Abstract
The contribution of molecular genetics to colorectal cancer has been largely restricted to relatively rare inherited tumours and to the detection of germ line mutations predisposing to these cancers. However, much is now known about the somatic events leading to colorectal cancer in general. Several studies have examined the relation between genetic features and prognosis. The purpose of this article is to review these studies and summarise the current state of this subject. Although many of the published studies are small and inconclusive, it is clear that several different pathways exist for the development of this cancer, and some molecular characteristics seem to correlate with clinicopathological features. At present, studies are confined to evaluating a small number of molecular markers; however, with the advent of methods for the rapid genetic profiling of large numbers of colorectal cancers, it will be possible to evaluate fully the clinical usefulness of a range of colorectal cancer genotypes.
Keywords: colorectal cancer, prognosis, genes
Colorectal adenocarcinoma accounts for over 90% of the malignant tumours of the large bowel. After lung and breast cancer, colorectal cancer is the most common cause of death from malignant disease in the Western world. The incidence of the disease in England and Wales is about 30 000 cases/year,1 resulting in approximately 17 000 deaths/annum,2 and it has been estimated that at least half a million cases of colorectal cancer occur each year world wide.3 Incidence rates of colorectal cancer are increasing in many countries. Unfortunately, despite improvements in medical and surgical provision, there has been comparatively little change in mortality from colorectal cancer during the past 40 years,4 and the overall five year survival is only around 40%.
Natural history of colorectal cancer
In Western countries, approximately 60% of primary colorectal cancers are situated in either the rectum or sigmoid. Of the remainder, a half arise within the caecum. Colorectal cancers are generally staged according to Dukes's system into categories A, B, C, and D.5 Grade can be either expressed simply as degree of differentiation (well, medium, or poorly differentiated) or according to the more complex Jass grouping.6 Prognosis correlates extremely well with both stage and grade.
Patients with colorectal cancer fall broadly into two groups at time of presentation. The first group has either non-resectable or disseminated disease. These patients have a very poor prognosis, with a median survival of seven months.3 The other two thirds of patients will undergo a resection of their primary tumour. Despite an apparently “curative” resection, approximately 50% of patients die within five years, and of these around 80% will have had a detectable recurrence within two years. Most of these patients die as a result of liver metastases, but there is evidence that they also have extensive extrahepatic disease. Studies of occult hepatic metastases have estimated that the mean age of deposits at time of surgery is 18 months.7 This suggests that many colorectal cancers metastasise early, but that some tumours cannot or do not metastasise, and that the factors that determine the propensity to metastasise may have acted before presentation. Improved success in the treatment of colorectal cancer clearly requires a better understanding of its development and behaviour. Molecular studies have shown that the natural history of all colorectal cancers is not identical. The molecular basis of the clinicopathological features of some tumours has been determined. If genotypic markers could be identified that correlate with tumour behaviour and patient prognosis, this should lead to a more accurate prediction of prognosis and tailoring of treatment.
Molecular genetics of colorectal cancer
THE ADENOMA–CARCINOMA SEQUENCE
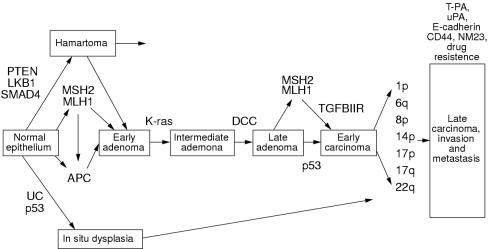
Histological observations led to the concept that most colorectal cancers develop from normal epithelium through sequentially worsening degrees of adenomatous dysplasia.8 The genetic pathway model for the pathogenesis of sporadic colorectal cancer proposed by Fearon and Vogelstein is based upon this concept of an adenoma to carcinoma sequence (fig 1 ▶).9 Although the total accumulation of mutations is the principal factor, the model proposed that the causative mutations in tumour suppressor genes and oncogenes occur in a specific order in most colorectal cancers (specifically, adenomatous polyposis coli (APC) gene mutations, global hypomethylation, K-ras mutations, deleted in colon cancer (DCC) gene mutations, and finally mutations in the p53 gene). The Fearon and Vogelstein model of colorectal carcinogenesis was proposed over 10 years ago. During this time, other mutations that occur at a high frequency in colorectal cancer have been identified, and the original model can be considerably elaborated to take in account the alternative pathways for the development of cancer that are now known to exist.
Figure 1.
Genetic pathways of colorectal carcinogenesis.
INITIATION OF COLORECTAL CARCINOGENESIS
There is good evidence that only two mutations are required for the initiation of colorectal carcinogenesis. In most cases, these mutations occur at the APC tumour suppressor locus (5q21–q22).10–12 APC mutations, which generally lead to a truncated APC protein,13 or take the form of allele loss,14 are detected in about 75% of sporadic colorectal cancers15 and are observed in the earliest adenomas.10 In addition to the role of the APC gene in the aetiology of sporadic colorectal cancer, germline mutations in this gene cause familial adenomatous polyposis coli (FAP), which is characterised by florid adenomas within the gastrointestinal tract. The APC protein acts as a dimer.16 It is likely that the gene product exerts its tumour suppressor actions through intracellular signalling, interactions with the cytoskeleton, and the control of cellular proliferation, possibly by affecting the rate of cell division or apoptosis.17–22
Whether APC mutations are always the first events in colorectal carcinogenesis or whether germline defects in one of the mismatch repair (MMR) genes could provide an alternative initiating step has been questioned. Mutations in three MMR genes primarily cause the dominantly inherited syndrome hereditary non-polyposis colorectal cancer (HNPCC): MSH2 on chromosome 2p, MLH1 on chromosome 3p, and MSH6 on chromosome 2p16.23–26 Colorectal cancers from patients with mutations in these MMR genes consistently show microsatellite instability (MSI), a form of replication error (RER). Although it is generally assumed that mutations in the MMR genes in HNPCC families act only to increase the mutation rate (including mutations in APC), it is also possible that the MMR mutations themselves have a direct role in initiation. MMR mutations also occur in sporadic coloectal cancers27; however, when these mutations arise somatically they occur after APC mutations and are therefore involved in the progression of tumours rather than initiation.28
Colorectal cancers associated with ulcerative colitis do not usually develop from adenomas,29 suggesting a different genetic pathway from sporadic cancers.30 The low frequency of APC mutations in inflammatory bowel disease associated cancers suggests that mutations in this gene are not the initiating event in these tumour types.31–33
The possibility that mutations in genes other than APC can initiate colorectal tumorigenesis is suggested by reports of adenoma families unlinked to APC.34 In addition, there is emerging evidence that a hamartoma–adenoma–carcinoma sequence exists,35 and genes for several hamartoma syndromes have been identified (such as Peutz Jeghers syndrome caused by LKB1 mutations,36 some forms of juvenile polyposis caused by SMAD4 mutations,37 and Cowden's syndrome caused by PTEN mutations38). Furthermore, there is some support for a hyperplastic polyp adenoma carcinoma sequence (fig 1 ▶).39
COLORECTAL CANCER PROGRESSION: EARLY ADENOMA TO CARCINOMA
Although mutations in the APC gene are initiating events in colorectal tumorigenesis, these mutations alone are probably insufficient for adenomas to progress, and without mutations at other loci regression might occur.40, 41 Several genes are involved in the progression of early adenomas to early carcinomas. Early candidates for adenoma progression were the ras oncogenes. The K-ras gene is one of a family of three human ras genes (K-ras, H-ras, and N-ras).42 These encode small GTP binding proteins localised to the inner leaflet of the cell membrane and are involved in transducing signals from receptor tyrosine kinases such as epidermal growth factor receptor (EGFR). The receptors are coupled to the ras proteins through an intermediate complex of GRB and SOS2 proteins. Downstream elements of this transduction pathway include the cytoplasmic RAF serine threonine kinase and mitogen activated protein (MAP) kinase cascade. The ras proteins are activated on binding GTP and deactivated by intrinsic GTPase activity from two GTPase activating (GAP) proteins. One of these is ras-GAP-p120 and the other neurofibromin, the product of the NF1 gene. The ras oncogenes are activated by point mutations that prevent the activation of GTPase.42 More than 50% of colorectal cancers display specific mutations in the K-ras gene, with an increasing frequency in larger and more advanced lesions.43 The consequence of K-ras mutations during tumour development may be a growth advantage of those cells with both APC and K-ras mutations over cells with APC mutations alone. Whereas K-ras mutations are seen within histologically normal mucosa,44 they appear only to be present in dysplastic mucosa with coexisting APC mutations.45, 46 This supports the notion that K-ras mutations confer no growth advantage in the absence of a mutation in the APC gene.
The MCC (mutated in colon cancer) and DCC tumour suppressor genes were originally thought to play a role in colorectal carcinogenesis. In the model of Fearon and Vogelstein, mutation at the DCC locus represented the third step in the genetic pathway.9 The MCC and DCC genes were identified as a result of the frequent allele loss close to their locations on 5q21–q22 and 18q21.3, respectively, in colorectal cancers.47, 48 A small number of mutations at MCC were originally described in colorectal cancers,49 but subsequent studies have found very few mutations, suggesting that APC is the primary target for allele loss on 5q21–q22.50 DCC is a neural cell adhesion molecule homologue and DCC mutations may therefore have a role in colorectal tumour progression, invasion, and metastasis (although allele loss at DCC generally occurs before malignancy). However, there is evidence suggesting that SMAD4 may also be the target of allele loss on chromosome 18q in some cancers.51
There is no doubt about the role of p53 mutations in the progression of colorectal tumours. The p53 protein is important in maintaining DNA integrity. DNA damage results in p53 mediated arrest in G1 phase of the cell cycle, followed by repair or, if the damage is too great, p53 induced apoptosis. Therefore, loss of function of p53 by mutation or deletion allows cells to accumulate mutations throughout the genome and results in karyotypic instability, impaired G1 cell cycle arrest, and reduced apoptosis.52–55 Mutations in the p53 gene occur in around 75% of colorectal cancers, but the frequency is lower in mucinous cancers and those that arise in the proximal colon, as seen in HNPCC. p53 mutations are rare in adenomas, suggesting that p53 plays a role in tumour progression, but it is not an absolute requirement for malignant transformation because a large proportion of cases have no demonstrable abnormality. p53 mutations tend to occur at the late adenoma stage (although earlier in inflammatory bowel disease associated colorectal cancers, which do not develop from adenomas).56 Dominant, gain of function mutations in p53 are common in colorectal cancers, and these can be detected reliably using immunohistochemistry for the p53 protein.57, 58 Allele loss near p53 (chromosome 17p13.1) also occurs frequently,56 either because of loss of the wild-type allele or possibly because another gene nearby is targeted.
The sites of other candidate tumour suppressor genes that might be involved in colorectal tumour progression have been identified by allele loss studies. Mutations of the FHIT gene59 and at the p16 (MTS1) locus60–62 may be important in colorectal tumours, the latter through failure of cell cycle arrest. Locations of other tumour suppressor loci include chromosomes 1p (near the putative human Mom-1 homologue),63, 64 6q,65 8p,66, 67 14q,68 and 22q.69 Allele loss typically occurs at these locations at frequencies of between 30% and 60%.
The roles of MMR mutations in colorectal tumorigenesis have been discussed briefly. In HNPCC tumours, one mutation is inherited and the other occurs somatically; in about 15% of sporadic colon cancers, two MMR mutations (or two mutations at a related locus) occur in the soma.70 Normal mucosa from patients with HNPCC does not display MSI; only 50% of HNPCC adenomas (compared with 90% of cancers) exhibit MSI, and the frequency of early lesions such as APC mutations is similar in MSI and MSS (microsatellite stable) tumours.71, 72 Therefore, in sporadic cancers, defective MMR function might be an alternative method to allele loss of acquiring mutations, and loss of MMR may simply “catalyse” the progress of a tumour down the same pathway as MSS cases. It is possible that MMR mutations act as alternatives to p53 mutations in colorectal tumours, albeit through a different mechanism. Whereas genomic instability in p53 mutant cancers tends to take the form of karyotypic abnormalities, instability resulting from MMR mutations leads to near diploid lesions. It has been found that MMR mutations are negatively associated with mutant p53 and that, like p53 mutations, MMR mutations often occur in late colonic adenomas.72, 73 Genomic instability may also be caused by somatic or germline mutations in other genes involved in DNA replication and repair. There is support for this from a study of two apparently sporadic colorectal cancer cases that harboured DNA polymerase δ variants.74
MALIGNANCY
Few genetic changes specific to mature colorectal cancers have been identified. Several regions of allele loss have been detected, but their roles in tumour progression are unclear. The types of mutations that will be important in mature colorectal cancer are those that cause faster replication, decreased apoptosis, or angiogenesis. Malignancy requires colorectal tumour cells to exhibit several features, namely: (1) the ability to erode the basement membrane; (2) the ability to disrupt normal cell junctions; and (3) the capacity to survive in the blood or lymphatic systems and in a new tissue environment.
Cell adhesion molecules are candidates for involvement in the process of invasion and metastasis of colorectal cancers. Mutations at these loci may have effects on growth, in addition to those on adhesion. For example, E cadherin forms part of the adherens junction complex of epithelial cells. Loss of E cadherin protein occurs in several cancers, including colorectal cancer, and is associated with the development of invasive properties.75–77 Other proteins that may be associated with invasion of colorectal cancers include those involved in tissue degradation, such as urokinase plasminogen activators and matrix metalloproteinases/collagenases.78, 79 The cells of metastases may have genotypes and/or patterns of gene expression distinct from primary tumours. Variation at several gene loci may alter the behaviour pattern of the mature colorectal cancer. These include the NM23 gene, which has a possible role in the metastasis of several cancers, and CD44.80–85
Clinicopathological correlations: prediction of prognosis
The recognition that there are probably several different genetic pathways for colorectal cancer suggests that correlations exist between the molecular and clinicopathogical features of tumours that are not apparent using routine methods such as histology. These correlations may serve as prognostic determinants and/or enable the partitioning of patients with colorectal cancer into groups for different treatments. Several studies have sought to examine the relation between genotypic variation in colorectal cancers and clinicopathological features, especially prognosis. Most work has been in the form of case control studies using a comparison of the frequency of genotypes in primary and secondary tumours as a surrogate for survival. However, a small number of studies have examined the relation between genotype and prognosis by classic survival analysis. In this section, the evidence for genetic variation in colorectal cancers as markers of prognosis is reviewed, including some studies of protein or mRNA expression that have been assumed to be indicators of underlying mutations.
ALLELE LOSS STUDIES
In an early allelotyping study based upon 56 patients with colorectal cancer, Vogelstein et al showed that patients with more than the median percentage of allelic deletions had a worse prognosis.86 Later studies have examined the relation between specific chromosome abnormalities and tumour behaviour.
Chromosome 18q loss has been evaluated extensively as a prognostic marker in several studies.47, 87–93 In a study of 145 patients with resected stage II or stage III disease reported by Jen et al,47 the five year survival rate was 93% in those with no loss and 54% in those with chromosome 18q loss in stage II disease, and 52% and 38%, respectively, with stage III disease. The overall estimated hazard ratio (HR) for death associated with tumour chromosome 18q loss was 2.8 (p < 0.01) in a univariate analysis. Allelic loss remained a strong predictive factor after adjustment for tumour differentiation, vein invasion, and TNM stage (HR = 2.46; 95% confidence interval (CI), 1.06 to 5.71; p = 0.04). A similar finding was reported by Ogunbiyi et al from an analysis of 151 patients who had undergone potentially curative surgery for colonic disease.91 Chromosome 18q allelic loss was a negative prognostic indicator of both disease free (HR = 1.65; p = 0.01) and disease specific survival (HR = 2.0; p = 0.003). Furthermore, 18q loss was associated with significantly reduced disease free and disease specific survival in cases with stage II (p = 0.05 and p = 0.016) and III (p = 0.038 and p = 0.032) disease. Two studies have specifically examined the relation between 18q allele loss and prognosis in stage II disease.92, 93 The study reported by Martinez-Lopez et al based on 144 patients supported the notion that allele loss in tumours is associated with an unfavourable outcome.93 Five year survival was 42% in those with chromosome 18q loss and 73% in those without detectable loss (p < 0.01). Multivariate analysis showed that tumour site (p < 0.001) and 18q loss (p = 0.01) were the only independent prognostic factors. Furthermore, loss had a significant influence on survival (p = 0.016). In contrast, the study reported by Carethers et al,92 based on 70 patients, found that 18q allelic loss was not associated with a survival disadvantage (HR = 1.17; 95% CI, 0.27 to 5.10).
Cytogenetic and allele loss studies of chromosome 17 (and in particular at the NM23 locus) have been based on fewer patients than the analyses of chromosome 18q.87, 94–96 Most studies have found that both 17p and 17q anomalies are associated with invasion and metastasis, and allele loss at 17q has been proposed to provide independent prognostic information.95
Mutations that are likely to have prognostic relevance are those that occur in genes involved in tumour progression rather than initiation. Therefore, it is not surprising that allele loss at chromosome 5q, the site of the APC gene, has not been shown to have prognostic value.87, 88, 90 The high rate of allele loss in other chromosomes such as 8p, 1p, and 11q during tumour progression suggests that these may be sites of other tumour suppressor genes important for the progression of colon tumours. A correlation between 8p allele loss and microinvasion (a prognostic marker independent of Dukes's stage) has been reported in one small study of 14 patients with cancer.97 A relation between tumour progression and chromosome 1 deletions has also been shown in one study of 116 patients who had undergone curative treatment (HR = 4.1; 95%CI, 1.25 to 9.23).98
Allele loss at other chromosomes has been evaluated less extensively. An analysis of 126 sporadic colorectal cancers for allele loss at chromosome 11q22 failed to show a relation with Dukes's grade or degree of differentiation.99 A prospective study assessing allelic loss at chromosome 4p14–16 in 181 patients has suggested that allele loss may be associated with a shorter disease free survival.100
K-RAS
Along with p53, K-ras mutations are one of the most common genetic lesions in human cancer. Since the discovery of the human ras gene family, the effect of different ras mutations on tumour behaviour have been debated. Point mutations in codons 12, 13, and 61 of the K-ras gene are early events in the pathogenesis of colorectal cancer. However, the impact of the number, type, and position of such mutations on the progression of adenomas, in addition to the clinical behaviour of colorectal carcinomas, is not fully established. To date, most studies have indicated that the second base of codon 12 is more heavily mutated in colorectal cancer than the first or the third bases. Therefore, it is conceivable that the type of K-ras mutation directly determines tumour behaviour.
In a study of 194 consecutive primary, recurrent, and metastatic colorectal adenocarcinomas, Finkelstein et al reported a significantly higher mutation rate of K-ras mutations in lymphogenous haematogenous metastatic disease.101 When colorectal carcinomas were analysed by specific K-ras mutation type, codon 13 mutated tumours did not progress locally or metastasise. Tumours with a codon 12 valine substitution did not metastasise beyond pericolonic perirectal lymph nodes. In contrast, codon 12 aspartic acid substitutions were common in cancers exhibiting distant deposits. No mutations were common in tumours with intraperitoneal deposits. On the basis of these data, Finkelstein et al proposed that genotyping of colorectal adenocarcinoma for K-ras status would identify subsets of patients likely to have indolent or aggressive forms of disease.101 Some, but not all, reports have supported the proposal that the possession of a K-ras mutation is independently associated with shorter survival.102–106 To clarify the association between K-ras mutations, patient outcome, and tumour characteristics a meta-analysis of data from 22 research groups (total number of cases 2721) was undertaken by Andreyev et al.107 Mutations were not associated with sex, age, site, or stage. Poorly differentiated tumours were less frequently mutated (p = 0.002). Multivariate analysis suggested that the presence of a mutation increased risk of recurrence (p < 0.001) and death (p = 0.004). In particular, any mutation of guanine to thymine but not to adenine or to cytosine increased the risk of recurrence (p = 0.006) and death (p < 0.001). When specific mutations were evaluated, only the codon 12 valine mutation was found to convey an independent, increased risk of recurrence (p = 0.007) and death (p = 0.004). The biological basis of a relation between a specific K-ras mutation and tumour behaviour is not straightforward. Early in vitro observations suggested that codon 12 K-ras mutations elicited stronger transformation responses than codon 13 K-ras changes in NIH/3T3 cell assays.108–110 However, this notion has not been supported by biochemical analyses of different ras proteins.111–113 On the basis of the available clinicopathological data, it is likely that patient survival is related to the occurrence of K-ras mutations, but not necessarily to the specific type of mutation.
DCC
If allele loss of chromosome 18q predicts a poor outcome in colorectal cancer, then the DCC gene must represent a prime candidate as the cause for this association. In a study of 132 patients with curatively resected stage II and III carcinomas, the expression of the DCC protein has been shown to be a strong positive predictive factor for survival.114 Patients with stage II disease whose tumours expressed DCC had a five year survival rate of 94%, compared with a survival rate of 62% for patients with DCC negative tumours. Similarly, in individuals with stage III disease, the respective survival rates were 59% and 33% in those with and without detectable DCC expression. This finding has been supported by a recently published small study of 23 patients.115
MISMATCH REPAIR GENES AND MICROSATELLITE INSTABILITY
Evidence directly correlating molecular and clinicopathological data for colorectal cancer has come from HNPCC. Colorectal cancers developing in carriers of HNPCC mutations are poorly differentiated and frequently multiple. Paradoxically, despite multiplicity and poor differentiation of cancers, early observations suggested that colorectal cancers in HNPCC carried a more favourable prognosis that in sporadic cases. Convincing evidence for improved survival in HNPCC is provided by studies from Finland116 and Japan.117
Whether MSI characterises a subset of sporadic colorectal cancers with a different prognosis has been evaluated in several studies. One of the early studies reported by Bubb et al in 1996 was based on a systematic analysis of 215 sporadic cases.118 Patients with MSI tumours had a significant survival advantage over those with MSS tumours, independent of other prognostic factors (HR = 0.39; 95% CI, 0.19 to 0.82). Several subsequent studies have reinforced this finding. In a study of 66 cases, Massa et al found that MSI status was independently associated with an improved prognosis (defined by overall survival and disease free survival).119 A large study based on 607 patients reported by Gryfe et al also found that MSI status conferred a significant survival advantage, independent of all standard prognostic factors, including tumour stage (HR = 0.42; 95% CI, 0.27 to 0.67).120 Regardless of the depth of tumour invasion, colorectal cancers with MSI had a decreased likelihood of metastasising to regional lymph nodes (HR = 0.33; 95% CI, 0.21 to 0.53) or distant organs (HR = 0.49; 95%, 0.29 to 0.89). A similar relation was seen between MSI status and prognosis in a study of 197 patients reported by Johannsdottir et al.121 Although MSI was not associated with clinicopathological parameters, such as Dukes's stage and tumour differentiation, this phenotype was associated with better overall survival. From an analysis of 225 colorectal cancer cases, Jernvall et al found that the five year survival rate in MSI cancers of the proximal colon was much better (100%) than that of those with MSS proximal disease (74%).122 However, an opposite effect was seen in relation to distal disease. In a study of a consecutive series of 388 Dukes's C colon carcinomas with five year median follow up reported by Elsaleh et al,123 the presence of MSI in the proximal transverse colon carcinoma group was associated with a significantly better prognosis (58% v 32%; p = 0.015). This was largely the result of the better survival seen in the MSI subgroup that received adjuvant chemotherapy, leading to the proposal that MSI status might determine the response to adjuvant chemotherapy. However, this seems unlikely to be the sole explanation of a better prognosis. Wright et al found MSI status conferred a significant survival advantage in patients who had not been in receipt of chemotherapy.124 Furthermore, Hemminki et al found that adjuvant 5-FU based chemotherapy is feasible both for patients with MSI and those with MSS.125 The three year recurrence free survivals were 90% and 43% in the MSI and MSS groups, respectively. Although most studies have found a relation between MSI status and prognosis some have not, including a report by Salahshor et al,126 based on a survival analysis at five to 10 years follow up of 181 unselected colorectal cases. Given that only approximately 15% of cancers display MSI, failure to demonstate a difference might be the result of a lack of power in this study.
Overall, the weight of evidence supports the tenant that although the genetic basis of HNPCC and sporadic cancers with MSI is different, tumours in the two groups share some biological characteristics in terms of prognosis. MSI in colorectal cancer appears to be an independent predictor of a relatively favourable outcome and, in addition, reduces the likelihood of metastases.
p53 AND p27
An increased intracellular concentration of p53, which is frequently but not systematically related to p53 mutation, has been proposed to be associated with poor prognosis in some tumour types. In colorectal cancer, although p53 overexpression in tumours correlates with chromosome 17p loss, hyperdiploid DNA content, and tumour site, there have been conflicting findings about its role as a prognostic indicator in studies based on immunohistochemistry.127–140 This reflects the fact that the degree of association between p53 mutations and protein expression depends in part on the specific antibody used. In studies of the relation between p53 mutations and prognosis, the situation is clearer. Studies suggest that colorectal cancers harbouring p53 mutations are more aggressive, are associated with a higher propensity for lymphatic and haematogenous spread, and have a worse prognosis.141–147 However, this is not universal.123
p27 is a member of the cip/kip family of cyclin dependent kinase inhibitors, which bind to cyclin:cyclin dependent kinase (cdk) complexes and block progression through the cell cycle. p27 regulates progression from G1 into S phase by binding to and inhibiting the cyclin E/Cdk2 complex, which is required for cells to enter S phase. In contrast to the p53 gene, mutations in p27 are rare. However, cell cycle regulation of p27 concentrations are regulated at the post transcriptional level through proteasome mediated degradation.148 Reduced expression of p27 was first shown to correlate with poor survival in a study of 149 patients reported by Loda et al.149 Patients whose tumours expressed p27 had a median survival of 151 months, whereas those that lacked p27 (10%) had a median survival of only 69 months. In the study, p27 expression was reported to be an independent prognostic marker and the risk of death associated with reduced expression was increased 2.9-fold. Subsequent studies have confirmed that p27 appears to have prognostic importance.150–152 Furthermore, decreased p27 expression has been associated with an increased likelihood of lymph node metastases in colon cancers, independent of depth of tumour invasion.151
Conclusions
The incidence of colorectal cancer is increasing and unfortunately the prognosis remains poor for most patients. The identification of those patients who are at a high risk of recurrent local and metastatic disease is important in selecting the appropriate treatment. Prognostic variables that have been found to have a significant effect include pathological stage and grade, type of tumour growth, chromosomal aneuploidy, and the presence of microinvasion. Until recently, there has been little understanding of the molecular basis of these indices. Despite the continuing use of histopathology as the “gold standard”, the genetic features of colorectal tumours will almost certainly become useful indicators of prognosis and of the most appropriate treatment. One of the problems with clinicomolecular associations reported to date has been that most studies have, for entirely understandable reasons, analysed only small numbers of tumours. Publication bias is a serious problem in assessing the usefulness of any given marker because positive associations have a far higher probability of being published than negative ones. Contradictory results between studies may reflect in part heterogeneity in colorectal cancers. It has been suggested that multiple biopsies and DNA sampling preceded by careful morphological examination must be standard if the preparation of DNA is required.153
Accepting these caveats, there is evidence that colorectal cancers harbouring defects in the MMR genes are associated with a better prognosis and those with chromosome anomalies, such as chromosome 18q or 17 deletions and mutations in K-ras and p53, with a worse prognosis. With the advent of methods for rapid genotyping it should be possible to construct mutation profiles of tumours and use multivariate analysis to determine which molecular features correlate with the clinicopathological data.
1st Asia Pacific Forum on Quality Improvement in Health Care.
Three day conference
Wednesday 19 to Friday 21 September 2001
Sydney, Australia
We are delighted to announce this forthcoming conference in Sydney. Authors are invited to submit papers (call for papers closes on Friday 6 April), and delegate enquiries are welcome.
The themes of the Forum are:
Improving patient safety
Leadership for improvement
Consumers driving change
Building capacity for change: measurement, education and human resources
The context: incentives and barriers for change
Improving health systems
The evidence and scientific basis for quality improvement.
Presented to you by the BMJ Publishing Group (London, UK) and Institute for Healthcare Improvement (Boston, USA), with the support of the the Commonwealth Department of Health and Aged Care (Australia), Safety and Quality Council (Australia), NSW Health (Australia), and Ministry of Health (New Zealand).
For more information contact: quality@bma.org.uk or fax +44 (0)20 7383 6869
References
- 1.Office of National Statistics. Cancer Statistics. Registrations. England and Wales. London: HMSO, 1989.
- 2.Office of National Statistics. Mortality statistics. Cause. England and Wales. London: HMSO, 1992.
- 3.Finlay IG, Pickford IR. Colorectal carcinoma. In: Lawson DH, ed. Current medicine, 4th ed. Edinburgh: Churchill Livingstone, 1994:51–64.
- 4.Beart RW, Steele GJ, Menck HR, et al. Management and survival of patients with adenocarcinoma of the colon and rectum: a national survey of the commission on cancer. J Am Coll Surg 1995;181:225–36. [PubMed] [Google Scholar]
- 5.Dukes CE, Bussey HJR. The spread of cancer and its effect on prognosis. Cancer 1958;12:309–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jass JR, Love SB, Northover JMA. A new prognostic classification of rectal cancer. Lancet 1987;ii:1303–6. [DOI] [PubMed] [Google Scholar]
- 7.Finlay IG, Meck D, Bruton F, et al. Growth rate of hepatic metastases in colorectal cancer. Br J Surg 1988;75:641–4. [DOI] [PubMed] [Google Scholar]
- 8.Morson B, Dawson I, Day D, et al. Morson and Dawson's gastrointestinal pathology, 3rd ed. Oxford: Blackwell Scientific Publications, 1997.
- 9.Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell 1990;61:759–67. [DOI] [PubMed] [Google Scholar]
- 10.Powell SM, Zilz N, Beazer Barclay Y, et al. APC mutations occur early during colorectal tumorigenesis. Nature 1992;359:235–7. [DOI] [PubMed] [Google Scholar]
- 11.Groden J, Thliveris A, Samowitz W, et al. Identification and characterization of the familial adenomatous polyposis coli gene. Cell 1991;66:589–600. [DOI] [PubMed] [Google Scholar]
- 12.Kinzler KW, Nilbert MC, Su LK, et al. Identification of FAP locus genes from chromosome 5q21. Science 1991;253:661–5. [DOI] [PubMed] [Google Scholar]
- 13.Miyoshi Y, Nagase H, Ando H, et al. Somatic mutations of the APC gene in colorectal tumors: mutation cluster region in the APC gene. Hum Mol Genet 1992;1:229–33. [DOI] [PubMed] [Google Scholar]
- 14.Solomon E, Voss R, Hall V, et al. Chromosome 5 allele loss in human colorectal carcinomas. Nature 1987;328:616–19. [DOI] [PubMed] [Google Scholar]
- 15.Miyaki M, Konishsi M, Kikuchi Yanoshita R, et al. Characteristics of somatic mutation of the adenomatous polyposis coli gene in colorectal tumours. Cancer Res 1994;54:3011–20. [PubMed] [Google Scholar]
- 16.Joslyn G, Richardson DS, White R, et al. Dimer formation by an N terminal coiled coil in the APC protein. Proc Natl Acad Sci U S A 1993;90:11109–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Baeg GH, Matsumine A, Kuroda T, et al. The tumour suppressor gene product APC blocks cell cycle progression from G0/G1 to S phase. EMBO J 1995;14:5618–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Su LK, Vogelstein B, Kinzler KW. Association of the APC tumor suppressor protein with catenins. Science 1993;262:1734–7. [DOI] [PubMed] [Google Scholar]
- 19.Rubinfeld B, Souza B, Albert I, et al. Association of the APC gene product with beta catenin. Science 1993;262:1731–4. [DOI] [PubMed] [Google Scholar]
- 20.Browne S, Williams A, Hague A, et al. Loss of apc protein expressed by human colonic epithelial cells and the appearance of a specific low molecular weight form is associated with apoptosis in vitro. Int J Cancer 1994;59:56–64. [DOI] [PubMed] [Google Scholar]
- 21.Burchill SA. The tumour suppressor APC product is associated with cell adhesion. Bioessays 1994;16:225–7. [DOI] [PubMed] [Google Scholar]
- 22.Munemitsu S, Souza B, Muller O, et al. The APC gene product associates with microtubules in vivo and promotes their assembly in vitro. Cancer Res 1994;54:3676–81. [PubMed] [Google Scholar]
- 23.Leach FS, Nicolaides NC, Papadopoulos N, et al. Mutations of a mutS homolog in hereditary nonpolyposis colorectal cancer. Cell 1993;75:1215–25. [DOI] [PubMed] [Google Scholar]
- 24.Fishel R, Lescoe MK, Rao MR, et al. The human mutator gene homolog MSH2 and its association with hereditary nonpolyposis colon cancer. Cell 1993;75:1027–38. [DOI] [PubMed] [Google Scholar]
- 25.Aaltonen LA, Peltomaki P, Leach FS, et al. Clues to the pathogenesis of familial colorectal cancer. Science 1993;260:812–16. [DOI] [PubMed] [Google Scholar]
- 26.Kolodner RD, Tytell JD, Schmeits JL, et al. Germ-line msh6 mutations in colorectal cancer families. Cancer Res 1999;59:5068–74. [PubMed] [Google Scholar]
- 27.Liu B, Nicolaides NC, Markowitz S, et al. Mismatch repair gene defects in sporadic colorectal cancers with microsatellite instability. Nat Genet 1995;9:48–55. [DOI] [PubMed] [Google Scholar]
- 28.Tomlinson IPM, Novelli MR, Bodmer WF. The mutation rate and cancer. Proc Natl Acad Sci U S A 1996;93:14800–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Connell WR, Talbot IC, Harpaz N, et al. Clinicopathological characteristics of colorectal carcinoma complicating ulcerative colitis. Gut 1994;35:1419–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ilyas M, Tomlinson IPM. Genetic pathways in colorectal cancer. Histopathology 1996;28:389–99. [DOI] [PubMed] [Google Scholar]
- 31.Redston M, Papadopoulos N, Caldas C, et al. Common occurrence of APC and K ras mutation in the spectrum of colitis associated neoplasias. Gastroenterology 1995;108:383–92. [DOI] [PubMed] [Google Scholar]
- 32.Tarmin L, Yin J, Harpaz N, et al. Adenomatous polyposis coli gene mutations in ulcerative colitis associated dysplasias and cancers versus sporadic colon neoplasms. Cancer Res 1995;55:2035–8. [PubMed] [Google Scholar]
- 33.Brentnall TA, Crispin DA, Rabinovitch PS, et al. Mutations in the p53 gene: an early marker of neoplastic progression in ulcerative colitis. Gastroenterology 1994;107:369–78. [DOI] [PubMed] [Google Scholar]
- 34.Tops CM, van der Klift HM, van der Luijt RB, et al. Non allelic heterogeneity of familial adenomatous polyposis. Am J Med Genet 1993;47:563–7. [DOI] [PubMed] [Google Scholar]
- 35.Whitelaw SC, Murday VA, Tomlinson IPM, et al. Clinical and molecular features of the hereditary mixed polyposis syndrome. Gastroenterology 1997;112:327–34. [DOI] [PubMed] [Google Scholar]
- 36.Hemminki A, Markie D, Tomlinson I, et al. A serine/threonine kinase gene defective in Peutz-Jeghers syndrome. Nature 1998;391:184–7. [DOI] [PubMed] [Google Scholar]
- 37.Howe JR, Roth S, Ringold JC, et al. Mutations in the SMAD4/DPC4 gene in juvenile polyposis. Science 1998;280:1086–8. [DOI] [PubMed] [Google Scholar]
- 38.Liaw D, Marsh DJ, Li J, et al. Germline mutations of the PTEN gene in Cowden disease, an inherited breast and thyroid cancer syndrome. Nat Genet 1997;16:64–7. [DOI] [PubMed] [Google Scholar]
- 39.Jeevarathnam P, Cottier DS, Browett PJ, et al. Familial giant hyperplastic polyposis predisposing to colorectal cancer a new hereditary bowel cancer syndrome. J Pathol 1996;179:20–5. [DOI] [PubMed] [Google Scholar]
- 40.Shepherd JA. Regression phenomenon in familial polyposis. Proc R Soc Med 1972;65:169. [PMC free article] [PubMed] [Google Scholar]
- 41.Giardello FM. Sulindac and polyp regression. Cancer Metastasis Rev 1994;13:279–83. [DOI] [PubMed] [Google Scholar]
- 42.Bos JL. The ras gene family and human carcinogenesis. Mutat Res 1988;195:255–71. [DOI] [PubMed] [Google Scholar]
- 43.Smith AJ, Stern HS, Penner M, et al. Somatic APC and K ras codon 12 mutations in aberrant crypt foci from human colons. Cancer Res 1994;54:5527–30. [PubMed] [Google Scholar]
- 44.Minamoto T, Yamashita N, Ochiai A, et al. Mutant K ras in apparently normal mucosa of colorectal cancer patients. Its potential as a biomarker of colorectal tumorigenesis. Cancer 1995;75(suppl 6):1520–6. [DOI] [PubMed] [Google Scholar]
- 45.Pretlow TP. Aberrant crypt foci and K ras mutations: earliest recognised players or innocent bystanders in colon carcinogenesis? Gastroenterology 1995;108:600–3. [DOI] [PubMed] [Google Scholar]
- 46.Bird RP. Role of aberrant crypt foci in understanding the pathogenesis of colon cancer. Cancer Lett 1995;93:55–71. [DOI] [PubMed] [Google Scholar]
- 47.Jen J, Kim H, Piantadosi S, et al. Allelic loss of chromosome 18q and prognosis in colorectal cancer. N Engl J Med 1994;331:213–21. [DOI] [PubMed] [Google Scholar]
- 48.Vogelstein BV, Fearon ER, Hamilton SR, et al. Genetic alterations during colorectal tumour development. N Engl J Med 1988;319:525–32. [DOI] [PubMed] [Google Scholar]
- 49.Kinzler KW, Nilbert MC, Vogelstein B, et al. Identification of a gene located at chromosome 5q21 that is mutated in colorectal cancers. Science 1991;251:1366–70. [DOI] [PubMed] [Google Scholar]
- 50.Curtis LJ, Bubb VJ, Gledhill S, et al. Loss of heterozygosity of MCC is not associated with mutation of the retained allele in sporadic colorectal cancer. Hum Mol Genet 1994;3:443–6. [DOI] [PubMed] [Google Scholar]
- 51.Hahn SA, Hoque AT, Moskaluk CA, et al. Homozygous deletion map at 18q21.1 in pancreatic cancer. Cancer Res 1996;56:490–4. [PubMed] [Google Scholar]
- 52.Lane DP. Cancer. p53, guardian of the genome. Nature 1992;358:15–16. [DOI] [PubMed] [Google Scholar]
- 53.Donehower LA, Bradley A. The tumor suppressor p53. Biochim Biophys Acta 1993;1155:181–205. [DOI] [PubMed] [Google Scholar]
- 54.Carder P, Wyllie AH, Purdie CA, et al. Stabilised p53 facilitates aneuploid clonal divergence in colorectal cancer. Oncogene 1993;8:1397–401. [PubMed] [Google Scholar]
- 55.Krawczak M, Smith SB, Schmidtke J, et al. Somatic spectrum of cancer associated single basepair substitutions in the p53 gene is determined mainly by endogenous mechanisms of mutation and by selection. Hum Mutat 1995;5:48–57. [DOI] [PubMed] [Google Scholar]
- 56.Baker SJ, Preisinger AC, Jessup JM, et al. p53 gene mutations occur in combination with 17p allelic deletions as late events in colorectal tumorigenesis. Cancer Res 1990;50:7717–22. [PubMed] [Google Scholar]
- 57.Cunningham J, Lust JA, Schaid DJ, et al. Expression of p53 and allelic loss in colorectal carcinoma. Cancer Res 1992;52:1974–80. [PubMed] [Google Scholar]
- 58.Kawasaki Y, Monden T, Morimoto H, et al. Immunohistochemical study of p53 expression in microwave fixed, paraffin embedded sections of colorectal carcinoma and adenoma. Am J Clin Pathol 1992;97:244–9. [DOI] [PubMed] [Google Scholar]
- 59.Ohta M, Inoue H, Cotticelli MG, et al. The FHIT gene, spanning the chromosome 3p14.2 fragile site and renal carcinoma associated t(3 ,8) breakpoint, is abnormal in digestive tract cancers. Cell 1996;84:587–97. [DOI] [PubMed] [Google Scholar]
- 60.Okamoto A, Demetrick DJ, Spillare EA, et al. Mutations and altered expression of p16INK4 in human cancer. Proc Natl Acad Sci U S A 1994;91:11045–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Herman JG, Merlo A, Mao L, et al. Inactivation of the CDKN2/p16/MTS1 gene is frequently associated with aberrant DNA methylation in all common human cancers. Cancer Res 1995;55:4525–30. [PubMed] [Google Scholar]
- 62.Gonzalez ZM, Bender CM, Yang AS, et al. Methylation of the 5′CpG island of the p16/CDKN2 tumor suppressor gene in normal and transformed human tissues correlates with gene silencing. Cancer Res 1995;55:4531–5. [PubMed] [Google Scholar]
- 63.Leister I, Weith A, Bruderlein S, et al. Human colorectal cancer: high frequency of deletions at chromosome 1p35. Cancer Res 1990;50:7232–5. [PubMed] [Google Scholar]
- 64.Praml C, Finke LH, Herfarth C, et al. Deletion mapping defines different regions in 1p34.2 pter that may harbor genetic information related to human colorectal cancer. Oncogene 1995;11:1357–62. [PubMed] [Google Scholar]
- 65.Wildrick D, Alfaro S, Gope R, et al. A study of chromosome 6 allele loss in human colorectal carcinomas. Anticancer Res 1992;12:1717–19. [PubMed] [Google Scholar]
- 66.Fujiwara Y, Emi M, Ohata H, et al. Evidence for the presence of two tumor suppressor genes on chromosome 8p for colorectal carcinoma. Cancer Res 1993;53:1172–4. [PubMed] [Google Scholar]
- 67.Cunningham C, Dunlop MG, Wyllie AH, et al. Deletion mapping in colorectal cancer of a putative tumour suppressor gene in 8p22 p21.3. Oncogene 1993;8:1391–6. [PubMed] [Google Scholar]
- 68.Young J, Leggett B, Ward M, et al. Frequent loss of heterozygosity on chromosome 14 occurs in advanced colorectal carcinomas. Oncogene 1993;8:671–5. [PubMed] [Google Scholar]
- 69.Yana I, Kurahashi H, Nakamori S, et al. Frequent loss of heterozygosity at telomeric loci on 22q in sporadic colorectal cancers. Int J Cancer 1995;60:174–7. [DOI] [PubMed] [Google Scholar]
- 70.Liu B, Parsons R, Papadopoulos N, et al. Analysis of mismatch repair genes in hereditary non polyposis colorectal cancer patients. Nat Med 1996;2:169–74. [DOI] [PubMed] [Google Scholar]
- 71.Kim H, Jen J, Vogelstein B, et al. Clinical and pathological characteristics of sporadic colorectal carcinomas with DNA replication errors in microsatellite sequences. Am J Pathol 1994;145:148–56. [PMC free article] [PubMed] [Google Scholar]
- 72.Young J, Leggett B, Gustafson C, et al. Genomic instability occurs in colorectal carcinomas but not in adenomas. Hum Mutat 1993;2:351–4. [DOI] [PubMed] [Google Scholar]
- 73.Ilyas M, Tomlinson IPM, Novelli MR, et al. Clinico pathological features and p53 expression in left sided sporadic colorectal cancers with and without microsatellite instability. J Pathol 1996;179:370–5. [DOI] [PubMed] [Google Scholar]
- 74.da Costa LT, Liu B, El Deiry WS, et al. Polymerase and variants in RER colorectal tumours. Nat Genet 1995;9:10–11. [DOI] [PubMed] [Google Scholar]
- 75.Linn SC, Giaccone G. MDR1/P glycoprotein expression in colorectal cancer. Eur J Cancer 1995;31A:1291–4. [DOI] [PubMed] [Google Scholar]
- 76.Nuovo GJ. In situ PCR: protocols and applications. PCR Methods Appl 1995;4:S151–67. [DOI] [PubMed] [Google Scholar]
- 77.Pignatelli M, Liu D, Nasim MM, et al. Morphoregulatory activities of E cadherin and beta 1 integrins in colorectal tumour cells. Br J Cancer 1992;66:629–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.De Bruin PAF, Griffioen G, Verspaget HW, et al. Plasminogen activator profiles in neoplastic tissues of the human colon. Cancer Res 1988;48:4520–4. [PubMed] [Google Scholar]
- 79.Sier CFM, Vloedgraven HJM, Griffioen G, et al. Plasminogen activators and inhibitor type 1 in neoplastic colonic tissue from patients with familial adenomatous polyposis. Br J Cancer 1995;71:393–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.MacDonald NJ, de la Rosa A, Steeg PS. The potential roles of nm23 in cancer metastasis and cellular differentiation. Eur J Cancer 1995;31A:1096–100. [DOI] [PubMed] [Google Scholar]
- 81.Martinez JA, Prevot S, Nordlinger B, et al. Overexpression of nm23 H1 and nm23 H2 genes in colorectal carcinomas and loss of nm23 H1 expression in advanced tumour stages. Gut 1995;37:712–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Iacopetta B, DiGrandi S, Dix B, et al. Loss of heterozygosity of tumour suppressor gene loci in human colorectal carcinoma. Eur J Cancer 1994;30A:664–70. [DOI] [PubMed] [Google Scholar]
- 83.Cawkwell L, Lewis FA, Quirke P. Frequency of allele loss of DCC, p53, RBI, WT1, NF1, NM23 and APC/MCC in colorectal cancer assayed by fluorescent multiplex polymerase chain reaction. Br J Cancer 1994;70:813–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Campo E, Miquel R, Jares P, et al. Prognostic significance of the loss of heterozygosity of nm23 h1 and p53 genes in human colorectal carcinomas. Cancer 1994;73:2913–21. [DOI] [PubMed] [Google Scholar]
- 85.Ichikawa W. Positive relationship between expression of CD44 and hepatic metastases in colorectal cancer. Pathobiology 1994;62:172–9. [DOI] [PubMed] [Google Scholar]
- 86.Vogelstein B, Fearon ER, Kern SE, et al. Allelotype of colorectal carcinomas. Science 1989;244:207–11. [DOI] [PubMed] [Google Scholar]
- 87.Gerdes H, Chen Q, Elahi AH, et al. Recurrent deletions involving chromosomes 1, 5, 17, and 18 in colorectal carcinoma: possible role in biological and clinical behavior of tumors. Anticancer Res 1995;15:13–24. [PubMed] [Google Scholar]
- 88.Laurent-Puig P, Olschwang S, Delattre O, et al. Survival and acquired genetic alterations in colorectal cancer. Gastroenterology 1992;102:1136–41. [PubMed] [Google Scholar]
- 89.Cohn KH, Ornstein DL, Wang F, et al. The significance of allelic deletions and aneuploidy in colorectal carcinoma. Results of a 5 year follow up study. Cancer 1997;79:233–44. [PubMed] [Google Scholar]
- 90.Kern SE, Fearon ER, Tersmette KW, et al. JAMA 1989;261:3099–103. [DOI] [PubMed] [Google Scholar]
- 91.Ogunbiyi OA, Goodfellow PJ, Herfarth K, et al. Confirmation that chromosome 18q allelic loss in colon cancer is a prognostic indicator. J Clin Oncol 1998;16:427–33. [DOI] [PubMed] [Google Scholar]
- 92.Carethers JM, Hawn MT, Greenson JK, et al. Prognostic significance of allelic lost at chromosome 18q21 for stage II colorectal cancer. Gastroenterology 1998;114:1188–95. [DOI] [PubMed] [Google Scholar]
- 93.Martinez-Lopez E, Abad A, Font A, et al. Allelic loss on chromosome 18q as a prognostic marker in stage II colorectal cancer. Gastroenterology 1998;114:1180–7. [DOI] [PubMed] [Google Scholar]
- 94.Khine K, Smith DR, Goh HS. High frequency of allelic deletion on chromosome 17p in advanced colorectal cancer. Cancer 1994;73:28–35. [DOI] [PubMed] [Google Scholar]
- 95.Purdie CA, Piris J, Bird CC, et al. 17q allele loss is associated with lymph node metastasis in locally aggressive human colorectal cancer. J Pathol 1995;175:297–302. [DOI] [PubMed] [Google Scholar]
- 96.Berney CR, Fisher RJ, Yang J, et al. Genomic alterations (LOH, MI) on chromosome 17q21–23 and prognosis of sporadic colorectal cancer. Int J Cancer 2000;89:1–5. [DOI] [PubMed] [Google Scholar]
- 97.Kelemen PR, Yaremko ML, Kim AH, et al. Loss of heterozygosity in 8p is associated with microinvasion in colorectal carcinoma. Genes Chromosomes Cancer 1994;11:195–8. [DOI] [PubMed] [Google Scholar]
- 98.Ogunbiyi OA, Goodfellow PJ, Gagliardi G, et al. Prognostic value of chromosome 1p allelic loss in colon cancer. Gastroenterology 1997;113:761–6. [DOI] [PubMed] [Google Scholar]
- 99.Gustafson CE, Young J, Leggett B, et al. Loss of heterozygosity on the long arm of chromosome 11 in colorectal tumours. Br J Cancer 1994;70:395–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Arribas R, Ribas M, Risques RA, et al. Prospective assessment of allelic losses at 4p14–16 in colorectal cancer: two mutational patterns and a locus associated with poorer survival. Clin Cancer Res 1999;5:3454–9. [PubMed] [Google Scholar]
- 101.Finkelstein SD, Sayegh R, Christensen S, et al. Genotypic classification of colorectal adenocarcinoma. Biologic behavior correlates with K ras 2 mutation type. Cancer 1993;71:3827–38. [DOI] [PubMed] [Google Scholar]
- 102.Moerkerk P, Arends JW, van Driel M, et al. Type and number of Ki ras point mutations relate to stage of human colorectal cancer. Cancer Res 1994;54:3376–8. [PubMed] [Google Scholar]
- 103.Span M, Moerkerk PT, De Goeij AF, et al. A detailed analysis of K ras point mutations in relation to tumor progression and survival in colorectal cancer patients. Int J Cancer 1996;69:241–5. [DOI] [PubMed] [Google Scholar]
- 104.Kastrinakis WV, Ramchurren N, Maggard M, et al. K ras status does not predict successful hepatic resection of colorectal cancer metastasis. Arch Surg 1995;130:9–14. [DOI] [PubMed] [Google Scholar]
- 105.Benhattar J, Losi L, Chaubert P, et al. Prognostic significance of K ras mutations in colorectal carcinoma. Gastroenterology 1993;104:1044–8. [DOI] [PubMed] [Google Scholar]
- 106.Pricolo VE, Finkelstein SD, Wu TT , et al. Prognostic value of p53 and K ras 2 mutational analysis in stage III carcinoma of the colon. Am J Surg 1996;171:41–6. [DOI] [PubMed] [Google Scholar]
- 107.Andreyev HJ, Norman AR, Cunningham D, et al. Kirsten ras mutations in patients with colorectal cancer: the multicenter “RASCAL” study. J Natl Cancer Inst 1998;90:675–84. [DOI] [PubMed] [Google Scholar]
- 108.Seeburg PH, Colby WW, Capon DJ, et al. Biological properties of human c Ha ras1 genes mutated at codon 12. Nature 1984;312:71–5. [DOI] [PubMed] [Google Scholar]
- 109.Bos JL, Toksoz D, Marshall CJ, et al. Amino acid substitutions at codon 13 of the N ras oncogene in human acute myeloid leukaemia. Nature 1985;315:726–30. [DOI] [PubMed] [Google Scholar]
- 110.Fasano O, Aldrich T, Tamanoi F, et al. Analysis of the transforming potential of the human H ras gene by random mutagenesis. Proc Natl Acad Sci U S A 1984;81:4008–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Manne V, Bekesi E, Kung HF. Ha ras proteins exhibit GTPase activity: point mutations that activate Ha ras gene products result in decreased GTPase activity. Proc Natl Acad Sci U S A 1985;82:376–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Der CJ, Finkel T, Cooper GM. Biological and biochemical properties of human rasH genes mutated at codon 61. Cell 1986;44:167–76. [DOI] [PubMed] [Google Scholar]
- 113.McGrath JP, Capon DJ, Goeddel DV, et al. Comparative biochemical properties of normal and activated human ras p21 protein. Nature 1984;310:644–9. [DOI] [PubMed] [Google Scholar]
- 114.Shibata D, Reale MA, Lavin P, et al. The DCC protein and prognosis in colorectal cancer. N Engl J Med 1996;335:1727–32. [DOI] [PubMed] [Google Scholar]
- 115.Saito M, Yamaguchi A, Goi T, et al. Expression of DCC protein in colorectal tumors and its relationship to tumor progression and metastasis. Oncology 1999;56:134–41. [DOI] [PubMed] [Google Scholar]
- 116.Sankila R, Aaltonen LA, Jarvinen HJ, et al. Better survival rates in patients with MLH1-associated hereditary colorectal cancer. Gastroenterology 1996;110:682–7. [DOI] [PubMed] [Google Scholar]
- 117.Fujita S, Moriya Y, Sugihara K, et al. Prognosis of hereditary nonpolyposis colorectal cancer (HNPCC) and the role of Japanese criteria for HNPCC. Jpn J Clin Oncol 1996;26:351–5. [DOI] [PubMed] [Google Scholar]
- 118.Bubb VJ, Curtis LJ, Cunningham C, et al. Microsatellite instability and the role of hMSH2 in sporadic colorectal cancer. Oncogene 1996;12:2641–9. [PubMed] [Google Scholar]
- 119.Massa MJ, Iniesta P, Gonzalez-Quevedo R, et al. Differential prognosis of replication error phenotype and loss of heterozygosity in sporadic colorectal cancer. Eur J Cancer 1999;35:1676–82. [DOI] [PubMed] [Google Scholar]
- 120.Gryfe R, Kim H, Hsieh ET, et al. Tumor microsatellite instability and clinical outcome in young patients with colorectal cancer. N Engl J Med 2000;342:69–77. [DOI] [PubMed] [Google Scholar]
- 121.Johannsdottir JT, Bergthorsson JT, Gretarsdottir S, et al. Replication error in colorectal carcinoma: association with loss of heterozygosity at mismatch repair loci and clinicopathological variables. Anticancer Res 1999;19:1821–6. [PubMed] [Google Scholar]
- 122.Jernvall P, Makinen MJ, Karttunen TJ, et al. Microsatellite instability: impact on cancer progression in proximal and distal colorectal cancers. Eur J Cancer 1999;35:197–201. [DOI] [PubMed] [Google Scholar]
- 123.Elsaleh H, Powell B, Soontrapornchai P, et al. p53 gene mutation, microsatellite instability and adjuvant chemotherapy: impact on survival of 388 patients with Dukes' C colon carcinoma. Oncology 2000;58:52–9. [DOI] [PubMed] [Google Scholar]
- 124.Wright CM, Dent OF, Barker M, et al. Prognostic significance of extensive microsatellite instability in sporadic clinicopathological stage C colorectal cancer. Br J Surg 2000;87:1197–202. [DOI] [PubMed] [Google Scholar]
- 125.Hemminki A, Mecklin JP, Jarvinen H, et al. Microsatellite instability is a favorable prognostic indicator in patients with colorectal cancer receiving chemotherapy. Gastroenterology 2000;119:921–8. [DOI] [PubMed] [Google Scholar]
- 126.Salahshor S, Kressner U, Fischer H, et al. Microsatellite instability in sporadic colorectal cancer is not an independent prognostic factor. Br J Cancer 1999;81:190–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Remvikos Y, Tominaga O, Hammel P, et al. Increased p53 protein content of colorectal tumours correlates with poor survival. Br J Cancer 1992;66:758–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Kressner U, Lindmark G, Gerdin B, et al. Immunohistological p53 staining is of limited value in the staging and prognostic prediction of colorectal cancer. Anticancer Res 1996;16:951–7. [PubMed] [Google Scholar]
- 129.Diez M, Enriquez JM, Camunas J, et al. Prediction of recurrence in B C stages of colorectal cancer by p53 nuclear overexpression in comparison with standard pathological features. Eur J Surg Oncol 1995;21:635–9. [DOI] [PubMed] [Google Scholar]
- 130.Grewal H, Guillem JG, Klimstra DS, et al. p53 nuclear overexpression may not be an independent prognostic marker in early colorectal cancer. Dis Colon Rectum 1995;38:1176–81. [DOI] [PubMed] [Google Scholar]
- 131.Lazaris AC, Theodoropoulos GE, Anastassopoulos P, et al. Prognostic significance of p53 and c erbB 2 immunohistochemical evaluation in colorectal adenocarcinoma. Histol Histopathol 1995;3:661–8. [PubMed] [Google Scholar]
- 132.Houbiers JG, van der Burg SH, van de Watering LM, et al. Antibodies against p53 are associated with poor prognosis of colorectal cancer. Br J Cancer 1995;72:637–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Tomoda H , Kakeji Y. Immunohistochemical analysis of p53 in colorectal cancer regarding clinicopathological correlation and prognostic significance. J Surg Oncol 1995;58:125–8. [DOI] [PubMed] [Google Scholar]
- 134.Morrin M, Kelly M, Barrett N, et al. Mutations of Ki ras and p53 genes in colorectal cancer and their prognostic significance. Gut 1994;35:1627–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Zeng ZS, Sarkis AS , Zhang ZF, et al. p53 nuclear overexpression: an independent predictor of survival in lymph node positive colorectal cancer patients. J Clin Oncol 1994;12:2043–50. [DOI] [PubMed] [Google Scholar]
- 136.Tanaka M, Omura K, Watanabe Y, et al. Prognostic factors of colorectal cancer: K ras mutation, overexpression of the p53 protein, and cell proliferative activity. J Surg Oncol 1994;57:57–64. [DOI] [PubMed] [Google Scholar]
- 137.Suzuki H, Matsumoto K, Koide A, et al. Correlation of p53 with the clinicopathologic features and prognosis of colorectal adenocarcinoma. Surg Today 1994;24:85–7. [DOI] [PubMed] [Google Scholar]
- 138.Nathanson SD, Linden MD, Tender P, et al. Relationship among p53, stage, and prognosis of large bowel cancer. Dis Colon Rectum 1994;37:527–34. [DOI] [PubMed] [Google Scholar]
- 139.Bell SM, Scott N, Cross D, Sagar P, et al. Prognostic value of p53 overexpression and c Ki ras gene mutations in colorectal cancer. Gastroenterology 1993;104:57–64. [DOI] [PubMed] [Google Scholar]
- 140.Yamaguchi A, Kurosaka Y, Fushida S, et al. Expression of p53 protein in colorectal cancer and its relationship to short term prognosis. Cancer 1992;70:2778–84. [DOI] [PubMed] [Google Scholar]
- 141.Goh HS, Yao J, Smith DR. p53 point mutation and survival in colorectal cancer patients. Cancer Res 1995;55:5217–21. [PubMed] [Google Scholar]
- 142.Hamelin R, Laurent Puig P, Olschwang S, et al. Association of p53 mutations with short survival in colorectal cancer. Gastroenterology 1994;106:42–8. [DOI] [PubMed] [Google Scholar]
- 143.Bertorelle R, Esposito G, Del Mistro A, et al. Association of p53 gene and protein alterations with metastases in colorectal cancer. Am J Surg Pathol 1995;19:463–71. [DOI] [PubMed] [Google Scholar]
- 144.Kastrinakis WV, Ramchurren N, Rieger KM, et al. Increased incidence of p53 mutations is associated with hepatic metastasis in colorectal neoplastic progression. Oncogene 1995;11:647–52. [PubMed] [Google Scholar]
- 145.Goh HS, Chan CS, Khine K, et al. p53 and behaviour of colorectal cancer. Lancet 1994;344:233–4. [DOI] [PubMed] [Google Scholar]
- 146.Bosari S, Viale G, Roncalli M, et al. p53 gene mutations, p53 protein accumulation and compartmentalization in colorectal adenocarcinoma. Am J Pathol 1995;147:790–8. [PMC free article] [PubMed] [Google Scholar]
- 147.Smith DR, Ji CY, Goh HS. Prognostic significance of p53 overexpression and mutation in colorectal adenocarcinomas. Br J Cancer 1996;74:216–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Steeg PS, Abrams JS. Cancer prognostics: past, present and p27. Nat Med 1997;3:152–4. [DOI] [PubMed] [Google Scholar]
- 149.Loda M, Cukor B, Tam SW, et al. Increased proteasome dependent degradation of the cyclin dependent kinase inhibitor p27 in aggressive colorectal carcinomas. Nat Med 1997;3:231–4. [DOI] [PubMed] [Google Scholar]
- 150.Tenjo T, Toyoda M, Okuda J, et al. Prognostic significance of p27 (kip1) protein expression and spontaneous apoptosis in patients with colorectal adenocarcinomas. Oncology 2000;58:45–51. [DOI] [PubMed] [Google Scholar]
- 151.Liu DF, Ferguson K, Cooper GS, et al. p27 cell-cycle inhibitor is inversely correlated with lymph node metastases in right-sided colon cancer. J Clin Lab Anal 1999;13:291–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Palmqvist R, Stenling R, Oberg A, et al. Prognostic significance of p27 (Kip1) expression in colorectal cancer: a clinico-pathological characterization. J Pathol 1999;188:18–23. [DOI] [PubMed] [Google Scholar]
- 153.Lindforss U, Fredholm H, Papadogiannakis N, et al. Allelic loss is heterogeneous throughout the tumor in colorectal carcinoma. Cancer 2000;88:2661–7. [PubMed] [Google Scholar]