Abstract
Background
Preconception care provided by family physicians/general practitioners (FP/GPs) can provide predictable benefits to mothers and infants. The objective of this study was to elucidate knowledge of, attitudes about, and practices of preconception care by FP/GPs in Japan.
Methods
A survey was distributed to physician members of the Japanese Academy of Family Medicine. The questionnaire addressed experiences of preconception education in medical school and residency, frequency of preconception care in clinical practice, attitudes about providing preconception care, and perceived need for preconception education to medical students and residents.
Results
Two hundred and sixty-eight of 347 (77%) eligible physicians responded. The most common education they reported receiving was about smoking cessation (71%), and the least was about folic acid supplementation (12%). Many participants reported providing smoking cessation in their practice (60%), though only about one third of respondents advise restricting alcohol intake. Few reported advising calcium supplementation (10%) or folic acid supplementation (4%). About 70% reported their willingness to provide preconception care. Almost all participants believe medical students and residents should have education about preconception care.
Conclusion
FP/GPs in Japan report little training in preconception care and few currently provide it. With training, most participants are willing to provide preconception care themselves and think medical students and residents should receive this education.
Background
Appropriate preconception care provided by family physician/general practitioners (FP/GPs) can provide great benefits to mothers and infants. [1-4] In spite of many potentially helpful interventions prior to conception, there is little literature illustrating the effectiveness of preconception services delivery through primary care settings. Muchowski and Paladine present the evidence of effectiveness for components of preconception care that could be provided in primary care settings.[4] Korenbrot and colleagues conducted a systematic review and found no RCTs of prepregnancy interventions, though one RCT was conducted among women who had a negative pregnancy test.[5] Despite recent research demonstrating the importance of assessing primary care workers views on preconception care,[6] we found no published research on Japanese FP/GPs' approaches to the provision of preconception care to women of reproductive age.
Such research is needed because obstetricians in Japan usually cannot provide preconception counseling. Women infrequently present to OB/GYN physicians prior to conception unless they have gynecological problems. Many of our primary care colleagues consider women's health issues to be outside the realm of their practice, and they lack systematic education in preventive care during family/general medicine training. Despite a longstanding call for family physicians to provide preventive care in Japan,[7] we hypothesized that few FP/GPs are providing preconception counseling.
The best proven preconception intervention, taking folic acid supplements one to two months prior to conception, has been shown to prevent neural tube defects.[8] Unfortunately, many pregnant women do not have their first visit for prenatal care until eight weeks of pregnancy or later, even though fetal development is most vulnerable to development of neural tube defects during this time.[1] Epidemiological studies published over the last fifteen years document that prenatal supplementation with folic acid reduces the risk of neural tube defects, such as spina bifida and anencephaly. [9-11] In many countries, daily consumption of 0.4 mg of folic acid is recommended for reproductive-aged women, and 4 mg is recommended for those who previously had an affected fetus/infant.[12,13] The World Health Organization (WHO) recommends preconception care, including folic acid supplementation, for primary prevention of birth defects in developing and developed countries alike.[14]
Until recently, there has been no recommendation for Japanese women to take a folic acid supplement prior to conception. In December 2000, the Ministry of Health, Labour and Welfare (MHLW) formally recognized the importance of reproductive-aged women taking folic acid supplementation for the prevention of neural tube defects.[15] This recommendation was based on research showing that the rate of neural tube defects is reduced by about 72% when women take folic acid supplementation one to three months prior to conception. The MHLW recommended to the Japan Medical Association, Japan Society of Obstetrics and Gynecology, and Japan Pediatric Society that these organizations should provide their membership with adequate information about the value of taking folic acid to reproductive-aged women.[15]
In addition, there are other compelling topics to cover during preconception counseling based on theoretical considerations and indirect evidence. A particularly important topic in Japan is screening for immunity to rubella. The prevalence of rubella vaccination in Japan is only about 70%.[16] Rubella vaccination is not mandatory due in part to serious side effects that resulted from an MMR vaccination manufactured in Japan several years ago.[16] Antibody negative women can be safely vaccinated prior to pregnancy during preconception care.[17]
Excessive alcohol intake during pregnancy causes fetal alcohol syndrome.[18] Smoking during pregnancy is associated with low birth rate infants.[19] As post-partum hemorrhage is the most important cause of preventable maternal mortality in Japan,[20] prevention of anemia through early detection and treatment with iron supplementation merits consideration. As the average intake of calcium, especially in reproductive women in Japan, is lower than recommended in general, calcium intake is a particularly salient issue for Japanese women of childbearing age. Though controversial, exercise, and mechanisms to optimize pregnancy are among other potentially beneficial effects of preconception counseling. [1-4] Based on clinical experience with a large population of Japanese couples desiring pregnancy, but having difficulty conceiving and not willing to see an infertility specialist, we consider brief counseling on basal body temperature monitoring and timing of intercourse as topics relevant in Japan.
Given the importance of these issues in maternal child health, the purpose of this research was to elucidate the knowledge of, attitudes about, and practices of preconception care for reproductive-aged women by FP/GPs in Japan.
Methods
In this survey research, we distributed a structured questionnaire to physicians who were registered members of the Japanese Academy of Family Medicine (JAFM). The JAFM has membership based on interest, not criteria such as board certification or completion of family medicine residency training. As family medicine is still a young discipline in Japan, most members have trained in non-family medicine programs. The physician members include a diverse group: those trained in a family medicine training program in the US or Japan, those trained in another specialty or multiple specialties and became a general practitioner after entering practice, and those who trained in a general internal medicine program in Japan or the US.
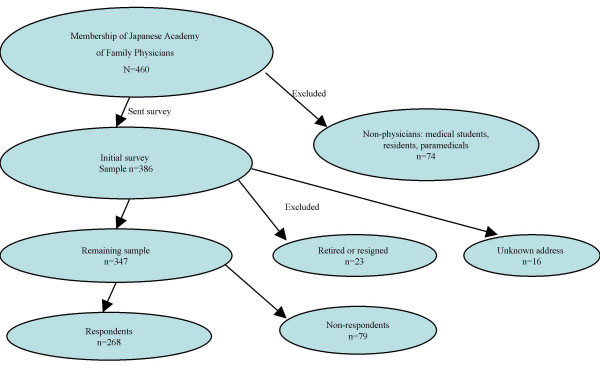
The JAFM was established in 1986 and has taken a leadership role in establishing family medicine in Japan.[21] The academy had a membership of 460 during the research period. Most members of the JAFM are practicing physicians and/or teachers of family medicine. The membership also includes medical students, residents and paramedical staff who are interested in family medicine. We excluded from the analysis non-physician members, medical students, physicians not in active practice, and those who had resigned from the JAFM (Figure 1).
Figure 1.
Selection of survey participants.
All participants were asked to complete a questionnaire with items addressing: 1) experiences in preconception education during medical school and residency training; 2) the frequency of providing preconception care in their practice; 3) their attitudes about providing preconception care; and 4) their perceptions of the need for preconception education for medical students and residents. The instrument was distributed with a cover letter requesting their participation. A reminder was sent to non-respondents twice at two-week intervals. A fourth mailing included the final request and a second copy of the instrument.
The components of preconception care we investigated are depicted in Table 1. Some are compelling based on best evidence (such as folic acid supplementation, smoking cessation),[5] while others were chosen based on circumstances particular to Japan as presented above.
Table 1.
Preconception Care Interventions
| Services | Intervention |
| Folic acid supplementation | Advise 0.4 mg of folic acid daily (4 mg if previous pregnancy with neural tube defect) three months prior to conception. |
| Smoking cessation | Educate about the risks of smoking during pregnancy and counsel about smoking cessation. |
| Anemia screen | Check hematocrit/CBC and recommend iron supplement if anemia is detected. |
| Testing for rubella antibody | Check IgG rubella antibody before conception. If the test is negative, vaccinate and avoid conception for three months. |
| Alcohol restriction | Screen for alcoholism by using a validated questionnaire, and counsel or refer if positive screen. |
| Restricting caffeine | Restrict caffeine intake to less than 250 mg a day. |
| Exercise | Advise regular to moderate exercise before and during pregnancy. |
| Calcium supplementation | Assess calcium intake and as needed supplement for a target of 1200 mg daily. |
| Use of basal body temperature* | Conduct basal body temperature every morning to identify the day of ovulation. |
| Timing of intercourse* | Advise intercourse every other day around time of ovulation to maximize chances of conception. |
*For couples having difficulty conceiving
We analyzed the data using SPSS (Statistical Package for Social Sciences). Simple statistics were calculated on the demographics data. Statistical significance of continuous measures was tested by two-tailed student t-test, and categorical data were tested by the chi-square test where appropriate. Physicians who reported their specialty as family medicine were compared for differences with physicians who reported their specialty as general internal medicine.
Results
Of the 460 members of the JAFM during the study period, we excluded the 74 non-physician and medical student members from the survey. Of the 386 physicians to whom we distributed instruments, 291 physician members responded. Sixteen letters were returned because of unknown addresses. We dropped 23 physicians from the analysis who reported that they were retired or had resigned from the academy. Thus, 268 of 347 eligible physicians (response rate 77.2%) were included in the analysis (Figure 1). The demographics of the participants are listed in Table 2. Most were men (86%) and the mean age was almost 40 years. Most physicians reported seeing reproductive-aged women in their offices.
Table 2.
Participant Demographics (n = 268)
| n | (%) | |
| Gender | ||
| Male | 230 | (85.8) |
| Age | ||
| Mean (range) | 40.1 (25–73) | |
| Period after graduating from med school (yrs) | ||
| Mean (range) | 14.4 (1–26) | |
| Specialty (total response = 308)* | ||
| General Internal Medicine | 140 | (45.5) |
| Family Medicine | 102 | (33.1) |
| Specialty in Internal Medicine | 19 | (6.2) |
| General Medicine | 10 | (3.2) |
| Surgery | 8 | (2.6) |
| Pediatrics | 8 | (2.6) |
| Psychiatry | 6 | (1.9) |
| Orthopedics | 5 | (1.6) |
| Others | 10 | (3.2) |
| Experiences of out-patient training in | ||
| Pediatrics | 160 | (59.7) |
| OB/GYN | 99 | (36.9) |
| Average number of patients per week | ||
| All | 142 /wk | |
| Reproductive women | 11 /wk | |
| Average number of patients by age | ||
| Child (0–15) | 15.3 | (8.9) |
| Adolescence (16–19) | 9.5 | (7.0) |
| Adult (20–64) | 43.9 | (35.0) |
| Elderly (65 and more) | 69.5 | (49.4) |
*multiple responses were possible
With regard to educational experiences in preconception counseling during medical school and residency training (Table 3), most participants reported they had received little. The most common relevant training they reported receiving included: smoking cessation (71%), screening for anemia (64%), and blood testing for rubella antibody (58%). Few reported training experiences in providing folic acid supplementation (12%), timing of intercourse to maximize chances of conception (14%), or exercise during pregnancy (18%).
Table 3.
Japanese family physicians' experiences in preconception education during medical school and residency training (n = 268)
| n | (%) | |
| Smoking cessation | 191 | (71.3) |
| Testing for anemia | 172 | (64.2) |
| Blood testing for rubella antibody | 156 | (58.2) |
| Use of basal body temperature monitoring | 125 | (46.6) |
| Restricting alcohol intake | 120 | (44.8) |
| Increasing calcium intake | 86 | (32.1) |
| Restricting caffeine intake | 52 | (19.4) |
| Exercise during pregnancy | 48 | (17.9) |
| Timing of intercourse to maximize chances of conception | 38 | (14.2) |
| Folic acid supplementation | 31 | (11.6) |
Preconception care practices of the respondents are depicted in Table 4. Many participants reported often or always addressing smoking cessation with reproductive-aged women (60%). Some reported they provide screening for anemia (35%) and counseling about restricting alcohol intake (27%). Few reported they addressed either calcium intake through foods/supplements (10%), or folic acid supplementation (4%).
Table 4.
Japanese family physicians' self-reports of preconception care in their clinical practice (n = 268)
| Never/Almost Never | Sometimes | Often/Always | No Response | |||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Timing of intercourse to maximize chances of conception | 222 | (82.8) | 20 | (7.5) | 9 | (3.6) | 17 | (6.3) |
| Folic acid supplementation | 217 | (81.0) | 24 | (9.0) | 11 | (4.1) | 16 | (6.0) |
| Exercise during pregnancy | 198 | (73.9) | 32 | (11.9) | 20 | (7.5) | 18 | (6.7) |
| Testing for rubella antibody | 180 | (67.2) | 55 | (20.5) | 21 | (7.8) | 12 | (4.5) |
| Increasing calcium intake | 168 | (62.7) | 61 | (22.7) | 27 | (10.1) | 12 | (4.5) |
| Restricting caffeine intake | 166 | (61.9) | 55 | (20.5) | 31 | (11.6) | 16 | (6.0) |
| Use of basal body temperature monitoring | 157 | (58.6) | 60 | (22.4) | 38 | (14.2) | 13 | (4.9) |
| Restricting alcohol intake | 107 | (39.9) | 74 | (27.6) | 72 | (26.9) | 15 | (5.6) |
| Testing for anemia | 56 | (20.9) | 112 | (41.8) | 94 | (35.1) | 6 | (2.2) |
| Smoking cessation | 37 | (13.8) | 63 | (23.5) | 162 | (60.4) | 6 | (2.2) |
Their attitudes about providing preconception care are depicted in Table 5. About two thirds of participants reported their willingness to provide preconception care about such topics as calcium intake (70%), blood testing for rubella antibody (69%), and restricting caffeine intake (64%). On the other hand, some expressed dissatisfaction with counseling about timing of intercourse to maximize chances of conception (46%), and use of basal body temperature monitoring (22%). More than 60% reported their willingness to provide folic acid supplementation, though one in four stated they would not provide it. Almost all participants think medical students (95%), and residents (91%), should have education in preconception care.
Table 5.
Japanese family physicians' willingness to provide preconception care in their practice (n = 268)
| Currently Provide | Willing to Provide | Would Not Provide | No Response | |||||
| n | (%) | n | (%) | n | (%) | n | (%) | |
| Smoking cessation | 154 | (57.5) | 103 | (38.4) | 5 | (1.9) | 6 | (2.2) |
| Screening for anemia | 103 | (38.4) | 145 | (54.1) | 11 | (4.1) | 9 | (3.4) |
| Restricting alcohol intake | 90 | (33.6) | 143 | (53.4) | 26 | (9.7) | 9 | (3.4) |
| Use of basal body temperature monitoring | 61 | (22.8) | 137 | (51.1) | 59 | (22.0) | 9 | (4.1) |
| Restricting caffeine intake | 42 | (15.7) | 171 | (63.8) | 42 | (15.7) | 13 | (3.8) |
| Blood testing for rubella antibody | 41 | (15.3) | 186 | (69.4) | 30 | (11.2) | 11 | (4.1) |
| Increasing calcium intake | 37 | (13.8) | 18 | (70.1) | 34 | (12.7) | 9 | (3.4) |
| Exercise during pregnancy | 30 | (11.2) | 165 | (61.6) | 57 | (21.3) | 16 | (6.0) |
| Folic acid supplementation | 14 | (5.2) | 170 | (54.1) | 68 | (25.4) | 16 | (6.0) |
| Timing of intercourse to maximize chances of conception | 14 | (5.2) | 114 | (42.5) | 122 | (45.5) | 18 | (6.7) |
Though the instrument did not have open-ended questions, a number of respondents (n = 69, 26%) provided comments indicating they had been unaware of the recommendation for women to take folic acid supplementation and they were pleased to learn from the survey about this important issue. In contrast, a few (n = 11, 4%) stated they did not understand why FP/GPs should provide preconception care.
There were no statistical or clinically meaningful differences between the reports of physicians who reported their specialty as family medicine and physicians who reported their specialty as general internal medicine.
Discussion
The movement to establish family medicine in Japan started at least 20 years ago.[7] There has been much debate about whether Japanese family physicians should provide obstetric and other women's health care. There are few FP/GPs who provide OB care in Japan.[22] Our study reveals that few FP/GPs have educational experiences in the provision of preconception care, and few actually provide this care in their practices. However, it also reveals their willingness to provide preconception care in the future after appropriate educational experiences.
Japanese FP/GPs seem reluctant to inquire about human sexuality issues.[23] In the current study, some reported they could not ask patients about future pregnancy plans during a routine acute visit. Our results show FP/GPs in Japan are not accustomed to addressing preconception-related topics (timing of intercourse, folic acid supplementation, exercise during pregnancy), while they are familiar with more general topics (smoking cessation, screening for anemia, calcium intake). FP/GPs are in the unique position to provide health care services to male and female patients of all ages,[24,25] and they have many opportunities to discuss patients' concerns. For example, young parents do not often visit family physicians for their own health problems, but do come for their children. At these visits, family physicians can also discuss family planning. For this reason, FP/GPs in Japan need training in women's health care, even if they will not provide deliveries in the future. We hope these data will provide a catalyst for dialogue among Japan's FP/GPs about regular provision of preconception counseling.
Remarkably, only 10 % of participants reported knowledge of folic acid supplementation and few reported providing this care. Yamanaka surveyed pregnant women about the importance of folic acid.[26] This research revealed that only 8% reported they knew well about its importance, and 46% stated they did not know at all. Furthermore, the small percentage of participants who knew well about the importance of folic acid reported that they learned it from a newspaper, TV, or magazine, while only 16% learned it from medical professionals. Based on these data, Yamanaka emphasized that medical professionals should provide correct and concise information about folic acid.
As the MHLW only recently recommended folic acid supplementation to reproductive-aged women,[15] it is not too surprising that many FP/GPs do not know the importance of folic acid and few provide this care. The JAFM was not included in the list of organizations notified of the MHLW policy change. Based on these data it is clear that its membership is interested in women's health issues and should be included in notifications about women's health policy changes formulated at the government level.
About 70% of participants reported they are willing to screen women for rubella antibody, though almost 70% reported not providing this care in their practice. Given the historic mistrust of the rubella vaccine and the low rate of vaccination in Japan,[16] Japanese family doctors need to proactively address the topic. The lack of mandatory vaccination is a loophole in public health policy[16] and highlights why screening women of childbearing potential for rubella antibody is especially important. Delay in testing, and hence immunization, leads to an increased risk for congenital rubella, a highly serious disease. Non-immune pregnant women should post-pone rubella vaccination until after delivery.
Japan's FP/GPs must learn to provide preconception counseling in order to close this important gap in women's health. Fortunately, many of these respondents are willing to provide some level of preconception care even though they currently are not – presumably due in part to a lack of educational experience. Japan's FP/GPs need educational materials and clinical tools to encourage women to make an office visit and receive preconception care. Family medicine training in Japan heavily emphasizes adult and geriatric medicine with little emphasis on prenatal, newborn, children, adolescent, or women's health.[7,21,27] Initial efforts to disseminate information about preconception care are underway through the medical literature,[25] though other educational efforts will no doubt be needed. Data from Japanese women from Japan who are on temporary assignment in the United States, illustrate low levels of knowledge about prenatal folic acid supplementation and resistance to take supplements.[28]
A potential limitation of this study is selection bias. The participants are limited to physician members of the JAFM and the data might not reflect the current situation of all FP/GPs in Japan. This bias would likely favor the most motivated physicians and the estimates herein probably represent the upper limits of willingness to provide preconception care by the population of primary care providers in Japan. If this interpretation is correct, the need for public campaigns about the importance of preconception care and training of Japan's family physicians are even more imperative.
Despite compelling evidence of the effectiveness of folic acid supplementation and other preconception care for the reduction of serious birth defects at a very low cost, these data provide evidence that the WHO's message about the importance has not filtered down to the clinical level even in a developed country like Japan. Continued efforts to spread and diffuse the WHO's message are desperately needed for the advancement of maternal-child health.
Conclusion
Our study reveals that many Japan's FP/GPs have limited training in preconception care and few currently provide it. Most participants report their willingness to provide preconception care themselves and educational campaigns are needed to enhance preventive care provided by FP/GPs in Japan.
List of abbreviations used
CBC – complete blood count
FP/GPs – family physicians and general practitioners
IgG – immunoglobulin G
JAFM – Japanese Academy of Family Medicine
mg – milligrams
MHLW – Ministry of Health, Labour and Welfare
OB/GYN – obstetrics and gynecology
RCT – randomized controlled trial
SPSS – Statistical Package for the Social Sciences
WHO – World Health Organization
wk – week
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
KK contributed to the conception and study design, performed data analysis, interpretation, and draft the manuscript. MDF contributed to the conception and study design and critical revision of the manuscript. NB participated in the study design and critical revision of the manuscript. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Acknowledgments
Acknowledgements
We gratefully acknowledge all responding physician members of the Japanese Academy of Family Medicine.
Contributor Information
Kazuya Kitamura, Email: kitayann@zf7.so-net.ne.jp.
Michael D Fetters, Email: mfetters@umich.edu.
Nobutaro Ban, Email: nobuban@med.nagoya-u.ac.jp.
References
- Leuzzi RA, Scoles KS. Preconception counseling for the primary care physician. Medical Clinics of North America. 1996;80:337–374. doi: 10.1016/s0025-7125(05)70444-2. [DOI] [PubMed] [Google Scholar]
- Gjerdingen DK, Fontaine P. Preconception health care: a critical task for family physicians. Journal of the American Board of Family Practice. 1991;4:237–250. [PubMed] [Google Scholar]
- Brundage SC. Preconception health care. American Family Physician. 2002;65:2507–2514. [PubMed] [Google Scholar]
- Muchowski K, Paladine H. An ounce of prevention: The evidence supporting periconception health care. Journal of Family Practice. 2004;53:126–133. [PubMed] [Google Scholar]
- Korenbrot CC, Steinberg A, Bender C, Newberry S. Preconception care: a systematic review. Matern Child Health J. 2002;6:75–88. doi: 10.1023/A:1015460106832. [DOI] [PubMed] [Google Scholar]
- Heyes T, Long S, Mathers N. Preconception care: Practice and beliefs of primary care workers. Family Practice. 2004;21:22–27. doi: 10.1093/fampra/cmh106. [DOI] [PubMed] [Google Scholar]
- Ishibashi Y. Why is family medicine needed in Japan. Journal of Family Practice. 1987;25:83–86. [PubMed] [Google Scholar]
- Lumley J, Watson L, Watson M, Bower C. Periconceptional supplementation with folate and/or multivitamins for preventing neural tube defects. Cochrane Database of Systematic Reviews. 2005;1 [Google Scholar]
- Berry RJ, Li Z, Erickson JD, Li S, Moore CA, Wang H, Mulinare J, Zhao P, Wong LY, Gindler J, Hong SX, Correa A. Prevention of neural-tube defects with folic acid in China. China-U.S. Collaborative Project for Neural Tube Defect Prevention. New England Journal of Medicine. 1999;341:1485–1490. doi: 10.1056/NEJM199911113412001. [DOI] [PubMed] [Google Scholar]
- Czeizel AE, Dudas I. Prevention of the first occurrence of neural-tube defects by periconceptional vitamin supplementation. New England Journal of Medicine. 1992;327:1832–1835. doi: 10.1056/NEJM199212243272602. [DOI] [PubMed] [Google Scholar]
- Wald N. Prevention of neural tube defects: Results of the Medical Research Council Vitamin Study. Lancet. 1991;338:131–137. doi: 10.1016/0140-6736(91)90133-A. [DOI] [PubMed] [Google Scholar]
- Clark NA, Fisk NM. Minimal compliance with the Department of Health recommendation for routine folate prophylaxis to prevent fetal neural tube defects. British Journal of Obstetrics and Gynaecology. 1994;101:709–710. doi: 10.1111/j.1471-0528.1994.tb13190.x. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention Recommendations for the use of folic acid to reduce the number of cases of spina bifida and other neural tube defects. MMWR. 1992;41:1–7. [PubMed] [Google Scholar]
- World Health Organization . Community Genetics. Vol. 2. World Health Organization; 1999. Services for the prevention and management of genetic disorders and birth defects in developing countries; pp. 196–201. [DOI] [PubMed] [Google Scholar]
- Ministry of Health Labor and Welfare . The recommendation of taking folic acid for reproductive-aged women to decrease risk of neural tube defects (Japanese) Vol. 2005. Tokyo, Japan ; 2000. [Google Scholar]
- Miyazaki C. MMR vaccine. Pediatrics of Japan. 2002;43:585–590. [Google Scholar]
- Centers for Disease Control and Prevention (CDC) Revised ACIP recommendation for avoiding pregnancy after receiving a rubella-containing vaccine . MMWR. 2001;50:1117. [PubMed] [Google Scholar]
- American Academy of Pediatrics Fetal alcohol syndrome and fetal alcohol effects. Pediatrics. 1993;91:1004–1006. [PubMed] [Google Scholar]
- Lumley J, Oliver SS, Chamberlain C, Oakley L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database of Systematic Reviews. 2005;1 doi: 10.1002/14651858.CD001055.pub2. [DOI] [PubMed] [Google Scholar]
- Nagaya K, Fetters MD, Ishikawa M, Kubo T, Koyanagi T, Saito Y, Sameshima H, Sugimoto M, Takagi K, Chiba Y, Honda H, Mukubo M, Kawamura M, Satoh S, Neki R. Causes of maternal mortality in Japan. Journal of the American Medical Association. 2000;283:2661–2667. doi: 10.1001/jama.283.20.2661. [DOI] [PubMed] [Google Scholar]
- Smith BW, Demers R, Garcia-Shelton L. Family medicine in Japan. Arch Fam Med. 1997;6:59–62. doi: 10.1001/archfami.6.1.59. [DOI] [PubMed] [Google Scholar]
- Okkes IM, Polderman GO, Fryer GE, Yamada T, Bujak M, Oskam SK, Green LA, Lamberts H. The role of family practice in different health care systems: a comparison of reasons for encounter, diagnoses, and interventions in primary care populations in the Netherlands, Japan, Poland, and the United States. J Fam Pract. 2002;51:72–73. [PubMed] [Google Scholar]
- Ban N. Medical interview: How to evoke sex-related issues (Japanese) Journal of International Medicine. 2001;11:697–700. [Google Scholar]
- Narato K. What is a family physician (Japanese) In: Japanese Academy of Family Medicine, editor. The Introduction of Family Physicians and Primary Care Physicians. Osaka , Premaid Press; 2001. pp. 18–22. [Google Scholar]
- Kitamura K, Ban N. Family physicians and preconception care (Japanese) Japanese Journal of Family Practice. 2002;9:89–94. [Google Scholar]
- Yamanaka M. Folic acid can prevent neural tube defect: The importance is not recognized (Japanese) Medical Tribune. 2002;8:16. [Google Scholar]
- Kitamura K, Fetters MD, Ban N. The experiences of Japanese generalist physicians in overseas faculty development programs. Family Medicine. 2002;34:761–765. [PubMed] [Google Scholar]
- Yeo SA, Fetters MD, Maeda Y. Japanese couples' childbirth experiences in Michigan: Implications for care. Birth. 2000;27:191–198. doi: 10.1046/j.1523-536x.2000.00191.x. [DOI] [PubMed] [Google Scholar]