Abstract
Heart failure (HF) represents one of the leading causes of morbidity and mortality worldwide. In recent years, remote monitoring (RM) and telemedicine have emerged as a promising strategy to improve the management of patients with HF, reducing hospitalizations and enhancing the quality of life. Through the integration of technologies such as implantable sensors, home monitoring devices, and mobile applications, it is possible to detect clinical changes early, enabling timely interventions. This article provides an overview of available technologies for RM in HF, analyses the clinical benefits observed in various studies, and addresses the remaining challenges, such as the need for standardization, long-term sustainability, and widespread adoption. Remote monitoring offers significant potential to improve clinical outcomes but requires further research and development to optimize its use in clinical practice.
Keywords: Heart failure, Remote monitoring, Multi-parametric evaluation, Connectivity
Introduction
Heart failure (HF) is a chronic ‘pandemic’ condition characterized by the heart’s inability to pump blood effectively, leading to significant morbidity and mortality.1 The goals of treatment in patients with HF are to improve their clinical status, functional capacity, and quality of life (QoL), prevent hospital admissions, and reduce mortality. Traditionally, HF management has heavily relied on the optimization of medical and device therapy, in-person clinical visits, and hospitalizations.2 However, in recent years, patient management with HF has shifted towards care models based on prevention and continuous monitoring of clinical conditions, aiming to avoid exacerbations and hospitalizations, which represent a major economic burden on healthcare systems.3 Remote monitoring (RM), or telemonitoring, is a significant innovation in this regard. This technology enables physicians to remotely monitor patients’ vital signs and clinical data in real time, allowing for rapid intervention in case of deterioration of the patient’s condition.4
Remote monitoring technologies in heart failure
Remote monitoring technologies can be divided into several categories, depending on the type of device used and the data monitored.5 Among the most relevant are as follows:
-
Pulmonary artery pressure monitoring:
CardioMEMS™: This implantable sensor uses microelectromechanical system technology to monitor and transmit pulmonary artery pressure. The CHAMPION trial6 showed that CardioMEMS reduced HF hospitalizations and improved QoL. It was effective regardless of ejection fraction, with a 48% reduction in hospitalizations after 6 months. Medicare data confirmed similar outcomes in real-world use.
-
Cardiac and vital parameter monitoring:
Wearable devices: Devices like portable electrocardiograms (ECGs) and KardiaMobile continuously track heart rate (HR), variability, and ECG, transmitting real-time data to clinicians.
Smartwatches/fitness trackers: New models (e.g. Apple Watch) monitor ECG, blood oxygen levels, and other health metrics.
-
Fluid and body weight monitoring:
Smart scales: These scales detect weight changes related to fluid retention, a sign of worsening HF (e.g. Withings Body Cardio).
Thoracic impedance sensors: These sensors estimate lung fluid levels to catch early signs of pulmonary congestion (e.g. Zephyr BioPatch, Zoll HFMS).
-
Telemedicine and health monitoring:
Telemedicine platforms: Enable regular patient–doctor communication via video and chat, with patients manually inputting vital signs.
Health monitoring apps: Patients can track symptoms, medications, and vitals, while some apps use artificial intelligence (AI) for personalized feedback.
-
Cardiac and respiratory function monitoring:
Implantable monitors: Devices like pacemakers (PMK), implantable cardioverter-defibrillator (ICD), and implantable cardiac monitor (e.g. Reveal LINQII™) continuously monitor arrhythmias and transmit data to healthcare teams for real-time analysis.
Respiratory monitors: Sensors track respiratory rate and air volume to detect HF deterioration (e.g. ResMed AirSense 10).
These technologies enhance HF management by improving condition control, reducing hospitalizations, and improving QoL.
Technological advancements in remote monitoring
Remote monitoring technologies have evolved significantly, integrating various physiological sensors and advanced data analytics to monitor HF patients. Among the most promising studies in this area is certainly the SELENE-HF study, published in 2022 by D’Onofrio et al.7 in Europace. This multi-centre study explored a new algorithm to predict hospitalizations in HF patients using implanted cardiac devices, leveraging RM data combined with a risk stratification model based on physiological parameters. The algorithm integrated several parameters, including HR variability, physical activity, thoracic impedance, and arrhythmia burden, along with the ‘Seattle Heart Failure Model’, a well-known risk stratification model for HF patients. When the data indicated a high risk of disease progression, an alert was generated, allowing physicians to intervene proactively. The results were promising: the algorithm predicted two-thirds of the first post-implant hospitalizations for HF, with an average lead time of 42 days before the event. This early warning allowed clinicians to take preventive measures, potentially reducing hospitalizations. Additionally, the false alarm rate was low, with only 0.7 false positives per patient per year. In conclusion, this study demonstrated that the combined use of RM and risk stratification can be effective in predicting HF worsening, offering clinicians a valuable tool to improve patient management and reduce hospitalizations. The SELENE-HF study led to the synthesis of a predictive algorithm for HF based on daily transmissions from home monitoring (HM).7
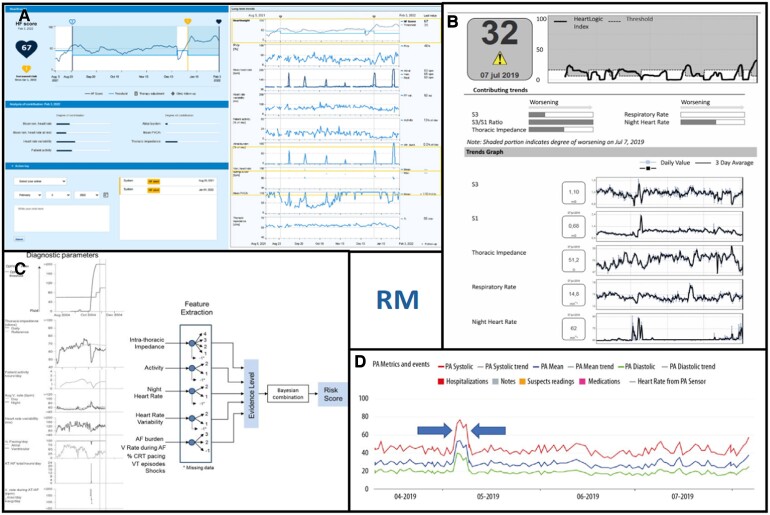
From these results, predictive algorithms for HF were derived, based on daily transmissions from HM, and were implemented in clinical practice onboard implantable devices (Table 1). The HeartInsight system, for example, exemplifies a modern RM tool designed for ICDs. It tracks seven parameters such as HR, HR variability, patient activity, thoracic impedance, atrial, and ventricular arrhythmic episodes, providing a comprehensive overview of the patient’s cardiac status. HeartInsight uses Biotronik’s RM system, called HM, which transmits daily data from the patient’s implanted device to a central server. The collected data are processed by a predictive algorithm that combines the eight critical parameters into a single score.8 This score reflects the patient’s cardiac health and is tracked over time. When it surpasses a preset threshold, HeartInsight triggers an alert. This alert (Figure 1A) is based on long-term analysis, not short-term fluctuations, and signals an increased risk of HF. The warning arrives an average of 42 days before possible hospitalization, enabling preventive interventions. Importantly, HeartInsight generates only one alert per patient, minimizing notification overload and false positives. Data are organized in a digital dashboard, easily integrated with electronic health records (EHRs), allowing quick consultation and data-driven decisions. This proactive approach helps avoid hospitalizations, optimizing resources and improving patient QoL.8
Table 1.
Overview of research articles on heart failure management and remote monitoring
| Author | Year of publication | Article title | Topic |
|---|---|---|---|
| McDonagh et al. | 2021 | 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure | ESC guidelines for the diagnosis and treatment of acute and chronic HF |
| Gheorghiade et al. | 2005 | Pathophysiologic targets in the early phase of acute Heart Failure syndromes | Pathophysiologic targets in the early phase of acute HF syndromes |
| Stevenson et al. | 2023 | Remote monitoring for heart failure management at home | RM for home HF management |
| Taylor and Ahmed. | 2023 | Clinical pathways guided by remotely monitoring cardiac device data: the future of device heart failure management? | HF management through remotely monitored cardiac devices |
| Bezerra Giordan et al. | 2022 | The use of mobile apps for heart failure self-management: systematic review of experimental and qualitative studies | Systematic review on the use of mobile apps for HF self-management |
| Abraham et al. | 2014 | Benefits of pulmonary artery pressure monitoring in patients with NYHA Class III HF and chronic kidney disease: results from the CHAMPION trial | Benefits of pulmonary artery pressure monitoring in patients with NYHA Class III HF and chronic kidney disease |
| D’Onofrio et al. | 2022 | Combining home monitoring temporal trends from implanted defibrillators and baseline patient risk profile to predict heart failure hospitalizations: results from the SELENE HF study | Prediction of HF hospitalizations based on RM and patient risk profile |
| Cowie et al. | 2013 | Development and validation of an integrated diagnostic algorithm derived from parameters monitored in implantable devices for identifying patients at risk for heart failure hospitalization in an ambulatory setting | Development of an integrated diagnostic algorithm for identifying patients at risk of HF hospitalization through implantable devices |
| Botto et al. | 2024 | Predicting worsening heart failure hospitalizations in patients with implantable cardioverter defibrillators: is it all about alerts? A pooled analysis of nine trials | Prediction of WHFhospitalizations in patients with ICD defibrillators |
| Santini et al. | 2024 | Optimizing remote heart failure management: first experiences with the HeartInsight score for implanted defibrillators | Optimizing remote HF management through the HeartInsight score for implanted defibrillators |
| Alvarez et al. | 2021 | Chronic disease management in heart failure: focus on telemedicine and remote monitoring | Chronic disease management in HF, focusing on telemedicine and RM |
| Boehmer et al. | 2017 | A multisensor algorithm predicts heart failure events in patients with implanted devices | Multi-sensor algorithm for predicting HF events in patients with implanted devices |
| Liu et al. | 2024 | Unveiling the potential: remote monitoring and telemedicine in shaping the future of heart failure management | RM and telemedicine in shaping the future of HF management |
| Ferrick et al. | 2023 | 2023 HRS/EHRA/APHRS/LAHRS expert consensus statement on practical management of the remote device clinic | Expert consensus statement on practical management of the remote device clinic |
Figure 1.
(A) HeartInsight system interface. (B) HeartLogic system interface. (C) Triage heart failure system algorithm. (D) CardioMEMS system interface.
A recent meta-analysis by Botto et al.9 examined data from nine clinical trials on patients with ICDs to understand whether the HeartInsight algorithm could predict hospitalizations due to worsening HF hospitalization (WHFH) in advance. The main findings are that patients who experienced a WHFH had significantly higher HF scores as early as 12 weeks before hospitalization compared with those who did not experience hospitalizations. The score continued to rise markedly until the hospitalization event. Some parameters, such as 24-h HR, HR variability, and thoracic impedance, were already higher in patients destined for a WHFH compared with the control group, while others, such as nighttime HR and arrhythmias, showed an increase closer to the hospitalization event. The various components of the HF score exhibited different temporal patterns, indicating that not all parameters rise simultaneously, but each contributes differently to the worsening of the cardiac condition. Further real-world data confirmed usefulness of HeartInsight algorithm.10
In summary, the HeartInsight algorithm appears to be a valuable tool for monitoring and predicting HF exacerbations, enabling timely interventions to prevent hospitalizations.9
The ‘HeartLogic’ algorithm by Boston Scientific (Boston Scientific, Boston, MA, USA), is integrated into the resonate series of cardiac resynchronization therapy devices and ICDs. The system operates by collecting data from five sensors that monitor various physiological parameters associated with HF: heart sounds (indicative of cardiac function), thoracic impedance (reflecting pulmonary congestion), respiratory rate, HR, and physical activity level. These data are processed daily to produce an index, the ‘HeartLogic Index’, which is patient specific and continuously updated (Figure 1B). When this index exceeds a preset threshold (usually 16), the algorithm generates an alert that signals to physicians an increased risk of HF. The RM system Latitude NXT allows medical staff to remotely track the index’s progress and intervene before the patient requires hospitalization.11,12 The MultiSENSE study validated the effectiveness of HeartLogic, demonstrating 70% sensitivity in predicting HF episodes with an average lead time of 34 days and a very low false alarm rate (1.47 per patient per year). This system has been shown to significantly reduce hospitalizations, improve patients’ QoL, and reduce healthcare costs.12
Triage HF (Medtronic Inc., Minneapolis, MN, USA; Figure 1C) is an algorithm available in all cardiac implantable electronic devices (CIEDs) manufactured by Medtronic. It integrates multiple parameters [thoracic impedance measured by Optivol™ algorithm, patient activity, burden of atrial fibrillation, ventricular rate during atrial fibrillation, ventricular pacing rate, nocturnal HR, heart rate variability (HRV), shocks delivered, and treated episodes of ventricular tachycardia (VT)/ventricular fibrillation (VF)]. The main difference with the already mentioned algorithms is that it does not compute a numerical index but a score of risk of hospitalization for acute HF in the next 30 days divided into HIGH, MEDIUM, and LOW. Based on a Bayesian probabilistic model, it uses 30 days of diagnostic data to predict the risk of decompensation in the next 30 days. The risk score starts to be calculated upon receipt of data on Carelink (Medtronic Inc.) after the first 65 days after implantation (34 days for Optivol calibration and 30 days for TriageHF risk stratification).
The efficacy of this algorithm in accurately categorizing patients according to their risk of a HF exacerbation has been substantiated by multiple studies.8
Benefits of remote monitoring
Remote monitoring in HF management provides key advantages, including early decompensation detection, reduced hospitalizations, better clinical outcomes, and improved QoL. Remote monitoring systems can detect subtle physiological changes before clinical signs emerge, such as a rise in HR or a drop in thoracic impedance indicating fluid build-up. More impactful than individual metrics, RM allows a multi-parametric assessment, integrating different clinical indicators into a single index. Alerts from RM systems enable early interventions, preventing hospitalizations and reducing episode severity. Studies confirm RM’s role in significantly lowering HF-related hospitalizations, improving patient outcomes, and reducing healthcare costs. For example, in a multi-centre study of over 1000 patients, the CardioMEMS system (Figure 1D) cut HF hospitalizations by 33%.6 Remote monitoring also enhances clinical outcomes through better symptom control, reduced mortality, and fewer complications, largely due to timely interventions and improved treatment adherence. Patients benefit from less frequent hospital visits, reduced stress, and increased confidence, knowing their health is constantly monitored.
Compared with traditional care, RM and telemedicine offer several advantages: better accessibility, more frequent monitoring, active patient engagement, faster response times, improved data collection, and better care coordination. Traditional management is constrained by location and infrequent check-ups, whereas RM offers continuous, real-time monitoring. It also promotes patient involvement via regular updates and mobile apps. Telemedicine enables rapid responses to clinical changes, reducing travel and hospitalizations.
Implementing RM entails initial and operational costs; however, the long-term benefits can outweigh these investments. According to data from AIAC and ANMCO in 2020, RM led to a 66.4% reduction in visit-related expenses for patients and a 70.4% decrease in the monetary value of lost work hours for family members. For the healthcare system, there was a 54% reduction in the annual cost per patient, while healthcare providers experienced a 60% decrease in unnecessary outpatient visits, allowing resources to be reallocated to other activities. Additionally, RM reduced the number of outpatient visits by 50% and decreased the duration of individual follow-ups from 26 min in traditional controls to 4–8 min, enhancing QoL, compliance, and patient satisfaction.
Continuous data collection via RM devices offers a more detailed clinical picture, while integrated care platforms enhance co-ordination among healthcare providers. Ultimately, RM and telemedicine improve clinical outcomes through early diagnosis, personalized interventions, and real-time data collection.13
Challenges and barriers to implementation
Despite the significant benefits, several challenges hinder the widespread adoption of RM in HF management.13 Implementing RM systems requires sophisticated technology and infrastructure. Ensuring reliable data transmission, maintaining system accuracy, and integrating RM data into existing EHRs are critical challenges. Furthermore, a strict organizational model needs to be set-up, providing for a dedicated staff and clearly establishing roles and competencies. At the outset of the implementation of a RM structure, there is a risk of an increase in workload for centres, as RM has been shown to potentially led to a paradoxical increase the number of accesses to hospitals consequently increasing the workload of the centres themselves.
An integrated and efficient organizational model must be developed. The guidelines14 recommend adopting an alert-based strategy to reduce the workload of operators and optimize resources. This strategy manages only clinically relevant transmissions and avoids reviewing scheduled transmissions, which diverts time and resources from patients who need them most. The evidence from real-life experiences and published literature is clear: multi-parametric evaluation algorithms are highly effective at stratifying patients according to risk of decompensation. Patients out of an alert status were free from incoming events. To adopt an alert-based strategy effectively and safely, it is essential to ensure constant connectivity of the patients. This requires devoting time and resources to systematically contact disconnected patients to verify the causes of missed transmissions and re-establish the connection as soon as possible. Finally, it is crucial that alarms are correctly and personally programmed and set up and that only the necessary and actionable alerts are activated for each patient.
Additionally, the initial cost of setting up RM systems can be a barrier for many healthcare providers. The large volumes of data generated by RM systems necessitate robust data management strategies. Protecting patient data privacy and ensuring compliance with regulations such as the General Data Protection Regulation (GDPR) is essential. Healthcare providers must implement stringent data security measures to prevent unauthorized access and breaches. The ownership and storage of data generated by RM systems represent critical aspects for the adoption and acceptance of these technologies. There are significant differences between data managed by academic institutions and data controlled by private industries. Academic management typically emphasizes transparency and shared access for research purposes, while private industries may prioritize data for proprietary use. Legal and ethical considerations require clear policies to ensure that patients and healthcare providers are fully informed about who owns the data, how it is stored, and how it is utilized. Compliance with regulations such as GDPR in Europe and Health Insurance Portability and Accountability Act (HIPAA) in the USA12 is paramount to protect patient privacy and maintain trust in these systems. Future systems will likely include better patient education tools and apps to enhance self-management and adherence to treatment plans. For RM to be effective, patients must be actively engaged and compliant with the monitoring protocols. Educating patients about the importance of RM, how to use the devices, and what to do in case of alerts is crucial. Non-compliance can lead to missed alerts and delayed interventions, undermining the effectiveness of RM. Remote monitoring requires a multi-disciplinary approach involving cardiologists, HF specialists, nurses, and IT professionals. Co-ordinating care among different healthcare providers and ensuring seamless communication is challenging but necessary for successful RM implementation.
Legal responsibility
Legal responsibility is a pivotal issue in the deployment of RM systems. Manufacturers, healthcare providers, and patients each bear specific responsibilities regarding the use, maintenance, and interpretation of RM data. To mitigate legal risks, it is essential to establish clear contractual agreements outlining responsibilities and liabilities. For instance, device manufacturers must ensure the accuracy and reliability of their systems, while healthcare providers are responsible for appropriate interpretation and timely intervention based on transmitted data. Regulatory frameworks, such as those enforced by GDPR and HIPAA, play a crucial role in defining these responsibilities and safeguarding patient rights.
Future directions
The future of RM in HF is promising, thanks to advancements in technology and data analytics. Key trends include the integration of RM with wearable devices, such as smartwatches and fitness trackers, improving patient engagement and offering real-time health data. Predictive analytics and AI will enhance RM by identifying early signs of HF exacerbation, enabling personalized and preventive care. The COVID-19 pandemic gave a ‘Tech-celleration’ to the use of telemedicine, highlighting RM’s potential to provide continuous monitoring, virtual consultations, and remote care, reducing the need for in-person visits. Personalized medicine, guided by RM, will tailor treatment to individual needs, improving patient outcomes.
Conclusions
Remote monitoring offers a transformative way to manage HF by enabling early detection, reducing hospitalizations, and improving patient outcomes and QoL. Despite implementation challenges, advances in technology and data analytics will drive its wider adoption. The future of RM in HF lies in integrating predictive analytics, wearables, telemedicine, and personalized care, improving both treatment and patient outcomes. Ongoing innovation will allow healthcare providers to deliver more effective, efficient care, ultimately easing the burden on healthcare systems and enhancing patient lives.
Contributor Information
Nicola Pierucci, Department of Clinical Internal Anesthesiologic and Cardiovascular Sciences, Sapienza University of Rome, Rome 00161, Italy.
Domenico Laviola, Department of Clinical Internal Anesthesiologic and Cardiovascular Sciences, Sapienza University of Rome, Rome 00161, Italy.
Marco Valerio Mariani, Department of Clinical Internal Anesthesiologic and Cardiovascular Sciences, Sapienza University of Rome, Rome 00161, Italy.
Alessio Nardini, General Direction of the Mission Unit for the Implementation of PNRR Interventions, Italian Ministry of Health.
Francesco Adamo, Cardiology Unit, Ospedale G.B. Grassi, Ostia, Rome, Italy.
Karim Mahfouz, Cardiology Unit, Ospedale G.B. Grassi, Ostia, Rome, Italy.
Carlo Colaiaco, Cardiology Unit, Ospedale G.B. Grassi, Ostia, Rome, Italy.
Fabrizio Ammirati, Cardiology Unit, Ospedale G.B. Grassi, Ostia, Rome, Italy.
Luca Santini, Cardiology Unit, Ospedale G.B. Grassi, Ostia, Rome, Italy.
Carlo Lavalle, Department of Clinical Internal Anesthesiologic and Cardiovascular Sciences, Sapienza University of Rome, Rome 00161, Italy.
Funding
This manuscript received no funding.
Data availability
All data discussed are publicly available in the sources cited within the manuscript.
References
- 1. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 2021;42:3599–3726. [DOI] [PubMed] [Google Scholar]
- 2. Gheorghiade M, De Luca L, Fonarow GC, Filippatos G, Metra M, Francis GS. Pathophysiologic targets in the early phase of acute heart failure syndromes. Am J Cardiol 2005;96:11–17. [DOI] [PubMed] [Google Scholar]
- 3. Stevenson LW, Ross HJ, Rathman LD, Boehmer JP. Remote monitoring for heart failure management at home. J Am Coll Cardiol 2023;81:2272–2291. [DOI] [PubMed] [Google Scholar]
- 4. Taylor JK, Ahmed FZ. Clinical pathways guided by remotely monitoring cardiac device data: the future of device heart failure management? Arrhythm Electrophysiol Rev 2023;12:e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Bezerra Giordan L, Tong HL, Atherton JJ, Ronto R, Chau J, Kaye D et al. The use of mobile apps for heart failure self-management: systematic review of experimental and qualitative studies. JMIR Cardio 2022;6:e33839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Abraham WT, Adamson PB, Stevenson LW, Yadav J. Benefits of pulmonary artery pressure monitoring in patients with NYHA class III heart failure and chronic kidney disease: results from the CHAMPION trial. J Card Fail 2014;20:S93. [Google Scholar]
- 7. D’Onofrio A, Solimene F, Calò L, Calvi V, Viscusi M, Melissano D et al. Combining home monitoring temporal trends from implanted defibrillators and baseline patient risk profile to predict heart failure hospitalizations: results from the SELENE HF study. EP Europace 2022;24:234–244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cowie MR, Sarkar S, Koehler J, Whellan DJ, Crossley GH, Tang WH et al. Development and validation of an integrated diagnostic algorithm derived from parameters monitored in implantable devices for identifying patients at risk for heart failure hospitalization in an ambulatory setting. Eur Heart J 2013;34:2472–2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Botto GL, Sinagra G, Bulava A, Gargaro A, Timmel T, Giacopelli D et al. Predicting worsening heart failure hospitalizations in patients with implantable cardioverter defibrillators: is it all about alerts? A pooled analysis of nine trials. Europace 2024;26:euae032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Santini L, Adamo F, Danisi N, Mahfouz K, Colaiaco C, Finamora I et al. Optimizing remote heart failure management: first experiences with the HeartInsight score for implanted defibrillators. J Arrhythm 2024;40:643–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Alvarez P, Sianis A, Brown J, Ali A, Briasoulis A. Chronic disease management in heart failure: focus on telemedicine and remote monitoring. Rev Cardiovasc Med 2021;22:403. [DOI] [PubMed] [Google Scholar]
- 12. Boehmer JP, Hariharan R, Devecchi FG, Smith AL, Molon G, Capucci A et al. A multisensor algorithm predicts heart failure events in patients with implanted devices. JACC Heart Fail 2017;5:216–225. [DOI] [PubMed] [Google Scholar]
- 13. Liu J-C, Cheng C-Y, Cheng T-H, Liu C-N, Chen J-J, Hao W-R. Unveiling the potential: remote monitoring and telemedicine in shaping the future of heart failure management. Life 2024;14:936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ferrick AM, Raj SR, Deneke T, Kojodjojo P, Lopez-Cabanillas N, Abe H et al. 2023 HRS/EHRA/APHRS/LAHRS expert consensus statement on practical management of the remote device clinic. Heart Rhythm 2023;20:e92–e144. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data discussed are publicly available in the sources cited within the manuscript.