Abstract
Background
Global aphasia is a severe communication disorder affecting all language modalities, commonly caused by stroke. Evidence as to whether the functional communication of people with global aphasia (PwGA) can improve after speech and language therapy (SLT) is limited and conflicting. This is partly because cognition, which is relevant to participation in therapy and implicated in successful functional communication, can be severely impaired in global aphasia. Cognitive treatments that aim to improve functional communication for people with aphasia do exist, but few have been trialled with PwGA and no studies have robustly demonstrated gains.
Aim
This study aimed to explore the effect of a novel non‐linguistic cognitive intervention on the functional communication skills of PwGA.
Method
A non‐linguistic intervention, developed to target cognitive skills underpinning functional communication, was delivered to six participants three times weekly for up to 6 weeks (depending on the rate of progression through the intervention programme). All participants met the criteria for global aphasia following screening with the Western Aphasia Battery Bedside Record Form. A multiple baseline case series design was employed to investigate changes in functional communication using the American Speech and Hearing Association Functional Assessment of Communication (ASHA‐FACS). Secondary outcome measures were auditory comprehension and informal tests of non‐verbal cognition. Statistical analyses of change after intervention were performed using the Wilcoxon signed‐ranks test and weighted statistics.
Results
Participants completed the intervention programme in an average of nine sessions. Four out of six participants made statistically significant gains in functional communication as measured by communication independence (amount of assistance or prompting required) on the ASHA‐FACS. Five of six participants made statistically significant gains in non‐verbal semantics, two in non‐verbal reasoning and two in auditory comprehension.
Conclusion
The findings provide preliminary evidence that a non‐linguistic cognitive intervention delivered with a dose replicable in clinical practice can improve functional communication and non‐verbal cognition in some PwGA. This finding contrasts with much existing evidence suggesting that improvements in global aphasia can be achieved only after intensive or prolonged input over many years.
WHAT THIS PAPER ADDS
What is already known on the subject
People with global aphasia (PwGA) have the potential to make impairment level gains after intensive or prolonged speech and language therapy (SLT). However, evidence of functional communication gains is limited. Cognition plays an important role in functional communication, particularly the ability to switch to alternative means of communication and switch modalities.
What this study adds
Contrary to many previous studies, the findings indicate that PwGA can benefit from SLT and make functional communication gains with a relatively low dose of intervention. The findings highlight cognitive skills that appear relevant to basic functional communication abilities in PwGA. These are: attention, visual perception, semantics and non‐verbal problem solving.
What are the clinical implications of this work?
This work suggests that clinicians should offer cognitive, non‐linguistic interventions to PwGA and consider delivering intervention using little to no verbal language.
Keywords: cognition, global aphasia, intervention
Background
Global aphasia is widely accepted to be ‘a severe acquired impairment of communicative ability across all language modalities where often no single communicative modality is strikingly better than another’ (Collins, 1986, p. 6). Usually, a distinction is drawn between ‘severe’ and ‘global’ aphasia, with the former term often used to describe severe impairments in expressive language only. Despite global aphasia affecting up to 30% of post‐stroke aphasia cases (Collins, 1986) and being the most severe and disabling of all the aphasia sub‐types, it is significantly under‐researched.
Intervention studies targeting global aphasia are few compared to those involving other aphasia sub‐types. Salis and Edwards (2015) note that as a result, evidence is often drawn from research into severe aphasia, in which compensatory communication approaches focusing on the development of skills such as gesture and drawing are routinely used. However, there is little published evidence of successful functional communication outcomes when such approaches are applied to global aphasia.
In the small number of intervention studies that have demonstrated gains after speech and language therapy (SLT) in people with global aphasia (PwGA), intervention has either been delivered at doses incompatible with clinical practice, or functional communication outcomes have not been measured or have not been robust. For example, Denes et al. (1996) reported impairment level language gains in a group of eight PwGA following daily SLT involving language, total communication and conversation training delivered over a 6‐month period. However, no functional communication outcome measure was included. Ho et al. (2005) targeted behaviours relevant to functional communication such as topic initiation, pointing and turn‐taking using remnant picture books and standard picture books in two PwGA. They reported an increase in the frequency of pointing and initiating a topic after intervention with both types of picture book, but slightly more instances of pointing with remnant picture books. In this study the sample size was small and only visual inspection (no statistical analysis) was used to analyse data. Due to limited evidence of response to therapy, many have assumed that prognosis in global aphasia is poor (Munro & Siyambalapitiya, 2016). The lack of intervention studies available to inform clinical practice and the limited evidence of functional communication gains motivated the study reported in this paper.
The limited evidence of positive functional communication changes in global aphasia can, in part, be attributed to the challenges in assessing functional communication and demonstrating change in this population. In severe aphasia, where individuals often have the comprehension skills to participate, measures involving role play are used and non‐verbal responses are accepted (for example, The Scenario Test, Hilari & Dipper, 2020). However, for PwGA test instructions are inaccessible due to linguistic complexity, and the requirement to engage in hypothetical/abstract situations with little environmental or contextual cues can require more advanced cognitive skills than many PwGA possess. Proxy measures such as the American Speech and Hearing Association Functional Assessment of Communication (ASHA‐FACS; Frattali et al., 1995; revised Frattali et al., 2017) despite being subject to rater bias (Van Der Meulen et al., 2010) have been deemed to be a more authentic way of assessing functional communication in those with severe aphasia (Manochiopinig et al., 1992).
Cognition and global aphasia
Post‐intervention functional communication gains in PwGA may be limited by cognitive deficits. Cognition has been found to play a role in overall functional outcomes for people with aphasia (El Hachioui et al., 2014) and to correlate with successful functional communication (Fridriksson et al., 2006). Cognitive deficits have been found to occur alongside aphasia, particularly in the domains of attention and executive functioning (Helm‐Estabrooks, 2002). Cognitive flexibility, a component of executive functioning, has been found to be particularly relevant to functional communication in less severe forms of aphasia, for example when switching communication modalities (Chiou & Kennedy, 2009; Purdy, 2002).
Severe cognitive deficits may exist in many PwGA (Adjei‐Nicol, 2023). Using a neuropsychological battery designed for PwGA, van Mourik et al. (1992) found that 13 of 17 individuals had deficits in attention and visual and auditory recognition memory. The authors suggested that those with the most severe cognitive deficits such as reduced communicative intent, limited ability to draw and inconsistent yes‐no responses may not be able to benefit from direct SLT and therefore intervention should be delivered indirectly with communication partners and target social interaction. Studies by Marinelli et al. (2017) and Olsson et al. (2019) further suggest that within the range of people with severe or global aphasia, those with more severe linguistic impairments (for example those who are non‐verbal and/or have severe naming, comprehension, reading and spelling difficulties) also have more marked cognitive deficits.
Cognitive interventions have been trialled with people with aphasia with the aim of improving language. For example, Helm‐Estabrooks et al. (2000) reported improvements in auditory comprehension in two people with moderate‐severe aphasia following a cognitive intervention known as attention treatment programme (ATP). ATP is a hierarchical intervention which targets non‐linguistic visual memory, mathematics, visual perception, semantics, and problem‐solving. However, many of the tasks are unsuitable for PwGA due to the level of auditory comprehension required to understand task instructions. In global aphasia specifically, improvements in auditory comprehension of spoken nouns and verbs were reported by Helm‐Estabrooks et al. (1982) following visual action therapy (VAT), a non‐linguistic intervention. VAT targets gesture alongside cognitive skills such as visual perception, visual recognition and visual semantics. Helm‐Estabrooks et al. (1982) delivered VAT intensively to eight PwGA daily for 30‐min for up to 14 weeks and found improvements in gestural comprehension, gestural production and spoken word comprehension on the PICA (Porch, 1967). The authors hypothesised that improvement in auditory comprehension may be an indirect consequence of improved cognitive skills, such as attention, visual spatial skills and visual search skills. These results suggest that treating cognition may improve auditory comprehension and gesture production in some people with severe or global aphasia. However, VAT was delivered intensively which may be difficult to replicate clinically and neither study of APT or VAT measured the impact of the cognitive intervention on functional communication.
In summary, there is need for an intervention that targets cognitive skills in global aphasia, is accessible for PwGA, has the potential to improve functional communication and is deliverable within a dose replicable clinically.
Aim
The aim of this intervention study was to measure the effect of a novel non‐linguistic cognitive intervention, designed specifically for PwGA, on functional communication, non‐verbal cognition (as measured by tests of visual perception, visual semantics, auditory semantics and non‐verbal reasoning) and auditory comprehension.
Method
Design
The study was a case series of six PwGA using a single‐subject multiple‐baseline ABA design. This comprised 6 weeks of baseline testing (A1), followed by 6 weeks of intervention (B) and 2 weeks of post‐intervention re‐assessment (A2). After a 3‐month no‐intervention period, participants were assessed for maintenance of change (A3). Primary, secondary and control outcome measures were administered before and after intervention, and again at maintenance. The study was approved under the Mental Capacity Act (MCA 2005) by NHS East of England Research Ethics Committee (reference: 14/EE/1076). All participants lacked capacity to consent to participate and a relative/friend was appointed as personal consultee in accordance with the MCA (2005).
Participants
Participants with global aphasia were recruited from NHS community SLT services and independent neurological rehabilitation centres in the United Kingdom. All participants were adults over 18 years of age who had experienced at least one stroke (as diagnosed by a physician) of which the most recent was at least 6 months prior to entering the study. Six participants were recruited, see Table 1 for demographic details. All participants were confirmed to have English as their main language of use and to not be receiving SLT or any other therapy or rehabilitation. They were screened by the first author (a qualified speech and language therapist) using the Western Aphasia Battery‐Revised bedside screening form (WAB‐R; Kertesz, 2006) to confirm a diagnosis of global aphasia. This short screening tool was used due to the severity of impairments and limited ability of participants to complete lengthy formal assessments. Central semantics was profiled using the Pyramids and Palm Trees Test (Howard & Patterson, 1992) (see Table 2). An attempt was made to profile cognition (in the form of non‐verbal reasoning) using the Wisconsin Card Sorting Test‐64 card version (WCST‐64; Kongs et al., 2000). This has been used widely in studies of aphasia. However, no participant was able to understand the requirements of the assessment, highlighting the difficulty in assessing cognition in this population. Further to this, participants were confirmed by their referring speech and language therapist to display the following characteristics of global aphasia, which were based on clinician responses to a survey conducted during the first author's wider PhD study (Adjei‐Nicol, 2020) and descriptions of global aphasia in the literature (Collins, 1986):
Little or no verbal output.
Inconsistent single word comprehension.
Little or no ability to read or write.
Little or no ability to use alternative modes of communication.
Little or no ability to make functional choices.
TABLE 1.
Demographic information for participants with global aphasia.
| Participant (pseudonym) | Gender | Age (years) | Aetiology | Time post stroke | Pre‐morbid handedness | Residence |
|---|---|---|---|---|---|---|
| Bernard | Male | 57 | L MCA infarct | 3 y 9 m | Left | Home with son |
| Peter | Male | 61 | L MCA infarct | 3 y 9 m | Right | Nursing home |
| Alan | Male | 80 | L parietal infarct | 6 m | Right | Home with wife |
| Ruby | Female | 81 | L MCA infarct | 1 y 3 m | Right | Nursing home |
| Henry | Male | 58 | L MCA infarct | 1 y 6 m | Right | Home with wife |
| Kevin | Male | 72 |
|
|
Right | Nursing home |
Abbreviations: L, left; m, month(s); MCA, middle cerebral artery; R, right; y, year(s).
TABLE 2.
Participant profiles.
| WAB‐R bedside record form (Kertesz, 2006) | Pyramids and palm trees test (Howard & Patterson, 1992) | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| SSC | SSF | AVC | SC | REP | ON | BAS | WRI | REA | BLS | RS | Observations | |
| n = 10 | n = 10 | n = 10 | n = 10 | n = 10 | n = 10 | n = 100 | n = 10 | n = 10 | n = 100 | n = 52 | ||
| Bernard | 1 | 0 | 3 | 0 | 0 | 0 | 7 | 0 | 0 | 5 | 0 | Selects all three options (target, response and distractor) |
| Peter | 0 | 0 | 2 | 3 | 0 | 0 | 10 | 0 | 0 | 7.5 | 6 | Gives no response or selecting item on left side |
| Alan | 0 | 0 | 5 | 3 | 2 | 0 | 17 | 0 | 0 | 21 | 0 | No response to any item |
|
Ruby |
0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | No response to any item |
|
Henry |
1 | 0 | 3 | 2 | 2 | 0 | 15 | 0 | 0 | 19 | 0 | Selects all three options (target, response and distractor) |
|
Kevin |
0 | 0 | 2 | 1 | 1 | 0 | 7 | 0 | 0 | 9 | 0 | Selects all three options (target, response and distractor) |
Abbreviations: AVC, auditory verbal comprehension; BAS, bedside aphasia score; BLS, bedside language score; ON, object naming; REA, reading; REP, repetition; RS, raw score; SC, sequential commands; SSC, spontaneous speech content; SSF, spontaneous speech fluency; WAB‐R, Western Aphasia Battery‐Revised; WRI, writing.
Exclusion criteria were diagnosis of a progressive neurological condition, history/current diagnosis of a mental health condition, hearing loss that was not age related.
Outcome measures
Table 3 summarises the assessment procedure.
TABLE 3.
Assessment procedure.
| Baseline testing (A1) | Post intervention testing | Maintenance testing | |||||
|---|---|---|---|---|---|---|---|
| (A2) | (A3) | ||||||
| Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
Week 13 Week 14 |
Week 25 |
| ASHA‐FACS |
Obj‐pic match (n = 15 items: 5TR, 5UR, 5UU) |
Spoken word repetition□ (control task) |
Obj‐pic match (n = 10 items: 5TR, 5UR) |
Spoken word repetition□ (control task) |
Obj‐pic match (n = 10 items: 5TR, 5UR) |
ASHA‐FACS Spoken word repetition□ (control task) |
ASHA‐FACS Spoken word repetition□ (control task) |
| Auditory comprehension◊ |
Sound‐pic match (n‐15 items: 5TR, 5UR, 5UU) |
Sound‐pic match (n = 10 items: 5TR, 5UR) |
Sound‐pic match (n = 10 items: 5TR, 5UR) |
RCPM Auditory Comprehension◊ |
RCPM Auditory Comprehension◊ |
||
| RCPM |
Gesture‐pic match (n = 15 items: 5TR, 5UR, 5UU) |
Gesture‐pic match (n = 10 items: 5TR, 5UR) |
Gesture‐pic match (n = 10 items: 5TR, 5UR) |
Obj‐pic match (n = 15 items: 5TR, 5UR, 5UU) |
Obj‐pic match (n = 15 items: 5TR, 5UR, 5UU) |
||
|
Spoken word repetition (control task)□ |
Pic categorisation (n = 30 items: 10TR, 10UR, 10UU) |
Pic categorisation (n = 20 items: 10TR, 10UR) |
Pic categorisation (n = 20 items: 10TR, 10UR) |
Sound‐pic match (n‐15 items: 5TR, 5UR, 5UU) Gesture‐pic match (n = 15 items: 5TR, 5UR, 5UU) Pic categorisation (n = 30 items: 10TR, 10UR, 10UU) |
Sound‐pic match (n‐15 items: 5TR, 5UR, 5UU) Gesture‐pic match (n = 15 items: 5TR, 5UR, 5UU) Pic categorisation (n = 30 items: 10TR, 10UR, 10UU) |
||
Abbreviations: ASHA‐FACS, American Speech and Hearing Association Functional Assessment of Communication (Frattali et al., 1995); Gesture‐pic match, gesture‐to‐picture matching; Obj‐pic match, object‐to‐picture matching; Sound‐pic match, environmental sound‐to‐picture matching; Pic. categorisation, picture categorisation; RCPM, Raven's Coloured Progressive Matrices (Raven et al., 1990); TR, treated and repeated; UR, untreated and repeated; UU, untreated and unrepeated.
Functional communication
The primary outcome measure was the ASHA‐FACS (Frattali et al., 1995), a proxy measure which assesses 43 communication behaviours. Many of the target behaviours are non‐verbal, basic and thus relevant for PwGA. Each behaviour is rated on a scale of 1–7 for communication independence (CI). CI is based on the level of assistance or prompting required to carry out a behaviour. The behaviours are divided into four sub‐categories: social communication, communication of basic needs, reading/writing/number concepts and daily planning. Each sub‐category is rated on a scale of 1–5 for qualitative communication (QC) based on four domains: adequacy, appropriateness, promptness and communication sharing (the degree to which the communication partner carries the burden of communication). The consultee of each participant with global aphasia completed ratings once at baseline (A1), once post intervention (A2) and once at maintenance (A3). A mean CI and QC rating was calculated for each participant.
Non‐verbal cognition
Four informal non‐verbal semantic tasks (object‐to‐picture matching, gesture‐to‐picture matching, environmental sound‐to‐picture matching, and picture categorisation) were completed as secondary outcome measures. All items were high‐frequency exemplars from chosen categories based on the data of Van Overschelde et al. (2004). For object‐to‐picture matching, gesture‐to‐picture matching and environmental sound‐to‐picture matching 15 items were assessed, five of which were treated and assessed three times at A1, then once at A2 and A3 (TR: treated and repeated), five were assessed three times at A1, once at A2 and A3 but were not treated (UR: untreated repeated), and five were not treated and only assessed once at A1, once at A2 and once at A3 (UU: untreated and unrepeated). For picture categorisation, participants were asked to sort three sets of 10 pictures (30 in total) into categories. One set of pictures were treated and assessed three times at A1, once at A2 and once at A3 (TR: treated and repeated), one set were untreated and assessed three times at A1, once at A2 and once at A3 (UR: untreated repeated), and one set were untreated and only assessed once at A1, once at A2 and once at A3 (UU: untreated and unrepeated). This procedure enabled exploration of generalisation to untreated items. All treated and untreated items were matched for familiarity using Snodgrass and Vanderwart (1980).
In addition, Raven's Coloured Progressive Matrices (RCPM; Raven et al., 1990) was completed once during A1–A3 to assess non‐verbal reasoning.
Auditory comprehension
The auditory comprehension sub‐section of the Aphasia Screening Test (AST; Whurr, 2011) was completed once during A1–A3 to establish whether the intervention indirectly improved auditory comprehension.
Control measure
The spoken word repetition sub‐test of the Comprehensive Aphasia Test (CAT; Swinburn et al., 2004) was deployed as a control measure and completed three times during A1 then once during A2 and A3. The intervention in this study targeted underlying cognitive skills relevant to functional communication and had the potential to lead to improvement in a range of cognitive domains. However, because it was non‐linguistic in nature and largely completed non‐verbally, verbal repetition skills were chosen as a control measure as they were not expected to improve.
Intervention development and procedure
The novel non‐linguistic cognitive intervention developed for this study is described according to the Template for Intervention Description and Replication (TIDieR; Hoffmann et al., 2014; see Appendix A). It aims to improve cognitive skills relevant to functional communication specifically:
Understanding of non‐verbal cues such as iconic gestures.
Ability to express a want, need or choice through pointing at a picture/object from an array of options.
Ability to understand gestures and make choices in the presence of visual or auditory distractors.
The intervention consists of 16 tasks (see Appendix B) hierarchically ordered by level of difficulty based on a review of the literature on cognitive interventions in stroke and brain injury (Adjei‐Nicol, 2020). Five tasks were computer‐based and developed for the purpose of this study and the remainder were paper‐based. All tasks were non‐linguistic in keeping with other cognitive interventions used in aphasia such as VAT (Helm‐Estabrooks et al., 1982) and ATP (Sohlberg & Mateer, 1987). Tasks were designed to link to skills required for basic functional communication, such as making a choice through pointing, or understanding iconic gestures and be accessible for PwGA. Whilst VAT is completely non‐verbal, in this intervention some verbal language was used when providing task instructions, in the form of 10 words or phrases: ‘look’/‘looking’, ‘this’, ‘and’, ‘or’, ‘good’, ‘together’, ‘here’, ‘your turn’, ‘yes’ and ‘no’. This was done to more closely resemble real life communication where simple verbal language might be used by a communication partner. Gestures such as thumbs up/down and facial expression were the main means of communication used to demonstrate tasks and provide feedback throughout the intervention.
For each task, a participant was provided with two demonstrations then instructed to take their turn. The success criterion for each task was set at 90% (consistent with other cognitive interventions such as ATP, Sohlberg & Mateer, 1987). If a participant failed to achieve 90% on the first attempt, a standardised protocol of additional support was followed (see Appendix C for an example for object matching). The exact nature of the additional support depended on the particular task. In some cases, the success criterion was reduced to 51%, whilst for other tasks additional demonstrations were provided or the number of options to select from was systematically reduced. Once a participant had been provided with additional support, they were given up to five further attempts to reach the threshold score before the task was abandoned. If this occurred, a participant moved on to the next task in the hierarchical order. Allowing participants to move on despite not reaching task criterion is unusual in cognitive and language intervention studies but it facilitated participants being able to complete the programme. Completion of the programme enabled authors to analyse the theoretical rigour of the hierarchical order of tasks and alleviated participant boredom.
The intervention was delivered by the first author (a speech and language therapist with expertise in the management of severe and global aphasia and aphasia interventions) three times a week for up to 6 weeks (18 sessions in total). Sessions were completed in the participants’ place of residence. Total number of sessions was dependent on participants’ progression through the task hierarchy and the individual participant's attention and fatigue levels. Participants who could tolerate longer sessions, for example 45 min, and/or complete tasks at first attempt without need for additional support, would complete the intervention programme in fewer sessions than those who could only tolerate short sessions, for example 20 min, and/or required additional support for tasks.
Data analysis
For each case, statistical analysis of the ASHA‐FACS was performed using a Wilcoxon signed‐ranks test to determine whether there was a statistically significant median increase in CI or QC rating after intervention. A ≥ 10% increase in ASHA‐FACS rating score and/or a change in ASHA‐FACS descriptive category was deemed clinically significant. This was based on rehabilitation literature on the minimally important difference or minimally clinically important difference (Van der Lee et al., 2001) and findings from other studies that have used the ASHA‐FACS as an outcome measure (e.g. Hoover et al., 2017).
Weighted statistics (WEST; Howard et al., 2015) were used to measure effects of treatment on non‐verbal cognitive tasks and on the control task. In line with Howard et al. (2015), WEST Compare Level of performance (WEST‐COL) was used where there was a stable baseline, to assess whether there was a statistically significant improvement in performance accuracy after intervention. Alternatively, when baseline testing showed instability or improvement, WEST‐Rate of Change (WEST‐ROC) was used to assess whether there was a significantly greater amount of change or improvement after intervention compared to baseline. Analysis of raw scores was used to determine the direction of this change. When WEST statistics identified a significant change in the direction of a treatment effect, generalisation to untreated items was investigated. This was conducted by comparing scores for treated and untreated items using an independent samples t test.
Finally, the McNemar Test was used to measure the effect of intervention on performance on the auditory comprehension sub‐test of the AST (Whurr, 2011), and on the RCPM (Raven et al., 1990).
Statistical tests of significance were completed using Statistical Package for Social Sciences version 22 (IBM Corp., 2013) with alpha set at 0.05. In keeping with aphasia intervention studies such as Best et al. (2013) and Croot et al (2015), one‐tailed significance tests were completed to test directional hypotheses for skills directly linked to the intervention and expected to benefit/improve (functional communication, object‐to‐picture matching, gesture‐to‐picture matching, sound‐to‐picture matching and picture categorisation). More conservative two‐tailed significance tests were completed to test non‐directional hypotheses for skills indirectly linked to the intervention (non‐verbal problem solving, auditory comprehension, single word repetition).
Results
Participants completed the intervention within nine sessions on average (range 5–15 sessions). Session duration averaged 36 min each (range 17–54 min). Only one participant (Ruby) did not complete the intervention programme within the maximum 18 sessions.
Functional communication
The intervention led to improvements in functional communication as measured by a proxy with the ASHA‐FACS (Frattali et al., 1995). Five participants made clinically significant gains in ASHA‐FACS CI after intervention (see Table 4), improving by 0.6 points (10%) or more. Gains were most notably demonstrated in the CI sub‐category of communication of basic needs. For four of the five participants, the improvements were also statistically significant and resulted in a change in ASHA‐FACS descriptive category (Bernard z = −2.979 p = 0.015, one‐tailed; Alan z = −1.876 p = 0.031, one‐tailed; Henry z = −3.833 p < 0.0001, one‐tailed; Kevin, z = −2.684 p = 0.0035, one‐tailed). Furthermore, for these four participants, gains made were maintained at follow up (Bernard z = −2.787 p = 0.0025, one‐tailed; Alan z = −3.098 p = 0.001, one‐tailed; Henry z = −4.741 p < 0.001, one‐tailed; Kevin z = −1.795, p = 0.035, one‐tailed).
TABLE 4.
ASHA‐FACS communication independence (CI) raw scores and results of statistical testing.
| Overall communication independence | ASHA‐FACS CI subcategory | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Social communication | Communication of basic needs | Reading, writing & number concepts | Daily planning | ||||||||||||||
| Pa | B | P | M | B to P comparison | B to M comparison | B | P | M | B | P | M | B | P | M | B | P | M |
| Be | 2.2 | 3.1 | 2.8 | z = −2.979 p = 0.015 * | z = −2.787 p = 0.0025 * | 2.1 | 3.1 | 2.6 | 3.3 | 5.8 | 5 | 1.7 | 1.6 | 1.75 | 1.75 | 1.75 | 1.8 |
| Pe | 2.3 | 2.9 | 2.7 | z = −1.415 p = 0.079 | z = −1.512 p = 0.0655 | 2.65 | 2.8 | 2.9 | 4.6 | 5.4 | 5.4 | 1 | 1.25 | 1 | 1 | 2 | 1.6 |
| A | 1.65 | 2.4 | 2.9 | z = ‐1.876 p = 0.031 * | z = ‐3.098 p = 0.001 * | 2.3 | 2.3 | 3 | 1.9 | 4.7 | 5.3 | 1 | 1.4 | 1.6 | 1.4 | 1 | 1.6 |
| R | 1.4 | 1.2 | 1.1 | z = −1.841 p = 0.96 | z = −1.89 p = 0.097 | 1.2 | 1 | 1 | 2.2 | 1.9 | 1.2 | 1 | 1 | 1 | 1 | 1 | 1 |
| H | 2.3 | 3.9 | 4.3 | z = −3.833 p < 0.0001 * | z = −4.741 p < 0.001 * | 2.1 | 3.95 | 4.6 | 3.7 | 5.2 | 6 | 2.1 | 3.3 | 4.1 | 1.4 | 3 | 5.6 |
| K | 1.25 | 2.4 | 2 | z = −2.684 p = 0.0035 * | z = −1.795, p = 0.035 * | 2 | 2.3 | 2.4 | 3 | 4.6 | 3.6 | 1 | 1.2 | 1 | 1 | 1.4 | 1.2 |
Abbreviations: A, Alan; B, baseline; Be, Bernard; H, Henry; K, Kevin; M, maintenance; P, post intervention; Pa, participant; Pe, Peter; R, Ruby. CI scores range from 1 (The client does not perform behaviours even with maximal assistance and prompting) to 7 (The client does perform the communication behaviour, needing no assistance and/or prompting).
= statistically significant improvement. Bold indicates clinically significant improvements.
Four of five participants made clinically significant gains in ASHA‐FACS QC after intervention (see Table 5), improving by 0.4 points (10%) or more in QC sub‐categories of adequacy, appropriateness, promptness, and communication sharing. For three of the four participants, gains were statistically significant (Alan z = −2.863 p = 0.002, one‐tailed; Henry z = −3.358 p = 0.0005, one‐tailed; Kevin z = −3.000 p = 0.002, one‐tailed) and maintained at follow up (Alan z = −2.707 p = 0.0035, one‐tailed; Henry z = −3.115 p = 0.001, one tailed; Kevin z = −2.111 p = 0.018, one‐tailed). For Bernard, improvement immediately after intervention approached significance (z = −1.633 p = 0.051, one‐tailed) and at maintenance reached significance (z = −3 p = 0.0015, one‐tailed). Peter had also made statistically significant gains by maintenance (z = −1.732 p = 0.042, one‐tailed) despite no significant improvement immediately after intervention.
TABLE 5.
ASHA‐FACS qualitative communication (QC) raw scores and results of statistical testing.
| Overall qualitative communication | ASHA‐FACS QC domain | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adequacy | Appropriateness | Promptness | Communication sharing | ||||||||||||||
| Pa | B | P | M | B to P comparison | B to M comparison | B | P | M | B | P | M | B | P | M | B | P | M |
| Be | 2.2 | 2.6 | 2.8 | z = −1.633 p = 0.051 | z = −3 p = 0.0015 * | 2 | 2.5 | 2.75 | 2.25 | 2.5 | 3 | 2 | 2.5 | 2.75 | 2.5 | 3 | 3.5 |
| Pe | 2.3 | 2.4 | 2.5 | z = −0.577 p = 0.282 | z = −1.732 p = 0.042 * | 2.5 | 2.25 | 2.5 | 2.3 | 2.5 | 2.75 | 2 | 2.23 | 2.25 | 2.5 | 2.5 | 2.5 |
| A | 1.57 | 2.75 | 2.7 | z = −2.863 p = 0.002 * | z = −2.707 p = 0.0035 * | 1.8 | 2.5 | 2.5 | 1.5 | 2.75 | 2.75 | 1.5 | 2.75 | 3 | 1.25 | 2.75 | 2.5 |
| R | 1 | 1 | 1 | z = 0 p = 0.5 | z = 0 p = 0.5 | 1.25 | 1 | 1 | 1.25 | 1 | 1 | 1.25 | 1 | 1 | 1 | 1 | 1 |
| H | 2.13 | 3.25 | 3.6 | z = −3.358 p = 0.0005 * | z = −3.115 p = 0.001 * | 2.5 | 3.75 | 3.5 | 2 | 3.5 | 4 | 2 | 2.75 | 3.5 | 1 | 3 | 3.5 |
| K | 2 | 2.63 | 2.4 | z = −3.000 p = 0.002 * | z = −2.111 p = 0.018 * | 1.75 | 2.75 | 2.5 | 2 | 2.5 | 2.5 | 1.75 | 2.25 | 2.25 | 2.5 | 3 | 2.5 |
Abbreviations: A, Alan; B, baseline; Be, Bernard; H, Henry; K, Kevin; M, maintenance; P, post intervention; Pa, participant; Pe, Peter; R, Ruby.
QC scores range from 1 (The Client's communication is never adequate/relevant/prompt, Partner carries all of the communication burden) to 5 (Client's communication is always adequate/relevant/prompt, Client and partner share equally in communication).
= statistically significant improvement. Bold indicates clinically significant improvement.
Non‐verbal cognition
All participants made statistically significant improvements in at least one of the four cognitive measures targeting skills treated in the intervention (object‐to‐picture matching, gesture‐to‐picture matching, sound‐to‐picture matching, picture categorisation) and demonstrated generalisation to untreated items (Table 6).
TABLE 6.
Results of statistical testing for non‐verbal cognitive measures.
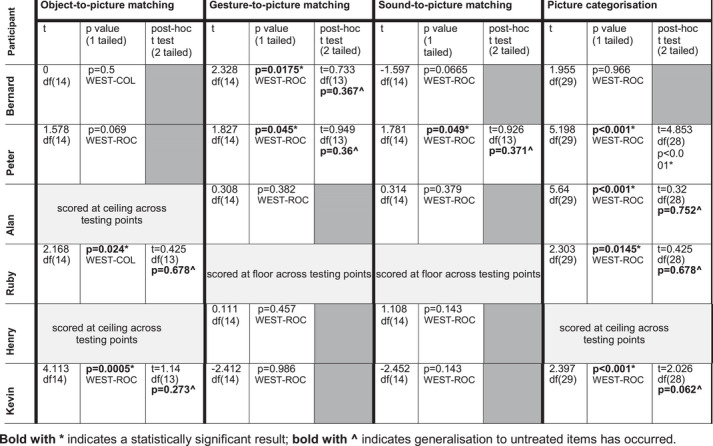
|
Visual perceptual skills as measured by object‐to‐picture matching improved for two participants, Ruby and Kevin (Ruby t(14) = 2.168 p = 0.024, one‐tailed; Kevin t(14) = 4.113 p = 0.0005, one‐tailed), with generalisation to untreated items observed (see Table 6).
Two participants (Bernard and Peter) made statistically significant improvements in non‐verbal visual semantics as measured by gesture‐to‐picture matching (Bernard t(14) = 2.328 p = 0.0175, one‐tailed; Peter t(14) = 1.827 p = 0.045 one‐tailed) with generalisation to untreated items observed.
Auditory semantics as measured by sound‐to‐picture matching improved for one participant (Peter t(14) = 1.781 p = 0.049, one‐tailed) with generalisation to untreated items observed.
Four participants (Peter, Alan, Ruby, Kevin) made statistically significant improvements in non‐verbal visual semantics as measured by picture categorisation (Peter (t(29) = 5.198 p < 0.001, one‐tailed; Alan t(29) = 5.64, p < 0.001, one‐tailed; Ruby t(29) = 2.303 p = 0.0145 one‐tailed; Kevin t(29) = 2.397 p < 0.001, one‐tailed). For three of the four (Alan, Ruby and Kevin) there was generalisation of improvement to untreated items.
The McNemar Test conducted on RCPM scores showed statistically significant changes for two participants (Bernard p = 0.002, two tailed; Henry p = 0.002, two‐tailed). Inspection of scores shows improvement in non‐verbal reasoning, with Bernard's score increasing from 4/36 to 14/36 after intervention and Henry's from 20/36 to 31/36 (Table 7).
TABLE 7.
Raw scores and results of statistical testing for non‐verbal reasoning as measured by the RCPM.
|
B n = 36 |
P n = 36 |
McNemar p value (two tailed) | |
|---|---|---|---|
| Bernard | 4 | 14 | p = 0.002 * |
| Peter | 3 | 7 | p = 0.216 n.s |
| Alan | 27 | 28 | p = 1 n.s |
| Ruby | 0 | 0 | n/a |
| Henry | 20 | 31 | p = 0.002 * |
| Kevin | 1 | 7 | p = 0.7 n.s. |
Abbreviations: B, baseline; P, post intervention; RCPM, Raven's Coloured Progressive Matrices.
*Statistically significant result n.s. indicates a non‐significant result.
Auditory comprehension
Two participants, Bernard and Peter, made statistically significant improvements in auditory comprehension as measured by the AST (Whurr, 2011), thus demonstrating indirect improvements in language skills (Table 8). Bernard's score increased from 2/40 to 11/40 (p = 0.002 two‐tailed) and Peter's from 0/40 to 9/40 (p = 0.004 two‐tailed).
TABLE 8.
Raw scores and results of statistical testing for auditory comprehension as measured by AST.
| Participant |
B n = 40 |
P n = 40 |
McNemar p value (two tailed) |
|---|---|---|---|
| Bernard | 2 | 11 | p = 0.002 * |
| Peter | 0 | 9 | p = 0.004 * |
| Alan | 12 | 11 | p = 1 n.s |
| Ruby | 0 | 0 | n/a n.s |
| Henry | 10 | 10 | p = 1 n.s |
| Kevin | 4 | 3 | p = 1 n.s |
Abbreviations: AST, Aphasia Screening Test; B, baseline; P, post intervention.
*Indicates a statistically significant result n.s. indicates a non‐significant result.
Control task
Three participants (Bernard, Peter and Ruby) were unable to perform the spoken word repetition control task at any testing occasion. Those that completed the task (Alan, Henry and Kevin) showed baseline instability (Table 9). As a result, WEST‐ROC was used to determine whether there was a significant difference in the amount of change over the baseline testing period compared with after intervention. Results indicate no significant difference for Alan and Henry, but a statistically significant difference was found for Kevin (t(15) = 3.36, p = 0.008 (two tailed)). Kevin therefore showed improvement in single word repetition after intervention, scoring 7/16, 3/16, 3/16 at baseline (mean 4.3), and 8/16 at both post intervention and maintenance.
TABLE 9.
Raw scores and results of statistical testing for spoken word repetition as measured by the CAT (control task).
|
B1 n = 32 |
B2 n = 32 |
B3 n = 32 |
P n = 32 |
M n = 32 |
Statistic | t |
p value (two tailed) |
|
|---|---|---|---|---|---|---|---|---|
| Bernard | 0 | 0 | 0 | 0 | 0 | n/a | n/a | n/a |
| Peter | 0 | 0 | 0 | 0 | 0 | n/a | n/a | n/a |
| Alan | 2 | 4 | 4 | 4 | 4 | WEST‐ROC | 0.696 df (15) | p = 0.994 |
| Ruby | 0 | 0 | 0 | 0 | 0 | n/a | n/a | n/a |
| Henry | 5 | 7 | 7 | 4 | 5 | WEST‐ROC | −1.809 df(15) | p = 0.182 |
| Kevin | 7 | 3 | 3 | 8 | 8 | WEST‐ROC | 3.36 df(15) | p = 0.008* |
Abbreviations: B, baseline; P, post intervention; M, maintenance.
* = statistically significant result.
Discussion
Few intervention studies have explored functional communication gains in PwGA and this is the first study to do so in the context of investigating the impact of a cognitive intervention. Results show that a non‐linguistic cognitive intervention, delivered at a dose replicable in clinical practice (three times weekly for up to 6 weeks), led to statistically significant improvements in functional communication for four of six PwGA, and clinically significant functional communication improvements for five of six. The functional communication gains seen on the ASHA‐FACS were in communication of basic needs, adequacy, appropriateness, promptness and communication sharing, and were maintained 3 months after intervention. Statistically significant improvements in visual perception and non‐verbal semantics were also noted for some participants. Specifically, these were improvements in sound to picture matching (one participant), gesture‐to‐picture and object to picture matching (two participants), and picture categorisation (four participants). Generalisation to untreated items was observed in all but one case (Peter made a statistically significant improvement in picture categorisation after intervention but this did not generalise to untreated items). Statistically significant gains in non‐verbal reasoning were made by two participants, as measured by RCPM, and there were also indirect linguistic gains in auditory comprehension for two participants.
To ensure this intervention was accessible and acceptable for people with the most severe cognitive and communication deficits, there was flexibility in session duration depending on client tolerance. Whilst sessions ranged from 17 to 54 min, the order of tasks and intervention procedure, including supports, was consistent for all participants. There is no obvious link between results and session duration. For example, Alan who tolerated the longest sessions (40–54 min) completed the intervention in five sessions and improved in both domains of the ASHA‐FACS immediately after intervention. However, so did Henry, who tolerated sessions of only 25–30 min and required 11 sessions to complete the intervention. Kevin also improved in both domains of the ASHA‐FACS immediately after intervention with a similar session duration tolerance to Henry, but he required 15 sessions to complete the intervention.
The results of this study provide new insights into global aphasia. All six PwGA involved in this study had severe cognitive deficits alongside their severe language and communication impairments. This aligns with studies that report the presence of severe cognitive deficits in some with the condition (Marinelli et al., 2017; Olsson et al., 2019; van Mourik et al., 1992). However, despite this, they were able to participate in and make positive gains after a non‐intensive dose of intervention that focused on non‐linguistic cognitive tasks. The study was based on the premise that treating cognitive deficits may improve functional communication. Previous studies have concluded that relatively spared cognition is required to benefit from SLT or that PwGA with profound cognitive deficits cannot benefit from direct intervention (van Mourik et al., 1992). However, this study has found otherwise, demonstrating that the cognitive skills of some PwGA can be developed or enhanced through direct therapy which in turn can lead to improvements in functional communication.
The findings here support a link between cognition and functional communication but, in contrast to studies of milder aphasia which emphasise the importance of executive functioning and cognitive flexibility for successful functional communication (Chiou & Kennedy, 2009; Purdy, 2002), this study suggests that attention, visual perceptual and non‐verbal semantic skills may underpin basic functional communication, and thus treating them is particularly relevant in global aphasia. The findings support those of other studies of severe aphasia in which semantics have played a significant role in outcomes (Hogrefe et al., 2012).
Despite the intervention being mediated through non‐linguistic tasks, two participants made statistically significant gains in language (auditory comprehension) consistent with findings from VAT (Helm‐Estabrooks et al., 1982). This provides support for non‐linguistic interventions positively impacting skills that may underpin language and specifically auditory comprehension.
Clinical implications
Contrary to much existing literature, this study has found that PwGA can make functional communication gains after a relatively low dose of intervention (an average of nine sessions of 36 min duration three times a week). Improvements were observed in participants who were on average 2.5 years post onset. This suggests the prognosis for global aphasia can be more favourable than many have documented and there are implications for commissioning and managing SLT services. Services must ensure that PwGA are not only offered intervention in the immediate months after their stroke, but also can also access and re‐access services further down the line. Gains documented in attention, visual perception, semantics and functional communication after receiving this non‐linguistic intervention may result in PwGA being able to access and respond positively to typical language‐based SLT interventions. This intervention may also enable PwGA to better access other aspects of rehabilitation such as occupational therapy and physiotherapy. Clinicians may however require training in delivering non‐linguistic cognitive interventions and there are implications for pre‐registration SLT training also.
Given the limited availability of functional communication measures suitable for use in global aphasia, findings suggest the ASHA‐FACS (Frattali et al., 1995; revised 2017) is an appropriate option for measuring gains in basic communication behaviours relevant to this population. Although participants’ scores on the ASHA‐FACS remained relatively low after intervention, small improvements in the skills measured such as communication of basic needs and communication sharing (burden of communication on the communication partner), are highly clinically significant. Such improvements can have a positive impact on everyday life of both PwGA and their loved ones.
Limitations and future directions
This was an exploratory study of a novel intervention. The preliminary findings are promising but require cautious interpretation due to the small sample size and some aspects of the methodology.
There are multiple components to the intervention including non‐verbal delivery, non‐linguistic stimuli, 16 tasks and a range of targeted skills. Further research is required to determine the key ingredients of the intervention and the underlying mechanism of change by manipulating components such as the number and order of tasks in the intervention programme, progression through the programme and the use of spoken language within sessions. As a case series study involves repeated assessments, it is possible that learning effects could have influenced findings. However, to mitigate for this the non‐verbal semantic tasks used as secondary outcome measures all assessed untreated and unrepeated items. The use of WEST‐ROC statistics also mitigated for this as it measures whether any change or improvement after intervention was statistically significantly greater than any change or improvement at baseline.
The use of a proxy measure in the form of the ASHA‐FACS (Frattali et al., 1995) introduces the possibility of bias, but as discussed earlier no direct functional communication measure appropriate for global aphasia exists. In this study proxies were provided with training to maximise the likelihood of them using the ASHA‐FACS (Frattali et al., 1995) rating scales as intended by the authors, and in the same way as each other. In order to move away from proxy measures for this client group, there is a need to fully understand the interactional competencies and challenges they face in their everyday communication contexts and conversations, ascertain which communication behaviours might be objectively assessed and develop direct functional communication measures capable of capturing changes in these behaviours.
Cautious interpretation of results is also required due to issues with the control task. Ideally, a control task should be one which participants can complete but is not subject to change because of the intervention. Due to the breadth of communicative and cognitive deficits PwGA can present with, finding a task that they could successfully complete was challenging. This was further compounded by the fact that this intervention targeted a range of skills with direct and indirect changes possible in many areas. A follow‐up study in the form of a multi‐site feasibility study with a larger sample size and use of a control group would provide more robust evidence that the changes observed here are directly linked to the intervention. A feasibility study would also enable exploration of acceptability, cost effectiveness and viability for delivery within NHS services.
A carer‐focused outcome measure was not used as part of this study. Given the burden that severe communication deficits can place on significant others, future studies should seek to understand whether there are positive implications for the communication experience and quality of life of friends, relatives and paid carers.
Conclusion
This study has shown that a novel non‐linguistic cognitive intervention can improve functional communication and non‐verbal cognition in PwGA. The findings suggest that this client group can make functional gains in the communication of basic needs, and in adequacy, appropriateness and promptness of communication. Participants were able to do so with a relatively low dose of intervention and maintain these gains after intervention ceased. The intervention also led to a reduction in the burden of communication for communication partners as measured by ASHA‐FACS qualitative communication. These preliminary findings offer an encouraging narrative on prognosis in global aphasia and show promise for the development of better SLT services for individuals and families affected by this severe and neglected condition.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflicts of interest.
ACKNOWLEDGEMENTS
This work formed part of the first author's PhD studies at University College London. The authors thank the participants and their families for their time and engagement with the study. This research did not receive any specific grant from funding agencies in the public, commercial or not‐for‐profit sectors.
APPENDIX A. Tidier (Template for intervention description and replication) checklist (Hoffmann et al., 2014).
| 1. | Name | Non‐linguistic cognitive intervention for people with global aphasia (see Adjei‐Nicol, 2020) |
| 2. | Why | Cognition is important for successful functional communication. People with global aphasia have limited language skills and have responded positively to non‐linguistic interventions such as Visual Action Therapy (Helm‐Estabrooks et al., 1982) but it is unclear if cognitive or non‐linguistic interventions can improve functional communication skills. |
| 3. | What | Computer and paper‐based non‐linguistic tasks (16 in total) targeting attention, visual perception, non‐verbal visual and auditory semantics. |
| 4. | Procedures | Hierarchical programme of tasks followed (see Appendix B) |
| 5. | Who provided | Speech and language therapist |
| 6. | How | Individual in‐person sessions |
| 7. | Where | Participant's own home |
| 8. | When and how much | Three times weekly for up to 6‐weeks depending on how quickly participants progressed through the intervention programme (see Tailoring). |
| 9 | Tailoring | Intervention duration was dependent on the rate of participant's progression through the hierarchical intervention programme (consisting of 16 tasks). Step‐down tasks and/or additional demonstrations were provided if required. Treatment session duration varied between 20 and 45 min depending on participants’ tolerance and fatigue levels on a given day. |
| 10 | Modifications | No modifications were made during the study |
| 11 | How well (planned) |
Intervention manual was developed and followed. Intervention fidelity was not assessed |
| 12 | How well (actual) | N/A |
APPENDIX B. Description of intervention tasks and aims.
| Task | Aim |
|---|---|
| 1. Visual trackinga | To visually track a target moving across a computer screen |
| 2. Shift gaze with no competing target* | To focus eye gaze on a target then disengage and shift gaze to a different target as original disappears |
| 3. Shift gaze with a competing targeta | To focus eye gaze on a target then disengage and shift gaze to look at a different target, while original target remains |
| 4. Visual sustained attentiona | To maintain focus and detect an unpredictably occurring visual stimulus |
| 5. Auditory sustained attentiona | To maintain focus and detect an unpredictably occurring auditory stimulus |
| 6. Object matching | To match identical objects. |
| 7. Visual selective attentiona | To discretely respond to a target picture and ignore distractors |
| 8. Object to non‐ identical picture matching | To match an object to a pictorially represented different exemplar |
| 9. Gesture to picture matching | To match an iconic gesture to an object picture |
| 10. Match two connected pictures | To point to one picture from an array that is semantically related to the target |
| 11. Picture categorisation | To sort pictures according to their category |
| 12. Match environmental sound to pictures | To match an environmental sound to an object |
| 13. Odd one out | To point to the item that is not semantically related to others from an array |
| 14. Complete the category | To point to the picture (from a choice of two) that belongs to the same semantic category as pictured targets |
| 15. Choose and collect a similar item | To collect different (non‐identical) pictured exemplars of a target item a large array |
| 16. Choose and collect items in the same category | To collect pictures of items belonging to the same superordinate category as a target from an array containing semantic and unrelated distractors |
aComputer‐based task.
APPENDIX C. Example of task modification and support.
| Task | Modifications and support |
|---|---|
| 6. Object matching |
Aim: For participant to correctly match two identical objects from an array of five. Items: Twelve pairs of identical objects: two demonstration items (fork, comb); five pairs for practice set one (glass, pen, key, toothbrush, spoon) and five pairs for practice set two (apple, stamp, mug, coin scissors). Demonstration: Five items are laid in a horizontal row in front of the participant, two demonstration items and three randomly selected from the remaining items. The researcher then takes one demonstration object (e.g. fork) from the duplicate set and moves it across the five items exaggerating non‐verbally through head gesture and facial expression, the objects it does not match with before placing it next to the object it matches. The demonstration is repeated with the second demonstration object (comb) before the participant takes a turn. Procedure: The five set one objects are laid out. The participant is handed one object from the duplicate set at a time for matching. Each time an object is correctly matched, these two matched objects are removed and replaced with any randomly selected object from the set two or demonstration items. After all five set one items have been completed, the task is repeated with set two. A score of 1 is given for each correctly matched item, The maximum score is 10. |
| Task modifications |
At the end of the task if the participant scored 9/10 or more, they progress to the next task in the hierarchy (Task 7. Visual selective attention). If the participant scores 8/10 or less, the task is repeated but with a decreased array of four items using any four objects from each set. The task is demonstrated again. The maximum score possible is 8. If the participant scores above 50% (5/8 or more) they step‐up and repeat the task with two sets of five items. If they score 4/8 or less, the number of items in the array is reduced again, this time to two (any two objects from each set). The task is demonstrated again. The maximum score is four. If the participant scores 3/4 or more they step‐up and repeat the task with two sets of four items. If they score 2/4 or less they complete step‐down practice tasks outlined below. |
|
Step‐down practice tasks (matching colours and shapes) |
Aim: For the participant to match two identical colour cards from a choice of two followed by two identical shape cards from a choice of two. Items: Two sets of coloured square cards (red, blue), two sets of shape cards (circle, triangle), all black. Demonstration: The researcher demonstrates matching the colour cards. One red and one blue card is placed in a horizontal row, the researcher picks one card from the duplicate set (e.g. red) and uses exaggerated nonverbal gesture and facial expression to indicate that it does not match with the blue and places the card down next to the corresponding red card. The researcher then removes the matched cards, reverses the layout of the cards on the table and completes the demonstration with the alternative colour. This is immediately followed by an identical demonstration using shape cards. Procedure: The participant completes the task with the same colours and shapes that have been used in the demonstration. The participant must match red/blue twice (with positions reversed), followed by circle/triangle twice (again with positions reversed). The maximum score is 8. If the participant scores 5/8 or higher on the step‐down practice tasks they return to the main task (Task 6. Object matching) starting with a choice of 2, then stepping up to a choice of 4 if they meet the threshold score, and further stepping up to a choice of 5 if they meet the threshold score. If the participant scores 4/8 or lower, the step‐down practice tasks are repeated up to 5 additional times to enable the participant to score 5/8 or above, thus returning to the main task. If they fail to do so after 5 additional attempts, the practice tasks are abandoned, and the participant moves on to the next task in the hierarchy. (Task 7. Visual selective attention). |
Adjei‐Nicol, S. , Sacchett, C. & Beeke, S. (2025) Evaluating the effect of a non‐linguistic cognitive intervention on functional communication in global aphasia: a case series study. International Journal of Language & Communication Disorders, 60, e13155. 10.1111/1460-6984.13155
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are openly available in UCL Discovery https://discovery.ucl.ac.uk, reference 10107050.
REFERENCES
- Adjei‐Nicol, S. (2023) Working with global aphasia: theory and practice. Oxon: Routledge. [Google Scholar]
- Adjei‐Nicol, S.K. (2020) An investigation into the effect of a novel non‐linguistic cognitive intervention on functional communication in global aphasia. [Doctoral thesis, UCL (University College London)]. UCL Discovery Available: https://discovery.ucl.ac.uk/id/eprint/10107050/[accessed 01 April 2024]
- Best, W. , Greenwood, A. , Grassly, J. , Herbert, R. , Hickin, J. & Howard, D. (2013) Aphasia rehabilitation: does generalisation from anomia therapy occur and is it predictable? A case series study. Cortex; A Journal Devoted to the Study of the Nervous System and Behavior, 49, 2345–2357. [DOI] [PubMed] [Google Scholar]
- Chiou, H.S. & Kennedy, M.R.T. (2009) Switching in adults with aphasia. Aphasiology, 23(7–8), 1065–1075 [Google Scholar]
- Collins, M. (1986) Diagnosis and treatment of global aphasia. London: Taylor & Francis. [Google Scholar]
- Croot, K. , Taylor, C. , Abel, S. , Jones, K. , Krein, L. , Hameister, I. , Ruggero, L. & Nickels, L. (2015) Measuring gains in connected speech following treatment for word retrieval: a study with two participants with primary progressive aphasia. Aphasiology, 29(11), 1265–1288. [Google Scholar]
- Denes, G. , Perazzolo, C. , Piani, A. & Piccione, F. (1996) Intensive versus regular speech therapy in global aphasia: a controlled study. Aphasiology, 10(4), 385–394. [Google Scholar]
- El Hachioui, H. , Visch‐Brink, E.G. , Lingsma, H.F. , Van De Sandt‐Koenderman, M.W.M.E. , Dippel, D.W.J. , Koudstaal, P.J. & Middelkoop, H.A.M. (2014) Non‐linguistic cognitive impairment in poststroke aphasia: a prospective study. Neurorehabilitation and Neural Repair, 28(3), 273–281. [DOI] [PubMed] [Google Scholar]
- Frattali, C.M. , Thompson, C.K. , Holland, A. , Wohl, C.B. & Ferketic, M.M. (1995) American speech‐language hearing association functional assessment of communication (ASHA‐FACS). Rockville: American Speech‐Language Hearing Association. [Google Scholar]
- Frattali, C.M. , Thompson, C.K. , Holland, A. , Wohl, C.B. , Wenck, C.J. , Slater, S.C. & Paul, D. (2017) American speech‐language hearing association functional assessment of communication skills for adults (ASHA‐FACS). Rockville: American Speech‐Language Hearing Association. [Google Scholar]
- Fridriksson, J. , Nettles, C. , Davis, M. , Morrow, L. & Montgomery, A. (2006) Functional communication and executive function in aphasia. Clinical Linguistics & Phonetics, 20(6), 401–410. [DOI] [PubMed] [Google Scholar]
- Helm‐Estabrooks, N. (2002) Cognition and aphasia: a discussion and a study. Journal of Communication Disorders, 35, 171–186. [DOI] [PubMed] [Google Scholar]
- Helm‐Estabrooks, N. , Connor, L. & Albert, M. (2000) Treating attention to improve auditory comprehension in aphasia. Brain and Language, 74(1), 469–472. [Google Scholar]
- Helm‐Estabrooks, N. , Fitzpatrick, P.M. & Barresi, B. (1982) Visual Action Therapy for Global Aphasia. Journal of Speech and Hearing Disorders, 47(4), 385–389. [DOI] [PubMed] [Google Scholar]
- Hilari, K. & Dipper, L. (2020) The scenario test (validated in the UK). Havant: J & R Press. [Google Scholar]
- Ho, K.M. , Weiss, S.J. , Garrett, K.L. & Lloyd, L.L. (2005) The effect of remnant and pictographic books on the communicative interaction of individuals with global aphasia. Augmentative and Alternative Communication, 21(3), 218–232. [Google Scholar]
- Hoffmann, T. , Glasziou, P. , Boutron, I. , Milne, R. , Perera, R. , Moher, D. , Altman, D. , Barbour, V. , Macdonald, H. , Johnston, M. , Lamb, S. , Dixon‐Woods, M. , Mcculloch, P. , Wyatt, J. , Chan, A. & Michie, S. (2014) Better reporting of interventions: template for intervention description and replication (TIDieR) checklist and guide. Bmj, 348, g1687. [DOI] [PubMed] [Google Scholar]
- Hogrefe, K. , Ziegler, W. , Weidinger, N. & Goldenberg, G. (2012) Non‐verbal communication in severe aphasia: influence of aphasia, apraxia or semantic processing? Cortex; A Journal Devoted to the Study of the Nervous System and Behavior, 48, 952–962. [DOI] [PubMed] [Google Scholar]
- Hoover, E.L. , Caplan, D.N. , Waters, G.S. & Carney, A. (2017) Communication and quality of life outcomes from an interprofessional intensive, comprehensive, aphasia program (ICAP). Topics in Stroke Rehabilitation, 24(2), 82–90. [DOI] [PubMed] [Google Scholar]
- Howard, D. , Best, W. & Nickels, L. (2015) Optimising the design of intervention studies: critiques and ways forward. Aphasiology, 29(5), 526–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard, D. & Patterson, K. (1992) The pyramids and palm trees test: a test of semantic access from words and pictures. Suffolk: Thames Valley Test Company. [Google Scholar]
- IBM Corp . (2013) SPSS Statistics for Windows. Armonk, New York: IBM Corp. [Google Scholar]
- Kertesz, A. (2006) Western aphasia battery revised. San Antonio: Pearson. [Google Scholar]
- Kongs, S.K. , Thompson, L.L. , Iverson, G.L. & Heaton, R.K. (2000) Wisconsin card sorting test‐64 card version. Florida: Par Inc. [Google Scholar]
- Manochiopinig, S. , Sheard, C. & Reed, V.A. (1992) Pragmatic assessment in adult aphasia: a clinical review. Aphasiology, 6(6), 519–533. [Google Scholar]
- Marinelli, C.V. , Spaccavento, S. , Craca, A. , Marangolo, P. & Angelelli, P. (2017) Different cognitive profiles of patients with severe aphasia. Behavioural Neurology, 2017, 1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mental capacity act . (2005) [online] Available: https://www.legislation.gov.uk/ukpga/2005/9/pdfs/ukpga_20050009_en.pdf [accessed 01 April 2024]
- Munro, P. & Siyambalapitiya, S. (2016) Improved word comprehension in global aphasia using a modified semantic feature analysis treatment. Clinical Linguistics & Phonetics, 31(2), 119–136. [DOI] [PubMed] [Google Scholar]
- Olsson, C. , Arvidsson, P. & Blom Johansson, M. (2019) Relations between executive function, language, and functional communication in severe aphasia. Aphasiology, 33(7), 821–845. [Google Scholar]
- Porch, B.E. (1967) Porch index of communicative ability. California: Consulting Psychologists Press. [Google Scholar]
- Purdy, M. (2002) Executive function ability in persons with aphasia. Aphasiology, 16(4–6), 549–557 [Google Scholar]
- Raven, J.C. , Court, J.H. & Raven, J. (1990) Raven's coloured progressive matrices. Oxford: Oxford Psychology Press. [Google Scholar]
- Salis, C. & Edwards, S. (2015) What is effective in the treatment of global aphasia? RCSLT Bulletin , April, 20–21.
- Snodgrass, J.G. & Vanderwart, M. (1980) A standardized set of 260 pictures : norms for name agreement, image agreement, familiarity, and visual complexity, Journal of experimental psychology. Human Learning and Memory, 6(2), 174–215. [DOI] [PubMed] [Google Scholar]
- Sohlberg, M.M. & Mateer, C.A. (1987) Effectiveness of an attention‐training program. Journal of Clinical and Experimental Neuropsychology, 9(2), 117–130. [DOI] [PubMed] [Google Scholar]
- Swinburn, K. , Porter, G. & Howard, D. (2004) CAT: comprehensive aphasia test. Hove: Psychology Press. [Google Scholar]
- Van der Lee, J.H. , De Groot, V. , Beckerman, H. , Wagenaar, R.C., Lankhorst, G.J. & Bouter, L.M. (2001) The intra‐ and interrater reliability of the action research arm test: a practical test of upper extremity function in patients with stroke. Archives of Physical Medicine and Rehabilitation, 82(1), 14–19. [DOI] [PubMed] [Google Scholar]
- Van Der Meulen, I. , Van De Sandt‐Koenderman W.M.E., Duivenvoorden H.J. & Ribbers G.M. (2010) Measuring verbal and non‐verbal communication in aphasia: reliability, validity, and sensitivity to change of the Scenario Test. International Journal of Language and Communication Disorders, 45(4), 424–435. [DOI] [PubMed] [Google Scholar]
- Van Mourik, M. , Verschaeve, M. , Boon, P. & Paquier, P. (1992) Cognition in global aphasia: indicators for therapy. Aphasiology, 6(5), 491–499. [Google Scholar]
- Van Overschelde, J.P. , Rawson, K.A. & Dunlosky, J. (2004) Category norms: an updated and expanded version of the Battig and Montague (1969) norms. Journal of Memory and Language, 50, 289–335. [Google Scholar]
- Whurr, R. (2011) Aphasia screening test: a multi‐dimensional assessment procedure for adults with acquired aphasia (3rd ed). Milton Keynes: Speechmark Publishing. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are openly available in UCL Discovery https://discovery.ucl.ac.uk, reference 10107050.


