Summary
Background
Myopia rates have risen in the past decades in China. New strategies for the prevention and control of myopia are now available, and understanding the prevalence and future trends in myopia and high myopia in children and adolescents in China may provide insights into the impact of implementing these measures. The study aims to provide updated data on the prevalence of myopia and high myopia in children and to project temporal trends in prevalence from 2020 to 2050 in China.
Methods
A systematic review and meta-analysis searching several databases in both English and Chinese: PubMed, Web of Science, Science Direct, China National Knowledge Infrastructure (CNKI), Wanfang, China Science and Technology Journal Database (CSTJ) with date limits from 01/01/2010 to 11/23/2024 was conducted. We included population-based or school-based studies in China that determined the myopia prevalence, based on the cycloplegic refraction, in children under 20. Studies with a response rate <70% or sample size <200 were excluded. A fixed-effect meta-analysis was used, and projections were made based on three scenarios: experience-based, maximum growth (maximum near-work, minimal outdoor time), and minimum growth (2 h outdoor time daily).
Findings
From 6555 reports, 82 studies with 218,794 participants were included. The overall myopia prevalence was 36.6% (95% CI: 36.4%, 36.8%), with rates of 2.6% in ages 0–4, 22.0% in ages 5–9, 45.4% in ages 10–14, and 67.2% in ages 15–19. High myopia prevalence was 5.3% overall, with rates of 0.1% in ages 0–4, 1.1% in ages 5–9, 3.0% in ages 10–14, and 9.5% in ages 15–19. Projections for 2030 under minimum growth, experience-based, and maximum growth scenarios were 26.8%, 46.2%, 56.0%; 2040 were 19.6%, 54.4%, 65.6%; and 2050 were 14.4%, 61.3%, 71.9%, respectively.
Interpretation
China is facing a substantial and potentially worsening epidemic of childhood myopia. This information will provide data for guiding implementation and evaluating the effectiveness of existing and new nationwide myopia prevention and control programs.
Funding
The Science and Technology Innovation Program of Hunan Province, China (2023RC1079, 2024RC5002).
Keywords: Myopia, Childhood, China, Trend, Outdoor, Near work, Prediction, Review
Research in context.
Evidence before this study
Accurate data, based on the gold standard of cycloplegic refraction, on the prevalence of myopia and high myopia in Chinese children and adolescents is limited. There have been two meta-analysis studies of the prevalence of myopia and high myopia in Chinese children, with different time ranges (1998–2016, 1983–2017), which may be somewhat out-dated. Both of the previous meta-analyses included studies that used non-cycloplegic measurements, which are known to overestimate myopia prevalence. A highly cited paper by Holden et al. projected global myopia prevalence trend from 2010 to 2050, however the paper's methodology and accuracy are questionable, in part due to the same concerns. This study reviewed six databases (PubMed, Web of Science, Science Direct, CNKI, Wanfang, VIP) from 01/01/2010 to 11/23/2024.
Added value of this study
This study provides up-to-date data on the prevalence of myopia and high myopia in Chinese children and adolescents based on cycloplegic refraction. It further projects future prevalence trends up to 2050, from empirically determined local trends, and from maximum and minimum growth scenarios based on observational data.
Implications of all the available evidence
There is an epidemic of childhood myopia in China, other parts of East Asia and Singapore. Our projections derived from Chinese data provide critical information and significant implications for setting goals, implementing and evaluating the effectiveness of existing and new nation-wide myopia prevention and control programs for Chinese authorities and others countries faced with a myopia epidemic.
Introduction
Myopia is a major public health problem, requiring timely correction to maintain good distance visual acuity and effective intervention to avoid the development of high myopia, and preventive interventions and effective interventions if possible.1,2 Myopia with any severity, especially high myopia, is a significant cause of visual impairment and blindness, and is associated with various vision-threatening conditions.3, 4, 5 In the meta-analysis by Holden et al., it is predicted that about 50% of the world's population will be myopic and 10% highly myopic by 2050,6 making myopia a global health epidemic. Independent of these general predictions, myopia is a clearly a major problem in China.7, 8, 9 The economic burden associated with myopia in the whole country was estimated as 1.3% of total GDP in China 2015.10
The projections by Holden et al., specifically forecast the overall population prevalence of myopia, covering both children and adults, in the East Asia region would reach 51.6% in 2020, 56.9% in 2030, 61.4% in 2040, and 65.3% by 2050.6 However, this estimation may not accurately reflect the prevalence of and temporal trends in childhood myopia in China by 2050. Firstly, the predictive model applied was based on six longitudinal studies from different countries and continents, which had different baseline prevalences and change in the rate of prevalence from each other. Secondly, even though the study divided age into 5-year groups, the projections were focused on the prevalence of myopia and high myopia in the whole population, and the age-group-specific prevalence was only reported in the meta-analysis results for 2010. Thirdly, the data used for meta-analysis was often quite out-of-date, from 1995 to 2015, included data obtained without cycloplegia, and included data on older adults, where myopia is often associated with the development of cataract, rather than with schooling. Thus, a contemporary meta-analysis with temporal trends devoted specifically to childhood myopia in China is needed.
The re-assessment is of extra importance for China. First, since 2010 a marked increase in near-work activities coincided with the introduction of smartphones and other digital devices in China (for example, the iPhone 3G in 2008 was released in 2008, and the iPad in 2010). A 2019 survey conducted by China Youth Daily revealed that nearly 93% of 1939 parents provided smartphones for daily use to their primary and middle school-aged children for daily use.11 The extended use of these digital devices, often up to 8 h a day, has been described as a new type of near-work activity.12, 13, 14 Second, a variety of new intervention strategies to control progression and potentially prevent the development of myopia have been introduced and applied in China recently,1 and accurate estimation and future projection of myopia and high myopia prevalence is therefore especially valuable.
To the best of our knowledge, there are two review articles that conducted meta-analyses on childhood myopia in China.15,16 However, these reviews included studies that did not use cycloplegia, leading to an overestimation of the prevalence of myopia. There was also one report that predicted the trend in myopia children from 2010 to 2050. But, again, the data used included studies that were based on non-cycloplegic refractive error.17 To establish an up-to-dated and more accurate baseline data on prevalence of myopia and high myopia in Chinese children and adolescents, the present study was conducted using only the gold standard measures of myopia based on cycloplegic refraction. In addition, the study aimed to provide forecasts of future trends of myopia prevalence up to 2050 based on different hypotheses, varying from empirically determined local trends to maximum and minimum growth scenarios based on observational data.
Methods
The analysis in this study comprises two main components: Firstly, a systematic review followed by a meta-analysis; secondly, a projection of the prevalence of myopia and high myopia from 2020 to 2050. The methodology for the two parts aligns with the approach used by Holden et al.,6 in that it applies a predictive model based on the existing prevalence of myopia. Since the education system and cultural attitudes can significantly affect the development of myopia during childhood, the data utilized in this study is specifically sourced from studies conducted in China. In addition, two extreme scenarios were used in projecting the future trends: one featuring maximum near-work intensity and minimum time outdoors (maximum growth scenario), akin to the conditions of home quarantine during the Coronavirus disease 2019 (COVID-19), and the other scenario (minimum growth scenario) assuming general adherence to 2-h of daily outdoor time in children.
Compliance with ethics guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Systemic review and meta-analysis
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA), 2020.18
Search strategies
The search protocol is summarized in Fig. 1. Two authors (WP and WZL) searched PubMed, Web of Science, Science Direct, China National Knowledge Infrastructure (CNKI), Wanfang Database, China Science and Technology Journal Database (CSTJ), using terms: “myopia” AND “prevalence” AND (“China” OR “Hong Kong” OR “Macau” OR “Taiwan”) and “refractive error” AND “prevalence” AND (“China” OR “Hong Kong” OR “Macau” OR “Taiwan”). The search results were confined to papers published between 1 January 2010 and 23 November 2024.
Fig. 1.
Flow diagram of the systemic review following the PRISMA 2020 standard. A total of 6555 studies from 6 databases were identified, 2733 were duplicate, 3229 were excluded based on title or abstract, after assessing for eligibility, 82 were included in the final meta-analysis.
Inclusion and exclusion criteria
Inclusion criteria were 1) representative population-based or school-based studies; 2) studies that reported prevalence of myopia or high myopia in children under age of 20 in China; 3) clear definition of myopia and high myopia; 4) studies conducted in China reported in English or Chinese.
Exclusion criteria included 1) studies without cycloplegia; 2) studies with obvious flaws in study design (eg. response rate<70%) or power to detect the prevalence (eg. total study sample size under 200).
Data extraction
Two authors (WP and WZL) assessed the quality of the studies and extracted data independently. Any disagreements between the reviewers were resolved by consensus. Data extracted included author, publication year, study design, myopia and high myopia prevalence, sample size, geographical location (rural or urban), and age. Data for different ages was combined into 5-year age groups from 0 to 19, aligning with Holden et al.6 In this study, we adopted the same 5-year age groupings (0–19 years) used in Holden et al.'s study to facilitate comparisons. In addition, the 0–4 age group typically represents early childhood, the age groups 5–9, and 10–14 allow for progress through schools, while the 15–19 group encompasses high school students preparing for the “Gaokao,” the Chinese college entrance examination–arguably the most critical exams in their lifetime. Additionally, this age grouping allowed for the inclusion of more studies in the meta-analysis, enhancing the robustness of the findings.
Myopia was defined as spherical equivalent (SER) ≤ −0.50 D after cycloplegia, and high myopia as SER ≤ −6.00 D after cycloplegia. The spherical equivalent was defined as sphere+0.5∗cylinder.
Meta-analysis
The prevalence of myopia and high myopia, in the overall childhood population, in rural and urban areas from the 82 studies, and within each age group was pooled using Comprehensive Meta-Analysis software version 3 (Biostat, Englewood, NJ). Prevalence and the 95% confidence interval (95% CI) were generated from fixed-effect models. The resulting prevalence values were used as point estimates of the prevalence status of children in China for the year 2020 in projection models.
Projection across decades (experience-based scenario)
The prevalence of myopia and high myopia for each year was calculated using the following formula based on the method used in Holden et al.6:
Model 1. E (Prevalencet) = Prevalencet-1 ∗ (1+annual percentage change of prevalence).
Where the expected prevalence at year t is equal to the prevalence at year t-1 multiplied by the sum of one and annual percentage change in prevalence.
However, whereas Holden et al. used a universal model based on parameters derived from a limited set of international data for predictions,6 our model used a value for annual percentage change derived from local data. The annual percentage change of prevalence was generated from linear regression models fitted using data from longitudinal and repeated cross-sectional studies. Each study provided annual percentage change of prevalence and baseline prevalence, and the data covered children under age 20 in China. By fitting the log of annual percentage change of prevalence against the baseline prevalence, projection models for myopia (Model 2, R2 = 0.79) and high myopia (Model 3, R2 = 0.99) were generated.
Model 2. Annual percentage change of prevalence in myopia = Exp(−2.12077−0.03984∗Prevalence).
Model 3. Annual percentage change of prevalence in high myopia = Exp(−2.447321−0.071791∗Prevalence).
For children in the age group 0–4, the annual percentage change of prevalence both in myopia and high myopia was set as 0, as children in this age range are in early development and the prevalence of myopia is very low.19 The data used in fitting the annual percentage change of prevalence in myopia and high myopia is summarized in eTable 2 and eTable 3, respectively.20, 21, 22, 23, 24, 25
Simulation of maximum growth scenario
We assumed that the maximum growth scenario is when children experience maximum near work time with little outdoor time. The massive home quarantine in China caused by the outbreak of COVID-19 provided a relevant natural experiment. Since Wang et al. concluded environmental changes caused by home quarantine affect young children from age 6–8 the most,26 we included cycloplegic data during COVID-19 pandemic on 6-year-olds from Hong Kong and 7- to 8-year-old from Lhasa to fit a linear regression (eTable 4).20, 21, 22, 23, 24,27 The projection model for myopia (Model 4, R2 = 0.95) is shown below:
Model 4. Annual percentage change of prevalence in myopia = Exp(−0.01562−0.06821∗Prevalence).
Simulation of minimum growth scenario
Increasing children's time spent outdoors is effective in preventing myopia. The myopia control and prevention program “Tian–Tian 120” in Taiwan showed promising results in reducing the myopia prevalence after years of increasing trend.28 Randomized controlled trials conducted in Guangzhou (“GOALS” study) and Shanghai (“STORM” study) further provided evidences.29,30 In the minimum growth scenario, we assumed the government required all schools to enforce 120 min of outdoor time for children in China. Thus we derived the annual percentage change of prevalence in myopia by averaging results from the “Tian–Tian 120” study, the “YMVIP” study, the “GOALS” study, and the “STORM” study, which was then set as −3.07%.28, 29, 30, 31 It is important to note that the outcome in the “Tian–Tian 120” study was prevalence of reduced visual acuity instead of myopia prevalence (eTable 5),28,31 but this is a good surrogate measure in children.32 The “GOALS” and “STORM” studies applied an additional 40 min of outdoor time during school days instead of 120 min, and these two studies reported myopia incidence rates instead of prevalence rates.
Role of the funding sources
The funders had no role in study design, data collection, data analysis, interpretation, or writing of the report.
Results
From 6555 identified myopia prevalence studies among children in China, 2723 were duplicates, and 3229 were excluded based on title and abstract (Fig. 1). A total of 595 articles were retrieved, 57 of them did not report prevalence of myopia in children, 28 were not representative of the general population of children in China, and 428 articles did not define myopia based on spherical equivalent after cycloplegia. Finally, 82 articles involving 218,794 participants were included in the meta-analysis (eTable 1 & Fig. 2).
Fig. 2.
Geographic distribution of 82 articles in China included in the meta-analysis. 64 studies were conducted in urban areas (in red) from Northern, Eastern, and Southern China; 18 studies of rural areas (in green) were mainly from Northeastern, Northwestern, Western, and Southwestern of China.
Pooled myopia and high myopia prevalence
As shown in Table 1 & eFig. 1, in the 0–4 age group, the pooled prevalence of myopia was 2.6% (95% CI: 2.3%, 2.8%) and the prevalence of high myopia was 0.1% (95% CI: 0.0%, 0.6%). In the 5–9 age group, the pooled prevalence of myopia was 22.0% (95% CI: 21.8%, 22.2%) and that of high myopia was 1.1% (95% CI: 1.0%, 1.2%). In the 10–14 age group, the pooled prevalences were 45.4% (95% CI: 45.1%, 45.7%) and 3.0% (95% CI: 2.8%, 3.1%), respectively. And in the 15–19 age group, the pooled prevalences were 67.2% (95% CI: 66.7%, 67.7%) and 9.5% (95% CI: 9.2%, 9.9%). The overall pooled prevalences of myopia and high myopia in China between 2010 and 2024 were 36.6% (95% CI: 36.4%, 36.8%) and 5.3% (95% CI: 5.2%, 5.5%). Children growing up in urban areas showed higher prevalence of myopia and high myopia than those in rural areas. The pooled myopia prevalences were 39.5% (95% CI: 39.3%, 39.7%) in urban areas, and 28.5% (95% CI: 28.2%, 28.9%) in rural areas. The pooled high myopia prevalences were 6.2% (95% CI: 6.0%, 6.4%) in urban areas, and 0.8% (95% CI: 0.7%, 0.9%) in rural areas.
Table 1.
Pooled prevalence of myopia and high myopia in children, stratified by urban/rural location and age (with cycloplegia; time 2010–2024) in China from 82 studies.
| Characteristics | Prevalence % (95% CI) |
||||
|---|---|---|---|---|---|
| Overall | Aged 0–4 | Aged 5–9 | Aged 10–14 | Aged 15–19 | |
| Myopia | |||||
| References = 82 | References = 10 N = 16,861 |
References = 59 N = 153,801 |
References = 33 N = 91,554 |
References = 18 N = 41,444 |
|
| Overall | 36.6% (36.4%, 36.8%) | 2.6% (2.3%, 2.8%) | 22.0% (21.8%, 22.2%) | 45.4% (45.1%, 45.7%) | 67.2% (66.7%, 67.7%) |
| References = 64 | References = 7 N = 14,979 |
References = 44 N = 108,031 |
References = 23 N = 70,070 |
References = 12 N = 26,919 |
|
| Urban | 39.5% (39.3%, 39.7%) | 2.6% (2.4%, 2.9%) | 24.7% (24.4%, 25.0%) | 48.4% (48.0%, 48.7%) | 77.8% (77.3%, 78.3%) |
| References = 18 | References = 3 N = 1882 |
References = 15 N = 45,770 |
References = 10 N = 21,484 |
References = 6 N = 14,525 |
|
| Rural | 28.5% (28.2%, 28.9%) | 2.0% (0.15%, 2.8%) | 14.2% (13.8%, 14.5%) | 35.8% (35.1%, 36.5%) | 49.2% (48.4%, 50.1%) |
| High Myopia | |||||
| References = 28 | References = 2 N = 2292 |
References = 13 N = 59,296 |
References = 17 N = 56,411 |
References = 9 N = 34,284 |
|
| Overall | 5.3% (5.2%, 5.5%) | 0.1% (0.0%, 0.6%) | 1.1% (1.0%, 1.2%) | 3.0% (2.8%, 3.1%) | 9.5% (9.2%, 9.9%) |
| References = 20 | References = 1 N = 2091 |
References = 9 N = 47,144 |
References = 11 N = 30,556 |
References = 7 N = 24,534 |
|
| Urban | 6.2% (6.0%, 6.4%) | 0.0% (0.0%, 0.4%) | 1.2% (1.1%, 1.3%) | 3.7% (3.5%, 3.9%) | 10.6% (10.2%, 11.0%) |
| References = 8 | References = 1 N = 201 |
References = 4 N = 12,152 |
References = 6 N = 25,855 |
References = 2 N = 9750 |
|
| Rural | 0.8% (0.7%, 0.9%) | 0.2% (0.0%, 3.8%) | 0.2% (0.1%, 0.3%) | 0.6% (0.5%, 0.7%) | 1.3% (1.1%, 1.5%) |
Projection of myopia and high myopia prevalence
Based on the pooled prevalences and the experience-based projection models, the overall myopia and high myopia prevalences were 36.6% and 5.3% (2020), 46.2% and 8.9% (2030), 54.4% and 13.2% (2040), 61.3% and 17.6% (2050) (Fig. 3a). The myopia prevalence in rural areas was 28.5%, 39.1%, 48.3%, 56.2% in 2020, 2030, 2040, and 2050, respectively, while the prevalence in urban areas was 39.5%, 48.7%, 56.5%, 63.1% in 2020, 2030, 2040, and 2050, respectively (Fig. 3a). The high myopia prevalence in rural areas was initially low, but started to increase over time (0.8%, 1.7%, 3.5%, and 6.3% from 2020 to 2050), however, it always lagged behind that in urban areas. Here the prevalence of high myopia increased from 6.2% in 2020 to 10.0%, 14.4%, and 18.8% in 2030, 2040, and 2050, respectively (Fig. 3a). Projections stratified by age are shown in Fig. 3b–d.
Fig. 3.
Projection of the prevalence of myopia and high myopia in urban and rural China from 2020 to 2050. a) Overall: projected prevalence of overall myopia (in blue line) and high myopia (in orange line) across different years: 2020, 2030, 2040, and 2050, and stratified by urban (shaded bars), rural areas (bars without shading); b) Age group 5–9: the myopia prevalence increase rapidly in both urban and rural areas, with about 10% increase each decade. High myopia in urban areas increase rapidly; c) Age group 10–14: myopia and high myopia increase rapidly in both urban and rural areas, especially high myopia in urban areas; d) Age group 15–19: myopia prevalence growth slows down as the prevalence has already reached a high level. High myopia in urban areas was reaches 23.3% in urban areas by 2050.
Projection under three scenarios
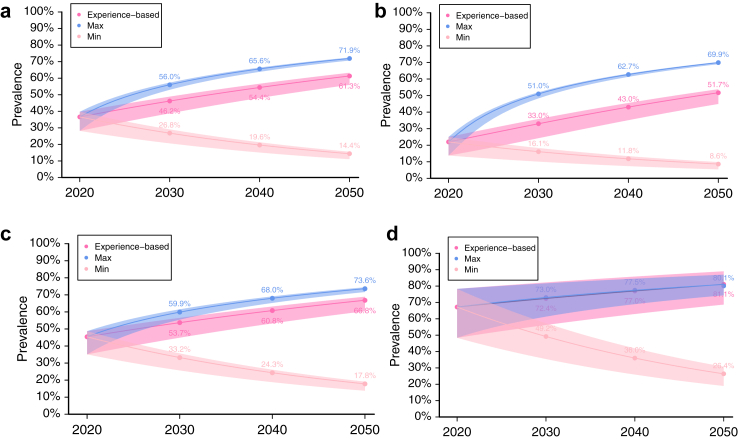
The overall myopia prevalence using the experience-based projection would be 46.2%, 54.4%, and 61.3% in year 2030, 2040, and 2050, respectively (Fig. 4a); in the maximum growth scenario, the overall myopia prevalence would be 56.0%, 65.6%, and 71.9% in year 2030, 2040, and 2050, respectively; and in the minimum growth scenario, the overall myopia prevalence would be 26.8%, 19.6%, and 14.4% in year 2030, 2040, and 2050, respectively. When stratified by age, by year 2050, the age group 5–9 could have myopia prevalence values of 8.6%, 51.7%, and 69.9% in minimum, experience-based, and maximum growth scenarios, respectively (Fig. 4b); age group 10–14 would be 17.8%, 66.8%, and 73.6%, respectively (Fig. 4c); and age group 15–19 would be 26.4%, 81.1%, and 80.1%, respectively (Fig. 4d).
Fig. 4.
Myopia prevalence projection in experience-based, maximum, and minimum growth models. The upper bound of the projection utilized the upper 95% CI of urban myopia prevalence, and the lower utilized the lower 95% CI of rural myopia prevalence. a) Overall: the pooled myopia prevalence was 36.6% (lower bound: 28.2%, upper bound: 39.7%) in 2020, the projected prevalence in 2050 was 71.9%, 61.3, 13.0% in maximum, experience-based, and minimum growth scenario among China's 0–19 year-old children; b) Age group 5–9: the pooled myopia prevalence was 22.0% (13.8%, 25.0%) in 2020; c) Age group 10–14: the pooled myopia prevalence was 45.4% (35.1%, 48.7%) in 2020; d) Age group 15–19: the pooled myopia prevalence was 67.2% (48.4%, 78.3%) in 2020.
Discussion
This study provided an estimate of the prevalence of myopia and high myopia in Chinese children between 2010 and 2024, based on a meta-analysis using only data based on cycloplegic refraction, from articles published from Jan 2010 to Nov 2024. It then projected the trend in childhood myopia and high myopia in China from 2020 to 2050, using three different models. The experience-based model projected that 61.3% and 17.6% of children in China would be myopic and highly myopic in 2050. Rural areas would have a similar myopia prevalence to urban areas, but urban areas would have a much higher prevalence of high myopia. In the extreme model, when maximum intensity of near-work and minimum time outdoors was assumed, the myopia prevalence in 2050 could be as much as 71.9%. However, if the government successfully implemented interventions such as a nationwide program of 2-h/day outdoors, with success rates as reported from Taiwan, the myopia prevalence could drop to as low as 14.4% overall, of 26.4% at the age of entering universities by 2050.
As mentioned before, the meta-analysis conducted by Holden et al., in 2016 focused on the global myopia prevalence and trends in the whole population, from ages 0 to 100.6 Though Holden et al. provided the prevalence of myopia and high myopia in children, the prevalence was pooled for multiple countries in a region. Comparison with the childhood myopia and high myopia prevalence between the East Asia region in Holden et al.'s study and the findings from our meta-analysis for 2010 to 2024 showed inconsistencies (eFig. 2), possibly due to differences in the countries included and the periods covered by the source studies.
Our meta-analysis showed that 36.6% of subjects had myopia and 5.3% had high myopia during the period 2010–2024 (Table 1), aligning closely with the findings of previous meta-analyses by Dong et al. (1998–2016: 37.7% myopia, 3.1% high myopia) and Tang et al. (1983–2017: 38.0% myopia, 2.8% high myopia) in terms of overall myopia prevalence but with a higher prevalence of high myopia.15,16 We believe this discrepancy is, at least in part, attributed to the different time periods of the studies included in the analyses, and their inclusion of non-cycloplegic data. When attempting to compare our results with those from other East and Southeast Asian countries (eg. Japan, South Korea, and Singapore), we found no articles or meta-analyses that met the inclusion and exclusion criteria of this study.
Based on our forecast that assumed increased educational pressures and deprivation of time outdoors comparable to those experienced during the COVID pandemic, in the 15–19 age group, the myopia prevalence could be as high as 80.1% (Fig. 4d). Zhang et al. predicted in 2050, 99.7% of 13–18-year-old children in China would be myopic,17 which is even higher than our estimate. However, Zhang et al.'s predictions were based on non-cycloplegic refractions, which would have over-estimated the prevalence at baseline. Secondly, Zhang et al. did not consider the possibility of reaching a “saturation point” in the prevalence of myopia; that is, when prevalence increased to a certain point, the prevalence would no longer increase, or at least increase more slowly. Some longitudinal studies, which were included in developing our prediction model, already showed almost no annual increase in myopia prevalence in 18-year-old students, with the prevalence reaching a plateau at 80% in Fenghua, and 93% in Tianjin (eTable 2).22,24 For the same reason, it is noticeable that the annual change in myopia prevalence slows down in our prediction model after 2030.
When distinguishing urban and rural populations, the gap in myopia prevalence narrows down over time, with rural areas reaching about 89.1% of the prevalence of urban areas (56.2% vs 63.1%) by 2050 (Fig. 3a). This might reflect the fact that, with the urbanization process occurring in China, the schooling, lifestyle and social environments in rural areas are becoming increasingly similar to those in urban areas, except in the most remote of rural areas. In addition, as China experiences economic growth, a notable trend of “left-behind children” has emerged in rural areas. These children remain with grandparents or other relatives while their parents seek better-paid jobs in cities.11 This separation often leads to increased vulnerability to parental neglect.33 The China Rural Governance Research Center at Wuhan University estimated that in central China's villages, around 50% of children were left behind.34 A survey by the center involving 13,172 parents of “left-behind children” revealed that 89.7% of these children had access to smartphones for playing video games or watching short videos, such as TikTok, without supervision and restriction.34 The rapid pace of economic and technological development, coupled with a lack of parental supervision and peer influence, likely drives high smartphone usage among these children and those in rural areas. Collectively, all these factors probably reduce the myopiagenic environmental difference between the rural and urban areas and lead to the reduced rural-urban gap of myopia prevalence over time.
The findings of this study underscore that high myopia remains a significant public health challenge in China, with its prevalence expected to increase in the coming years. Currently, the prevalence of high myopia among urban children aged 15–19 years stands at 10.6%, with projections suggesting an increase to 23.3% by 2050 (Fig. 3d). Previously, Li et al. simulated a Markov model of a hypothetical 6-year-old cohort's natural progression of myopia to the age of 18, and found that in both China rural and urban settings, the high myopia rate in 18-year-old reached 40%.35 Multiple myopia control interventions (eg. Low-concentration atropine, Orthokeratology, Peripheral defocus spectacles or soft-contact lenses) were developed and were proven effective in recent years.2,36 The high myopia projection in our study was based on trend observed between 1983-2018,22, 23, 24, 25 when there was a low rate of utilization of these effective instruments. According to a cross-sectional study in 2022, 80% of Chinese children in the 10–19 year-old group has single-vision spectacles or contact lenses, which do not slow the progression of myopia, whereas utilization of orthokeratology was only 3%.7 So et al. suggested that 100% uptake of Defocus Incorporated Multiple Segment (DIMS) lenses among 6–11 year-old Hong Kong children, may result in a 44.7% reduction of high myopia prevalence at the age of 18.37,38 Hypothetically, in extreme scenario of largely uptake of myopia control interventions and without changing the current myopia prevalence projections, applying 44.7% reduction, the high myopia prevalence could be 4.9% in 2030, 7.3% in 2040, 9.7% in 2050 among 0–19 year-old children overall. However, 100% uptake is unlikely, and long-term efficacy, compliance issue, varying treatment effects on severity of myopia (spherical equivalent) and age of the child under treatment are all important influencing factors of the high myopia prevalence. Therefore, more comprehensive and refined predictive models that incorporate the above factors are warranted.
Using the data from the period of COVID-19 pandemic as the maximum growth scenario, the projected overall myopia prevalence was estimated to be as high as 71.9% by 2050. When stratified by age, the prevalence showed the greatest difference compared to the experience-based projection in the 5–9 age group, while in the 15–19 age group, the two projections align closely. The result of the 5–9 age group is consistent with Wang et al.'s conclusion that home quarantine (or maximum growth scenario in our study) affects myopia development and progression the most in younger children (6–8 years old).26 And in the 15–19 age group, the results suggested older children were operating with close to maximum near-work intensity and minimum time outdoors already before the COVID-19 outbreak, perhaps due to the high levels of education pressure in the Chinese school system.
Current effective interventions for myopia prevention include increased time spent outdoors, red light therapy, and low-dose atropine.39,40 Considering the cost and side-effect of all these interventions, increasing time spent outdoor may be the most cost-effective strategy and may be applied to the majority of children. In Taiwan, large-scale myopia prevention programs such as the “Tian–Tian 120” initiative,28 and the Yilan Myopia Prevention and Vision Improvement Program (YMVIP),31 had shown positive effects in limiting the rising trend in childhood myopia. In Guangzhou and Shanghai, the ‘Guangzhou Outdoor Activity Longitudinal Study’ (GOALS study), and the ‘Shanghai Time Outside to Reduce Myopia trial’ (STORM study) also supported this strategy. In the minimum growth scenario of our study, mimicking “Tian–Tian 120” and VMVIP where at least 2 h of daily outdoor time are aimed at for all children in China, the forecast myopia prevalence drastically reduces to 14.4% by 2050.
The true childhood myopia prevalence in the next few decades may lie between the two extreme scenarios. Increasing educational pressures and adoption of indoor life-styles could possibly lead to outcomes similar to our experience-based projections. Recognizing the growing concern of myopia among children, the Chinese government has introduced the “Comprehensive Complementation Plan for the Prevention and Control of Myopia” since 2018.41,42 A primary goal of this initiative is to decrease the prevalence of myopia among children by 0.5% annually.
This initiative includes increased time outdoors and reduced time for homework. According to the minimum growth projection, 2 h of daily outdoor time alone may be able to achieve 22.2% (or 0.74% annually) decrease in myopia prevalence by 2050. In addition, the Chinese government has introduced the “Double Reductions” policy in 2021 aimed at reducing educational loads in the compulsory years of schooling, and particularly in the early school years.43 This may create additional space for time outdoors, particularly in the context of full-service schools that provide after school care. But it should be pointed out that it is vital to monitor the impact of these measures as the interventions are rolled out. At one level, the impact can be assessed by current school screening programs, although they do not measure the gold standard of cycloplegic refraction, and educational outcomes can be monitored through current assessment regimes. However, it is noteworthy that the Chinese government has defined priority areas for implementation of these policies, and we suggest that in these areas, monitoring of the prevalence of myopia and high myopia also be carried out on more limited but well-defined populations, using cycloplegic refraction, possibly combined with more rigorous assessment of educational outcomes.
Limitations
There are several limitations in this study. First, variation of actual subjects' age in different studies may influence the results of the meta-analysis. Second, though there were 82 articles included in the meta-analysis, in some subgroups, the number of studies was small, and the majority of included studies were from urban areas, which may also influence the final results. Third, the projection model was based on past experience, which may not reflect actual changes in the future, including more effective myopia prevention and control innovations, or changing penetration rate of myopia prevention and control interventions. Fourth, the number of references used to develop the projection model for the minimum growth scenario was limited, and the referred study's outcome focused on the reduced visual acuity prevalence rather than myopia prevalence.
Conclusion
In summary, this study has established benchmarks for the prevalence of myopia and high myopia based on the gold standard, cycloplegic refraction, for the period 2010 to 2024 in China. This information will provide data for implementing and evaluating the effectiveness of existing and new national-wide myopia prevention and control programs. Projections with our experience-based model suggest an increasing burden for individuals and society, if current trends continue. Our model based on changes that occurred during the COVID pandemic suggests even greater individual and social burdens. Our model, based on the experience of myopia prevention in Taiwan, suggests that substantial reductions in the prevalence of myopia and high myopia can be achieved by increasing time outdoors. Monitoring future changes as China develops its myopia prevention and control policies should provide valuable information for other countries faced with an epidemic of myopia.
Contributors
Idea conception: Weizhong Lan.
Study design: Wei Pan, Weizhong Lan.
Data preparation and analysis: Wei Pan, Weizhong Lan, Ian Morgan.
Manuscript drafting: Wei Pan.
Manuscript criticizing and revising: Zhikuan Yang, Seang-Mei Saw, Tien Yin Wong, Ian Morgan, Weizhong Lan.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval to the version to be published. Wei Pan and Weizhong Lan have access to raw data. Weizhong Lan has the final responsibility for the decision to submit for publication.
Data sharing statement
All data relevant to the study are included in the article or uploaded as online supplementary information.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
TYW receives consulting fees from Abbvie Pte Ltd, Aldropika Therapeutics, Bayer, Boehringer-Ingelheim, Carl Zeiss, Genentech, Novartis, Opthea Limited, Plano, Quaerite Biopharm Research Ltd, Regeneron Pharmaceuticals Inc, Roche, Sanofi, Shanghai Henlius. TYW is an inventor, and hold patents and am a co-founder of start-up companies EyRiS and Visre, which have interests in, and develop digital solutions for eye diseases, including diabetic retinopathy. IM has Personal research advisory contract with State Key Laboratory of Ophthalmology, Guangzhou, China. IM receives support for conference attendance from Eyerising International, and Aier Hospital Group. Other authors declare no conflicts of interest to the current work.
Acknowledgement
This study was funded by the Science and Technology Innovation Program of Hunan Province, China (2023RC1079, 2024RC5002). The authors alone are responsible for the content and writing of the paper.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2025.101484.
Appendix A. Supplementary data
References
- 1.Lawrenson J.G., Shah R., Huntjens B., et al. Interventions for myopia control in children: a living systematic review and network meta-analysis. Cochrane Database Syst Rev. 2023;2(2) doi: 10.1002/14651858.CD014758.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lanca C., Pang C.P., Grzybowski A. Effectiveness of myopia control interventions: a systematic review of 12 randomized control trials published between 2019 and 2021. Front Public Health. 2023;11 doi: 10.3389/fpubh.2023.1125000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haarman A.E.G., Enthoven C.A., Tideman J.W.L., Tedja M.S., Verhoeven V.J.M., Klaver C.C.W. The complications of myopia: a review and meta-analysis. Invest Ophthalmol Vis Sci. 2020;61(4):49. doi: 10.1167/iovs.61.4.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Leveziel N., Marillet S., Dufour Q., et al. Prevalence of macular complications related to myopia - results of a multicenter evaluation of myopic patients in eye clinics in France. Acta Ophthalmol. 2020;98(2):e245–e251. doi: 10.1111/aos.14246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bullimore M.A., Ritchey E.R., Shah S., Leveziel N., Bourne R.R.A., Flitcroft D.I. The risks and benefits of myopia control. Ophthalmology. 2021;128(11):1561–1579. doi: 10.1016/j.ophtha.2021.04.032. [DOI] [PubMed] [Google Scholar]
- 6.Holden B.A., Fricke T.R., Wilson D.A., et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi: 10.1016/j.ophtha.2016.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Ma Y., Wen Y., Zhong H., et al. Healthcare utilization and economic burden of myopia in urban China: a nationwide cost-of-illness study. J Glob Health. 2022;12 doi: 10.7189/jogh.12.11003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dolgin E. The myopia boom. Nature. 2015;519(7543):276–278. doi: 10.1038/519276a. [DOI] [PubMed] [Google Scholar]
- 9.Pan W., Lan W. The current and future landscape of the childhood myopia epidemic in China-A review. Ophthalmol Ther. 2024;13(4):883–894. doi: 10.1007/s40123-024-00887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.M.thepaper.cn Study reveals 450 million people in China are nearsighted, annual socioeconomic costs exceed 680 billion Yuan. https://m.thepaper.cn/kuaibao_detail.jsp?contid=1479289&from=kuaibao.html Available from:
- 11.Shuo Z. Children are becoming increasingly reliant on digital devices. https://www.chinadaily.com.cn/a/202104/13/WS6074ec6ea31024ad0bab50c1.html Available from:
- 12.Foreman J., Salim A.T., Praveen A., et al. Association between digital smart device use and myopia: a systematic review and meta-analysis. Lancet Digit Health. 2021;3(12):e806–e818. doi: 10.1016/S2589-7500(21)00135-7. [DOI] [PubMed] [Google Scholar]
- 13.Cuellar J.M., Lanman T.H. "Text neck": an epidemic of the modern era of cell phones? Spine J. 2017;17(6):901–902. doi: 10.1016/j.spinee.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 14.Bababekova Y., Rosenfield M., Hue J.E., Huang R.R. Font size and viewing distance of handheld smart phones. Optom Vis Sci. 2011;88(7):795–797. doi: 10.1097/OPX.0b013e3182198792. [DOI] [PubMed] [Google Scholar]
- 15.Dong L., Kang Y.K., Li Y., Wei W.B., Jonas J.B. Prevalence and time trends of myopia in children and adolescents in China: a systemic review and meta-analysis. Retina. 2020;40(3):399–411. doi: 10.1097/IAE.0000000000002590. [DOI] [PubMed] [Google Scholar]
- 16.Tang Y., Chen A., Zou M., et al. Prevalence and time trends of refractive error in Chinese children: a systematic review and meta-analysis. J Glob Health. 2021;11 doi: 10.7189/jogh.11.08006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang X., Zhou Y., Wang Y., Du W., Yang J. Trend of myopia through different interventions from 2010 to 2050: findings from Eastern Chinese student surveillance study. Front Med. 2022;9 doi: 10.3389/fmed.2022.1069649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372 doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Brown N.P., Koretz J.F., Bron A.J. The development and maintenance of emmetropia. Eye. 1999;13(Pt 1):83–92. doi: 10.1038/eye.1999.16. [DOI] [PubMed] [Google Scholar]
- 20.Zhang X.J., Zhang Y., Kam K.W., et al. Prevalence of myopia in children before, during, and after COVID-19 restrictions in Hong Kong. JAMA Netw Open. 2023;6(3) doi: 10.1001/jamanetworkopen.2023.4080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ma Y., Lin S., Zhu J., et al. Different patterns of myopia prevalence and progression between internal migrant and local resident school children in Shanghai, China: a 2-year cohort study. BMC Ophthalmol. 2018;18(1):53. doi: 10.1186/s12886-018-0716-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Chen M., Wu A., Zhang L., et al. The increasing prevalence of myopia and high myopia among high school students in Fenghua city, eastern China: a 15-year population-based survey. BMC Ophthalmol. 2018;18(1):159. doi: 10.1186/s12886-018-0829-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li Y., Liu J., Qi P. The increasing prevalence of myopia in junior high school students in the Haidian District of Beijing, China: a 10-year population-based survey. BMC Ophthalmol. 2017;17(1):88. doi: 10.1186/s12886-017-0483-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhang H.M., Li B.Q., Zhu Y., Liu S.X., Wei R.H. Time trends in myopia and high myopia prevalence in young university adults in China. Int J Ophthalmol. 2023;16(10):1676–1681. doi: 10.18240/ijo.2023.10.18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lin L.L., Shih Y.F., Hsiao C.K., Chen C.J. Prevalence of myopia in Taiwanese schoolchildren: 1983 to 2000. Ann Acad Med Singap. 2004;33(1):27–33. [PubMed] [Google Scholar]
- 26.Wang J., Li Y., Musch D.C., et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139(3):293–300. doi: 10.1001/jamaophthalmol.2020.6239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yao Y., Fu J., Liu J., et al. Distribution, progression, and associated factors of refractive status of children in Lhasa, Tibet, after COVID-19 quarantine. Ophthalmic Res. 2022;65(3):321–327. doi: 10.1159/000522548. [DOI] [PubMed] [Google Scholar]
- 28.Wu P.C., Chen C.T., Chang L.C., et al. Increased time outdoors is followed by reversal of the long-term trend to reduced visual acuity in taiwan primary school students. Ophthalmology. 2020;127(11):1462–1469. doi: 10.1016/j.ophtha.2020.01.054. [DOI] [PubMed] [Google Scholar]
- 29.He M., Xiang F., Zeng Y., et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 2015;314(11):1142–1148. doi: 10.1001/jama.2015.10803. [DOI] [PubMed] [Google Scholar]
- 30.He X., Sankaridurg P., Wang J., et al. Time outdoors in reducing myopia: a school-based cluster randomized trial with objective monitoring of outdoor time and light intensity. Ophthalmology. 2022;129(11):1245–1254. doi: 10.1016/j.ophtha.2022.06.024. [DOI] [PubMed] [Google Scholar]
- 31.Yang Y.C., Hsu N.W., Wang C.Y., Shyong M.P., Tsai D.C. Prevalence trend of myopia after promoting eye care in preschoolers: a serial survey in taiwan before and during the Coronavirus disease 2019 pandemic. Ophthalmology. 2022;129(2):181–190. doi: 10.1016/j.ophtha.2021.08.013. [DOI] [PubMed] [Google Scholar]
- 32.Leone J.F., Mitchell P., Morgan I.G., Kifley A., Rose K.A. Use of visual acuity to screen for significant refractive errors in adolescents: is it reliable? Arch Ophthalmol. 2010;128(7):894–899. doi: 10.1001/archophthalmol.2010.134. [DOI] [PubMed] [Google Scholar]
- 33.Wen Y.J., Hou W.P., Zheng W., et al. The neglect of left-behind children in China: a meta-analysis. Trauma Violence Abuse. 2021;22(5):1326–1338. doi: 10.1177/1524838020916837. [DOI] [PubMed] [Google Scholar]
- 34.thepaper.cn M. Rural left-behind children addicted to mobile phones: problem investigation and countermeasures. https://m.thepaper.cn/newsDetail_forward_21875874.html Available from:
- 35.Li R., Zhang K., Li S.M., et al. Implementing a digital comprehensive myopia prevention and control strategy for children and adolescents in China: a cost-effectiveness analysis. Lancet Reg Health West Pac. 2023;38 doi: 10.1016/j.lanwpc.2023.100837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ha A., Kim S.J., Shim S.R., Kim Y.K., Jung J.H. Efficacy and safety of 8 atropine concentrations for myopia control in children: a network meta-analysis. Ophthalmology. 2022;129(3):322–333. doi: 10.1016/j.ophtha.2021.10.016. [DOI] [PubMed] [Google Scholar]
- 37.So C., Lian J., McGhee S.M., Sum R.W.M., Lam A.K.C., Yap M.K.H. Lifetime cost-effectiveness of myopia control intervention for the children population. J Glob Health. 2024;14 doi: 10.7189/jogh.14.04183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lam C.S.Y., Tang W.C., Tse D.Y., et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomised clinical trial. Br J Ophthalmol. 2020;104(3):363–368. doi: 10.1136/bjophthalmol-2018-313739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jonas J.B., Ang M., Cho P., et al. IMI prevention of myopia and its progression. Invest Ophthalmol Vis Sci. 2021;62(5):6. doi: 10.1167/iovs.62.5.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jiang Y., Zhu Z., Tan X., et al. Effect of repeated low-level red-light therapy for myopia control in children: a multicenter randomized controlled trial. Ophthalmology. 2022;129(5):509–519. doi: 10.1016/j.ophtha.2021.11.023. [DOI] [PubMed] [Google Scholar]
- 41.Jan C.L., Congdon N. Chinese national policy initiative for the management of childhood myopia. Lancet Child Adolesc Health. 2018;2(12):845–846. doi: 10.1016/S2352-4642(18)30318-3. [DOI] [PubMed] [Google Scholar]
- 42.Www.gov.cn Notice of Comprehensive prevention and control of children and adolescents myopia implementation plan. https://www.gov.cn/gongbao/content/2019/content_5361801.htm?ivk_sa=1024320u.html Available from:
- 43.Morgan I.G., Jan C.L. China turns to school reform to control the myopia epidemic: a narrative review. Asia Pac J Ophthalmol (Phila) 2022;11(1):27–35. doi: 10.1097/APO.0000000000000489. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.