Abstract
Background
Dental implants are a reliable solution for tooth loss, but challenges remain regarding osseointegration and complications. Photobiomodulation therapy (PBMT), including Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy, has shown potential in enhancing bone healing. However, comparative studies on their effects on osteoblasts and osteoclasts are limited.
Aim
To compare the effects of LLLT and LED therapy on osteoblast proliferation and osteoclast suppression in an in vitro co-culture model.
Materials and methods
MG-63 osteoblast-like cells and RAW 264.7 osteoclasts were co-cultured on titanium discs. Discs were treated with LLLT (940 nm, 50 mW) or LED (660 nm, 89 mW) for different durations. Osteoblast proliferation was measured by MTT assay, and osteoclast activity was evaluated using TRAP staining and resorption pit analysis.
Results
LED therapy significantly enhanced osteoblast proliferation and suppressed osteoclast activity more effectively than LLLT. Optimal results were observed with a 6-min LED exposure.
Conclusion
LED therapy shows greater potential than LLLT for promoting osteoblast proliferation and suppressing osteoclast activity, indicating its clinical value for improving bone regeneration and implant integration.
Keywords: Photobiomodulation therapy, Low-level laser therapy (LLLT), Light emitting diode(LED) therapy, Bone regeneration, Dental implants, Titanium integration
1. Introduction
Dental implants have revolutionized restorative dentistry by providing an effective and long-lasting solution for tooth replacement. They address significant oral and overall health issues that arise from tooth loss, including functional impairments in eating, speaking, and maintaining oral hygiene. The absence of teeth leads to jawbone deterioration due to the lack of stimulation from natural tooth roots. This bone loss can alter facial structure and complicate subsequent dental procedures.
The success of dental implants depends on their ability to integrate with the jawbone through a process known as osseointegration. While dental implants have a high success rate of 90 %–95 % over ten years in healthy individuals, certain factors such as inadequate osseointegration, mechanical failures, and peri-implant infections can lead to complications. Systemic conditions like diabetes and osteoporosis may further jeopardize the success of implants by impairing the healing process.1
Recently, photobiomodulation therapy (PBMT) has gained prominence for its potential to enhance wound healing and tissue regeneration. PBMT involves the use of non-ionizing light sources, such as Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy, to stimulate cellular processes that aid in tissue repair. LLLT uses low-power lasers to enhance bone density and reduce inflammation, while LED therapy uses visible light to boost adenosine triphosphate (ATP) production, thereby accelerating tissue repair.2,3
Despite the promising results of PBMT, its use in dental implantology is still under-explored, with inconsistent study methodologies leading to mixed outcomes. There is a notable lack of comparative research evaluating the effects of LLLT and LED therapy on both osteoblastic (bone-forming) and osteoclastic (bone-resorbing) activities, which are crucial for successful implant integration.4
This study aims to address these gaps by comparing the osteogenic potential and osteoclastic suppression effects of LLLT and LED therapy in a co-culture system. By assessing these therapies across multiple exposure durations, this research seeks to refine PBMT protocols and enhance their application in dental implant procedures, ultimately improving clinical outcomes and implant success rates.
The aim of this study is to evaluate and compare the osteogenic potential and osteoclastic suppression effects of Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy on MG 63 osteoblast-like cells and RAW 264.7 osteoclasts -like cells cultured on titanium discs in a co-culture medium. This will be done across multiple exposure durations to determine their influence on bone regeneration. Specifically, the study aims to assess and compare the effects of LLLT and LED therapy on osteoblast growth and proliferation, as well as their ability to reduce osteoclast activity and bone resorption. Additionally, the study seeks to identify the most effective exposure duration—2, 4, or 6 mins—for both therapies in enhancing osteoblast proliferation and suppressing osteoclast function.
Furthermore, the study will investigate the impact of LLLT and LED therapy on cell migration, attachment, and osseointegration with titanium surfaces using scanning electron microscopy. Ultimately, a comparative analysis will be conducted to determine which therapy is more effective in promoting bone regeneration and integration with titanium implants.
2. Materials and methodology
The study was conducted following approval from the Institutional Ethics Committee (IEC), with the approval number [SRMDC/IRB/2024/PhD/No.157]. All procedures adhered to ethical guidelines for in vitro research. The study was conducted over a period of 3 months, from March 2024 to July 2024, allowing time for sample preparation, treatment, and evaluations.
2.1. Study design
The study is an in vitro experimental investigation designed to evaluate and compare the effects of two photobiomodulation therapies—Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy—on both osteogenic potential and osteoclastic suppression. The study employs a co-culture system, incorporating both osteoblastic and osteoclastic cells, to simulate the complex interactions occurring in bone regeneration.
2.2. Experimental setup
2.2.1. Sample preparation and group allocation
Titanium discs, 10 mm in diameter and 3 mm in thickness, were prepared from Ti6Al4V rods, cleaned, and autoclaved as previously described. A total of 42 titanium discs were allocated into three groups: Control Group (6 samples), Experimental Group I (LLLT) with 18 samples, and Experimental Group II (LED) with 18 samples (Fig. 1, Fig. 2). Each experimental group was further subdivided based on exposure durations of 2 min, 4 min, and 6 min, resulting in three subcategories per group. Randomization of the discs was carried out using a random number generator to assign them to LLLT, LED, or control groups, ensuring the elimination of bias. Sample size determination was based on a statistical power analysis, aiming for an 80 % power level to detect moderate to large effect sizes, in alignment with prior research findings. To maintain objectivity, a double-blind approach was employed, with both the personnel administering the treatments and those performing the assays and data analyses blinded to the group allocations. The discs were coded accordingly to uphold the blinding throughout the experiment.
Fig. 1.
Grouping of samples.
Fig. 2.
Preparation and group allocation of titanium discs.
2.2.2. Co-culture system
The co-culture system included MG-63 human osteosarcoma cells (representing osteoblasts) and RAW 264.7 cells (representing osteoclasts).Cells were co-cultured in Dulbecco's Modified Eagle Medium (DMEM) supplemented with 10 % fetal bovine serum (FBS) and 1 % penicillin-streptomycin. Cultures were maintained in a humidified incubator at 37 °C with 5 % carbondioxide.5
2.2.3. Treatment protocols
-
◦
Experimental Group I (LLLT): Irradiation with infrared Ga-As-P laser diodes at a wavelength of 940 nm, with an output power of 50 mW and a total energy density of 6 J/cm2 in continuous wave mode. The treatment was administered from a distance of 3 cm (Fig. 3).6
-
◦
Experimental Group II (LED): Exposure to visible red LEDs at a wavelength of 660 nm, with a beam power of 89 mW, power density of 12.59 mW/cm2, and an energy density of 10 J/cm2. The treatment was applied from a distance of 3 cm (Fig. 4).7
Fig. 3.
Lllt device and irradiation on cultured titanium discs.
Fig. 4.
Led device and irradiation on cultured titanium discs.
2.2.4. Evaluation parameters
Each experimental subgroup (totally 6 samples) was further divided into two sets for evaluation purposes. One set of samples (3 samples of each subgroup) was utilized to assess osteoblast proliferation, while the other set (3 samples of each subgroup) was used to evaluate osteoclastic activity. This division allowed for a focused analysis of the effects of Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy on both osteoblast growth and osteoclast suppression.
-
◦
Osteoblast Proliferation: Assessed using the Dimethyl thiazolyl diphenyl tetrazolium (MTT) assay at 72 h, The evaluation of the osteogenic potential and osteoclastic suppression was carried out using a comprehensive set of assays and analyses designed to capture various aspects of cell behavior and functionality. Cell viability and proliferation were assessed using the MTT assay, which measures the metabolic activity of cells by detecting the reduction of MTT to formazan crystals. In addition, cell attachment, growth, and proliferation were further evaluated by incubating the cells with MTT solution, followed by dissolution of the formazan crystals in dimethyl sulfoxide (DMSO), and measuring absorbance at 570 nm. Enhanced absorbance indicated increased cell attachment, growth, and proliferation (Fig. 5, Fig. 6).
-
◦
Osteoclast Suppression: Evaluated using Tartrate-Resistant Acid Phosphatase (TRAP) staining to measure osteoclast activity and resorption pit formation at 72 hr.TRAP staining was employed to identify and quantify osteoclast activity. This method involves staining for TRAP, an enzyme specific to osteoclasts, and visualizing the TRAP-positive cells under a microscope. The number of TRAP-positive cells was counted to assess the extent of osteoclastic activity. Additionally, the resorption pit assay was conducted to evaluate the area of bone resorption, providing a measure of osteoclast-induced bone degradation.
-
◦
Post-treatment analysis: It included scanning electron microscopy to observe the morphology of the cells and the formation of osseointegration and cell migration patterns. These combined evaluation parameters allowed for a detailed analysis of the effects of Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy on both osteogenic and osteoclastic activities in the co-culture system.6
-
◦
Data Collection: Results were compiled to assess the comparative effectiveness of LLLT and LED therapy in enhancing osteogenic potential and suppressing osteoclastic activity within the co-culture system.
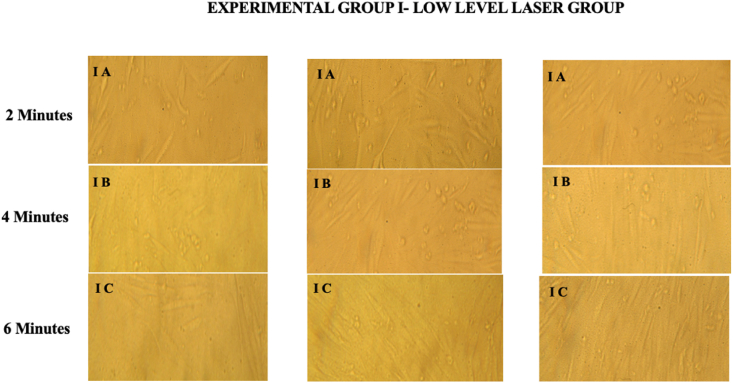
Fig. 5.
Osteoblast Proliferation in LLLT Group at Different Exposure Durations (2 min, 4 min, 6 min).
Fig. 6.
Osteoblast Proliferation in LED Group at Different Exposure Durations (2 min, 4 min, 6 min).
This experimental design enables a comprehensive comparison of LLLT and LED therapy effects on both osteoblast and osteoclast cells, providing insights into their combined impact on bone regeneration and implant integration.Table 1 provides the mean values of osteoblast proliferation and osteoclast suppression (TRAP-positive cells and resorption pit area) across different subgroups, demonstrating the effects of LLLT and LED treatments.
Table 1.
Mean values of osteoblast proliferation and osteoclast suppression across subgroups.
| Subgroup | Osteoblast Proliferation (OD at 570 nm) | Osteoclast Suppression (TRAP-Positive Cells) | Resorption Pit Area (mm2) |
|---|---|---|---|
| Control | 0.35 ± 0.03 | 112 ± 9 | 1.8 ± 0.2 |
| LLLT Subgroup IA (2 min) | 0.48 ± 0.04 | 97 ± 8 | 1.5 ± 0.3 |
| LLLT Subgroup IB (4 min) | 0.55 ± 0.05 | 89 ± 7 | 1.3 ± 0.2 |
| LLLT Subgroup IC (6 min) | 0.60 ± 0.06 | 82 ± 7 | 1.2 ± 0.2 |
| LED Subgroup IIA (2 min) | 0.52 ± 0.04 | 79 ± 6 | 1.1 ± 0.2 |
| LED Subgroup IIB (4 min) | 0.62 ± 0.05 | 63 ± 5 | 0.9 ± 0.1 |
| LED Subgroup IIC (6 min) | 0.70 ± 0.07 | 45 ± 4 | 0.5 ± 0.1 |
∗LLLT- Low level laser Therapy, LED- Light emitting diode, OD -Optical Density.
3. Statistical analysis
For statistical analysis, data were first assessed for normality using the Shapiro-Wilk test, which confirmed normal distribution for all subgroups (p > 0.05). Homogeneity of variances was tested with Levene's test, showing equal variances across groups (p > 0.05). To compare the mean values of osteoblast proliferation and osteoclast suppression among the control, LLLT, and LED groups, a one-way ANOVA was performed. The results indicated statistically significant differences between the groups for both outcomes (p < 0.001). Post-hoc Tukey HSD tests revealed that the LED treatment in Subgroup IIC resulted in significantly higher osteoblast proliferation compared to the control and all LLLT subgroups (p < 0.001). Additionally, LED Subgroup IIC demonstrated significantly lower TRAP-positive cell counts and reduced resorption pit areas, reflecting enhanced osteoclast suppression compared to both control and LLLT subgroups (p < 0.001). Effect sizes, as measured by partial η2, indicated large differences between groups (partial η2 > 0.14), highlighting the substantial impact of LED treatment on both osteoblast proliferation and osteoclast suppression. The present study result analysis confirms that LED treatment, particularly in Subgroup IIC, resulted in significantly enhanced osteoblast proliferation and osteoclast suppression compared to LLLT and control groups(Graph, Graph 2).
Graph.
1Mean values of osteoblast proliferation across subgroups.
Graph 2.
Mean values of osteoclast suppression across subgroup.
4. Discussion
This study was conducted to evaluate the effects of low-level laser therapy (LLLT) and light-emitting diode (LED) therapy on osteoblast proliferation and osteoclast suppression in a co-culture system. The study successfully met its objectives by providing a comprehensive evaluation of the effects of Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy on osteoblast and osteoclast activities. The motivation behind this research was to explore non-invasive treatments that could enhance bone regeneration and manage bone resorption, which is crucial in dental and orthopedic applications. Osteoblasts and osteoclasts play significant roles in bone homeostasis, and understanding how different light therapies influence these cells can provide insights into improving treatment outcomes for bone-related conditions.7, 8
The co-culture system of osteoblastic and osteoclastic cells was selected to closely mimic the in vivo bone environment, allowing for a comprehensive assessment of light therapies' effects on both bone formation and resorption. LLLT and LED therapy were chosen based on their established roles in modulating cellular processes. LLLT is known for promoting cell proliferation and tissue repair through photobiomodulation, while LED therapy offers similar benefits with the added advantages of lower cost and easier application. LLLT was administered with a wavelength of 940 nm, and LED therapy with a wavelength of 660 nm, targeting cellular pathways involved in osteogenesis and osteoclastogenesis.
Overall, the study's comparative analysis highlighted LED therapy as more effective in enhancing bone regeneration and integrating with titanium surfaces compared to LLLT. And the study's results align with previous research showing that both LLLT and LED therapy enhance osteoblast proliferation. This finding supports earlier studies, which reported increased osteoblastic activity following LLLT.9 Notably, the LED treatment showed a more pronounced increase in osteoblast proliferation compared to LLLT, consistent with findings by Cankaya et al. (2011)10 that specific LED wavelengths could more effectively stimulate osteoblastic activity. In terms of osteoclast suppression, our results indicate that LED therapy significantly reduced osteoclast activity, corroborating research by camolesi et al. (2023),11 which found that LED light could inhibit osteoclastogenesis. This contrasts with some studies reporting minimal effects of LLLT on osteoclast suppression, highlighting the potential of LED therapy as a more effective tool for managing bone resorption.
Limitations of this study include the use of an in vitro co-culture system, which may not fully replicate the complex in vivo bone environment, and the focus on short-term effects of light therapy. Future research should include in vivo studies to validate these findings and assess long-term outcomes. Additionally, exploring various wavelengths, intensities, and treatment durations could offer deeper insights into optimizing light therapy parameters.12,13
Clinically, the study's findings suggest that LED therapy could be a valuable adjunctive treatment for bone repair and regeneration, potentially offering improved outcomes over traditional LLLT in specific scenarios. Despite the valuable insights provided, the study's limitations include its reliance on an in vitro model, which may not fully replicate the complexities of the in vivo bone environment, and the short-term nature of the evaluation.Clinicians should consider incorporating LED therapy into treatment protocols to enhance bone healing and minimize bone resorption, as suggested by the results of this study. Further exploration and integration of LED therapy into clinical practice are warranted to fully leverage its benefits.
5. Conclusion
-
•
Both Low-Level Laser Therapy (LLLT) and Light Emitting Diode (LED) therapy demonstrated positive effects on osteoblast proliferation and osteoclast suppression, both of which are essential for successful bone regeneration and implant integration.
-
•
LED therapy was found to be superior to LLLT, particularly with a 6-min exposure duration, in enhancing osteoblast growth and reducing osteoclast activity.
-
•
LED therapy showed significantly greater osteogenic potential and more effective osteoclastic suppression compared to LLLT and control groups.
-
•
These findings align with prior research on the role of light-based therapies in bone regeneration and suggest that LED therapy may be a valuable adjunctive tool in managing bone resorption and promoting healing.
-
•
Future research should focus on expanding these findings through in vivo studies and exploring various light therapy parameters, such as wavelength and intensity, to refine treatment protocols.
-
•
Clinically, the incorporation of LED therapy holds promise for enhancing bone healing outcomes, offering a more accessible and potentially superior alternative to traditional LLLT in dental and orthopedic applications.
Patients or guardian consent
Not applicable - Since its an vitro study.
Funding
No Funding; All the expenses for the study provided on there own(Authors).
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgement
No Acknowledgement.
Graphs
This figure illustrates the osteoblastic activity in three subgroups of the LLLT group: IA (2 min), IB (4 min), and IC (6 min), with three samples per subgroup.
This figure displays osteoblastic activity in three subgroups of the LED group: II A (2 min), II B (4 min), and II C (6 min), with three samples per subgroup.
References
- 1.Diz P., Scully C., Sanz M. Dental implants in the medically compromised patient. J Dent. 2013 Mar;41(3):195–206. doi: 10.1016/j.jdent.2012.12.008. Epub 2013 Jan 11. PMID: 23313715. [DOI] [PubMed] [Google Scholar]
- 2.Mohajerani H., Salehi A.M., Tabei F., Shafiei R., Tabrizi R.T. Can low-level laser and light-emitting diode enhance the stability of dental implants? J Maxillofac Oral Surg. 2020 Apr-Jun;19(2):302–306. doi: 10.1007/s12663-019-01210-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Anders J.J. Inc.; 2016. Photobiomodulation. American Society for Laser Medicine and Surgery.https://www.aslms.org/for-the-public/treatments-using-lasers-and-energy-based-devices/photobiomodulation Available from: [Google Scholar]
- 4.Heiskanen V., Hamblin M.R. Photobiomodulation: lasers vs. light emitting diodes. Photochem Photobiol Sci. 2018 Aug 8;17(8):1003–1017. doi: 10.1039/c8pp90049c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sieberath A., Della Bella E., Ferreira A.M., Gentile P., Eglin D., Dalgarno K. A comparison of osteoblast and osteoclast in vitro Co-culture models and their translation for preclinical drug testing applications. Int J Mol Sci. 2020 Jan 30;21(3):912. doi: 10.3390/ijms21030912. PMID: 32019244; PMCID: PMC7037207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taradaj J., Halski T., Kucharzewski M., Urbanek T., Halska U., Kucio C. Effect of laser irradiation at different wavelengths (940, 808, and 658 nm) on pressure ulcer healing: results from a clinical study. Evid Based Complement Alternat Med. 2013;2013 doi: 10.1155/2013/960240. Epub 2013 Sep 12. PMID: 24159357; PMCID: PMC3789441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Selvam Divyabharathi, Natrajan Shanmuganathan1, Seenivasan Madhan Kumar1, Lavu Vamsi1. Effect of photobiomodulation therapy in type 2 diabetic patients on peri-implant osteoblastic activity, soft-tissue healing, and postoperative pain discomfort: a pilot study. Journal of Interdisciplinary Dentistry. May–Aug 2024;14(2):85–91. doi: 10.4103/jid.jid_66_23. [DOI] [Google Scholar]
- 8.Naderi M.S., Razzaghi M., Esmaeeli Djavid G., Hajebrahimi Z. A comparative study of 660 nm low-level laser and light emitted diode in proliferative effects of fibroblast cells. J Laser Med Sci. 2017;8(Suppl 1):S46–S50. doi: 10.15171/jlms.2017.s9. Epub 2017 Aug 29. PMID: 29071035; PMCID: PMC5642178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karakaya M., Demirbaş A.E. Effect of low-level laser therapy on osseointegration of titanium dental implants in ovariectomized rabbits: biomechanics and micro-CT analysis. Int. J. Implant Dent. 2020 Oct 12;6(1):61. doi: 10.1186/s40729-020-00257-z. PMID: 33043397; PMCID: PMC7548265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cankaya Abdulkadir, Erdem Mehmet, Erdem Arzu, et al. Evaluation of light-emitting diode (LED-660 Nm) application over primary osteoblast-like cells on titanium surfaces: an in vitro study. Int J Med Sci. 2011;8:584–593. doi: 10.7150/ijms.8.584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Camolesi G.C.V., Somoza-Martín J.M., Reboiras-López M.D., Camacho-Alonso F., Blanco-Carrión A., Pérez-Sayáns M. Photobiomodulation in dental implant stability and post-surgical healing and inflammation. A randomised double-blind study. Clin Oral Implants Res. 2023 Feb;34(2):137–147. doi: 10.1111/clr.14026. Epub 2022 Dec 28. PMID: 36541106; PMCID: PMC10107821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fernandes P.F., Grenho L., Fernandes M.H., Sampaio‐Fernandes J.C., Gomes P.S. Microgap and bacterial microleakage during the osseointegration period: an in vitro assessment of the cover screw and healing abutment in a platform‐switched implant system. J Prosthet Dent. 2021 doi: 10.1016/j.prosdent.2021.07.030. [DOI] [PubMed] [Google Scholar]
- 13.Trelles Mario, Allones Inés, Mayo Esther. Combined visible light and infrared light-emitting diode (LED) therapy enhances wound healing after laser ablative resurfacing of photodamaged facial skin. Med Laser Appl. 2006;21:165–175. doi: 10.1016/j.mla.2006.06.001. [DOI] [Google Scholar]