Abstract
Purpose of review
To summarize the heterogeneity in the elite controllers population with the aim to identify a compatible profile with a persistent HIV remission, making distinction between persistent elite controllers, people with HIV (PWHIV) who permanently maintain virological control in the absence of antiretroviral treatment (ART), and transient elite controllers, PWHIV who eventually lose virological control. For this purpose, it is important to consider the mechanisms and biomarkers that have previously been associated with the maintenance and loss of the natural virological control.
Recent findings
Transient elite controllers, before losing virological control, exhibit a distinct metabolomic, proteomic, microRNAs (miRNA), immunological and virological profile compared to persistent elite controllers. In addition to a reduced and less polyfunctional HIV-specific T-cell response, transient elite controllers show a greater proportion of intact proviruses integrated into genic regions. In contrast, persistent elite controllers display a privileged HIV-1 reservoir profile with absence of detected intact proviruses or low proportion of clonal intact proviruses preferentially integrated into genomic features associated with HIV-1 transcriptional repression.
Summary
According to previous studies, the comprehensive characterization of persistent elite controllers might be crucial to identify other PWHIV with this distinct profile as spontaneously cured.
Keywords: cure, elite controllers, HIV, persistent elite controllers, transient elite controllers
INTRODUCTION
Despite major scientific advances during more than 40 years, no functional or sterilizing cure is available for HIV-1 infection. The main barrier for eradicating HIV-1 is the latent reservoir, infected cells, mainly CD4+ T cells, harboring full length replication-competent proviruses that persist despite antiretroviral treatment (ART) [1]. ART has improved life expectancy [2], but its interruption, in most cases, leads to a viral rebound within a few weeks due to long-lived reservoirs. However, there are groups of people with HIV (PWHIV) who can naturally control viral replication off ART to low HIV-1 levels, as the viremic controllers, or to undetectable levels in plasma by commercially available assay, as the elite controllers or in the case of HIV-1 posttreatment controllers (PTC) after analytical treatment interruption (ATI).
For this reason, reaching an approach that involves permanent virological control without ART, even if the reservoir persists, is a crucial milestone that turns elite controllers in the closest opportunity to achieve an HIV cure.
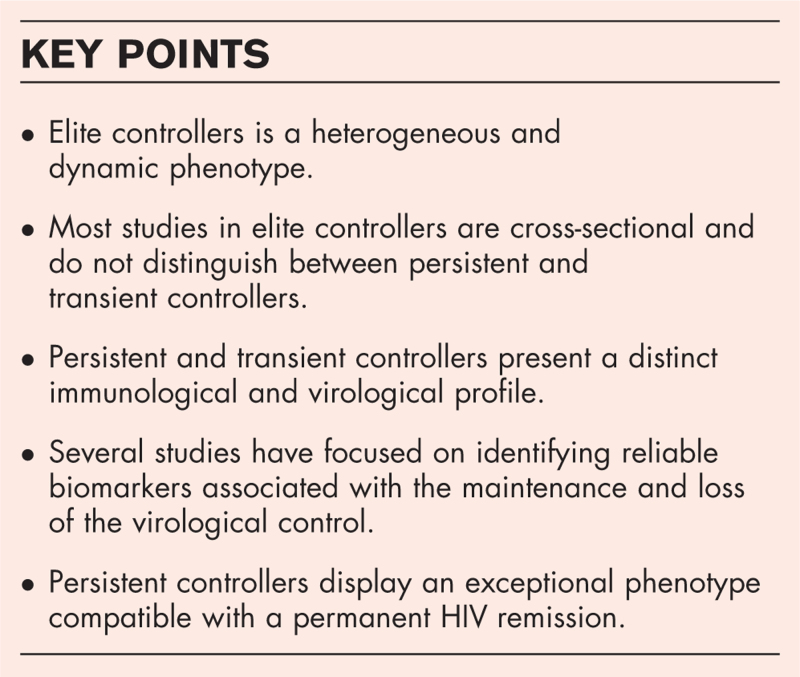
Box 1.
no caption available
ELITE CONTROLLERS: A HETEROGENEOUS AND DYNAMIC GROUP OF PEOPLE WITH HIV
Elite controllers are a unique group of PWHIV, less than 1%, that can naturally control viral replication to undetectable levels in plasma by current commercial assays in the absence of previous ART. However, some elite controllers can experience virological and/or immunological progression and AIDS and/or non-AIDS events [3–5]. This review is focused on virological progression; nevertheless, the long-term control of viral load to undetectable levels is, in most cases, accompanied by preserved long-term CD4+ T-cell levels [6–8].
Elite controllers are a heterogeneous and dynamic group regarding immunological and virological factors. Consequently, over the years, different elite controllers definitions have been described in literature, being important to bring consensus to identify the right study model for a permanent HIV remission. These differences have allowed to differentiate elite controllers in two different phenotypes: those who persistently maintain virological control indefinitely overtime [9,10], the persistent controllers; and those who eventually lose the virological control after being able to control viral replication without ART, the transient controllers.
Most studies in elite controllers are cross-sectional, and consequently, both groups, persistent and transient controllers, have been analyzed in the same group over time. For that reason, without a comprehensive and longitudinal immunological and virological characterization, it is difficult to determine if an elite controllers, that suppress viral replication, will lose the virological control at some point. However, after the analysis of several studies focused on persistent controllers, also known as long-term nonprogressor elite controllers (LTNP-EC) [11,12], long-term elite controllers (LTECs) [13], exceptional elite controllers (EEC) [6], human immunodeficiency virus controllers (HICs) [14] and supercontrollers if they are also able to clear hepatitis C virus (HCV) [15], elite controllers can be classified as persistent controllers if they maintain permanently undetectable viral load without ART for more than 20 years and with stable, nondeclining CD4+ T-cell counts with more than 500 cells/μl [6,10,14,16▪]. However, the mechanisms responsible for the maintenance and loss of the spontaneous virological control in persistent and transient controllers, respectively, remain not clearly defined.
IMMUNOLOGICAL FACTORS ASSOCIATED WITH A PERSISTENT SPONTANEOUS HIV CONTROL
Seminal studies associated the spontaneous HIV control with host immune factors such as human leukocyte antigen class I alleles (HLA-I) [17–21], and immune responses mediated by T-cells [10,22–24]. Several HLA-B alleles have proved effective to restrict virus replication [20,21] whereas others have been associated with risk of HIV progression [25,26]. Some of these protective alleles, especially HLA-B∗57 [12,27,28] and HLA-B∗27 [29], are overrepresented in persistent controllers [6,16▪], suggesting that the associated HIV-1-specific cytotoxic T-lymphocyte (CTL) responses [18,19,27,30] likewise the HIV-1-specific natural killer (NK) cell activation by certain killer cell immunoglobulin receptors (KIR) molecules [31,32] restricted by these alleles may be crucial for the persistent spontaneous control of HIV infection. Furthermore, more recently, the heterozygosity of HLA-I has also been related to HIV control, but its effects on the HIV persistent control are still undetermined [33▪].
The existence of persistent controllers, which maintain virological control without any of these alleles [34], and transient controllers, in a smaller proportion [16▪], which lose the control of the viral replication with that protective alleles, suggests the presence of other immune mechanisms responsible for the persistent spontaneous HIV control [16▪,17]. These immune mechanisms may be also involved in a better ability of persistent controllers, compared to transient controllers, to spontaneously clear or control other chronic infection such as HCV [15,35].
Furthermore, persistent controllers present a stable CD4+ T-cell counts and CD4+ and CD8+ T-cell homeostasis alterations characterized by increased naive T-cells, nonsenescent effector CD8+ T-cells and central memory CD4+ T-cells [13]. These attributes might be related to the greater and stable HIV-specific CD4+[10] and CD8+ T-cell responses over the years in persistent controllers [6,10,12]. In addition, a highly polyfunctional HIV-1-specific T-cell response, especially in CD8+ T-cells, has been associated with the control of viral replication in persistent controllers [6,10,12]. By contrast, transient controllers, before losing virological control, present lower CD4/CD8 ratio, with decreased CD4+ and increased CD8+ T-cell levels [9,14], and a lower and drastic decrease of HIV-specific CD4+ and CD8+ T-cell response, compared to persistent controllers, at 1 year before losing the virological control [10], in agreement with a previous study that comprehensively analyzed the cytotoxic impairment of HIV-specific CD8+ T-cells preceding the aborted spontaneous control of viremia [36]. Interestingly, that study also observed low CD8+ T-cell proliferation, as previously reported in other studies comparing noncontrollers with the overall elite controller population [23,37–39]. However, Collins et al. and others [40] analyzed loss of spontaneous control mostly in viremic controllers with detectable viral loads before the aborted control [36]. This may be the reason why the transient controller phenotype has, interestingly, been associated with increased HIV-specific CD8+ T-cell proliferation prior to the loss of control, likely as an antiviral mechanism aimed at suppressing viral replication below detectable levels [16▪] as indicated by higher viral diversity before viral rebound in transient controllers compared to persistent controllers [10]. In this sense, the time before losing virological control might be key to distinguish both phenotypes since no differences were found in the HIV-specific T-cell response at 2 years before the loss [10]. Despite the high levels of CD8+ T-cells and the increased HIV-specific CD8+ T-cell proliferation, the low polyfunctional HIV-1 specific T-cell response in transient controllers, compared to persistent controllers, may contribute to the loss of the virological control [10,16▪].
Other immunological factors associated with spontaneous control have been NK cells [35,41] and dendritic cells (DC) [6,35]. However, limited data are available regarding the role of NK and DC in the persistent virological control. It is known that persistent controllers display a specific NK profile with an increase of CD16dimCD56dim subset [35,41] and low NK CD56dim cells expressing HLA-DR, exhaustion markers such as TIGIT and Lag3, and CXCR6 [35]. Regarding dendritic cells, persistent controllers have increased number of myeloid dendritic cells (mDCs) [6] and plasmacytoid dendritic cells (pDCs) expressing the lymph node homing marker CCR7 [35].
BIOMARKERS ASSOCIATED WITH THE MAINTENANCE AND LOSS OF VIROLOGICAL CONTROL
Several studies have focused on identifying reliable biomarkers associated with the maintenance and loss of the virological control [10,42–44] with the aim of distinguishing elite controllers that are going to lose the virological control to treat them before the viral rebound; and identifying persistent controllers as the key model to identify permanent HIV remission.
Specific metabolomic, proteomic, and miRNA profiles have been associated with the loss of virological control in transient controllers [42–44], suggesting that they might be important factors to restrict viral replication.
Concerning metabolism, persistent and transient controllers present different metabolomic signature with significant differences in glycolysis, the Krebs cycle, and amino acid catabolism pathways [44]. Transient controllers metabolism is mainly characterized by an aerobic glycolytic metabolism, a deregulated mitochondrial function, oxidative stress, and increased immunological activation [44]. Transient controllers display a similar metabolic profile to what is generally describe for HIV infection, lower glucose concentration due to a significant increase in energy demand, and consequently, an increase in glycolytic intermediates as 3P-glycerate, phosphoenolpyruvate and pyruvate, and branched-chain amino acids as valine, that proved to be the main differentiating metabolomic factor between persistent and transient controllers [44]. The increased levels of Krebs cycle intermediates in transient controllers, as α-ketoglutarate, are possibly supplied by anaplerotic reactions with the aim of trying to compensate the lack of oxidative Krebs cycle activity [44].
The proteomic signature associated with the loss of the virological control is characterized by an increased expression of proteins related to transendothelial migration, coagulation, and inflammation mechanisms, some of them related to HIV-1 replication and pathogenesis and interactions with structural viral proteins [10,43]. Coagulation factor XI, α-1-antichymotrypsin, ficolin-2, 14–3–3 protein, platelet-derived growth factor AA (PDGF-AA), RANTES, and galectin-3-binding protein (LG3BP) are considered potential biomarkers to predict the loss of the virological control [10,43]. Importantly, LG3BP previously associated with increased HIV-1 replication through a direct interaction with gp120 and host CD4+ T-cells [45,46], and the proinflammatory cytokine RANTES associated with HIV progression, proved to be the main biomarkers to identify transient controllers that are about to lose the virological control [47]. Other potential biomarkers are related to extracellular vesicles [48], since persistent controllers present greater levels of extracellular vesicles-associated cytokines, particularly IL-3 and tumor necrosis factor-related apoptosis inducing ligand (TRAIL), compared to transient elite controllers [48]. Furthermore, elevated levels of IL-8, IP-10, and activated CD8+ T-cells (CD38+HLA+DR+) have been associated with disease progression [49].
miRNAs expression is also involved in HIV infection, regulating genes that facilitate and/or restrict viral replication [50]. The expression of hsa-miR-27a-3p, hsa-miR-376a-3p, and hsa-miR-199a-3p, related to lipid metabolism, have been associated with the loss of the virological control, suggesting a lipid dysregulation in transient controllers [42]. Among them, hsa-miR-199a-3p demonstrates to be the best miRNA to identify transient controllers that are going to lose the virological control [42]. The increased lipid levels in transient controllers, before the loss, might be a compensatory mechanism against the viral replication fueled by the aerobic glycolytic pathways that consequently may increase anabolic metabolism [44].
IMPACT OF THE HIV RESERVOIR ON THE SPONTANEOUS PERSISTENT HIV CONTROL
First studies suggested that elite controllers were infected with attenuated quasi species of defective HIV-1 variants, specifically deletions in the nef/long terminal repeat (LTR) [51]. However, a later study in the same cohort demonstrated clinical progression in some of these elite controllers [52]. Subsequently, it was demonstrated that elite controllers can present replication-competent virus and yet control the viral replication [53,54].
Originally, it was known that persistent controllers presented low levels of total HIV-1 DNA with low viral diversity in env and gag genes compared to transient controllers [6,10]. Currently, cutting-edge technology has changed the paradigm, enabling a comprehensive characterization of HIV reservoirs by distinguishing between intact and defective provirus and identifying the integration site of the provirus in the genome [55].
Overall, elite controllers are characterized by a small HIV-1 reservoir with few intact proviruses, compared to PWHIV on ART [55]. In particular, persistent controllers display a distinct HIV-1 reservoir profile with low levels of total HIV-1 DNA and cell-associated HIV-1 RNA [6,16▪], and lower intact proviruses levels, mainly driven by clonally expanded HIV-1 infected cells, compared to transient controllers [10,16▪], and without evidence of replication-competent viruses [6]. Interestingly, no genome-intact HIV-1 proviruses and, in some cases, no cell associated HIV-1 RNA have been detected in a large proportion of persistent controllers [16▪]. Furthermore, persistent controllers show a privileged integration site profile with intact proviruses preferentially located into centromeric satellite DNA or zinc finger genes [16▪], both related to heterochromatin features and consequently with a transcriptional repression [56]. Remarkably, a subgroup of elite controllers present the same integration site profile in another cohort [55]. By contrast, transient controllers’ intact proviruses, before losing virological control, are located into genic regions, as an indicative factor of the viral rebound [16▪]. Interestingly, persistent controllers seem to follow a ‘block and lock’ mechanism [57] by silencing intact proviral gene expression through chromosomal integration into repressive chromatin locations [16▪,55]. Importantly, defective proviruses produce viral proteins that might act as a therapeutic vaccine magnifying the antiviral host immune activity in persistent controllers [58,59]. Despite these findings, it is possible that the virus transmitted to some persistent controllers was permanently defective [60,61].
Unique similar HIV-1 reservoir profiles are observed in other PWHIV as the HIV pediatric cohort, neonates treated within hours after birth [62,63], and PWHIV on long-term ART [64▪▪]. These findings suggest that an early initiation and/or long-term ART induce an HIV-1 reservoir landscape compatible with characteristics of deep latency, as previously reported in persistent controllers [16▪], and possibly, a higher ability to maintain virological control upon ATI.
PERSISTENT CONTROLLERS AS A KEY MODEL TO IDENTIFY A PERMANENT VIROLOGICAL REMISSION
Currently, no cure off ART is available for HIV-1 due to long-lived viral reservoirs. Interestingly, the eradication of HIV-1 reservoir cells has apparently been possible by hematopoietic stem-cell transplantation (HSCT) i.e., in the Berlin [65], London [66,67], Duesseldorf [68], and New York patients [69]. However, HSCT is an impractical approach as HIV cure strategy, due to the difficulty to scale this procedure to the general PWHIV population for safety reasons [70].
Considering this and all the above-mentioned, persistent controllers turn into the closest model for achieving an HIV cure (Fig. 1). However, these findings have to be taken with caution since a limited amount of peripheral blood mononuclear cells (PBMCs) have been analyzed in these studies, with the exception of the San Francisco [55] and the Esperanza patient [71▪▪], in whom a spontaneous HIV cure has been postulated without stem cell transplantation. This has been possible after analyzing a massive number of cells, and even placenta tissue, and not detecting any intact provirus. These cases must be corroborated in a greater number of PWHIV with this persistent controller phenotype, not only in large number of PBMCs but also in tissues.
FIGURE 1.
Persistent controllers as the key model to identify permanent HIV remission. Schematic diagram of different mechanisms associated to the maintenance and loss of the virological control.
Interestingly, this privileged immunological and virological profile has also been reported in other unique PWHIV as PTC [72], and the pediatric cohorts [62,63] and people on long-term ART [64▪▪], suggesting that they might maintain the virological control upon ATI. Therefore, the identification of biomarkers associated with permanent viral remission in these unique PWHIV, including persistent controllers, remain a crucial pending question.
This HIV cure profile found in persistent controller phenotype re-opens the question whether ART is necessary in elite controllers. We believe that ART may be beneficial in transient controllers before losing virological control. This is compatible with some studies where ART has proved to decrease circulating CD4+ T-cells, which contain replication competent HIV, and immune activation in elite controllers [73,74]. Again, we need to define biomarkers that may predict the loss of virological control and act accordingly. However, the profile compatible with an HIV cure found in persistent controllers would advise against ART in these people. This is in favor of some findings that have not found any benefit of ART in elite controllers compared to PWHIV on ART [75]. This is why we think that the recommendations to treat all elite controllers with ART should be taken with caution since they are based on studies that have not considered the natural heterogeneity of elite controllers and their differentiation into persistent and transient controllers’ phenotypes.
CONCLUSION
Persistent controllers display an exceptional phenotype associated with a permanent HIV remission. Further studies designed to identify other PWHIV with this beneficial profile as spontaneously cured based on a comprehensive characterization of the HIV reservoir in high amounts of PBMCs and tissues will be crucial for a better understanding of the specific mechanisms responsible for virological control and for the design of immunotherapeutic strategies aimed to achieve a persistent HIV-1 remission in most of the PWHIV.
Acknowledgements
The authors would like to thank to all the research groups that have been working on defining elite controllers phenotypes, especially those involved in the HIV-1 Elite Controllers Study Group (ECRIS) of the Spanish AIDS Research Network, as well as the study participants. They would also like to thank Laura Tarancon-Diez for her help in designing the figure.
Financial support and sponsorship
This work was supported by the Instituto de Salud Carlos III (Fondo Europeo de Desarrollo Regional, FEDER, “a way to make Europe”, research contracts FI19/00083 and MV20/00057 to C.G.C. and research projects PI19/01127 and PI22/01796 to E.R.M.) and Gilead Fellowships (GLD22/00147 to E.R.M.). E.R.M. was granted by the Spanish National Research Council (CSIC).
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Eisele E, Siliciano RF. Redefining the viral reservoirs that prevent HIV-1 eradication. Immunity 2012; 37:377–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jarrin I, Rava M, Del Romero Raposo J, et al. Life expectancy of people with HIV on antiretroviral therapy in Spain. AIDS 2024; 38:387–395. [DOI] [PubMed] [Google Scholar]
- 3.Crowell TA, Gebo KA, Blankson JN, et al. Hospitalization rates and reasons among HIV elite controllers and persons with medically controlled HIV infection. J Infect Dis 2015; 211:1692–1702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dominguez-Molina B, Leon A, Rodriguez C, et al. Analysis of non-AIDS-defining events in HIV controllers. Clin Infect Dis 2016; 62:1304–1309. [DOI] [PubMed] [Google Scholar]
- 5.Leon A, Perez I, Ruiz-Mateos E, et al. Rate and predictors of progression in elite and viremic HIV-1 controllers. AIDS 2016; 30:1209–1220. [DOI] [PubMed] [Google Scholar]
- 6.Casado C, Galvez C, Pernas M, et al. Permanent control of HIV-1 pathogenesis in exceptional elite controllers: a model of spontaneous cure. Sci Rep 2020; 10:1902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Okulicz JF, Lambotte O. Epidemiology and clinical characteristics of elite controllers. Curr Opin HIV AIDS 2011; 6:163–168. [DOI] [PubMed] [Google Scholar]
- 8.Okulicz JF, Marconi VC, Landrum ML, et al. Clinical outcomes of elite controllers, viremic controllers, and long-term nonprogressors in the US Department of Defense HIV natural history study. J Infect Dis 2009; 200:1714–1723. [DOI] [PubMed] [Google Scholar]
- 9.Chereau F, Madec Y, Sabin C, et al. Impact of CD4 and CD8 dynamics and viral rebounds on loss of virological control in HIV controllers. PLoS One 2017; 12:e0173893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pernas M, Tarancon-Diez L, Rodriguez-Gallego E, et al. Factors leading to the loss of natural elite control of HIV-1 infection. J Virol 2018; 92:e01805-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lopez-Galindez C, Pernas M, Casado C, et al. Elite controllers and lessons learned for HIV-1 cure. Curr Opin Virol 2019; 38:31–36. [DOI] [PubMed] [Google Scholar]
- 12.Mendoza D, Johnson SA, Peterson BA, et al. Comprehensive analysis of unique cases with extraordinary control over HIV replication. Blood 2012; 119:4645–4655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Benito JM, Jimenez-Carretero D, Restrepo C, et al. T cell homeostasis disturbances in a cohort of long-term elite controllers of HIV infection. Int J Mol Sci 2024; 25:5937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Canoui E, Lecuroux C, Avettand-Fenoel V, et al. A subset of extreme human immunodeficiency virus (HIV) controllers is characterized by a small HIV blood reservoir and a weak T-cell activation level. Open Forum Infect Dis 2017; 4:ofx064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dominguez-Molina B, Tarancon-Diez L, Milanes-Guisado Y, et al. Persistent HIV-controllers are more prone to spontaneously clear HCV: a retrospective cohort study. J Int AIDS Soc 2020; 23:e25607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16▪.Gasca-Capote C, Lian X, Gao C, et al. The HIV-1 reservoir landscape in persistent elite controllers and transient elite controllers. J Clin Invest 2024; 134:e174215. [DOI] [PMC free article] [PubMed] [Google Scholar]; Recent study focused on the comprehensive characterization of persistent and transient elite controllers HIV-1 reservoir. Persistent elite controllers seem to follow a ‘block and lock’ mechanism with no intact proviruses detected or with intact proviruses located into regions associated with HIV-1 transcriptional repression, while intact proviruses from transient elite controllers, before losing the virological control, were located into permissive genic euchromatic positions.
- 17.Emu B, Sinclair E, Hatano H, et al. HLA class I-restricted T-cell responses may contribute to the control of human immunodeficiency virus infection, but such responses are not always necessary for long-term virus control. J Virol 2008; 82:5398–5407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Migueles SA, Sabbaghian MS, Shupert WL, et al. HLA B∗5701 is highly associated with restriction of virus replication in a subgroup of HIV-infected long term nonprogressors. Proc Natl Acad Sci U S A 2000; 97:2709–2714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miura T, Brockman MA, Schneidewind A, et al. HLA-B57/B∗5801 human immunodeficiency virus type 1 elite controllers select for rare gag variants associated with reduced viral replication capacity and strong cytotoxic T-lymphocyte [corrected] recognition. J Virol 2009; 83:2743–2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.International HIVCS, Pereyra F, Jia X, et al. The major genetic determinants of HIV-1 control affect HLA class I peptide presentation. Science 2010; 330:1551–1557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fellay J, Shianna KV, Ge D, et al. A whole-genome association study of major determinants for host control of HIV-1. Science 2007; 317:944–947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Migueles SA, Osborne CM, Royce C, et al. Lytic granule loading of CD8+ T cells is required for HIV-infected cell elimination associated with immune control. Immunity 2008; 29:1009–10021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ndhlovu ZM, Chibnik LB, Proudfoot J, et al. High-dimensional immunomonitoring models of HIV-1-specific CD8 T-cell responses accurately identify subjects achieving spontaneous viral control. Blood 2013; 121:801–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saez-Cirion A, Lacabaratz C, Lambotte O, et al. HIV controllers exhibit potent CD8 T cell capacity to suppress HIV infection ex vivo and peculiar cytotoxic T lymphocyte activation phenotype. Proc Natl Acad Sci U S A 2007; 104:6776–6781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Betts MR, Nason MC, West SM, et al. HIV nonprogressors preferentially maintain highly functional HIV-specific CD8+ T cells. Blood 2006; 107:4781–4789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Naranbhai V, Carrington M. Host genetic variation and HIV disease: from mapping to mechanism. Immunogenetics 2017; 69:489–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Dominguez-Molina B, Tarancon-Diez L, Hua S, et al. HLA-B∗57 and IFNL4-related polymorphisms are associated with protection against HIV-1 disease progression in controllers. Clin Infect Dis 2017; 64:621–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Migueles SA, Connors M. Long-term nonprogressive disease among untreated HIV-infected individuals: clinical implications of understanding immune control of HIV. JAMA 2010; 304:194–201. [DOI] [PubMed] [Google Scholar]
- 29.Pereyra F, Addo MM, Kaufmann DE, et al. Genetic and immunologic heterogeneity among persons who control HIV infection in the absence of therapy. J Infect Dis 2008; 197:563–571. [DOI] [PubMed] [Google Scholar]
- 30.Tarancon-Diez L, Dominguez-Molina B, Viciana P, et al. Long-term persistent elite HIV-controllers: the right model of functional cure. EBioMedicine 2018; 28:15–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tano-Menka R, Singh NK, Muzhingi I, et al. Polymorphic residues in HLA-B that mediate HIV control distinctly modulate peptide interactions with both TCR and KIR molecules. Structure 2024; 32:1121–1136.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin MP, Naranbhai V, Shea PR, et al. Killer cell immunoglobulin-like receptor 3DL1 variation modifies HLA-B∗57 protection against HIV-1. J Clin Invest 2018; 128:1903–1912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33▪.Viard M, O’HUigin C, Yuki Y, et al. Impact of HLA class I functional divergence on HIV control. Science 2024; 383:319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]; Authors developed a functional divergence metric of HLA class I allotype pairs that was associated with the protection against viral disease. In particular, a greater functional divergence for HLA-I allotypes pairs was associated with slower AIDS progression and HIV control, likely mediated by a higher breadth of HIV epitope presentation and cytotoxic T cell response.
- 34.Bendenoun M, Samri A, Avettand-Fenoel V, et al. What is the most important for elite control: genetic background of patient, genetic background of partner, both or neither? Description of complete natural history within a couple of MSM. EBioMedicine 2018; 27:51–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dominguez-Molina B, Ferrando-Martinez S, Tarancon-Diez L, et al. Immune correlates of natural HIV elite control and simultaneous HCV clearance-supercontrollers. Front Immunol 2018; 9:2897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Collins DR, Urbach JM, Racenet ZJ, et al. Functional impairment of HIV-specific CD8(+) T cells precedes aborted spontaneous control of viremia. Immunity 2021; 54:2372–2384. e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gaiha GD, McKim KJ, Woods M, et al. Dysfunctional HIV-specific CD8+ T cell proliferation is associated with increased caspase-8 activity and mediated by necroptosis. Immunity 2014; 41:1001–1012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Migueles SA, Laborico AC, Shupert WL, et al. HIV-specific CD8+ T cell proliferation is coupled to perforin expression and is maintained in nonprogressors. Nat Immunol 2002; 3:1061–1068. [DOI] [PubMed] [Google Scholar]
- 39.Rutishauser RL, Deguit CDT, Hiatt J, et al. TCF-1 regulates HIV-specific CD8+ T cell expansion capacity. JCI Insight 2021; 6:136648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rosas-Umbert M, Llano A, Bellido R, et al. Mechanisms of abrupt loss of virus control in a cohort of previous HIV controllers. J Virol 2019; 93:e01436-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rallon N, Jimenez-Carretero D, Restrepo C, et al. A specific natural killer cells phenotypic signature associated to long term elite control of HIV infection. J Med Virol 2024; 96:e29646. [DOI] [PubMed] [Google Scholar]
- 42.Masip J, Gasca-Capote C, Jimenez-Leon MR, et al. Differential miRNA plasma profiles associated with the spontaneous loss of HIV-1 control: miR-199a-3p and its potential role as a biomarker for quick screening of elite controllers. Clin Transl Med 2021; 11:e474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rodriguez-Gallego E, Tarancon-Diez L, Garcia F, et al. Proteomic profile associated with loss of spontaneous human immunodeficiency virus type 1 elite control. J Infect Dis 2019; 219:867–876. [DOI] [PubMed] [Google Scholar]
- 44.Tarancon-Diez L, Rodriguez-Gallego E, Rull A, et al. Immunometabolism is a key factor for the persistent spontaneous elite control of HIV-1 infection. EBioMedicine 2019; 42:86–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.St-Pierre C, Manya H, Ouellet M, et al. Host-soluble galectin-1 promotes HIV-1 replication through a direct interaction with glycans of viral gp120 and host CD4. J Virol 2011; 85:11742–11751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wang SF, Tsao CH, Lin YT, et al. Galectin-3 promotes HIV-1 budding via association with Alix and Gag p6. Glycobiology 2014; 24:1022–1035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zhao J, She S, Xie L, et al. The effects of RANTES polymorphisms on susceptibility to HIV-1 infection and disease progression: evidence from an updated meta-analysis. AIDS Res Hum Retroviruses 2016; 32:517–528. [DOI] [PubMed] [Google Scholar]
- 48.Poveda E, Fitzgerald W, Reglero C, et al. Interleukin 18 (IL-18) and IL-3 in extracellular vesicles: biomarkers for durable elite control of HIV-1. J Infect Dis 2023; 227:1381–1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Cortes FH, de Paula HHS, Bello G, et al. Plasmatic levels of IL-18, IP-10, and activated CD8(+) T cells are potential biomarkers to identify HIV-1 elite controllers with a true functional cure profile. Front Immunol 2018; 9:1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chinniah R, Adimulam T, Nandlal L, et al. The effect of miRNA gene regulation on HIV disease. Front Genet 2022; 13:862642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Deacon NJ, Tsykin A, Solomon A, et al. Genomic structure of an attenuated quasi species of HIV-1 from a blood transfusion donor and recipients. Science 1995; 270:988–991. [DOI] [PubMed] [Google Scholar]
- 52.Churchill MJ, Rhodes DI, Learmont JC, et al. Longitudinal analysis of human immunodeficiency virus type 1 nef/long terminal repeat sequences in a cohort of long-term survivors infected from a single source. J Virol 2006; 80:1047–1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bailey JR, O’Connell K, Yang HC, et al. Transmission of human immunodeficiency virus type 1 from a patient who developed AIDS to an elite suppressor. J Virol 2008; 82:7395–7410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Blankson JN, Bailey JR, Thayil S, et al. Isolation and characterization of replication-competent human immunodeficiency virus type 1 from a subset of elite suppressors. J Virol 2007; 81:2508–2518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Jiang C, Lian X, Gao C, et al. Distinct viral reservoirs in individuals with spontaneous control of HIV-1. Nature 2020; 585:261–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vogel MJ, Guelen L, de Wit E, et al. Human heterochromatin proteins form large domains containing KRAB-ZNF genes. Genome Res 2006; 16:1493–1504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Woldemeskel BA, Kwaa AK, Blankson JN. Viral reservoirs in elite controllers of HIV-1 infection: implications for HIV cure strategies. EBioMedicine 2020; 62:103118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Imamichi H, Smith M, Adelsberger JW, et al. Defective HIV-1 proviruses produce viral proteins. Proc Natl Acad Sci U S A 2020; 117:3704–3710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pollack RA, Jones RB, Pertea M, et al. Defective HIV-1 proviruses are expressed and can be recognized by cytotoxic T lymphocytes, which shape the proviral landscape. Cell Host Microbe 2017; 21:494–506. e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lian X, Gao C, Sun X, et al. Signatures of immune selection in intact and defective proviruses distinguish HIV-1 elite controllers. Sci Transl Med 2021; 13:eabl4097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Casado C, Marrero-Hernandez S, Marquez-Arce D, et al. Viral characteristics associated with the clinical nonprogressor phenotype are inherited by viruses from a cluster of HIV-1 elite controllers. mBio 2018; 9:e02338-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Garcia-Broncano P, Maddali S, Einkauf KB, et al. Early antiretroviral therapy in neonates with HIV-1 infection restricts viral reservoir size and induces a distinct innate immune profile. Sci Transl Med 2019; 11:eaax7350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hartana CA, Garcia-Broncano P, Rassadkina Y, et al. Immune correlates of HIV-1 reservoir cell decline in early-treated infants. Cell Rep 2022; 40:111126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64▪▪.Lian X, Seiger KW, Parsons EM, et al. Progressive transformation of the HIV-1 reservoir cell profile over two decades of antiviral therapy. Cell Host Microbe 2023; 31:83–96. e5. [DOI] [PMC free article] [PubMed] [Google Scholar]; People with HIV after long-term ART seem to follow a ‘block and lock’ mechanism similar to what it is observed in elite controllers, intact proviruses predominantly integrated into heterochromatin locations. These deep latency features might be indicative of a virological control upon treatment interruption.
- 65.Allers K, Hutter G, Hofmann J, et al. Evidence for the cure of HIV infection by CCR5Delta32/Delta32 stem cell transplantation. Blood 2011; 117:2791–2799. [DOI] [PubMed] [Google Scholar]
- 66.Gupta RK, Abdul-Jawad S, McCoy LE, et al. HIV-1 remission following CCR5Delta32/Delta32 haematopoietic stem-cell transplantation. Nature 2019; 568:244–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gupta RK, Peppa D, Hill AL, et al. Evidence for HIV-1 cure after CCR5Delta32/Delta32 allogeneic haemopoietic stem-cell transplantation 30 months post analytical treatment interruption: a case report. Lancet HIV 2020; 7:e340–e347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Jensen BO, Knops E, Cords L, et al. In-depth virological and immunological characterization of HIV-1 cure after CCR5Delta32/Delta32 allogeneic hematopoietic stem cell transplantation. Nat Med 2023; 29:583–587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hsu J, Van Besien K, Glesby MJ, et al. HIV-1 remission and possible cure in a woman after haplo-cord blood transplant. Cell 2023; 186:1115–1126. e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Bhatia S. Long-term health impacts of hematopoietic stem cell transplantation inform recommendations for follow-up. Expert Rev Hematol 2011; 4:437–452. quiz 453-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71▪▪.Turk G, Seiger K, Lian X, et al. A possible sterilizing cure of HIV-1 infection without stem cell transplantation. Ann Intern Med 2022; 175:95–100. [DOI] [PMC free article] [PubMed] [Google Scholar]; Recent case of a permanent HIV-1 remission without stem cell transplantation. Intact HIV-1 proviruses were not detected after analyzing billion of cells.
- 72. Roseto IC, Lian X, Seiger K, et al. Distinct integration sites of intact HIV-1 proviruses in post treatment controllers. Conference on Retroviruses and Opportunistic Infections; 2023; Seattle, WA. [Accessed 19 February to 22 February 2023] [Google Scholar]
- 73.Chun TW, Shawn Justement J, Murray D, et al. Effect of antiretroviral therapy on HIV reservoirs in elite controllers. J Infect Dis 2013; 208:1443–1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Li JZ, Segal FP, Bosch RJ, et al. Antiretroviral therapy reduces T-cell activation and immune exhaustion markers in human immunodeficiency virus controllers. Clin Infect Dis 2020; 70:1636–1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Crowell TA, Ganesan A, Berry SA, et al. Hospitalizations among HIV controllers and persons with medically controlled HIV in the U.S. Military HIV Natural History Study. J Int AIDS Soc 2016; 19:20524. [DOI] [PMC free article] [PubMed] [Google Scholar]