Abstract
Engineering of the influenza A virus NS1 protein became an attractive approach to the development of influenza vaccine vectors since it can tolerate large inserts of foreign proteins. However, influenza virus vectors expressing long foreign sequences from the NS1 open reading frame (ORF) are usually replication deficient in animals due to the abrogation of their NS1 protein function. In this study, we describe a bicistronic expression strategy based on the insertion of an overlapping UAAUG stop-start codon cassette into the NS gene, allowing the reinitiation of translation of a foreign sequence. Although the expression level of green fluorescent protein (GFP) from the newly created reading frame was significantly lower than that obtained previously from an influenza virus vector expressing GFP from the NS1 ORF, the bicistronic vector appeared to be replication competent in mice and showed outstanding genetic stability. All viral isolates derived from mouse lungs at 10 days postinfection were still capable of expressing GFP in infected cells. Utilizing this bicistronic approach, we constructed another recombinant influenza virus, allowing the secretion of biologically active human interleukin-2 (IL-2). Although this virus also replicated to high titers in mouse lungs, it did not display any mortality rate in infected animals, in contrast to control viruses. Moreover, the IL-2-expressing virus showed an enhanced CD8+ response to viral antigens in mice after a single intranasal immunization. These results indicate that influenza viruses could be engineered for the expression of biologically active molecules such as cytokines for immune modulation purposes.
The generation of viral vectors for the delivery of foreign proteins and biologically active molecules remains an attractive approach for gene therapy, the treatment of cancer, and the prevention of infectious diseases. Since reverse genetic methods were developed, influenza viruses have also been considered potential vaccine vectors (7, 8, 10, 28, 29, 33, 34). Recently, cold-adapted intranasal influenza vaccines have been licensed for children and adults (4, 13). In theory, the viral strains comprising the live influenza vaccine could be further modified for the delivery and expression of additional proteins. In contrast to other vectors such as adenoviruses or retroviruses, influenza virus does not form a DNA intermediate during its replication cycle and is not able to integrate into the host's chromosomes, making it attractive in terms of safety. There are several options for how to manipulate the influenza virus genome, depending on the desired aims and possibilities, to produce recombinant viruses. These strategies include the insertion of foreign proteins into the surface glycoproteins NA and HA (24, 29), the creation of additional genomic fragments (10, 34), and the manipulation of the nonstructural NS1 protein (8, 33).
The influenza virus NS1 protein has several advantages as a target for engineering since it does not presumably interfere with the structure of the virions but is synthesized in large quantities in infected cells and tolerates long insertions of up to several hundred nucleotides. Additionally, because NS1 is not incorporated into virions, alterations of this protein would not change the antigenicity of the influenza virus itself. Furthermore, the attenuation mechanism of the currently used cold-adapted influenza vaccine is not based on the NS gene, implying the ability to integrate the recombinant NS gene into live influenza virus vaccine strains (15). Despite these advantages, due to the intracellular localization of NS1, the development of the immune response to the NS1 protein or to the proteins fused to NS1 is limited mainly to the induction of CD8+ T-cell immunity (7, 33). Obviously, for the induction of a B-cell response or for the expression of biologically active molecules, efficient delivery of the recombinant protein to the cell surface is required. This could be achieved by constructing an additional reading frame within the NS gene and by supplementation of the foreign proteins with secretory signal sequences. Several approaches have been used to create bicistronic mRNAs for influenza viruses, including the incorporation of an internal ribosome entry site element (11) and a doubling of influenza virus promoter sequences (20). For the present work, we exploited a simple bicistronic strategy analogous to the influenza B virus M gene (14) in order to create an additional reading frame within the NS gene of influenza A virus. The stop-start cassette UAAUG was inserted into the influenza A virus NS1 coding sequence corresponding to amino acid (aa) position 125, followed by the insertion of the green fluorescent protein (GFP) sequence. As expected, the expression of GFP by this virus was diminished compared to that by a previously obtained vector (NS1-GFP) which expresses GFP from the NS1 reading frame (16). Nevertheless, in contrast to the latter vector, the bicistronic expression vector could replicate to high titers in mouse lungs without losing its ability to express the foreign sequence. We concluded that bicistronic influenza virus NS vectors could be suitable for the expression of biologically active molecules such as cytokines, which are effective even in small quantities. To prove this hypothesis, we created an influenza virus expressing human interleukin-2 (IL-2) by using the described bicistronic approach. We demonstrated that this virus could stably express biologically active IL-2 in various cells and in vivo, creating a prominent immunomodulatory effect in mice.
MATERIALS AND METHODS
Viruses and cells.
The Vero, MDCK, and CTLL2 cell lines originated from the American Type Culture Collection. Vero cells were adapted to and further cultivated in Dulbecco's modified Eagle's medium (DMEM)/Ham's F12 medium (Biochrom F4815) with 4 mM l-glutamine and protein-free supplement (proprietary formulation; Polymun Scientific GmbH, Austria). MDCK cells were cultivated in DMEM/Ham's F12 medium containing 2% heat-inactivated fetal calf serum (HyClone SH30071) and 4 mM l-glutamine. The IL-2-dependent T-cell line CTLL2 was grown in RPMI 1640 medium supplemented with 10% fetal calf serum, 8 mM l-glutamine, 1 mM sodium pyruvate, 25 μM 2-mercaptoethanol, and 20 U/ml recombinant human IL-2 (Proleukin, Chiron, CA). Influenza virus mutants A/PR8/NS1-125 (NS1-125) and A/PR8/NS1-125GFP (NS1-GFP) were obtained in Vero cells by using a previously described transfection protocol (6, 16). All viruses were grown and titrated in Vero cells at 37°C by a limiting dilution assay.
Generation of transfectant viruses.
Plasmid pPolI-NS HDV (30), containing the NS gene of influenza virus A/PR/8/34 (H1N1) between the polymerase I (Pol I) promoter and the hepatitis delta virus (HDV) terminator, was opened at nucleotide position 400 of NS using inverse PCR, and a stop-start pentanucleotide cassette (TAATG) was introduced. The coding sequence of either GFP (Quantum's SuperGlo GFP) or IL-2 (PCR extracted from the cDNA derived from human peripheral blood monocytes) was blunt end cloned downstream of the stop-start cassette, and the plasmids were designated pPol-NS1-125GFPStSt-HDV and pPol-NS1-125IL2StSt-HDV, respectively. Viruses were rescued using a previously described protocol (16). In brief, Vero cells were cotransfected with plasmids expressing the viral RNA of the recombinant NS gene in addition to the RNP proteins of influenza virus A/PR/8/34 and subsequently infected with the interferon-sensitive helper virus delNS1. Using recombinant alpha interferon (IFN-α) as a selection pressure, a pure recombinant virus expressing either GFP or IL-2 was obtained after several rounds of plaque purification and designated A/PR8/NS1-125GFPStSt (NS1-GFPStSt) or A/PR8/NS1-125IL2StSt (NS1-IL2StSt), respectively. The correct sequence was confirmed by nucleotide sequence analysis.
Animal studies.
To test viral replication, 4- to 6-week-old B6D2F1/Crl mice were infected intranasally (i.n.) with 2 × 105 PFU/animal of the virus under narcosis. On days 2, 4, 6, 8, 10, and 12, mice were sacrificed and their lungs were aseptically removed. A 10% tissue extract in phosphate-buffered saline was prepared by grinding the tissue samples with a rotor homogenizer. The suspension was centrifuged at 2,000 × g for 5 min, and the viral yield of the supernatants was determined by a limiting-dilution assay using Vero cells. For enzyme-linked immunospot (ELISPOT) assays, mice were infected with 2 × 103 PFU/animal without narcosis. On day 10, spleens were aseptically removed and ELISPOT was performed as described below.
Cytometric bead array.
Vero cells were infected with NS1-IL2StSt or NS1-GFPStSt as a negative control (multiplicity of infection [MOI] = 1) and incubated at 37°C for 24 h. Supernatants were harvested and analyzed for the presence of IL-2 using a cytometric bead array human TH1/TH2 cytokine kit (BD Bioscience) according to the manufacturer's instruction manual.
Cell proliferation assay.
CTLL2 cells were plated at a concentration of 1 × 104 cells/well into a 96-well plate. An IL-2 standard (Proleukin, Chiron, CA) or the supernatant from infected Vero cells, as described above, was added to the cells in descending concentrations, and the cells were incubated for 72 h at 37°C. An MTT [3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (Sigma)] colorimetric assay was performed using 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (Sigma) (22), and the concentration of active IL-2 in the infected cell supernatant was determined using a standard calibration curve.
Enzyme-linked immunosorbent assay.
A modified enzyme-linked immunosorbent assay was performed (7) Briefly, sucrose-purified and UV-inactivated PR8 wild-type virus (adjusted to 20 hemagglutination units/well in carbonate buffer [pH 9.6]) was used as a coating antigen. Serial dilutions of pooled sera in phosphate-buffered saline containing 1% skim milk (Serva) were added to the coated plates, and the mixtures were incubated for 1.5 h at room temperature. Bound antibodies were detected with goat anti-mouse immunoglobulin G1 (IgG1), IgG2a, or IgA conjugated with horseradish peroxidase (Zymed). Plates were stained with TMB (Sigma) as a substrate, and the absorbance was measured (wavelength, 450 nm). The cutoff value was defined as the mean value of absorption of negative control sera plus 2 standard deviations.
ELISPOT assay.
A protocol for an immediate ex vivo CD8+ IFN-γ-specific ELISPOT assay (31) was adapted utilizing the synthetic peptide A/PR/8/34 NP147-155 (NP peptide TYQRTRALV), an H-2Kd-restricted immunodominant cytotoxic T lymphocyte epitope of the influenza A virus nucleoprotein (23). Briefly, twofold serial dilutions of cell populations derived from murine spleens were transferred to wells coated with an anti-IFN-γ monoclonal antibody (MAb; R4-6A2; BD PharMingen). The cells were incubated for 24 h at 37°C and 5% CO2 in DMEM containing 10% fetal calf serum, IL-2 (30 U/ml), penicillin, streptomycin, and 50 μM 2-mercaptoethanol in the presence of synthetic peptides. A biotinylated anti-IFN-γ MAb (XMG1.2; BD PharMingen) was utilized as a conjugate antibody, followed by incubation of the plates with streptavidin peroxidase (0.25 U/ml; Boehringer Mannheim Biochemica). Spots representing IFN-γ-secreting CD8+ cells were developed utilizing the substrate 3-amino-9-ethylcarbazole (Sigma) containing hydrogen peroxide in 0.1 M sodium acetate, pH 5.0. The spots were counted with the help of a dissecting microscope, and the results were expressed as mean numbers of IFN-γ-secreting cells ± standard errors of the means for triplicate cultures from two independent experiments. Cells incubated in the absence of synthetic peptides developed <15 spots/106 cells. Since the depletion of CD8+ cells usually resulted in a 92% reduction in spot formation, cell separation was omitted from most assays (data not shown).
RESULTS
Rescue of recombinant influenza viruses.
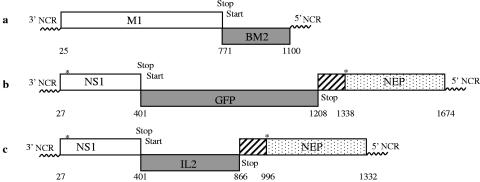
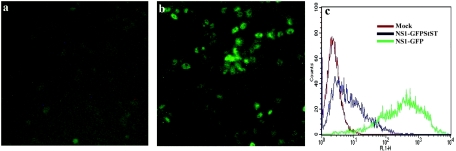
Influenza B virus uses a unique strategy to encode one of its proteins. The BM2 gene, located on segment 7 of influenza B virus, is expressed by a coupled translational termination-reinitiation mechanism (Fig. 1a). The initiation codon of the BM2 gene overlaps the termination codon of the upstream gene for the M1 protein, forming a stop-start pentanucleotide (UAAUG). Utilizing this strategy, we first constructed a recombinant influenza virus in which the stop codon of the stop-start cassette terminates the translation of NS1 after 125 aa and the start codon reinitiates the translation of GFP (Fig. 1b). This virus was rescued in Vero cells by use of our previously developed transfection system and was designated A/PR8/NS1-GFPStSt (NS1-GFPStSt) (16). As demonstrated by confocal microscopy and fluorescence-activated cell sorting analysis (Fig. 2), the NS1-GFPStSt virus was able to express GFP in infected Vero cells (MOI = 1) at 24 h postinfection (p.i.), although the level of fluorescence was approximately 100 times lower than that of the previously published NS1-GFP virus, in which GFP is expressed from the NS1 open reading frame (ORF) (16).
FIG. 1.
Schematic structures of recombinant NS genes. (a) Genetic organization of influenza B virus BM2 gene. (b and c) Structures of influenza A virus NS genes expressing GFP (b) and IL-2 (c). Hatched boxes represent nontranslated parts. Asterisks indicate splicing signals of NEP.
FIG. 2.
GFP expression levels. Vero cells were infected at an MOI of 1 with the NS1-GFPStSt (a) or NS1-GFP (b) virus, in which GFP is fused to NS1 and posttranslationally cleaved. At 24 h postinfection, fluorescence was analyzed using confocal microscopy (a and b) or FACS (c).
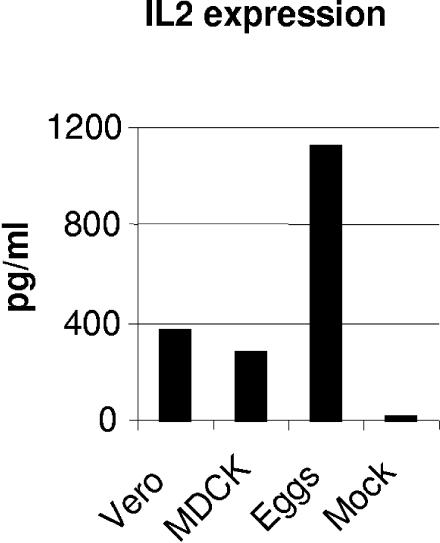
Using the same strategy, we constructed an influenza virus vector expressing human IL-2 instead of GFP, designated A/PR8/NS1-IL2StSt (NS1-IL2StSt) (Fig. 1c). In order to estimate the expression level of IL-2, Vero or MDCK cells or eggs were infected with NS1-IL2StSt at an MOI of 1 or with 2 × 105 PFU, respectively, and supernatants or allantoic fluids were analyzed at 48 h postinfection. Production levels of up to 1,100 pg/ml for eggs and 250 to 350 pg/ml for cell culture were detected using a cytometric bead array kit (BD Bioscience) (Fig. 3). In addition, the supernatant of infected Vero cells was also analyzed for the biological activity of IL-2. The growth of the CTLL2 detector cell line, which is only able to proliferate in the presence of IL-2, was measured using an MTT test. Approximately 5 IU/ml was detected in the supernatant of infected cells, confirming that biologically active IL-2 was secreted from the infected cells.
FIG. 3.
IL-2 expression rates. Vero or MDCK cells were infected with NS1-IL2StSt at an MOI of 1 and incubated for 48 h. Ten-day-old embryonated chicken eggs were infected with 2 × 105 PFU of NS1-IL2StSt and harvested at 2 days postinfection. Supernatants were analyzed for the presence of IL-2 antigen using a cytometric bead array human TH1/TH2 cytokine kit.
Properties of rescued viruses.
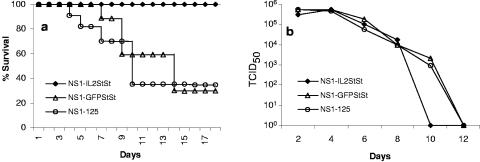
Both the NS1-GFPStSt and NS1-IL2StSt viruses replicated with titers of up to 7 to 8 log in Vero and MDCK cells. To check the genetic stability of the viruses, both viruses were passaged five times on Vero or MDCK cells at an MOI of approximately 0.1. The last passage was analyzed for the expression of GFP or IL-2. Both viruses were still capable of expressing the inserted protein. The replication of NS1-GFPStSt and NS1-IL2StSt in mice was compared with that of the NS1-125 control virus, which does not contain any insert and in which the translation of NS1 is terminated after 125 aa. Mice were infected with 2 × 105 PFU/animal of the indicated virus under narcosis. During the first 8 days postinfection, no difference in viral titer was observed in mouse lungs (Fig. 4). However, at 10 days p.i., mice had cleared the NS1-IL2StSt virus, whereas viruses NS1-GFPStSt and NS1-125 were still replicating, with complete viral clearance only on day 12. Additionally, the survival of infected mice was monitored for 18 days. All mice infected with NS1-IL2StSt survived, whereas approximately 70% of mice infected with NS1-GFPStSt or NS1-125 died (Fig. 4).
FIG. 4.
Viral replication and survival rates in mice. B6D2F1/Crl mice were infected i.n. under narcosis with 2 × 105 PFU/animal of either NS1-IL2StSt, NS1-GFPStSt, or NS1-125. Mouse survival was monitored for 18 days (a). (b) On days 2, 4, 6, 8, 10, and 12, viruses in mouse lungs were titrated using a limiting dilution assay on Vero cells. Titers (TCID50) are shown as geometric means.
The hallmark of the viruses constructed using the stop-start approach seems to be their outstanding genetic stability. Even at 10 days p.i., the viral isolates derived from lung homogenates infected with NS1-GFPStSt formed only fluorescent plaques in tissue. Similarly, the IL-2 vector retained its capacity to express biologically active IL-2 after 8 days of replication in mouse lungs (data not shown).
Immune response in mice.
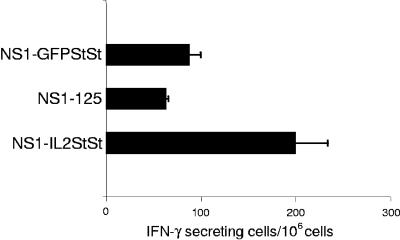
Since it is known that IL-2 could have immune adjuvant activity, we tested the immunogenicity of the recombinant viruses in mice. Mice were infected with NS1-IL2StSt, NS1-GFPStSt, or NS1-125 at different viral concentrations ranging from 2 × 105 to 2 × 101 PFU/animal under narcosis. At 21 days p.i., mouse serum samples were analyzed for the presence of influenza virus-specific antibodies. We found that irrespective of the virus used, neither the 50% infective doses nor the maximum hemagglutination inhibition titers were significantly different, reflecting the equal levels of viral replication in mouse respiratory organs. The determination of the IgG1/IgG2A isotype profile of induced antibodies also did not reveal any differences in the polarization of the immune response (data not shown). To investigate whether the expression of IL-2 stimulates the virus-specific T-cell response, 4- to 6-week-old B6D2F1/Crl mice were primed i.n. in the absence of anesthesia with NS1-125, NS1-GFPStSt, or NS1-IL2StSt (2 × 103 PFU/animal). The NP peptide-specific CD8+ T-cell response was assessed at 10 days postinfection by an ELISPOT assay. A marked increase in the frequency of IFN-γ-secreting CD8+ T cells was determined for mice immunized with the IL-2-expressing NS1-IL2StSt virus (200 ± 34 spots) compared with those for groups of mice immunized with the NS1-125 (64 ± 2 spots) and NS1-GFPStSt (88 ± 11 spots) viruses (Fig. 5).
FIG. 5.
CD8+ primary responses. Three mice per group were immunized once i.n. in the absence of anesthesia with 2 × 103 PFU/animal of the influenza virus NS1-IL2StSt, NS1-GFPStSt, or NS1-125, as indicated. At 10 days postinfection, a single-cell suspension obtained from the spleens of the mice was assessed for NP peptide-specific IFN-γ-secreting CD8+ T cells in an ELISPOT assay. The data shown are the mean numbers of antigen-specific IFN-γ-secreting cells ± standard errors of the means for triplicate cultures from two independent experiments.
DISCUSSION
Influenza viruses are now considered potential viral vectors for mucosal immunization against a variety of infectious diseases and also for cancer treatment (3, 8, 33). However, since influenza virus has a relatively small genome, there are several technical problems with obtaining recombinant influenza virus vectors, including their genetic instability and an unpredictable level of attenuation. Due to the high mutational rate of the RNA genome, influenza viruses can easily eliminate nonessential sequences within several cycles of replication. Although it has been shown that influenza A virus can tolerate large insertions of foreign sequences into the NS gene, the incorporation of the 275-aa GFP into the NS1 ORF resulted in a replication-deficient phenotype in mice, restricting the practical value of such vectors (16). Moreover, influenza virus vectors expressing GFP or other long sequences as fusion peptides with a truncated NS1 protein appeared to be genetically stable only in interferon-deficient Vero cells and not in interferon-competent cells such as MDCK cells, where the inserted foreign sequences were partially knocked out after several rounds of replication (data not shown). Obviously, an interaction with the added sequences seems to affect the functional activity of the N-terminal 125 amino acids of the NS1 protein, which was shown to be one of the main determinants of viral resistance to the interferon system. We tried to circumvent those limitations by constructing a bicistronic NS1 gene expressing foreign sequences from a separate reading frame inserted after aa position 125. For that purpose, we chose a strategy whereby an overlapping stop-start codon was inserted, analogous to the compact genetic organization of the influenza B virus BM2 gene. Using this approach, we first rescued a virus expressing GFP as a separate product and compared its fluorescence capacity with that of a previously obtained virus expressing GFP from the NS1 ORF. Because ribosomes preferentially initiate translation from the AUG codon closest to the 5′ end of the mRNA (17), the bicistronic construct had a reduced level of fluorescence. Nevertheless, it appeared to be completely genetically stable and was able to replicate to high titers in mouse respiratory organs, causing a moderate mortality rate. Interestingly, even after 10 days of replication in mouse lungs, all viral isolates were capable of expressing GFP. The genetic stability of the NS1-GFPStSt virus was also confirmed by multiple passages in MDCK cells.
Another advantage of bicistronic approaches is that the foreign proteins, supplemented with a foreign leader sequence or containing their own, could be expressed and secreted from infected cells. Therefore, these methods could be suitable for the expression of surface glycoproteins and biologically active molecules such as cytokines. Since the expression levels of foreign proteins from the stop-start codon inserted in the middle of the NS1 gene were relatively low, the expression of biologically active molecules rather than foreign antigens seems to be more feasible. Therefore, we tested the possibility of expressing human IL-2 as a model for the construction of influenza virus vectors expressing various cytokines.
IL-2 is an immunomodulatory, T-cell-derived molecule which is required for the clonal expansion of antigen-activated T cells. The secretion of IL-2 by CD4+ T lymphocytes has multiple biologic effects, such as the induction of proliferation of T-helper and T-killer cells and the stimulation of T cells to produce other cytokines such as IFN-γ and IL-4. Furthermore, IL-2 can also activate B cells, NK cells, and macrophages (5). When IL-2 is expressed from recombinant viruses infecting nonlymphoid cells, its secretion could dramatically change the pathogenesis of viral infection and modify the immune response. As shown with several viral vectors, including vaccinia virus (9, 32), adenovirus (18), and herpes simplex virus type 1 (12), the expression of IL-2 usually results in a less virulent phenotype in animal models. It is also known that IL-2 acts as an immune adjuvant. Encouraging results were obtained with mice when IL-2 was coadministered with a liposome-based influenza vaccine, resulting in an increased antibody titer and the induction of better heterosubtypic protective immunity (1, 2).
Thus, we constructed an influenza virus expressing IL-2 analogous to the NS1-GFPStSt virus. This virus replicated to high titers in Vero and MDCK cells and in embryonated chicken eggs, and biologically active IL-2 was detected in tissue culture supernatants and even in allantoic fluids, proving that it was exported outside the cells. Moreover, this virus was completely stable when replicating in Vero or MDCK cells or in mouse respiratory organs, as confirmed by a functional IL-2 assay. Despite its high replication capacity in mouse lungs, the IL-2 vector was not lethal in mice, presumably due to the accelerated clearance of viral infection. Since a dramatic drop in virus replication in mice was not detected earlier than day 8, its fast clearance most likely could be explained by the fast mobilization of the specific immune response rather than the effect of natural killer cell activation. As a matter of fact, mice infected with the IL-2-expressing influenza virus showed increased T-cell responses compared to mice infected with control viruses. It should be mentioned that human IL-2 and murine IL-2 have a homology of approximately 65% and that human IL-2 also stimulates the proliferation of mouse T cells at similar concentrations to those of murine IL-2 (27). However, we did not find any significant differences in either the antibody titer against hemagglutinin or the polarization of the immune response in mice infected with NS1-IL2StSt compared to mice infected with the control viruses. All tested viruses stimulated a high antibody response and similar ratios of IgG1 and IgG2A isotypes in infected mice (data not shown), reflecting their comparably good replication in mouse respiratory tissues.
One application for the IL-2-expressing influenza virus could be the development of a vaccine with improved immunogenicity, especially for an aged population. It is known that with increasing age, the antigen-stimulated synthesis of IL-2, and therefore the T-cell-mediated immune response, decreases. In consequence, the currently used influenza vaccine has a much lower efficiency in the elderly than in healthy young adults (25, 26). Therefore, attempts have been made to improve the immunogenicity of influenza vaccines, especially in the elderly, by supplementation with recombinant IL-2 (21). In our experiments, the IL-2-expressing influenza virus showed an increased T-cell response already in 6-week-old mice, and therefore we would expect an even more prominent effect in elderly mice; this is currently being investigated.
Another application of this virus could be the treatment of malignant tumors. It was shown that recombinant IL-2 could be effective for the treatment of patients with melanomas or kidney cancer (19). The problems with intravenously administered IL-2 are its short half-life and its cytotoxicity, possibly resulting in severe side effects. Viral vectors in this respect provide the possibility for the local expression of cytokines at the site of tumor growth. Although viruses by themselves, including influenza virus (3), could have oncolytic properties, the most encouraging results were obtained with viral vectors expressing IL-2, IL-12, and other cytokines which were injected directly into the tumor, providing a local boost of the immune response against tumor antigens (18). Hence, the oncolytic properties of the NS1-IL2StSt virus are currently under closer investigation.
Acknowledgments
This work was financed by Polymun Scientific, Immunbiologische Forschung GmbH, Vienna, Austria.
REFERENCES
- 1.Babai, I., Y. Barenholz, Z. Zakay-Rones, E. Greenbaum, S. Samira, I. Hayon, M. Rochman, and E. Kedar. 2001. A novel liposomal influenza vaccine (INFLUSOME-VAC) containing hemagglutinin-neuraminidase and IL-2 or GM-CSF induces protective anti-neuraminidase antibodies cross-reacting with a wide spectrum of influenza A viral strains. Vaccine 20:505-515. [DOI] [PubMed] [Google Scholar]
- 2.Babai, I., S. Samira, Y. Barenholz, Z. Zakay-Rones, and E. Kedar. 1999. A novel influenza subunit vaccine composed of liposome-encapsulated haemagglutinin/neuraminidase and IL-2 or GM-CSF. II. Induction of TH1 and TH2 responses in mice. Vaccine 17:1239-1250. [DOI] [PubMed] [Google Scholar]
- 3.Bergmann, M., I. Romirer, M. Sachet, R. Fleischhacker, A. Garcia-Sastre, P. Palese, K. Wolff, H. Pehamberger, R. Jakesz, and T. Muster. 2001. A genetically engineered influenza A virus with Ras-dependent oncolytic properties. Cancer Res. 61:8188-8193. [PubMed] [Google Scholar]
- 4.Cox, R. J., K. A. Brokstad, and P. Ogra. 2004. Influenza virus: immunity and vaccination strategies. Comparison of the immune response to inactivated and live, attenuated influenza vaccines. Scand. J. Immunol. 59:1-15. [DOI] [PubMed] [Google Scholar]
- 5.Dela Cruz, J. S., T. H. Huang, M. L. Penichet, and S. L. Morrison. 2004. Antibody-cytokine fusion proteins: innovative weapons in the war against cancer. Clin. Exp. Med. 4:57-64. [DOI] [PubMed] [Google Scholar]
- 6.Egorov, A., S. Brandt, S. Sereinig, J. Romanova, B. Ferko, D. Katinger, A. Grassauer, G. Alexandrova, H. Katinger, and T. Muster. 1998. Transfectant influenza A viruses with long deletions in the NS1 protein grow efficiently in Vero cells. J. Virol. 72:6437-6441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ferko, B., D. Katinger, A. Grassauer, A. Egorov, J. Romanova, B. Niebler, H. Katinger, and T. Muster. 1998. Chimeric influenza virus replicating predominantly in the murine upper respiratory tract induces local immune responses against human immunodeficiency virus type 1 in the genital tract. J. Infect. Dis. 178:1359-1368. [DOI] [PubMed] [Google Scholar]
- 8.Ferko, B., J. Stasakova, S. Sereinig, J. Romanova, D. Katinger, B. Niebler, H. Katinger, and A. Egorov. 2001. Hyperattenuated recombinant influenza A virus nonstructural-protein-encoding vectors induce human immunodeficiency virus type 1 Nef-specific systemic and mucosal immune responses in mice. J. Virol. 75:8899-8908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flexner, C., A. Hugin, and B. Moss. 1987. Prevention of vaccinia virus infection in immunodeficient mice by vector-directed IL-2 expression. Nature 330:259-262. [DOI] [PubMed] [Google Scholar]
- 10.Flick, R., and G. Hobom. 1999. Transient bicistronic vRNA segments for indirect selection of recombinant influenza viruses. Virology 262:93-103. [DOI] [PubMed] [Google Scholar]
- 11.Garcia-Sastre, A., T. Muster, W. S. Barclay, N. Percy, and P. Palese. 1994. Use of a mammalian internal ribosomal entry site element for expression of a foreign protein by a transfectant influenza virus. J. Virol. 68:6254-6261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ghiasi, H., Y. Osorio, G. C. Perng, A. B. Nesburn, and S. L. Wechsler. 2001. Recombinant herpes simplex virus type 1 expressing murine interleukin-4 is less virulent than wild-type virus in mice. J. Virol. 75:9029-9036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glueck, R. 2001. Review of intranasal influenza vaccine. Adv. Drug Deliv. Rev. 51:203-211. [DOI] [PubMed] [Google Scholar]
- 14.Horvath, C. M., M. A. Williams, and R. A. Lamb. 1990. Eukaryotic coupled translation of tandem cistrons: identification of the influenza B virus BM2 polypeptide. EMBO J. 9:2639-2647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jin, H., B. Lu, H. Zhou, C. Ma, J. Zhao, C. F. Yang, G. Kemble, and H. Greenberg. 2003. Multiple amino acid residues confer temperature sensitivity to human influenza virus vaccine strains (FluMist) derived from cold-adapted A/Ann Arbor/6/60. Virology 306:18-24. [DOI] [PubMed] [Google Scholar]
- 16.Kittel, C., S. Sereinig, B. Ferko, J. Stasakova, J. Romanova, A. Wolkerstorfer, H. Katinger, and A. Egorov. 2004. Rescue of influenza virus expressing GFP from the NS1 reading frame. Virology 324:67-73. [DOI] [PubMed] [Google Scholar]
- 17.Kozak, M. 1999. Initiation of translation in prokaryotes and eukaryotes. Gene 234:187-208. [DOI] [PubMed] [Google Scholar]
- 18.Liu, M., B. Acres, J. M. Balloul, N. Bizouarne, S. Paul, P. Slos, and P. Squiban. 2004. Gene-based vaccines and immunotherapeutics. Proc. Natl. Acad. Sci. USA 101:14567-14571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.MacFarlane, M. P., J. C. Yang, A. S. Guleria, R. L. White, Jr., C. A. Seipp, J. H. Einhorn, D. E. White, and S. A. Rosenberg. 1995. The hematologic toxicity of interleukin-2 in patients with metastatic melanoma and renal cell carcinoma. Cancer 75:1030-1037. [DOI] [PubMed] [Google Scholar]
- 20.Machado, A. V., N. Naffakh, S. van der Werf, and N. Escriou. 2003. Expression of a foreign gene by stable recombinant influenza viruses harboring a dicistronic genomic segment with an internal promoter. Virology 313:235-249. [DOI] [PubMed] [Google Scholar]
- 21.Mbawuike, I. N., P. R. Wyde, and P. M. Anderson. 1990. Enhancement of the protective efficacy of inactivated influenza A virus vaccine in aged mice by IL-2 liposomes. Vaccine 8:347-352. [DOI] [PubMed] [Google Scholar]
- 22.Mosmann, T. 1983. Rapid colorimetric assay for cellular growth and survival: application to proliferation and cytotoxicity assays. J. Immunol. Methods 65:55-63. [DOI] [PubMed] [Google Scholar]
- 23.Murata, K., A. Garcia-Sastre, M. Tsuji, M. Rodrigues, D. Rodriguez, J. R. Rodriguez, R. S. Nussenzweig, P. Palese, M. Esteban, and F. Zavala. 1996. Characterization of in vivo primary and secondary CD8+ T cell responses induced by recombinant influenza and vaccinia viruses. Cell Immunol. 173:96-107. [DOI] [PubMed] [Google Scholar]
- 24.Muster, T., R. Guinea, A. Trkola, M. Purtscher, A. Klima, F. Steindl, P. Palese, and H. Katinger. 1994. Cross-neutralizing activity against divergent human immunodeficiency virus type 1 isolates induced by the gp41 sequence ELDKWAS. J. Virol. 68:4031-4034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nichol, K. L., K. L. Margolis, J. Wuorenma, and T. Von Sternberg. 1994. The efficacy and cost effectiveness of vaccination against influenza among elderly persons living in the community. N. Engl. J. Med. 331:778-784. [DOI] [PubMed] [Google Scholar]
- 26.Nichol, K. L., J. Wuorenma, and T. von Sternberg. 1998. Benefits of influenza vaccination for low-, intermediate-, and high-risk senior citizens. Arch. Intern. Med. 158:1769-1776. [DOI] [PubMed] [Google Scholar]
- 27.Novak, T. J., P. M. White, and E. V. Rothenberg. 1990. Regulatory anatomy of the murine interleukin-2 gene. Nucleic Acids Res. 18:4523-4533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Palese, P., F. Zavala, T. Muster, R. S. Nussenzweig, and A. Garcia-Sastre. 1997. Development of novel influenza virus vaccines and vectors. J. Infect. Dis. 176(Suppl. 1):S45-S49. [DOI] [PubMed] [Google Scholar]
- 29.Percy, N., W. S. Barclay, A. Garcia-Sastre, and P. Palese. 1994. Expression of a foreign protein by influenza A virus. J. Virol. 68:4486-4492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Poomputsa, K., C. Kittel, A. Egorov, W. Ernst, and R. Grabherr. 2003. Generation of recombinant influenza virus using baculovirus delivery vector. J. Virol. Methods 110:111-114. [DOI] [PubMed] [Google Scholar]
- 31.Power, C. A., C. L. Grand, N. Ismail, N. C. Peters, D. P. Yurkowski, and P. A. Bretscher. 1999. A valid ELISPOT assay for enumeration of ex vivo, antigen-specific, IFNgamma-producing T cells. J. Immunol. Methods 227:99-107. [DOI] [PubMed] [Google Scholar]
- 32.Ramshaw, I. A., M. E. Andrew, S. M. Phillips, D. B. Boyle, and B. E. Coupar. 1987. Recovery of immunodeficient mice from a vaccinia virus/IL-2 recombinant infection. Nature 329:545-546. [DOI] [PubMed] [Google Scholar]
- 33.Takasuka, N., M. Enami, S. Itamura, and T. Takemori. 2002. Intranasal inoculation of a recombinant influenza virus containing exogenous nucleotides in the NS segment induces mucosal immune response against the exogenous gene product in mice. Vaccine 20:1579-1585. [DOI] [PubMed] [Google Scholar]
- 34.Watanabe, T., S. Watanabe, T. Noda, Y. Fujii, and Y. Kawaoka. 2003. Exploitation of nucleic acid packaging signals to generate a novel influenza virus-based vector stably expressing two foreign genes. J. Virol. 77:10575-10583. [DOI] [PMC free article] [PubMed] [Google Scholar]