Abstract
Background:
Pickleball is currently the fastest-growing sport in the United States, and participation has increased 3-fold throughout the study period.
Purpose/Hypothesis:
This study aimed to evaluate the epidemiology of pickleball-related injuries, detailing the descriptive data, injury patterns, and health care utilization at a single center over 6 years. It was hypothesized that there would be a substantial increase in pickleball-related injuries during the study period, particularly with increasing age, along with increased orthopaedic visits for pickleball-related injuries.
Study Design:
Case series; Level of evidence, 4.
Methods:
We systematically queried the Electronic Health Record System at a single institution from January 1, 2017, to December 31, 2022, to identify patients with injuries associated with pickleball participation. Data were collected on descriptive data, injury characteristics, and health care utilization.
Results:
Pickleball injuries were confirmed in 487 patients, accounting for a total of 618 injuries. Patient age ranged from 12 to 82 years (mean, 62 years), and 53% of injuries occurred in male patients. The number of injuries increased 6.8-fold from 2017 to 2022. Overall, soft tissue strain or rupture (n = 296; 47.9%) was the most common injury category, followed by arthritis-related pain (n = 62; 10%) and fracture (n = 57; 9.2%). However, age-stratified analysis revealed a shift toward fractures and arthritis-related pain in patients >60 years. Women were 2 times more likely to sustain fractures. Injuries to the rotator cuff were most commonly seen (n = 67, 11%), followed by those to the back (n = 48; 7.8%) and calf (n = 35; 5.6%). Most patients (n = 426; 87%) were initially evaluated by a nonorthopaedic provider, with orthopaedic/sports medicine providers seeing 63% of patients.
Conclusion:
Our institution observed a 6.8-fold increase in pickleball-related injuries from 2017 to 2022, which far outpaces the reported increase in pickleball participation nationally. Women >60 years were found to be at the highest risk of injury and were more likely to sustain fractures. Most injuries were musculoskeletal related, with soft tissue injury occurring most commonly in patients <60 years and fractures more commonly seen in patients >60 years.
Keywords: fracture, injury, muscle strain, pickleball, sports medicine
Pickleball has been the fastest-growing sport in the United States (US) for the past 5 years. 23 Since 2017, the number of pickleball players has increased 3-fold to an estimated 8.9 million players 17 in the US in 2022. In 2023 participation is expected to continue to increase with a projected 36.5 million people estimated to participate at least once. 20 While the sport's rapid expansion is particularly notable among the younger age groups, pickleball became known for its popularity among older age groups drawn to its cardiovascular benefits, accessibility, ease of learning, and adaptability across fitness/activity levels (smaller court sizes, less running, lower impact, etc). As opposed to other racket sports with relatively few older participants, one-third of pickleball players are ≥65 years. 2
Because of this remarkable rise in participation, there has been an increased interest in understanding the potential risks and economic impact associated with pickleball participation. While it is generally considered a low-impact sport, pickleball still involves twisting, jumping, lunging, pivoting, and shifting, which puts stress on the body and the joints and presents a risk of injury. Recent reports suggest that pickleball-related injuries are projected to cost Americans 500 million dollars in 2023, or nearly 10% of total unexpected medical costs in the US. 6
Despite the noteworthy increase in public attention, there remains a paucity of comprehensive epidemiological studies that systematically characterize the injury profile associated with the sport. To date, most existing research has primarily focused on specific injury types5,10,14,16 or mental health, 8 which limits the ability to draw conclusions about the overall risk profile of pickleball. Only 1 study to date conducted a survey of pickleball injuries; however, this study was limited to patients evaluated in emergency departments and was conducted before the rise in pickleball popularity. 24
In this study, we aimed to evaluate the epidemiology of pickleball-related injuries, detailing the descriptive data, injury patterns, and health care utilization at a single center over 6 years. We hypothesized that there would be a substantial increase in pickleball-related injuries, particularly with increasing age, along with increased orthopaedic visits for pickleball-related injuries.
Methods
We conducted a descriptive epidemiologic study of pickleball-related injuries at our institution (Vanderbilt University Medical Center) from January 1, 2017, to December 31, 2022. We used the Vanderbilt Research Derivative to systematically query the electronic health record (EHR) system for any mention of keywords “pickle,”“pickleball,” or “pickle ball.” Patient charts flagged by the search were then manually reviewed by 2 independent reviewers (S.D.H. and K.L.H.) and screened for inclusion. To capture the overall prevalence of orthopaedic injuries in pickleball and to present a full picture of the spectrum of pickleball illnesses, participants were eligible for inclusion if there was any documentation in their chart of evaluation by a medical professional for an injury or ailment identified in relation to a pickleball incident during the collection period. Patients were excluded if they did not have a pickleball-related injury event or if their injury occurred outside of the timeframe of the study. This study was deemed exempt from institutional review board approval.
Data were collected using a structured extraction form developed a priori. We collected information on patient characteristics; injury diagnosis, category, and location; injury evaluation location and timing; diagnostic testing; treatment/interventions; follow-up; and interaction with an orthopaedic specialist. Each chart was manually reviewed to ensure proper classification of injury events—including quantifying the presence of multiple injuries among patients (ie, single evaluation for multiple unique injuries, as well as independent evaluations for subsequent injuries) and to ensure proper classification of injury events (ie, avoid falsely duplicating/elevating injury counts in event of multiple follow-up visits associated with a single injury). If a single patient sustained multiple injuries, the first injury was defined as the injury at their initial evaluation. If a patient had multiple injuries at their initial evaluation, then each of the injuries was counted as a separate “first injury.” All injuries were defined as any unique injury sustained throughout the study period.
Data Management and Analysis
Study data were collected and managed using REDCap electronic data capture tools hosted at our institution.12,13
Statistical Analyses
All data analyses were performed in Stata 16.1 (StataCorp). Two-tailed chi-square tests were used to model differences in observed versus expected data for categorical variables (ie, year of injury). The 1-sample proportion test was used to compare observed versus expected results of categorical variables with only 2 categories (ie, sex), as the chi-square test has been known to underestimate P values in these scenarios. The 1-sample t test was used to model differences in observed versus expected results for continuous data (ie, age at injury). Linear regression was used to evaluate injury trends across the study (ie, mean age across study years). Linear regression with an indicator variable (injury or participation) was used to evaluate the difference in the rate of injury versus the rate of participation across the study period, with expected data based on national trends in pickleball participation as reported by the Association of Pickleball Players.1,20
Results
Overview
A total of 1846 patients had mention of “pickle,”“pickleball,” or “pickle ball” in their EHR, among whom 487 patients had confirmed pickleball-related injuries and 131 patients (21.2%) had multiple separate pickleball-related injuries, totaling 618 injuries. Among players with multiple injuries, 24 had 2 diagnoses associated with a single visit, while 107 had separate visits for pickleball-related injuries occurring at distinct events.
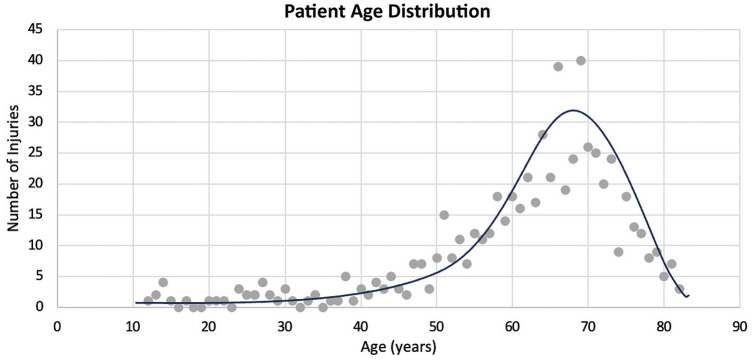
Age at Injury
Age at injury ranged from 12 to 82 years, with a median age of injury of 65 years (interquartile range, 57-70 years) and a strongly left-skewed distribution (Figure 1). The mean age at injury (62 ± 13.1 years) was significantly greater than the mean age of pickleball participants nationally (36 years1,20) (P < .001). The mean age of injury over the study period ranged from 59.9 (in 2022) to 65.1 (in 2019), and although linear regression revealed a statistically significant decrease in the age of injury of 1 year per study year (β = 0.99; P = .003), there was no significant difference in age across the study period (Appendix Table A1).
Figure 1.
Age of patients with pickleball-related injury diagnosis (N = 618) at Vanderbilt University Medical Center, 2017-2022.
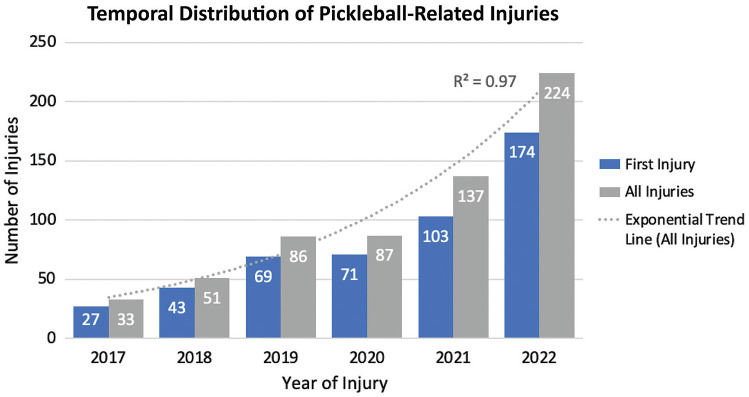
Pickleball Injuries During the Study Period
The number of pickleball injuries increased exponentially from 2017 to 2022 (y = 24.326e0.3586x; R2 = 0.97), with a 6.8-fold increase in injuries in 2022 as compared with 2017 (Figure 2). The rate of increase in injuries across this study was significantly greater than the rate of increase in participation in pickleball nationally from 2017 to 2022 (P = .002).
Figure 2.
Distribution of pickleball-related injuries from 2017 to 2022. The trend line for all injuries was fit with an exponential model across the study duration (y = 24.326e0.3586x; R2 = 0.97).
Injuries by Category
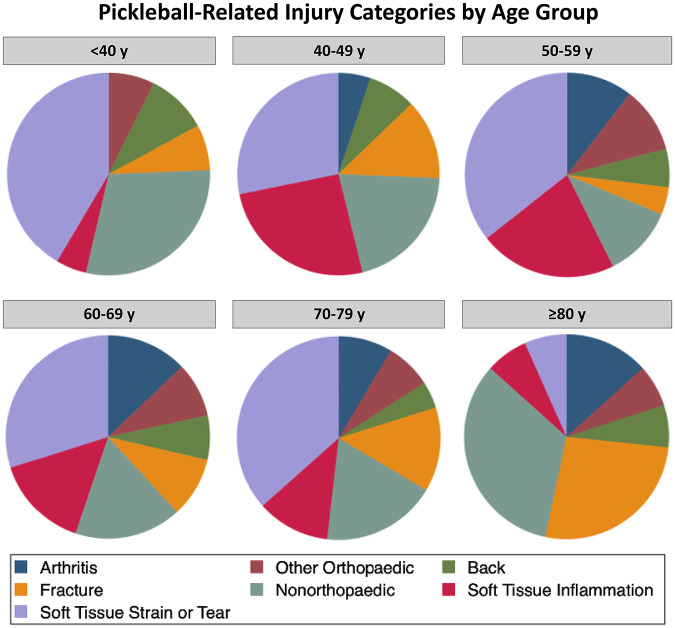
Injuries were divided into several categories as shown in Appendix Figure A1, with soft tissue strain or rupture (n = 296; 47.9%) being the most prevalent injury category. Overall, the most common diagnoses were injuries to the rotator cuff (n = 67; 10.8%), arthritis-related pain of any joint (n = 62; 10%), back pain/strain (n = 48; 7.8%), and calf strain or tear (n = 35; 5.7%) (Table 1). Among nonorthopaedic injuries, the most common injuries were cardiac-related chest pain/palpitations (n = 24; 3.9%) and facial lacerations (n = 15; 2.4%) (Table 1). There was no observable trend in nonorthopaedic injuries throughout the study period, indicating a relatively proportional increase in both orthopaedic and nonorthopaedic conditions over the study period. When further divided by age group, soft tissue injuries (including strain/tear and inflammation) became less common in patients >60 years, while fractures (most commonly hip or wrist fractures) and arthritis-related pain became more common (Figure 3).
Table 1.
Diagnosis of Pickleball-Related Injuries at Vanderbilt University Medical Center, 2017-2022 a
| Injury Diagnosis (Orthopaedic) | n (%) | Injury Diagnosis (Nonorthopaedic) | n (%) |
|---|---|---|---|
| Rotator cuff impingement/strain/tear | 67 (13.2) | Cardiac-related chest pain/palpitations | 24 (22.02) |
| Arthritis-related pain | 62 (12.2) | Facial laceration | 15 (13.76) |
| Back pain/sciatica | 48 (9.43) | Contusion/laceration (nonfacial) | 11 (10.09) |
| Calf strain/tear | 35 (6.88) | Syncope | 10 (9.17) |
| Knee sprain | 31 (6.09) | Head injury | 10 (9.17) |
| Hand/wrist fracture | 30 (5.89) | Rib fracture | 7 (6.42) |
| Achilles tendon tear/strain | 27 (5.30) | Shortness of breath/dyspnea | 6 (5.50) |
| Meniscus tear | 27 (5.30) | Cellulitis | 4 (3.67) |
| Lateral epicondylitis | 20 (3.90) | Hernia | 3 (2.75) |
| Plantar fasciitis/rupture | 19 (3.73) | Incontinence | 2 (1.83) |
| Hip pain | 18 (3.54) | Osteoporosis | 2 (1.83) |
| Ankle sprain | 16 (3.14) | Hepatic cyst | 1 (<1) |
| Wrist sprain | 15 (2.95) | Oblique strain | 1 (<1) |
| Hand injury | 14 (2.75) | Iliac vein stenosis | 1 (<1) |
| Ankle/foot fracture | 11 (2.16) | Rhabdomyolysis | 1 (<1) |
| Hip/pelvic fracture | 11 (2.16) | Hypertensive emergency | 1 (<1) |
| Hamstring tear/strain | 10 (1.96) | Deep vein thrombosis | 1 (<1) |
| ACL or MCL tear | 9 (1.77) | Neuropathy | 1 (<1) |
| Shoulder strain/pain (not rotator cuff-related) | 8 (1.57) | Periarticular juvenile rheumatoid arthritis | 1 (<1) |
| Neck pain | 7 (1.38) | Broken nose | 1 (<1) |
| Foot pain (not fracture or plantar fasciitis) | 6 (1.18) | Exertional hyperthermia | 1 (<1) |
| Labral tear | 4 (<1) | Subglottic stenosis | 1 (<1) |
| Olecranon bursitis | 3 (<1) | COVID-19 | 1 (<1) |
| Tibia fracture | 3 (<1) | Corneal abrasion | 1 (<1) |
| Pectoralis muscle strain | 1 (<1) | Transient vision loss | 1 (<1) |
| Patellar dislocation | 1 (<1) | Osteomyelitis and open wound | 1 (<1) |
| Humerus fracture | 1 (<1) | Acute kidney injury | 1 (<1) |
| Soft Tissue shoulder mass | 1 (<1) | Total | 109 |
| Greater tuberosity fracture | 1 (<1) | ||
| Quadriceps tear | 1 (<1) | ||
| Shoulder dislocation | 1 (<1) | ||
| Total | 509 |
ACL, anterior cruciate ligament; COVID-19, coronavirus disease 2019; MCL, medial collateral ligament;
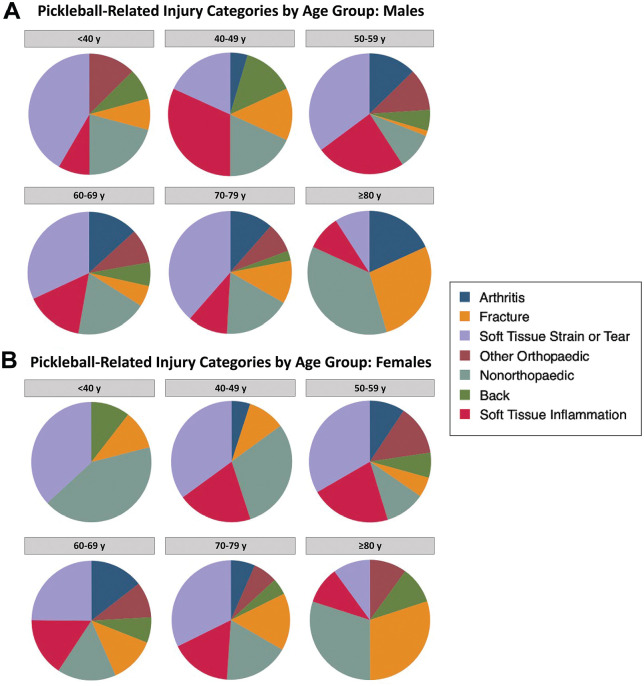
Figure 3.
Pickleball-related injuries categorized according to age group.
Injuries by Sex
Injuries were approximately evenly distributed between the sexes, with 53% of injuries occurring in men. However, a significantly lower proportion of injuries was observed in men than expected given that 62% of pickleball players are men, 1 suggesting that women might be at increased risk of injury (P < .001). Results of sex-stratified injuries according to category and age group are presented in Appendix Figure A2. Across all age groups, women were 2 times more likely to sustain fractures than men (odds ratio [OR], 2.03; P = .021). Men sustained more soft tissue strain or rupture, although this association did not reach statistical significance (OR, 1.26; P = .206).
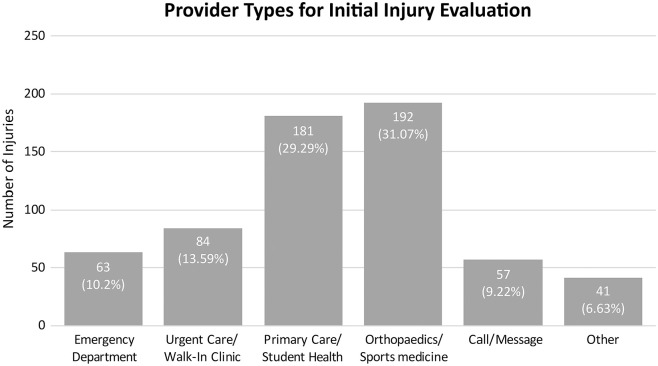
Injuries by Provider Type
We also collected information on injuries according to evaluation providers, as well as time for evaluation and follow-up. Overall, patients most commonly were seen by a provider within 1 week of injury (n = 298; 48.2%), with most patients (n = 470; 76%) being evaluated less than a month from the time of injury (Appendix Figure A3). In most injuries (n = 426; 68.9%), patients were initially seen by a nonorthopaedic provider, while for the other 192 (31.1%) injuries, patients were evaluated directly by an orthopaedic or sports medicine specialist (Figure 4). Among the injuries that were initially not evaluated by an orthopaedic provider, 329 (53.2%) were referred to orthopaedics/sports medicine specialists, and in total, 307 (63%) patients saw an orthopaedic or sports medicine provider at some point in the course of treatment for a pickleball-related injury. Further, among patients who saw an orthopaedic specialist, 233 (75.9%) had an additional follow-up visit (>1 appointment) with the specialist for their injury.
Figure 4.
Initial point of contact for patients evaluated for pickleball-related injuries, 2017-2022.
Injury Evaluation/Treatment
Injury evaluation and treatment varied widely across the study, with medication being the most common treatment modality followed by rest and advanced imaging. A total of 388 (62.8%) injuries were evaluated with at least 1 form of imaging. Among these, radiography was the most common, followed by magnetic resonance imaging and ultrasound. Importantly, 16.7% of patients went on to require surgical intervention for an injury sustained during pickleball (Table 2). Among these surgeries, the most common procedures were arthroscopic (eg, rotator cuff repair, anterior cruciate ligament reconstruction, subacromial decompression; n = 36; 34.9%), followed by open soft tissue repair (eg, Achilles tendon repair; n = 17; 16.5%), and open reduction and internal fixation/intramedullary nail (eg, distal radius fixation; n = 14; 13.6%) (Appendix Table A2).
Table 2.
Subsequent Treatments or Interventions at Vanderbilt University Medical Center for Pickleball-Related Injuries, 2017-2022 a
| Treatment Category | No. of Injuries (%) |
|---|---|
| Rest | 452 (73.1) |
| Brace | 182 (29.5) |
| Medication | 511 (82.7) |
| Referral | 362 (58.6) |
| Physical therapy | 295 (47.7) |
| Advanced imaging | 388 (62.8) |
| Radiograph | 316 (51.1) |
| MRI | 99 (16) |
| CT | 30 (4.9) |
| Ultrasound | 80 (12.9) |
| Other (eg, EKG, bronchoscopy) | 19 (3.1) |
| Injection | 80 (12.9) |
| Surgery | 103 (16.7) |
CT, computed tomography; EKG, electrocardiogram; MRI, magnetic resonance imaging.
Discussion
We identified 618 pickleball-related injuries, with a 6.8-fold increase in pickleball injuries throughout the study period. Players <60 years were found to be at higher risk of soft-tissue strain or tear, and players >60 years were at greater risk of fracture. Women were 2 times more likely to sustain a fracture.
As compared with other racket sports—such as tennis 19 or squash/racquetball 18 —the age of injury in pickleball is notably older, consistent with the broader demographic trend of the pickleball community. Although pickleball is quickly gaining popularity among younger age groups, the mean age of injury remained relatively steady over the study period. As with other racket sports, the predominance of injuries consisted of soft tissue strain or rupture.3,4,9,11,15 However, we found a prominent transition in injury patterns with advancing age, characterized by an increased prevalence of fractures and arthritis-related pain. These findings emphasize an age-specific risk profile that could lead to targeted intervention and prevention.
In addition, there were some important sex-based differences in injury patterns. Namely, although most pickleball players were men, women were more likely to sustain pickleball-related injuries. Further investigation into injury types revealed that women were almost twice as likely as men to sustain a fracture from pickleball. Although very little data surrounding pickleball-related injuries exist, 1 preliminary study that investigated pickleball- and tennis-related injuries specifically among older populations found a similar trend. 24 Together, these studies suggest a potential role for interventions such as wrist bracing and medication supplementation that might decrease the risk of fracture, particularly among older women engaging in pickleball.
As expected with sports-related injuries, our study revealed a strong orthopaedic injury burden. The preponderance of musculoskeletal injuries highlights the importance of orthopaedic evaluation in the management of pickleball-related incidents. Moreover, we found a high treatment burden associated with pickleball-related injuries, indicating that while pickleball is generally considered a safe leisurely activity, there is a meaningful risk of the consequent financial and personal impact associated with participation. Together, the overview of the pickleball injury profile and subsequent treatment burden presented in this study can provide valuable insight into injury characteristics and help inform providers’ (both orthopaedic and general practitioner) approach to patient education, diagnosis, treatment, and rehabilitation.
Importantly, although most injuries were orthopaedic, a substantial number of patients initially sought care from nonorthopaedic, particularly primary care providers, emphasizing the pivotal role of general practitioners in the early stages of injury management and the necessity for a multidisciplinary approach to pickleball-related injuries. Given the broad presentation pattern of patients in this study, both orthopaedic specialists and primary care providers need to be equipped to educate and deliver care for persons engaged in this increasingly popular sport. Furthermore, we found a high level of treatment burden (assessment time, diagnostic workup, surgical intervention, follow-up, etc) associated with pickleball-related injuries. Thus, treating pickleball-related injuries not only has personal risks for the patient but also a potentially dramatic financial impact.
Notably, although older individuals are often drawn to the sport's social and low-impact attributes, our findings indicate a meaningful risk of injury associated with pickleball, particularly among this age group. Moreover, the injury patterns shift with age, wherein the prevalence of fractures and arthritis-related pain increases with age. Decreasing balance and coordination, coupled with increasing injury risk in this population appears to be a detrimental combination. Patients should be counseled to approach the sport slowly, learn about technique, and improve strength, flexibility, and balance before participation. The evolving risk profile as players transition into different stages of life suggests that future investigations are warranted into targeted interventions, especially in older patients, that could potentially mitigate this risk.
Last, while this study highlighted the potential risks of pickleball, there are many benefits to pickleball participation—including physical, mental, and social. In a recent review, Stroesser et al 22 reported that pickleball participation was associated with greater life satisfaction, decreased rates of depression, and improved psychological well-being across all age groups, particularly among older participants. These mental health benefits are partially attributed to the increased social connection associated with pickleball participation, wherein seniors participating in pickleball reported lower rates of loneliness and a greater sense of social integration and interaction. 7 Moreover, while less established than the psychological and social benefits, pickleball participation has also been associated with improvements in physical health such as up to 3000 increased steps per day, increased caloric expenditure, and cardiovascular benefits (eg, decreased systolic blood pressure and decrease in coronary artery disease). 21 Together, these studies highlight the many benefits of pickleball participation—particularly in older populations—and underscore the importance of weighing the potential risks outlined in this study against these benefits.
Limitations
There are several limitations of our study inherent to the study design. First, although the Vanderbilt Research Derivative offers a robust collection of EHR at our institution, reliance on chart review always introduces the possibility of incomplete or inaccurate documentation, potentially leading to underreporting or misclassification of injuries. In addition, as a single-institution study, the data were confined to a specific geographic area and patient population. It is therefore possible that we may not have captured the full spectrum of pickleball-related injuries, potentially restricting the generalizability of our findings. Moreover, because the exact population of pickleball players in the study region is unknown, we cannot directly infer the incidence or risk of injury in our population. However, we compared injury trends and reported national statistics across the study time frame to mitigate this limitation.1,20 Nevertheless, there could be regional differences in participation. Last, the cross-sectional nature of this study lacks temporality and thus we were unable to infer the overall odds of injury among those who play pickleball. Further studies evaluating the overall time of participation and total population of players in the region are necessary to evaluate the risk of injury. Based on these limitations, caution should be used when extending these findings to the broader community of pickleball players. Future research is needed to address these constraints and enhance the understanding of pickleball-related injuries.
Conclusion
We observed a 6.8-fold increase in pickleball-related injuries at our institution from 2017 to 2022, which far outpaces the reported increase in pickleball participation nationally. Women >60 years were found to be at the highest risk of injury and were more likely to sustain fractures. Most injuries were musculoskeletal related, with soft tissue injury occurring most commonly in patients <60 years and fractures more common in those >60 years.
Appendix
Table A1.
Age of Pickleball-Related Injury by Year
| Year of Injury | Age, Years, Mean (Range) |
|---|---|
| 2017 | 63.9 (47-77) |
| 2018 | 63.2 (13-81) |
| 2019 | 65.1 (27-82) |
| 2020 | 62.1 (12-81) |
| 2021 | 62.5 (15-82) |
| 2022 | 59.8 (14-82) |
Figure A1.
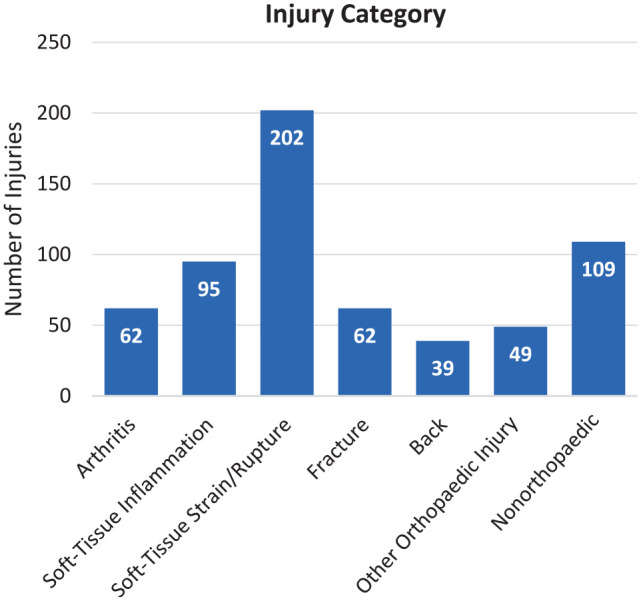
Pickleball-related injuries according to category.
Figure A2.
Pickleball-related injuries according to injury category and age group in (A) men and (B) women.
Figure A3.
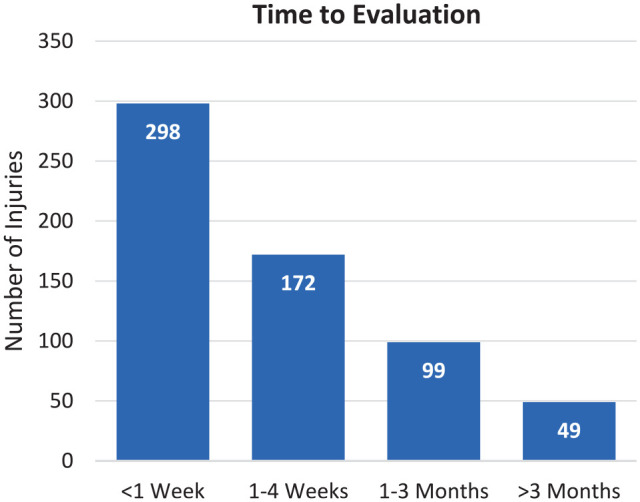
Time from injury to initial evaluation.
Table A2.
Surgeries According to Category a
| Surgery Category | n |
|---|---|
| Arthroscopy | 36 |
| Soft tissue repair | 17 |
| ORIF/IMN | 14 |
| Arthroplasty | 11 |
| Spine | 8 |
| Hand | 3 |
| Bone biopsy | 1 |
| Nonorthopaedic | 13 |
ORIF/IMN, open reduction and internal fixation/intramedullary nail.
Footnotes
Final revision submitted September 17, 2024; accepted September 19, 2024.
One or more of the authors has declared the following potential conflict of interest or source of funding: Funding for this study was received from the National Institute of Arthritis and Musculoskeletal and Skin Diseases of the National Institutes of Health (grants T32GM007347 [to S.D.H.]; 1F31AR082662-01 [to S.D.H.]). E.N.B. has received education payments from Alpha Orthopedic Systems. K.L.H. has received education payments from Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by Vanderbilt University.
ORCID iD: Simone D. Herzberg  https://orcid.org/0000-0001-9971-9821
https://orcid.org/0000-0001-9971-9821
Eric N. Bowman  https://orcid.org/0000-0003-2703-5038
https://orcid.org/0000-0003-2703-5038
Kelly L. Hill  https://orcid.org/0000-0003-2080-2943
https://orcid.org/0000-0003-2080-2943
References
- 1. 2023 APP pickleball participation report. Accessed October 10, 2023. https://cdn.prod.website-files.com/642c2ebf6376c444976a3f95/648b7da1f7224a74177f1223_2023_APP_Pickleball_Participation_Report_-_March_2023.pdf [Google Scholar]
- 2. 2023 USA pickleball fact sheet. Accessed October 10, 2023. https://www.usapickleball.org/docs/USA-Pickleball-Fact-Sheet-2023.pdf [Google Scholar]
- 3. Abrams GD, Renstrom PA, Safran MR. Epidemiology of musculoskeletal injury in the tennis player. Br J Sports Med. 2012;46(7):492-498. doi: 10.1136/bjsports-2012-091164 [DOI] [PubMed] [Google Scholar]
- 4. Alrabaa RG, Lobao MH, Levine WN. Rotator cuff injuries in tennis players. Curr Rev Musculoskelet Med. 2020;13(6):734-747. doi: 10.1007/s12178-020-09675-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Atkinson CF, Patron ME, Joondeph BC. Retinal tears due to pickleball injury. Retin Cases Brief Rep. 2022;16(3):312-313. doi: 10.1097/ICB.0000000000000965 [DOI] [PubMed] [Google Scholar]
- 6. Bohannon M. Pickleball injuries cost Americans nearly $400 million this year—and seniors are hit the hardest. Forbes. Published June 27, 2023. Accessed October 10, 2023. https://www.forbes.com/sites/mollybohannon/2023/06/26/pickleball-injuries-cost-americans-nearly-400-million-this-year—and-seniors-are-hit-hardest/?sh=1eec5a8fc266
- 7. Casper JM, Bocarro JN, Lothary AF. An examination of pickleball participation, social connections, and psychological well-being among seniors during the COVID-19 pandemic. World Leis J. 2021;63(3):330-346. doi: 10.1080/16078055.2021.1957708 [DOI] [Google Scholar]
- 8. Cerezuela JL, Lirola MJ, Cangas AJ. Pickleball and mental health in adults: a systematic review. Front Psychol. 2023;14:1137047. doi: 10.3389/fpsyg.2023.1137047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Changstrom B, McBride A, Khodaee M. Epidemiology of racket and paddle sports-related injuries treated in the United States emergency departments, 2007-2016. Phys Sportsmed. 2022;50(3):197-204. doi: 10.1080/00913847.2021.1892467 [DOI] [PubMed] [Google Scholar]
- 10. Ghattas YS, Zeblisky P, Cassinat J, Aceto M, Spindler KP, Cannada LK. Pickleball-related fractures in the United States from 2002 to 2022: an analysis using the NEISS database. Orthop J Sports Med. 2024;12(6):23259671241255674. doi: 10.1177/23259671241255674 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Guermont H, Mittelheisser G, Reboursière E, Gauthier A, Drigny J. Shoulder muscle imbalance as a risk factor for shoulder injury in elite badminton players: a prospective study. Physical Therapy in Sport. 2023;61:149-155. doi: 10.1016/j.ptsp.2023.04.002 [DOI] [PubMed] [Google Scholar]
- 12. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377-381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Huang H, Greven MA. Traumatic lens subluxation from pickleball injury: a case series. Retin Cases Brief Rep. Published online August 12, 2022. doi: 10.1097/ICB.0000000000001312 [DOI] [PubMed] [Google Scholar]
- 15. Jørgensen U, Winge S. Injuries in badminton Sports Medicine. 1990;10(1):59-64. doi: 10.2165/00007256-199010010-00006 [DOI] [PubMed] [Google Scholar]
- 16. Kasper AA, Gibbons JL, Abboudi J, et al. Pickleball- and paddleball-related injuries to the upper extremity. Cureus. 2023;15(6):e39831. doi: 10.7759/cureus.39831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kerman A. 2023Sports, fitness, and leisure activities topline participation report. SFIA. Published online January 1, 2023. Accessed October 10, 2023. https://sfia.org/resources/sfias-topline-participation-report-shows-strong-positive-trends-across-multiple-sports-and-fitness-categories-2/
- 18. Nhan DT, Klyce W, Lee RJ. Epidemiological patterns of alternative racquet-sport injuries in the United States, 1997-2016. Orthop J Sports Med. 2018;6(7):232596711878623. doi: 10.1177/2325967118786237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pluim BM, Staal JB, Windler GE, Jayanthi N. Tennis injuries: occurrence, etiology, and prevention. Br J Sports Med. 2006;40(5):415-423. doi: 10.1136/bjsm.2005.023184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Sagerman D. APP reveals 36.5 million adult Americans played pickleball in 2022. Association of Pickleball Players. Published January 4, 2023. Accessed October 10, 2023. https://www.theapp.global/news/app-reveals-36-5-million-adult-americans-played-pickleball-in-2022
- 21. Smith L, Buchanan C, Dalleck L. The acute and chronic physiological responses to pickleball in middle-aged and older adults. Int J Appl Exerc Physiol. 13(2):21-32. [Google Scholar]
- 22. Stroesser K, Mulcaster A, Andrews DM. Pickleball participation and the health and well-being of adults—a scoping review. J Phys Act Health. Published online 2024:1-14. doi: 10.1123/jpah.2024-0092 [DOI] [PubMed] [Google Scholar]
- 23. USA pickleball annual growth report. Accessed October 10, 2023. https://usapickleball.org/about-us/organizational-docs/pickleball-annual-growth-report/
- 24. Weiss H, Dougherty J, DiMaggio C. Non-fatal senior pickleball and tennis-related injuries treated in United States emergency departments, 2010-2019. Inj Epidemiol. 2021;8(1):34. doi: 10.1186/s40621-021-00327-9 [DOI] [PMC free article] [PubMed] [Google Scholar]