Abstract
Parvovirus B19 (B19) was discovered in 1974 and is the only member of the family Parvoviridae known to be pathogenic in humans. Despite the inability to propagate the virus in cell cultures, much has been learned about the pathophysiology of this virus, including the identification of the cellular receptor (P antigen), and the control of the virus by the immune system. B19 is widespread, and manifestations of infection vary with the immunologic and hematologic status of the host. In healthy immunocompetent individuals B19 is the cause of erythema infectiosum and, particularly in adults, acute symmetric polyarthropathy. Due to the tropism of B19 to erythroid progenitor cells, infection in individuals with an underlying hemolytic disorder causes transient aplastic crisis. In the immunocompromised host persistent B19 infection is manifested as pure red cell aplasia and chronic anemia. Likewise, the immature immune response of the fetus may render it susceptible to infection, leading to fetal death in utero, hydrops fetalis, or development of congenital anemia. B19 has also been suggested as the causative agent in a variety of clinical syndromes, but given the common nature, causality is often difficult to infer. Diagnosis is primarily based on detection of specific antibodies by enzyme-linked immunosorbent assay or detection of viral DNA by dot blot hybridization or PCR. Treatment of persistent infection with immunoglobulin reduces the viral load and results in a marked resolution of anemia. Vaccine phase I trials show promising results.
INTRODUCTION
Parvovirus B19 (B19) was discovered serendipitously in 1974 and is the only member of the family Parvoviridae known to be pathogenic in humans. The virus is widespread, and manifestations of infection vary with the immunologic and hematologic status of the host. In healthy immunocompetent children, B19 is the cause of erythema infectiosum, an innocuous rash illness. Infection is occasionally, especially in adults, associated with an acute symmetric polyarthropathy that may mimic rheumatoid arthritis. Due to the tropism of B19 to erythroid progenitor cells, infection in individuals with an underlying hemolytic disorder causes transient aplastic crisis. In the immunocompromised host, persistent B19 infection is manifested as pure red cell aplasia and chronic anemia. Likewise, the immature immune response of the fetus may render it susceptible to infection, leading to fetal death in utero, hydrops fetalis, or development of congenital anemia. Diagnosis is primarily based on detection of specific antibodies by enzyme-linked immunosorbent assay or detection of viral DNA by dot blot hybridization or PCR. Treatment of persistent infection with immunoglobulin reduces the viral load and results in a marked resolution of anemia.
DISCOVERY AND BRIEF HISTORY
In 1974, Cossart et al. first identified B19 while evaluating tests for hepatitis B virus surface antigen (74). The name originates from the coding of a serum sample, number 19 in panel B, that gave anomalous results when tested by counterimmunoelectrophoresis and radioimmunoassay. Electron microscopy (EM) revealed the presence of 23-nm-diameter particles resembling animal parvoviruses. B19 was independently described in Japan 5 years later as “Nakatani” virus, but subsequent testing proved the two viruses to be identical (Okochi et al., Letter, Lancet i:160-161, 1984). Extraction of DNA revealed complementary single strands of approximately 5.5 kb encapsidated in separate virions (329), and the viral proteins were found to copurify with viral antigen at a density of 1.43 g/ml (64), indicating that the virus was a member of the genus Parvovirus. Although originally labeled “serum parvovirus-like particle” or human parvovirus, it was officially recognized in 1985 as a member of the Parvoviridae and given the name B19 by the International Committee on Taxonomy of Viruses (310).
In 1980 a brief and uneventful febrile episode was noted in two soldiers, and B19 was detected in serum by EM (309). There was still no disease distinctly connected with the virus until an association with transient aplastic crisis in patients with sickle cell anemia was observed in 1981 (Pattison et al., Letter, Lancet i:664-665, 1981). Sera from Jamaican children residing in London were observed to contain B19 antigen at the time of aplastic crisis, while convalescent-phase sera showed evidence of seroconversion. Two years later, erythema infectiosum was seroepidemiologically linked to B19 infection in healthy children (Anderson et al., Letter, Lancet i:1378, 1983) and is now accepted as the etiological agent of this disease. Shortly thereafter, other clearly defined syndromes related to B19 infection were described, such as fetal loss in the midtrimester of pregnancy due to intrauterine transmission from an infected mother (46) and postinfectious symmetrical peripheral polyarthropathy or arthritis in adults (267, 360). In its chronic form B19 was found to cause pure red cell aplasia, which could be ameliorated by immunoglobulin (171).
CLASSIFICATION, STRUCTURE, AND ORGANIZATION
Taxonomy
The classification of the family Parvoviridae relies on morphology and functional characteristics. Parvoviruses are common animal and insect pathogens. Until the recent identification of the circoviruses and the related TT viruses, parvoviruses were among the smallest DNA-containing viruses able to infect mammalian cells; hence, the name “parvum” (Latin), meaning small (27). Based on the ability to infect vertebrate or invertebrate cells the Parvoviridae are divided into Parvovirinae and Densovirinae, respectively (27, 147). Parvovirinae are subdivided into three genera according to their transcription maps, the nature of the terminal repeats, and the ability to efficiently replicate either autonomously (genus Parvovirus), with helper virus (genus Dependovirus), or preferentially in erythroid cells (genus Erythrovirus) (Table 1). Only members of the Dependovirus and Erythrovirus genera are known to infect humans. The members of genus Dependovirus, which includes the adeno-associated viruses 1 to 6, require coinfection of target cells with adenovirus or herpesvirus for efficient replication. So far no dependovirus has been definitively associated with human disease (28). B19 is autonomous in the sense that it does not require the presence of a helper virus and was, therefore, until recently classified in the genus Parvovirus. Since replication only occurs in erythrocyte precursors, B19 is now classified as a member of the Erythrovirus genus, of which it is the only accepted member and type species (147). Closely related viruses, which cause similar diseases in primates, have been proposed as additional members in the Erythrovirus genus (Table 1).
TABLE 1.
Excerpt of the current classification of the subfamily Parvovirinae, including proposed members of the genus Erythrovirus placed tentatively (147)
| Genus | Virus | Natural host(s) | Clinical spectrum |
|---|---|---|---|
| Parvovirus | Aleutian mink disease virus | Mink, ferret, skunk, raccoon | Immune complex disease and fetal death |
| Canine parvovirus | Dog | Enteritis, myocarditis | |
| Mice minute virus | Mouse, rat | No known disease | |
| Porcine parvovirus | Pig | Abortion, fetal death | |
| Dependovirus | Adeno-associated virus 1 to 6 | Human | No known disease |
| Avian adeno-associated virus | Birds | No known disease | |
| Canine adeno-associated virus | Dog | No known disease | |
| Bovine adeno-associated virus | Cow | No known disease | |
| Erythrovirus | Parvovirus B19 | Human | Erythema infectiosum, aplastic crisis, arthritis, hydrops fetalis, etc. |
| Parvovirus V9a | Human | Aplastic crisis? | |
| Chipmunk parvovirusa | Chipmunk | No known disease | |
| Simian parvovirusa | Cynomolgus monkeys | Anemia | |
| Pig-tailed macaque parvovirusa | Pig-tailed macaques | Anemia and immunosuppression | |
| Rhesus parvovirusa | Rhesus monkeys | Anemia |
Proposed member of genus.
Morphology
The B19 virion has a simple structure composed of only two proteins and a linear, single-strand DNA molecule (27). The nonenveloped viral particles are ∼22 to 24 nm in diameter and show icosahedral symmetry, and often both empty and full capsids are visible by negative staining and EM (Fig. 1) (27, 74). Mature infectious viral particles have a molecular weight of 5.6 × 106 and a buoyant density in a cesium chloride gradient of 1.41 g/ml (27, 160). The virion is composed of 60 copies of capsomer, and both negative and positive strands of DNA are packaged (27, 379). X-ray crystallography has shown that the surface of B19 is significantly different from those of other parvoviruses by lacking prominent spikes on the threefold icosahedral axes involved in host recognition and antigenicity (2, 27). The limited DNA content and the absence of a lipid envelope make B19 extremely resistant to physical inactivation. The virus is stable at 56°C for 60 min, and lipid solvents have no effect (298). Inactivation of virus may be achieved by formalin, β-propiolactone, and gamma irradiation (Cohen and Brown, Letter, J. Infect. 24:113-114, 1992).
FIG. 1.
Viral particles at a magnification of ×250,000. Scale bar = 100 nm.
Genomic Structure and Organization
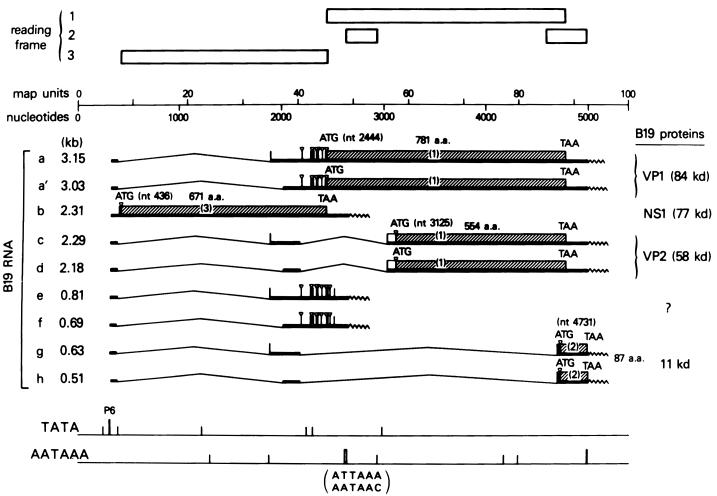
The single-stranded genome contains 5,596 nucleotides (nt), composed of an internal coding sequence of 4,830 nt flanked by the terminal repeat sequences of 383 nt each (80) (Fig. 2). The terminal sequences are palindromic and capable of assuming hairpin duplex configurations, serving as primers for the synthesis of the complementary strand (14). As in most animal parvoviruses, the B19 genome has two large open reading frames, with the single nonstructural protein (NS1) encoded by genes on the left side of the genome and the two capsid proteins (VP1 and VP2) by genes on the right side. Transcription produces at least nine overlapping mRNA transcripts, all initiating from the single P6 promoter at the extreme left side of the genome (80, 186, 246). The most important viral proteins include the major nonstructural protein NS1 and the two structural proteins VP1 and VP2 (76, 246). In addition, while other parvoviruses coterminate RNA species at polyadenylation sites at the far right side, several B19 transcripts terminate in the middle of the genome and use an unusual polyadenylation signal (328). These RNAs are derived from the left side of the genome and share an open reading frame with NS1.
FIG. 2.
Transcription map of B19. Transcripts are in order by length. Open bars indicate reading frames. Adapted from reference 246 with permission.
Sequence Variability
The nucleotide sequence of B19 was originally established by sequencing a viral isolate designated pvbaua obtained from the serum of a child with homozygous sickle cell disease (303). Since then a large number of isolates have been sequenced entirely or in part, and although sequence differences can be detected by restriction enzyme analysis, single-stranded conformational polymorphism analysis of PCR products, and sequencing (94), by multiple alignment the reported B19 isolates are all intimately clustered and show only 6% divergence among themselves. Not unexpectedly, the NS1 gene is well conserved among most field isolates, consistent with a required role in virus propagation, while the VP1 and VP2 regions may occasionally show a greater variability of 2 to 3% (140, 206). No correlation between specific disease symptoms and B19 sequence has been observed (140, 341, 342), and the conservation of sequence is such that sequencing is generally unhelpful in investigating single-source outbreaks.
Recently, a B19 isolate, tentatively termed V9, was identified in a French child with transient aplastic anemia, and on sequence analysis this isolate was seen to be markedly (>11%) different from other B19 sequences (229; Nguyen et al., Letter, Lancet 352:1524, 1998). Standard B19 serological tests failed to demonstrate an acute B19 infection, and it was therefore suggested that the observed aplastic crisis was due to infection by V9, a putative emerging virus, which did not show cross-reactivity with B19-specific tests. Many standard B19 PCR primers would have missed V9, demonstrating the need for specific techniques when examining samples for V9 and possibly related viruses. Although in one study using such V9 primers and screening plasma pools no V9 isolates were identified (131), the prevalence of V9 and its association with clinical disease remains unknown.
Capsid and Nonstructural Proteins
Capsid proteins.
The B19 capsid is composed of two capsomer proteins, VP1 and VP2, which are encoded by overlapping reading frames (76, 246). Each capsid consists of an icosahedral structure with a total of 60 capsomers: VP2 is the major structural protein, accounting for 96% of total capsid protein (250). The VP2 protein is encoded by sequences from nt 3125 to 4786 and has a molecular mass of 58 kDa (250, 303). The minor capsid protein, VP1, is encoded by the sequence from nt 2444 to 4786 and is identical to VP2 with the addition of 227 amino acids (termed the VP1 unique region) at the amino terminus (250, 303). The VP1 protein has a molecular mass of 84 kDa and makes up the remaining 4% of the total capsid protein (250). VP2 and VP1 can be expressed in bacterial, mammalian, and insect cells. In mammalian and insect cells, expression of VP2 can self-assemble in the absence of viral DNA to produce virus-like particles (VLP) that are physically, antigenically and immunogenically similar to native virions (155, 156).
Although a divergence of up to 3% on the amino acid level has been noted in different B19 strains, there is no evidence of more than one antigenic strain. Similarly, translation of the recently identified V9 sequence indicates that despite a significant genetic variation on the DNA level, the majority of the discrepant DNA sequence represents silent mutations, leading to an amino acid sequence very similar to those of the known B19 strains (96 to 97% homology). Based on the V9 VP2 protein, baculovirus-expressed capsids show 100% serologic cross-reactivity between B19 and V9 (136).
Nonstructural proteins.
A number of nonstructural proteins have been identified (76, 246, 250). The major nonstructural protein, NS1 (nt 435 to 2448), has a molecular mass of 77 kDa (76, 246, 250, 303). The function of the NS1 protein is not fully characterized, although, based on data from other parvoviruses, it is thought to possess site-specific DNA-binding, DNA-nicking, ATPase, transcriptional, and helicase activities (60-62, 75, 84, 361), which may explain its pronounced cytotoxicity (84, 200, 247, 324). Accordingly, it was demonstrated that NS1 cytotoxicity is closely related to apoptosis by a pathway involving caspase 3, whose activation may be a key event during NS1-induced cell death (200). NS1 contains a well-conserved nucleoside triphosphate-binding motif, which is essential for a variety of biological functions (201). Cytotoxicity is abolished when single amino acid mutations are introduced in this domain. The cloning and expression of NS1 protein in prokaryotic (139, 152, 300, 345, 349, 350) and eukaryotic (141) systems have provided an opportunity to study the functional and immunologic properties of NS1. The results of these studies are equivocal and have been the subject of ongoing investigations, as discussed below under “Detection of NS1-specific antibodies.”
In addition to those expressing NS1 protein, other open reading frames have been discovered on the left side of the genome, but the roles of the derived proteins are not known. The smallest RNAs of 500 to 600 nt are translated into at least two 11-kDa proteins in B19-infected human leukemic bone marrow (BM) cells (327), and a second minor open reading frame directs synthesis of a 7.5-kDa protein (186). The function of both classes of proteins is currently unknown.
PATHOGENESIS AND INFECTION
Viral Life Cycle and Blood Group P Receptor
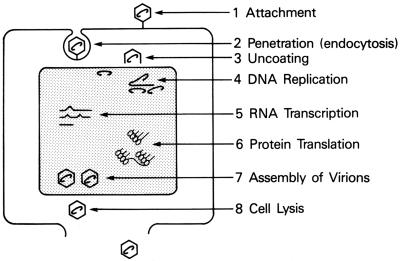
The life cycle of B19, like those of other nonenveloped DNA viruses, includes binding of the virus to host cell receptors, internalization, translocation of the genome to the host nucleus, DNA replication, RNA transcription, assembly of capsids and packaging of the genome, and finally cell lysis with release of the mature virions (Fig. 3).
FIG. 3.
Schematic life cycle of B19.
B19 was initially shown to agglutinate human red cells (41), and it was hypothesized that the same agglutinin may act as the host cell receptor on erythroid progenitor cells. Thus, the hemagglutinin was identified as the glycolipid globoside, also known as the blood group P antigen, by using hemagglutination as a surrogate marker (40). B19 and B19 VP2 VLP both bind directly to P antigen, and in tissue culture either excess P antigen or anti-P monoclonal antibody can protect erythroid progenitors from infection with B19, thus demonstrating that P antigen is the B19 receptor (40). In addition, individuals who genetically lack P antigen (1 in 200,000 individuals) are naturally resistant to B19 infection: none show serologic evidence of past infection, and BM cells in in vitro studies maintain normal erythropoiesis and cannot be infected even in the presence of high concentrations of virus (43).
P antigen is expressed on erythroid progenitors, consistent with the observed tropism of B19 (347). However, the presence of P antigen is almost certainly not sufficient to explain the tropism of B19 to erythroid cells. P antigen is also present on megakaryocytes, endothelial cells, and fetal myocytes (276); however, none of these cell types have been shown to be permissive for B19 replication. Transfection studies of permissive and nonpermissive cells with plasmids containing B19 genome suggest that in cells nonpermissive for B19 there may be a block in full-length transcript production, leading to expression of the cytotoxic NS1 but no production of capsid transcripts (184). Alternatively, tropism may be mediated by the presence of a second, as yet unidentified receptor. However, the expression of P antigen on these cell types may mediate transplacental infection, contribute to the rash of erythema infectiosum, or lead to myocarditis. Also, the level of P-antigen expression does not correlate with the efficiency of viral binding, providing further evidence for the existence of a putative cellular coreceptor for efficient entry of B19 into human cells (356).
Culture
There is no animal model for B19, and virus can only be grown in culture with difficulty. In vitro studies of B19 in explanted human BM cultures have confirmed the erythroid specificity of this virus (249), with B19 inhibition of the colony formation of late erythroid progenitors and the more primitive burst-forming erythroid progenitors and sparing of the myeloid precursors (208). While the pluripotent stem cell is sheltered, the susceptibility of erythroid progenitors to B19 infection increases with differentiation (332). B19 can be cultured in erythroid progenitor cells from a variety of sources, including human BM (248, 249, 325), fetal liver (44, 204, 368), umbilical blood (322, 326), and peripheral blood (297, 302). In all culture systems erythropoietin is required to maintain viral replication, probably by supporting the rapid division of erythroid progenitors. All systems are culture explants only and are not suitable for long-term culture.
However, B19 can also be propagated in a few specialized cell lines: two megakaryoblastoid cell lines, MB-02 (212) and UT-7/Epo (305), and two human erythroid leukemia cell lines, JK-1 (333) and KU812Ep6 (197). These lines have been used to study mechanisms of replication and to develop neutralization (33) and infectivity assays (197). However, the yield of virus from all these cultures is poor, and they cannot be used as a source of antigen for diagnostic tests.
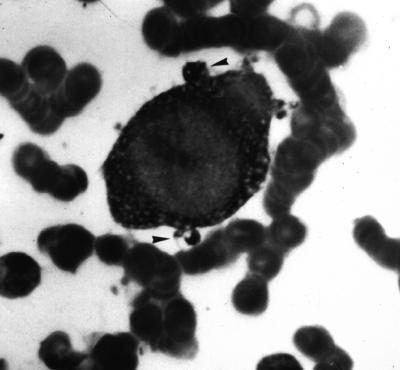
Cytopathology
The cytopathic effect of infection of erythroid progenitor cells with B19, both in vivo and in vitro, is manifested as giant pronormoblasts (alternately referred to as lantern cells), first recognized in 1948 in the BM of patients with transient aplastic crisis (245). Giant pronormoblasts are early erythroid cells with a diameter of 25 to 32 μm, large eosinophilic nuclear inclusion bodies, and cytoplasmic vacuolization, and occasionally, “dog-ear” projections may be observed (as indicated in Fig. 4) (44, 55, 168, 249). EM of cells reveals cytopathic ultrastructural changes that include pseudopod formation, marginated chromatin, and virus particles in the nucleus (378).
FIG. 4.
Giant pronormoblast. Arrowheads indicate dog-ear projections.
Pathogenesis and Immune Response
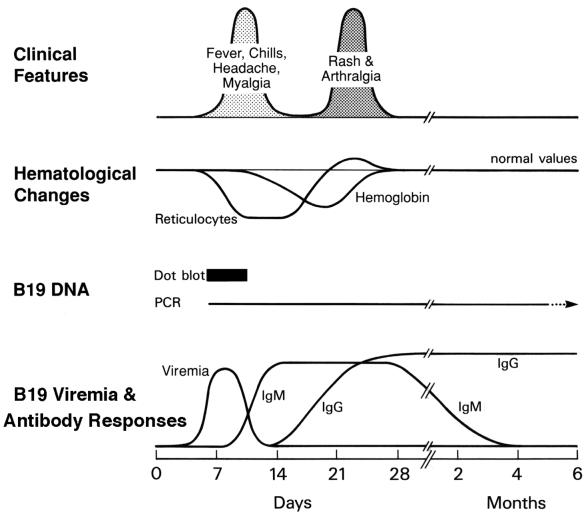
Specific immunoglobulin M (IgM) and IgG antibodies are produced following experimental (8, 260) and natural (279) B19 infection (Fig. 5). Infection leads to a biphasic clinical course: One week after intranasal inoculation with B19 in healthy adult volunteers viremia was detected in seronegative individuals accompanied by a mild illness with pyrexia, malaise, myalgia, itching, and excretion of virus from the respiratory tract. About 17 to18 days after infection, a second phase of symptoms commenced and was characterized by rash, itching, or arthralgia. Recovery involves production of IgM antibody 10 to 12 days postinfection, coinciding with a peak in virus level. IgM usually persists in serum samples for approximately 3 months but may be found for several months (6). IgG antibody is detectable in volunteers about 2 weeks after inoculation and presumably persists for life and protects against secondary infections. IgA may also be detected and probably plays a role in protection against infection by the natural nasopharyngeal route (95).
FIG. 5.
Virologic, immunologic, and clinical course following B19 infection. Data from references 8 and 254.
During viremia reticulocyte numbers fall to undetectable levels, recovering 7 to 10 days later, resulting in a temporary drop in hemoglobin of 1 g/dl (0.6 mmol/liter) in a healthy person (Fig. 5). Clinically nonsignificant lymphopenia, neutropenia, and thrombocytopenia occur 6 to 10 days after inoculation. All hematologic parameters may exhibit a brief overshoot prior to stabilizing at preincubation levels. Viral replication in neutrophils has been proposed by one group (174), but these results have not been confirmed by others. This may provide an explanation for the neutropenia sometimes observed, although B19 is apparently not linked to the development of clinically significant neutropenia (174; Hartman et al., Letter, Br. J. Haematol. 88:895-896, 1994). The infrequently reported fulminant thrombocytopenia associated with B19 infection may consist of two types. In one type, thrombocytopenia precedes the onset of rash due to BM suppression, while the other type is probably mediated by immunologic mechanisms, which will be discussed in further detail below under “Thrombocytopenia”.
In healthy B19-infected individuals the predominant immune response is humoral (173). The early antibody response consists of IgM and is directed against VP2, while the mature response is characterized by an increased avidity that involves IgG as the major antibody subclass and VP1 as the primary target, despite its less-abundant relative concentration in the virion (115, 173). Several regions containing neutralizing epitopes have been located to VP2 (36, 287, 288, 371) and the VP1-unique region (86, 274). However, neutralizing linear epitopes seem to cluster in the VP1-unique and VP1-VP2 junction regions, eliciting a far more efficient immune response compared to the VP2 region (282). Accordingly, VP1 is the major conformational antigen recognized by convalescent-phase sera and commercial immunoglobulin preparations (173). While recombinant empty capsids composed of VP2 only do elicit a weak neutralizing activity, the findings suggest that the conformation of some VP2 determinants is altered by insertion of one to two VP1 molecules per 60-protein-subunit native viral capsid, and the unique region of VP1 is, therefore, necessary for the virus to assume its mature capsid conformation (275).
A cellular immune response to B19 has been much harder to detect, although it must be present to illicit the humoral response (173). Recent studies have suggested that individuals mount a classic Th1 response to the virus (71), with capsid proteins presented to CD4 T cells through class II molecules (104, 348).
The pattern of clinical disease is strongly influenced by the hematologic and immunologic status of the host. In the healthy host, B19 infection may cause a self-limiting subclinical erythroid aplasia, followed by rash or arthralgia mediated by the immune response (8, 260). In patients suffering from diminished production or increased destruction of erythrocytes, infection can result in a dramatic decrease of hemoglobin, leading to aplastic crisis (Pattison et al., letter), whereas immunocompromised individuals might fail to eradicate virus, thereby generating a state of chronic anemia (166).
EPIDEMIOLOGY
Prevalence and Incidence
B19 is a global and common infectious pathogen in humans. The prevalence of IgG antibodies directed against B19 ranges from 2 to 15% in children 1 to 5 years old, 15 to 60% in children 6 to 19 years old, 30 to 60% in adults, and more than 85% in the geriatric population (6, 68, 159, 339). Women of childbearing age show an annual seroconversion rate of 1.5% (165). Although antibody is prevalent in the general population, viremia or presence of viral DNA is rare. The frequency of B19 viremia in voluntary blood donors has been estimated at rates of 1:167 to 1:35,000 (Table 2) (153, 303, 339, 351, 375). As opposed to the many studies on B19 serology and viremia, information on the presence of B19 DNA in the BM of healthy individuals is limited. While no serum was available for comparison, one study discovered B19 DNA in BM of 4 of 45 (9%) healthy BM donors (52), and another reported no evidence of B19 DNA in the BM of 13 bone donors (103).
TABLE 2.
Prevalence of B19 DNA in blood donors
| Reference | No. of samples | No. of B19-positive samples | Frequency | % Prevalence |
|---|---|---|---|---|
| Tsujimura et al. (339) | 560,000 | 16 | 1:35,000 | 0.003 |
| Wakamatsu et al. (351) | 257,710 | 31 | 1:8,313 | 0.012 |
| Heegaard et al. (131) | 100,000 | 17 | 1:5,882 | 0.017 |
| McOmish et al. (193) | 20,000 | 6 | 1:3,333 | 0.03 |
| Jordan et al. (153) | 9,568 | 11 | 1:870 | 0.11 |
| Yoto et al. (375) | 1,000 | 6 | 1:167 | 0.6 |
Seasonal Changes and Contagiousness
The peak incidence of erythema infectiosum shows seasonal variation, occurring mainly during the months of late winter and early spring. Rates of infection may rise to an epidemic level every 3 to 4 years, which is then reflected in the community by an increased number of children with erythema infectiosum, or, where applicable, transient aplastic crisis. During outbreaks of erythema infectiosum or B19-induced aplastic crisis, 10% of cases occur among children <5 years old, 70% of cases occur in children aged 5 to 15 years, and 20% of cases occur among patients older than 15 years (4).
Secondary spread to seronegative contacts is very common. In school or household settings the secondary attack rate during epidemics of erythema infectiosum is about 50% in susceptible children and 20 to 30% in susceptible teachers (5, 364). Apart from teachers, the highest occupational risk of infection is generally found in people in close contact with children, such as day care workers (9%) and homemakers (9%), while women working in other settings have a reduced risk (4%) (51, 112).
Transmission
Transmission of infection occurs via the respiratory route, through blood-derived products administered parenterally, and vertically from mother to fetus. B19-specific DNA has been detected in respiratory secretions at the time of viremia, suggesting that virus is generally spread in the community by a respiratory route. The case-to-case interval is 6 to 11 days irrespective of the type of B19-related disease. Vertical transmission occurs in one-third of cases involving serologically confirmed primary maternal infections (261). Nosocomial transmission has been described infrequently (98, 170, 198), and transmission has also been reported among staff in laboratories handling native virus (69, 306; Cohen and Brown, letter).
The risk of infection using single-donor blood products is reportedly varied but is probably low as outlined in Table 2 (153). Conversely, as a large number of blood donations make up the plasma pools used to produce plasma derivatives, clotting-factor concentrates may very often be contaminated. Studies have detected B19 in two of three unheated batches of factor preparations and in 20 to 25% of solvent- or detergent-treated batches, while the fractionation process used to obtain albumin preparations is apparently more efficient at eliminating virus (369), but B19 was still found in 3 of 12 batches in one study (181-183, 193, 273, 284). B19 DNA has also been detected in all of 25 solvent- or detergent-treated plasma batches (321).
Even after the introduction of virus-inactivated clotting-factor concentrates, a B19 seroprevalence among hemophiliacs of ∼90% has been observed, with correlation to the amount of clotting factor received (17, 272). B19 may also infrequently be transmitted by BM (133) and blood-derived products such as platelets (66), intravenous immunoglobulin (93), and fibrin products (143), and B19 infection and seroconversion have been observed in patients after receiving solvent- or detergent-treated plasma units (17, 45).
DIAGNOSIS OF B19
Diagnostic Cytopathology
Although the presence of giant pronormoblasts in either BM or peripheral blood is suggestive of B19 infection, their presence or absence should not be used alone to make a diagnosis of B19 infection. These cells are often absent in patients with human immunodeficiency virus (HIV) infection or other chronic infections.
Detection of B19 Virus
Although B19 can be detected in serum by EM, B19 antigen enzyme-linked immunosorbent assays, and even hemagglutination, B19 virus is usually detected by isolation of viral DNA by direct hybridization or PCR. Direct hybridization, usually as a slot blot or dot blot format, generally employs an almost-full-length viral DNA probe labeled with 32P, digoxigenin, or biotin to bind to DNA in clinical specimens (10, 207). Results of the hybridization assay are readily quantifiable, with a detection limit of ∼105 genome copies/ml, and the hybridization assay will detect all known variants of B19, including V9 (230).
Although direct hybridization is sensitive enough to detect B19 levels in acute transient aplastic crisis and pure red cell aplasia due to B19 infection in immunosuppressed patients, lower levels of viremia will be missed. The advent of PCR has greatly increased the sensitivity of DNA detection in serum and tissue samples, although it possesses a great propensity for contamination (153, 183, 193, 254, 311, 375). DNA may be detectable for extended periods of time in serum (54, 218, 254), synovial membranes (278), and BM (52), even in healthy individuals. Therefore, the presence of low levels of B19 DNA alone cannot be used to diagnose acute B19 infection. In addition, although most primer pairs based on the pvbaua isolate are able to detect temporally and geographically diverse B19 isolates (89), most primer pairs would not have detected the V9 variant, and ideally two sets of primers should be used to ensure that B19 has not been missed.
Detection of Antibodies
Although B19 DNA-based assays are crucial for the diagnosis of B19 infection presenting as transient aplastic crisis (before the antibody response) and in chronic infections in immunosuppressed individuals (who fail to make an immune response), diagnosis of B19 infection in immunocompetent individuals presenting with erythema infectiosum or B19-induced arthropathy is by detection of B19-specific antibody. Due to the inability of B19 to efficiently replicate in culture systems, viral capsids were initially purified from serum with high virus titer and used for antibody tests (6, 351). B19 antigen can be expressed in bacteria, in cell lines (24), or as peptides, but currently most antigen is produced in insect cell lines with recombinant baculovirus (156). These recombinant antigens are noninfectious, and serologic results correlate well with those using native virus (155). Commercial assays are dependent upon expression of capsid proteins as VLP in the baculovirus expression system, which has proven to be very efficient in producing large quantities of empty VP1/VP2 and VP2 capsids (37-39, 115, 167, 285).
IgM capture assays will reliably detect a current or recent infection in immunocompetent persons (48, 52, 151, 295). Accordingly, more than 85% of patients with erythema infectiosum or aplastic crisis due to B19 exhibit specific IgM (6), and these antibodies will remain detectable for 2 to 3 months following infection. Tests using an indirect method of detection are less useful for diagnosis due to reduced specificity and sensitivity. In contrast, for detection of IgG both capture assays and indirect assays may be used. Two weeks following infection IgG is usually present and persists for life. Sequential sera may show a decline in IgG titer, but detection of IgG is generally not useful for diagnosis of acute infection, apart from detecting a seroconversion in immunocompromised patients, who may not be able to produce IgM. However, a significant correlation between the relative amounts of low-avidity specific IgG antibodies and time after onset of illness has been documented (115, 318) but is probably of minor clinical use.
Detection of NS1-specific antibodies.
The significance of detecting NS1-specific IgG has been continuously discussed and contested since this antibody was suggested to be associated with an altered course of disease (349, 350). One group has repeatedly argued that NS1-specific IgG is primarily found in patients with arthritis or persistent B19 infection (139, 161, 349, 350). It is believed that prolonged viremia may lead to infection of cells outside the erythroid lineage (nonpermissive cells) in which gene expression shifts towards the preferential transcription of the NS1 gene rather than the VP1 and VP2 genes (184, 251, 303). The cytotoxic and apoptotic effects of NS1 (84, 200, 247, 303, 324) may result in cell lysis and the release of NS1 protein, thereby rendering this nonstructural viral component accessible to the immune system of the host. Hence, viral persistence may be a precondition for the formation of NS1-specific antibodies (139, 247). Conversely, others have found no evidence of NS1 IgG representing a marker of persistent infection or contributing to pathogenesis (152, 196, 300, 345). Most of the studies find that, irrespective of the underlying disease, NS1-specific IgG appears late in infection (>6 weeks), and the NS1 antibody test may, therefore, be used to exclude very recent infections in patients with an otherwise unclear serology (139, 152, 300, 345).
CLINICAL ASPECTS
The spectrum of disease linked to B19 primarily involves infection in the healthy host manifested as erythema infectiosum, arthralgia, and hydrops, as well as a number of hematologic symptoms in predisposed individuals (Table 3). In addition, detection of B19 DNA has been linked to a heterogeneous group of diseases in which the causality is unconfirmed.
TABLE 3.
Summary of clinical manifestations following B19 infection
| Manifestation | References |
|---|---|
| Infection in the healthy host | |
| Asymptomatic infection | 51, 364 |
| Erythema infectiosum | 8, 13, 19, 221, 223, 258, 364, 380, and lettera |
| Arthropathy | 8, 83, 154, 222, 225, 265, 267, 278, 319, 323, 334, 360, 363, 364 |
| B19 infection in pregnancy | 3, 42, 46, 47, 90, 91, 97, 102, 117, 123, 129, 130, 158, 163, 195, 202, 261, 270, 277, 292, 296, 299, 314, 317, 335, 358, 365, 366, 367 |
| Thrombocytopenia | 8, 137, 146, 157, 215, 220, 260, 376, and lettersb |
| TEC and neutropenia | 49, 85, 119, 166, 192, 199, 211, 220, 226, 271, 362, 377, and lettersc |
| Neurologic disease | 20, 34, 53, 99, 135, 146, 231, 240, 256, 312, 338, 344, 353, 355, 372, 380, and lettersd |
| Myocarditis | 11, 30, 32, 58, 92, 128, 150, 202, 203, 205, 217, 226, 237, 259, 283, 293, 294, 337, and letterse |
| Hepatitis | 29, 87, 142, 224, 236, 252, 281, 320, 373 |
| Putative associations | 57, 63, 82, 122, 188, 209, 213, 227, 233, 253, 291, 307, 370, 374, and lettersf |
| Infection in the immunodeficient host | |
| Chronic pure red cell aplasia | 1, 15, 16, 23, 35, 50, 56, 70, 73, 77, 79, 96, 100, 105, 106, 108, 109, 110, 114, 126, 127, 132, 134, 138, 162, 166, 171, 172, 173, 175, 178, 194, 219, 228, 232, 257, 262, 263, 290, 313, 315, 312, 330, 331, 344, and lettersg |
| VAHS | 145, 191, 280, 286, 308, 340, 352, and letterh |
| Infection in patients with increased red cell turnover: transient aplastic crisis | 7, 26, 59, 85, 88, 113, 114, 120, 124, 177, 179, 185, 187, 210, 264, 266, 279, 289, 301, and lettersi |
Anderson et al., Lancet i:1378, 1983.
Foreman et al., Lancet ii:1426-1427, 1988; Oeda et al., Am. J. Hematol. 45:274-275, 1994.
Bhambhani et al., Lancet i:509, 1986; Hartman et al., Br. J. Haematol. 88:895-896, 1994; Nikkari et al., Br. J. Haematol. 83:679, 1993.
Denning et al., J. Neurol. Neurosurg. Psychiatry 50:641-642, 1987; Oeda et al., Am. J. Hematol. 45:274-275, 1994.
Beghetti et al., Eur. J. Pediatr. 159:135-136, 2000; Malm et al., Lancet 341:1408-1409, 1993; Orth et al., Eur. Heart J. 18:524-525, 1997.
Bagot and Revuz, J. Am. Acad. Dermatol. 25:341-342, 1991; Cohen, Lancet 344:59, 1994; Corman and Dolson, Lancet 339:491, 1992; Kiraz et al., Ann. Rheum. Dis. 60:814-815, 2001; Lefrere et al., Pediatrics 78:183-184, 1986.
Anderson et al., Lancet i:1378, 1983; Courouce et al., Lancet i:160, 1984; Hitchins and Sloots, Aust. N. Z. J. Med. 23:217-218, 1993; Itala et al., Leukemia 11:171, 1997; Malarme et al., Lancet i:1457, 1989; Murray et al., J. Pediatr. Hematol. Oncol. 18:97-98, 1996; Smith et al., Am. J. Hematol. 50:226-227, 1995; Vernazza et al., Clin. Infect. Dis. 22:198-199, 1996; Weiland et al., Br. J. Haematol. 71:300, 1989.
Toyoshige and Takahashi, Int. J. Hematol. 67:205-206, 1998.
Hamon et al., J. Clin. Pathol. 41:1242, 1988; Pattison et al., Lancet i:664-665, 1981.
Infection in the Healthy Host
Asymptomatic infection.
Subclinical B19 infection is a common finding in both children and adults. One study revealed 25% of infected persons had no recollection of specific symptoms (364), and fewer than half of IgM-positive women show signs of rash or arthralgia (51). Asymptomatic seroconversion following recent transfusion in patients with hemolytic anemia suggests that symptoms may be masked by transfusion of erythrocytes with a longer life span than the defective erythrocytes of the host (7). In some cases nonspecific symptoms indistinguishable from the common flu may be noted.
Erythema infectiosum.
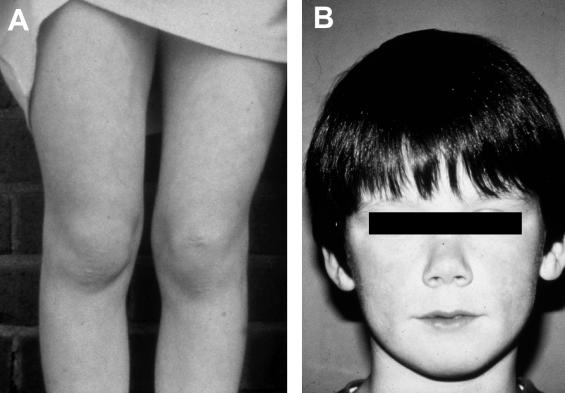
Erythema infectiosum, also referred to as “slapped cheek” disease or fifth disease, is the most prevalent manifestation of infection in children (8). Following an outbreak of erythema infectiosum an association with B19 was made by the discovery of specific IgM in specimens from the involved patients (Anderson et al., letter, 1983). This disease entity was well known prior to the discovery of B19 (19), which is now recognized as the only etiologic agent of erythema infectiosum (13, 221, 258). Prodromal symptoms often go unnoticed but may include fever, coryza, headache, and nausea. Erythema infectiosum is characterized by a facial erythema of medium intensity involving the cheeks, but with relative circumoral pallor (slapped cheek appearance) beginning 18 days after infection (Fig. 6). A second stage consisting of a rash involving the trunk and limbs occurs 1 to 4 days later. The rash is frequently lacy or reticular and consists of pink maculae that usually undergo a central fading, which causes the rash to take on a festooned appearance. The rash may be transient or recurrent, and fluctuations of intensity can be linked to environmental factors such as exposure to sunlight and heat (223). Other symptoms include itching, vesicles, and scaly dermatitis (364, 380).
FIG. 6.
Erythema infectiosum with a reticular rash of the legs(A) and slapped cheeks (B).
Arthropathy.
In 1985 an association between arthropathy and B19 infection was made (267, 360). In children with erythema infectiosum the incidence of arthralgia is approximately 10% or less, while 19% of children with recent-onset arthritis showed evidence of recent B19 infection (235). Among the latter persistent arthritis for 2 to 13 months, which would fulfill criteria for the diagnosis of juvenile rheumatoid arthritis, was observed.
In contrast, arthralgia and arthritis are the most common manifestations of primary B19 infection in adults, affecting 60% of females and 30% of males, while dermal affection is less frequent and uncharacteristic in the adult population (8, 154, 364). The arthropathy is presumably immunologically mediated since the onset coincides with the appearance of circulating antibodies. Joint symptoms appear as an acute, moderately severe peripheral polyarthritis involving the metacarpophalangeal joints (75%), knees (65%), wrists (55%), and ankles (40%), showing no articular erosions (363). About 50% of patients with chronic B19 arthropathy meet the criteria of the American Rheumatoid Association for a diagnosis of rheumatoid arthritis (222, 225). It has been postulated that B19 is involved in the initiation and perpetuation of rheumatoid arthritis leading to joint lesions (334), but these results have not been reproduced by other groups (and Brown, unpublished observations). Recently, an experimental in vitro system was established in which healthy primary human synovial fibroblasts were treated with or without B19-containing human sera and then tested for their ability to degrade reconstituted cartilage matrix (265). Incubation with B19 induced an invasive phenotype in the fibroblasts, and preincubation of viremic serum with a neutralizing antibody to B19 eliminated the observed effect. It seems unlikely, though, that B19 plays a role in classic erosive rheumatoid arthritis, but understanding the pathogenesis of B19 arthropathy may provide insight into the mechanisms by which rheumatoid arthritis develops (222). Accordingly, during long-term follow-up none of 54 patients with B19-associated arthralgia reported persistence of joint swelling or restricted motion, and no evidence of inflammatory joint disease was found (323). In conclusion, despite B19 mimicking rheumatoid arthritis in the acute stage and detection of B19 DNA in synovial fluid (83) and synovial biopsy specimens (278), a convincing link to chronic erosive arthropathy has yet to be demonstrated (319).
B19 infection in pregnancy. (i) Hydrops fetalis.
The discovery of B19 causing nonimmune hydrops fetalis has led to significant public concern (46). It has since been found that fetal B19 infection may also cause fetal or congenital anemia, abortion, or stillbirth or result in an asymptomatic self-limiting episode. A few case reports have speculated on B19 causing congenital malformations (158, 335; Weiland et al., Letter, Lancet i:682-683, 1987), though systematic studies have failed to substantiate this hypothesis (47, 117, 261).
The pathogenesis of fetal damage appears to be similar to that of patients with aplastic crisis in which the erythrocytes have a reduced life span. Erythroblasts in the fetal liver exhibit signs of B19 infection, including pathognomic cytopathology, viral DNA, and antigen (3, 55). In utero infection is persistent and characterized by severe anemia, high-output cardiac failure, and death (365). Impaired circulation due to fetal myocarditis may contribute to the accumulation of fluids (Fig. 7) (202). B19 might also be associated with cases of nonhydropic intrauterine fetal death (314).
FIG. 7.
B19-associated hydrops fetalis.
The incidence of primary B19 infection during pregnancy has been estimated at 1 to 5% (47, 123, 163), and the subsequent transplacental transmission is 24 to 33% (3, 90, 261, 367). The risk of developing hydrops following this infection is reportedly varied (0 to 24%) (3, 91, 97, 102, 117, 270, 296), but according to recent studies the rate is probably quite low (1 to 1.6%) (123, 195, 299). However, in pregnant women with a confirmed primary infection, the overall risk of an abnormal outcome is approximately 5 to 10% (91, 261, 270). Nonimmune hydrops fetalis is rare (1 in 3,000), and in 20 to 50% of cases the etiology is unknown (148, 354). Meta-analysis has shown that B19 accounts for 15 to 20% of cases of nonimmune hydrops fetalis, with a mean interval between the onset of maternal infection and fetal symptoms of 6 weeks (367). The chance of an adverse fetal outcome after infection seems to be greatest between 11 and 23 weeks of gestation, which correlates with the hepatic period of hematopoietic activity (366, 367). Cordocentesis allows precise assessment of fetal anemia, which might then be corrected by intravenous transfusion of erythrocytes (292). Accordingly, in series of hydropic fetuses the case fatality rate may be almost 50% (102, 195, 317), but transfusions have proved beneficial, lowering the mortality rate to 18% (292).
(ii) Congenital anemia.
Hematologic evaluation has revealed anemia in each of the examined B19-associated hydropic fetuses reported (102, 292, 304, 317), although no cases of congenital anemia have been found in prognostic studies on outcome of series of hydropic fetuses following B19 infection (102, 195, 304, 317). However, three infants with hydrops and congenital anemia due to transplacental B19 infection have been described (42). In all three the sera lacked B19 DNA, but viral DNA was found in BM. One infant died, and the others remained persistently anemic despite continued treatment with immunoglobulin. In children diagnosed with Diamond-Blackfan anemia, a congenital anemia disorder, B19 DNA was detected in 3 of 11 BM smears, and giant pronormoblasts showed low sensitivity (33%) and poor specificity (75%) (129). The B19-positive children were the only children who experienced a remission, while the seven surviving B19-negative patients remained on steroid treatment. In another report, an infant developed congenital anemia due to a possible B19 infection (277). At the age of 10 months immunoglobulin therapy was commenced, and 8 months later the anemia gradually resolved. Recently, B19 infection causing severe hydrops fetalis and subsequent congenital anemia, which was corrected by multiple intrauterine transfusions and postnatal immunoglobulin, was described (130). Despite frequent reports of intrauterine B19 infection and hydrops, the risk of associated congenital anemia is apparently low. This may be explained by B19 causing severe disease in only the first two trimesters (366, 367). Ordinarily, infection probably leads to one of two outcomes: lethal hydrops or a milder course of disease in which the virus is eradicated and the ill effects ameliorated before term. However, the paucity of cases of congenital anemia may also reflect underdiagnosis.
Thrombocytopenia.
In children, unlike in adults, most cases of idiopathic thrombocytopenic purpura (ITP) are of acute onset and are often preceded by a specific viral infection (22, 157). Accordingly, B19 infection may result in subclinical or overt thrombocytopenia in volunteers and patients (8, 215, 260, 376; Foreman et al., Letter, Lancet ii:1426-1427, 1988). One study demonstrated a current or recent B19 infection in 6 of 47 pediatric ITP patients (13%), and it was suggested that children with ITP and associated B19 infection are characterized by acute onset of profound thrombocytopenia (137). Among the B19-positive children, duration of disease was brief in three children treated with immunoglobulin but chronic in the remaining three patients given high-dose steroids.
B19-induced thrombocytopenia seems to consist of a central and a peripheral type (157). Thrombocytopenia of central origin is due to BM suppression (220), and the possible cytopathologic effect is underlined by the finding that the NS1 protein, produced by B19, has been found to inhibit the megakaryocytic colony formation (247, 324). This indicates tissue tropism of B19 beyond the erythroid progenitor cell and shows that viral proteins may be toxic to cell populations that are nonpermissive for viral DNA replication. Destructive thrombocytopenia of peripheral origin may result from immunologically mediated antiplatelet antibody production with subsequent excessive platelet clearance in the reticuloendothelial system (146; Foreman et al., letter; Oeda et al., Letter, Am. J. Hematol. 45:274-275, 1994).
TEC and neutropenia.
Transient erythroblastopenia of childhood (TEC) is a disorder of young children, ages 3 to 4 years, characterized by anemia, reticulocytopenia, and decreased red blood cell precursors in the BM aspirate. TEC is the most common single cause of red cell aplasia in immunocompetent children, and other cytopenias are increasingly being recognized in these patients (119, 176, 220). B19 has been a prime viral suspect in TEC patients due to its hematopoietic effects and has been implicated in a number of cases (199, 220, 362; Muir and Fitzsimons, Letter, Br. J. Haematol. 81:622, 1992; Nikkari et al., Letter, Br. J. Haematol. 83:679, 1993). Review of the literature, however, indicates that B19 is not the cause of anemia in young patients with typical features of TEC (271, 377; Bhambhani et al., Letter, Lancet i:509, 1986). Rather, B19 infection may occasionally cause a protracted anemia, often with thrombocytopenia, which erroneously may be diagnosed by some as TEC, leaving the etiology of TEC unresolved.
Primary autoimmune neutropenia is caused by granulocyte-specific autoantibodies and occurs predominantly in infancy. Encouraged by initial case reports (85, 119, 166, 226, 362) and volunteer studies (8, 260) the BM of children with neutropenia was examined for B19 DNA (192). Results indicated that B19 infection may be a common cause of immune-mediated neutropenia in childhood (15 of 19 patients), but larger, more recent studies have not been able to verify this (49; Hartman et al., letter).
Neurologic disease.
Prior to the advent of specific virologic techniques, neurologic symptoms associated with erythema infectiosum were reported in a few cases (20, 34). Since, B19-specific antibodies and/or DNA in blood and cerebrospinal fluid have been detected in fatal (135) and nonfatal cases of encephalopathy (231, 380; Watanabe et al., Letter, Arch. Dis. Child. 70:71, 1994; Yoto et al., Letter, Lancet 344:624-625, 1994) and aseptic meningitis (53, 146, 240, 312; Tsuji et al., Letter, Eur. J. Pediatr. 149:449-450, 1990; Oeda et al., letter). Neuropathy (Faden et al., Letter, J. Infect. Dis. 161:354-355, 1990), complex regional pain syndrome (343, 353), and neuralgic amyotrophy (Denning et al., Letter, J. Neurol. Neurosurg. Psychiatry 50:641-642, 1987; Pellas et al., Letter, Lancet 342:503-504, 1993) have also been observed after B19 infection. Detection of IgM (Tsuji et al., letter) and DNA (53, 240; Watanabe et al., letter; Yoto et al., Letter, Lancet 344:624-625, 1994) in cerebrospinal fluid seems to be a very rare event, reported in only five patients. One patient suffering from seizures received successful immunoglobulin therapy (231). The mechanism for the neurological symptoms is unknown, but frequently rash or arthralgia is also present, suggesting that the neuropathy may be immune mediated.
Myocarditis.
Histologic examination and the finding of specific DNA in the nuclei of fetal myocytes demonstrate the cardiac tropism of B19 (30, 202, 203, 205, 226, 259; Anderson et al., Letter, Lancet i:535, 1988), which may contribute to the development of hydrops fetalis. Clinically significant myocarditis and perimyocarditis have been diagnosed in a few children (32, 92; Beghetti et al., Letter, Eur. J. Pediatr. 159:135-136, 2000; Saint-Martin et al., Letter, J. Pediatr. 116:1007-1008, 1990) and adults (58, 128, 337; Malm et al., Letter, Lancet 341:1408-1409, 1993). In addition, in pediatric cardiac transplant recipients B19 infection has been noted to cause general disease (150, 237) as well as possible myocarditis (293, 294). The finding of myocarditis is puzzling since B19 is thought to replicate only in rapidly dividing cells of hematopoietic origin but may be explained by the tissue distribution of the viral receptor (P antigen) involving myocytes (40) or from immunological cross-reaction to epitopes shared between the virus and the myocardium (217). Considering that B19 is a common infectious agent, and that resulting myocarditis is currently believed to be a rare event, either the virus is only mildly cardiotropic or other unknown concerted factors are required to cause clinical disease.
Hepatitis.
The role of B19 in hepatitis remains unclear. Although transient elevation of liver transaminases is not uncommon in B19 infection, and B19 was originally identified in a sample sent for hepatitis testing, frank hepatitis associated with B19 infection has only rarely been reported (142, 320, 373; Drago et al., Letter, Br. J. Dermatol. 141:160-161, 1999), and in some of these cases the diagnosis of B19 as the cause of the fulminant hepatitis has been questioned (Bernuau et al., Letter, Lancet 353:754-755, 1999). Studies of blood donors with raised transaminases do not suggest that B19 is a major cause of seronegative hepatitis (236). Similarly, B19 has been suggested as a possible causative agent of fulminant liver failure and associated aplastic anemia based on PCR studies (252; Naides et al., Letter, Lancet 347:1563-1564, 1996). However, in both studies the numbers are small and other studies in this area have not confirmed the association (281; Brown et al., unpublished observations).
Putative associations.
B19 has been suggested as the causative agent in a variety of clinical syndromes, but given the common nature, causality is often difficult to infer. Many of these studies are based on case reports or on detection of B19 DNA in tissues by PCR with no corresponding control group.
One investigation of children with Kawasaki disease found B19 viremia in 67% (233), while others subsequently have found no such evidence (63; Cohen, Letter, Lancet 344:59, 1994; Yoto et al., Letter, Lancet 344:58-59, 1994). Other vasculitic and dermatologic syndromes proposedly caused by B19 include purpura (307), thrombotic renal graft microangiopathy (213), Raynaud's phenomenon (122), Henoch-Schönlein purpura (Lefrere et al., Letter, Pediatrics 78:183-184, 1986), polyarteritis nodosa (Corman and Dolson, Letter, Lancet 339:491, 1992), “gloves and socks” papular purpuric syndrome (253; Bagot and Revuz, Letter, J. Am. Acad. Dermatol. 25:341-342, 1991), dermatomyositis (57), and systemic lupus erythematosus (188). Severe pneumonia (150), conjunctivitis (370), Behcet's disease (Kiraz et al., Letter, Ann. Rheum. Dis. 60:814-815, 2001), idiopathic collapsing glomerulopathy (209), chronic autoimmune thrombocytopenia or neutropenia (291), and acute glomerulonephritis (82, 227) have also been suggested as possible manifestations of B19 infection.
Infection in the Immunodeficient Host
Chronic pure red cell aplasia.
In immunocompromised patients unable to mount a neutralizing antibody response due to a persistent BM insufficiency, B19 infection may cause chronic anemia. Predisposing conditions include Nezelof's syndrome (175), acute lymphatic leukemia (ALL) (166, 172), acute myeloid leukemia (Weiland et al., Letter, Br. J. Haematol. 71:300, 1989), chronic myeloid leukemia (106), myelodysplastic syndrome (126), Burkitt's lymphoma (Courouce et al., Letter, Lancet i:160, 1984), lymphoblastic lymphoma (114), myelodysplastic syndrome (23), astrocytoma (114), Wilms's tumor (114), HIV infection (105, 232, 330), SCID (110), BM transplantation (15, 106; Weiland et al., letter, 1989), organ transplantation (73, 228, 237), class switch defect (171), steroid and cancer chemotherapy treatment (114), and defect antibody specificity and neutralization (127, 173).
Patients have absent or low levels of specific antibodies, with persistent or recurrent viremia being detected (175). Clinical hallmarks include fatigue and pallor, while immune-mediated symptoms (rash and arthralgia) are generally not present (166, 175). Infection may serve as a prodrome of an underlying disease (178; Murray et al., Letter, J. Pediatr. Hematol. Oncol. 18:97-98, 1996), and anemia may promptly remit after immunoglobulin (109, 262) or antiviral chemotherapy (in HIV patients) (1, 56, 219, 290). Temporary cessation of maintenance chemotherapy has also led to resolution of anemia (315).
(i) AIDS.
In one initial study involving 50 patients with AIDS, no cases of B19 viremia were identified (Anderson et al., Letter, Ann. Intern. Med. 102:275, 1985). However, the prevalence of B19-induced anemia in HIV-seropositive patients may be underestimated (162; Vernazza et al., Letter, Clin. Infect. Dis. 22:198-199, 1996). Accordingly, B19 DNA was detected by dot blot hybridization in sera from 5 of 30 (17%) HIV-infected patients with hematocrits of ≤24 and 4 of 13 (31%) patients with hematocrits of ≤20, suggesting that B19 is a reasonably common cause of severe anemia in HIV infection (1). The presence of IgM to B19, the clinical circumstance under which anemia developed, and the marrow morphology were poor predictors of chronic B19 infection.
(ii) Acute lymphatic leukemia.
Chronic B19 infection has been described in case reports of adult (96, 257, 313; Hitchins and Sloots, Letter, Aust. N. Z. J. Med. 23:217-218, 1993; Itala et al., Letter, Leukemia 11:171, 1997; Malarme et al., Letter, Lancet i:1457, 1989; Takahashi et al., Letter, Eur. J. Haematol. 46:47, 1991) and pediatric (16, 35, 50, 70, 77, 79, 100, 108, 114, 166, 172, 178, 194, 263, 312, 315, 344; Smith et al., Letter, Am. J. Hematol. 50:226-227, 1995) patients with leukemia. Though no conclusions can be drawn on the basis of these single observations, the reported cases indicate that ALL patients with B19 infection typically present with persistent anemia, while rash or arthropathy is commonly absent. Children with leukemia share the chief age of B19 infections and may be particularly vulnerable to the ill effects of B19 due to immunosuppression. In one study, 8% of B19-seronegative ALL patients seroconverted while on maintenance chemotherapy, and there was a cluster of cases coinciding with a well-established B19 epidemic (138). B19 infection was able to mimic a leukemic relapse or therapy-induced cytopenia and contributed to the development of chronic anemia and profound thrombocytopenia in the majority of infected individuals. Infrequently, isolated thrombocytopenia (132) or transient pancytopenia preceding ALL (134) has also been observed.
Virus-associated hemophagocytic syndrome.
Virus-associated hemophagocytic syndrome (VAHS) is characterized by histiocytic hyperplasia, marked hemophagocytosis, and cytopenia, in association with a systemic viral illness (269). In contrast to malignant histiocytosis, VAHS is usually a benign self-limiting illness, in which histiocytic proliferation is reversible. Hemophagocytosis is not uncommon and occurs in the setting of a wide range of infections, not only viral, but also in the context of bacterial, rickettsial, fungal, and parasitic infections (268). However, in many patients there is underlying immunosuppression, usually iatrogenic, so that the role of the incriminated pathogen as the etiological agent or a coincidental opportunistic infection remains unclear. In two reported cases of VAHS, pure red cell aplasia was concurrent (121, 268).
B19 infection has been detected in cases of hemophagocytosis syndrome among children and adults (145, 191, 280, 286, 308, 340, 352; Toyoshige and Takahashi et al., Letter, Int. J. Hematol. 67:205-206, 1998). Although the majority of patients reported to have VAHS were previously healthy, several patients were immunosuppressed by drug therapies. Further studies are required to determine if B19 is a major cause of VAHS as well as the rate of VAHS in otherwise uncomplicated B19 infection.
Infection in Patients with Increased Red Cell Turnover
Transient aplastic crisis.
Transient aplastic crisis, the first disease to be associated with B19, refers to a brief self-limited episode of pure red cell aplasia and was originally described in patients with hemolytic anemia. However, any person suffering from decreased red cell production or increased destruction or loss will be in danger of developing aplastic crisis following B19 infection. Cessation of the production of erythrocytes for 10 to 15 days, as seen during infection in healthy individuals, will in hemolytic patients lead to a marked drop in hemoglobin due to the underlying decrease in red cell survival in these patients.
Conditions associated with decreased red cell production, thereby rendering patients susceptible to B19-induced aplastic crisis, include iron deficiency (Graeve and Elliott, Letter, J. Pediatr. 118:830, 1991), congenital dyserythropoietic anemia (359), and α- and β-thalassemias (59, 85, 179, 279; Lortholary et al., Letter, Eur. J. Haematol. 49:219, 1992). Infection may also cause transient aplastic crisis in patients with increased red cell destruction or loss, including hereditary spherocytosis (59, 120, 179, 279), hereditary stomatocytosis (187), hereditary elliptocytosis (Lortholary et al., letter), glucose-6-phosphate dehydrogenase deficiency (Lortholary et al., letter), pyruvate kinase deficiency (88), pyrimidine-5′-nucleotidase deficiency (266), sickle cell disease (7, 59, 179, 264, 279, 301; Pattison et al., letter), malaria (Lortholary et al., letter), chronic autoimmune hemolytic anemia (179), cold and heat antibody-mediated autoimmune hemolytic disease (85), paroxysmal nocturnal hemoglobinuria (177), and even blood loss (124). The aplasia may also be associated with hemophagocytic syndrome (289). Severe anemia associated with B19 can also rarely affect apparently healthy subjects with no underlying hematologic disorder (214; Hamon et al., Letter, J. Clin. Pathol. 41:1242, 1988).
Although the erythrocytes are predominantly affected, with presentation often of a pure red cell aplasia, concurrent thrombocytopenia, neutropenia, or pancytopenia is found infrequently (179, 187, 210, 264, 279). While the anemia may be lethal, the aplastic crisis itself is usually terminated by the appearance of specific antibodies and thus rarely lasts for more than 2 weeks. In predisposed individuals 70 to 80% of aplastic episodes are caused by B19 infection (7, 59, 179). The annual incidence is 1 to 5%, predominantly affecting children and representing a unique event in life (7, 59). Aplastic crisis usually presents with pallor, weakness, and lethargy, and patients are highly viremic, thereby posing a risk of transmission to others (7, 26, 59).
TREATMENT
In most cases erythema infectiosum requires no treatment, while some patients with B19-induced arthralgia may need symptomatic treatment (i.e., anti-inflammatory drugs). In cases of transient aplastic crisis caused by B19, prognosis is excellent once a satisfactory hemoglobin concentration is obtained by erythrocyte transfusion (124). B19 infection in pregnant seronegative women should be monitored by weekly ultrasound examinations, and cordocentesis and intrauterine transfusions are effective in lowering the mortality in cases of hydrops fetalis (292). Effective therapy of persistent B19 infection (pure red cell aplasia) consists of infusion of immunoglobulin (0.4 g/kg of body weight/day for 5 days or 1g/kg/day for 2 to 3 days), which is a good source of neutralizing antibodies as the majority of the adult population has been exposed to the virus. This treatment is usually ameliorative and very often curative (105, 107, 169, 171), leading to a marked increase in reticulocyte count and corresponding rise in hemoglobin. On a more experimental note, generation of neutralizing human monoclonal antibodies directed against B19 proteins have been proposed as an immunotherapy of chronically infected individuals and acutely infected pregnant women (111).
FUTURE ADVANCES
Prevention of B19 Infection
Though there is insufficient evidence to recommend universal testing, especially for single units, it has been proposed that B19 screening of blood components destined for children with malignancies be implemented (45). When germane, testing BM donors should also be considered prior to transplantation (133). In addition, assaying of B19 is essential at diagnosis of ALL and HIV to avoid subsequent diagnostic uncertainty and during treatment in other B19-seronegative immunocompromised patients exhibiting unexplained cytopenia.
Empty B19 VP1/VP2 capsids expressed in baculovirus induce neutralizing antibodies in inoculated animals (155) and have been evaluated for immunogenicity in guinea pigs, mice, and rabbits. The presence of VP1 protein is important for elicitation of potent virus-neutralizing activity, and results indicate that VP1-enriched empty capsids could serve as candidates of a recombinant vaccine (21). Sera from experimental animals and human volunteers immunized with such a VLP vaccine candidate exhibit titers of neutralizing antibody equal to or greater than those observed in natural infections (33). Phase I trial results appear promising, and phase II trials are planned.
Animal Models of B19 Infection
Although currently B19 is the only member of the Erythrovirus genus, three primate parvoviruses which are similar to the human B19 parvovirus at the genome level and in their predilection for host BM in vitro have been identified (116, 242, 244). The identification of theses viruses, and especially the simian parvovirus, originally isolated from cynomolgus monkeys, has allowed the development of an animal model for B19 infection. Infection of immunosuppressed macaques with simian parvovirus leads to persistent anemia, whereas in immunocompetent animals there is a transient drop in reticulocytes (243). And as in B19, infection of the immunologically immature fetus leads to the development of hydrops fetalis (M. G. O'Sullivan, D. A. Feeney, et al., Abstr. VIIIth Parvovirus Workshop, abstr. 13.5, 2000). This animal model is currently being used to learn more about the pathophysiology of B19-induced hydrops and to develop better methods for treating infected fetuses.
REFERENCES
- 1.Abkowitz, J. L., K. E. Brown, R. W. Wood, N. L. Kovach, S. W. Green, and N. S. Young. 1997. Clinical relevance of parvovirus B19 as a cause of anemia in patients with human immunodeficiency virus infection. J. Infect. Dis. 176:269-273. [DOI] [PubMed] [Google Scholar]
- 2.Agbandje, M., S. Kajigaya, R. McKenna, N. S. Young, and M. G. Rossmann. 1994. The structure of human parvovirus B19 at 8 A resolution. Virology 203:106-115. [DOI] [PubMed] [Google Scholar]
- 3.Anand, A., E. S. Gray, T. Brown, J. P. Clewley, and B. J. Cohen. 1987. Human parvovirus infection in pregnancy and hydrops fetalis. N. Engl. J. Med. 316:183-186. [DOI] [PubMed] [Google Scholar]
- 4.Anderson, L. J. 1987. Role of parvovirus B19 in human disease. Pediatr. Infect. Dis. J. 6:711-718. [DOI] [PubMed] [Google Scholar]
- 5.Anderson, L. J., S. M. Gillespie, T. J. Torok, E. S. Hurwitz, C. J. Tsou, and G. W. Gary. 1990. Risk of infection following exposures to human parvovirus B19. Behring Inst. Mitt. 85:60-63. [PubMed] [Google Scholar]
- 6.Anderson, L. J., C. Tsou, R. A. Parker, T. L. Chorba, H. Wulff, P. Tattersall, and P. P. Mortimer. 1986. Detection of antibodies and antigens of human parvovirus B19 by enzyme-linked immunosorbent assay. J. Clin. Microbiol. 24:522-526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson, M. J., L. R. Davis, J. Hodgson, S. E. Jones, L. Murtaza, J. R. Pattison, C. E. Stroud, and J. M. White. 1982. Occurrence of infection with a parvovirus-like agent in children with sickle cell anaemia during a two-year period. J. Clin. Pathol. 35:744-749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Anderson, M. J., P. G. Higgins, L. R. Davis, J. S. Willman, S. E. Jones, I. M. Kidd, J. R. Pattison, and D. A. Tyrrell. 1985. Experimental parvoviral infection in humans. J. Infect. Dis. 152:257-265. [DOI] [PubMed] [Google Scholar]
- 9.Reference deleted.
- 10.Anderson, M. J., S. E. Jones, and A. C. Minson. 1985. Diagnosis of human parvovirus infection by dot-blot hybridization using cloned viral DNA. J. Med. Virol. 15:163-172. [DOI] [PubMed] [Google Scholar]
- 11.Reference deleted.
- 12.Reference deleted.
- 13.Anderson, M. J., E. Lewis, I. M. Kidd, S. M. Hall, and B. J. Cohen. 1984. An outbreak of erythema infectiosum associated with human parvovirus infection. J. Hyg. (London) 93:85-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Astell, C. R. 1990. Terminal hairpins of parvovirus genomes and their role in DNA replication, p. 59-80. In P. Tijssen (ed.), Handbook of parvoviruses. CRC Press, Inc., Boca Raton, Fla.
- 15.Azzi, A., R. Fanci, S. Ciappi, K. Zakrzewska, and A. Bosi. 1993. Human parvovirus B19 infection in bone marrow transplantation patients. Am. J. Hematol. 44:207-209. [DOI] [PubMed] [Google Scholar]
- 16.Azzi, A., P. A. Macchia, C. Favre, M. Nardi, K. Zakrzewska, and O. B. Corsi. 1989. Aplastic crisis caused by B19 virus in a child during induction therapy for acute lymphoblastic leukemia. Haematologica 74:191-194. [PubMed] [Google Scholar]
- 17.Azzi, A., M. Morfini, and P. M. Mannucci. 1999. The transfusion-associated transmission of parvovirus B19. Transfus. Med. Rev. 13:194-204. [DOI] [PubMed] [Google Scholar]
- 18.Reference deleted.
- 19.Balfour, H. H. J. 1969. Erythema infectiosum (fifth disease). Clinical review and description of 91 cases seen in an epidemic. Clin. Pediatr. (Philadelphia) 8:721-727. [DOI] [PubMed] [Google Scholar]
- 20.Balfour, H. H. J., G. M. Schiff, and J. E. Bloom. 1970. Encephalitis associated with erythema infectiosum. J. Pediatr. 77:133-136. [DOI] [PubMed] [Google Scholar]
- 21.Bansal, G. P., J. A. Hatfield, F. E. Dunn, A. A. Kramer, F. Brady, C. H. Riggin, M. S. Collett, K. Yoshimoto, S. Kajigaya, and N. S. Young. 1993. Candidate recombinant vaccine for human B19 parvovirus. J. Infect. Dis. 167:1034-1044. [DOI] [PubMed] [Google Scholar]
- 22.Baranski, B., and N. Young. 1987. Hematologic consequences of viral infections. Hematol. Oncol. Clin. N. Am. 1:167-183. [PubMed] [Google Scholar]
- 23.Baurmann, H., T. F. Schwarz, J. Oertel, S. Serke, M. Roggendorf, and D. Huhn. 1992. Acute parvovirus B19 infection mimicking myelodysplastic syndrome of the bone marrow. Ann. Hematol. 64:43-45. [DOI] [PubMed] [Google Scholar]
- 24.Beard, C., J. St. Amand, and C. R. Astell. 1989. Transient expression of B19 parvovirus gene products in COS-7 cells transfected with B19-SV40 hybrid vectors. Virology 172:659-664. [DOI] [PubMed] [Google Scholar]
- 25.Reference deleted.
- 26.Bell, L. M., S. J. Naides, P. Stoffman, R. L. Hodinka, and S. A. Plotkin. 1989. Human parvovirus B19 infection among hospital staff members after contact with infected patients. N. Engl. J. Med. 321:485-491. [DOI] [PubMed] [Google Scholar]
- 27.Berns, K. I. 1996. Parvoviridae: the viruses and their replication, p. 2173-2197. In B. N. Fields, D. M. Knipe, P. M. Howley, R. M. Chanock, J. L. Melnick, T. P. Monath, B. Roizman, and S. E. Straus (ed.), Fields virology. Lippincott-Raven, Philadelphia, Pa.
- 28.Berns, K. I., and R. A. Bohenzky. 1987. Adeno-associated viruses: an update. Adv. Virus Res. 32:243-306. [DOI] [PubMed] [Google Scholar]
- 29.Reference deleted.
- 30.Berry, P. J., E. S. Gray, H. J. Porter, and P. A. Burton. 1992. Parvovirus infection of the human fetus and newborn. Semin. Diagn. Pathol. 9:4-12. [PubMed] [Google Scholar]
- 31.Reference deleted.
- 32.Borreda, D., S. Palomera, B. Gilbert, A. Lienhardt, and L. de Lumley. 1992. 24 cases of human parvovirus B19 infection in children. Ann. Pediatr. (Paris) 39:543-549. (In French.) [PubMed] [Google Scholar]
- 33.Bostic, J. R., K. E. Brown, N. S. Young, and S. Koenig. 1999. Quantitative analysis of neutralizing immune responses to human parvovirus B19 using a novel reverse transcriptase-polymerase chain reaction-based assay. J. Infect. Dis. 179:619-626. [DOI] [PubMed] [Google Scholar]
- 34.Breese, C., and F. A. Horner. 1977. Encephalopathy with erythema infectiosum. Am. J. Dis. Child. 131:65-67. [PubMed] [Google Scholar]
- 35.Broliden, K., T. Tolfvenstam, S. Ohlsson, and J. I. Henter. 1998. Persistent B19 parvovirus infection in pediatric malignancies. Med. Pediatr. Oncol. 31:66-72. [DOI] [PubMed] [Google Scholar]
- 36.Brown, C. S., T. Jensen, R. H. Meloen, W. Puijk, K. Sugamura, H. Sato, and W. J. Spaan. 1992. Localization of an immunodominant domain on baculovirus-produced parvovirus B19 capsids: correlation to a major surface region on the native virus particle. J. Virol. 66:6989-6996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Brown, C. S., M. M. Salimans, M. H. Noteborn, and H. T. Weiland. 1990. Antigenic parvovirus B19 coat proteins VP1 and VP2 produced in large quantities in a baculovirus expression system. Virus Res. 15:197-211. [DOI] [PubMed] [Google Scholar]
- 38.Brown, C. S., M. J. van Bussel, A. L. Wassenaar, A. M. van Elsacker-Niele, H. T. Weiland, and M. M. Salimans. 1990. An immunofluorescence assay for the detection of parvovirus B19 IgG and IgM antibodies based on recombinant viral antigen. J. Virol. Methods 29:53-62. [DOI] [PubMed] [Google Scholar]
- 39.Brown, C. S., J. W. Van Lent, J. M. Vlak, and W. J. Spaan. 1991. Assembly of empty capsids by using baculovirus recombinants expressing human parvovirus B19 structural proteins. J. Virol. 65:2702-2706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brown, K. E., S. M. Anderson, and N. S. Young. 1993. Erythrocyte P antigen: cellular receptor for B19 parvovirus. Science 262:114-117. [DOI] [PubMed] [Google Scholar]
- 41.Brown, K. E., and B. J. Cohen. 1992. Haemagglutination by parvovirus B19. J. Gen. Virol. 73:2147-2149. [DOI] [PubMed] [Google Scholar]
- 42.Brown, K. E., S. W. Green, d. M. Antunez, J. A. Bellanti, S. D. Smith, T. J. Smith, and N. S. Young. 1994. Congenital anaemia after transplacental B19 parvovirus infection. Lancet 343:895-896. [DOI] [PubMed] [Google Scholar]
- 43.Brown, K. E., J. R. Hibbs, G. Gallinella, S. M. Anderson, E. D. Lehman, P. McCarthy, and N. S. Young. 1994. Resistance to parvovirus B19 infection due to lack of virus receptor (erythrocyte P antigen). N. Engl. J. Med. 330:1192-1196. [DOI] [PubMed] [Google Scholar]
- 44.Brown, K. E., J. Mori, B. J. Cohen, and A. M. Field. 1991. In vitro propagation of parvovirus B19 in primary foetal liver culture. J. Gen. Virol. 72:741-745. [DOI] [PubMed] [Google Scholar]
- 45.Brown, K. E., N. S. Young, B. M. Alving, and L. H. Barbosa. 2001. Parvovirus B19: implications for transfusion medicine. Summary of a workshop. Transfusion 41:130-135. [DOI] [PubMed] [Google Scholar]
- 46.Brown, T., A. Anand, L. D. Ritchie, J. P. Clewley, and T. M. Reid. 1984. Intrauterine parvovirus infection associated with hydrops fetalis. Lancet ii:1033-1034. [DOI] [PubMed] [Google Scholar]
- 47.Bruu, A. L., and L. B. Flugsrud. 1994. Erythema infectiosum in pregnancy. A follow-up of children after 2 years. Tidsskr. Nor. Laegeforen 114:308-310. [PubMed] [Google Scholar]
- 48.Bruu, A. L., and S. A. Nordbo. 1995. Evaluation of five commercial tests for detection of immunoglobulin M antibodies to human parvovirus B19. J. Clin. Microbiol. 33:1363-1365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bux, J., G. Behrens, G. Jaeger, and K. Welte. 1998. Diagnosis and clinical course of autoimmune neutropenia in infancy: analysis of 240 cases. Blood 91:181-186. [PubMed] [Google Scholar]
- 50.Carstensen, H., K. Ornvold, and B. J. Cohen. 1989. Human parvovirus B19 infection associated with prolonged erythroblastopenia in a leukemic child. Pediatr. Infect. Dis. J. 8:56. [DOI] [PubMed] [Google Scholar]
- 51.Cartter, M. L., T. A. Farley, S. Rosengren, D. L. Quinn, S. M. Gillespie, G. W. Gary, and J. L. Hadler. 1991. Occupational risk factors for infection with parvovirus B19 among pregnant women. J. Infect. Dis. 163:282-285. [DOI] [PubMed] [Google Scholar]
- 52.Cassinotti, P., G. Burtonboy, M. Fopp, and G. Siegl. 1997. Evidence for persistence of human parvovirus B19 DNA in bone marrow. J. Med. Virol. 53:229-232. [PubMed] [Google Scholar]
- 53.Cassinotti, P., D. Schultze, P. Schlageter, S. Chevili, and G. Siegl. 1993. Persistent human parvovirus B19 infection following an acute infection with meningitis in an immunocompetent patient. Eur. J. Clin. Microbiol. Infect. Dis 12:701-704. [DOI] [PubMed] [Google Scholar]
- 54.Cassinotti, P., and G. Siegl. 2000. Quantitative evidence for persistence of human parvovirus B19 DNA in an immunocompetent individual. Eur. J. Clin. Microbiol. Infect. Dis. 19:886-887. [DOI] [PubMed] [Google Scholar]
- 55.Caul, E. O., M. J. Usher, and P. A. Burton. 1988. Intrauterine infection with human parvovirus B19: a light and electron microscopy study. J. Med Virol. 24:55-66. [DOI] [PubMed] [Google Scholar]
- 56.Chen, M. Y., C. C. Hung, C. T. Fang, and S. M. Hsieh. 2001. Reconstituted immunity against persistent parvovirus B19 infection in a patient with acquired immunodeficiency syndrome after highly active antiretroviral therapy. Clin. Infect Dis. 32:1361-1365. [DOI] [PubMed] [Google Scholar]
- 57.Chevrel, G., A. Calvet, V. Belin, and P. Miossec. 2000. Dermatomyositis associated with the presence of parvovirus B19 DNA in muscle. Rheumatology (Oxford) 39:1037-1039. [DOI] [PubMed] [Google Scholar]
- 58.Chia, J. K., and B. Jackson. 1996. Myopericarditis due to parvovirus B19 in an adult. Clin. Infect. Dis. 23:200-201. [DOI] [PubMed] [Google Scholar]
- 59.Chorba, T., P. Coccia, R. C. Holman, P. Tattersall, L. J. Anderson, J. Sudman, N. S. Young, E. Kurczynski, U. M. Saarinen, and R. Moir. 1986. The role of parvovirus B19 in aplastic crisis and erythema infectiosum (fifth disease). J. Infect. Dis. 154:383-393. [DOI] [PubMed] [Google Scholar]
- 60.Christensen, J., S. F. Cotmore, and P. Tattersall. 1995. Minute virus of mice transcriptional activator protein NS1 binds directly to the transactivation region of the viral P38 promoter in a strictly ATP-dependent manner. J. Virol. 69:5422-5430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Christensen, J., S. F. Cotmore, and P. Tattersall. 1997. A novel cellular site-specific DNA-binding protein cooperates with the viral NS1 polypeptide to initiate parvovirus DNA replication. J. Virol. 71:1405-1416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Christensen, J., M. Pedersen, B. Aasted, and S. Alexandersen. 1995. Purification and characterization of the major nonstructural protein (NS-1) of Aleutian mink disease parvovirus. J. Virol. 69:1802-1809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Chua, P. K., V. R. Nerurkar, Q. Yu, C. L. Woodward, M. E. Melish, and R. Yanagihara. 2000. Lack of association between Kawasaki syndrome and infection with parvovirus B19, human herpesvirus 8, TT virus, GB virus C/hepatitis G virus or Chlamydia pneumoniae. Pediatr. Infect. Dis. J. 19:477-479. [DOI] [PubMed] [Google Scholar]
- 64.Clewley, J. P. 1984. Biochemical characterization of a human parvovirus. J. Gen. Virol. 65:241-245. [DOI] [PubMed] [Google Scholar]
- 65.Reference deleted.
- 66.Cohen, B. J., S. Beard, W. A. Knowles, J. S. Ellis, D. Joske, J. M. Goldman, P. Hewitt, and K. N. Ward. 1997. Chronic anemia due to parvovirus B19 infection in a bone marrow transplant patient after platelet transfusion. Transfusion 37:947-952. [DOI] [PubMed] [Google Scholar]
- 67.Reference deleted.
- 68.Cohen, B. J., and M. M. Buckley. 1988. The prevalence of antibody to human parvovirus B19 in England and Wales. J. Med. Microbiol. 25:151-153. [DOI] [PubMed] [Google Scholar]
- 69.Cohen, B. J., A. M. Courouce, T. F. Schwarz, K. Okochi, and G. J. Kurtzman. 1988. Laboratory infection with parvovirus B19. J. Clin. Pathol. 41:1027-1028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Corbett, T. J., H. Saw, U. Popat, E. MacMahon, B. J. Cohen, W. A. Knowles, S. Beard, and H. G. Prentice. 1995. Successful treatment of parvovirus B19 infection and red cell aplasia occurring after an allogeneic bone marrow transplant. Bone Marrow Transplant. 16:711-713. [PubMed] [Google Scholar]
- 71.Corcoran, A., S. Doyle, D. Waldron, A. Nicholson, and B. P. Mahon. 2000. Impaired gamma interferon responses against parvovirus B19 by recently infected children. J. Virol. 74:9903-9910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Reference deleted.
- 73.Corral, D. A., F. S. Darras, C. W. Jensen, T. R. Hakala, S. J. Naides, J. R. Krause, T. E. Starzl, and M. L. Jordan. 1993. Parvovirus B19 infection causing pure red cell aplasia in a recipient of pediatric donor kidneys. Transplantation 55:427-430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Cossart, Y. E., A. M. Field, B. Cant, and D. Widdows. 1975. Parvovirus-like particles in human sera. Lancet i:72-73. [DOI] [PubMed] [Google Scholar]
- 75.Cotmore, S. F., J. Christensen, J. P. Nuesch, and P. Tattersall. 1995. The NS1 polypeptide of the murine parvovirus minute virus of mice binds to DNA sequences containing the motif [ACCA]2-3. J. Virol. 69:1652-1660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Cotmore, S. F., V. C. McKie, L. J. Anderson, C. R. Astell, and P. Tattersall. 1986. Identification of the major structural and nonstructural proteins encoded by human parvovirus B19 and mapping of their genes by procaryotic expression of isolated genomic fragments. J. Virol. 60:548-557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Coulombel, L., F. Morinet, F. Mielot, and G. Tchernia. 1989. Parvovirus infection, leukemia, and immunodeficiency. Lancet i:101-102. [Google Scholar]
- 78.Reference deleted.
- 79.Crook, T. W., B. B. Rogers, R. D. McFarland, S. H. Kroft, P. Muretto, J. A. Hernandez, M. J. Latimer, and R. W. McKenna. 2000. Unusual bone marrow manifestations of parvovirus B19 infection in immunocompromised patients. Hum. Pathol. 31:161-168. [DOI] [PubMed] [Google Scholar]
- 80.Deiss, V., J. D. Tratschin, M. Weitz, and G. Siegl. 1990. Cloning of the human parvovirus B19 genome and structural analysis of its palindromic termini. Virology 175:247-254. [DOI] [PubMed] [Google Scholar]
- 81.Reference deleted.
- 82.Diaz, F., and J. Collazos. 2000. Glomerulonephritis and Henoch-Schoenlein purpura associated with acute parvovirus B19 infection. Clin. Nephrol. 53:237-238. [PubMed] [Google Scholar]
- 83.Dijkmans, B. A., A. M. van Elsacker-Niele, M. M. Salimans, G. A. van Albada-Kuipers, E. de Vries, and H. T. Weiland. 1988. Human parvovirus B19 DNA in synovial fluid. Arthritis Rheum. 31:279-281. [DOI] [PubMed] [Google Scholar]
- 84.Doerig, C., B. Hirt, J. P. Antonietti, and P. Beard. 1990. Nonstructural protein of parvoviruses B19 and minute virus of mice controls transcription. J. Virol. 64:387-396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Doran, H. M., and A. J. Teall. 1988. Neutropenia accompanying erythroid aplasia in human parvovirus infection. Br. J. Haematol. 69:287-288. [DOI] [PubMed] [Google Scholar]
- 86.Dorsch, S., B. Kaufmann, U. Schaible, E. Prohaska, H. Wolf, and S. Modrow. 2001. The VP1-unique region of parvovirus B19: amino acid variability and antigenic stability. J. Gen. Virol. 82:191-199. [DOI] [PubMed] [Google Scholar]
- 87.Reference deleted.
- 88.Duncan, J. R., C. B. Potter, M. D. Cappellini, J. B. Kurtz, M. J. Anderson, and D. J. Weatherall. 1983. Aplastic crisis due to parvovirus infection in pyruvate kinase deficiency. Lancet ii:14-16. [DOI] [PubMed] [Google Scholar]
- 89.Durigon, E. L., D. D. Erdman, G. W. Gary, M. A. Pallansch, T. J. Torok, and L. J. Anderson. 1993. Multiple primer pairs for polymerase chain reaction (PCR) amplification of human parvovirus B19 DNA. J. Virol. Methods 44:155-165. [DOI] [PubMed] [Google Scholar]
- 90.Eis-Hubinger, A. M., D. Dieck, R. Schild, M. Hansmann, and K. E. Schneweis. 1998. Parvovirus B19 infection in pregnancy. Intervirology 41:178-184. [DOI] [PubMed] [Google Scholar]
- 91.Enders, G., and M. Biber. 1990. Parvovirus B19 infections in pregnancy. Behring Inst. Mitt. 1990:74-78. [PubMed] [Google Scholar]
- 92.Enders, G., J. Dotsch, J. Bauer, W. Nutzenadel, H. Hengel, D. Haffner, G. Schalasta, K. Searle, and K. E. Brown. 1998. Life-threatening parvovirus B19-associated myocarditis and cardiac transplantation as possible therapy: two case reports. Clin. Infect. Dis. 26:355-358. [DOI] [PubMed] [Google Scholar]
- 93.Erdman, D. D., B. C. Anderson, T. J. Torok, T. H. Finkel, and L. J. Anderson. 1997. Possible transmission of parvovirus B19 from intravenous immune globulin. J. Med. Virol. 53:233-236. [PubMed] [Google Scholar]
- 94.Erdman, D. D., E. L. Durigon, Q. Y. Wang, and L. J. Anderson. 1996. Genetic diversity of human parvovirus B19: sequence analysis of the VP1/VP2 gene from multiple isolates. J. Gen. Virol. 77:2767-2774. [DOI] [PubMed] [Google Scholar]
- 95.Erdman, D. D., M. J. Usher, C. Tsou, E. O. Caul, G. W. Gary, S. Kajigaya, N. S. Young, and L. J. Anderson. 1991. Human parvovirus B19 specific IgG, IgA, and IgM antibodies and DNA in serum specimens from persons with erythema infectiosum. J. Med. Virol. 35:110-115. [DOI] [PubMed] [Google Scholar]
- 96.Ergas, D., P. Resnitzky, and A. Berrebi. 1996. Pure red blood cell aplasia associated with parvovirus B19 infection in large granular lymphocyte leukemia. Blood 87:3523-3524. [PubMed] [Google Scholar]
- 97.Essary, L. R., C. L. Vnencak-Jones, S. S. Manning, S. J. Olson, and J. E. Johnson. 1998. Frequency of parvovirus B19 infection in nonimmune hydrops fetalis and utility of three diagnostic methods. Hum. Pathol. 29:696-701. [DOI] [PubMed] [Google Scholar]
- 98.Evans, J. P., M. A. Rossiter, T. O. Kumaran, G. W. Marsh, and P. P. Mortimer. 1984. Human parvovirus aplasia: case due to cross infection in a ward. Br. Med. J. (Clin. Res. Ed.) 288:681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Reference deleted.
- 100.Fisher, D., D. Spencer, H. Iland, S. Brammah, and Y. Cossart. 1992. Red cell aplasia caused by human parvovirus B19 in acute leukaemia. Aust. N. Z. J. Med. 22:303-304. [DOI] [PubMed] [Google Scholar]
- 101.Reference deleted.
- 102.Forestier, F., J. D. Tissot, Y. Vial, F. Daffos, and P. Hohlfeld. 1999. Haematological parameters of parvovirus B19 infection in 13 fetuses with hydrops foetalis. Br. J. Haematol. 104:925-927. [DOI] [PubMed] [Google Scholar]
- 103.Foto, F., K. G. Saag, L. L. Scharosch, E. J. Howard, and S. J. Naides. 1993. Parvovirus B19-specific DNA in bone marrow from B19 arthropathy patients: evidence for B19 virus persistence. J. Infect. Dis. 167:744-748. [DOI] [PubMed] [Google Scholar]
- 104.Franssila, R., K. Hokynar, and K. Hedman. 2001. T helper cell-mediated in vitro responses of recently and remotely infected subjects to a candidate recombinant vaccine for human parvovirus b19. J. Infect. Dis. 183:805-809. [DOI] [PubMed] [Google Scholar]
- 105.Frickhofen, N., J. L. Abkowitz, M. Safford, J. M. Berry, J. Antunez-de-Mayolo, A. Astrow, R. Cohen, I. Halperin, L. King, and D. Mintzer. 1990. Persistent B19 parvovirus infection in patients infected with human immunodeficiency virus type 1 (HIV-1): a treatable cause of anemia in AIDS. Ann. Intern. Med. 113:926-933. [DOI] [PubMed] [Google Scholar]
- 106.Frickhofen, N., R. Arnold, B. Hertenstein, M. Wiesneth, and N. S. Young. 1992. Parvovirus B19 infection and bone marrow transplantation. Ann. Hematol. 64(Suppl.):A121-A124. [DOI] [PubMed] [Google Scholar]
- 107.Frickhofen, N., Z. J. Chen, N. S. Young, B. J. Cohen, H. Heimpel, and J. L. Abkowitz. 1994. Parvovirus B19 as a cause of acquired chronic pure red cell aplasia. Br. J. Haematol. 87:818-824. [DOI] [PubMed] [Google Scholar]
- 108.Fujita, H., K. Takada, K. Kuremoto, K. Ishimoto, N. Sato, A. Tsuji, H. Yoshida, M. Kaneko, H. Hirai, and T. Yamaguchi. 1993. Human parvovirus B19 infection in patients with hematologic disorders on chemotherapy. Rinsho Ketsueki 34:28-33. (In Japanese.) [PubMed] [Google Scholar]
- 109.Fuller, A., L. Moaven, D. Spelman, W. J. Spicer, H. Wraight, D. Curtis, J. Leydon, J. Doultree, and S. Locarnini. 1996. Parvovirus B19 in HIV infection: a treatable cause of anemia. Pathology 28:277-280. [DOI] [PubMed] [Google Scholar]
- 110.Gahr, M., A. Pekrun, and H. Eiffert. 1991. Persistence of parvovirus B19-DNA in blood of a child with severe combined immunodeficiency associated with chronic pure red cell aplasia. Eur. J. Pediatr. 150:470-472. [DOI] [PubMed] [Google Scholar]
- 111.Gigler, A., S. Dorsch, A. Hemauer, C. Williams, S. Kim, N. S. Young, S. Zolla-Pazner, H. Wolf, M. K. Gorny, and S. Modrow. 1999. Generation of neutralizing human monoclonal antibodies against parvovirus B19 proteins. J. Virol. 73:1974-1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Gillespie, S. M., M. L. Cartter, S. Asch, J. B. Rokos, G. W. Gary, C. J. Tsou, D. B. Hall, L. J. Anderson, and E. S. Hurwitz. 1990. Occupational risk of human parvovirus B19 infection for school and day-care personnel during an outbreak of erythema infectiosum. JAMA 263:2061-2065. [PubMed] [Google Scholar]
- 113.Reference deleted.
- 114.Graeve, J. L., P. A. de Alarcon, and S. J. Naides. 1989. Parvovirus B19 infection in patients receiving cancer chemotherapy: the expanding spectrum of disease. Am. J. Pediatr. Hematol. Oncol. 11:441-444. [PubMed] [Google Scholar]
- 115.Gray, J. J., B. J. Cohen, and U. Desselberger. 1993. Detection of human parvovirus B19-specific IgM and IgG antibodies using a recombinant viral VP1 antigen expressed in insect cells and estimation of time of infection by testing for antibody avidity. J. Virol. Methods 44:11-23. [DOI] [PubMed] [Google Scholar]
- 116.Green, S. W., I. Malkovska, M. G. O'Sullivan, and K. E. Brown. 2000. Rhesus and pig-tailed macaque parvoviruses: identification of two new members of the erythrovirus genus in monkeys. Virology 269:105-112. [DOI] [PubMed] [Google Scholar]
- 117.Guidozzi, F., D. Ballot, and A. D. Rothberg. 1994. Human B19 parvovirus infection in an obstetric population. A prospective study determining fetal outcome. J. Reprod. Med. 39:36-38. [PubMed] [Google Scholar]
- 118.Reference deleted.
- 119.Hanada, T., K. Koike, C. Hirano, T. Takeya, T. Suzuki, Y. Matsunaga, and H. Takita. 1989. Childhood transient erythroblastopenia complicated by thrombocytopenia and neutropenia. Eur. J. Haematol. 42:77-80. [DOI] [PubMed] [Google Scholar]
- 120.Hanada, T., K. Koike, T. Takeya, T. Nagasawa, Y. Matsunaga, and H. Takita. 1988. Human parvovirus B19-induced transient pancytopenia in a child with hereditary spherocytosis. Br. J. Haematol. 70:113-115. [DOI] [PubMed] [Google Scholar]
- 121.Hanada, T., H. Yamamura, T. Isobe, M. Nakazawa, T. Abe, and H. Takita. 1986. Pure red cell aplasia in association with malignant histiocytosis. Cancer 57:2325-2328. [DOI] [PubMed] [Google Scholar]
- 122.Harel, L., R. Straussberg, H. Rudich, A. H. Cohen, and J. Amir. 2000. Raynaud's phenomenon as a manifestation of parvovirus B19 infection: case reports and review of parvovirus B19 rheumatic and vasculitic syndromes. Clin. Infect. Dis. 30:500-503. [DOI] [PubMed] [Google Scholar]
- 123.Harger, J. H., S. P. Adler, W. C. Koch, and G. F. Harger. 1998. Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. Obstet. Gynecol. 91:413-420. [DOI] [PubMed] [Google Scholar]
- 124.Harris, J. W. 1992. Parvovirus B19 for the hematologist. Am. J. Hematol. 39:119-130. [DOI] [PubMed] [Google Scholar]
- 125.Reference deleted.
- 126.Hasle, H., E. Heegaard, G. Kerndrup, I. M. Jensen, N. A. Peterslund, and A. Hornsleth. 1996. Parvovirus B19 infection infrequently involved in children and adults with myelodysplastic syndrome. Leuk. Res. 20:81-83. [DOI] [PubMed] [Google Scholar]
- 127.Hasle, H., G. Kerndrup, B. B. Jacobsen, E. D. Heegaard, A. Hornsleth, and S. T. Lillevang. 1994. Chronic parvovirus infection mimicking myelodysplastic syndrome in a child with subclinical immunodeficiency. Am. J. Pediatr. Hematol. Oncol. 16:329-333. [PubMed] [Google Scholar]
- 128.Heegaard, E. D., H. Eiskjaer, U. Baandrup, and A. Hornsleth. 1998. Parvovirus B19 infection associated with myocarditis following adult cardiac transplantation. Scand. J. Infect. Dis. 30:607-610. [DOI] [PubMed] [Google Scholar]
- 129.Heegaard, E. D., H. Hasle, N. Clausen, A. Hornsleth, and G. B. Kerndrup. 1996. Parvovirus B19 infection and Diamond-Blackfan anaemia. Acta Paediatr. 85:299-302. [DOI] [PubMed] [Google Scholar]
- 130.Heegaard, E. D., H. Hasle, L. Skibsted, J. Bock, and K. E. Brown. 2000. Congenital anemia caused by parvovirus B19 infection. Pediatr. Infect. Dis. J. 19:1216-1218. [DOI] [PubMed] [Google Scholar]
- 131.Heegaard, E. D., I. P. Jensen, and J. Christensen. 2001. Novel PCR assay for differential detection and screening of erythrovirus B19 and erythrovirus V9. J. Med. Virol. 65:362-367. [DOI] [PubMed] [Google Scholar]
- 132.Heegaard, E. D., G. B. Kerndrup, N. T. Carlsen, K. Schmiegelow, and A. K. Hornsleth. 1999. Thrombocytopenia caused by Parvovirus B19 infection in a child with acute lymphatic leukemia. Ugeskr. Laeger 161:6501-6502. (In Danish.) [PubMed] [Google Scholar]
- 133.Heegaard, E. D., and P. B. Laub. 2000. Parvovirus B19 transmitted by bone marrow. Br. J. Haematol. 111:659-661. [DOI] [PubMed] [Google Scholar]
- 134.Heegaard, E. D., H. O. Madsen, and K. Schmiegelow. 2001. Transient pancytopenia preceding acute lymphoblastic leukemia (preALL) precipitated by parvovirus B19. Br. J. Haematol. 114:810-813. [DOI] [PubMed] [Google Scholar]
- 135.Heegaard, E. D., N. A. Peterslund, and A. Hornsleth. 1995. Parvovirus B19 infection associated with encephalitis in a patient suffering from malignant lymphoma. Scand. J. Infect. Dis. 27:631-633. [DOI] [PubMed] [Google Scholar]
- 136.Heegaard, E. D., K. Qvortrup, and J. Christensen. 2002. Baculovirus expression of erythrovirus V9 capsids and screening by ELISA: Serologic cross-reactivity with erythrovirus B19. J. Med. Virol. 66:246-252. [DOI] [PubMed] [Google Scholar]
- 137.Heegaard, E. D., S. Rosthoj, B. L. Petersen, S. Nielsen, P. F. Karup, and A. Hornsleth. 1999. Role of parvovirus B19 infection in childhood idiopathic thrombocytopenic purpura. Acta Paediatr. 88:614-617. [DOI] [PubMed] [Google Scholar]
- 138.Heegaard, E. D., and K. Schmiegelow. Serologic study on parvovirus B19 infection in childhood acute lymphoblastic leukemia during chemotherapy: clinical and hematologic implications. J. Pediatr. Hematol. Oncol., in press. [DOI] [PubMed]
- 139.Hemauer, A., A. Gigler, K. Searle, K. Beckenlehner, U. Raab, K. Broliden, H. Wolf, G. Enders, and S. Modrow. 2000. Seroprevalence of parvovirus B19 NS1-specific IgG in B19-infected and uninfected individuals and in infected pregnant women. J. Med. Virol. 60:48-55. [DOI] [PubMed] [Google Scholar]
- 140.Hemauer, A., A. von Poblotzki, A. Gigler, P. Cassinotti, G. Siegl, H. Wolf, and S. Modrow. 1996. Sequence variability among different parvovirus B19 isolates. J. Gen. Virol. 77:1781-1785. [DOI] [PubMed] [Google Scholar]
- 141.Hicks, K. E., R. C. Cubel, B. J. Cohen, and J. P. Clewley. 1996. Sequence analysis of a parvovirus B19 isolate and baculovirus expression of the nonstructural protein. Arch. Virol. 141:1319-1327. [DOI] [PubMed] [Google Scholar]
- 142.Hillingso, J. G., I. P. Jensen, and L. Tom-Petersen. 1998. Parvovirus B19 and acute hepatitis in adults. Lancet 351:955-956. [DOI] [PubMed] [Google Scholar]
- 143.Hino, M., O. Ishiko, K. I. Honda, T. Yamane, K. Ohta, T. Takubo, and N. Tatsumi. 2000. Transmission of symptomatic parvovirus B19 infection by fibrin sealant used during surgery. Br. J. Haematol. 108:194-195. [DOI] [PubMed] [Google Scholar]
- 144.Reference deleted.
- 145.Hoang, M. P., D. B. Dawson, Z. R. Rogers, R. H. Scheuermann, and B. B. Rogers. 1998. Polymerase chain reaction amplification of archival material for Epstein-Barr virus, cytomegalovirus, human herpesvirus 6, and parvovirus B19 in children with bone marrow hemophagocytosis. Hum. Pathol. 29:1074-1077. [DOI] [PubMed] [Google Scholar]
- 146.Inoue, S., N. K. Kinra, S. R. Mukkamala, and R. Gordon. 1991. Parvovirus B-19 infection: aplastic crisis, erythema infectiosum and idiopathic thrombocytopenic purpura. Pediatr. Infect. Dis. J. 10:251-253. [PubMed] [Google Scholar]
- 147.International Committee on Taxonomy of Viruses. 2000. Virus taxonomy: classification and nomenclature of viruses. Seventh report of the International Committee on Taxonomy of Viruses. Springer-Verlag, Vienna, Austria.
- 148.Ismail, K. M., W. L. Martin, S. Ghosh, M. J. Whittle, and M. D. Kilby. 2001. Etiology and outcome of hydrops fetalis. J. Matern. Fetal Med. 10:175-181. [DOI] [PubMed] [Google Scholar]
- 149.Reference deleted.
- 150.Janner, D., J. Bork, M. Baum, and R. Chinnock. 1994. Severe pneumonia after heart transplantation as a result of human parvovirus B19. J. Heart Lung Transplant. 13:336-338. [PubMed] [Google Scholar]
- 151.Jensen, I. P., and B. F. Vestergaard. 1997. Assessment of the specificity of a commercial human parvovirus B19 IgM assay. Clin. Diagn. Virol. 7:133-137. [DOI] [PubMed] [Google Scholar]
- 152.Jones, L. P., D. D. Erdman, and L. J. Anderson. 1999. Prevalence of antibodies to human parvovirus B19 nonstructural protein in persons with various clinical outcomes following B19 infection. J. Infect. Dis. 180:500-504. [DOI] [PubMed] [Google Scholar]
- 153.Jordan, J., B. Tiangco, J. Kiss, and W. Koch. 1998. Human parvovirus B19: prevalence of viral DNA in volunteer blood donors and clinical outcomes of transfusion recipients. Vox Sang. 75:97-102. [PubMed] [Google Scholar]
- 154.Joseph, P. R. 1986. Fifth disease: the frequency of joint involvement in adults. N. Y. State J. Med. 86:560-563. [PubMed] [Google Scholar]
- 155.Kajigaya, S., H. Fujii, A. Field, S. Anderson, S. Rosenfeld, L. J. Anderson, T. Shimada, and N. S. Young. 1991. Self-assembled B19 parvovirus capsids, produced in a baculovirus system, are antigenically and immunogenically similar to native virions. Proc. Natl. Acad. Sci. USA 88:4646-4650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Kajigaya, S., T. Shimada, S. Fujita, and N. S. Young. 1989. A genetically engineered cell line that produces empty capsids of B19 (human) parvovirus. Proc. Natl. Acad. Sci. USA 86:7601-7605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Kaplan, C., F. Morinet, and J. Cartron. 1992. Virus-induced autoimmune thrombocytopenia and neutropenia. Semin. Hematol. 29:34-44. [PubMed] [Google Scholar]
- 158.Katz, V. L., M. C. McCoy, J. A. Kuller, and W. F. Hansen. 1996. An association between fetal parvovirus B19 infection and fetal anomalies: a report of two cases. Am. J. Perinatol. 13:43-45. [DOI] [PubMed] [Google Scholar]
- 159.Kelly, H. A., D. Siebert, R. Hammond, J. Leydon, P. Kiely, and W. Maskill. 2000. The age-specific prevalence of human parvovirus immunity in Victoria, Australia compared with other parts of the world. Epidemiol. Infect. 124:449-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kerr, J. R. 2000. The Parvoviridae; an emerging virus family. Infect. Dis. Rev. 2:99-109. [Google Scholar]
- 161.Kerr, J. R., and V. S. Cunniffe. 2000. Antibodies to parvovirus B19 nonstructural protein are associated with chronic but not acute arthritis following B19 infection. Rheumatology (Oxford) 39:903-908. [DOI] [PubMed] [Google Scholar]
- 162.Kerr, J. R., D. Kane, B. Crowley, N. Leonard, S. O'Briain, P. V. Coyle, and F. Mulcahy. 1997. Parvovirus B19 infection in AIDS patients. Int. J. STD AIDS 8:184-186. [DOI] [PubMed] [Google Scholar]
- 163.Kerr, J. R., H. J. O'Neill, P. V. Coyle, and W. Thompson. 1994. An outbreak of parvovirus B19 infection; a study of clinical manifestations and the incidence of fetal loss. Ir. J. Med. Sci. 163:65-67. [DOI] [PubMed] [Google Scholar]
- 164.Reference deleted.
- 165.Koch, W. C., and S. P. Adler. 1989. Human parvovirus B19 infections in women of childbearing age and within families. Pediatr. Infect. Dis. J. 8:83-87. [PubMed] [Google Scholar]
- 166.Koch, W. C., G. Massey, C. E. Russell, and S. P. Adler. 1990. Manifestations and treatment of human parvovirus B19 infection in immunocompromised patients. J. Pediatr. 116:355-359. [DOI] [PubMed] [Google Scholar]
- 167.Kock, W. C. 1995. A synthetic parvovirus B19 capsid protein can replace viral antigen in antibody-capture enzyme immunoassays. J. Virol. Methods 55:67-82. [DOI] [PubMed] [Google Scholar]
- 168.Koduri, P. R. 1998. Novel cytomorphology of the giant proerythroblasts of parvovirus B19 infection. Am. J. Hematol. 58:95-99. [DOI] [PubMed] [Google Scholar]
- 169.Koduri, P. R., R. Kumapley, J. Valladares, and C. Teter. 1999. Chronic pure red cell aplasia caused by parvovirus B19 in AIDS: use of intravenous immunoglobulin--a report of eight patients. Am. J. Hematol. 61:16-20. [DOI] [PubMed] [Google Scholar]
- 170.Koziol, D. E., G. Kurtzman, J. Ayub, N. S. Young, and D. K. Henderson. 1992. Nosocomial human parvovirus B19 infection: lack of transmission from a chronically infected patient to hospital staff. Infect. Control Hosp. Epidemiol. 13:343-348. (Erratum, 13:511.) [DOI] [PubMed] [Google Scholar]
- 171.Kurtzman, G., N. Frickhofen, J. Kimball, D. W. Jenkins, A. W. Nienhuis, and N. S. Young. 1989. Pure red-cell aplasia of 10 years' duration due to persistent parvovirus B19 infection and its cure with immunoglobulin therapy. N. Engl. J. Med. 321:519-523. [DOI] [PubMed] [Google Scholar]
- 172.Kurtzman, G. J., B. Cohen, P. Meyers, A. Amunullah, and N. S. Young. 1988. Persistent B19 parvovirus infection as a cause of severe chronic anaemia in children with acute lymphocytic leukaemia. Lancet ii:1159-1162. [DOI] [PubMed] [Google Scholar]
- 173.Kurtzman, G. J., B. J. Cohen, A. M. Field, R. Oseas, R. M. Blaese, and N. S. Young. 1989. Immune response to B19 parvovirus and an antibody defect in persistent viral infection. J. Clin. Investig. 84:1114-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Kurtzman, G. J., P. Gascon, M. Caras, B. Cohen, and N. S. Young. 1988. B19 parvovirus replicates in circulating cells of acutely infected patients. Blood 71:1448-1454. [PubMed] [Google Scholar]
- 175.Kurtzman, G. J., K. Ozawa, B. Cohen, G. Hanson, R. Oseas, and N. S. Young. 1987. Chronic bone marrow failure due to persistent B19 parvovirus infection. N. Engl. J. Med. 317:287-294. [DOI] [PubMed] [Google Scholar]
- 176.Kynaston, J. A., N. C. West, and M. M. Reid. 1993. A regional experience of red cell aplasia. Eur. J. Pediatr. 152:306-308. [DOI] [PubMed] [Google Scholar]
- 177.Lakhani, A. K., V. Malkovska, D. H. Bevan, and M. J. Anderson. 1987. Transient pancytopenia associated with parvovirus infection in paroxysmal nocturnal haemoglobinuria. Postgrad. Med. J. 63:483-484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Lee, S. M., D. G. Kim, and D. Bang. 1994. Persistent erythema infectiosum-like rash as a prodrome of acute lymphocytic leukemia. Pediatr. Dermatol. 11:156-159. [DOI] [PubMed] [Google Scholar]
- 179.Lefrere, J. J., A. M. Courouce, Y. Bertrand, R. Girot, and J. P. Soulier. 1986. Human parvovirus and aplastic crisis in chronic hemolytic anemias: a study of 24 observations. Am. J. Hematol. 23:271-275. [DOI] [PubMed] [Google Scholar]
- 180.Reference deleted.
- 181.Lefrere, J. J., and M. Mariotti. 1995. Use of digoxigenin-labelled probes for the detection of B19 parvovirus DNA in batches of blood products. Cell. Mol. Biol. 41:985-988. [PubMed] [Google Scholar]
- 182.Lefrere, J. J., M. Mariotti, I. de la Croix, J. Lerable, M. Thauvin, T. Burnouf, and G. Follea. 1995. Albumin batches and B19 parvovirus DNA. Transfusion 35:389-391. [DOI] [PubMed] [Google Scholar]
- 183.Lefrere, J. J., M. Mariotti, and M. Thauvin. 1994. B19 parvovirus DNA in solvent/detergent-treated anti-haemophilia concentrates. Lancet 343:211-212. [DOI] [PubMed] [Google Scholar]
- 184.Liu, J. M., S. W. Green, T. Shimada, and N. S. Young. 1992. A block in full-length transcript maturation in cells nonpermissive for B19 parvovirus. J. Virol. 66:4686-4692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Reference deleted.
- 186.Luo, W., and C. R. Astell. 1993. A novel protein encoded by small RNAs of parvovirus B19. Virology 195:448-455. [DOI] [PubMed] [Google Scholar]
- 187.Mabin, D. C., and V. Chowdhury. 1990. Aplastic crisis caused by human parvovirus in two patients with hereditary stomatocytosis. Br. J. Haematol. 76:153-154. [DOI] [PubMed] [Google Scholar]
- 188.Magro, C. M., M. R. Dawood, and A. N. Crowson. 2000. The cutaneous manifestations of human parvovirus B19 infection. Hum. Pathol. 31:488-497. [DOI] [PubMed] [Google Scholar]
- 189.Reference deleted.
- 190.Reference deleted.
- 191.Matsumoto, Y., D. Naniwa, S. Banno, and Y. Sugiura. 1998. The efficacy of therapeutic plasmapheresis for the treatment of fatal hemophagocytic syndrome: two case reports. Ther. Apher. 2:300-304. [DOI] [PubMed] [Google Scholar]
- 192.McClain, K., Z. Estrov, H. Chen, and D. H. J. Mahoney. 1993. Chronic neutropenia of childhood: frequent association with parvovirus infection and correlations with bone marrow culture studies. Br. J. Haematol. 85:57-62. [DOI] [PubMed] [Google Scholar]
- 193.McOmish, F., P. L. Yap, A. Jordan, H. Hart, B. J. Cohen, and P. Simmonds. 1993. Detection of parvovirus B19 in donated blood: a model system for screening by polymerase chain reaction. J. Clin. Microbiol. 31:323-328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Mihal, V., J. Dusek, M. Hajduch, B. J. Cohen, H. Fingerova, and J. Vesely. 1996. Transient aplastic crisis in a leukemic child caused by parvovirus B19 infection. Pediatr. Hematol. Oncol. 13:173-177. [DOI] [PubMed] [Google Scholar]
- 195.Miller, E., C. K. Fairley, B. J. Cohen, and C. Seng. 1998. Immediate and long term outcome of human parvovirus B19 infection in pregnancy. Br. J. Obstet. Gynaecol. 105:174-178. [DOI] [PubMed] [Google Scholar]
- 196.Mitchell, L. A., R. Leong, and K. A. Rosenke. 2001. Lymphocyte recognition of human parvovirus B19 nonstructural (NS1) protein: associations with occurrence of acute and chronic arthropathy? J. Med. Microbiol. 50:627-635. [DOI] [PubMed] [Google Scholar]
- 197.Miyagawa, E., T. Yoshida, H. Takahashi, K. Yamaguchi, T. Nagano, Y. Kiriyama, K. Okochi, and H. Sato. 1999. Infection of the erythroid cell line, KU812Ep6 with human parvovirus B19 and its application to titration of B19 infectivity. J. Virol. Methods 83:45-54. [DOI] [PubMed] [Google Scholar]
- 198.Miyamoto, K., M. Ogami, Y. Takahashi, T. Mori, S. Akimoto, H. Terashita, and T. Terashita. 2000. Outbreak of human parvovirus B19 in hospital workers. J. Hosp. Infect. 45:238-241. [DOI] [PubMed] [Google Scholar]
- 199.Miyata, H., K. Yagi, T. Takemura, and S. Maki. 1994. Transient erythroblastopenia due to human parvovirus B19 infection: a case report of a boy suffering from purpura. Acta Paediatr. Jpn. 36:217-219. [DOI] [PubMed] [Google Scholar]
- 200.Moffatt, S., N. Yaegashi, K. Tada, N. Tanaka, and K. Sugamura. 1998. Human parvovirus B19 nonstructural (NS1) protein induces apoptosis in erythroid lineage cells. J. Virol. 72:3018-3028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Momoeda, M., S. Wong, M. Kawase, N. S. Young, and S. Kajigaya. 1994. A putative nucleoside triphosphate-binding domain in the nonstructural protein of B19 parvovirus is required for cytotoxicity. J. Virol. 68:8443-8446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Morey, A. L., J. W. Keeling, H. J. Porter, and K. A. Fleming. 1992. Clinical and histopathological features of parvovirus B19 infection in the human fetus. Br. J. Obstet. Gynaecol. 99:566-574. [DOI] [PubMed] [Google Scholar]
- 203.Morey, A. L., H. J. O'Neill, P. V. Coyle, and K. A. Fleming. 1992. Immunohistological detection of human parvovirus B19 in formalin-fixed, paraffin-embedded tissues. J. Pathol. 166:105-108. [DOI] [PubMed] [Google Scholar]
- 204.Morey, A. L., G. Patou, S. Myint, and K. A. Fleming. 1992. In vitro culture for the detection of infectious human parvovirus B19 and B19-specific antibodies using foetal haematopoietic precursor cells. J. Gen. Virol. 73:3313-3317. [DOI] [PubMed] [Google Scholar]
- 205.Morey, A. L., H. J. Porter, J. W. Keeling, and K. A. Fleming. 1992. Non-isotopic in situ hybridisation and immunophenotyping of infected cells in the investigation of human fetal parvovirus infection. J. Clin. Pathol. 45:673-678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Mori, J., P. Beattie, D. W. Melton, B. J. Cohen, and J. P. Clewley. 1987. Structure and mapping of the DNA of human parvovirus B19. J. Gen. Virol. 68:2797-2806. [DOI] [PubMed] [Google Scholar]
- 207.Mori, J., A. M. Field, J. P. Clewley, and B. J. Cohen. 1989. Dot blot hybridization assay of B19 virus DNA in clinical specimens. J. Clin. Microbiol. 27:459-464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Mortimer, P. P., R. K. Humphries, J. G. Moore, R. H. Purcell, and N. S. Young. 1983. A human parvovirus-like virus inhibits haematopoietic colony formation in vitro. Nature 302:426-429. [DOI] [PubMed] [Google Scholar]
- 209.Moudgil, A., C. C. Nast, A. Bagga, L. Wei, A. Nurmamet, A. H. Cohen, S. C. Jordan, and M. Toyoda. 2001. Association of parvovirus B19 infection with idiopathic collapsing glomerulopathy. Kidney Int. 59:2126-2133. [DOI] [PubMed] [Google Scholar]
- 210.Muir, K., W. T. Todd, W. H. Watson, and E. Fitzsimons. 1992. Viral-associated haemophagocytosis with parvovirus-B19-related pancytopenia. Lancet 339:1139-1140. [DOI] [PubMed] [Google Scholar]
- 211.Reference deleted.
- 212.Munshi, N. C., S. Zhou, M. J. Woody, D. A. Morgan, and A. Srivastava. 1993. Successful replication of parvovirus B19 in the human megakaryocytic leukemia cell line MB-02. J. Virol. 67:562-566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.Murer, L., G. Zacchello, D. Bianchi, R. Dall'Amico, G. Montini, B. Andreetta, M. Perini, E. C. Dossi, G. Zanon, and F. Zacchello. 2000. Thrombotic microangiopathy associated with parvovirus B 19 infection after renal transplantation. J. Am. Soc. Nephrol. 11:1132-1137. [DOI] [PubMed] [Google Scholar]
- 214.Murray, J. C., M. V. Gresik, F. Leger, and K. L. McClain. 1993. B19 parvovirus-induced anemia in a normal child. Initial bone marrow erythroid hyperplasia and response to intravenous immunoglobulin. Am. J. Pediatr. Hematol. Oncol. 15:420-423. [PubMed] [Google Scholar]
- 215.Murray, J. C., P. K. Kelley, W. R. Hogrefe, and K. L. McClain. 1994. Childhood idiopathic thrombocytopenic purpura: association with human parvovirus B19 infection. Am. J. Pediatr. Hematol. Oncol. 16:314-319. [PubMed] [Google Scholar]
- 216.Reference deleted.
- 217.Murry, C. E., K. R. Jerome, and D. D. Reichenbach. 2001. Fatal parvovirus myocarditis in a 5-year-old girl. Hum. Pathol. 32:342-345. [DOI] [PubMed] [Google Scholar]
- 218.Musiani, M., M. Zerbini, G. Gentilomi, M. Plazzi, G. Gallinella, and S. Venturoli. 1995. Parvovirus B19 clearance from peripheral blood after acute infection. J. Infect. Dis. 172:1360-1363. [DOI] [PubMed] [Google Scholar]
- 219.Mylonakis, E., B. P. Dickinson, M. D. Mileno, T. Flanigan, F. J. Schiffman, A. Mega, and J. D. Rich. 1999. Persistent parvovirus B19 related anemia of seven years' duration in an HIV-infected patient: complete remission associated with highly active antiretroviral therapy. Am. J. Hematol. 60:164-166. [DOI] [PubMed] [Google Scholar]
- 220.Nagai, K., T. Morohoshi, T. Kudoh, Y. Yoto, N. Suzuki, and Y. Matsunaga. 1992. Transient erythroblastopenia of childhood with megakaryocytopenia associated with human parvovirus B19 infection. Br. J. Haematol. 80:131-132. [DOI] [PubMed] [Google Scholar]
- 221.Naides, S. J. 1988. Erythema infectiosum (fifth disease) occurrence in Iowa. Am. J. Public Health 78:1230-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Naides, S. J. 1998. Rheumatic manifestations of parvovirus B19 infection. Rheum. Dis. Clin. N. Am. 24:375-401. [DOI] [PubMed] [Google Scholar]
- 223.Naides, S. J. 1999. Infection with parvovirus B19. Curr. Infect. Dis. Rep. 1:273-278. [DOI] [PubMed] [Google Scholar]
- 224.Reference deleted.
- 225.Naides, S. J., L. L. Scharosch, F. Foto, and E. J. Howard. 1990. Rheumatologic manifestations of human parvovirus B19 infection in adults. Initial two-year clinical experience. Arthritis Rheum. 33:1297-1309. [DOI] [PubMed] [Google Scholar]
- 226.Naides, S. J., and C. P. Weiner. 1989. Antenatal diagnosis and palliative treatment of nonimmune hydrops fetalis secondary to fetal parvovirus B19 infection. Prenat. Diagn. 9:105-114. [DOI] [PubMed] [Google Scholar]
- 227.Nakazawa, T., N. Tomosugi, K. Sakamoto, M. Asaka, T. Yuri, I. Ishikawa, and S. Kitagawa. 2000. Acute glomerulonephritis after human parvovirus B19 infection. Am. J. Kidney Dis. 35:E31. [DOI] [PubMed] [Google Scholar]
- 228.Neild, G., M. Anderson, S. Hawes, and B. T. Colvin. 1986. Parvovirus infection after renal transplant. Lancet ii:1226-1227. [DOI] [PubMed] [Google Scholar]
- 229.Nguyen, Q. T., C. Sifer, V. Schneider, X. Allaume, A. Servant, F. Bernaudin, V. Auguste, and A. Garbarg-Chenon. 1999. Novel human erythrovirus associated with transient aplastic anemia. J. Clin. Microbiol. 37:2483-2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 230.Nguyen, Q. T., S. Wong, E. D. Heegaard, and K. E. Brown. Identification and characterization of a second novel erythrovirus, AG. Virology, in press. [DOI] [PubMed]
- 231.Nigro, G., P. D'Eufemia, M. Zerbini, A. Krzysztofiak, R. Finocchiaro, and O. Giardini. 1994. Parvovirus B19 infection in a hypogammaglobulinemic infant with neurologic disorders and anemia: successful immunoglobulin therapy. Pediatr. Infect. Dis. J. 13:1019-1021. [PubMed] [Google Scholar]
- 232.Nigro, G., G. Luzi, E. Fridell, M. Ferrara, P. Pisano, G. C. Gattinara, I. Mezzaroma, M. Soderlund, D. Rasnoveanu, and F. Aiuti. 1992. Parvovirus infection in children with AIDS: high prevalence of B19-specific immunoglobulin M and G antibodies. AIDS 6:679-684. [PubMed] [Google Scholar]
- 233.Nigro, G., M. Zerbini, A. Krzysztofiak, G. Gentilomi, M. A. Porcaro, T. Mango, and M. Musiani. 1994. Active or recent parvovirus B19 infection in children with Kawasaki disease. Lancet 343:1260-1261. [DOI] [PubMed] [Google Scholar]
- 234.Reference deleted.
- 235.Nocton, J. J., L. C. Miller, L. B. Tucker, and J. G. Schaller. 1993. Human parvovirus B19-associated arthritis in children. J. Pediatr. 122:186-190. [DOI] [PubMed] [Google Scholar]
- 236.Notari, E. P., S. L. Orton, R. G. Cable, A. J. Grindon, B. A. Lenes, A. E. Williams, K. M. McMillan, J. J. Trouern-Trend, J. S. Wolf-Nugent, Y. L. Xu, and R. Y. Dodd. 2001. Seroprevalence of known and putative hepatitis markers in United States blood donors with ALT levels at least 120 IU per L. Transfusion 41:751-755. [DOI] [PubMed] [Google Scholar]
- 237.Nour, B., M. Green, M. Michaels, J. Reyes, A. Tzakis, J. C. Gartner, L. McLoughlin, and T. E. Starzl. 1993. Parvovirus B19 infection in pediatric transplant patients. Transplantation 56:835-838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Reference deleted.
- 239.Reference deleted.
- 240.Okumura, A., and T. Ichikawa. 1993. Aseptic meningitis caused by human parvovirus B19. Arch. Dis. Child. 68:784-785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 241.Reference deleted.
- 242.O'Sullivan, M. G., D. C. Anderson, J. D. Fikes, F. T. Bain, C. S. Carlson, S. W. Green, N. S. Young, and K. E. Brown. 1994. Identification of a novel simian parvovirus in cynomolgus monkeys with severe anemia. A paradigm of human B19 parvovirus infection. J. Clin. Investig. 93:1571-1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 243.O'Sullivan, M. G., D. K. Anderson, J. A. Goodrich, H. Tulli, S. W. Green, N. S. Young, and K. E. Brown. 1997. Experimental infection of cynomolgus monkeys with simian parvovirus. J. Virol. 71:4517-4521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 244.O'Sullivan, M. G., D. K. Anderson, J. E. Lund, W. P. Brown, S. W. Green, N. S. Young, and K. E. Brown. 1996. Clinical and epidemiological features of simian parvovirus infection in cynomolgus macaques with severe anemia. Lab. Anim. Sci. 46:291-297. [PubMed] [Google Scholar]
- 245.Owren, P. A. 1948. Congenital hemolytic jaundice: the pathogenesis of the hemolytic crisis. Blood 3:231-248. [PubMed] [Google Scholar]
- 246.Ozawa, K., J. Ayub, Y. S. Hao, G. Kurtzman, T. Shimada, and N. Young. 1987. Novel transcription map for the B19 (human) pathogenic parvovirus. J. Virol. 61:2395-2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 247.Ozawa, K., J. Ayub, S. Kajigaya, T. Shimada, and N. Young. 1988. The gene encoding the nonstructural protein of B19 (human) parvovirus may be lethal in transfected cells. J. Virol. 62:2884-2889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.Ozawa, K., G. Kurtzman, and N. Young. 1986. Replication of the B19 parvovirus in human bone marrow cell cultures. Science 233:883-886. [DOI] [PubMed] [Google Scholar]
- 249.Ozawa, K., G. Kurtzman, and N. Young. 1987. Productive infection by B19 parvovirus of human erythroid bone marrow cells in vitro. Blood 70:384-391. [PubMed] [Google Scholar]
- 250.Ozawa, K., and N. Young. 1987. Characterization of capsid and noncapsid proteins of B19 parvovirus propagated in human erythroid bone marrow cell cultures. J. Virol. 61:2627-2630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 251.Pallier, C., A. Greco, J. Le Junter, A. Saib, I. Vassias, and F. Morinet. 1997. The 3′ untranslated region of the B19 parvovirus capsid protein mRNAs inhibits its own mRNA translation in nonpermissive cells. J. Virol. 71:9482-9489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 252.Pardi, D. S., Y. Romero, L. E. Mertz, and D. D. Douglas. 1998. Hepatitis-associated aplastic anemia and acute parvovirus B19 infection: a report of two cases and a review of the literature. Am. J. Gastroenterol. 93:468-470. [DOI] [PubMed] [Google Scholar]
- 253.Passoni, L. F., S. R. Ribeiro, M. L. Giordani, J. A. Menezes, and J. P. Nascimento. 2001. Papular-purpuric “gloves and socks” syndrome due to parvovirus B19: report of a case with unusual features. Rev. Inst. Med. Trop. Sao Paulo 43:167-170. [DOI] [PubMed] [Google Scholar]
- 254.Patou, G., D. Pillay, S. Myint, and J. Pattison. 1993. Characterization of a nested polymerase chain reaction assay for detection of parvovirus B19. J. Clin. Microbiol. 31:540-546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Reference deleted.
- 256.Reference deleted.
- 257.Petrella, T., F. Bailly, F. Mugneret, D. Caillot, P. Chavanet, H. Guy, E. Solary, A. Waldner, E. Devilliers, and P. M. Carli. 1992. Bone marrow necrosis and human parvovirus associated infection preceding an Ph1+ acute lymphoblastic leukemia. Leuk. Lymphoma 8:415-419. [DOI] [PubMed] [Google Scholar]
- 258.Plummer, F. A., G. W. Hammond, K. Forward, L. Sekla, L. M. Thompson, S. E. Jones, I. M. Kidd, and M. J. Anderson. 1985. An erythema infectiosum-like illness caused by human parvovirus infection. N. Engl. J. Med. 313:74-79. [DOI] [PubMed] [Google Scholar]
- 259.Porter, H. J., A. M. Quantrill, and K. A. Fleming. 1988. B19 parvovirus infection of myocardial cells. Lancet i:535-536. [DOI] [PubMed] [Google Scholar]
- 260.Potter, C. G., A. C. Potter, C. S. Hatton, H. M. Chapel, M. J. Anderson, J. R. Pattison, D. A. Tyrrell, P. G. Higgins, J. S. Willman, and H. F. Parry. 1987. Variation of erythroid and myeloid precursors in the marrow and peripheral blood of volunteer subjects infected with human parvovirus (B19). J. Clin. Investig. 79:1486-1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 261.Public Health Laboratory Service Working Party on Fifth Disease. 1990. Prospective study of human parvovirus (B19) infection in pregnancy. Br. Med. J. 300:1166-1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Ramratnam, B., A. Gollerkeri, F. J. Schiffman, P. Rintels, and T. P. Flanigan. 1995. Management of persistent B19 parvovirus infection in AIDS. Br. J. Haematol. 91:90-92. [DOI] [PubMed] [Google Scholar]
- 263.Rao, S. P., S. T. Miller, and B. J. Cohen. 1990. Severe anemia due to B19 parvovirus infection in children with acute leukemia in remission. Am. J. Pediatr. Hematol. Oncol. 12:194-197. [DOI] [PubMed] [Google Scholar]
- 264.Rao, S. P., S. T. Miller, and B. J. Cohen. 1992. Transient aplastic crisis in patients with sickle cell disease. B19 parvovirus studies during a 7-year period. Am. J. Dis. Child. 146:1328-1330. [DOI] [PubMed] [Google Scholar]
- 265.Ray, N. B., D. R. Nieva, E. A. Seftor, Z. Khalkhali-Ellis, and S. J. Naides. 2001. Induction of an invasive phenotype by human parvovirus B19 in normal human synovial fibroblasts. Arthritis Rheum. 44:1582-1586. [DOI] [PubMed] [Google Scholar]
- 266.Rechavi, G., A. Vonsover, Y. Manor, F. Mileguir, O. Shpilberg, G. Kende, F. Brok-Simoni, M. Mandel, T. Gotlieb-Stematski, and I. Ben-Bassat. 1989. Aplastic crisis due to human B19 parvovirus infection in red cell pyrimidine-5′-nucleotidase deficiency. Acta Haematol. 82:46-49. [DOI] [PubMed] [Google Scholar]
- 267.Reid, D. M., T. M. Reid, T. Brown, J. A. Rennie, and C. J. Eastmond. 1985. Human parvovirus-associated arthritis: a clinical and laboratory description. Lancet i:422-425. [DOI] [PubMed] [Google Scholar]
- 268.Reiner, A. P., and J. L. Spivak. 1988. Hematophagic histiocytosis. A report of 23 new patients and a review of the literature. Medicine 67:369-388. [PubMed] [Google Scholar]
- 269.Risdall, R. J., R. W. McKenna, M. E. Nesbit, W. Krivit, H. H. J. Balfour, R. L. Simmons, and R. D. Brunning. 1979. Virus-associated hemophagocytic syndrome: a benign histiocytic proliferation distinct from malignant histiocytosis. Cancer 44:993-1002. [DOI] [PubMed] [Google Scholar]
- 270.Rodis, J. F., A. F. Borgida, M. Wilson, J. F. Egan, M. V. Leo, A. O. Odibo, and W. A. Campbell. 1998. Management of parvovirus infection in pregnancy and outcomes of hydrops: a survey of members of the Society of Perinatal Obstetricians. Am. J. Obstet. Gynecol. 179:985-988. [DOI] [PubMed] [Google Scholar]
- 271.Rogers, B. B., Z. R. Rogers, and C. F. Timmons. 1996. Polymerase chain reaction amplification of archival material for parvovirus B19 in children with transient erythroblastopenia of childhood. Pediatr. Pathol. Lab. Med. 16:471-478. [DOI] [PubMed] [Google Scholar]
- 272.Rollag, H., G. Patou, J. R. Pattison, M. Degre, S. A. Evensen, S. S. Froland, and A. Glomstein. 1991. Prevalence of antibodies against parvovirus B19 in Norwegians with congenital coagulation factor defects treated with plasma products from small donor pools. Scand. J. Infect. Dis. 23:675-679. [DOI] [PubMed] [Google Scholar]
- 273.Rollag, H., B. G. Solheim, and J. L. Svennevig. 1998. Viral safety of blood derivatives by immune neutralization. Vox Sang. 74(Suppl. 1):213-217. [DOI] [PubMed] [Google Scholar]
- 274.Rosenfeld, S. J., K. Yoshimoto, S. Kajigaya, S. Anderson, N. S. Young, A. Field, P. Warrener, G. Bansal, and M. S. Collett. 1992. Unique region of the minor capsid protein of human parvovirus B19 is exposed on the virion surface. J. Clin. Investig. 89:2023-2029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 275.Rosenfeld, S. J., N. S. Young, D. Alling, J. Ayub, and C. Saxinger. 1994. Subunit interaction in B19 parvovirus empty capsids. Arch. Virol. 136:9-18. [DOI] [PubMed] [Google Scholar]
- 276.Rouger, P., P. Gane, and C. Salmon. 1987. Tissue distribution of H, Lewis and P antigens as shown by a panel of 18 monoclonal antibodies. Rev. Fr. Transfus. Immunohematol. 30:699-708. [DOI] [PubMed] [Google Scholar]
- 277.Rugolotto, S., E. M. Padovani, A. Sanna, G. P. Chiaffoni, P. L. Marradi, and C. Borgna-Pignatti. 1999. Intrauterine anemia due to parvovirus B19: successful treatment with intravenous immunoglobulins. Haematologica 84:668-669. [PubMed] [Google Scholar]
- 278.Saal, J. G., M. Steidle, H. Einsele, C. A. Muller, P. Fritz, and J. Zacher. 1992. Persistence of B19 parvovirus in synovial membranes of patients with rheumatoid arthritis. Rheumatol. Int. 12:147-151. [DOI] [PubMed] [Google Scholar]
- 279.Saarinen, U. M., T. L. Chorba, P. Tattersall, N. S. Young, L. J. Anderson, E. Palmer, and P. F. Coccia. 1986. Human parvovirus B19-induced epidemic acute red cell aplasia in patients with hereditary hemolytic anemia. Blood 67:1411-1417. [PubMed] [Google Scholar]
- 280.Sadahira, Y., S. Yoshimoto, and T. Manabe. 1998. Parvovirus B19-associated transient pure red cell aplasia with lymphadenopathy: a case report. Pathol. Int. 48:829-833. [DOI] [PubMed] [Google Scholar]
- 281.Safadi, R., R. Or, Y. Ilan, E. Naparstek, A. Nagler, A. Klein, M. Ketzinel-Gilaad, K. Ergunay, D. Danon, D. Shouval, and E. Galun. 2001. Lack of known hepatitis virus in hepatitis-associated aplastic anemia and outcome after bone marrow transplantation. Bone Marrow Transplant. 27:183-190. [DOI] [PubMed] [Google Scholar]
- 282.Saikawa, T., S. Anderson, M. Momoeda, S. Kajigaya, and N. S. Young. 1993. Neutralizing linear epitopes of B19 parvovirus cluster in the VP1 unique and VP1-VP2 junction regions. J. Virol. 67:3004-3009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 283.Reference deleted.
- 284.Saldanha, J., and P. Minor. 1996. Detection of human parvovirus B19 DNA in plasma pools and blood products derived from these pools: implications for efficiency and consistency of removal of B19 DNA during manufacture. Br. J. Haematol. 93:714-719. [DOI] [PubMed] [Google Scholar]
- 285.Salimans, M. M., M. J. van Bussel, C. S. Brown, and W. J. Spaan. 1992. Recombinant parvovirus B19 capsids as a new substrate for detection of B19-specific IgG and IgM antibodies by an enzyme-linked immunosorbent assay. J. Virol. Methods 39:247-258. [DOI] [PubMed] [Google Scholar]
- 286.Sano, F., M. Takahashi, Y. Shibuya, T. Kanamori, D. Miyamoto, S. Hasegawa, M. Koike, and H. Ishida. 1999. Case of hereditary spherocytosis complicated by human parvovirus B19-associated hemophagocytosis syndrome and aplastic crisis. Nippon Naika Gakkai Zasshi 88:127-129. (In Japanese.) [PubMed] [Google Scholar]
- 287.Sato, H., J. Hirata, M. Furukawa, N. Kuroda, H. Shiraki, Y. Maeda, and K. Okochi. 1991. Identification of the region including the epitope for a monoclonal antibody which can neutralize human parvovirus B19. J. Virol. 65:1667-1672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 288.Sato, H., J. Hirata, N. Kuroda, H. Shiraki, Y. Maeda, and K. Okochi. 1991. Identification and mapping of neutralizing epitopes of human parvovirus B19 by using human antibodies. J. Virol. 65:5485-5490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 289.Sato, T., D. Ueda, S. Sakota, K. Haseyama, S. Chiba, and T. Kudoh. 1999. Pancytopenia with hemophagocytosis secondary to parvovirus B19 infection in a family with hereditary spherocytosis. Pediatr. Int. 41:561-564. [DOI] [PubMed] [Google Scholar]
- 290.Scapellato, P. G., A. M. Palumbo, and S. Del Valle. 2000. Improvement of anemia induced by parvovirus B19 in a patient with AIDS after combined antiretroviral therapy. Mayo Clin. Proc. 75:215-216. [PubMed] [Google Scholar]
- 291.Scheurlen, W., K. Ramasubbu, O. Wachowski, A. Hemauer, and S. Modrow. 2001. Chronic autoimmune thrombopenia/neutropenia in a boy with persistent parvovirus B19 infection. J. Clin. Virol. 20:173-178. [DOI] [PubMed] [Google Scholar]
- 292.Schild, R. L., R. Bald, H. Plath, A. M. Eis-Hubinger, G. Enders, and M. Hansmann. 1999. Intrauterine management of fetal parvovirus B19 infection. Ultrasound Obstet. Gynecol. 13:161-166. [DOI] [PubMed] [Google Scholar]
- 293.Schowengerdt, K. O., J. Ni, S. W. Denfield, R. J. Gajarski, N. E. Bowles, G. Rosenthal, D. L. Kearney, J. K. Price, B. B. Rogers, G. M. Schauer, R. E. Chinnock, and J. A. Towbin. 1997. Association of parvovirus B19 genome in children with myocarditis and cardiac allograft rejection: diagnosis using the polymerase chain reaction. Circulation 96:3549-3554. [DOI] [PubMed] [Google Scholar]
- 294.Schowengerdt, K. O., J. Ni, S. W. Denfield, R. J. Gajarski, B. Radovancevic, H. O. Frazier, G. J. Demmler, D. Kearney, J. T. Bricker, and J. A. Towbin. 1996. Diagnosis, surveillance, and epidemiologic evaluation of viral infections in pediatric cardiac transplant recipients with the use of the polymerase chain reaction. J. Heart Lung Transplant. 15:111-123. [PubMed] [Google Scholar]
- 295.Schwarz, T. F., G. Jager, and S. Gilch. 1997. Comparison of seven commercial tests for the detection of parvovirus B19-specific IgM. Zentbl. Bakteriol. 285:525-530. [DOI] [PubMed] [Google Scholar]
- 296.Schwarz, T. F., A. Nerlich, and M. Roggendorf. 1990. Parvovirus B19 infection in pregnancy. Behring Inst. Mitt. 1990:69-73. [PubMed] [Google Scholar]
- 297.Schwarz, T. F., S. Serke, B. Hottentrager, A. von Brunn, H. Baurmann, A. Kirsch, W. Stolz, D. Huhn, F. Deinhardt, and M. Roggendorf. 1992. Replication of parvovirus B19 in hematopoietic progenitor cells generated in vitro from normal human peripheral blood. J. Virol. 66:1273-1276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 298.Schwarz, T. F., S. Serke, A. von Brunn, B. Hottentrager, D. Huhn, F. Deinhardt, and M. Roggendorf. 1992. Heat stability of parvovirus B19: kinetics of inactivation. Zentbl. Bakteriol. 277:219-223. [DOI] [PubMed] [Google Scholar]
- 299.Searle, K., C. Guilliard, S. Wallat, G. Schalasta, and G. Enders. 1998. Acute parvovirus B19 infection in pregnant women--an analysis of serial samples by serological and semi-quantitative PCR techniques. Infection 26:139-143. [DOI] [PubMed] [Google Scholar]
- 300.Searle, K., G. Schalasta, and G. Enders. 1998. Development of antibodies to the nonstructural protein NS1 of parvovirus B19 during acute symptomatic and subclinical infection in pregnancy: implications for pathogenesis doubtful. J. Med. Virol. 56:192-198. [DOI] [PubMed] [Google Scholar]
- 301.Serjeant, G. R., J. M. Topley, K. Mason, B. E. Serjeant, J. R. Pattison, S. E. Jones, and R. Mohamed. 1981. Outbreak of aplastic crises in sickle cell anaemia associated with parvovirus-like agent. Lancet ii:595-597. [DOI] [PubMed] [Google Scholar]
- 302.Serke, S., T. F. Schwarz, H. Baurmann, A. Kirsch, B. Hottentrager, A. von Brunn, M. Roggendorf, D. Huhn, and F. Deinhardt. 1991. Productive infection of in vitro generated haemopoietic progenitor cells from normal human adult peripheral blood with parvovirus B19: studies by morphology, immunocytochemistry, flow-cytometry and DNA-hybridization. Br. J. Haematol. 79:6-13. [DOI] [PubMed] [Google Scholar]
- 303.Shade, R. O., M. C. Blundell, S. F. Cotmore, P. Tattersall, and C. R. Astell. 1986. Nucleotide sequence and genome organization of human parvovirus B19 isolated from the serum of a child during aplastic crisis. J. Virol. 58:921-936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 304.Sheikh, A. U., J. M. Ernest, and M. O'Shea. 1992. Long-term outcome in fetal hydrops from parvovirus B19 infection. Am. J. Obstet. Gynecol. 167:337-341. [DOI] [PubMed] [Google Scholar]
- 305.Shimomura, S., N. Komatsu, N. Frickhofen, S. Anderson, S. Kajigaya, and N. S. Young. 1992. First continuous propagation of B19 parvovirus in a cell line. Blood 79:18-24. [PubMed] [Google Scholar]
- 306.Shiraishi, H., T. Sasaki, M. Nakamura, N. Yaegashi, and K. Sugamura. 1991. Laboratory infection with human parvovirus B19. J. Infect. 22:308-310. [DOI] [PubMed] [Google Scholar]
- 307.Shiraishi, H., K. Umetsu, H. Yamamoto, Y. Hatakeyama, N. Yaegashi, and K. Sugamura. 1989. Human parvovirus (HPV/B19) infection with purpura. Microbiol. Immunol. 33:369-372. [DOI] [PubMed] [Google Scholar]
- 308.Shirono, K., and H. Tsuda. 1995. Parvovirus B19-associated haemophagocytic syndrome in healthy adults. Br. J. Haematol. 89:923-926. [DOI] [PubMed] [Google Scholar]
- 309.Shneerson, J. M., P. P. Mortimer, and E. M. Vandervelde. 1980. Febrile illness due to a parvovirus. Br. Med. J. 280:1580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 310.Siegl, G., R. C. Bates, K. I. Berns, B. J. Carter, D. C. Kelly, E. Kurstak, and P. Tattersall. 1985. Characteristics and taxonomy of Parvoviridae. Intervirology 23:61-73. [DOI] [PubMed] [Google Scholar]
- 311.Siegl, G., and P. Cassinotti. 1998. Presence and significance of parvovirus B19 in blood and blood products. Biologicals 26:89-94. [DOI] [PubMed] [Google Scholar]
- 312.Sinclair, J. P., M. C. Croxson, S. M. Thomas, L. R. Teague, and D. C. Mauger. 1999. Chronic parvovirus B19 meningitis in a child with acute lymphocytic leukemia. Pediatr. Infect. Dis. J. 18:395-396. [DOI] [PubMed] [Google Scholar]
- 313.Sitar, G., C. L. Balduini, L. Manenti, A. Castello, D. Balanzin, and E. Ascari. 1999. Possible evolution of human parvovirus B19 infection into erythroleukemia. Haematologica 84:957-959. [PubMed] [Google Scholar]
- 314.Skjoldebrand-Sparre, L., T. Tolfvenstam, N. Papadogiannakis, B. Wahren, K. Broliden, and M. Nyman. 2000. Parvovirus B19 infection: association with third-trimester intrauterine fetal death. Br. J. Obstet. Gynaecol. 107:476-480. [DOI] [PubMed] [Google Scholar]
- 315.Smith, M. A., N. R. Shah, J. S. Lobel, P. J. Cera, G. W. Gary, and L. J. Anderson. 1988. Severe anemia caused by human parvovirus in a leukemia patient on maintenance chemotherapy. Clin. Pediatr. (Philadelphia) 27:383-386. [DOI] [PubMed] [Google Scholar]
- 316.Reference deleted.
- 317.Smoleniec, J. S., and M. Pillai. 1994. Management of fetal hydrops associated with parvovirus B19 infection. Br. J. Obstet. Gynaecol. 101:1079-1081. [DOI] [PubMed] [Google Scholar]
- 318.Soderlund, M., C. S. Brown, B. J. Cohen, and K. Hedman. 1995. Accurate serodiagnosis of B19 parvovirus infections by measurement of IgG avidity. J. Infect. Dis. 171:710-713. [DOI] [PubMed] [Google Scholar]
- 319.Soderlund, M., R. von Essen, J. Haapasaari, U. Kiistala, O. Kiviluoto, and K. Hedman. 1997. Persistence of parvovirus B19 DNA in synovial membranes of young patients with and without chronic arthropathy. Lancet 349:1063-1065. [DOI] [PubMed] [Google Scholar]
- 320.Sokal, E. M., M. Melchior, C. Cornu, A. T. Vandenbroucke, J. P. Buts, B. J. Cohen, and G. Burtonboy. 1998. Acute parvovirus B19 infection associated with fulminant hepatitis of favourable prognosis in young children. Lancet 352:1739-1741. [DOI] [PubMed] [Google Scholar]
- 321.Solheim, B. G., H. Rollag, J. L. Svennevig, O. Arafa, E. Fosse, and U. Bergerud. 2000. Viral safety of solvent/detergent-treated plasma. Transfusion 40:84-90. [DOI] [PubMed] [Google Scholar]
- 322.Sosa, C. E., J. B. Mahony, K. E. Luinstra, M. Sternbach, and M. A. Chernesky. 1992. Replication and cytopathology of human parvovirus B19 in human umbilical cord blood erythroid progenitor cells. J. Med. Virol. 36:125-130. [DOI] [PubMed] [Google Scholar]
- 323.Speyer, I., F. C. Breedveld, and B. A. Dijkmans. 1998. Human parvovirus B19 infection is not followed by inflammatory joint disease during long term follow-up. A retrospective study of 54 patients. Clin. Exp. Rheumatol. 16:576-578. [PubMed] [Google Scholar]
- 324.Srivastava, A., E. Bruno, R. Briddell, R. Cooper, C. Srivastava, K. van Besien, and R. Hoffman. 1990. Parvovirus B19-induced perturbation of human megakaryocytopoiesis in vitro. Blood 76:1997-2004. [PubMed] [Google Scholar]
- 325.Srivastava, A., and L. Lu. 1988. Replication of B19 parvovirus in highly enriched hematopoietic progenitor cells from normal human bone marrow. J. Virol. 62:3059-3063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 326.Srivastava, C. H., S. Zhou, N. C. Munshi, and A. Srivastava. 1992. Parvovirus B19 replication in human umbilical cord blood cells. Virology 189:456-461. [DOI] [PubMed] [Google Scholar]
- 327.St Amand, J., and C. R. Astell. 1993. Identification and characterization of a family of 11-kDa proteins encoded by the human parvovirus B19. Virology 192:121-131. [DOI] [PubMed] [Google Scholar]
- 328.St Amand, J., C. Beard, K. Humphries, and C. R. Astell. 1991. Analysis of splice junctions and in vitro and in vivo translation potential of the small, abundant B19 parvovirus RNAs. Virology 183:133-142. [DOI] [PubMed] [Google Scholar]
- 329.Summers, J., S. E. Jones, and M. J. Anderson. 1983. Characterization of the genome of the agent of erythrocyte aplasia permits its classification as a human parvovirus. J. Gen. Virol. 64:2527-2532. [DOI] [PubMed] [Google Scholar]
- 330.Taillan, B., P. Heudier, E. Ferrari, G. Garnier, J. G. Fuzibet, and P. Dujardin. 1992. Pure red-cell aplasia due to parvovirus B19 infection in a patient with AIDS-related complex. Ann. Med. 24:137. [DOI] [PubMed] [Google Scholar]
- 331.Reference deleted.
- 332.Takahashi, T., K. Ozawa, K. Takahashi, S. Asano, and F. Takaku. 1990. Susceptibility of human erythropoietic cells to B19 parvovirus in vitro increases with differentiation. Blood 75:603-610. [PubMed] [Google Scholar]
- 333.Takahashi, T., K. Ozawa, K. Takahashi, Y. Okuno, Y. Muto, F. Takaku, and S. Asano. 1993. DNA replication of parvovirus B 19 in a human erythroid leukemia cell line (JK-1) in vitro. Arch. Virol. 131:201-208. [DOI] [PubMed] [Google Scholar]
- 334.Takahashi, Y., C. Murai, S. Shibata, Y. Munakata, T. Ishii, K. Ishii, T. Saitoh, T. Sawai, K. Sugamura, and T. Sasaki. 1998. Human parvovirus B19 as a causative agent for rheumatoid arthritis. Proc. Natl. Acad. Sci. USA 95:8227-8232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 335.Tiessen, R. G., A. M. van Elsacker-Niele, C. Vermeij-Keers, D. Oepkes, J. van Roosmalen, and M. C. Gorsira. 1994. A fetus with a parvovirus B19 infection and congenital anomalies. Prenat. Diagn. 14:173-176. [DOI] [PubMed] [Google Scholar]
- 336.Reference deleted.
- 337.Tsuda, H., Y. Maeda, K. Nakagawa, M. Nakayama, H. Nishimura, A. Ishihara, and H. Miyayama. 1994. Parvovirus B19-associated haemophagocytic syndrome with prominent neutrophilia. Br. J. Haematol. 86:413-414. [DOI] [PubMed] [Google Scholar]
- 338.Reference deleted.
- 339.Tsujimura, M., K. Matsushita, H. Shiraki, H. Sato, K. Okochi, and Y. Maeda. 1995. Human parvovirus B19 infection in blood donors. Vox Sang. 69:206-212. [DOI] [PubMed] [Google Scholar]
- 340.Uike, N., T. Miyamura, K. Obama, H. Takahira, H. Sato, and M. Kozuru. 1993. Parvovirus B19-associated haemophagocytosis in Evans syndrome: aplastic crisis accompanied by severe thrombocytopenia. Br. J. Haematol. 84:530-532. [DOI] [PubMed] [Google Scholar]
- 341.Umene, K., and T. Nunoue. 1990. The genome type of human parvovirus B19 strains isolated in Japan during 1981 differs from types detected in 1986 to 1987: a correlation between genome type and prevalence. J. Gen. Virol. 71:983-986. [DOI] [PubMed] [Google Scholar]
- 342.Umene, K., and T. Nunoue. 1991. Genetic diversity of human parvovirus B19 determined using a set of restriction endonucleases recognizing four or five base pairs and partial nucleotide sequencing: use of sequence variability in virus classification. J. Gen. Virol. 72:1997-2001. [DOI] [PubMed] [Google Scholar]
- 343.van de Vusse, A. C., V. J. Goossens, M. A. Kemler, and W. E. Weber. 2001. Screening of patients with complex regional pain syndrome for antecedent infections. Clin. J. Pain 17:110-114. [DOI] [PubMed] [Google Scholar]
- 344.Van Horn, D. K., P. P. Mortimer, N. Young, and G. R. Hanson. 1986. Human parvovirus-associated red cell aplasia in the absence of underlying hemolytic anemia. Am. J. Pediatr. Hematol. Oncol. 8:235-239. [DOI] [PubMed] [Google Scholar]
- 345.Venturoli, S., G. Gallinella, E. Manaresi, G. Gentilomi, M. Musiani, and M. Zerbini. 1998. IgG response to the immunoreactive region of parvovirus B19 nonstructural protein by immunoblot assay with a recombinant antigen. J. Infect. Dis 178:1826-1829. [DOI] [PubMed] [Google Scholar]
- 346.Reference deleted.
- 347.von dem, B., M. J. Bos, N. Joustra-Maas, J. F. Tromp, M. B. van't Veer, B. van Wijngaarden-du, and P. A. Tetteroo. 1986. A murine monoclonal IgM antibody specific for blood group P antigen (globoside). Br. J. Haematol. 63:35-46. [DOI] [PubMed] [Google Scholar]
- 348.von Poblotzki, A., C. Gerdes, U. Reischl, H. Wolf, and S. Modrow. 1996. Lymphoproliferative responses after infection with human parvovirus B19. J. Virol. 70:7327-7330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 349.von Poblotzki, A., A. Gigler, B. Lang, H. Wolf, and S. Modrow. 1995. Antibodies to parvovirus B19 NS-1 protein in infected individuals. J. Gen. Virol. 76:519-527. [DOI] [PubMed] [Google Scholar]
- 350.von Poblotzki, A., A. Hemauer, A. Gigler, E. Puchhammer-Stockl, F. X. Heinz, J. Pont, K. Laczika, H. Wolf, and S. Modrow. 1995. Antibodies to the nonstructural protein of parvovirus B19 in persistently infected patients: implications for pathogenesis. J. Infect. Dis. 172:1356-1359. [DOI] [PubMed] [Google Scholar]
- 351.Wakamatsu, C., F. Takakura, E. Kojima, Y. Kiriyama, N. Goto, K. Matsumoto, M. Oyama, H. Sato, K. Okochi, and Y. Maeda. 1999. Screening of blood donors for human parvovirus B19 and characterization of the results. Vox Sang. 76:14-21. [DOI] [PubMed] [Google Scholar]
- 352.Wakamoto, H., and M. Miyazaki. 1996. Leukophagocytosis in human parvovirus B19-induced transient bicytopenia in a healthy child. Acta Paediatr. Jpn. 38:278-281. [DOI] [PubMed] [Google Scholar]
- 353.Walsh, K. J., R. D. Armstrong, and A. M. Turner. 1988. Brachial plexus neuropathy associated with human parvovirus infection. Br. Med. J. (Clin. Res. Ed.) 296:896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 354.Warsof, S. L., K. H. Nicolaides, and C. Rodeck. 1986. Immune and non-immune hydrops. Clin. Obstet. Gynecol. 29:533-542. [DOI] [PubMed] [Google Scholar]
- 355.Reference deleted.
- 356.Weigel-Kelley, K. A., M. C. Yoder, and A. Srivastava. 2001. Recombinant human parvovirus B19 vectors: erythrocyte P antigen is necessary but not sufficient for successful transduction of human hematopoietic cells. J. Virol. 75:4110-4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 357.Reference deleted.
- 358.Reference deleted.
- 359.West, N. C., R. E. Meigh, M. Mackie, and M. J. Anderson. 1986. Parvovirus infection associated with aplastic crisis in a patient with HEMPAS. J. Clin. Pathol. 39:1019-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 360.White, D. G., A. D. Woolf, P. P. Mortimer, B. J. Cohen, D. R. Blake, and P. A. Bacon. 1985. Human parvovirus arthropathy. Lancet i:419-421. [DOI] [PubMed] [Google Scholar]
- 361.Wilson, G. M., H. K. Jindal, D. E. Yeung, W. Chen, and C. R. Astell. 1991. Expression of minute virus of mice major nonstructural protein in insect cells: purification and identification of ATPase and helicase activities. Virology 185:90-98. [DOI] [PubMed] [Google Scholar]
- 362.Wodzinski, M. A., and J. S. Lilleyman. 1989. Transient erythroblastopenia of childhood due to human parvovirus B19 infection. Br. J. Haematol. 73:127-128. [DOI] [PubMed] [Google Scholar]
- 363.Woolf, A. D. 1990. Human parvovirus B19 and arthritis. Behring Inst. Mitt. 1990:64-68. [PubMed] [Google Scholar]
- 364.Woolf, A. D., G. V. Campion, A. Chishick, S. Wise, B. J. Cohen, P. T. Klouda, O. Caul, and P. A. Dieppe. 1989. Clinical manifestations of human parvovirus B19 in adults. Arch. Intern. Med. 149:1153-1156. [PubMed] [Google Scholar]
- 365.Wright, C., S. A. Hinchliffe, and C. Taylor. 1996. Fetal pathology in intrauterine death due to parvovirus B19 infection. Br. J. Obstet. Gynaecol. 103:133-136. [DOI] [PubMed] [Google Scholar]
- 366.Yaegashi, N., T. Niinuma, H. Chisaka, S. Uehara, K. Okamura, O. Shinkawa, A. Tsunoda, S. Moffatt, K. Sugamura, and A. Yajima. 1999. Serologic study of human parvovirus B19 infection in pregnancy in Japan. J. Infect. 38:30-35. [DOI] [PubMed] [Google Scholar]
- 367.Yaegashi, N., T. Niinuma, H. Chisaka, T. Watanabe, S. Uehara, K. Okamura, S. Moffatt, K. Sugamura, and A. Yajima. 1998. The incidence of, and factors leading to, parvovirus B19-related hydrops fetalis following maternal infection; report of 10 cases and meta-analysis. J. Infect. 37:28-35. [DOI] [PubMed] [Google Scholar]
- 368.Yaegashi, N., H. Shiraishi, T. Takeshita, M. Nakamura, A. Yajima, and K. Sugamura. 1989. Propagation of human parvovirus B19 in primary culture of erythroid lineage cells derived from fetal liver. J. Virol. 63:2422-2426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 369.Yee, T. T., B. J. Cohen, K. J. Pasi, and C. A. Lee. 1996. Transmission of symptomatic parvovirus B19 infection by clotting factor concentrate. Br. J. Haematol. 93:457-459. [DOI] [PubMed] [Google Scholar]
- 370.Yoshida, M., and T. Tezuka. 1994. Conjunctivitis caused by human parvovirus B19 infection. Ophthalmologica 208:161-162. [DOI] [PubMed] [Google Scholar]
- 371.Yoshimoto, K., S. Rosenfeld, N. Frickhofen, D. Kennedy, R. Hills, S. Kajigaya, and N. S. Young. 1991. A second neutralizing epitope of B19 parvovirus implicates the spike region in the immune response. J. Virol. 65:7056-7060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 372.Reference deleted.
- 373.Yoto, Y., T. Kudoh, K. Haseyama, N. Suzuki, and S. Chiba. 1996. Human parvovirus B19 infection associated with acute hepatitis. Lancet 347:868-869. [DOI] [PubMed] [Google Scholar]
- 374.Reference deleted.
- 375.Yoto, Y., T. Kudoh, K. Haseyama, N. Suzuki, T. Oda, T. Katoh, T. Takahashi, S. Sekiguchi, and S. Chiba. 1995. Incidence of human parvovirus B19 DNA detection in blood donors. Br. J. Haematol. 91:1017-1018. [DOI] [PubMed] [Google Scholar]
- 376.Yoto, Y., T. Kudoh, N. Suzuki, S. Katoh, Y. Matsunaga, and S. Chiba. 1993. Thrombocytopenia induced by human parvovirus B19 infections. Eur. J. Haematol. 50:255-257. [DOI] [PubMed] [Google Scholar]
- 377.Young, N., and B. P. Alter. 1993. Aplastic anemia acquired and inherited, p. 384-390. W. B. Saunders Company, Philadelphia, Pa.
- 378.Young, N., M. Harrison, J. Moore, P. Mortimer, and R. K. Humphries. 1984. Direct demonstration of the human parvovirus in erythroid progenitor cells infected in vitro. J. Clin. Investig. 74:2024-2032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 379.Young, N. S. 1995. B19 parvovirus. Baillieres Clin. Haematol. 8:25-56. [DOI] [PubMed] [Google Scholar]
- 380.Zerbini, M., M. Musiani, S. Venturoli, G. Gallinella, D. Gibellini, G. Gentilomi, and M. La Placa. 1992. Different syndromes associated with B19 parvovirus viraemia in paediatric patients: report of four cases. Eur. J. Pediatr. 151:815-817. [DOI] [PubMed] [Google Scholar]