0.002), 0.6% (95% CI 0.0%, 1.8%; I2 = 42.4%, Q test P value = 0.108), and 0.9% (95% CI 0.0%, 2.9%; I2 = 0.0%, Q test P value = 0.875), respectively (Figure 4). Leave-one-out analysis revealed no source of heterogeneity in the lateral approach. No publication bias was detected in the lateral approach studies.
Figure 4.
Forest plot of pooled revision rates for three approaches to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin. N, number; CI, confidence interval.
Analyses of the impact of different implant types on the revision rate for the lateral approach revealed that the pooled revision rate for iFuse implants was 3.3% (95% CI 2.1%, 4.7%), which was numerically higher than that for non-iFuse implants at 1.1% (95% CI 0.2%, 2.4%; Supplemental Figure S3).
Fusion rate
Seven studies on the lateral approach and four studies on the posterolateral approach reported fusion rates,13,16,26,28,38–40,53–56 with pooled fusion rates of 88.1% (95% CI 76.7%, 96.4%; I2 = 83.0%, Q test P value <0.001) and 95.2% (95% CI 84.7%, 100.0%; I2 = 76.0%, Q test P value = 0.006), respectively. Following the leave-one-out analysis, no studies were excluded. The pooled fusion rate for four studies on the posterior approach was 66.9% (95% CI 29.9%, 95.5%; I2 = 91.5%, Q test P value <0.001).43–45,52 Through leave-one-out analysis, the study by Fuchs et al. 45 was identified as the source of heterogeneity, with a fusion rate of 31%, significantly lower than other studies, possibly due to suboptimal implant positioning and shorter follow-up duration. After excluding this study, heterogeneity decreased, and the pooled fusion rate was recalculated using a fixed-effects model to be 83.1% (95% CI 69.5%, 93.8%; I2 = 0.0%, Q test P value = 0.427; Supplemental Figure S4).
Summary of the three approaches
The outcomes of the three surgical approaches are summarized in Table 2.
Table 2.
Summary of the therapeutic effects of lateral, posterior, and posterolateral minimally invasive sacroiliac joint fusion techniques for low back pain of sacroiliac joint origin.
| Variable | Technique |
||
|---|---|---|---|
| Lateral | Posterior | Posterolateral | |
| VAS score improvement | |||
| 6 months postoperatively | 4.3 (3.6, 5.0) | 4.8 (3.6, 6.0) | 3.0 (1.6, 4.4) |
| 12 months postoperatively | 5.0 (4.5, 5.4) | 4.9 (3.6, 6.2) | 3.8 (1.9, 5.7) |
| Pooled total complication rate, % | 9.2 (4.4, 15.2) | 1 (0.1, 2.6) | 3.7 (0, 21) |
| Pooled revision rate, % | 2.4 (1.3, 3.9) | 0.6 (0, 1.8) | 0.9 (0, 2.9) |
| Pooled fusion rate, % | 88.1 (76.7, 96.4) | 83.1 (69.5, 93.8) | 95.2 (84.7, 100.0) |
Data presented as mean difference (95% CI) or % (95% CI).
VAS score improvement is defined as the mean difference in low back pain scores before and after surgery.
CI, confidence interval; VAS, visual analog scale.
The pooled complication rate for the lateral approach was 9.2% (95% CI 4.4%, 15.2%), numerically higher than 1% (95% CI 0.1%, 2.6%) for the posterior approach. The pooled revision rate for the lateral approach was 2.4% (95% CI 1.3%, 3.9%), also numerically higher than 0.6% (95% CI 0%, 1.8%) for the posterior approach. The remaining indicators were numerically similar.
Discussion
Diagnosing sacroiliac joint-related pain requires imaging studies to exclude other causes of low back pain, such as lumbar spine disorders and peripheral plexopathies. Peripheral plexopathies often affect multiple nerve roots, while lumbar spine disorders typically involve a single nerve root. 57 Currently, there are two ways to achieve sacroiliac joint fusion: minimally invasive surgery and open surgery. According to the literature, minimally invasive sacroiliac joint fusion is generally believed to be superior to open surgery. For example, minimally invasive sacroiliac joint fusion has been associated with less blood loss and a shorter operation time than open fusion, but with similar Oswestry Disability Index. 5 In another study, open sacroiliac joint fusion was associated with greater hospitalization costs than minimally invasive fusion, 58 and minimally invasive sacroiliac joint fusion has been associated with better patient-reported outcomes than open fusion. 59
To the best of our knowledge, there are very few studies comparing different surgical approaches for minimally invasive sacroiliac joint fusion. Claus et al. 11 reported similar pain relief at 6 and 12 months postoperatively between the lateral approach and the posterolateral approach, which is consistent with the present conclusions.
Cahueque et al. 12 reported a case of nerve compression following lateral approach surgery, requiring revision surgery. However, no such cases were observed with the posterolateral approach, which aligns with the present pooled findings of a higher complication and revision rate with the lateral approach.
In the present study, literature on the treatment of low back pain of sacroiliac joint origin with minimally invasive sacroiliac joint fusion was analyzed. Although pain relief and fusion rates were similar across all approaches, the lateral approach might be associated with a higher risk of total complications and revision surgery.
In 2024, a meta-analysis by Ghaddaf et al. 60 concluded that minimally invasive sacroiliac joint fusion using triangular titanium implants is superior to non-surgical treatments in terms of pain relief, functional improvement, and enhanced quality of life. A review by Mehkri et al. 61 suggested that VAS scores significantly decreased during follow-up after minimally invasive sacroiliac joint fusion, with an average reduction of 50.33% at 6 months postoperatively and 61.94% at 12 months postoperatively. The mean fusion rate was 84.92%. These findings are similar to those in the present meta-analysis; however, previous meta-analyses have generally not differentiated between the surgical approaches. Of note, the 2023 study by Whang et al. 62 compared pain relief across three different surgical approaches for sacroiliac joint fusion but did not evaluate pain relief at specific time points, whereas the present review included updated studies and pain improvement was calculated at 6 and 12 months postoperatively.
The studies included in the present investigation displayed a wide range of demographic characteristics, with mean ages spanning between 32 and 69.8 years, and the proportions of female patients ranging from 21% to 100% (see Table 1). These demographic factors may have influenced the differences in therapeutic outcomes among the different surgical approaches.
Low back pain may be caused by various conditions located in the lumbar and pelvic regions. Prior lumbar fusion is a common comorbidity, and has been reported in several studies (see Table 1).4,11,12,17,19,21, 23,25,26,28,29,31,34,36,39,40,43,44,54–56 However, the vast majority of studies did not perform subgroup analyses or provide specific data for such analyses, making it impossible to merge this information. The impact of comorbidities on the treatment outcomes of minimally invasive sacroiliac joint fusion warrants further investigation.
At present, there are many studies on minimally invasive sacroiliac joint fusion via the lateral approach, and iFuse is the main implant type. However, there are limited studies involving the posterior and posterolateral approaches. The current meta-analysis indicated that surgery via the posterior approach might offer the advantage of fewer complications. Therefore, minimally invasive sacroiliac joint fusion via the posterior approach has potential for development and deserves additional research.
The results of the present meta-analysis may be limited by several factors: (1) few studies on the posterior and posterolateral approaches were included; (2) most of the studies included in this meta-analysis were case series, providing very low-quality evidence. There were no RCTs on the posterior and posterolateral approach; (3) the search strategy required the inclusion of the terms ‘minimally’ or ‘minimal’ in the title or abstract to ensure a focused selection of studies. However, this approach may have constrained the comprehensiveness of the search, potentially omitting studies that did not use these specific keywords; and (4) through the bias assessment, some articles were found to have a high risk of bias. However, since sensitivity analysis indicated that these high-bias articles were not a source of significant heterogeneity, and the number of studies on the posterior and posterolateral approaches was relatively small, exclusion was considered inappropriate. Therefore, the present findings should be interpreted with caution. More high-quality studies on minimally invasive sacroiliac joint fusion are required in the future to obtain more convincing results.
Conclusions
Pain relief and fusion rates were similar across all approaches to minimally invasive sacroiliac joint fusion for low back pain of sacroiliac joint origin. However, it is important to note that the lateral approach might be associated with a higher risk of total complications and revision surgery.
Supplemental Material
Supplemental material, sj-pdf-1-imr-10.1177_03000605251315300 for Minimally invasive lateral, posterior, and posterolateral sacroiliac joint fusion for low back pain: a systematic review and meta-analysis by Kai Xu, Ya-Ling Li, Song-Hua Xiao and Yong-Wei Pan in Journal of International Medical Research
Author contributions: KX contributed to design, data collection and writing. YLL contributed to data collection and analysis. SHX contributed to data analysis and critical revision. YWP contributed to concept and critical revision. All authors read and approved the final version of the manuscript.
The Authors declare that there are no conflicts of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Song-Hua Xiao https://orcid.org/0000-0001-6298-9633
Data availability
The datasets are available from the corresponding author upon reasonable request.
Supplemental material
Supplemental tables and figures are provided within the Supplementary materials file, available online.
References
- 1.Capobianco R, Cher D; SIFI Study Group. Safety and effectiveness of minimally invasive sacroiliac joint fusion in women with persistent post-partum posterior pelvic girdle pain: 12-month outcomes from a prospective, multi-center trial. Springerplus 2015; 4: 570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Polly DW, Cher DJ, Wine KD; INSITE Study Group et al. Randomized controlled trial of minimally invasive sacroiliac joint fusion using triangular titanium implants vs nonsurgical management for sacroiliac joint dysfunction: 12-month outcomes. Neurosurgery 2015; 77: 674–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Matias CM, Velagapudi L, Montenegro TS, et al. Minimally invasive sacroiliac fusion-a review. Curr Pain Headache Rep 2022; 26: 173–182. [DOI] [PubMed] [Google Scholar]
- 4.Vanaclocha V, Herrera JM, Sáiz-Sapena N, et al. Minimally invasive sacroiliac joint fusion, radiofrequency denervation, and conservative management for sacroiliac joint pain: 6-year comparative case series. Neurosurgery 2018; 82: 48–55. [DOI] [PubMed] [Google Scholar]
- 5.Ledonio CGT Polly DW JrandSwiontkowski MF.. Minimally invasive versus open sacroiliac joint fusion: are they similarly safe and effective? Clin Orthop Relat Res 2014; 472: 1831–1838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Page MJ, Moher D, Bossuyt PM, et al. PRISMA 2020 explanation and elaboration: updated guidance and exemplars for reporting systematic reviews. BMJ 2021; 372: n160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25: 603–605. [DOI] [PubMed] [Google Scholar]
- 8.Higgins JP, Altman DG, Gøtzsche PC; Cochrane Statistical Methods Group et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011; 343: d5928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Munn Z, Barker TH, Moola S, et al. Methodological quality of case series studies: an introduction to the JBI critical appraisal tool. JBI Evid Synth 2020; 18: 2127–2133. [DOI] [PubMed] [Google Scholar]
- 10.Atkins D, Best D, Briss PA; GRADE Working Group et al. Grading quality of evidence and strength of recommendations. BMJ 2004; 328: 1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Claus CF, Lytle E, Kaufmann A, et al. Minimally invasive sacroiliac joint fusion using triangular titanium versus cylindrical threaded implants: a comparison of patient-reported outcomes. World Neurosurg 2020; 133: E745–E750. [DOI] [PubMed] [Google Scholar]
- 12.Cahueque M, Grajeda J, Ardebol J, et al. Posterior oblique technique for sacroiliac joint fusion leads to greater pain relief and similar improvement in function compared to the lateral technique: A retrospective, comparative study. N Am Spine Soc J 2023; 15: 100259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Khurana A, Guha AR, Mohanty K, et al. Percutaneous fusion of the sacroiliac joint with hollow modular anchorage screws: clinical and radiological outcome. J Bone Joint Surg Br 2009; 91: 627–631. [DOI] [PubMed] [Google Scholar]
- 14.Mason LW, Chopra I, Mohanty K. The percutaneous stabilisation of the sacroiliac joint with hollow modular anchorage screws: a prospective outcome study. Eur Spine J 2013; 22: 2325–2331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Soliman O, Pflugmacher R, Koch EM, et al. One-year results of minimally invasive fusion surgery of the sacroiliac joint as an alternative treatment after failed endoscopic thermal coagulation. Technol Health Care 2022; 30: 1125–1138. [DOI] [PubMed] [Google Scholar]
- 16.Bornemann R, Roessler PP, Strauss AC, et al. Two-year clinical results of patients with sacroiliac joint syndrome treated by arthrodesis using a triangular implant system. Technol Health Care 2017; 25: 319–325. [DOI] [PubMed] [Google Scholar]
- 17.Bricard R, Pelletier Y, Allia J, et al. Minimally invasive sacroiliac joint fusion secondary to lumbosacral fusion: clinical and functional results at 2 years of follow-up. Orthop Traumatol Surg Res 2024; 103892. [DOI] [PubMed] [Google Scholar]
- 18.Cleveland AW 3rd, Nhan DT, Akiyama M, et al. Mini-open sacroiliac joint fusion with direct bone grafting and minimally invasive fixation using intraoperative navigation. J Spine Surg 2019; 5: 31–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cummings J, Jr, Capobianco RA. Minimally invasive sacroiliac joint fusion: one-year outcomes in 18 patients. Ann Surg Innov Res 2013; 7: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dengler J, Kools D, Pflugmacher R, et al. Randomized trial of sacroiliac joint arthrodesis compared with conservative management for chronic low back pain attributed to the sacroiliac joint. J Bone Joint Surg Am 2019; 101: 400–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Duhon BS, Bitan F, Lockstadt H; SIFI Study Group et al. Triangular titanium implants for minimally invasive sacroiliac joint fusion: 2-year follow-up from a prospective multicenter trial. Int J Spine Surg 2016; 10: 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gaetani P, Miotti D, Risso A, et al. Percutaneous arthrodesis of sacro-iliac joint: a pilot study. J Neurosurg Sci 2013; 57: 297–301. [PubMed] [Google Scholar]
- 23.Hermans SMM, Knoef RJH, Schuermans VNE, et al. Double-center observational study of minimally invasive sacroiliac joint fusion for sacroiliac joint dysfunction: one-year results. J Orthop Surg Res 2022; 17: 570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Patel V, Kovalsky D, Meyer SC, et al. Prospective trial of sacroiliac joint fusion using 3D-printed triangular titanium implants: 24-month follow-up. Med Devices (Auckl) 2021; 14: 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Polly DW, Swofford J, Whang PG; INSITE Study Group et al. Two-year outcomes from a randomized controlled trial of minimally invasive sacroiliac joint fusion vs. non-surgical management for sacroiliac joint dysfunction. Int J Spine Surg 2016; 10: 28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Rainov NG, Schneiderhan R, Heidecke V. Triangular titanium implants for sacroiliac joint fusion. Eur Spine J 2019; 28: 727–734. [DOI] [PubMed] [Google Scholar]
- 27.Randers EM, Gerdhem P, Stuge B, et al. The effect of minimally invasive sacroiliac joint fusion compared to sham operation: a double-blind randomized-controlled trial. EClinicalMedicine 2024; 68: 102438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rudolf L, Capobianco R. Five-year clinical and radiographic outcomes after minimally invasive sacroiliac joint fusion using triangular implants. Open Orthop J 2014; 8: 375–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sachs D, Kovalsky D, Redmond A, et al. Durable intermediate-to long-term outcomes after minimally invasive transiliac sacroiliac joint fusion using triangular titanium implants. Med Devices (Auckl) 2016; 9: 213–222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schmidt GL, Bologna M, Schorr R. Patient reported clinical outcomes of minimally invasive sacroiliac joint arthrodesis. Orthop Surg 2021; 13: 71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Smith AG, Capobianco R, Cher D, et al. Open versus minimally invasive sacroiliac joint fusion: a multi-center comparison of perioperative measures and clinical outcomes. Ann Surg Innov Res 2013; 7: 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kancherla VK, McGowan SM, Audley BN, et al. Patient reported outcomes from sacroiliac joint fusion. Asian Spine J 2017; 11: 120–126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Agarwal R, Moreau JL, Mohanty K. Hydroxyapatite-coated screws versus titanium triangular dowels for sacroiliac joint fusion: results from a nonrandomized prospective outcome study. World Neurosurg 2024; 184: e367–e373. [DOI] [PubMed] [Google Scholar]
- 34.Chaves JPG, Maalouly J, Choi JYS. Clinical results following robotic navigation guidance for sacroiliac joint fusion in 36 patients. Neurosurg Focus 2022; 52: E6. [DOI] [PubMed] [Google Scholar]
- 35.Jedi F, Krysiak R, Hirsch JA, et al. Chronic sacroiliac joint dysfunction and CT-guided percutaneous fixation: a 6-year experience. Neuroradiology 2023; 65: 1527–1534. [DOI] [PubMed] [Google Scholar]
- 36.Mohit A, Shirk T. Minimally invasive sacroiliac joint fusion using a novel hydroxyapatite-coated screw system improves functional outcomes in patients with sacroiliitis at two year follow-up. Interdisciplinary Neurosurgery 2020; 22: 100834. [Google Scholar]
- 37.Rappoport LH, Helsper K, Shirk T. Minimally invasive sacroiliac joint fusion using a novel hydroxyapatite-coated screw: final 2-year clinical and radiographic results. J Spine Surg 2021; 7: 155–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cross WW, Delbridge A, Hales D, et al. Minimally invasive sacroiliac joint fusion: 2-year radiographic and clinical outcomes with a principles-based SIJ fusion system. Open Orthop J 2018; 12: 7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Kube RA, Muir JM. Sacroiliac joint fusion: one year clinical and radiographic results following minimally invasive sacroiliac joint fusion surgery. Open Orthop J 2016; 10: 679–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kucharzyk D, Colle K, Boone C, et al. Clinical outcomes following minimally invasive sacroiliac joint fusion with decortication: The EVoluSIon clinical study. Int J Spine Surg 2022; 16: 168–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kasapovic A, Schwetje D, Ali T, et al. First clinical results of a novel minimally-invasive fusion system for the sacroiliac joint. Technol Health Care 2022; 30: 1139–1145. [DOI] [PubMed] [Google Scholar]
- 42.Abbasi H, Storlie N, Rusten M. Perioperative outcomes of minimally invasive sacroilliac joint fusion using hollow screws through a lateral approach: a single surgeon retrospective cohort study. Cureus 2021; 13: e16517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Davies M, Dreischarf M, Yusufbekov R. Catamaran SI joint fusion system(R) MAINSAIL™ study: a prospective, single-arm, multi-center, post-market study of six-month clinical outcomes and twelve-month radiographic findings. Expert Rev Med Devices 2024; 21: 851–858. [DOI] [PubMed] [Google Scholar]
- 44.Endres S, Ludwig E. Outcome of distraction interference arthrodesis of the sacroiliac joint for sacroiliac arthritis. Indian J Orthop 2013; 47: 437–442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Fuchs V, Ruhl B. Distraction arthrodesis of the sacroiliac joint: 2-year results of a descriptive prospective multi-center cohort study in 171 patients. Eur Spine J 2018; 27: 194–204. [DOI] [PubMed] [Google Scholar]
- 46.Calodney A, Azeem N, Buchanan P, et al. Safety, efficacy, and durability of outcomes: results from SECURE: a single arm, multicenter, prospective, clinical study on a minimally invasive posterior sacroiliac fusion allograft implant. J Pain Res 2024; 17: 1209–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Moghim R, Bovinet C, Jin MY, et al. Clinical outcomes for minimally invasive sacroiliac joint fusion with allograft using a posterior approach. Pain Pract 2025; 25: e13406. [DOI] [PubMed] [Google Scholar]
- 48.Sayed D, Balter K, Pyles S, et al. A multicenter retrospective analysis of the long-term efficacy and safety of a novel posterior sacroiliac fusion device. J Pain Res 2021; 14: 3251–3258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kaye AD, Okereke JS, Howe CA, et al. Posterior sacroiliac fusion surgery: a retrospective single center study. Pain Physician 2024; 27: 321–331. [PubMed] [Google Scholar]
- 50.Deer TR, Rupp A, Budwany R, et al. Pain relief salvage with a novel minimally invasive posterior sacroiliac joint fusion device in patients with previously implanted pain devices and therapies. J Pain Res 2021; 14: 2709–2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lynch PJ, Tubic G, Foster JM, et al. Minimally invasive inferior intra-articular sacroiliac joint fusion: successful application of osseous stabilization using allograft bone. Orthop Res Rev 2022; 14: 429–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wise CL, Dall BE. Minimally invasive sacroiliac arthrodesis: outcomes of a new technique. J Spinal Disord Tech 2008; 21: 579–584. [DOI] [PubMed] [Google Scholar]
- 53.Cross WW, 3rd, Tomov MN, Hung MY, et al. Patient-reported outcomes and computed tomography review after minimally invasive fusion of the sacroiliac joint with aggressive joint decortication and joint compression. Orthopedics 2024; 47: 101–107. [DOI] [PubMed] [Google Scholar]
- 54.Anton G, Alsalahi A, Yoon EJ, et al. Fusion and patient-reported outcomes after navigated decortication and direct arthrodesis in minimally invasive sacroiliac joint fusion using cylindrical threaded implants: a case series and literature review. Neurosurg Focus 2023; 55: E2. [DOI] [PubMed] [Google Scholar]
- 55.Rajpal S, Burneikiene S. Minimally invasive sacroiliac joint fusion with cylindrical threaded implants using intraoperative stereotactic navigation. World Neurosurg 2019; 122: e1588–e1591. [DOI] [PubMed] [Google Scholar]
- 56.Raikar SV, Nilles-Melchert T, Patil AA, et al. Posterior oblique approach for sacroiliac joint fusion. Cureus 2023; 15: e33502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Foreman M, Maddy K, Patel A, et al. Differentiating lumbar spinal etiology from peripheral plexopathies. Biomedicines 2023; 11: 756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ballatori AM, Shahrestani S, Chen XT, et al. Propensity-matched analysis of 1062 patients following minimally invasive versus open sacroiliac joint fusion. Clin Spine Surg 2021; 34: E477–E482. [DOI] [PubMed] [Google Scholar]
- 59.Yson SC, Sembrano JN, Polly DW., Jr. Sacroiliac joint fusion: approaches and recent outcomes. PM R 2019; 11: S114–S117. [DOI] [PubMed] [Google Scholar]
- 60.Ghaddaf AA, Alsharef JF, Alsharef NK, et al. Minimally invasive sacroiliac joint fusion using triangular titanium implants versus nonsurgical management for sacroiliac joint dysfunction: a systematic review and meta-analysis. Can J Surg 2024; 67: E16–E26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mehkri Y, Tishad A, Nichols S, et al. Outcomes after minimally invasive sacroiliac joint fusion: a scoping review. World Neurosurg 2022; 168: 120–132. [DOI] [PubMed] [Google Scholar]
- 62.Whang PG, Patel V, Duhon B, et al. Minimally invasive SI joint fusion procedures for chronic SI joint pain: systematic review and meta-analysis of safety and efficacy. Int J Spine Surg 2023; 17: 794–808. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-imr-10.1177_03000605251315300 for Minimally invasive lateral, posterior, and posterolateral sacroiliac joint fusion for low back pain: a systematic review and meta-analysis by Kai Xu, Ya-Ling Li, Song-Hua Xiao and Yong-Wei Pan in Journal of International Medical Research
Data Availability Statement
The datasets are available from the corresponding author upon reasonable request.