Abstract
Objective To compare the effectiveness of the Bug Buster kit with a single treatment of over the counter pediculicides for eliminating head lice.
Design Single blind, multicentre, randomised, comparative clinical study.
Setting Four counties in England and one county in Scotland.
Participants 133 young people aged 2-15 years with head louse infestation: 56 were allocated to the Bug Buster kit and 70 to pediculicide treatment.
Interventions Home use of proprietary pediculicides (organophosphate or pyrethroid) or the Bug Buster kit.
Main outcome measure Presence of head lice 2-4 days after end of treatment: day 5 for the pediculicides and day 15 for the Bug Buster kit.
Results The cure rate using the Bug Buster kit was significantly greater than that for the pediculicides (57% v 13%; relative risk 4.4, 95% confidence interval 2.3 to 8.5). Number needed to treat for the Bug Buster kit compared with the pediculicides was 2.26.
Conclusion The Bug Buster kit was the most effective over the counter treatment for head louse infestation in the community when compared with pediculicides.
Introduction
Infestation with head lice, Pediculosis capitis, is a widespread, persistent, and recurring problem and although it poses no direct threat to health, it may lead to secondary infections if untreated.1 The mere presence of head lice may cause distress to children and their families.2,3 Previous studies of insecticides have reported treatment failure in laboratory bioassays4-9 and field trials.4,5,9,10 Systematic reviews have identified several flaws in earlier study designs,11,12 and a clinical review of best practice compared the merits of each class of pesticide currently available.13 Several possible mechanisms for resistance in head lice have been reported.4,5,9,14 Treatment failure is likely to be an important factor in the reported rise in the incidence of head lice infestation, but of concern is the increased risk of toxicity this may pose to children. Although current insecticides registered for use against head lice are generally considered safe for occasional use,15 they may pose a greater risk of direct or cumulative toxicity if used frequently.
Wet combing with conditioner was first developed as a method of detecting head lice and was subsequently advocated as a means of treatment (“Bug Busting”) by the UK charity Community Hygiene Concern.16 The method involves using a fine toothed comb on thoroughly wet hair. Over several years the charity has developed and trialled a Bug Buster kit comprising instructions and materials to undertake four sequential combings on wet, conditioned hair, leaving three days between each.2 A recent Cochrane review highlighted the need for a clinical evaluation of the kit.11 The only randomised controlled trial to date was carried out in two Welsh counties, an area with head lice showing intermediate resistance to treatment.10 The cure rate for the kit was only 38% compared with 78% for two doses of 0.5% malathion lotion six days apart.10 This early study used a prototype kit (1996 version), which has since undergone major developments in the design of the comb for removing small nymphs. We compared the effectiveness of the current (1998) Bug Buster kit with over the counter pediculicides containing malathion or permethrin among representative populations from four counties in England and one county in Scotland. We aimed to measure the effectiveness of the treatments under realistic conditions, as used by people in practice following the recommendations of the manufacturers.
Methods
Participants were recruited through general practices in Bedfordshire, Cornwall, Cumbria, Dumfries and Galloway, and Surrey. The general practitioners were contacted by the study coordinator or local study nurse and given full details of the study with an invitation to take part. To widen participation to reflect the broader community, school nurses placed posters in local pharmacies and primary schools and the study nurses in Surrey and Cumbria handed out information sheets at parents' meetings. We aimed to recruit from families who would normally go to their general practitioner for advice on head louse treatment or would buy treatment from pharmacies. We had no upper age limit for the study, but participants were aged up to 15 years. A lower age limit of 2 years was chosen for safety reasons.
The general practitioner or community nurse recruited infested young people into the trial if they had a live head louse, they had had no treatment for head lice in the previous three weeks, they or their guardian agreed not to use other head louse treatments during the trial, they or their guardian had provided written informed consent, and the guardian agreed that the immediate family would be examined for lice and, if necessary, given the same treatment as allocated to the family member with confirmed head louse infestation.
Design
For ethical reasons, we did not use a conventional double blind, randomised, placebo controlled trial. We therefore carried out a randomised, comparative study of the Bug Buster kit against the currently recommended insecticide products in any given area. The specimen louse from the confirmed index case was removed by the general practitioner or community nurse and stuck on a record card for later confirmation by the local study nurse. Only this one participant from each family who fulfilled the inclusion criteria was included in later analysis after being randomly assigned to one of two treatment arms: the Bug Buster kit (Community Hygiene Concern: London) or a proprietary bottle of insecticide treatment containing either 0.5% aqueous malathion (Derbac-M; Seton-Scholl Healthcare, Oldham) or aqueous permethrin (1% Lyclear, crème rinse; Warner Lambert UK, Eastleigh). We chose two different insecticides on pragmatic grounds, as accessibility to treatment varies nationwide according to local policy. We selected aqueous solutions of insecticides as opposed to those with an alcohol base because they are widely used formulations and are suitable for people with asthma.
The Bug Buster kit is dispensed over the counter or through mail order. A survey of 92 pharmacies in our study areas (NH, unpublished data) found just 8% of outlets that offered the additional information of double dosing when a pediculicide was purchased. For this reason we provided no additional information on how to use the products other than that supplied with the products. Participants allocated to the Bug Buster kit used their own conditioner. The general practitioners stressed the importance of checking for lice in family members and reporting any finds. Each participating general practitioner was assigned an individual randomisation list at the start of the trial, generated using Minitab 11.0 for Windows, and provided with supplies of the treatments.
Participants were visited at home by the study coordinator or local study nurse or were asked to return to their surgery for follow-up five days after application of the pediculicides or 15 days after the start of the Bug Buster regimen. We decided to use different end points as the duration of treatments varied. We chose day 5 for pediculicides and day 15 for the Bug Buster kit to allow sufficient time for treatments to be completed and to provide a similar opportunity for reinfestation to occur (2-4 days after completion of treatment in each case). We did not evaluate ovicidal activity.
The study nurses attended a one day workshop on louse detection using the wet combing with conditioner method (combing wet and conditioned hair from root to tip across the whole scalp with a fine toothed comb, then repeated in rinsed hair). The nurses, unaware of treatment allocation, used this method at each follow-up. They recorded the presence, number, and stage of lice. From this we determined cure (no live lice) or failure (one or more live lice). Lice were stored at -20°C for detection of molecular or biochemical resistance mechanisms, specifically kdr-type mutations from genomic DNA.14 Participants or their guardians in both groups completed a simple questionnaire to determine compliance and satisfaction with the treatment and to obtain basic epidemiological information, including age, sex, number of siblings, history of head louse infestation and treatment, and recent use of antibiotics.
Statistical analysis
We calculated that we would need a sample size of 98 (49 in each arm) to detect a 30% difference between the two groups (80% for one treatment, 50% for the other), with a power of 80% and 5% significance (Stata 8.1). We analysed the data from those participants who completed the study and provided outcome data. We carried out a univariate analysis using Yates corrected χ2 test in Epi Info (version 6) to test the effect of treatment type (the relative risk) on cure rate. To estimate the effect of missing data for participants who were allocated treatment but did not complete the study, we used extreme case analysis. The number needed to treat was calculated.
Results
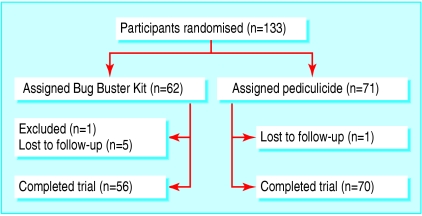
A total of 133 young people aged 2-15 years were recruited and received treatment: 66 from Bedfordshire, 15 from Cornwall, 34 from Cumbria, 4 from Dumfries and Galloway, and 14 from Surrey (figure). One participant from Surrey allocated the Bug Buster kit was excluded for also using an insecticide, and six participants were lost to follow-up (three each from Cumbria and Surrey; five received the Bug Buster kit and one malathion). We analysed the data on the remaining 126 participants who completed the study: 56 were allocated to the Bug Buster kit, 40 to permethrin, and 30 to malathion. The characteristics of the two groups were well matched at baseline (table 1).
Figure 1.
Flow of participants through trial
Table 1.
Baseline descriptive characteristics of participants with outcome data who were allocated to Bug Buster kit or pediculicide for eliminating head lice
| Characteristic | Bug Buster kit (n=56) | Pediculicide (n=70) |
|---|---|---|
| Mean (SD) age (years) | 7.66 (2.62) | 6.91 (2.42) |
| % (No) female | 77 (43) | 81 (57) |
| Mean (SD) No of children per family | 2.18 (0.94) | 2.06 (0.92) |
| % (No) who had past infestation | 79 (44) | 77 (54) |
The cure rates for malathion and permethrin were 17% (5/30) and 10% (4/40). The cure rate for the Bug Buster kit was significantly greater than that for the pediculicides (57% versus 13%; relative risk 4.4, 95% confidence interval 2.3 to 8.5; table 2). The significant difference remained after extreme case analysis, which included missing outcome data and assumed that all six missing or excluded participants allocated the Bug Buster kit were not cured but that the missing individual allocated insecticide was—that is, cure rates of 52% (32/62) and 14% (10/71), respectively (relative risk 3.7, 2.0 to 6.8). We determined that for every two or three people using the Bug Buster kit rather than pediculicides an extra person would be cured (number needed to treat 2.26).
Table 2.
Outcome measures at follow-up for participants allocated Bug Buster kit or pediculicide for eliminating head lice
|
Bug Buster kit (15 days)
|
Pediculicide (5 days)
|
|||||
|---|---|---|---|---|---|---|
| Analysis | Total | % (No) cured | Total | Cured | P value | Relative risk (95% CI) |
| Participants with complete outcome data | 56 | 57 (32) | 70 | 13 (9) | <0.0001 | 4.4 (2.3 to 8.5) |
| Assuming treatment failure for participants with missing data | 62 | 52 (32) | 71 | 13 (9) | <0.0001 | 4.1 (2.1 to 7.8) |
| Assuming treatment failure for participants with missing data in Bug Buster group but success in insecticide group* | 62 | 52 (32) | 71 | 14 (10) | <0.0001 | 3.7 (2.0 to 6.8) |
Extreme case analysis.
Head louse infestation occurred for the first time in 22% of the young people examined. In families of young people with previous head lice infestations, 55% usually went to their general practice for a pediculicide prescription and the remainder purchased treatment from a pharmacist or sought advice from friends. We had no reports of recent antibiotic use and no reports of lice among the family members of recruits during the trial.
Discussion
The Bug Buster kit was four times more effective than current over the counter pediculicides for eliminating head lice. This finding is contrary to a previous study in Wales in which malathion treatment was twice as effective as the Bug Buster regimen.10 It seems likely that the higher cure rate with the Bug Buster kit in our study is a result of improvements to the fine toothed comb, as this was the only major change. If so, it suggests that the success of fine toothed combing depends on the choice of comb. The effectiveness of the pediculicides was much lower in our trial than in the Welsh trial, and much more in line with the results from a previous trial in Bristol, which reported cure rates of 13% for permethrin and 36% for malathion.4
This discrepancy may be accounted for in several ways. Firstly, we used the manufacturer's recommended single dose of insecticide rather than two doses six days apart, which is now considered an unlicensed use.15 Owing to the limited residual effect, a double dose is likely to have greater success in killing nymphs that emerge from eggs not destroyed by the first dose. Secondly, our follow-up time was five days rather than seven days after insecticide treatment, as in the Welsh trial, but this is unlikely to have led to an underestimate of the cure rate given the lack of a significant residual effect. A longer period before measurement of outcomes increases the chance of nymphs emerging and being detected, and also increases the risk of reinfestation. Thirdly, we used an aqueous formulation rather than an alcohol one so that we could include people with allergies. The Welsh trial used either formulation, according to whether participants had allergies, but did not report any difference in effectiveness between the two. Fourthly, we recruited only people whose lice infestation had been reported by their families, rather than using school nurses to find cases by screening with fine toothed combs as in the Welsh trial. Our study population was reasonably representative of the population who normally seek treatment for head lice, as the ratio of those who had previously sought treatment from pharmacies or their doctors was similar to that reported in the national population.17 For several reasons we therefore believe our trial better reflects how over the counter products are used in the community.
Finally, the discrepancy may also be due to differences in resistance to insecticide, as our trial was carried out after the Welsh trial and included a range of urban settings. The particularly poor effectiveness of permethrin is likely to be due to widespread kdr-type resistance; all but one of the lice from treatment failures collected in this study were found to have the T929I and L932F resistant genotype mutations of the paratype sodium channel gene (MSW, unpublished data). On the basis of these and earlier similar findings we believe that the status of licensed insecticide treatments needs to be assessed as they potentially expose users to repeat applications without any important reduction in infestations.
The updated Bug Buster kit seems to provide a viable alternative to over the counter insecticide treatments. An observational study in Ghent, Belgium reported promising findings on satisfaction with wet combing as a treatment.18 In this study, families of head lice infested schoolchildren were given impartial advice on treatment options and then allowed to choose the treatment; most chose wet combing with conditioner (29%) over pediculicides (19%) or a combination of the two (15%), which suggests the Bug Buster regimen may be readily taken up by the community.
Some may consider that the cure rate of only 57% we detected with the Bug Buster kit is still unacceptable and may not provide an efficient treatment against head lice. At present there are no readily available products that provide fully effective control of head lice, and there is an urgent need to identify safe, novel insecticides of proved efficacy.
What is already known on this topic
Head lice have varying degrees of resistance to over the counter pediculicides
Fine tooth combing of wet hair is an effective method of detecting head lice but unproved as a treatment
What this study adds
Effectiveness of popular over the counter pediculicides for eliminating head lice is poor
The kdr-type resistance mechanism to pyrethroids is widespread in head lice in the United Kingdom
The Bug Buster kit is significantly more effective than common over the counter pediculicides for normal unsupervised use
We thank the general practices and participants involved in the study; Sir D Hall, M Nilsson, and J Figueroa for advice during the design and implementation of the study; and C Davies for his comments on the manuscript. J Gutmanis, J Dunstan, and J McNicol helped with access to head louse cases in Cornwall and Dumfries and Galloway.
Contributors: NH initiated the research, secured funding, and led the design of the study; he is guarantor. MMC led the analysis of data and writing the report. GM coordinated the trial and with AB and SP participated in the fieldwork and contributed to writing the report. MSW and CB carried out the analysis of kdr-type resistance mutations.
Funding: Health and social research grant from the Big Lottery Fund (formerly the National Lottery Charities Board) awarded to Community Hygiene Concern in collaboration with the London School of Hygiene and Tropical Medicine.
Competing interests: NH has received funding over the past 10 years to screen pediculicides but not products or companies involved in this study.
Ethical approval: London School of Hygiene and Tropical Medicine research ethics committee, London multicentre research ethics committee, and individual local research ethics committees of the health authorities in each study area.
References
- 1.Gratz N. Human lice—their prevalence, control and resistance to insecticides. Geneva: World Health Organization, 1997. (WHO/CTD/WHOPES/97.8.)
- 2.Figueroa J, Hall S, Ibarra J. Primary health care guide to common UK parasitic diseases. London: Community Hygiene Concern, 1998: 1-16.
- 3.Figueroa JI. Head lice: is there a solution? Curr Opin Infect Dis 2000;13: 135-9. [DOI] [PubMed] [Google Scholar]
- 4.Downs AMR, Stafford KA, Harvey I, Coles GC. Evidence for double resistance to permethrin and malathion in head lice. Br J Dermatol 1999;141: 508-11. [DOI] [PubMed] [Google Scholar]
- 5.Bingham P, Kirk S, Hill N, Figueroa J. The methodology and operation of a pilot randomized control trial of the effectiveness of the Bug Busting method against a single application insecticide product for head louse treatment. Public Health 2000;114: 265-8. [DOI] [PubMed] [Google Scholar]
- 6.Burgess I. Carbaryl lotions for head lice—new laboratory tests show variations in efficacy. Pharm J 1990;245: 159-61. [Google Scholar]
- 7.Burgess I. Malathion lotions for head lice—a less reliable treatment than commonly believed. Pharm J 1991;247: 630-2. [Google Scholar]
- 8.Burgess IF, Peock S, Brown CM, Kaufman J. Head lice resistant to pyrethroid insecticides in Britain. BMJ 1995;311: 752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Downs AMR, Stafford KA, Hunt LP, Ravenscroft JC, Coles GC. Widespread insecticide resistance in head lice to the over-the-counter pediculicides in England, and the emergence of carbaryl resistance. Br J Dermatol 2002;146: 88-93. [DOI] [PubMed] [Google Scholar]
- 10.Roberts RJ, Casey D, Morgan DA, Petrovic M. Comparison of wet combing with malathion for treatment of head lice in the UK: a pragmatic randomised controlled trial. Lancet 2000;356: 540-4. [DOI] [PubMed] [Google Scholar]
- 11.Dodd CS. Interventions for treating head lice. Cochrane Database Syst Rev 2001;(2): CD001165. [DOI] [PubMed]
- 12.Vander Stichele RH, Dezeure EM, Bogaert MG. Systematic review of clinical efficacy of topical treatments for head lice. BMJ 1995;311: 604-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nash B. Treating head lice. BMJ 2003;326: 1256-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee SH, Yoon KS, Williamson MS, Goodson SJ, Takano-Lee M, Edman JD, et al. Molecular analysis of kdr-like resistance in permethrin-resistant strains of head lice, Pediculus capitis. Pestic Biochem Physiol 2000;66: 130-43. [Google Scholar]
- 15.British Medical Association, Royal Pharmaceutical Society of Great Britain. British national formulary. BMA, RPS, 2004: 589-90 (No 48.).
- 16.Ibarra J. Pediculus capitis: the prevention and treatment of head lice. Nurse Prescribing 2005;3: 810-3. [Google Scholar]
- 17.Purcell S. Practical ways with parasites. Chemist Druggist 1998;250: 14-6. [Google Scholar]
- 18.Vander Stichele RH, Gyssels L, Bracke C, Meersschaut F, Blokland I, Wittouck E, et al. Wet combing for head lice: feasibility in mass screening, treatment preference and outcome. J R Soc Med 2002;95: 348-52. [DOI] [PMC free article] [PubMed] [Google Scholar]