Abstract
Environmental noise is a significant public health concern, ranking among the top environmental risks to citizens’ health and quality of life. Despite extensive research on atmospheric pollution’s impact on mental health, spatial studies on noise pollution effects are lacking. This study fills this gap by exploring the association between noise pollution and depression in England, with a focus on localised patterns based on area deprivation. Depression prevalence, defined as the percentage of patients with a recorded depression diagnosis, was calculated for small areas within Cheshire and Merseyside ICS using the Quality and Outcomes Framework Indicators dataset for 2019. Strategic noise mapping for rail and road noise (Lden) was used to measure 24-h annual average noise levels, with adjustments for evening and night periods. The English Index of Multiple Deprivation (IMD) was employed to represent neighborhood deprivation. Geographically weighted regression and generalised structural equation spatial modeling (GSESM) assessed the relationships between transportation noise, depression prevalence, and IMD at the Lower Super Output Area level. The study found that while transportation noise had a low direct effect on depression levels, it significantly mediated other factors associated with depression. Notably, GSESM showed that health deprivation and disability were strongly linked (0.62) to depression through the indirect effect of noise, especially where transportation noise exceeds 55 dB on a 24-h basis. Understanding these variations is crucial for developing noise mitigation strategies. This research offers new insights into noise, deprivation, and mental health, supporting targeted interventions to improve quality of life and address health inequalities.
Keywords: Noise pollution, Urban soundscape, Depression, Healthy aging, Transportation noise, Spatial
Introduction
The increased demand for aircraft, road, and railway transportation as a result of urbanisation has also increased noise pollution. Researchers, policymakers, and urban planners have devoted great attention to this matter as noise pollution is regarded as the second greater environmental stressor impacting human health and well-being, after air pollution [1].
According to the World Health Organization (WHO), noise has been recognised as the top environmental risk to health [2]. It is estimated that around a hundred million people in the European Union are influenced by traffic-related noise, according to the EU’s Environmental Noise Directive, and traffic-related noise alone in Western Europe is responsible for almost 1.6 million healthy years of life lost each year [3]. Also, there have been indications that at least 1 million deaths every year in Western Europe are a result of traffic-related noise [4].
In October 2022, the Journal of Mental Health editorial—an international forum for the latest research in the mental health field—quoted that there have been many studies that discussed the effects of the environment on mental health and have occasionally noted the possible ill effects of atmospheric pollution. A surprising omission, however, has been any discussion of the effects of noise pollution on mental health [5]. The exact quote was that “the extent to which the effects of noise on mental health are omitted from research is irritating.” There are many studies where noise pollution has simply not been taken into account. Furthermore, a recent systematic literature review and meta-analysis revealed that the current evidence regarding the link between traffic noise and depression is of a “very low” quality [6].
In the UK, research exploring the impact of noise pollution on mental health is also scarce [5], and given the existing mental health burden, this area of research presents a promising avenue for further investigation and for promoting the benefits of hearing conservation as a way to protect the population’s mental health. Furthermore, a review of the evidence in the WHO European Region revealed that the burden of noise seems to be unequally distributed in societies, calling for research on the social distribution of environmental noise exposure on a small spatial scale [3].
Therefore, the aim of this study was (a) to explore the link between noise pollution (from road and rail network) and depression in Cheshire and Merseyside Integrated Care System (ICS) and (b) investigate potential localised patterns according to area deprivation.
Material and Methods
Data Sources
To quantify noise pollution, we used the strategic noise mapping for rail and road noise (Lden) [7]. Lden indicates a 24-h annual average noise level with separate weightings for the evening and night periods, and we calculated the 24-h annual average noise levels in small areas in Cheshire and Merseyside ICS.
Our primary outcome measure was depression prevalence, defined as the percentage of patients with a diagnosis of depression in their medical records. We calculated depression prevalence in small areas in Cheshire and Merseyside ICS in 2019, extracting respective values from the dataset on Quality and Outcomes Framework Indicators: Depression prevalence (QOF_4_12) Version 1.00 [8].
To represent deprivation within these smaller areas, we utilised the English Index of Multiple Deprivation (IMD). The IMD is a widely used statistic within the UK that provides measures of relative deprivation in small areas in England. In our analyses, we used the latest English Index of Multiple Deprivation (IMD 2019), which measures relative deprivation in small areas in England [9].
All geospatial models employed in the study focused on the Lower Super Output Area (LSOA) as the unit of analysis. Cheshire and Merseyside (ICS) encompass 1562 LSOAs, each with an average population of 1500 individuals, according to data from the Office for National Statistics as of 21 March 2021 [10]. Furthermore, to facilitate comparisons among sub-Integrated Care Board locations in Cheshire and Merseyside ICS (Cheshire, Halton, Knowsley, Liverpool, South Sefton, Southport and Formby, St Helens, Warrington, and Wirral), digital vector boundaries for Integrated Care Boards in England were incorporated in the analyses [11].
Analytical Approach
The percentage of road and rail noise coverage was calculated based on intensity in dB within each LSOA in Cheshire and Merseyside. We considered five categories based on the 24-h annual average noise levels: 55–59.9 dB, 60–64.9 dB, 65–69.9 dB, 70–74.5 dB, and ≥ 75 dB. We calculated noise separately for rail and road noise in each area. Additionally, to assess the overall impact of rail and road noise in each area, we combined the two noise databases and calculated the total road and rail noise coverage for the 24-h annual average noise, considering noise levels exceeding 55 dB, and then subtracting the intersecting area.
The prevalence of depression was described with minimum and maximum values, central tendency measures (mean and median), and dispersion measures (range and standard deviation).
We employed geographical weighted regression and generalised structural equation spatial modeling (GSESM) to estimate the relationship between transportation noise, depression prevalence, and IMD. Mediation models (and the indirect effects) were tested with ordinary least squared (OLS) regression analyses using ArcGIS pro 2.9.2 OLS tool. We applied the four-step approach [12] to examine several OLS regression analysis models and examined the significance of the coefficients at each step to find the best-fitting path models. Next, we calculate the significance of mediation in the structural equation modeling by computing the difference between two regression coefficients [13]. Exponentiated coefficients and summary statistics are presented for each stage.
Statistical significance was set at the 99% confidence level. Analyses were performed in ArcGIS Pro Version 2.9.2 [14] using the following tools, in order of execution: Union, Tabulate Intersection, Spatial Join tool, the Analysis Toolbox, and the Spatial Statistic Toolbox.
Results
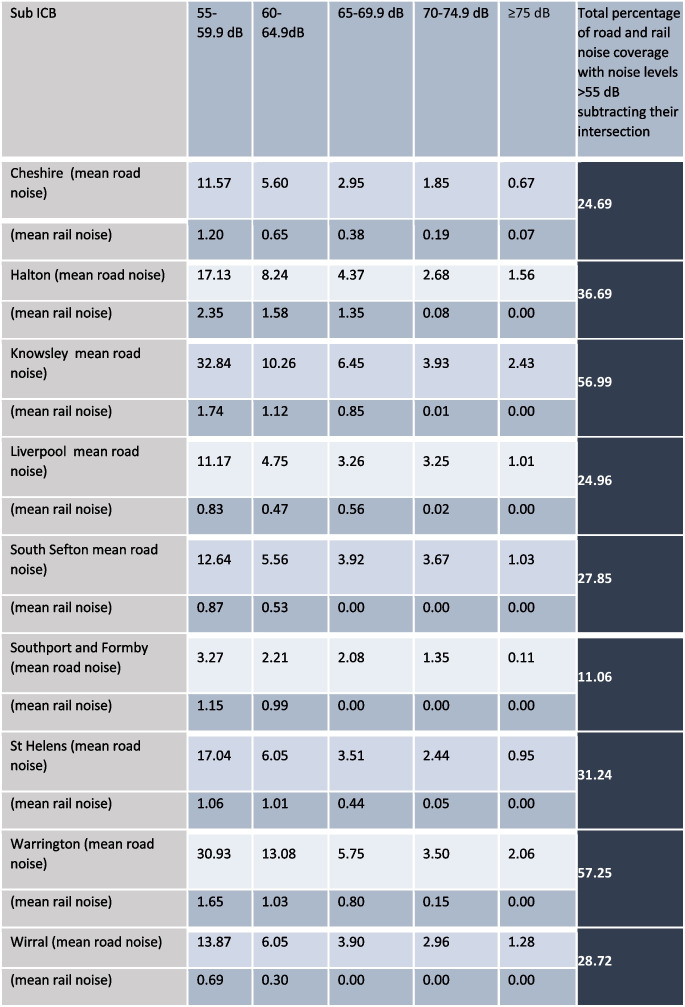
Table 1 shows the summary statistics for the percentage of road and rail noise coverage based on intensity in dB within each of the local authorities in Cheshire and Merseyside. We found that Knowsley had the highest coverage of areas exposed to road noise on a 24-h basis, followed by Warrington. Halton had the highest coverage of areas exposed to rail noise on a 24-h basis, followed by Warrington and Cheshire. Combining road and rail noise, we found that Warrington and Knowsley had the highest percentage of noise coverage, with over half of their respective areas exposed to transportation noise exceeding 55 dB on a 24-h basis. Figure 1 illustrates the correlation between areas with transportation noise levels of 55 dB or higher and the prevalence of depression, with brown denoting areas that experienced both high transportation noise and high depression prevalence in 2019.
Table 1.
Summary statistics for the mean road and rail noise coverage percentage (%) and dB levels in Cheshire and Merseyside ICS in 2019
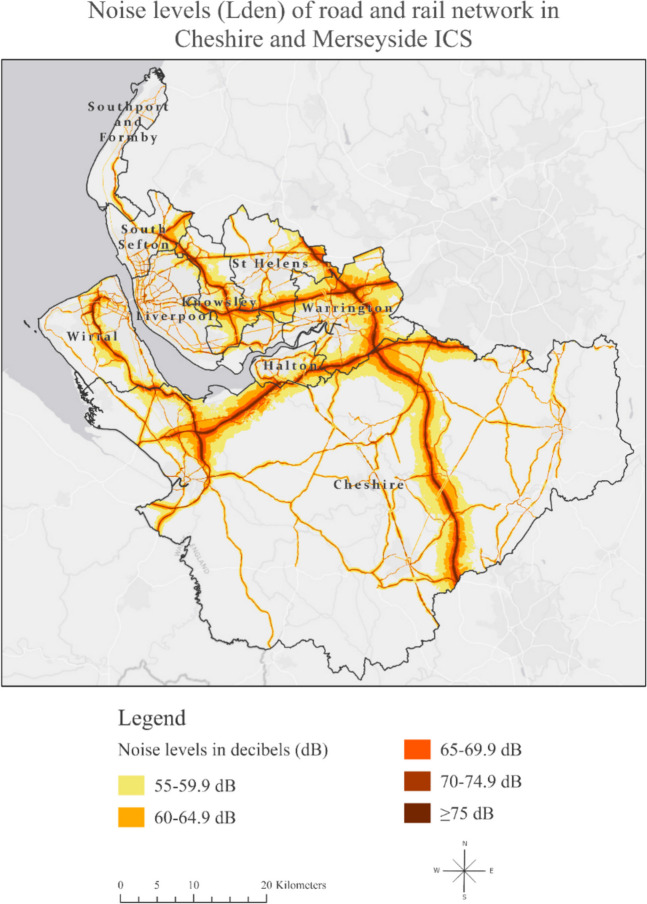
Fig. 1.
Noise levels of road and rail network in Cheshire and Merseyside ICS based on data derived from strategic noise mapping [7]
The summary statistics of depression prevalence in 2019 are shown in Table 2. Knowsley had the highest percentage of depression. Additionally, as we saw earlier, Knowsley also had the highest coverage of areas exposed to road noise on a 24-h basis, along with the highest percentage of total noise coverage. In fact, over half of their respective area was exposed to transportation noise exceeding 55 dB on a 24-h basis.
Table 2.
Summary statistics of recorded depression prevalence in Cheshire and Merseyside ICS in 2019
| Sub ICB | Number of LSOA | Mean | Median | Minimum | Maximum | Range | Standard deviation |
|---|---|---|---|---|---|---|---|
| Cheshire | 446 | 11.62 | 11.54 | 5.03 | 16.09 | 11.06 | 2.05 |
| Halton | 79 | 14.66 | 15.48 | 10.42 | 19.01 | 8.59 | 2.27 |
| Knowsley | 98 | 15.92 | 16.36 | 9.63 | 20.74 | 11.10 | 2.66 |
| Liverpool | 298 | 12.74 | 12.47 | 7.95 | 21.48 | 13.53 | 2.38 |
| South Sefton | 111 | 12.96 | 13.03 | 8.33 | 17.99 | 9.66 | 2.27 |
| Southport and Formby | 78 | 11.26 | 12.12 | 8.44 | 16.10 | 7.66 | 2.32 |
| St Helens | 119 | 15.14 | 15.32 | 10.17 | 18.50 | 8.33 | 1.47 |
| Warrington | 127 | 12.55 | 12.65 | 7.11 | 18.20 | 11.10 | 3.00 |
| Wirral | 206 | 16.42 | 16.60 | 10.88 | 25.51 | 14.62 | 3.17 |
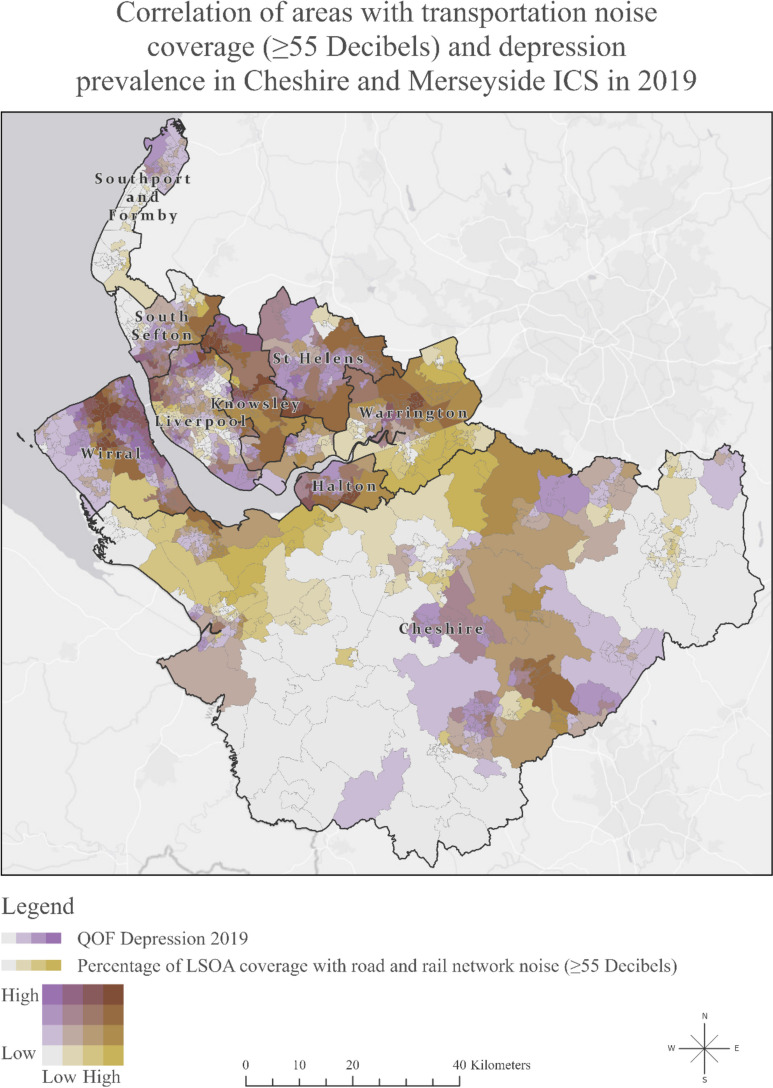
Figure 2 illustrates the correlation between areas with transportation noise levels of 55 dB or higher and the prevalence of depression. Darker shades of purple represent higher depression prevalence, while darker shades of green indicate a greater extent of road and rail network noise coverage exceeding 55 dB in that region. We can also observe their combined interaction, with the brown colour denoting areas that experienced both high transportation noise and high depression prevalence.
Fig. 2.
Map of Cheshire and Merseyside Integrated Care System showing the correlation of areas with transportation noise coverage (> 55 dB) and depression prevalence in 2019
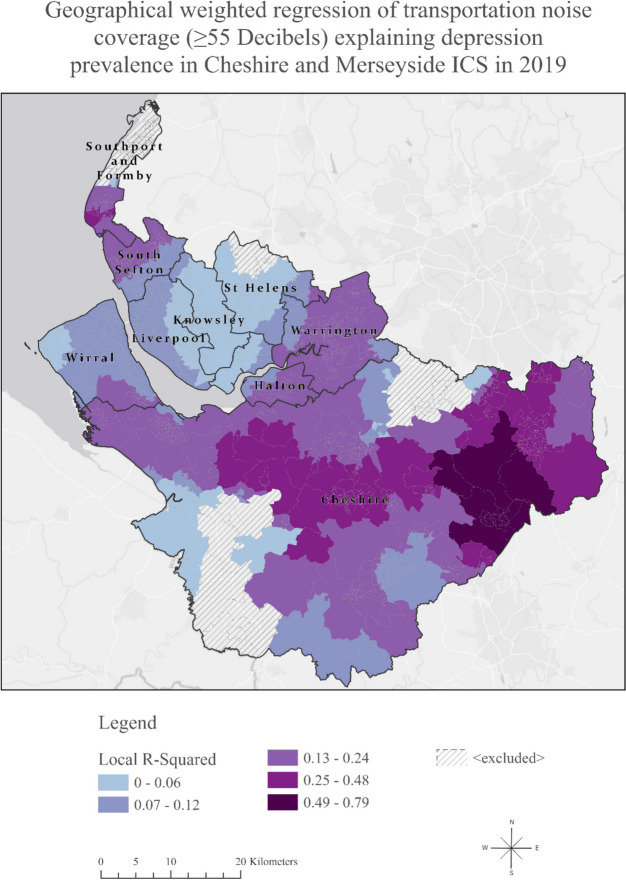
Figure 3 depicts the data on noise coverage 55 dB and above and depression in 2019 using the coefficients that show the correlation strength of the variables over space. The darker areas do not indicate where there is the highest noise pollution or highest depression prevalence; rather, they reveal where the relationship between noise pollution and depression is the strongest, informed by the results of geographical weighted regression (GWR) [15]. As we see, the local R-squared varies across the ICS, which shows that transportation noise may be a strong predictor of depression in one area, explaining up to 79% of the variance in depression in 2019 across the ICS. Summarised results of GWR between noise coverage and the prevalence of depression in 2019 in ICS are shown in Table 3.
Fig. 3.
Geographically weighted regression analysis: examining the relationship between transportation noise coverage and depression prevalence in Cheshire and Merseyside ICS, 2019
Table 3.
Summary statistics of the geographically weighted regression analysis: exploring the relationship between transportation noise coverage and depression prevalence in Cheshire and Merseyside ICS, 2019
| Sub ICB | Number of LSOA | Mean | Median | Minimum | Maximum | Range | Standard deviation |
|---|---|---|---|---|---|---|---|
| Cheshire | 446 | 0.18 | 0.15 | − 1.40 | 0.79 | 2.20 | 0.20 |
| Halton | 79 | 0.10 | 0.10 | 0.02 | 0.18 | 0.16 | 0.05 |
| Knowsley | 98 | 0.03 | 0.03 | 0.01 | 0.08 | 0.06 | 0.02 |
| Liverpool | 298 | 0.06 | 0.06 | 0.02 | 0.09 | 0.07 | 0.01 |
| South Sefton | 111 | 0.12 | 0.12 | 0.08 | 0.23 | 0.15 | 0.03 |
| Southport and Formby | 78 | − 0.03 | − 0.09 | − 0.19 | 0.27 | 0.46 | 0.14 |
| St Helens | 119 | 0.03 | 0.02 | − 0.05 | 0.13 | 0.18 | 0.03 |
| Warrington | 127 | 0.14 | 0.15 | 0.07 | 0.17 | 0.09 | 0.02 |
| Wirral | 206 | 0.08 | 0.08 | 0.02 | 0.13 | 0.11 | 0.02 |
Table 4 presents the results of GSESM. The analyses included the following four steps:
OLS regression analysis with all IMD domain scores predicting depression (step 1)
OLS regression analysis with all previously shown significant IMD domain scores predicting the percentage of environmental noise covered area per LSOA (step 2)
OLS regression analysis with the percentage of environmental noise covered area per LSOA predicting depression (step 3)
OLS significant IMD domain scores and environmental noise covered area per LSOA predicting depression (step 4)
Table 4.
Standardised effects of the generalised structural equation spatial modeling (GSESM) mediation analyses of transportation in QOF-Depression 2019 in Merseyside
| Step 1 | ||||
| IMD domain scores predicting QOF-depression | ||||
| Variable | Coefficienta | StdError | Robust Prb | |
| Income Deprivation | 11.673728 | 4.529014 | 0.005266* | |
| Employment Deprivation | − 3.623193 | 4.176416 | 0.385884 | |
| Education Skills and Training | 0.024592 | 0.007433 | 0.000852* | |
| Health Deprivation and Disability | 2.427641 | 0.201203 | 0.000000* | |
| Crime | − 0.032888 | 0.123761 | 0.7879 | |
| Barriers to Housing and Services | − 0.000566 | 0.007941 | 0.93813 | |
| Living Environment Deprivation | − 0.008936 | 0.004558 | 0.039140* | |
| Income Deprivation Affecting Children Index | − 2.215866 | 1.525089 | 0.091695 | |
| Income Deprivation Affecting Older People Index | − 12.597069 | 1.339679 | 0.000000* | |
| IMD predicting environmental noise | ||||
| Variable | Coefficienta | StdError | Robust Prb | |
| Income Deprivation Domain | − 84.985235 | 23.092033 | 0.000079* | |
| Education Skills and Training | 0.296406 | 0.088988 | 0.000615* | |
| Health Deprivation and Disability | 5.524358 | 2.041461 | 0.005514* | |
| Living Environment Deprivation | − 0.175043 | 0.051252 | 0.000082* | |
| Income Deprivation Affecting Older People Index | 19.430965 | 14.423783 | 0.108445 | |
| Step 3 | ||||
| Environmental noise per LSOA predicting depression | ||||
| Variable | Coefficienta | StdError | Robust Prb | |
| Environmental noise per LSOA | 0.015926 | 0.002496 | 0.000000* | |
| Step 4 | ||||
| IMD domain scores and environmental noise per LSOA predicting depression | ||||
| Variable | Coefficienta | StdError | Robust Prb | |
| Income Deprivation | − 2.327198 | 1.633573 | 0.24096 | |
| Education Skills and Training | 0.021382 | 0.007307 | 0.005960* | |
| Health Deprivation and Disability | 1.809736 | 0.161545 | 0.000000* | |
| Living Environment Deprivation | − 0.011395 | 0.004196 | 0.005322* | |
| Environmental noise per LSOA | 0.011346 | 0.002074 | 0.000000* | |
| Calculation of indirect effect (Judd & Kenny Difference of Coefficients Approach) | ||||
| Variable | Step 1 coefficient | Step 4 coefficient | Indirect effect of transportation noise (step1–step4 coefficients) | Robust Prb |
| Education Skills and Training | 0.024592 | 0.021382 | 0.00321 | 0.000000* |
| Health Deprivation and Disability | 2.427641 | 1.809736 | 0.617905 | 0.000000* |
| Living Environment Deprivation | − 0.008936 | − 0.011395 | 0.002459 | 0.000000* |
*An asterisk next to a number indicates a statistically significant p-value (p < 0.01)
aCoefficient: represents the strength and type of relationship between each explanatory variable and the dependent variable
bRobust probability (Robust Pr): asterisk (*) indicates a coefficient is statistically significant (p < 0.01)
Through steps 1–4, we established that zero-order relationships among the variables exist to establish that IMD and percentage of environmental noise covered area per LSOA have mediating effects.
The calculation of indirect effect through the Judd & Kenny Difference of Coefficients Approach [13] suggested that although transportation noise had low direct effect in explaining depression levels in Cheshire and Merseyside ICS, it did significantly mediate other factors associated with depression prevalence. One of the most significant findings from the GSESM is the importance of noise in the effects of health deprivation and disability. Health deprivation and disability were strongly associated (0.62) with depression through the indirect effect of environmental noise where exceeding 55 dB Lden.
Discussion
Summary of Main Findings
To the best of our knowledge, this is the first study to investigate the impact of transportation noise pollution on mental health in England. Our study identified areas with a heavier noise burden, offering the opportunity to tailor public health interventions in these regions to enhance the quality of life in urban environments. Combining transportation noise from road and rail networks, we found that Warrington and Knowsley had the highest percentage of noise coverage, with over half of their respective areas exposed to transportation noise exceeding 55 dB on a 24-h basis.
Our research revealed that, although transportation noise did not have an equal direct role in explaining depression levels in all areas, it did play a significant mediating role, amplifying the effect of other factors on depression, such as the impact of health deprivation and disability.
Comparison with Previous Literature
Environmental noise pollution has been associated, in general, with poor mental health indirectly [16–18], and the effects are varying from increased stress and anxiety levels [19, 20] to hyperactivity [21, 22], a decline of well-being [23], and an increase of psychotropic medication [24, 25].
Previous studies investigating explicitly the association between environmental noise pollution and depression have yielded conflicting research results and an incomplete overview of the effects of all noise sources on mental health. As suggested by the systematic review and meta-analysis by Hegewald et al. [26], which included 11 studies of road and 3 studies of railway traffic noise, there were indications of 2–3% increases in depression risk per 10 dB Lden [26]. Interestingly, a recent big data analysis using data from the UK Biobank found a negative association between moderate road traffic noise and major depression [27].
However, no previous study has examined local regression models to comprehend the varying relationships and spatial patterns, aiming to understand how local geographical factors influence the connections between variables, recognising that different places possess unique characteristics that impact these relationships. Moreover, although a US-based nationally representative survey explored the association between noise pollution and mental health in adolescents [28], no previous study has spatially examined the combined impact of road and rail noise on adults’ mental health, evaluating primary care records of depression as an outcome assessment.
Strengths and Limitations
Our paper has a significant strength by employing an innovative structural equation spatial modeling methodology in small geographical areas. This approach allows for the examination of multiple mediators and links in the spatial chain during the model testing process. Additionally, the GSESM analysis furnishes crucial information on model fit, gauging the consistency of the hypothesised mediational model with the data and establishing zero-order relationships among variables. Notably, this methodology, which has not been previously utilised in the literature, leverages recent advancements in computing power, opening up new possibilities for the analysis and modeling of spatial data [15, 29].
Our study, therefore, breaks new ground by exploring the link between environmental noise and the spatial epidemiology of depression using spatial analysis methods. This unique aspect forms a significant strength, particularly as no prior research has delved into this connection using spatial methodologies. This research contributes to the field by expanding the scope beyond earlier investigations limited to selected primary care practices [30]. Instead, our study encompasses the entirety of practices in the Cheshire and Merseyside Integrated Care System (ICS), analysing records from a substantial 2.7 million individuals. The application of spatial methodology empowers us to identify spatial clustering patterns, pinpoint localised hotspots, and discern specific local risk factors—accomplishments that traditional non-spatial regression models are not achieving.
However, it is crucial to acknowledge several limitations. The data on depression are reliant on the recording practices of general practitioners (GPs), introducing a potential source of bias. GPs’ decisions to diagnose depression may also be influenced by personal biases or preferences, as they might record symptoms instead of providing a formal diagnosis of depression [31]. Another constraint is that the Quality and Outcomes Framework (QOF) depression prevalence offers aggregate data for all adults without specific information on adolescents or distinct age groups, nor details on those in retirement status, potentially confounding the associations [32].
In our analyses, we were constrained to using the weighted 24-h indicator (Lden) that combines daytime and nighttime exposures from strategic noise mapping for rail and road noise [7] that was used in accordance with EU Directive 2002/49/EC [33]. From a mental health perspective, we believe the 24-h exposure metric serves as an effective annoyance-based indicator, reflecting cumulative noise exposure (WHO & Theakston Frank, 2011). Previous studies have utilised both weighted and non-weighted averages (Leq, Ldn, and Lden), and we acknowledge that peaks and troughs of noise may have distinct effects on mental states, particularly regarding sleep disturbances caused by sudden sounds, such as sirens in urban settings [34]. As noted by Basner et al. [35], undisturbed sleep is crucial for high daytime performance, well-being, and overall health. Unfortunately, we were unable to analyse peak noise levels with the available data. Further investigation into the differential impacts of daytime noise exposure in living areas versus nighttime exposure, as well as the effects of noise peaks and troughs, is warranted.
Research and Policy Implications
The findings from this research carry significant implications for public health and the promotion of a healthy aging process, which involves sustaining functional ability to ensure well-being.
Understanding the extent of noise exposure in various local authorities, particularly in areas where transportation noise exceeds 55 dB on a 24-h basis, is essential.
This study goes one step further to pinpoint areas with a heavier noise burden, allowing for the tailoring of public health interventions in these regions to enhance the quality of life for older residents and support a healthier aging process.
Overall, this research offers a valuable foundation for informed decision-making and targeted strategies to reduce noise-related health risks in affected local authorities, ultimately contributing to the well-being and healthy aging of the population.
Future research should examine the impact of noise pollution on mental health in areas with persistently high depression rates [36] and explore the differences in mental health effects between urban environments characterised by frequent high-intensity sounds, such as police or ambulance sirens, and those with continuous, lower-intensity background noise, such as motorways.
Future research should also explore the spatial relationship between noise pollution and other health outcomes, including hearing loss [37], cardiovascular disease [1, 38], sleep disturbance [28, 39–41], cognitive decline [22, 42, 43], metabolic syndrome [44], diabetes [45], obesity [46], dementia [47], and tinnitus [4].
Conclusion
While numerous studies explore the impact of the environment on mental health and occasionally acknowledge the potential adverse effects of atmospheric pollution, a notable omission has been the absence of discussions regarding the effects of noise pollution on mental well-being. Our study addresses this gap by providing novel insights into the correlation between noise pollution and mental health and, first, revealing the impact of noise pollution as a mediator, exaggerating the impact of health deprivation and disability on depression.
This research establishes a crucial foundation for informed decision-making and the development of targeted strategies to mitigate noise-related mental health risks in affected local authorities where high-risk groups reside. Ultimately, this contribution aims to tackle mental health inequalities, address their widening, and promote healthy aging in the population.
Acknowledgements
This research was funded by the Institute of Population Health at the University of Liverpool and supported by the Centre for Research on Aging, the Sustainability and Resilience Institute (SRI) at the University of Southampton, and the UK Hearing Conservation Association.
Author Contribution
DT and AT made substantial contributions to the design of the work and were responsible for conducting the analyses, mapping, and drafting the manuscript. DT and AT contributed equally to this work and should be regarded as joint first authors. Both authors substantially contributed to the interpretation of data for the work and revised it critically for important intellectual content. Both authors have read and approved the final manuscript and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Data Availability
The Noise mapping Geographic Information Systems (GIS) datasets are openly available at: https://www.gov.uk/government/publications/strategic-noise-mapping-2019
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Vienneau D, Schindler C, Perez L, Probst-Hensch N, Röösli M. The relationship between transportation noise exposure and ischemic heart disease: a meta-analysis. Environ Res. 2015;138:372–80. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organization. Environmental noise guidelines for the European region. Copenhagen, Denmark: World Health Organization, Regional Office for Europe; 2018.
- 3.Dreger S, Schüle S, Hilz L, Bolte G. Social inequalities in environmental noise exposure: a review of evidence in the WHO European Region. IJERPH. 2019;16:1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.WHO, & Theakston Frank, editor. Burden of disease from environmental noise: quantification of healthy life years lost in Europe. Copenhagen: World Health Organization, Regional Office for Europe; 2011. Available from: https://www.who.int/publications/i/item/9789289002295. Accessed 7 Jan 2025
- 5.Guha M. Noise pollution and mental health. J Ment Health. 2022;31:605–6. [DOI] [PubMed] [Google Scholar]
- 6.Dzhambov AM, Lercher P. Road traffic noise exposure and depression/anxiety: an updated systematic review and meta-analysis. IJERPH. 2019;16:4134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Department for Environment, Food & Rural Affairs. Strategic noise mapping. 2019 Jul. Available from: https://www.gov.uk/government/publications/strategic-noise-mapping-2019. Accessed 7 Jan 2025
- 8.Daras K, Rose, Tanith, Tsimpida, Dialechti, Barr, Benjamin. Quality and outcomes framework indicators: depression prevalence (QOF_4_12). University of Liverpool; 2023 [cited 2023 Mar 28]. https://datacat.liverpool.ac.uk/2170/. Accessed 7 Jan 2025
- 9.McLennan D, Noble S, Noble M, Plunkett E, Wright G, Gutacker N. The English indices of deprivation 2019: technical report. [ Guidance ]
- 10.Office for National Statistics. Census 2021 geographies. 2021. Available from: https://www.ons.gov.uk/methodology/geography/ukgeographies/censusgeographies/census2021geographies. Accessed 7 Jan 2025
- 11.Office for National Statistics. Integrated Care Boards (April 2023) EN BGC. 2023. Available from: https://www.data.gov.uk/dataset/d6bcd7d1-0143-4366-9622-62a99b362a5c/integrated-care-boards-april-2023-en-bgc. Accessed 7 Jan 2025
- 12.Baron RM, Kenny DA. The moderator–mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173. [DOI] [PubMed] [Google Scholar]
- 13.Judd CM, Kenny DA. Process analysis: estimating mediation in treatment evaluations. Eval Rev. 1981;5:602–19. [Google Scholar]
- 14.Esri Inc. ArcGIS Pro. 2021. Available from: https://www.esri.com/en-us/arcgis/products/arcgis-pro/overview. Accessed 7 Jan 2025
- 15.Naqvi SAA, Sajjad M, Waseem LA, Khalid S, Shaikh S, Kazmi SJH. Integrating spatial modeling and space–time pattern mining analytics for vector disease-related health perspectives: a case of dengue fever in Pakistan. IJERPH. 2021;18:12018. [DOI] [PMC free article] [PubMed]
- 16.Dzhambov A, Tilov B, Markevych I, Dimitrova D. Residential road traffic noise and general mental health in youth: the role of noise annoyance, neighborhood restorative quality, physical activity, and social cohesion as potential mediators. Environ Int. 2017;109:1–9. [DOI] [PubMed] [Google Scholar]
- 17.Hammersen F, Niemann H, Hoebel J. Environmental noise annoyance and mental health in adults: findings from the cross-sectional German Health Update (GEDA) study 2012. IJERPH. 2016;13:954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Li A, Martino E, Mansour A, Bentley R. Environmental noise exposure and mental health: evidence from a population-based longitudinal study. Am J Prev Med. 2022;63:e39-48. [DOI] [PubMed] [Google Scholar]
- 19.Gong X, Fenech B, Blackmore C, Gulliver J, Hansell A. Association between noise annoyance and mental health outcomes - an evidence review. Inter Noise. 2021;263:3271–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jensen HAR, Rasmussen B, Ekholm O. Neighbour and traffic noise annoyance: a nationwide study of associated mental health and perceived stress. Eur J Pub Health. 2018;28:1050–5. [DOI] [PubMed] [Google Scholar]
- 21.Dreger S, Meyer N, Fromme H, Bolte G. Environmental noise and incident mental health problems: a prospective cohort study among school children in Germany. Environ Res. 2015;143:49–54. [DOI] [PubMed] [Google Scholar]
- 22.Haines MM, Stansfeld SA, Job RFS, Berglund B, Head J. Chronic aircraft noise exposure, stress responses, mental health and cognitive performance in school children. Psychol Med. 2001;31:265–77. [DOI] [PubMed] [Google Scholar]
- 23.Schreckenberg D, Benz S, Belke C, Möhler U, Guski R. The relationship between aircraft sound levels, noise annoyance and mental well-being: An analysis of moderated mediation. In Proceedings of the 12th ICBEN congress on noise as a public health problem 2017 Jun 18 (pp. 1–13).
- 24.Klompmaker JO, Hoek G, Bloemsma LD, Wijga AH, van den Brink C, Brunekreef B, et al. Associations of combined exposures to surrounding green, air pollution and traffic noise on mental health. Environ Int. 2019;129:525–37. [DOI] [PubMed] [Google Scholar]
- 25.Okokon EO, Yli-Tuomi T, Turunen AW, Tiittanen P, Juutilainen J, Lanki T. Traffic noise, noise annoyance and psychotropic medication use. Environ Int. 2018;119:287–94. [DOI] [PubMed] [Google Scholar]
- 26.Hegewald J, Schubert M, Freiberg A, Romero Starke K, Augustin F, Riedel-Heller SG, et al. Traffic noise and mental health: a systematic review and meta-analysis. IJERPH. 2020;17:6175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hao G, Zuo L, Xiong P, Chen L, Liang X, Jing C. Associations of PM2.5 and road traffic noise with mental health: evidence from UK Biobank. Environ Res. 2022;207:112221. [DOI] [PubMed] [Google Scholar]
- 28.Rudolph KE, Shev A, Paksarian D, Merikangas KR, Mennitt DJ, James P, et al. Environmental noise and sleep and mental health outcomes in a nationally representative sample of urban US adolescents. Environ Epidemiol. 2019;3:e056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lin C-H, Wen T-H. How spatial epidemiology helps understand infectious human disease transmission. TropicalMed. 2022;7:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Amoud MM, Omar DI, Almashjary EN, Alomary SA. Morbidity profile among older people at primary health care centers in Saudi Arabia during the period 2012–2020. SMJ. 2023;44:45–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Grigoroglou C, Munford L, Webb RT, Kapur N, Ashcroft DM, Kontopantelis E. Prevalence of mental illness in primary care and its association with deprivation and social fragmentation at the small-area level in England. Psychol Med. 2020;50:293–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsimpida D, Kontopantelis E, Ashcroft DM, Panagioti M. The dynamic relationship between hearing loss, quality of life, socioeconomic position and depression and the impact of hearing aids: answers from the English Longitudinal Study of Aging (ELSA). Soc Psychiatry Psychiatr Epidemiol. 2022;57:353–62. [DOI] [PMC free article] [PubMed]
- 33.European Parliament. Directive 2002/49/EC of the European Parliament and of the Council of 25th June 2002 relating to the assessment and management of environmental noise: Official Journal of the European Communities, L189, 2002. 2002. Available from: https://eur-lex.europa.eu/eli/dir/2002/49/oj/eng. Accessed 7 Jan 2025
- 34.Edworthy J, Hellier E. Auditory warnings in noisy environments. Noise Health. 2000;2:27–40. [PubMed] [Google Scholar]
- 35.Basner M, Clark C, Hansell A, Hileman JI, Janssen S, Shepherd K, et al. Aviation noise impacts: state of the science. Noise Health. 2017;19:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tsimpida D, Tsakiridi A, Daras K, Corcoran R, Gabbay M. Unravelling the dynamics of mental health inequalities in England: a 12-year nationwide longitudinal spatial analysis of recorded depression prevalence. SSM - Population Health. 2024;26:101669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tsimpida D, Piroddi R, Daras K, Melis G. Pioneering a new era in assessing hearing health inequalities: monitoring burden and distribution of hearing loss in older adults using routine health information systems. 2024 [cited 2024 Apr 10]. Available from: 10.2139/ssrn.4747384.
- 38.Münzel T, Sørensen M, Gori T, Schmidt FP, Rao X, Brook FR, et al. Environmental stressors and cardio-metabolic disease: part II–mechanistic insights. Eur Heart J. 2016;ehw294. [DOI] [PMC free article] [PubMed]
- 39.Sygna K, Aasvang GM, Aamodt G, Oftedal B, Krog NH. Road traffic noise, sleep and mental health. Environ Res. 2014;131:17–24. [DOI] [PubMed] [Google Scholar]
- 40.Van Kempen E, Babisch W. The quantitative relationship between road traffic noise and hypertension: a meta-analysis. J Hypertens. 2012;30:1075–86. [DOI] [PubMed] [Google Scholar]
- 41.Zaharna M, Guilleminault C. Sleep, noise and health: review. Noise Health. 2010;12:64. [DOI] [PubMed] [Google Scholar]
- 42.Stansfeld S, Clark C. Health effects of noise exposure in children. Curr Envir Health Rpt. 2015;2:171–8. [DOI] [PubMed] [Google Scholar]
- 43.Tzivian L, Dlugaj M, Winkler A, Weinmayr G, Hennig F, Fuks KB, et al. Long-term air pollution and traffic noise exposures and mild cognitive impairment in older adults: a cross-sectional analysis of the Heinz Nixdorf recall study. Environ Health Perspect. 2016;124:1361–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yu Y, Paul K, Arah OA, Mayeda ER, Wu J, Lee E, et al. Air pollution, noise exposure, and metabolic syndrome – a cohort study in elderly Mexican-Americans in Sacramento area. Environ Int. 2020;134:105269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zare Sakhvidi MJ, Zare Sakhvidi F, Mehrparvar AH, Foraster M, Dadvand P. Association between noise exposure and diabetes: a systematic review and meta-analysis. Environ Res. 2018;166:647–57. [DOI] [PubMed] [Google Scholar]
- 46.Wang Z, Zhao L, Huang Q, Hong A, Yu C, Xiao Q, et al. Traffic-related environmental factors and childhood obesity: a systematic review and meta-analysis. Obes Rev. 2021;22:e12995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cantuaria ML, Waldorff FB, Wermuth L, Pedersen ER, Poulsen AH, Thacher JD, Raaschou-Nielsen O, Ketzel M, Khan J, Valencia VH, Schmidt JH. Residential exposure to transportation noise in Denmark and incidence of dementia: national cohort study. BMJ. 2021;374. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The Noise mapping Geographic Information Systems (GIS) datasets are openly available at: https://www.gov.uk/government/publications/strategic-noise-mapping-2019