Abstract
Dysregulation of the cell cycle machinery, particularly the overactivation of cyclin-dependent kinases 4 and 6 (CDK4/6), is a hallmark of breast cancer pathogenesis. The introduction of CDK4/6 inhibitors has transformed the treatment landscape for hormone receptor-positive breast cancer by effectively targeting abnormal cell cycle progression. However, despite their initial clinical success, drug resistance remains a significant challenge, with no reliable biomarkers available to predict treatment response or guide strategies for managing resistant populations. Consequently, numerous studies have sought to investigate the mechanisms driving resistance to optimize the therapeutic use of CDK4/6 inhibitors and improve patient outcomes. Here we examine the molecular mechanisms regulating the cell cycle, current clinical applications of CDK4/6 inhibitors in breast cancer, and key mechanisms contributing to drug resistance. Furthermore, we discuss emerging predictive biomarkers and highlight potential directions for overcoming resistance and enhancing therapeutic efficacy.
Subject terms: Breast cancer, Checkpoints
Targeting cell cycle dysregulation to combat breast cancer
CDK4/6 inhibitors have revolutionized the treatment of hormone receptor-positive breast cancer by targeting abnormal cell growth. However, most patients eventually encounter drug resistance, and predicting responses remains a challenge. This Review delves into the mechanisms behind CDK4/6 inhibitor resistance and explores potential strategies to overcome it. The authors provide a comprehensive overview of the cell cycle and the role of CDK4/6 inhibitors, highlighting both genetic and nongenetic factors that drive resistance. Key insights reveal that mutations and alterations in signaling pathways significantly contribute to drug resistance, offering avenues for novel therapeutic targets. Moreover, the Review emphasizes the importance of biomarkers to better predict treatment outcomes. Understanding these resistance mechanisms is pivotal for developing advanced strategies to enhance therapy effectiveness and improve patient prognosis.
This summary was initially drafted using artificial intelligence, then revised and fact-checked by the author.
Introduction
Breast cancer is one of the most common cancers worldwide and a leading cause of cancer-related mortality among women1. Despite notable progress in early detection and treatment, resistance to conventional therapies remains a major challenge, underscoring the need for innovative therapeutic approaches. Targeting the cell cycle—a fundamental process that controls cell proliferation—presents a promising strategy in cancer treatment2. Dysregulation of the cell cycle is a hallmark of cancer, driving uncontrolled cell division and tumor growth3.
The cell cycle comprises a series of tightly regulated phases, ensuring the orderly progression of cells through growth, DNA replication and division4. Critical regulators of this process include cyclins, cyclin-dependent kinases (CDKs), CDK-inhibitor proteins and the retinoblastoma protein (Rb), which cooperatively control the transition between different cell cycle phases4,5. Alterations in these regulatory molecules can lead to aberrant cell proliferation in cancer. Overexpression of cyclin D is observed in 50–60% of breast cancer cases, indicating CDK4/6 overactivation6. Furthermore, cyclin E overexpression, CDK4/6 amplification and loss-of-function (LOF) mutations in tumor suppressor genes, such as p53, are frequently found in breast cancer and induce abnormal cell cycle progression7.
Breast cancer is classified on the basis of the expression of the following receptors: hormone receptors (HR: estrogen and progesterone receptors) and human epidermal growth factor receptor 2 (HER2). CDK4/6 inhibitors have emerged as promising therapeutic agents in HR-positive (HR+)/HER2-negative (HER2−) breast cancer. These inhibitors selectively target CDK4/6 to prevent Rb phosphorylation in the G1 phase, thereby blocking the G1/S transition8. Clinical trials have demonstrated that the addition of CDK4/6 inhibitors to endocrine therapy significantly improves progression-free survival (PFS) in patients with metastatic HR+/HER2− breast cancer9–12. However, despite their success, developing resistance to CDK4/6 inhibitors poses a significant challenge, promoting research into understanding resistance mechanisms and identifying new therapeutic targets.
Here, we discuss the molecular mechanisms underlying cell cycle regulation and resistance to CDK4/6 inhibitors in breast cancer. We also explore potential predictive biomarkers and therapeutic strategies to overcome drug resistance, providing an overview of current directions for targeting the cell cycle in breast cancer therapy.
Mechanisms of cell cycle entry
Entry into the cell cycle is tightly regulated to ensure cells advance to the S phase when all requisite conditions are satisfied13. Rb binds and sequesters E2F transcription factors during quiescence to prevent their activity and premature cell cycle entry14. In the canonical pathway, mitogenic stimulation induces cyclin D expression, which binds and activates CDK4/6, forming the active cyclin D–CDK4/6 complex15,16. Active CDK4/6 phosphorylates Rb, leading to the effective release of E2F transcription factors. The Rb-related pocket proteins Rbl1 (p107) and Rbl2 (p130), which recruit chromatin repressor complexes, are also substrates of CDK4/617. Released E2Fs initiate the transcription of genes involved in S-phase entry, including the CDK2 activators cyclins E and A17,18. The activation of CDK2 further phosphorylates Rb and various substrates necessary for DNA synthesis and replication, thereby driving S-phase entry19,20. Moreover, E2Fs regulate the expression of genes involved in nucleotide biosynthesis, such as DHFR, RRM1 and RRM2, and mitotic progression, including PLK1, BUB1 and MAD217,18.
In addition to cyclin binding, the full activation of CDK4/6 requires the phosphorylation of its T-loop by CDK-activating kinase (CAK)21–23. CAKs consist of CDK7, cyclin H and the assembly factor MAT1. The phosphorylation of the T-loop displaces it from the active site, allowing the formation of a functional cyclin–CDK–substrate complex. CAK also phosphorylates RNA polymerase II to regulate mRNA transcription, linking cell cycle regulation with transcriptional control24.
Several regulatory mechanisms suppress CDK4/6 activity under various conditions, such as contact inhibition, activation of the p53/p21 pathway, limited availability of mitogens, and expression of CDK inhibitor proteins25. The INK4 family of CDK4/6 inhibitors (p16, p15, p18 and p19) bind to the catalytic pocket of CDK4/6, competing with cyclin D and blocking CDK4/6 kinase activity26. Cyclin D is inherently unstable and undergoes phosphorylation at the end of the G1 phase, which enables its export to the cytoplasm via CRM127. In addition, recent genome-wide screening studies have identified autophagy and beclin 1 regulator 1 (AMBRA1) as an E3 ligase adaptor that regulates cyclin D levels through ubiquitylation and proteasomal degradation28–30. Cip/Kip family proteins (p21, p27 and p57) bind and inhibit active cyclin–CDK complexes, suppressing cell cycle progression31. However, previous studies have shown that these proteins can stabilize cyclin D–CDK4/6 complexes and facilitate their nuclear translocation26,32,33. Whereas Cip/Kip family proteins typically inactivate CDK4/634–36, phosphorylated p27 has been shown to activate CDK4/6 by dislodging itself from the CDK active site36,37. Nevertheless, other studies have demonstrated CDK4/6 activation in mouse embryonic fibroblasts lacking p21 and p27, as well as in nontransformed cell lines lacking p21, p27 and p5738,39, indicating the need for further investigation into the biological significance of p27 phosphorylation.
While CDK4/6 plays a central role in cell cycle entry through Rb phosphorylation, several studies have shown that cells can progress through the cell cycle in the absence of CDK4/6 activity. Early reports demonstrated cell proliferation in mice lacking all cyclin D1–3 isoforms or CDK4/640,41 and the initiation of DNA replication without CDK4/6 activity and Rb phosphorylation42. One possible mechanism is the dilution of the Rb concentration due to cell growth, which contributes to CDK4/6-independent Rb inactivation43. In addition, recent findings have indicated that nonphosphorylated Rb is intrinsically unstable, leading to reduced protein levels44. However, this passive Rb inactivation is insufficient for full E2F activation, necessitating a secondary amplification step. This amplification is driven primarily by the global transcriptional enhancer c-Myc, which is upregulated by mitogenic and hormone signaling45,46. Importantly, while c-Myc overexpression induces cyclin D expression to activate CDK4/6, it amplifies E2F activity following Rb reduction under CDK4/6 inhibition44. Other studies have also shown that c-Myc overexpression facilitates CDK2 activation, promoting cell cycle entry through a noncanonical pathway42,47. Several E3 ubiquitin ligases, including NRBE3, SETDB1, β-TRCP1 and UBR5, have been identified as mediators of Rb degradation48–51. By contrast, other studies failed to detect ubiquitination-dependent Rb degradation52–54; instead, they suggested that MDM252 and TTC39B53 promote Rb degradation through ubiquitination-independent, proteasome-driven mechanisms.
This comprehensive understanding of both the canonical and noncanonical pathways of cell cycle entry highlights the complex regulatory networks involved in cell proliferation, suggesting potential therapeutic targets and strategies for treating cancers characterized by cell cycle dysregulation.
Role of CDK4/6 inhibitors in breast cancer therapy
Over two decades ago, the first generation of CDK inhibitors, often called pan-CDK inhibitors, was developed as potential cancer therapeutics. However, the lack of selectivity led to significant toxicity and failure in clinical trials55. A breakthrough came with the development of selective CDK4/6 inhibitors, which have demonstrated efficacy in human luminal/estrogen receptor-positive cancer cells, suggesting their potential utility in breast cancer treatment56. Unlike first-generation inhibitors, these small molecules exhibit increased selectivity toward CDK4/6 and reduced toxicity57. CDK4/6 inhibition blocks cell cycle progression in the G1 phase and induces cellular senescence. HR+/HER2− breast cancer, which typically retains Rb function and activates the cyclin D–CDK4/6 pathway via estrogen signaling, has the highest sensitivity to CDK4/6 inhibition55. The promising efficacy of these inhibitors led to a series of clinical trials and subsequent Food and Drug Administration (FDA) approval of three CDK4/6 inhibitors—palbociclib (Ibrance), ribociclib (Kisqali) and abemaciclib (Verzenio)—for the treatment of HR+/HER2− metastatic breast cancer in combination with endocrine therapy. Several clinical trials, including MONARCH-3, PALOMA-1, PALOMA-2, MONALEESA-2 and MONALEESA-7, have evaluated the efficacy of these inhibitors in combination with endocrine therapy as a first-line treatment, demonstrating significant improvements in PFS compared with endocrine monotherapy58–62. Unlike palbociclib and ribociclib, abemaciclib has been approved as monotherapy owing to its additional off-target effects63. These promising results led to the combination of CDK4/6 inhibitors and endocrine therapy as standard therapy for HR+/HER2− metastatic breast cancer.
Recently, the China FDA approved dalpiciclib (Herngri) for the treatment of HR+/HER2− metastatic breast cancer64. The DAWNA-2 trial, which evaluated the efficacy of dalpiciclib in combination with endocrine therapy as a first-line treatment, reported a median PFS exceeding 30 months and a 49% reduction in the risk of disease progression65. Compared with endocrine monotherapy, the PALOMA-3, MONARCH-2 and MONALEESA-3 trials assessed CDK4/6 inhibitors in combination with endocrine therapy in endocrine therapy-resistant populations and demonstrated significant improvements in median PFS and objective response rates10,12,59. However, the impact on overall survival (OS) varied across these trials, with MONARCH-2 and MONALEESA-3 showing significant improvement in OS, whereas PALOMA-3 displayed a trend toward improvement in OS that did not reach statistical significance66.
The clinical success of CDK4/6 inhibitors in HR+/HER2− metastatic breast cancer has led to a significant expansion in their application, with over 100 clinical trials investigating CDK4/6 inhibitors in combination with chemotherapy, immunotherapy or other targeted therapies across different breast cancer subtypes and other tumor types (Table 1)67. For example, in HR+/HER2+ breast cancer, the HER2 signaling pathway enhances CDK4/6 activity, making CDK4/6 an ideal therapeutic target66. Six ongoing trials are exploring approved CDK4/6 inhibitors combined with endocrine therapy and/or anti-HER2 therapy for HR+/HER2+ metastatic breast cancer, with PFS or OS as the primary endpoint (NCT03304080, NCT02947685, NCT05969184, NCT03772353, NCT05800756 and NCT04334330). For triple-negative breast cancer (TNBC), four ongoing clinical trials are evaluating FDA-approved CDK4/6 inhibitors as monotherapies (NCT03979508) in combination with anti-androgen receptor (AR) therapy in AR-positive (AR+) populations (NCT02605486 and NCT03090165) or with a histone deacetylase (HDAC) inhibitor (NCT04315233). However, owing to the heterogeneous nature of TNBC, findings from different in vitro studies have been controversial, with some reporting insensitivity to CDK4/6 inhibition. By contrast, others, particularly in AR+ cell lines, have shown sensitivity68. In early-stage HR+ breast cancer, CDK4/6 inhibitors are being investigated for their potential use. Several translational studies using tumor biopsies have demonstrated that neoadjuvant endocrine therapy combined with CDK4/6 inhibition can reduce Ki67 expression and induce cellular senescence8,55. However, the clinical data have been inconsistent. The PENELOPE-B69 and PALLAS70 trials did not show significant improvements in PFS. By contrast, the monarchE trial reported significant improvement in PFS, leading to the approval of adjuvant abemaciclib therapy for patients with high-risk early HR+ breast cancer (Ki67 index >20%)71. In addition, four other clinical trials are evaluating PFS in early HR+/HER− patient populations receiving adjuvant endocrine therapy in combination with CDK4/6 inhibitors (NCT02513394, NCT02764541, NCT04293393 and NCT06341894). Notably, the NATALEE trial will assess PFS in 5,000 patients treated with ribociclib over 3 years, representing the most extended treatment duration among these trials (NCT03701334).
Table 1.
Ongoing clinical trials of CDK4/6 inhibitors in patients with HR+ breast cancer, HER2+ breast cancer or TNBC.
| Addition | CDK4/6 inhibitor | Phase | Tumor type | Start | Estimated completion | Trial |
|---|---|---|---|---|---|---|
| HR+ breast cancer | ||||||
| Endocrine therapy + locoregional treatment | Palbociclib | N/A | Treatment naive, HR+/HER2− metastatic | 2019-10-23 | 2027-10-23 | NCT03870919 (PALATINE) |
| Endocrine therapy | Palbociclib | II | Slowly proliferating, HR+ breast cancer | 2015-10 | 2029-02 | NCT02592083 (PREDIX LumA) |
| Endocrine therapy | Palbociclib | II | HR+ metastatic breast cancer | 2015-02 | 2031-12-31 | NCT02603679 (PREDIX LumB) |
| Endocrine therapy | Palbociclib, Ribociclib | III | HR+ metastatic breast cancer | 2017-11-09 | 2025-12 | NCT03425838 (SONIA) |
| Endocrine therapy | Palbociclib | III | HR+ metastatic breast cancer, treatment naive | 2015-03-23 | 2025-02-28 | NCT02297438 (PALOMA-4) |
| Endocrine therapy | Palbociclib | II | HR+/HER2− metastatic breast cancer | 2016-12-07 | 2026-06-30 | NCT02942355 |
| Endocrine therapy | Palbociclib | III | HR+/HER2− advanced breast cancer | 2018-02-09 | 2025-09 | NCT03423199 (PATHWAY) |
| Endocrine therapy | Palbociclib | II | Stage II/III HR+/HER2− breast cancer | 2013-04-10 | 2026-08-24 | NCT01723774 |
| Endocrine therapy | Palbociclib | II | HR+/HER2− metastatic breast cancer | 2016-10-25 | 2025-07 | NCT02738866 |
| Endocrine therapy | Palbociclib | III | HR+/HER2− early breast cancer | 2015-08 | 2025-09 | NCT02513394 (PALLAS) |
| Endocrine therapy | Palbociclib | II | Unresectable stage I HR+/HER2− breast cancer | 2017-02-16 | 2024-12-31 | NCT02760030 |
| Endocrine therapy | Palbociclib | III | HR+/HER2− metastatic breast cancer | 2017-03-22 | 2025-06-30 | NCT03079011 |
| Endocrine therapy | Palbociclib | II | HR+ early-stage breast cancer | 2016-05-24 | 2031-04 | NCT02764541 (PELOPS) |
| Endocrine therapy | Palbociclib | III | HR+/HER2− metastatic or locally advanced breast cancer | 2020-10-09 | 2028-03-25 | NCT04546009 |
| Endocrine therapy | Palbociclib | I/II | HR+ advanced breast cancer | 2017-09-20 | 2027-12-29 | NCT03284957 |
| Endocrine therapy | Palbociclib | I | HR+/HER2− metastatic or advanced breast cancer | 2017-11-27 | 2025-06-30 | NCT03332797 |
| Endocrine therapy | Palbociclib | III | HR+/HER2− breast cancer, resected isolated locoregional recurrence | 2019-08-27 | 2026-11-01 | NCT03820830 (POLAR) |
| Endocrine therapy | Ribociclib | II | HR+/HER2− advanced breast cancer | 2018-08-29 | 2025-06-16 | NCT03671330 |
| Endocrine therapy | Ribociclib | II | HR+/HER2− advanced breast cancer | 2018-12-27 | 2025-11-27 | NCT03944434 (FACILE) |
| Endocrine therapy | Abemaciclib | II | HR+/HER2− advanced breast cancer | 2020-01-07 | 2023-12 | NCT04227327 |
| Endocrine therapy | Abemaciclib | II | HR+/HER2− advanced breast cancer | 2020-09-14 | 2024-12-30 | NCT04352777 |
| Endocrine therapy | Abemaciclib | II | HR+/HER2− early BREAST CANcer | 2020-10-02 | 2033-02-28 | NCT04293393 |
| Endocrine therapy | Abemaciclib | I | HR+/HER2− metastatic breast cancer | 2014-03-10 | 2024-12 | NCT02057133 |
| Endocrine therapy | Abemaciclib | III | HR+/HER2− metastatic breast cancer | 2020-06-11 | 2028-06 | NCT04158362 |
| Endocrine therapy | Dalpiciclib | II | HR+/HER2− early breast cancer | 2023-11-17 | 2029-06 | NCT06341894 |
| Endocrine therapy | Ribociclib | III | HR+/HER2− early breast cancer | 2018-12-07 | 2026-05-29 | NCT03701334 (NATALEE) |
| HER2+ breast cancer | ||||||
| Anti-HER2 | Palbociclib | I/II | HR+/HER2+ metastatic breast cancer | 2017-12-20 | 2025-12-31 | NCT03304080 |
| Anti-HER2 | Palbociclib | III | HR+/HER2+ metastatic breast cancer | 2017-06-21 | 2026-07-31 | NCT02947685 |
| Endocrine therapy + anti-HER2 | Palbociclib | II | HR+/HER2+ metastatic breast cancer | 2021-12-25 | 2024-12-25 | NCT05969184 |
| Endocrine therapy + anti-HER2 | Dalpiciclib | I/II | HR+/HER2+ metastatic breast cancer | 2019-05-12 | 2025-12-10 | NCT03772353 |
| Endocrine therapy + anti-HER2 | Dalpiciclib | II | Stage II–III HR+/HER2+ breast cancer | 2022-08-04 | 2025-07-30 | NCT05800756 |
| Endocrine therapy + anti-HER2 | Palbociclib | II | HR+/HER2+ breast cancer with brain metastases | 2020-12-04 | 2024-12-31 | NCT04334330 |
| TNBC | ||||||
| AR inhibitor | Palbociclib | I/II | AR+, HR−/HER2− metastatic breast cancer | 2015-11-11 | 2025-11 | NCT02605486 |
| AR inhibitor | Ribociclib | I/II | AR+, HR−/HER2− advanced breast cancer | 2018-05-07 | 2025-09 | NCT03090165 |
| Not applicable | Abemaciclib | II | AR+, HR−/HER2− stage I–III breast cancer | 2020-01-10 | 2025-07-31 | NCT03979508 |
| HDAC inhibitor | Ribociclib | I | HR−/HER2− metastatic breast cancer | 2021-05-03 | 2026-08 | NCT04315233 |
The expanding role of CDK4/6 inhibitors in breast cancer therapy underscores their importance in both metastatic and early-stage disease, with ongoing research focused on refining their application across breast cancer subtypes.
Mechanisms of resistance to CDK4/6 inhibitors
Despite the initial success of CDK4/6 inhibitors in treating HR+/HER2− breast cancer, most patients eventually develop drug resistance, limiting the long-term efficacy of this treatment72,73. To address this, extensive research has focused on elucidating the mechanisms driving resistance. Approximately 30% of patients with HR+/HER2− breast cancer who develop resistance to CDK4/6 inhibitors acquire new genetic mutations11. As Rb is the primary substrate of CDK4/6, LOF mutations in Rb represent the most well-documented mechanisms in preclinical models2,67. Breast cancer cells harboring Rb LOF mutations are unresponsive to CDK4/6 inhibitors, but this primary resistance can be reversed by reintroducing wild-type Rb54. However, Rb LOF mutations are relatively rare in HR+/HER2− breast cancer, occurring in only 4.7% of cases11,74. Another notable mutation involves LOF mutations in FAT1, which are found in approximately 6% of HR+/HER2− metastatic breast cancers75. FAT1 mutations drive CDK6 overexpression via the Hippo pathway, leading to the formation of CDK6–INK4 complexes that are resistant to CDK4/6 inhibitors75,76. CDK6 amplification and the formation of distinct CDK6 complexes have also been consistently implicated in resistance77,78.
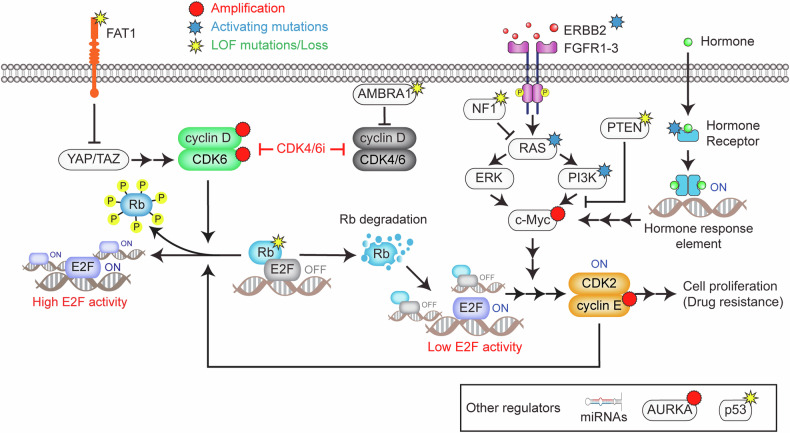
The mitogenic and hormone-signaling pathways induce cyclin D expression to activate CDK4/6, which is crucial in determining sensitivity to CDK4/6 inhibitors (Fig. 1). Tumors exhibiting increased FGFR2 or ERBB3 expression are associated with improved PFS when treated with CDK4/6 inhibitors79. However, numerous studies have demonstrated the association of mitogenic and hormone signaling with resistance to CDK4/6 inhibitors11,74,80–83. For example, amplification of the FGFR signaling pathway and PTEN loss are frequently observed in resistant tumors80,84, and alterations in KRAS have been linked to shorter PFS in HR+/HER2− breast cancer85. Most driver mutations that promote resistance are found in mitogenic and hormone-signaling genes, such as PIK3CA, ESR1, ERBB2, NF1 and FGFR1-311,74,80–82. Nevertheless, breast cancer can still respond to CDK4/6 inhibitors irrespective of ESR1 mutation status86, and PIK3CA alterations are present in both sensitive and resistant tumors74. These findings suggest that these genetic alterations may facilitate resistance while allowing an initial response to CDK4/6 inhibitors.
Fig. 1. Resistance mechanisms to CDK4/6 inhibitors.
This schematic illustrates the key genetic and nongenetic mechanisms contributing to resistance against CDK4/6 inhibitors in HR+/HER2− breast cancer. In the canonical pathway, mitogenic and hormone-signaling pathways activate the cyclin D–CDK4/6 complex, which phosphorylates Rb, effectively releasing E2F transcription factors and promoting cell cycle entry. LOF mutations in Rb represent the most well-documented primary resistance mechanism to CDK4/6 inhibitors. Another genetic mechanism involves FAT1 LOF mutations, which activate the Hippo pathway, leading to CDK6 overexpression and the formation of CDK6‒INK4 complexes resistant to CDK4/6 inhibitors. Mutations in mitogenic and hormone-signaling pathways, such as ERBB2, FGFR1-3, PIK3CA, NF1 and ESR1, which can increase c-Myc expression, are frequently observed in CDK4/6 inhibitor-resistant tumors. Nongenetic mechanisms include Rb degradation, bypassing CDK4/6 inhibition to alternatively enter the cell cycle. However, this noncanonical pathway for Rb inactivation is incomplete, necessitating E2F amplification by c-Myc, which has been shown to inversely correlate with the outcomes of CDK4/6 inhibitor therapies. The loss of AMBRA1 stabilizes cyclin D and enables its interaction with CDK2, driving resistance. In addition, amplification of AURKA and CCNE1/2 upregulates CDK2 activity, allowing tumor cells to bypass the dependency on CDK4/6. Alterations in specific miRNAs also contribute to CDK4/6 inhibitor resistance. This model emphasizes the multifaceted nature of resistance mechanisms, highlighting the roles of genetic mutations, signaling pathway alterations and transcriptional regulation.
Approximately 70% of patients with HR+/HER2− breast cancer who initially respond to CDK4/6 inhibitors develop resistance without acquiring new somatic mutations11, highlighting the role of nongenetic mechanisms. A previous study revealed the formation of a noncanonical cyclin D–CDK2 complex in HR+ breast cancer cells, leading to resistance through alternative CDK2 activation87. Loss of AMBRA1 has been shown to promote cyclin D overexpression, facilitating its interaction with CDK228,30. In addition, recent findings indicate that nonphosphorylated Rb is inherently unstable and undergoes proteolytic degradation54,88. While this Rb degradation can initiate E2F activation independently of CDK4/6, it provides only partial and low-level activation of E2F. The global transcription amplifier c-Myc plays a critical role in the development of CDK4/6 inhibitor resistance by increasing this low E2F activity. Therefore, in pretreatment samples, c-Myc expression levels, rather than Rb levels, inversely correlate with the therapeutic efficacy of combined CDK4/6 inhibitors and endocrine therapy as a first-line treatment in HR+/HER2− breast cancer. Consistently, pre- and post-treatment circulating tumor DNA analysis revealed increased c-Myc amplification in patients treated with abemaciclib compared with those treated with placebo, suggesting that c-Myc amplification may serve as a potential resistance mechanism89. This finding aligns with the frequent mutations found in mitogenic and hormone-signaling pathways that upregulate c-Myc expression in tumors resistant to CDK4/6 inhibitors. This may also account for PIK3CA mutations in both sensitive and resistant tumors34, as well as the efficacy of CDK4/6 inhibitors regardless of ESR1 mutation status36. Because hormone-signaling pathways upregulate c-Myc90, this may explain the synergistic effects observed between CDK4/6 inhibitors and endocrine therapy. Moreover, additional studies have highlighted the role of c-Myc in metabolic adaptation91 and CDK6 overexpression92, contributing to resistance.
The amplification of Aurora kinase A (AURKA), which regulates the G2/M transition, has been observed in 27% of HR+ breast tumors resistant to CDK4/6 inhibitors74. By contrast, tumors sensitive to CDK4/6 inhibitors retain regular AURKA expression. Amplifications of CCNE1 and CCNE2 (cyclin E1 and E2) are also frequently associated with resistance, as cyclin E upregulation enhances CDK2 activity, bypassing the need for CDK4/6 activity74,93,94. In one study, CCNE1 amplification was observed in HR+/HER2− cell lines with acquired resistance to palbociclib87. Inhibition of cyclin E1 or CDK2 restored sensitivity to CDK4/6 inhibitors, suggesting that cyclin E1 drives CDK2-dependent cell cycle progression in resistant cells.
MicroRNA (miRNA), noncoding RNA molecules, have also been implicated in mediating resistance to CDK4/6 inhibitors95. For example, the upregulation of miRNA-432-5p in resistant HR+/HER2− cells suppresses SMAD4 in the TGF-β pathway, leading to CDK6 upregulation and CDK4/6-inhibitor resistance96. Similarly, miRNA-29b-3p also regulates CDK6 expression and resistance92. miRNA-223 has been suggested as a potential marker of resistance, with its loss correlating with reduced OS in patients with breast cancer97. Other miRNAs, including miRNA-126, miRNA-326 and miRNA-3613-3p, have also been associated with sensitivity to CDK4/6 inhibitors in breast cancer cell lines95,98.
Emerging evidence indicates that CDK4/6 inhibition significantly alters the epigenetic landscape. A previous study showed that CDK4/6 inhibition upregulates the expression and activation of AP-1, a transcription factor that enhances the accessibility of regulatory enhancers99. These enhancers govern critical processes such as cellular differentiation, evasion of apoptosis, and long terminal repeats that may influence tumor immunogenicity. Another study revealed that the nonreceptor tyrosine kinase ACK1 is upregulated in tumors treated with CDK4/6 inhibitors100. This study indicates that ACK1 contributes to resistance by depositing epigenetic marks at key cell cycle regulator genes, including cyclin B1, B2 and CDC20. In TNBC models, BET inhibitors, which target regulators of transcriptional elements, have shown synergy with CDK4/6 inhibitors101. This combination disrupts mitosis, induces chromosomal instability and ultimately drives cellular senescence, suggesting a potential strategy to overcome resistance.
Potential predictive biomarkers of response to CDK4/6 inhibitors
The therapeutic efficacy of CDK4/6 inhibitors varies among patients with HR+/HER− breast cancer102,103, underscoring the need to identify reliable biomarkers that can predict the response to these treatments.
LOF mutations in Rb genes and Rb mRNA and protein levels
LOF mutations in the Rb gene represent one of the most prominent biomarkers for predicting primary resistance to CDK4/6 inhibitors79,104. A recent study identified germline BRCA2-mutant breast cancer as having significant enrichment of Rb LOF mutations, leading to poor PFS with CDK4/6 inhibitors105. However, in HR+/HER2− breast cancer, complete loss of Rb function is clinically rare, occurring in approximately 4.7% of cases11,74. In contrast to Rb LOF mutations, variations in Rb mRNA and protein expression among patients with intact Rb function do not reliably predict the response to CDK4/6 inhibitors104,106–108. These findings suggest that, while Rb LOF mutations are a clear driver of primary resistance, Rb mRNA or protein levels may not be sufficient to influence therapeutic outcomes in patients with functional Rb.
Cyclin D mRNA and protein levels
Given the role of cyclin D in activating CDK4/6, preclinical studies of breast cancer cell lines have revealed elevated levels of cyclin D proteins in cells sensitive to palbociclib109–111. These findings sparked interest in whether baseline cyclin D levels could predict patient response to CDK4/6 inhibitors. However, clinical data have shown that baseline cyclin D levels do not significantly correlate with patient response to CDK4/6 inhibitors106,108,112. Consistent with these clinical observations, basic research indicates that the ratio of cyclin D to Cip/Kip family members is a more reliable predictor of CDK4/6 activation than cyclin D levels alone34–36. Stabilizing cyclin D by Cip/Kip proteins can result in even higher cyclin D levels in quiescent cells than in proliferating cells, complicating the interpretation of cyclin D expression levels as a biomarker of CDK4/6 activation34.
LOF mutation in FAT1 gene
Genomic analysis of baseline HR+/HER− breast cancer biopsy samples revealed LOF mutations in the FAT1 gene as a significant predictor of early progression on CDK4/6 inhibitors. These mutations are found in approximately 6% of metastatic and 2% of primary tumor samples75.
LOF mutations in TP53 (p53) gene
Genomic analyses showed that LOF mutations in the TP53 gene are inversely correlated with PFS in patients treated with CDK4/6 inhibitors89,108,113. A recent study further demonstrated that TP53 LOF mutations can influence the long-term response to CDK4/6 inhibitors in breast cancer114. Despite this, patients with TP53 LOF mutations still responded to CDK4/6 inhibitor therapy and exhibited worse PFS, even in the control groups. These findings suggest that, although TP53 LOF mutations are associated with more aggressive tumor growth and reduced OS, they do not necessarily confer resistance to CDK4/6 inhibitors. Instead, TP53-mutated tumors are more likely to demonstrate rapid progression on CDK4/6 inhibitors.
Mitogenic and hormone signaling and c-Myc
Genetic mutations in key components of mitogenic and hormone-signaling pathways, such as PIK3CA, ESR1, FGFR1-3, KRAS and PTEN, are frequently identified in tumors resistant to CDK4/6 inhibitors11,74,80–84. Furthermore, baseline analysis of HR+/HER2− breast cancer samples revealed that phosphorylated AKT, which is indicative of PI3K pathway activation, along with c-Myc gene amplification and elevated c-Myc protein levels, was inversely correlated with PFS in patients receiving CDK4/6 inhibitors combined with endocrine therapy54,115. These findings suggest that both c-Myc and its regulatory pathways could serve as predictive biomarkers for assessing the efficacy of CDK4/6 inhibitors in breast cancer therapy.
CCNE1 (cyclin E1) amplification
The amplification of cyclin E1 is a known mechanism of CDK4/6 inhibitor resistance involving the activation of the cyclin E-CDK2 complex to promote S phase entry and bypass CDK4/6 activation. In breast tumor biopsies, CCNE1 overexpression was shown to significantly correlate with resistance to palbociclib74, whereas lower CCNE1 mRNA levels were associated with improved therapeutic response in HR+ breast cancer107,116. In the PALOMA-3 and NeoPalAna trials, high CCNE1 expression was associated with lower PFS and relative resistance to palbociclib107,117. Furthermore, selective CDK2 inhibitor treatment in CCNE1-amplified tumors resistant to CDK4/6 inhibition resulted in high sensitivity and resensitized tumors to CDK4/6 inhibition118,119. As such, CCNE1 amplification in resistant tumors may also serve as a biomarker of response to combined CDK2 and CDK4/6 inhibition.
The contribution of the tumor microenvironment
Recent studies have revealed that CDK4/6 inhibitors not only halt cancer cell proliferation but also increase anti-tumor immunity. For example, abemaciclib treatment significantly increased antigen presentation on MHC class I molecules120. Mechanistically, CDK4/6 inhibition enhances antigen presentation by suppressing the Rb–E2F axis and downregulating the expression of DNMT1, an E2F target. This leads to the demethylation of endogenous retroviral elements, resulting in the production of type III interferons and the upregulation of MHC class I molecules. In addition, CDK4/6 inhibition has been reported to increase MHC class II molecules and induce new antigen ligands on HR+ breast cancer cells, further improving immune visibility121,122.
Several studies have indicated that CDK4/6 inhibition augments T cell activation by reducing the proliferative capacity of immunosuppressive regulatory T (Treg) cells120,123,124. Treg cells are known to suppress immune responses, promote tumor immune evasion and are associated with poor prognosis in patients with breast cancer125. Notably, Treg cells express higher levels of CDK6 than other T cell subtypes, possibly increasing their sensitivity to CDK4/6 inhibition124. In mouse models treated with abemaciclib, the number of proliferating Treg cells significantly decreased, whereas CD8+ T cell levels remained unchanged, reducing the Treg-to-CD8+ T cell ratio120. Clinical studies have corroborated these findings, revealing significant downregulation of circulating Treg cells in HR+/HER2− breast cancer during CDK4/6 inhibitor treatment123. This reduction in Treg cells is correlated with an improved treatment response, suggesting that altering the Treg-to-CD8+ T cell ratio may alleviate immune suppression and enhance CD8+ T cell function.
Other studies have indicated that CDK4/6 inhibition augments the transcriptional activity of the NFAT family of transcription factors in activated T cells121,124. NFAT proteins are essential for T cell activation and regulate key cytokines such as IL-2, IL-4 and IFNγ126–129. Palbociclib treatment has been shown to increase NFAT nuclear localization and transcriptional activity in T cells, leading to elevated expression of NFAT target genes essential for T cell activation and anti-tumor immunity124. Similarly, abemaciclib treatment sustained NFAT nuclear retention, prolonging T cell activation by delaying NFAT phosphorylation121.
Modulation of the immunosuppressive factor PD-L1 by CDK4/6 inhibitors has also been observed, although this relationship is complex and context dependent. In one study, CDK4 was shown to phosphorylate and stabilize the SPOP E3 ligase, facilitating the ubiquitination and degradation of PD-L1130. CDK4/6 inhibition disrupts this process, resulting in PD-L1 accumulation on the cell surface in TNBC and HR+/HER2− tumors, which may contribute to an immunosuppressive tumor microenvironment by promoting immune evasion. However, other studies reported that palbociclib treatment reduces PD-L1 expression by repressing E2F-mediated transcription131. These contrasting findings suggest that the effect of CDK4/6 inhibitors on PD-L1 expression depends on the tumor context, the signaling pathways involved, or the CDK4/6 inhibitor used.
Despite these promising preclinical findings, translating these immunomodulatory effects of CDK4/6 inhibition into clinical practice has been challenging due to hematopoietic toxicity. In phase I and II trials, hematopoietic toxicity has been the primary dose-limiting toxicity of FDA-approved CDK4/6 inhibitors, necessitating intermittent drug treatment60,132–134. One study reported grade 3 hematologic toxicity, including neutropenia, anemia and leukopenia, occurring as early as the first treatment cycle, which involved 3 weeks of dosing followed by a 1-week break132. Preclinical and clinical studies have shown that CDK4/6 inhibitors impair bone marrow function, reducing the production of immune cells essential for effective tumor clearance112,132,135. Hematopoietic cells, including bone marrow progenitors, rely heavily on CDK4/6 for proliferation, making them particularly susceptible to these inhibitors135. In addition, CDK4/6 inhibition decreases the number of myeloid cells, which are crucial for antigen presentation and immune response coordination within the tumor microenvironment124,136. This reduction in immune cell proliferation complicates the balance between enhancing anti-tumor immunity and managing the toxic effects of CDK4/6 inhibitors.
In conclusion, the suppression of bone marrow function and associated reduction in immune cell production underscore the challenges of translating the preclinical immunomodulatory benefits of CDK4/6 inhibitors into clinical success. Continued research into the underlying mechanisms will be vital for optimizing the therapeutic potential of CDK4/6 inhibitors, especially in combination with other immunotherapies, while minimizing adverse effects.
Potential therapeutic strategies to overcome CDK4/6 inhibitor resistance
Despite the inevitable development of resistance to CDK4/6 inhibitors, no consensus has been established for second-line treatment options after disease progression. Several retrospective studies have provided valuable insights into potential treatment strategies. Multiinstitutional patient database analyses suggest that patients who continue with targeted therapies after progressing on CDK4/6 inhibitors have significantly improved PFS compared with those who switch to chemotherapy137–140. This trend underscores the importance of prioritizing continued targeted therapy as a second-line approach rather than shifting to systemic chemotherapy.
PI3K/AKT/mTOR inhibitors combined with endocrine therapy
Mutations and activation of the PI3K/AKT/mTOR pathway are common among patients with HR+/HER2− breast cancer141,142, making inhibitors of this pathway a logical choice after progression. Clinical trials of PI3K inhibitors combined with endocrine therapy have shown benefits in patients with PIK3CA mutations following progression on CDK4/6 inhibitors143,144. The CAPItello-291 trial evaluated AKT inhibitors in patients who had progressed on endocrine therapy (with or without CDK4/6 inhibitors), revealing a significant PFS benefit, particularly in patients with PIK3CA/AKT1/PTEN alterations145. This leads to the approval of the AKT inhibitor capivasertib for such mutations. Another ongoing trial is investigating the efficacy of the other AKT inhibitor ipatasertib in similar settings (NCT04650581). In addition, the use of mTOR inhibitors combined with endocrine therapy has demonstrated promise after progression with CDK4/6 inhibitors146,147.
Maintenance of CDK4/6 inhibitors with endocrine therapy
Several trials have investigated the potential benefits of continuing CDK4/6 inhibitors beyond disease progression. The PACE and PALMIRA trials assessed palbociclib continuation with a new endocrine therapy following resistance to CDK4/6 inhibitors, but these studies reported no significant improvement in PFS148,149. However, the MAINTAIN and postMONARCH trials, which examined second-line treatments using ribociclib and abemaciclib, demonstrated enhanced patient responses, suggesting that switching to a different CDK4/6 inhibitor may be beneficial after progression on palbociclib150–152. Retrospective analyses further support this maintenance approach, with higher response rates observed in patients treated with abemaciclib-based regimens153. A recent preclinical study indicated that continued CDK4/6 inhibition in drug-resistant cells activates a noncanonical pathway, leading to Rb degradation rather than phosphorylation for inactivation88. This mechanism results in low and gradual E2F activation kinetics, significantly attenuating drug-resistant tumor growth. Notably, this reduced E2F activity slows cell cycle progression without affecting cell cycle entry, suggesting that OS, rather than PFS, is probably a more suitable primary endpoint to capture the full benefit of sustained CDK4/6 inhibitor therapy.
Targeting CDK2, with or without CDK4/6 inhibitors
While CDK1 knockout in mice results in embryonic lethality, mice develop normally with either CDK4/6 or CDK2 knockout41,154,155, suggesting that neither CDK4/6 nor CDK2 is essential for cell proliferation. Further research using mice lacking CDK2/3/4/6 revealed that CDK1 alone is sufficient to drive cell cycle progression156. Given the critical role of CDK2 activity in the development of resistance to CDK4/6 inhibitors118,119,157,158, several studies have highlighted the potential of dual targeting of CDK4/6 and CDK2 activities to overcome resistance88,118,119,157,158. Despite this therapeutic promise, the clinical development of CDK2/4/6 inhibitors has been hampered by their prohibitive toxicity159,160. However, interim results from another trial suggested that combining CDK2 and CDK4/6 inhibitors may be feasible with manageable toxicity161. Ongoing clinical trials, including NCT05252416 and NCT05735080, are assessing the efficacy of CDK2 inhibitors, such as INX-315 and BLU-222, as monotherapies and in combination with endocrine therapies, with or without CDK4/6 inhibitors.
CDK7 inhibitor combined with endocrine therapy
While the effects of CDK7 inhibitors on breast cancer are not yet fully understood, CDK7 is known to play a dual role in cell cycle progression and transcription initiation by phosphorylating RNA polymerase II and priming cell cycle CDKs for activation, making it an attractive therapeutic target162. Selective CDK7 inhibitors have demonstrated greater tumor sensitivity than normal cells, driving apoptosis in CDK4/6 inhibitor-resistant breast cancer models163,164. A phase I clinical trial of the CDK7 inhibitor samuraciclib with endocrine therapy has shown encouraging clinical activity, suggesting that CDK7 inhibition is a potential approach for resistant breast cancers165. Other trials will provide insights into the safety and efficacy of CDK7 inhibitors after progression on CDK4/6 inhibitors166.
Immunotherapy
Preclinical studies suggest that CDK4/6 inhibitors can inhibit Treg cell proliferation and upregulate MHC molecule expression on tumor cells120–124, potentially enhancing anti-tumor immunity in breast cancer. However, initial clinical trials combining immune checkpoint inhibitors (ICIs) with CDK4/6 inhibitors in metastatic breast cancer did not yield significant PFS improvements167–169. In addition, severe adverse effects, including hepatotoxicity, led to treatment discontinuations. In the NEWFLAME trial, a combination of nivolumab (anti-PD1), abemaciclib and endocrine therapy demonstrated anti-tumor activity in HR+/HER2− metastatic breast cancer170. Although efficacy was promising, the trial was halted because of severe immune-related adverse events. Conversely, the PACE trial reported a significant increase in PFS with a combination of palbociclib, endocrine therapy and avelumab (anti-PD-L1) compared with palbociclib and endocrine therapy alone in patients previously treated with CDK4/6 inhibitors171. Additional trials are examining the safety and efficacy of combining CDK4/6 inhibitors with ICIs at various stages of breast cancer (NCT04841148 and NCT03280563). Given the overlapping toxicities of ICIs and CDK4/6 inhibitors, further research is essential to optimize this strategy.
Conclusions and future perspectives
Targeting the cell cycle machinery in breast cancer is a promising strategy for enhancing therapeutic outcomes. While CDK4/6 inhibitors have reshaped the treatment landscape, addressing resistance and exploring novel targets and therapeutic approaches are crucial for sustaining their effectiveness. Future research focused on combination therapies, noncanonical cell cycle entry pathways and the tumor microenvironment could pave the way for more effective and lasting treatments. Integrating these strategies into clinical practice will ultimately improve the management and prognosis of patients with breast cancer.
Acknowledgements
We thank the Yang lab members for their helpful comments. This work was supported by the Melanoma Research Foundation (H.W.Y.), Research Scholar Grant (H.W.Y., RSG-22-101-01-CDP), V Scholar Award (H.W.Y., V2023-017) and NIH grants R01-GM145884 (H.W.Y.).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sha, R., Kong, X. M., Li, X. Y. & Wang, Y. B. Global burden of breast cancer and attributable risk factors in 204 countries and territories, from 1990 to 2021: results from the Global Burden of Disease Study 2021. Biomark. Res.12, 87 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Goel, S., Bergholz, J. S. & Zhao, J. J. Targeting CDK4 and CDK6 in cancer. Nat. Rev. Cancer22, 356–372 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hanahan, D. Hallmarks of cancer: new dimensions. Cancer Discov.12, 31–46 (2022). [DOI] [PubMed] [Google Scholar]
- 4.Matson, J. P. & Cook, J. G. Cell cycle proliferation decisions: the impact of single cell analyses. FEBS J.284, 362–375 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barnum, K. J. & O’Connell, M. J. Cell cycle regulation by checkpoints. Methods Mol. Biol.1170, 29–40 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koboldt, D. C. et al. Comprehensive molecular portraits of human breast tumours. Nature490, 61–70 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Meiss, A. E. et al. Clinicopathologic characterization of breast carcinomas in patients with non-BRCA germline mutations: results from a single institution’s high-risk population. Hum. Pathol.82, 20–31 (2018). [DOI] [PubMed] [Google Scholar]
- 8.Pernas, S., Tolaney, S. M., Winer, E. P. & Goel, S. CDK4/6 inhibition in breast cancer: current practice and future directions. Ther. Adv. Med. Oncol.10, 1758835918786451 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Goetz, M. P. et al. MONARCH 3: abemaciclib as initial therapy for advanced breast cancer. J. Clin. Oncol.35, 3638–3646 (2017). [DOI] [PubMed] [Google Scholar]
- 10.Neven, P. et al. Updated overall survival from the MONALEESA-3 trial in postmenopausal women with HR+/HER2− advanced breast cancer receiving first-line ribociclib plus fulvestrant. Breast Cancer Res.25, 103 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O’Leary, B. et al. The genetic landscape and clonal evolution of breast cancer resistance to palbociclib plus fulvestrant in the PALOMA-3 trial. Cancer Discov.8, 1390–1403 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sledge, G. W. Jr et al. MONARCH 2: abemaciclib in combination with fulvestrant in women with HR+/HER2− advanced breast cancer who had progressed while receiving endocrine therapy. J. Clin. Oncol.35, 2875–2884 (2017). [DOI] [PubMed] [Google Scholar]
- 13.Pennycook, B. R. & Barr, A. R. Restriction point regulation at the crossroads between quiescence and cell proliferation. FEBS Lett. 10.1002/1873-3468.13867 (2020). [DOI] [PubMed]
- 14.Nevins, J. R. The Rb/E2F pathway and cancer. Hum. Mol. Genet.10, 699–703 (2001). [DOI] [PubMed] [Google Scholar]
- 15.Sherr, C. J. D-type cyclins. Trends Biochem. Sci.20, 187–190 (1995). [DOI] [PubMed] [Google Scholar]
- 16.Sherr, C. J. G1 phase progression: cycling on cue. Cell79, 551–555 (1994). [DOI] [PubMed] [Google Scholar]
- 17.Burkhart, D. L. & Sage, J. Cellular mechanisms of tumour suppression by the retinoblastoma gene. Nat. Rev. Cancer8, 671–682 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bracken, A. P., Ciro, M., Cocito, A. & Helin, K. E2F target genes: unraveling the biology. Trends Biochem. Sci.29, 409–417 (2004). [DOI] [PubMed] [Google Scholar]
- 19.Moiseeva, T. N. & Bakkenist, C. J. Regulation of the initiation of DNA replication in human cells. DNA Repair72, 99–106 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hwang, H. C. & Clurman, B. E. Cyclin E in normal and neoplastic cell cycles. Oncogene24, 2776–2786 (2005). [DOI] [PubMed] [Google Scholar]
- 21.Matsuoka, M., Kato, J. Y., Fisher, R. P., Morgan, D. O. & Sherr, C. J. Activation of cyclin-dependent kinase 4 (cdk4) by mouse MO15-associated kinase. Mol. Cell Biol.14, 7265–7275 (1994). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schachter, M. M. et al. A Cdk7–Cdk4 T-loop phosphorylation cascade promotes G1 progression. Mol. Cell50, 250–260 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher, R. P. Cdk7: a kinase at the core of transcription and in the crosshairs of cancer drug discovery. Transcription10, 47–56 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Gong, Y. & Li, H. CDK7 in breast cancer: mechanisms of action and therapeutic potential. Cell Commun. Signal.22, 226 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Malumbres, M. & Barbacid, M. Cell cycle, CDKs and cancer: a changing paradigm. Nat. Rev. Cancer9, 153–166 (2009). [DOI] [PubMed] [Google Scholar]
- 26.Sherr, C. J. & Roberts, J. M. Living with or without cyclins and cyclin-dependent kinases. Genes Dev.18, 2699–2711 (2004). [DOI] [PubMed] [Google Scholar]
- 27.Diehl, J. A., Cheng, M., Roussel, M. F. & Sherr, C. J. Glycogen synthase kinase-3β regulates cyclin D1 proteolysis and subcellular localization. Genes Dev.12, 3499–3511 (1998). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Simoneschi, D. et al. CRL4AMBRA1 is a master regulator of D-type cyclins. Nature592, 789–793 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maiani, E. et al. AMBRA1 regulates cyclin D to guard S-phase entry and genomic integrity. Nature592, 799–803 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chaikovsky, A. C. et al. The AMBRA1 E3 ligase adaptor regulates the stability of cyclin D. Nature592, 794–798 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Besson, A., Dowdy, S. F. & Roberts, J. M. CDK inhibitors: cell cycle regulators and beyond. Dev. Cell14, 159–169 (2008). [DOI] [PubMed] [Google Scholar]
- 32.Cheng, M. et al. The p21(Cip1) and p27(Kip1) CDK ‘inhibitors’ are essential activators of cyclin D-dependent kinases in murine fibroblasts. EMBO J.18, 1571–1583 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.LaBaer, J. et al. New functional activities for the p21 family of CDK inhibitors. Genes Dev.11, 847–862 (1997). [DOI] [PubMed] [Google Scholar]
- 34.Yang, H. W. et al. Competing memories of mitogen and p53 signalling control cell-cycle entry. Nature549, 404–408 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fan, Y. & Meyer, T. Molecular control of cell density-mediated exit to quiescence. Cell Rep36, 109436 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Guiley, K. Z. et al. p27 allosterically activates cyclin-dependent kinase 4 and antagonizes palbociclib inhibition. Science 10.1126/science.aaw2106 (2019). [DOI] [PMC free article] [PubMed]
- 37.Wu, Y. I. et al. A genetically encoded photoactivatable Rac controls the motility of living cells. Nature461, 104–108 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kim, S., Leong, A., Kim, M. & Yang, H. W. CDK4/6 initiates Rb inactivation and CDK2 activity coordinates cell-cycle commitment and G1/S transition. Sci. Rep.12, 16810 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sugimoto, M. et al. Activation of cyclin D1-kinase in murine fibroblasts lacking both p21(Cip1) and p27(Kip1). Oncogene21, 8067–8074 (2002). [DOI] [PubMed] [Google Scholar]
- 40.Kozar, K. et al. Mouse development and cell proliferation in the absence of D-cyclins. Cell118, 477–491 (2004). [DOI] [PubMed] [Google Scholar]
- 41.Malumbres, M. et al. Mammalian cells cycle without the D-type cyclin-dependent kinases Cdk4 and Cdk6. Cell118, 493–504 (2004). [DOI] [PubMed] [Google Scholar]
- 42.Liu, C. et al. Altered G1 signaling order and commitment point in cells proliferating without CDK4/6 activity. Nat. Commun.11, 5305 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zatulovskiy, E., Zhang, S., Berenson, D. F., Topacio, B. R. & Skotheim, J. M. Cell growth dilutes the cell cycle inhibitor Rb to trigger cell division. Science369, 466–471 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zhang, M., Kim, S. & Yang, H. W. Non-canonical pathway for Rb inactivation and external signaling coordinate cell-cycle entry without CDK4/6 activity. Nat. Commun.14, 7847 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zhu, J., Blenis, J. & Yuan, J. Activation of PI3K/Akt and MAPK pathways regulates Myc-mediated transcription by phosphorylating and promoting the degradation of Mad1. Proc. Natl Acad. Sci. USA105, 6584–6589 (2008). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tsai, W. B. et al. Activation of Ras/PI3K/ERK pathway induces c-Myc stabilization to upregulate argininosuccinate synthetase, leading to arginine deiminase resistance in melanoma cells. Cancer Res.72, 2622–2633 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Perez-Roger, I., Solomon, D. L., Sewing, A. & Land, H. Myc activation of cyclin E/Cdk2 kinase involves induction of cyclin E gene transcription and inhibition of p27(Kip1) binding to newly formed complexes. Oncogene14, 2373–2381 (1997). [DOI] [PubMed] [Google Scholar]
- 48.Zhang, S. et al. The G1-S transition is promoted by Rb degradation via the E3 ligase UBR5. Science Advances 10 (2024). [DOI] [PMC free article] [PubMed]
- 49.Wang, Y. et al. A novel retinoblastoma protein (RB) E3 ubiquitin ligase (NRBE3) promotes RB degradation and is transcriptionally regulated by E2F1 transcription factor. J. Biol. Chem.290, 28200–28213 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Huang, Z. et al. SETDB1 modulates degradation of phosphorylated RB and anticancer efficacy of CDK4/6 inhibitors. Cancer Res.83, 875–889 (2023). [DOI] [PubMed] [Google Scholar]
- 51.Dang, F. et al. Inhibition of CK1ε potentiates the therapeutic efficacy of CDK4/6 inhibitor in breast cancer. Nat. Commun.12, 5386 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sdek, P. et al. MDM2 promotes proteasome-dependent ubiquitin-independent degradation of retinoblastoma protein. Mol. Cell20, 699–708 (2005). [DOI] [PubMed] [Google Scholar]
- 53.Hsieh, J. et al. TTC39B destabilizes retinoblastoma protein promoting hepatic lipogenesis in a sex-specific fashion. J. Hepatol.76, 383–393 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kim, S. et al. Sequential activation of E2F via Rb degradation and c-Myc drives resistance to CDK4/6 inhibitors in breast cancer. Cell Rep.42, 113198 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Portman, N. et al. Overcoming CDK4/6 inhibitor resistance in ER-positive breast cancer. Endocr. Relat. Cancer26, R15–R30 (2019). [DOI] [PubMed] [Google Scholar]
- 56.Finn, R. S. et al. The cyclin-dependent kinase 4/6 inhibitor palbociclib in combination with letrozole versus letrozole alone as first-line treatment of oestrogen receptor-positive, HER2-negative, advanced breast cancer (PALOMA-1/TRIO-18): a randomised phase 2 study. Lancet Oncol.16, 25–35 (2015). [DOI] [PubMed] [Google Scholar]
- 57.Fry, D. W. et al. Specific inhibition of cyclin-dependent kinase 4/6 by PD 0332991 and associated antitumor activity in human tumor xenografts. Mol. Cancer Ther.3, 1427–1438 (2004). [PubMed] [Google Scholar]
- 58.Patnaik, A. et al. Efficacy and safety of abemaciclib, an inhibitor of CDK4 and CDK6, for patients with breast cancer, non–small cell lung cancer, and other solid tumors. Cancer Discov.6, 740–753 (2016). [DOI] [PubMed] [Google Scholar]
- 59.Turner, N. C. et al. Palbociclib in hormone-receptor–positive advanced breast cancer. New Engl. J. Med.373, 209–219 (2015). [DOI] [PubMed] [Google Scholar]
- 60.Infante, J. R. et al. A Phase I Study of the Cyclin-Dependent Kinase 4/6 Inhibitor Ribociclib (LEE011) in Patients with Advanced Solid Tumors and Lymphomas. Clin. Cancer Res22, 5696–5705 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Finn, R. S. et al. Efficacy and safety of palbociclib in combination with letrozole as first-line treatment of ER-positive, HER2-negative, advanced breast cancer: expanded analyses of subgroups from the randomized pivotal trial PALOMA-1/TRIO-18. Breast Cancer Res. 10.1186/s13058-016-0721-5 (2016). [DOI] [PMC free article] [PubMed]
- 62.Im, S.-A. et al. Overall survival with ribociclib plus endocrine therapy in breast cancer. New Engl. J. Med.381, 307–316 (2019). [DOI] [PubMed] [Google Scholar]
- 63.Hamilton, E. et al. nextMONARCH phase 2 randomized clinical trial: overall survival analysis of abemaciclib monotherapy or in combination with tamoxifen in patients with endocrine-refractory HR+, HER2− metastatic breast cancer. Breast Cancer Res. Treatm.195, 55–64 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu, B. Dalpiciclib in advanced breast cancer: introducing CDK4/6 inhibitors as a first-line treatment might not be the best strategy—author’s reply. Lancet Oncol.24, e357 (2023). [DOI] [PubMed] [Google Scholar]
- 65.Zhang, P. et al. Dalpiciclib plus letrozole or anastrozole versus placebo plus letrozole or anastrozole as first-line treatment in patients with hormone receptor-positive, HER2-negative advanced breast cancer (DAWNA-2): a multicentre, randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol.24, 646–657 (2023). [DOI] [PubMed] [Google Scholar]
- 66.Wang, X. et al. Recent progress of CDK4/6 inhibitors' current practice in breast cancer. Cancer Gene Ther31, 1283–1291 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fassl, A., Geng, Y. & Sicinski, P. CDK4 and CDK6 kinases: from basic science to cancer therapy. Science375, eabc1495 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hu, Y., Gao, J., Wang, M. & Li, M. Potential prospect of CDK4/6 inhibitors in triple-negative breast cancer. Cancer Manag. Res.13, 5223–5237 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Loibl, S. et al. Palbociclib for residual high-risk invasive HR-positive and HER2-negative early breast cancer—the PENELOPE-B trial. J. Clin. Oncol.39, 1518–1530 (2021). [DOI] [PubMed] [Google Scholar]
- 70.Gnant, M. et al. Adjuvant palbociclib for early breast cancer: the PALLAS trial results (ABCSG-42/AFT-05/BIG-14-03). J. Clin. Oncol.40, 282–293 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Johnston, S. R. et al. Abemaciclib combined with endocrine therapy for the adjuvant treatment of HR+, HER2−, node-positive, high-risk, early breast cancer (monarchE). J. Clin. Oncol.38, 3987–3998 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Hortobagyi, G. N. et al. Ribociclib as first-line therapy for HR-positive, advanced breast cancer. N. Engl. J. Med.375, 1738–1748 (2016). [DOI] [PubMed] [Google Scholar]
- 73.O’Leary, B., Finn, R. S. & Turner, N. C. Treating cancer with selective CDK4/6 inhibitors. Nat. Rev. Clin. Oncol.13, 417–430 (2016). [DOI] [PubMed] [Google Scholar]
- 74.Wander, S. A. et al. The genomic landscape of intrinsic and acquired resistance to cyclin-dependent kinase 4/6 inhibitors in patients with hormone receptor-positive metastatic breast cancer. Cancer Discov.10, 1174–1193 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Li, Z. et al. Loss of the FAT1 tumor suppressor promotes resistance to CDK4/6 inhibitors via the Hippo pathway. Cancer Cell34, 893–905 e898 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Li, Q. et al. INK4 tumor suppressor proteins mediate resistance to CDK4/6 kinase inhibitors. Cancer Discov.12, 356–371 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Yang, C. et al. Acquired CDK6 amplification promotes breast cancer resistance to CDK4/6 inhibitors and loss of ER signaling and dependence. Oncogene36, 2255–2264 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Wu, X. et al. Distinct CDK6 complexes determine tumor cell response to CDK4/6 inhibitors and degraders. Nat. Cancer2, 429–443 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Finn, R. S. et al. Biomarker analyses of response to cyclin-dependent kinase 4/6 inhibition and endocrine therapy in women with treatment-naive metastatic breast cancer. Clin. Cancer Res.26, 110–121 (2020). [DOI] [PubMed] [Google Scholar]
- 80.Formisano, L. et al. Aberrant FGFR signaling mediates resistance to CDK4/6 inhibitors in ER+ breast cancer. Nat. Commun.10, 1373 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.de Leeuw, R. et al. MAPK reliance via acquired CDK4/6 inhibitor resistance in cancer. Clin. Cancer Res.24, 4201–4214 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Mao, P. et al. Acquired FGFR and FGF alterations confer resistance to estrogen receptor (ER) targeted therapy in ER+ metastatic breast cancer. Clin. Cancer Res.26, 5974–5989 (2020). [DOI] [PubMed] [Google Scholar]
- 83.Razavi, P. et al. The genomic landscape of endocrine-resistant advanced breast cancers. Cancer Cell34, 427–438 e426 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Costa, C. et al. PTEN loss mediates clinical cross-resistance to CDK4/6 and PI3Kα inhibitors in breast cancer. Cancer Discov.10, 72–85 (2020). [DOI] [PubMed] [Google Scholar]
- 85.Raimondi, L. et al. Assessment of resistance mechanisms and clinical implications in patients with KRAS mutated-metastatic breast cancer and resistance to CDK4/6 inhibitors. Cancers13, 1928 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fribbens, C. et al. Plasma ESR1 mutations and the treatment of estrogen receptor-positive advanced breast cancer. J. Clin. Oncol.34, 2961–2968 (2016). [DOI] [PubMed] [Google Scholar]
- 87.Herrera-Abreu, M. T. et al. Early adaptation and acquired resistance to CDK4/6 inhibition in estrogen receptor–positive breast cancer. Cancer Res.76, 2301–2313 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Armand, J. et al. Therapeutic benefits of maintaining CDK4/6 inhibitors and incorporating CDK2 inhibitors beyond progression in breast cancer. eLife14, RP104545 (2025). [Google Scholar]
- 89.Goetz, M. P. et al. Landscape of baseline and acquired genomic alterations in circulating tumor DNA with abemaciclib alone or with endocrine therapy in advanced breast cancer. Clin. Cancer Res.30, 2233–2244 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Shang, Y., Hu, X., DiRenzo, J., Lazar, M. A. & Brown, M. Cofactor dynamics and sufficiency in estrogen receptor-regulated transcription. Cell103, 843–852 (2000). [DOI] [PubMed] [Google Scholar]
- 91.Tarrado‐Castellarnau, M. et al. De novo MYC addiction as an adaptive response of cancer cells to CDK 4/6 inhibition. Mol. Syst. Biol.13, 940 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Ji, W. et al. c-myc regulates the sensitivity of breast cancer cells to palbociclib via c-myc/miR-29b-3p/CDK6 axis. Cell Death Dis.11, 760 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Taylor-Harding, B. et al. Cyclin E1 and RTK/RAS signaling drive CDK inhibitor resistance via activation of E2F and ETS. Oncotarget6, 696–714 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Guarducci, C. et al. Cyclin E1 and Rb modulation as common events at time of resistance to palbociclib in hormone receptor-positive breast cancer. npj Breast Cancer4, 38 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Andrikopoulou, A. et al. MicroRNAs as potential predictors of response to CDK4/6 inhibitor treatment. Cancers13, 4114 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cornell, L., Wander, S. A., Visal, T., Wagle, N. & Shapiro, G. I. MicroRNA-mediated suppression of the TGF-β pathway confers transmissible and reversible CDK4/6 inhibitor resistance. Cell Rep.26, 2667–2680 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Citron, F. et al. Downregulation of miR-223 expression is an early event during mammary transformation and confers resistance to CDK4/6 inhibitors in luminal breast cancer. Cancer Res.80, 1064–1077 (2020). [DOI] [PubMed] [Google Scholar]
- 98.Krasniqi, E. et al. Biomarkers of response and resistance to CDK4/6 inhibitors in breast cancer: hints from liquid biopsy and microRNA exploration. Int. J. Mol. Sci.23, 14534 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Watt, A. C. et al. CDK4/6 inhibition reprograms the breast cancer enhancer landscape by stimulating AP-1 transcriptional activity. Nat. Cancer2, 34–48 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Sawant, M. et al. Epigenetic reprogramming of cell cycle genes by ACK1 promotes breast cancer resistance to CDK4/6 inhibitor. Oncogene42, 2263–2277 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Ge, J. Y. et al. Acquired resistance to combined BET and CDK4/6 inhibition in triple-negative breast cancer. Nat. Commun.11, 2350 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Schoninger, S. F. & Blain, S. W. The ongoing search for biomarkers of CDK4/6 inhibitor responsiveness in breast cancer. Mol. Cancer Ther.19, 3–12 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Anurag, M., Haricharan, S. & Ellis, M. J. CDK4/6 inhibitor biomarker research: are we barking up the wrong tree? Clin. Cancer Res.26, 3–5 (2020). [DOI] [PubMed] [Google Scholar]
- 104.Andre, F. et al. Pooled ctDNA analysis of MONALEESA phase III advanced breast cancer trials. Ann. Oncol.34, 1003–1014 (2023). [DOI] [PubMed] [Google Scholar]
- 105.Safonov, A. et al. Tumor suppressor heterozygosity and homologous recombination deficiency mediate resistance to front-line therapy in breast cancer. Preprint at bioRxiv 10.1101/2024.02.05.578934 (2024).
- 106.Zhu, Z. et al. Comparative biomarker analysis of PALOMA-2/3 trials for palbociclib. NPJ Precision Oncology6, 56 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Turner, N. C. et al. Cyclin E1 expression and palbociclib efficacy in previously treated hormone receptor-positive metastatic breast cancer. J. Clin. Oncol.37, 1169–1178 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Hortobagyi, G. N. et al. Updated results from MONALEESA-2, a phase III trial of first-line ribociclib plus letrozole versus placebo plus letrozole in hormone receptor-positive, HER2-negative advanced breast cancer. Ann. Oncol.29, 1541–1547 (2018). [DOI] [PubMed] [Google Scholar]
- 109.Finn, R. S. et al. PD 0332991, a selective cyclin D kinase 4/6 inhibitor, preferentially inhibits proliferation of luminal estrogen receptor-positive human breast cancer cell lines in vitro. Breast Cancer Res.11, R77 (2009). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Gong, X. et al. Genomic aberrations that activate D-type cyclins are associated with enhanced sensitivity to the CDK4 and CDK6 inhibitor abemaciclib. Cancer Cell32, 761–776 (2017). [DOI] [PubMed] [Google Scholar]
- 111.Shapiro, G. I. Genomic biomarkers predicting response to selective CDK4/6 inhibition: progress in an elusive search. Cancer Cell32, 721–723 (2017). [DOI] [PubMed] [Google Scholar]
- 112.DeMichele, A. et al. CDK 4/6 inhibitor palbociclib (PD0332991) in Rb+ advanced breast cancer: phase II activity, safety, and predictive biomarker assessment. Clin. Cancer Res.21, 995–1001 (2015). [DOI] [PubMed] [Google Scholar]
- 113.O’Leary, B. et al. Circulating tumor DNA markers for early progression on fulvestrant with or without palbociclib in ER+ advanced breast cancer. J. Natl Cancer Inst.113, 309–317 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kudo, R. et al. Long-term breast cancer response to CDK4/6 inhibition defined by TP53-mediated geroconversion. Cancer Cell 10.1016/j.ccell.2024.09.009 (2024).
- 115.Alves, C. L. et al. Co-targeting CDK4/6 and AKT with endocrine therapy prevents progression in CDK4/6 inhibitor and endocrine therapy-resistant breast cancer. Nat. Commun.12, 5112 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Arnedos, M. et al. Modulation of Rb phosphorylation and antiproliferative response to palbociclib: the preoperative-palbociclib (POP) randomized clinical trial. Ann. Oncol.29, 1755–1762 (2018). [DOI] [PubMed] [Google Scholar]
- 117.Ma, C. X. et al. NeoPalAna: neoadjuvant palbociclib, a cyclin-dependent kinase 4/6 inhibitor, and anastrozole for clinical stage 2 or 3 estrogen receptor–positive breast cancer. Clin. Cancer Res.23, 4055–4065 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Al-Qasem, A. J. et al. Co-targeting CDK2 and CDK4/6 overcomes resistance to aromatase and CDK4/6 inhibitors in ER+ breast cancer. npj Precis. Oncol.6, 68 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dietrich, C. et al. INX-315, a selective CDK2 inhibitor, induces cell cycle arrest and senescence in solid tumors. Cancer Discov. 10.1158/2159-8290.CD-23-0954 (2023). [DOI] [PMC free article] [PubMed]
- 120.Goel, S. et al. CDK4/6 inhibition triggers anti-tumour immunity. Nature548, 471–475 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Schaer, D. A. et al. The CDK4/6 inhibitor abemaciclib induces a T cell inflamed tumor microenvironment and enhances the efficacy of PD-L1 checkpoint blockade. Cell Rep.22, 2978–2994 (2018). [DOI] [PubMed] [Google Scholar]
- 122.Charles, A. et al. Low-dose CDK4/6 inhibitors induce presentation of pathway specific MHC ligands as potential targets for cancer immunotherapy. OncoImmunology10, 1916243 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Scirocchi, F. et al. Immune effects of CDK4/6 inhibitors in patients with HR+/HER2− metastatic breast cancer: relief from immunosuppression is associated with clinical response. eBioMedicine79, 104010 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Deng, J. et al. CDK4/6 inhibition augments antitumor immunity by enhancing T-cell activation. Cancer Discov.8, 216–233 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Syed Khaja, A. S. et al. Preferential accumulation of regulatory T cells with highly immunosuppressive characteristics in breast tumor microenvironment. Oncotarget8, 33159–33171 (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Macian, F. NFAT proteins: key regulators of T-cell development and function. Nat. Rev. Immunol.5, 472–484 (2005). [DOI] [PubMed] [Google Scholar]
- 127.Kaminuma, O. et al. Downregulation of NFAT3 due to lack of T-box transcription factor TBX5 is crucial for cytokine expression in T cells. J. Immunol.200, 92–100 (2018). [DOI] [PubMed] [Google Scholar]
- 128.Luo, C. et al. Recombinant NFAT1 (NFATp) is regulated by calcineurin in T cells and mediates transcription of several cytokine genes. Mol. Cell Biol.16, 3955–3966 (1996). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chow, C.-W., Rincón, M. & Davis, R. J. Requirement for transcription factor NFAT in interleukin-2 expression. Mol. Cell. Biol.19, 2300–2307 (1999). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Zhang, J. et al. Cyclin D–CDK4 kinase destabilizes PD-L1 via cullin 3–SPOP to control cancer immune surveillance. Nature553, 91–95 (2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Shrestha, M., Wang, D.-Y., Ben-David, Y. & Zacksenhaus, E. CDK4/6 inhibitors and the pRB-E2F1 axis suppress PVR and PD-L1 expression in triple-negative breast cancer. Oncogenesis12, 29 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Flaherty, K. T. et al. Phase I, dose-escalation trial of the oral cyclin-dependent kinase 4/6 inhibitor PD 0332991, administered using a 21-day schedule in patients with advanced cancer. Clin. Cancer Res.18, 568–576 (2012). [DOI] [PubMed] [Google Scholar]
- 133.DeMichele, A. et al. A phase II trial of an oral CDK 4/6 inhibitor, PD0332991, in advanced breast cancer. J. Clin. Oncol.31, 519–519 (2013). [Google Scholar]
- 134.Shapiro, G. et al. A first-in-human phase I study of the CDK4/6 inhibitor, LY2835219, for patients with advanced cancer. J. Clin. Oncol.31, 2500–2500 (2013).23715580 [Google Scholar]
- 135.Johnson, S. M. et al. Mitigation of hematologic radiation toxicity in mice through pharmacological quiescence induced by CDK4/6 inhibition. J. Clin. Invest.120, 2528–2536 (2010). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Bisi, J. E., Sorrentino, J. A., Roberts, P. J., Tavares, F. X. & Strum, J. C. Preclinical characterization of G1T28: a novel CDK4/6 inhibitor for reduction of chemotherapy-induced myelosuppression. Mol. Cancer Ther.15, 783–793 (2016). [DOI] [PubMed] [Google Scholar]
- 137.Martin, J. M., Handorf, E. A., Montero, A. J. & Goldstein, L. J. Systemic therapies following progression on first-line CDK4/6-inhibitor treatment: analysis of real-world data. Oncologist27, 441–446 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Xi, J. et al. Retrospective analysis of treatment patterns and effectiveness of palbociclib and subsequent regimens in metastatic breast cancer. J. Natl Compr. Cancer Netw.17, 141–147 (2019). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Princic, N. et al. Predictors of systemic therapy sequences following a CDK 4/6 inhibitor-based regimen in post-menopausal women with hormone receptor positive, HEGFR-2 negative metastatic breast cancer. Curr. Med. Res. Opin.35, 73–80 (2019). [DOI] [PubMed] [Google Scholar]
- 140.Basile, D. et al. First- and second-line treatment strategies for hormone-receptor (HR)-positive HER2-negative metastatic breast cancer: a real-world study. Breast57, 104–112 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Anderson, E. J. et al. A systematic review of the prevalence and diagnostic workup of PIK3CA mutations in HR+/HER2− metastatic breast cancer. Int. J. Breast Cancer2020, 3759179 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Miricescu, D. et al. PI3K/AKT/mTOR signaling pathway in breast cancer: from molecular landscape to clinical aspects. Int. J. Mol. Sci.22, 173 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Rugo, H. S. et al. Alpelisib plus fulvestrant in PIK3CA-mutated, hormone receptor-positive advanced breast cancer after a CDK4/6 inhibitor (BYLieve): one cohort of a phase 2, multicentre, open-label, non-comparative study. Lancet Oncol.22, 489–498 (2021). [DOI] [PubMed] [Google Scholar]
- 144.Chia, S. et al. Alpelisib + endocrine therapy in patients with PIK3CA-mutated, hormone receptor–positive, human epidermal growth factor receptor 2–negative, advanced breast cancer: analysis of all 3 cohorts of the BYLieve study. J. Clin. Oncol.41, 1078–1078 (2023). [Google Scholar]
- 145.Turner, N. C. et al. Capivasertib in hormone receptor–positive advanced breast cancer. New Engl. J. Med.388, 2058–2070 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Cook, M. M. et al. Everolimus plus exemestane treatment in patients with metastatic hormone receptor‐positive breast cancer previously treated with CDK4/6 inhibitor therapy. Oncologist26, 101–106 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Bardia, A. et al. Phase I/II trial of exemestane, ribociclib, and everolimus in women with HR+/HER2− advanced breast cancer after progression on CDK4/6 inhibitors (TRINITI-1). Clin. Cancer Res.27, 4177–4185 (2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Mayer, E. L. et al. Palbociclib after CDK and endocrine therapy (PACE): a randomized phase II study of fulvestrant, palbociclib, and avelumab for endocrine pre-treated ER+/HER2− metastatic breast cancer. J. Clin. Oncol.36, TPS1104 (2018). [Google Scholar]
- 149.Llombart-Cussac, A. et al. Second-line endocrine therapy (ET) with or without palbociclib (P) maintenance in patients (pts) with hormone receptor-positive (HR+)/human epidermal growth factor receptor 2-negative (HER2−) advanced breast cancer (ABC): PALMIRA trial. J. Clin. Oncol.41, 1001 (2023). [Google Scholar]
- 150.Kalinsky, K. et al. Randomized phase II trial of endocrine therapy with or without ribociclib after progression on cyclin-dependent kinase 4/6 inhibition in hormone receptor-positive, human epidermal growth factor receptor 2-negative metastatic breast cancer: MAINTAIN trial. J. Clin. Oncol. 10.1200/JCO.22.02392 (2023). [DOI] [PubMed]
- 151.Wander, S. A. et al. Clinical outcomes with abemaciclib after prior CDK4/6 inhibitor progression in breast cancer: a multicenter experience. J. Natl Compr. Cancer Netw. 10.6004/jnccn.2020.7662 (2021). [DOI] [PubMed]
- 152.Kalinsky, K. et al. Abemaciclib plus fulvestrant vs fulvestrant alone for HR+, HER2− advanced breast cancer following progression on a prior CDK4/6 inhibitor plus endocrine therapy: primary outcome of the phase 3 postMONARCH trial. J. Clin. Oncol.42, LBA1001 (2024). [Google Scholar]
- 153.Anjos, C. H. D. et al. A large retrospective analysis of CDK 4/6 inhibitor retreatment in ER+ metastatic breast cancer (MBC). J. Clin. Oncol.37, 1053 (2019). [Google Scholar]
- 154.Berthet, C., Aleem, E., Coppola, V., Tessarollo, L. & Kaldis, P. Cdk2 knockout mice are viable. Curr. Biol.13, 1775–1785 (2003). [DOI] [PubMed] [Google Scholar]
- 155.Barriere, C. et al. Mice thrive without Cdk4 and Cdk2. Mol. Oncol.1, 72–83 (2007). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Santamaria, D. et al. Cdk1 is sufficient to drive the mammalian cell cycle. Nature448, 811–815 (2007). [DOI] [PubMed] [Google Scholar]
- 157.Pandey, K. et al. Combined CDK2 and CDK4/6 inhibition overcomes palbociclib resistance in breast cancer by enhancing senescence. Cancers12, 3566 (2020). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Freeman-Cook, K. et al. Expanding control of the tumor cell cycle with a CDK2/4/6 inhibitor. Cancer Cell39, 1404–1421 e1411 (2021). [DOI] [PubMed] [Google Scholar]
- 159.Pfizer pipeline. Pfizerhttps://cdn.pfizer.com/pfizercom/product-pipeline/Pipeline_Update_31JAN2023.pdf?Y9dll8b2GbzLJ_q0NsCadkr_zh15l3or (2023).
- 160.Nuvation Bio Announces Discontinuation of NUV-422 Clinical Development Program. NuvationBiohttps://investors.nuvationbio.com/news/news-details/2022/Nuvation-Bio-Announces-Discontinuation-of-NUV-422-Clinical-Development-Program/default.aspx (2022).
- 161.Juric, D. et al. BLU-222, an investigational, oral, potent, and highly selective CDK2 inhibitor (CDK2i), as monotherapy in patients (pts) with advanced solid tumors and in combination with ribociclib (RIBO) and fulvestrant (FUL) in HR+/HER2− breast cancer (BC). J. Clin. Oncol.42, 1056 (2024). [Google Scholar]
- 162.Song, X. et al. Cyclin-dependent kinase 7 (CDK7) inhibitors as a novel therapeutic strategy for different molecular types of breast cancer. Br. J. Cancer130, 1239–1248 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Hu, S. et al. Discovery and characterization of SY-1365, a selective, covalent inhibitor of CDK7. Cancer Res.79, 3479–3491 (2019). [DOI] [PubMed] [Google Scholar]
- 164.Guarducci, C. et al. Selective CDK7 inhibition suppresses cell cycle progression and MYC signaling while enhancing apoptosis in therapy-resistant estrogen receptor–positive breast cancer. Clin. Cancer Res.30, 1889–1905 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Coombes, R. C. et al. Dose escalation and expansion cohorts in patients with advanced breast cancer in a phase I study of the CDK7-inhibitor samuraciclib. Nat. Commun.14, 4444 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bardia, A. et al. Elacestrant in ER+, HER2-MBC with ESR1-mutated tumors: Subgroup Analyses from the Phase III EMERALD Trial by Prior Duration of Endocrine Therapy Plus CDK4/6 Inhibitor and in Clinical Subgroups. Clin Cancer Res30, 4299–4309 (2024). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Rugo, H. S. et al. Abemaciclib in combination with pembrolizumab for HR+, HER2− metastatic breast cancer: phase 1b study. npj Breast Cancer8, 118 (2022). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Jerusalem, G. et al. Neoadjuvant nivolumab + palbociclib + anastrozole for oestrogen receptor-positive/human epidermal growth factor receptor 2-negative primary breast cancer: results from CheckMate 7A8. Breast72, 103580 (2023). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Herold, C. I. et al. A phase 1b study of the CDK4/6 inhibitor ribociclib in combination with the PD-1 inhibitor spartalizumab in patients with hormone receptor-positive metastatic breast cancer (HR plus MBC) and metastatic ovarian cancer (MOC). Cancer Res. 10.1158/1538-7445.Sabcs19-p3-14-03 (2020).
- 170.Masuda, J. et al. Efficacy, safety, and biomarker analysis of nivolumab in combination with abemaciclib plus endocrine therapy in patients with HR-positive HER2-negative metastatic breast cancer: a phase II study (WJOG11418B NEWFLAME trial). J. Immunother. Cancer 10.1136/jitc-2023-007126 (2023). [DOI] [PMC free article] [PubMed]
- 171.Mayer, E. L. et al. PACE: a randomized phase II study of fulvestrant, palbociclib, and avelumab after progression on cyclin-dependent kinase 4/6 inhibitor and aromatase inhibitor for hormone receptor-positive/human epidermal growth factor receptor-negative metastatic breast cancer. J. Clin. Oncol. 10.1200/JCO.23.01940 (2024). [DOI] [PubMed]