Abstract
In the clinical care of people with disproportionate short stature, healthcare practitioners need to accurately collect anthropometric measurements over time, including height, weight, head circumference, and lengths of affected limb and body segments. Accurate anthropometric measurements are important for diagnostic evaluation, tracking growth, measuring response to pharmacologic therapies or surgeries, and monitoring for potential complications. However, for this clinical population, anthropometric measurements may need to be adjusted or modified to accommodate characteristics such as body disproportions, joint contractures, long bone deformities, spinal deformities, or muscle hypotonia. This article provides guidance for key anthropometric measurements in children and adults with disproportionate short stature, with a focus on people with achondroplasia. The measurements described in this article and illustrated in the infographics can be performed without expensive specialized equipment and are suitable for a variety of clinical settings.
Supplementary Information
The online version contains supplementary material available at 10.1007/s12325-024-03061-y.
Keywords: Achondroplasia, Anthropometry, Body composition, Disproportionate short stature, Growth, Obesity, Short stature, Skeletal dysplasia
Key Summary Points
| This article provides guidance for key anthropometric measurements in children and adults with disproportionate short stature. |
| Reproducibility of measurements can be optimized by using a written local standard operating procedure, to ensure consistency in methods, training of personnel, and equipment calibration. |
| When performing anthropometric measurements, clinicians and investigators should pay special attention to joint contractures, bowing of legs, muscle hypotonia, and spinal deformities. |
Digital Features
This article is published with digital features, including a slide deck to facilitate understanding of the article. To view digital features for this article, go to 10.6084/m9.figshare.27225495.
Introduction
Among the more than 700 known genetic skeletal disorders, several are characterized by short stature with abnormalities of bone and cartilage development, affecting the growth plates of the long bones and spine [1]. Disproportion in body and/or limb segments is common in short stature conditions. In clinical care, healthcare practitioners need to accurately collect and monitor anthropometry, including height, weight, head circumference, and lengths of affected limb and body segments. These data are important to identify abnormal growth to guide diagnostic evaluation and genetic testing [2, 3], monitor for medical complications such as obesity or hydrocephalus [4–7], and measure response to pharmacologic therapies or surgeries. However, standard measurement techniques may not be sufficient for individuals with disproportionate short stature. Anthropometry methods may need modification due to joint contractures, long bone deformities (e.g., bowing), spinal deformities (e.g., kyphosis, scoliosis, or lordosis), inability to stand independently, and muscle hypotonia or joint laxity, which may be part of the underlying skeletal dysplasia. These complexities challenge the reproducibility of measurements, and an anthropometrist unfamiliar with these complexities may have more difficulty performing measurements, which also affects measurement accuracy and reliability.
The disproportionate short stature dysplasias may be divided into those with a normal or mildly reduced trunk relative to shortened limbs and those with greater shortening of the trunk relative to less affected limbs. Achondroplasia is the most common type of the former [6, 8, 9], with an upper-to-lower body segment ratio of ~ 2:1 [5] and greater involvement of the long bones versus the spine. Pathogenic variants in the gene encoding fibroblast growth factor receptor 3 (FGFR3) cause impaired overall linear bone growth [6, 8], resulting in the characteristic growth pattern of a close to average-sized torso with disproportionately shortened proximal and medial limb segments (i.e., rhizomelia and mesomelia) and macrocephaly with mid-face hypoplasia and prominent forehead [8]. Additionally, in achondroplasia, excessive lordosis, tibial bowing, and genu varus deformities must be taken into account when measuring total height or segmental growth.
Spondyloepiphyseal dysplasia congenita (SEDC), most commonly caused by pathogenic variants in the COL2A1 gene [10], is one of the most common disproportionate short stature dysplasias, with greater shortening of the trunk compared with the long bones [11]. In addition to abnormal formation and growth of the vertebrae in SEDC and other short trunk dysplasias, spine deformities such as kyphosis and scoliosis are also more common and could exacerbate the shortening. These spinal anomalies may also change over time in a given patient and must be accounted for in measuring longitudinal growth.
It has always been important to quantify growth in children with short stature dysplasias to direct their diagnostic workup and to identify complicating health issues in the clinical setting. However, several recent clinical trials of novel treatments to increase linear growth in patients with achondroplasia [12–16] have intensified the need for uniform, comprehensive, and accurate anthropometry to objectively demonstrate the effectiveness of these treatments. It is our intention with this article to share techniques and lessons learned from recent trials and other clinical research involving patients with achondroplasia that could be applied to future research endeavors with this population and people with other short stature dysplasias. It is also recognized that practical reference information is needed for community healthcare providers to monitor their patients for natural growth and/or the effect of these new pharmaceuticals once the trials conclude and they are available by prescription.
Therefore, the aim of this article is to provide simple, straightforward guidance for key anthropometric measurements in children and adults with disproportionate short stature, including potential pitfalls and difficulties with measurements for different disorders/conditions. These techniques can and should be used in individuals with average growth. The focus of this commentary is achondroplasia. However, we also provide important considerations for measuring non-ambulatory people with short stature skeletal dysplasias and those with limb and spine deformities and at all ages. The techniques and considerations presented here are applicable to people with any skeletal condition that results in disproportionate short stature. All the measurements described in this article can be performed without expensive specialized equipment and are therefore suitable for a variety of clinical settings. In addition to descriptions, we have developed infographic figures to illustrate the measurement techniques; these figures are also available as a slide deck (10.6084/m9.figshare.27225495).
General Considerations for Anthropometric Measurements
Regardless of the reason(s) for performing anthropometric measurements, there are several general guidelines for ensuring accuracy and consistency. These include the equipment used, training of staff, and development of a local protocol for measurements. In addition, where possible for longitudinal measures, and particularly in research, the time of day for measurement should be consistent for an individual. This is particularly important for height measurements, as height is known to vary diurnally [17, 18].
If anthropometric measurements are made as part of a clinical trial, there are likely to be very strict protocols around such aspects as the timing of measurements, how often equipment is standardized, the number of personnel performing measurements, and including a separate person to record the measurements. Outside of a clinical trial or other investigator-initiated research, we recommend that measurements made in a routine clinical setting be performed according to a local standard operating procedure (SOP) that takes into account the practicalities of measurement within the individual clinic. Realistic suggestions for optimizing measurement quality in the clinic are also provided.
Equipment and Calibration
Most of the basic anthropometric measurements can be performed using standard equipment found in many clinics, such as a wall-fixed stadiometer or wall-mounted tape measure for height measurements, an infant board for infant body length and crown–rump length, digital scales for weight, a non-stretchable tape measure for head circumference and arm span, and a stool for sitting height. Sitting height should also be measured with the wall-fixed stadiometer; therefore, the stool needs to be tall enough to reach the lower limit of the stadiometer.
Where possible, clinicians should use the same measurement device(s) at every visit. These device(s) should be appropriately standardized/calibrated to ensure that their measurements are accurate, particularly where it is not possible to use the same device(s) at every measurement. To ensure accurate measurements, the stadiometer should be mounted to the wall and positioned above solid flooring (not carpet). Digital scales should also be placed on solid flooring. Measuring devices can be standardized by checking their accuracy against a known weight or length. For instruments used in measuring length (such as tape measures and stadiometers), standard fixed-length rods are available for this purpose, and standard weights can be used for scales. For some devices, such as stadiometers, standardization is recommended very regularly (e.g., no more than 4 h before use), particularly if the measurements are being performed as part of a clinical trial. Scales and other devices may require less frequent standardization and calibration (e.g., at least yearly), so it is best to check with the manufacturer. Calibration, in which a measurement device is adjusted or corrected to measure a known weight or length, is necessary when the measurement device does not match the standardized value.
Personnel and Training
Consistency in measurement is just as important as the measurement tools used. Reliable and accurate measurement requires attention to detail. Staff training is important for both accuracy and consistency of measurement. Formal training and certification in anthropometry can be obtained, for example, from the International Society for the Advancement of Kinanthropometry (https://www.isak.global/), but there are currently no certifications specific to anthropometric measurement of people with skeletal dysplasias or disproportionate short stature. However, formal certified training is not essential, providing staff are trained in the SOP of the clinic and have received sufficient practice to ensure consistent technique, particularly if multiple individuals will be performing the measurements. Training of new personnel should include multiple opportunities for practice and evaluation of measurement techniques. Ideally, each child should be evaluated by the same anthropometrist throughout follow-up; where this is not practicable, a limited number of professionals should oversee this task.
In addition to accurate measurements, accurate recording of the measurements is important. Best practice is for the anthropometrist to work with a recorder whose primary purpose is to assist in documenting the measurement values. The recorder may also assist in positioning or preparing equipment for the anthropometrist. It is common practice for the recorder to repeat the values aloud as they are acquired, and for the anthropometrist to then confirm or correct the values. In routine clinical practice, simple measurements may not require a separate recorder; however, when multiple or more complex measurements are performed, having a recorder available is useful.
Developing a Local SOP
For best practice of anthropometric measurements, each clinic should have a local SOP that describes aspects in detail, including but not limited to: how to undertake each measurement in your clinic (e.g., clothes on or off, shoes off, number of staff assisting with measurement, etc.); level of accuracy to be recorded for each measurement (e.g., height/length to the nearest 0.1 cm); number of measurements to be recorded (e.g., measure in triplicate and take the average); comparison with previous measurements, and if further recordings are advisable in case of inconsistency; protocols for anticipated challenges, such as an uncooperative child, need for additional assistance, or potential diurnal variations in measurements; and standardization/calibration procedures, including how often standardizations should be recorded and how calibrations are to be performed. The recommendations and descriptions of measurement techniques in this commentary are intended to provide a basis for development of a local SOP for clinical use and are based on the authors’ clinical experience. When possible, technique modifications are offered to increase uniformity and accuracy when anthropometry is intended for research use. We have also provided an example data collection spreadsheet (Supplementary Table S1), which can be adjusted to the needs of individual clinics.
Accommodating Individual Differences
The local SOP should include standardized procedures for accommodating individual needs during measurement. Common modifications that may be needed include measuring the height of non-ambulatory patients in a supine position, measuring sitting height and leg segment lengths of wheelchair users, and measuring height with the patient standing on each leg separately if the patient has legs of different lengths. Arm span can also be used as a surrogate marker for height in individuals with trunk deformities or who cannot stand up for height measurements. For patients with joint contractures, any changes in the extent of contractures over time should be recorded. For all instances in which individual differences are accommodated, it is important to keep accurate records of the adjustments made and the reason(s) for the adjustments.
Anthropometric Measurement in Children with Disproportionate Short Stature
In children with disproportionate short stature, measurements are used to determine and track growth, both from the perspective of monitoring general health and development, and for recording responses to clinical treatment. It is recommended that practitioners track at least height, weight, and head circumference of children against standardized diagnosis-specific charts (e.g., achondroplasia [4, 19–24] or other short stature conditions [25–29]; Supplementary Table S2). Plotting weight and height immediately after measurement allows for re-measuring any individual points that appear to be outliers, to confirm their accuracy. If height and weight are used to calculate BMI, care should be taken to only make comparisons to BMI-for-age curves that are diagnosis-specific (e.g., achondroplasia [30]), as average stature BMI norms are inappropriate for this population.
Although it is not the focus of this commentary, we also recommend that anthropometric measurements and pubertal development (Tanner stage) are collected in combination with other developmental and health indicators that may also be potential indicators of response to clinical treatment. Indicators that should be considered include: developmental profile of the child, relative to diagnosis-specific charts [e.g., the Screening Tool for Everyday Mobility and Symptoms (STEMS) for skeletal dysplasia [31] or achondroplasia-specific development [32, 33]]; stamina and pain; and activities of daily living and independence skills.
To use growth and developmental charts, the child’s age should be determined and recorded correctly. In infants aged < 12 months, record the age in months, correcting for gestational age in the case of pre-term births. For children aged ≥ 12 months to ≤ 3 years, record age in months. For children aged > 3 years, record age in years and months.
The World Health Organization recommends measuring body length in children < 2 years old and standing height in children > 2 years old, unless unable to stand independently [34]. In children with disproportionate short stature, we recommend measuring both length and height in children aged ≥ 2 to ≤ 3 years. Note that, during this transition phase, there can be ~ 1-cm difference between body length and standing height measurement [35].
Outside of genetic disorders of skeletal growth, there is a strong genetic influence on height [36]. Thus, parental height may still have some influence on the height of children and adolescents with disproportionate short stature; for example, height variability in children with achondroplasia is strongly correlated with parental height [8]. Parental heights should be measured and recorded, particularly if one of the parents (or another family member) has the same form of disproportionate short stature as the child.
If a child with disproportionate short stature has pronounced genu varum/valgum and/or tibial bowing, or spinal deformities such as lordosis, kyphosis, or scoliosis, these may influence the accuracy of measurements. Therefore, the progression of these conditions must be followed over time. Although spinal deformities are best assessed via imaging, a simple lumbar spine lordosis measurement may be achieved by measuring the distance from the wall to the point of maximum lordosis. Scoliosis can also be assessed by letting the patient bend forward with their hands together and knees straight. If the back is tilted, there is a high possibility of scoliosis. Radiographic assessments must be performed on these patients [37, 38].
As children become older and with measurement experience, their capacity to cooperate with the anthropometrist during measurements will improve. However, any child may be or become uncooperative, particularly if tired. Therefore, the local SOP should include strategies for uncooperative or tired children, such as performing measurements at the beginning of each appointment, giving children short movement breaks between measurements, and providing small incentives (e.g., stickers) for each measurement achieved.
Specific Considerations for Achondroplasia
Both overweight/obesity and underweight are of concern in all children. In those with achondroplasia, there are specific complications to consider. Weight loss, poor weight gain, or being underweight for age may be indicators of severe complications, such as cranio-cervical compression [4]. Head circumference measurement allows for monitoring of potential complications of achondroplasia, such as hydrocephalus, and should be measured regularly at least up to 5–6 years of age [8], and measurement every 1–2 years thereafter, up to adulthood, should be considered. Children with achondroplasia may have atypical range of motion in some joints, such as elbow contractures and/or hyperextended knees; however, accurate measurement of the range of motion requires a special instrument (a goniometer) and specialized training.
In children with achondroplasia, we encourage the measurement of sitting height/crown–rump length and arm span (Table 1). Sitting height and arm span are useful measurements for patients newly undergoing pharmacologic therapy for short stature, as these enable the monitoring of changes in body proportions.
Table 1.
Recommended measurements in a clinical settinga for people with achondroplasia at different life stages
| Life stage | Recommended measurements | Measure to nearest | Notes on technique (see also Figs. 1, 2, 3, 4, 5, 6, 7, 8, 9) |
|---|---|---|---|
| Infancy | Weight | 0.1 kg | Use infant scale. Tare a dry diaper and weigh infant in dry diaper |
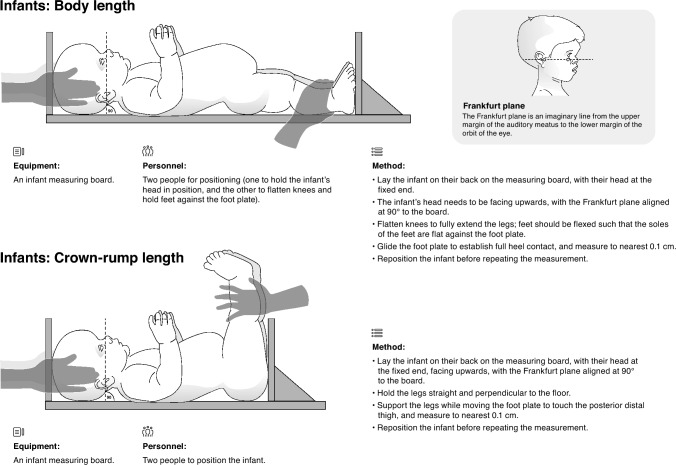
| Body length | 0.1 cm | Use infant board; measure with knees extended and feet at 90° to board, face looking upwards (head with Frankfurt planeb at 90° to board) | |
| Crown-rump length | 0.1 cm | Use infant board; measure with legs held straight and perpendicular to the floor, face looking upwards (head with Frankfurt plane at 90° to board) | |
| Head circumference | 0.1 cm | Use insertion tape or tape measure; move up and down to find largest circumference across the forehead and back of the head | |
| Children | Weight | 0.1 kg | In minimal or light clothing with empty pockets (loose/heavy objects such as toys, phone, etc. removed); no shoes. Dry diaper, if needed |
| Body lengthc | 0.1 cm | Use infant board; measure with knees extended and feet at 90° to board, head with Frankfurt plane at 90° to board | |
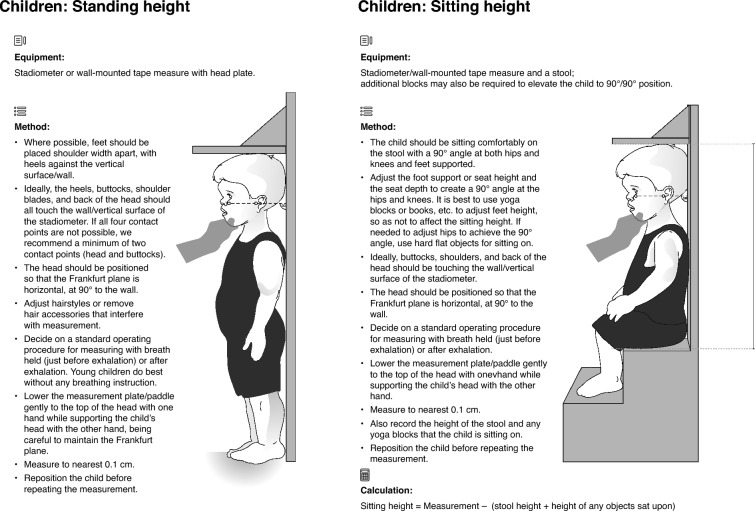
| Standing heightc | 0.1 cm |
Use wall-mounted tape measure or stadiometer; measure with feet shoulder-width apart, head facing forward with Frankfurt plane at 90° to wall It may not be possible for heels, buttocks, shoulder blades, and back of the head to all touch the wall; if so, head and buttocks are recommended contact points |
|
| Sitting heightd | 0.1 cm | Use wall-mounted tape measure, or wall stadiometer, and a stool; child to sit with hips and knees at 90° angles, feet supported, and head facing forward with Frankfurt plane at 90° to wall (may need to use yoga blocks or books to achieve 90° angles). There are also specific devices that can be used, e.g., sitting height table. Use standing height equipment to measure stool height | |
| Head circumference | 0.1 cm | Use insertion tape or tape measure; move up and down to find largest circumference | |
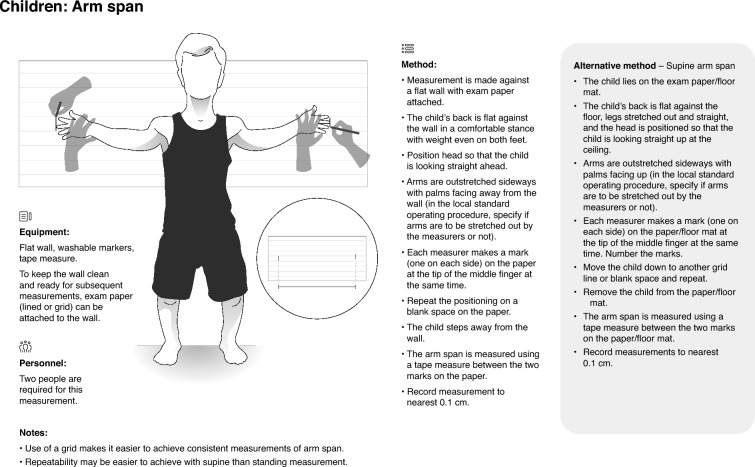
| Arm span | 0.1 cm | Can be measured supine or standing, though easiest for patient in supine position; whichever is chosen, it is important to be consistent. Head position can significantly change the measurement. The measurement must be taken with the person looking straight ahead, whether taken supine or standing | |
| Adolescents | Weight | 0.1 kg | In minimal or light clothing with empty pockets (loose/heavy objects such as wallet, phone, etc. removed); no shoes |
| Standing height | 0.1 cm |
Use wall-mounted tape measure or stadiometer; measure with feet shoulder-width apart, head facing forward with Frankfurt plane at 90° to wall It may not be possible for heels, buttocks, shoulder blades, and back of the head to all touch the wall; if so, head and buttocks are recommended contact points |
|
| Sitting height | 0.1 cm | Use wall-mounted tape measure and a stool; child to sit with hips and knees at 90° angles, with feet supported, and head facing forward with Frankfurt plane at 90° to wall (may need to use yoga blocks or books to achieve 90° angles) | |
| Arm span | 0.1 cm | Can be measured supine or standing; whichever is chosen, it is important to be consistent | |
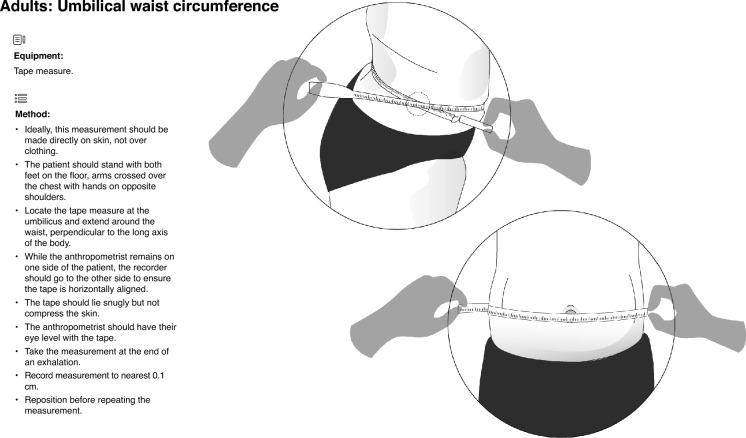
| Waist circumferencee | 0.1 cm | Locate the tape measure at umbilicus and perpendicular to the long axis of the body. Take measurement at the end of an exhalation. Use the technique for which there are data to compare for that specific population | |
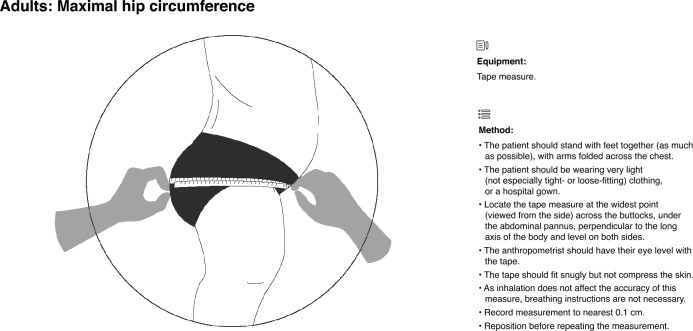
| Hip circumferenced | 0.1 cm | Locate the tape measure at the widest point across the buttocks, under the abdominal pannus, and perpendicular to the long axis of the body | |
| Adults | Weight | 0.1 kg | In minimal or light clothing with empty pockets (loose/heavy objects such as wallet, phone, keys, etc. removed); no shoes |
| Standing height | 0.1 cm |
Use wall-mounted tape measure or stadiometer; measure with feet shoulder-width apart, head facing forward with Frankfurt plane at 90° to wall It may not be possible for heels, buttocks, shoulder blades, and back of the head to all touch the wall; if so, head and buttocks are recommended contact points |
|
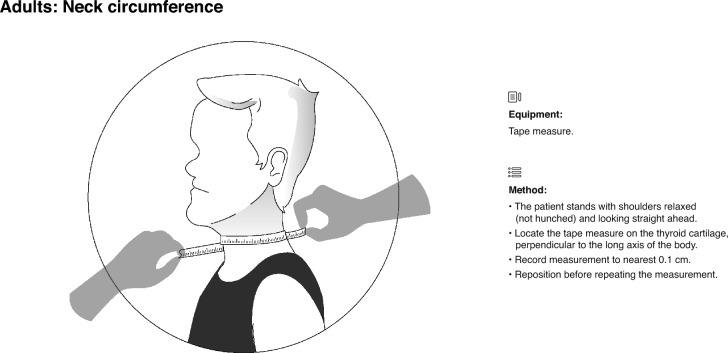
| Neck circumference | 0.1 cm | Locate the tape measure on thyroid cartilage, perpendicular to the long axis of the body | |
| Arm span | 0.1 cm | Can be measured supine or standing; whichever is chosen, it is important to be consistent | |
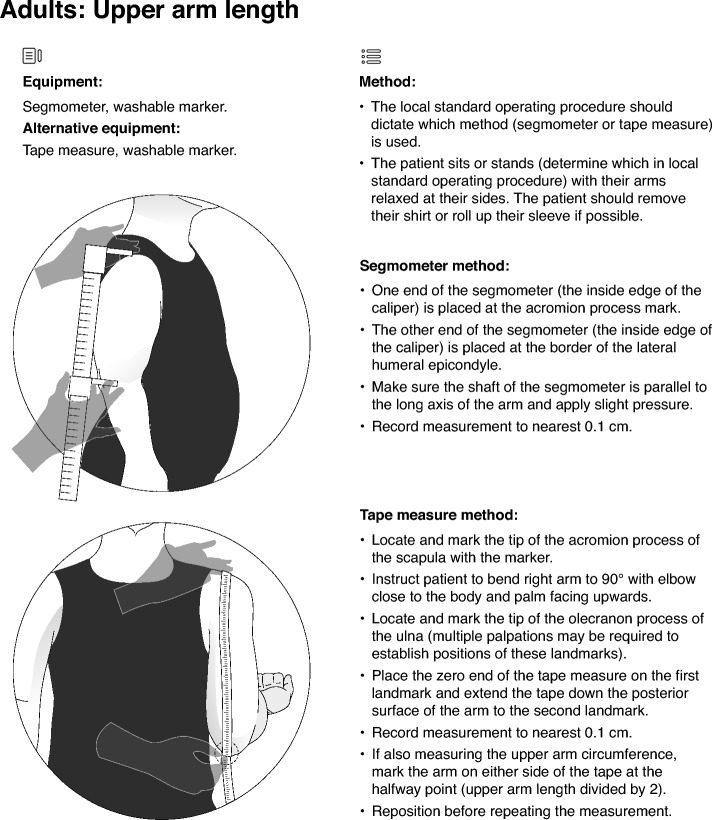
| Upper arm lengthf | 0.1 cm | Measure from acromion process of the scapula down the posterior surface of the arm to the olecranon process of the ulna. Multiple palpations may be required to establish positions of these landmarks | |
| Adults (continued) | Upper arm circumferencef | 0.1 cm | Encircle the arm at the halfway point between the acromion and olecranon processes. Arm muscles should be loose (not flexed) |
| Waist circumference | 0.1 cm | Locate the tape measure at umbilicus and perpendicular to the long axis of the body. Take measurement at the end of an exhalation | |
| Hip circumference | 0.1 cm | Locate the tape measure at the widest point across the buttocks, under the abdominal pannus, and perpendicular to the long axis of the body |
aIn clinical trials, multiple additional measurements may be included, such as upper/lower arm lengths, upper/lower leg lengths, flexion/extension of elbows and knees, etc. Note that using the patella as a measurement landmark is very difficult before it ossifies (typically between 3 and 5 years of age [50]). See Supplementary Table S3 for descriptions of some of these additional measurements
bThe Frankfurt plane is an imaginary line from the upper margin of the auditory meatus to the lower margin of the orbit of the eye (see Fig. 1)
cBody length only in children ages < 2 years, body length and standing height in children ages ≥ 2 to ≤ 3 years, standing height only in children > 3 years
dFor children unable to sit unaided, measure crown–rump length
eWe suggest tracking measurements of waist and hip circumference during any period in which it is not possible to measure weight in adolescent, e.g., during leg-lengthening procedures
fUpper arm measurements may also be considered in adolescents
Sitting height/crown–rump length are used along with standing height/body length to calculate the upper-to-lower body segment ratio as [5]:
| 1 |
OR
| 2 |
Sitting height is also used in the sitting height-to-height ratio, another metric used to assess body proportionality is:
| 3 |
Another option to quantify the upper-to-lower body segment ratio in a patient who is able to stand is to measure the lower segment with a tape measure and subtract that value from the standing height. One end of the tape measure should be held at the top of the symphysis pubis while it is extended perpendicular to the ground at the sole of one foot. The patient should be standing evenly on both feet, with feet a minimal distance apart while still comfortably balanced [39].
Reference charts for these recommended measurements, as well as for other disproportionate short stature disorders, are listed in Supplementary Table S2. Additional anthropometric measurements that may be considered for some conditions are described briefly in Supplementary Table S3.
Infants
During infancy, regular measurements will include head circumference, weight, body length, and crown–rump length. Measurement techniques for infants are described and illustrated in Figs. 1 and 2. The measurements of infants require a minimum of two people, and it is often preferable that a parent/carer is involved in the measurement process; however, this should be at the discretion of the anthropometrist. A recorder can assist in measurements with guidance from the anthropometrist. Ideally, the recorder should also be familiar with the SOP, but this is not required.
Fig. 1.
Anthropometric measurement techniques for infants with achondroplasia: body length and crown–rump length
Fig. 2.

Anthropometric measurement techniques for infants with achondroplasia: head circumference
Toddlers and School-Aged Children
During the toddler years, the transition is made from measuring body length to measuring standing height, and from measuring crown–rump length to measuring sitting height. In addition, this is usually the age in which arm span is first measured. Measurement techniques for standing height, sitting height, and arm span are described and illustrated in Figs. 3 and 4.
Fig. 3.
Anthropometric measurement techniques for toddlers and school-aged children with achondroplasia: standing height and sitting height. Note that the same techniques are also used for these measurements in adolescents and adults who are able to stand independently
Fig. 4.
Anthropometric measurement techniques for toddlers and school-aged children with achondroplasia: arm span. Note that the same techniques are also used for these measurements in adolescents and adults who are able to stand independently
Standing height should only be measured in children who can stand independently for more than 1 min, which may exclude individuals with significant kyphosis or scoliosis, and is likely to be at an older age in children with achondroplasia. Sitting height can be measured once a child without significant kyphosis or scoliosis can sit erect unsupported.
For all measurements that will be taken regularly, it is advisable to choose measurement methods that can be maintained over time. For example, young children with achondroplasia may be able to stand with their feet together when standing height is measured, but, as they age, they may require a wider base for balance. For this reason, we recommend that standing height is measured with feet shoulder-width apart from the time standing height is first measured. It is also recommended when measuring standing height that the heels, buttocks, shoulders, and head are all in contact with the wall. If this is not possible, then a minimum of two contact points is recommended (head and buttocks), and the other points should be as close as possible to the wall.
Adolescents
Generally, measurement protocols in adolescents will be the same as those for younger children (Table 1). However, in patients who have undergone leg lengthening procedures, problems may arise with some measurements. For example, if the calf muscles and Achilles tendons become tight, the heels of the patient may not touch the ground when standing straight, making it difficult to measure standing height. Moreover, during the leg lengthening process, an accurate weight measurement is not possible due to the fixation device (internal or external). In these patients, it may be useful to track measurements of waist and hip circumference during any period in which it is not possible to measure weight (see Fig. 5 and 6 for waist and hip circumference measurement techniques). However, we note that high-quality population norms for waist or hip circumference in adolescents with achondroplasia are not currently available.
Fig. 5.
Anthropometric measurements for adults with achondroplasia: umbilical waist circumference [adapted from National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. 2021; https://wwwn.cdc.gov/nchs/data/nhanes/public/2021/manuals/2021-Anthropometry-Procedures-Manual-508.pdf]
Fig. 6.
Anthropometric measurements for adults with achondroplasia: maximal hip circumference
An adolescent pubertal growth spurt is generally not present in children with achondroplasia and other short stature conditions [5, 22, 28].
Additional measurements that may be considered in adolescents are upper arm length and upper arm circumference (see Adult sections), knee to foot height, and tibial length (Supplementary Table S3).
Anthropometry in Adults with Disproportionate Short Stature
In adults with disproportionate short stature, there is still a need for anthropometric measurement. Although longitudinal growth has stopped, degenerative changes and spinal deformities can be tracked by monitoring height loss. There may also be benefits to tracking specific measurements as indicators of health status. In adults of average stature, health status is inversely associated with age [40], and multiple anthropometric measurements have been associated with poor health outcomes, including increased risk of sleep apnoea (specifically, increased apnoea-hypopnoea index and increased respiratory disturbance index) in people who are obese, with a large neck circumference, increased waist circumference, and/or those with increased waist-to-hip ratio [41, 42]; an association of low mid-upper arm circumference with thinness and higher mortality rate in older people [43]; and a greater risk of stroke and atherosclerotic disease in people with a large waist circumference and in people with larger waist-to-hip ratios [44]. However, risk relationships established based on measurements of adults of average stature may not be appropriate for people with disproportionate short stature. For example, BMI in adults with short stature is rendered very high due to the smaller height component, which means that it is more appropriate to use condition-specific BMI cut-offs for overweight and obesity [21, 45].
Specific Considerations for Achondroplasia in Adults
Adults with achondroplasia are known to be at high risk for poor health outcomes, including obstructive sleep apnoea [6], death from cardiovascular disease [46], and respiratory, metabolic, and neurologic complications [47]. To date, there have been few attempts to assess the risk of poor health outcomes against anthropometric measurements in people with achondroplasia. Despite having a higher BMI than adults of average stature, visceral and abdominal subcutaneous fat, liver fat, and total abdominal fat stores (measured via magnetic resonance imaging (MRI)] were low in Norwegian adults with achondroplasia [48]. However, MRI studies have suggested symptomatic spinal stenosis in adults with achondroplasia may be associated with fat infiltration in the thigh muscles [49]. Future investigations of the relationships between body composition and health outcomes in adults with achondroplasia will need to be underpinned by appropriate anthropometric measurement studies.
Modifications to Measurements Required for Adults with Achondroplasia
To investigate potential associations of anthropometric variables with health outcomes in adults with achondroplasia, a standardized methodology for body measurements is required in this population. To this end, a subset of authors of this publication (J. Hoover-Fong, B. Barron, and C. Koerner, along with their colleague Y. Alade) performed a pilot study involving 20 adults with achondroplasia (11 men and nine women) (data on file; J. Hoover-Fong). Participants were recruited from community and clinic populations local to Johns Hopkins Hospital, Baltimore, USA. The study was conducted in accordance with ethical principles that have their origin in the Declaration of Helsinki and was approved by the Johns Hopkins Medical Institute Institutional Review Board. Measurements were obtained in triplicate by two experienced dietitians.
In this pilot study, modifications were required to obtain anthropometric values for adults with achondroplasia, due to key anatomic differences from average stature adults, including aberrant skinfolds, displaced anatomic landmarks, and excessive body fat. Reliable measurements without special equipment and requiring minimal or no modifications were achieved for height, weight, neck circumference, upper arm length, upper arm circumference, umbilical waist circumference, and maximal hip circumference. However, measurement of triceps and subscapular skinfolds and iliac crest waist circumference were dismissed, as they could not be reasonably modified to achieve reliable measurement.
During the same study, some modifications to measurements needed to be made. Firstly, a minimum of two contact points (head and buttocks), rather than the usual four (head, shoulders, buttocks, heels), were used during height measurement. Secondly, as it was not possible to use the C7 cervical vertebra as a marker for neck circumference measurement, the thyroid cartilage was used as a marker with the tape measure perpendicular to the long axis of the body. Thirdly, upper arm length measurement required multiple palpations of landmarks (acromion process and olecranon process). Fourthly, both waist and hip measurements required modifications to accommodate lumbar lordosis. Finally, waist circumference at the umbilicus was preferred to waist circumference at the iliac crest because the visual landmark of the former is easier to locate in individuals with achondroplasia.
Recommendations for Measurements in Adults with Achondroplasia
The minimum routine anthropometric measurements we recommend for adults with achondroplasia are weight and height. Clinics may wish to include additional measurements in their SOP, such as head circumference, neck circumference, arm span, upper arm length, upper arm circumference, waist circumference (umbilical), or maximal hip circumference (Table 1). These additional measurements should be considered for specific situations. For example, waist and hip circumference measurements are used to calculate waist-to-hip ratio (waist-to-hip ratio = waist circumference / maximal hip circumference). The waist-to-hip ratio may be useful as an indicator of obesity, as both weight and BMI may be misleading in people with achondroplasia. Measurement techniques for waist circumference, maximal hip circumference, neck circumference, upper arm length, and upper arm circumference are described and illustrated in Figs. 5, 6, 7, 8, 9.
Fig. 7.
Anthropometric measurements for adults with achondroplasia: neck circumference
Fig. 8.
Anthropometric measurements for adults with achondroplasia: upper arm length [adapted from National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. 2021; https://wwwn.cdc.gov/nchs/data/nhanes/public/2021/manuals/2021-Anthropometry-Procedures-Manual-508.pdf]
Fig. 9.
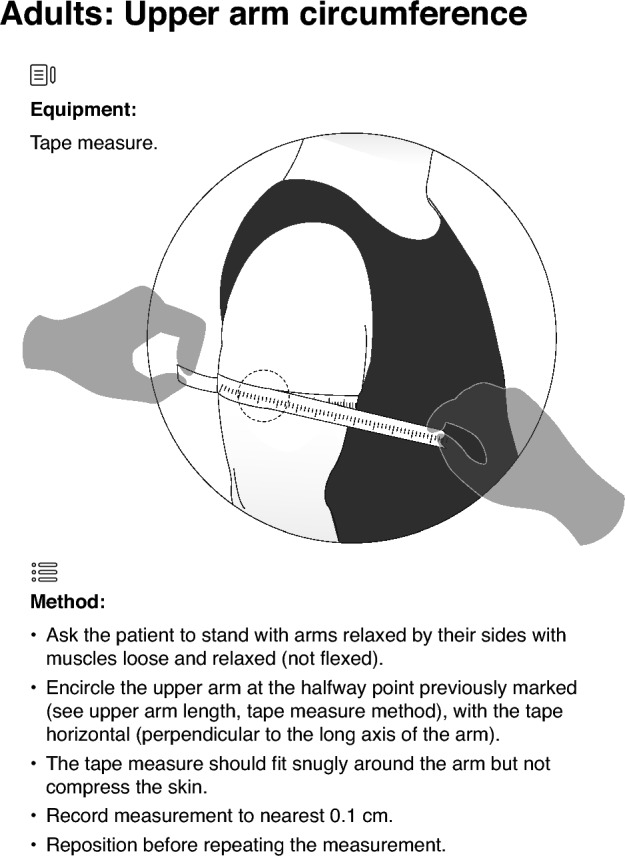
Anthropometric measurements for adults with achondroplasia: upper arm circumference [adapted from National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. 2021; https://wwwn.cdc.gov/nchs/data/nhanes/public/2021/manuals/2021-Anthropometry-Procedures-Manual-508.pdf]
Conclusion
Accurate, reliable anthropometric measurement of children and adults with disproportionate short stature, including achondroplasia, is required for clinical monitoring and for monitoring responses to pharmacologic treatments. This commentary, along with its accompanying infographics, provides guidance for key anthropometric measurements in children and adults with disproportionate short stature, in particular achondroplasia.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors thank all participants in the pilot study.
Medical Writing/Editorial Assistance
Medical writing assistance was provided by Koa Webster, PhD, CMPP, and Rebecca Lew, PhD, CMPP, of ProScribe – Envision Pharma Group, and funded by BioMarin Pharmaceutical Inc. ProScribe’s services complied with international guidelines for Good Publication Practice. The authors acknowledge the support of the Alan and Kathryn Greenberg Center for Skeletal Dysplasias and the Johns Hopkins Institute for Clinical and Translational Research, funders of the pilot study.
Author Contributions
Julie Hoover-Fong, Oliver Semler, Bobbie Barron, Paulo Ferrez Collett‑Solberg, Ellen Fung, Melita Irving, Taichi Kitaoka, Celide Koerner, Keita Okada, Katja Palm, Sérgio B. Sousa, and Klaus Mohnike were involved in the conceptualization of the content of the manuscript. Julie Hoover-Fong, Bobbie Barron, and Celide Koerner were involved in the study design, investigation, and data analysis of the pilot study of adults with achondroplasia. All authors participated in the drafting, critical revision, and approval of the final version of the manuscript.
Funding
BioMarin Pharmaceutical Inc., manufacturer of vosoritide, provided funding for medical writing assistance and publication fees (Open Access and Rapid Publication Fees). BioMarin facilitated the formation of the author team for this article and provided administrative and logistical support for manuscript development. BioMarin did not have any direct involvement in the drafting or preparation of the manuscript.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Declarations
Conflict of Interest
Julie Hoover-Fong has received honoraria from Ascendis, BioMarin, Innoskel, Medscape, QED Therapeutics, and Tyra for consulting, advisory board, and/or speaking for educational purposes, and participated as an investigator in clinical trials funded by Alexion, BioMarin, QED Therapeutics and Therachon/Pfizer. Oliver Semler has received speaker honoraria and travel support from BioMarin. Bobbie Barron is an employee of and receives funding from the Institute for Clinical and Translational Research, which is funded by the National Center for Advancing Translational Sciences through the Clinical & Translational Science Awards Program, grant number UL1TR003098. Paulo Ferrez Collett-Solberg has received speaker honoraria and travel support from BioMarin and from producers of recombinant human growth hormone. Ellen Fung was previously a consultant to BioMarin, and now receives grant funding from BioMarin for a research study of vosoritide in patients with mucopolysaccaridosis. Melita Irving has received honoraria from BioMarin for speaking, for participating in advisory board meetings, and as a member of the vosoritide experts steering committee. Taichi Kitaoka has received honoraria for lectures from BioMarin. Celide Koerner has no conflicts of interest to report. Keita Okada has received honoraria for lectures and travel support from BioMarin. Katja Palm has received speaker honoraria and travel support from BioMarin, and travel support from producers of growth hormone. Sérgio B. Sousa has received honoraria from BioMarin, Kyowa Kirin, and Ascendis for speaking, for participating in advisory board meetings, and for travel support; and participated as an investigator in achondroplasia clinical trials funded by Ascendis and Therachon/Pfizer. Klaus Mohnike has received honoraria from BioMarin, Novo-Nordisk and QED/Biogridge for speaking, for participating in advisory board meetings, and as a member of steering committees.
Ethical Approval
The pilot study briefly described in this commentary was conducted in accordance with ethical principles that have their origin in the Declaration of Helsinki and was approved by the JHMI Institutional Review Board.
References
- 1.Unger S, Ferreira CR, Mortier GR, et al. Nosology of genetic skeletal disorders: 2023 revision. Am J Med Genet A. 2023;191:1164–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fredriks AM, van Buuren S, van Heel WJ, Dijkman-Neerincx RH, Verloove-Vanhorick SP, Wit JM. Nationwide age references for sitting height, leg length, and sitting height/height ratio, and their diagnostic value for disproportionate growth disorders. Arch Dis Child. 2005;90:807–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Binder G, Ranke MB, Martin DD. Auxology is a valuable instrument for the clinical diagnosis of SHOX haploinsufficiency in school-age children with unexplained short stature. J Clin Endocrinol Metab. 2003;88:4891–6. [DOI] [PubMed] [Google Scholar]
- 4.Neumeyer L, Merker A, Hagenäs L. Clinical charts for surveillance of growth and body proportion development in achondroplasia and examples of their use. Am J Med Genet A. 2021;185:401–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Savarirayan R, Irving M, Harmatz P, et al. Growth parameters in children with achondroplasia: a 7-year, prospective, multinational, observational study. Genet Med. 2022;24:2444–52. [DOI] [PubMed] [Google Scholar]
- 6.Savarirayan R, Ireland P, Irving M, et al. International consensus statement on the diagnosis, multidisciplinary management and lifelong care of individuals with achondroplasia. Nat Rev Endocrinol. 2022;18:173–89. [DOI] [PubMed] [Google Scholar]
- 7.Nakano Y, Kubota T, Ohata Y, et al. Assessment of body fat mass, anthropometric measurement and cardiometabolic risk in children and adolescents with achondroplasia and hypochondroplasia. Endocr J. 2023;70:435–43. [DOI] [PubMed] [Google Scholar]
- 8.Pauli RM. Achondroplasia: a comprehensive clinical review. Orphanet J Rare Dis. 2019;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Foreman PK, van Kessel F, van Hoorn R, van den Bosch J, Shediac R, Landis S. Birth prevalence of achondroplasia: a systematic literature review and meta-analysis. Am J Med Genet A. 2020;182:2297–316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barat-Houari M, Dumont B, Fabre A, et al. The expanding spectrum of COL2A1 gene variants IN 136 patients with a skeletal dysplasia phenotype. Eur J Hum Genet. 2016;24:992–1000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gregersen PA, Savarirayan R, et al. Type II collagen disorders overview. In: Adam MP, Feldman J, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, et al., editors. GeneReviews®. Seattle, WA: University of Washington, Seattle; 1993. [PubMed] [Google Scholar]
- 12.Savarirayan R, Irving M, Bacino CA, et al. C-Type natriuretic peptide analogue therapy in children with achondroplasia. N Engl J Med. 2019;381:25–35. [DOI] [PubMed] [Google Scholar]
- 13.Savarirayan R, Tofts L, Irving M, et al. Once-daily, subcutaneous vosoritide therapy in children with achondroplasia: a randomised, double-blind, phase 3, placebo-controlled, multicentre trial. Lancet. 2020;396:684–92. [DOI] [PubMed] [Google Scholar]
- 14.Savarirayan R, Tofts L, Irving M, et al. Safe and persistent growth-promoting effects of vosoritide in children with achondroplasia: 2-year results from an open-label, phase 3 extension study. Genet Med. 2021;23:2443–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Savarirayan R, Hoernschemeyer DG, Ljungberg M, et al. Once-weekly TransCon CNP (navepegritide) in children with achondroplasia (ACcomplisH): a phase 2, multicentre, randomised, double-blind, placebo-controlled, dose-escalation trial. EClinicalMedicine. 2023;65: 102258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savarirayan R, De Bergua JM, Arundel P, et al. Infigratinib in children with achondroplasia: the PROPEL and PROPEL 2 studies. Ther Adv Musculoskelet Dis. 2022;14:1759720x221084848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Whitehouse R, Tanner J, Healy M. Diurnal variation in stature and sitting height in 12–14-year-old boys. Ann Hum Biol. 1974;1:103–6. [DOI] [PubMed] [Google Scholar]
- 18.Voss L, Bailey B. Diurnal variation in stature: is stretching the answer? Arch Dis Child. 1997;77:319–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Tofts L, Das S, Collins F, Burton KLO. Growth charts for Australian children with achondroplasia. Am J Med Genet A. 2017;173:2189–200. [DOI] [PubMed] [Google Scholar]
- 20.Hoover-Fong J, McGready J, Schulze K, Alade AY, Scott CI. A height-for-age growth reference for children with achondroplasia: expanded applications and comparison with original reference data. Am J Med Genet A. 2017;173:1226–30. [DOI] [PubMed] [Google Scholar]
- 21.Merker A, Neumeyer L, Hertel NT, et al. Growth in achondroplasia: development of height, weight, head circumference, and body mass index in a European cohort. Am J Med Genet Part A. 2018;176:1723–34. [DOI] [PubMed] [Google Scholar]
- 22.Hoover-Fong JE, Schulze KJ, Alade AY, et al. Growth in achondroplasia including stature, weight, weight-for-height and head circumference from CLARITY: achondroplasia natural history study-a multi-center retrospective cohort study of achondroplasia in the US. Orphanet J Rare Dis. 2021;16:522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merker A, Neumeyer L, Hertel NT, Grigelioniene G, Mohnike K, Hagenäs L. Development of body proportions in achondroplasia: sitting height, leg length, arm span, and foot length. Am J Med Genet A. 2018;176:1819–29. [DOI] [PubMed] [Google Scholar]
- 24.del Pino M, Fano V, Lejarraga H. Growth references for height, weight, and head circumference for Argentine children with achondroplasia. Eur J Pediatr. 2011;170:453–9. [DOI] [PubMed] [Google Scholar]
- 25.Mäkitie O, Kaitila I. Growth in diastrophic dysplasia. J Pediatr. 1997;130:641–6. [DOI] [PubMed] [Google Scholar]
- 26.Cheung MS, Cole TJ, Arundel P, et al. Growth reference charts for children with hypochondroplasia. Am J Med Genet A. 2024;194:243–52. [DOI] [PubMed] [Google Scholar]
- 27.Terhal PA, van Dommelen P, Le Merrer M, et al. Mutation-based growth charts for SEDC and other COL2A1 related dysplasias. Am J Med Genet C Semin Med Genet. 2012;160C:205–16. [DOI] [PubMed] [Google Scholar]
- 28.Montaño AM, Tomatsu S, Brusius A, Smith M, Orii T. Growth charts for patients affected with Morquio A disease. Am J Med Genet A. 2008;146a:1286–95. [DOI] [PubMed] [Google Scholar]
- 29.Robinson M-E, Rauch D, Glorieux FH, Rauch F. Standardized growth charts for children with osteogenesis imperfecta. Pediatr Res. 2023;94:1075–82. [DOI] [PubMed] [Google Scholar]
- 30.Hoover-Fong JE, Schulze KJ, McGready J, Barnes H, Scott CI. Age-appropriate body mass index in children with achondroplasia: interpretation in relation to indexes of height. Am J Clin Nutr. 2008;88:364–71. [DOI] [PubMed] [Google Scholar]
- 31.Ireland PJ, Savarirayan R, Pocovi T, et al. Development of the screening tool for everyday mobility and symptoms (STEMS) for skeletal dysplasia. Orphanet J Rare Dis. 2021;16:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Todorov AB, Scott CI Jr, Warren AE, Leeper JD. Developmental screening tests in achondroplastic children. Am J Med Genet. 1981;9:19–23. [DOI] [PubMed] [Google Scholar]
- 33.Ireland PJ, Donaghey S, McGill J, et al. Development in children with achondroplasia: a prospective clinical cohort study. Dev Med Child Neurol. 2012;54:532–7. [DOI] [PubMed] [Google Scholar]
- 34.World Health Organization. Child growth standards. Available from: https://www.who.int/tools/child-growth-standards/. Accessed Mar 28, 2024.
- 35.Tanner JM. Normal growth and techniques of growth assessment. Clin Endocrinol Metab. 1986;15:411–51. [DOI] [PubMed] [Google Scholar]
- 36.Garza C, Borghi E, Onyango AW, de Onis M. Parental height and child growth from birth to 2 years in the WHO multicentre growth reference study. Matern Child Nutr. 2013;9(Suppl 2):58–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Been E, Kalichman L. Lumbar lordosis. Spine J. 2014;14:87–97. [DOI] [PubMed] [Google Scholar]
- 38.Papaliodis DN, Bonanni PG, Roberts TT, et al. Computer assisted Cobb angle measurements: a novel algorithm. Int J Spine Surg. 2017;11:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.American Academy of Pediatrics. EQIPP Clinical Guide - Growth: Upper to Lower Segment Ratio. Available from: https://eqipp.aap.org/courses/growth2/mn/clinical-guide/popups/upper-to-lower-segment-ratio. Accessed Aug 8, 2024.
- 40.Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. Vital Health Stat 10. 2012;2012:1–207. [PubMed] [Google Scholar]
- 41.Young T, Shahar E, Nieto FJ, et al. Predictors of sleep-disordered breathing in community-dwelling adults: the sleep heart health study. Arch Intern Med. 2002;162:893–900. [DOI] [PubMed] [Google Scholar]
- 42.Subramanian S, Guntupalli B, Murugan T, et al. Gender and ethnic differences in prevalence of self-reported insomnia among patients with obstructive sleep apnea. Sleep Breath. 2011;15:711–5. [DOI] [PubMed] [Google Scholar]
- 43.Wijnhoven HA, van Bokhorst-de van der Schueren MA, Heymans MW, et al. Low mid-upper arm circumference, calf circumference, and body mass index and mortality in older persons. J Gerontol A Biol Sci Med Sci. 2010;65:1107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Yatsuya H, Folsom AR, Yamagishi K, North KE, Brancati FL, Stevens J. Race- and sex-specific associations of obesity measures with ischemic stroke incidence in the atherosclerosis risk in communities (ARIC) study. Stroke. 2010;41:417–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schulze KJ, Alade YA, McGready J, Hoover-Fong JE. Body mass index (BMI): the case for condition-specific cut-offs for overweight and obesity in skeletal dysplasias. Am J Med Genet A. 2013;161a:2110–2. [DOI] [PubMed] [Google Scholar]
- 46.Wynn J, King TM, Gambello MJ, Waller DK, Hecht JT. Mortality in achondroplasia study: a 42-year follow-up. Am J Med Genet A. 2007;143a:2502–11. [DOI] [PubMed] [Google Scholar]
- 47.Pimenta JM, Irving M, Cheung M, Mazzeo L, Landis S, Mukherjee S. Higher rates of non-skeletal complications and greater healthcare needs in achondroplasia compared to the general UK population: a matched cohort study using the CPRD database. Orphanet J Rare Dis. 2023;18:211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fredwall SO, Linge J, Leinhard OD, et al. Cardiovascular risk factors and body composition in adults with achondroplasia. Genet Med. 2021;23:732–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fredwall SO, Linge J, de Vries O, et al. Fat infiltration in the thigh muscles is associated with symptomatic spinal stenosis and reduced physical functioning in adults with achondroplasia. Orphanet J Rare Dis. 2023;18:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ogden JA. Radiology of postnatal skeletal development X Patella and tibial tuberosity. Skeletal Radiol. 1984;11:246–57. [DOI] [PubMed] [Google Scholar]
- 51.Centers for Disease Control, National Center for Health Statistics. National Health and Nutrition Examination Survey (NHANES): Anthropometry Procedures Manual. 2021 (updated May 2021). Available from: https://wwwn.cdc.gov/nchs/data/nhanes/public/2021/manuals/2021-Anthropometry-Procedures-Manual-508.pdf. Accessed Mar 27, 2024.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.