Abstract
The anterior cruciate ligament (ACL) is the most frequently injured knee ligament that requires surgical intervention. Surgical options to address ACL ruptures include reconstruction using autograft or allograft or performing primary repair. Subsequent ACL graft failure is a significant postoperative concern in the younger patient population. The addition of suture tape to the final construct is thought to protect the graft during moments of high stress by increasing graft stiffness under high load and preventing substantial graft elongation. Given the normal anatomic lengthening of the ACL from knee flexion to full extension, final fixation of both the suture tape and the graft is done with the knee hyperextended to avoid overconstraint. The use of adjustable loop fixation for both femoral and tibial fixation with the all-inside technique allows the graft to be retensioned after final suture tape fixation and subsequent knee cycling. This ensures that the suture tape is slightly laxer than the graft so that the graft experiences loads that are essential for its healing, with the suture tape sharing the load only during times of high stress.
Technique Video
As competitive sport participation among children and adolescents has increased, the incidence of anterior cruciate ligament (ACL) injuries has also risen.1, 2, 3 Furthermore, the rate of a second ACL injury, particularly graft failure, remains high, especially for younger patients who return to the same level of competition.4 ACL graft retear rates in younger athletes range from 9% to 23%, and most occur within the first 2 years after primary ACL reconstruction.4, 5, 6 Multiple factors play a role in the increased risk of graft failure, including participation in pivoting sports, as well as other characteristics such as younger age, knee recurvatum, sex, and type of graft used, among others.3,6, 7, 8
Independent suture tape augmentation (I-STA) has been proposed to mitigate the risk for retear due to its favorable biomechanical properties.9,10 Clinically, I-STA has been shown to result in a low retear rate in younger patients.11, 12, 13 We present a technique demonstrating an all-inside ACL reconstruction using a full-thickness all-soft-tissue quadriceps tendon autograft (ASTQA) with I-STA, highlighting final suture tape and graft fixation with the knee always in full hyperextension. Video 1 provides step-by-step visualization and Table 1 lists the pearls and pitfalls of this procedure.
Table 1.
Pearls and Pitfalls
| Pearls | Pitfalls |
|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
ACL, anterior cruciate ligament; ALD, adjustable loop device.
Surgical Technique
Step 1: Patient Setup
The patient is placed supine on a standard operating table. After examination under anesthesia, the left knee is prepped and draped in a sterile fashion with 2 g of Kefzol administered before the surgical timeout.
Step 2: Harvest of ASTQA
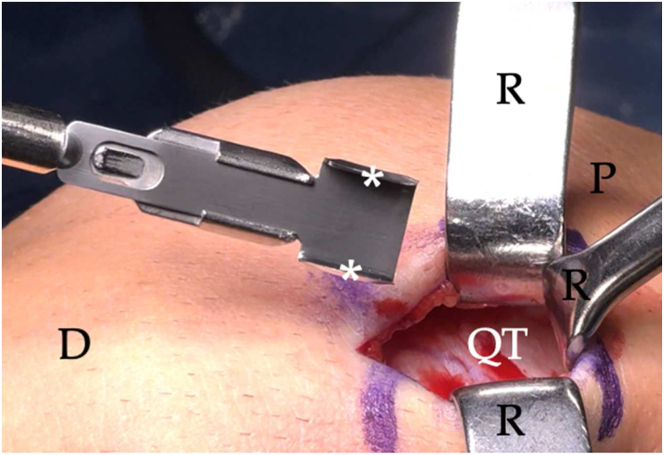
With the knee flexed at 100°, a 3-cm vertical incision is made to expose the quadriceps tendon. A 10-mm wide 7-mm deep double knife blade (Parallel Graft Knife Blade; Arthrex, Naples, FL) is used to incise the tendon from the superior patellar pole extending 65 mm proximally (Fig 1).
Fig 1.
Intraoperative photograph of the left knee flexed at 100° showing a 10-mm double knife blade (asterisk) used for initial harvesting of a full-thickness quadriceps tendon graft. (D, distal; P, proximal; QT, quadriceps tendon; R, retractors.)
The full-thickness quadriceps tendon is then released from the superior patellar pole. A suture is placed within the released end of the graft, which is threaded through a “cigar cutter” device (Quad Tendon Stripper Cutter; Arthrex) that is used to amputate the full-thickness graft proximally (Fig 2).
Fig 2.
Intraoperative photograph of a left knee flexed at 100° showing the released quadriceps tendon strip with attached sutures (black arrow) threaded through a “cigar cutter” (asterisk) used for graft amputation (A) and the subsequent harvested full-thickness all-soft-tissue quadriceps tendon graft measuring 65 mm in length with a width of 10 mm (B). (D, distal; P, proximal; QT, quadriceps tendon; R, retractors.)
After irrigation, with the knee still flexed at 100°, the quadriceps tendon defect is closed, followed by subcutaneous tissue and skin closure (Fig 3).
Fig 3.
Intraoperative photograph of a left knee flexed at 100° demonstrating the closed quadriceps tendon (asterisk) with interrupted Vicryl sutures (white arrowheads) in a horizontal mattress fashion (A) and the skin closure of the 3-cm vertical incision done with subcutaneous Prolene suture (white arrows) (B). (R, retractors.)
Step 3: Diagnostic Arthroscopy
A thorough diagnostic arthroscopy is performed. First, a standard lateral parapatellar portal is established, followed by a low anteromedial portal using an 18-gauge spinal needle for optimal localization. The suprapatellar pouch is first inspected, followed by the medial compartment including the Gillquist view, intercondylar notch, and finally the lateral compartment.
Step 4: All-Inside ACL Reconstruction Using a Full-Thickness ASTQA With Suture Tape Augmentation
First, a shaver is used to excise some of the torn ACL fibers, preserving the footprint of the native anteromedial and posterolateral bundle fibers both on the tibia and femur for orientation purposes to facilitate optimal socket creation.
With the knee flexed to approximately 120°, a pilot hole is drilled within the anteromedial bundle femoral footprint through the anteromedial portal. A measuring pin is then drilled across the joint from the anteromedial portal at this pilot hole to measure the femoral intraosseous distance. Next, a 10-mm reamer is used to drill over the pin, exceeding the expected graft length in the femur by 4 to 5 mm.
With the knee flexed to approximately 80°, a tibial aiming device (Tibial ACL Marking Hook; Arthrex) is positioned within the native ACL footprint, also indexing off the attachment of the anterior horn of the lateral meniscus (Fig 4).
Fig 4.
Arthroscopic view through the anterolateral portal of a left knee flexed at 80° demonstrating a tibial guide (G) placed directly on top of the tibial remnant (T) of the native anterior cruciate ligament, which also is in line with the attachment of the anterior horn of the lateral meniscus. (L, lateral femoral condyle; M, medial femoral condyle; P, posterior cruciate ligament; S, femoral shuttle suture.)
A 1.5-cm tibial incision is made over the anteromedial proximal tibia. The guide sleeve is placed down to bone, and a retro-cutter (FlipCutter III; Arthrex) is drilled through the center of the guide. The retro-cutter is opened to 10 mm, and a tibial socket is retrocut to a depth that allows space for graft retensioning. A suture passer is passed through the tibial socket where the suture is retrieved through the anteromedial portal. A measuring device is used to measure the intra-articular ACL length from the aperture of the femoral to the tibial socket. The graft is marked with the appropriate distances.
The femoral shuttle suture is used to pull across the blue passing suture and the white shortening strands of the femoral adjustable loop device (ALD) (TightRope; Arthrex) with the attached independent suture tape (InternalBrace; Arthrex). The button is flipped on the lateral femoral cortex and is additionally seated by pulling on the 2 free distal tape ends. The graft is then hoisted to the measured femoral depth.
The tibial end of the graft, with the 2 free suture tape ends and the shortening strands of the ALD (TightRope Attachable Button System; Arthrex), is shuttled through the tibial socket. The graft is then pulled into the tibial socket. On the tibial side, a 14-mm button (Attachable Button System button; Arthrex) is applied to the buttonless tibial ALD (Fig 5 A and B). The 2 suture tape ends are then passed through the buttonholes (Fig 5C).
Fig 5.
(A) Intraoperative photograph of a 14-mm button (asterisk) with 2 sets of distinct holes—2 slots (white arrowheads) and 2 closed holes (black arrowheads). (B) The 2 doubled segments of the adjustable loop are placed respectively within the 2 slots of the button with the button pulled distally to the base of the loop, allowing the 2 tibial shortening strands (white arrows) to run free distally. (C) The 2 distal tape ends (black arrows) are then placed through the 2 closed holes.
The button is then brought down to the tibia pulling on the ALD shortening strands with the knee in hyperextension, but the tibial end of the graft is not tightened yet (Fig 6).
Fig 6.
Intraoperative photograph of a left knee in full hyperextension demonstrating the distal adjustable loop device button (asterisk) brought down to the tibia using the shortening strands (white arrow) of the adjustable loop device before suture tape (black arrows) fixation. (R, retractors.)
A 4.5-mm hole is drilled 1 cm distal to the button and is subsequently tapped. The 2 tape ends are passed through a 4.75-mm absorbable anchor (BioComposite SwiveLock; Arthrex) and fixed in the distal hole with the knee hyperextended making sure the 2 shortening strands are free between the tapes (Fig 7).
Fig 7.
Intraoperative photograph of a left knee in full hyperextension demonstrating final suture tape fixation (white arrows) done 1 cm distal to the tibial tunnel with a suture anchor. Notice the 2 shortening strands (white arrowheads) are “free” between the 2 tapes to allow for unimpeded tibial graft tensioning. The tape ends distal to the fixation (black arrows) were then cut and discarded. Asterisk, tibial button. (A, anchor; R, retractors.)
After final suture tape fixation, tensioning handles are placed on the tibial shortening strands, which are then tensioned with the knee hyperextended. The knee is cycled 20 times. The tensioning handles are then placed on the femoral shortening strands, which are tensioned with the knee in hyperextension. After tensioning of the femoral shortening strands, the tibial shortening strands are retensioned with the knee hyperextended and then tied to the tibial button for backup fixation.
Stability testing is performed after final construct fixation. Final graft positioning and tautness are assessed arthroscopically. The suture tape is visualized running posterior to the graft and lax to probing at 90° (Fig 8).
Fig 8.
(A) Arthroscopic view through the anterolateral portal of a left knee flexed to 90° demonstrating the quadriceps tendon autograft final construct. (B) With use of the probe (black arrowhead) through the anteromedial portal, the suture tape (asterisk) can be visualized posterior to the graft and relatively lax in this flexed position compared with the graft. (LFC, lateral femoral condyle; LM, lateral meniscus; LTP, lateral tibial plateau; M, medial femoral condyle; P, posterior cruciate ligament; Q, quadriceps tendon autograft.)
Step 5: Postoperative Rehabilitation
Patients are placed in a splint locked in extension immediately postoperatively. All patients receive a continuous passive motion machine for the first 2 weeks. Physical therapy starts postoperative day 2 with a dressing change and a focus on quad sets and straight leg raises, emphasizing full extension without a lag. Closed-chain exercises begin once the patient achieves full-weightbearing status. Patients are cleared to jog in their functional brace by postoperative month 3, with agility exercises beginning by postoperative month 4 and sport-specific exercises beginning by postoperative month 5. Patients may be cleared to return to sport by the 6-month visit depending on physical examination, patient readiness, and results of return to sport functional testing performed in physical therapy.
Discussion
The surgical technique described in this Technical Note highlights an anatomic full-thickness ASTQA ACL reconstruction performed with a minimally invasive procedure and an all-inside technique using both proximal and distal adjustable loop fixation and I-STA. The use of combined femoral and tibial ALDs allows the graft to be retensioned after suture tape fixation and knee cycling. This ensures that the graft will be slightly more taut than the suture tape, which would allow the graft to take on all of the normal day-to-day loads that are crucial for adequate graft healing and ligamentization, with the tape then sharing the load during times of high stress to protect the graft from retear.9,10 This also mitigates the risk of “stress shielding” because the suture tape is completely independent of graft tensioning.
Because of normal anatomic shortening of the ACL from extension to flexion,14 both the final suture tape and graft fixation were done with the knee in hyperextension. Maintaining symmetric extension or hyperextension is important to consider because it may be favorable for long-term function to restore the patient’s normal kinematics to match that of the contralateral knee.
In conclusion, this Technical Note describes an all-inside ACL reconstruction using a full-thickness ASTQA with I-STA. The suture tape acts via a “safety-belt” mechanism that “catches” the graft during catastrophic loads that may otherwise have resulted in graft failure (Table 2).
Table 2.
Advantages and Disadvantages
| Advantages | Disadvantages |
|---|---|
|
|
|
|
|
|
|
ACL, anterior cruciate ligament; ALD, adjustable loop device.
Disclosures
The authors declare the following financial interests/personal relationships which may be considered as potential competing interests: P.A.S. has received consulting or advisory, funding grants, nonfinancial support, speaking and lecture fees, or travel reimbursement from Arthrex; has a patent issued to Arthrex; and is currently on the Education Committee for AANA. The other author (A.V.D.) declares that he has no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Supplementary Data
This technique describes a primary anterior cruciate ligament (ACL) reconstruction with a full-thickness all-soft-tissue quadriceps tendon autograft with additional suture tape augmentation. Here are our pertinent instructions. With the patient supine and the knee flexed to 100°, a marking pen is used to delineate a 3-cm vertical incision line starting from the suprapatellar pole extending proximally. Initial incision is done using a 10 blade, followed by further subcutaneous and peritenon dissection done with electrocautery, ultimately exposing the quad tendon. A 10-mm-wide double-knife blade, with a depth of 7 mm, is used starting at the suprapatellar pole and extending 65 mm proximally for initial graft width demarcation. A 10 blade is subsequently used to tease the distal portion of the quadriceps tendon off the suprapatellar pole. The teased-off portion of the tendon is tagged with a No. 2 suture. With tension on the suture limbs, a 10 blade is used to release the quadriceps tendon graft further both medially and laterally. This is also done to release the quad tendon graft further from the suprapatellar pole. The suture limbs are then passed through a “cigar cutter” device, which is then extended 65 mm proximally along the graft, ultimately amputating it. After thorough irrigation, the residual tendinous defect is closed using 5-6 No. 1 Vicryl sutures placed in an interrupted horizontal mattress fashion. The subcutaneous tissue is closed using No. 2-0 Monocryl, and a running subcuticular No. 2-0 Prolene suture is used for skin closure. With the knee flexed at 120°, a 7-mm offset guide is used to drill a pilot hole within the anteromedial bundle femoral footprint through the AM portal.
After inspection of the pilot hole, a calibrated measuring pin is drilled across the joint from the AM portal to measure intraosseous distance, and a low-profile 10-mm reamer is passed through the AM portal and drilled over the pin, exceeding the expected graft length in the femur by 4 to 5 mm. The pin is later used to pass a shuttle suture to the aperture of the femoral socket for later graft shuttling.
With the knee flexed to 80°, a tibial aiming device is positioned within the native ACL footprint. After tibial dissection, the guide sleeve is placed down to the bone and a FlipCutter is drilled through the center of the guide for optimal position within the joint. The FlipCutter is then opened to 10 mm in the tibial socket and is retro-cut to a depth exceeding the distal graft length by 4 to 5 mm to allow enough tunnel distance for graft re-tensioning to prevent the graft from “bottoming out.” A suture passer is passed through the tibial tunnel, and both the tibial and femoral shuttle sutures are retrieved through the AM portal. A measuring device is used to measure the intra-articular distance from the aperture of the femoral to the tibial socket. After obtaining the intraosseous and intra-articular distances, the graft, which has been prepared with a button-equipped femoral adjustable loop device (ALD) and a buttonless tibial ALD, is then marked accordingly. Importantly, the femoral shortening strands are marked distal to the button as the expected distance for the ALD button to flip on the femur, potentially to obviate the need for intraoperative fluoroscopy. The proximal graft is usually marked at 21 to 22 mm in the femoral socket with an intra-articular measurement of 20 to 21 mm, generally leaving 22 to 23 mm distally.
The femoral shuttle suture is used to pass the blue passing suture and the white shortening strands of the femoral ALD through the femoral tunnel. The femoral button is pulled with steady and even tension on all suture strands until it flips on the outer femoral cortex. The button is further seated by distally pulling on the free suture tape limbs. The graft is then hoisted to the measured femoral depth with the ALD’s femoral shortening strands, ensuring equal length of each shortening strand limb. The distal ALD, along with the free suture tape limbs, is shuttled distally through the tibial tunnel. The graft is then pulled into the tibial tunnel. On the tibial side, a 14-mm button is applied to the buttonless distal ALD, and the 2 distal tape limbs are passed through the 2 closed unoccupied holes of the distal button. The button is then brought down to the tibia with the knee held in hyperextension but the tibial end of the graft is not tightened at this time.
A 4.5-mm hole is drilled 1 cm distal to the button, which is subsequently tapped. The 2 tape ends are passed through a 4.75-mm anchor, and with the knee held in hyperextension, the suture-tape–loaded anchor is fixed in the distal hole. It is important to ensure that the 2 shortening strands are free between the tapes so that they can be used for retensioning later. After final suture tape fixation, attention is directed to tibial graft fixation. Tensioning handles are placed on the tibial shortening strands, which are then tensioned with the knee held in full hyperextension. The knee is then cycled 20 times to eliminate any residual creep in the final construct. Tensioning handles are placed on the femoral shortening strands, which are tensioned with the knee held again in full hyperextension. The tibial shortening strands are retensioned with the knee in full hyperextension. The tibial shortening strands are then tied over the button for backup fixation. After final construct fixation, stability testing is performed, followed by inspection of final graft positioning and tautness. The suture tape can be seen running posterior to the graft and is noted to be slightly lax in flexion. The knee is brought into hyperextension to assess for notch impingement. Additional notchplasty is usually unnecessary.
References
- 1.Johnsen M.B., Guddal M.H., Småstuen M.C., et al. Sport participation and the risk of anterior cruciate ligament reconstruction in adolescents: A population-based prospective cohort study (the Young-HUNT Study) Am J Sports Med. 2016;44:2917–2924. doi: 10.1177/0363546516643807. [DOI] [PubMed] [Google Scholar]
- 2.Sanders T.L., Maradit Kremers H., Bryan A.J., et al. Incidence of anterior cruciate ligament tears and reconstruction: A 21-year population-based study. Am J Sports Med. 2016;44:1502–1507. doi: 10.1177/0363546516629944. PMID: 26920430. [DOI] [PubMed] [Google Scholar]
- 3.Bram J.T., Magee L.C., Mehta N.N., Patel N.M., Ganley T.J. Anterior cruciate ligament injury incidence in adolescent athletes: A systematic review and meta-analysis. Am J Sports Med. 2021;49:1962–1972. doi: 10.1177/0363546520959619. [DOI] [PubMed] [Google Scholar]
- 4.Wiggins A.J., Grandhi R.K., Schneider D.K., Stanfield D., Webster K.E., Myer G.D. Risk of secondary injury in younger athletes after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Am J Sports Med. 2016;44:1861–1876. doi: 10.1177/0363546515621554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Runer A., Suter A., Roberti di Sarsina T., et al. Quadriceps tendon autograft for primary anterior cruciate ligament reconstruction show comparable clinical, functional, and patient-reported outcome measures, but lower donor-site morbidity compared with hamstring tendon autograft: A matched-pairs study with a mean follow-up of 6.5 years. J ISAKOS. 2023;8:60–67. doi: 10.1016/j.jisako.2022.08.008. [DOI] [PubMed] [Google Scholar]
- 6.Salmon L.J., Heath E., Akrawi H., Roe J.P., Linklater J., Pinczewski L.A. 20-year outcomes of anterior cruciate ligament reconstruction with hamstring tendon autograft: The catastrophic effect of age and posterior tibial slope. Am J Sports Med. 2018;46:531–543. doi: 10.1177/0363546517741497. [DOI] [PubMed] [Google Scholar]
- 7.Gornitzky A.L., Lott A., Yellin J.L., Fabricant P.D., Lawrence J.T., Ganley T.J. Sport-specific yearly risk and incidence of anterior cruciate ligament tears in high school athletes: A systematic review and meta-analysis. Am J Sports Med. 2016;44:2716–2723. doi: 10.1177/0363546515617742. [DOI] [PubMed] [Google Scholar]
- 8.Krebs N.M., Barber-Westin S., Noyes F.R. Generalized joint laxity is associated with increased failure rates of primary anterior cruciate ligament reconstructions: A systematic review. Arthroscopy. 2021;37:2337–2347. doi: 10.1016/j.arthro.2021.02.021. [DOI] [PubMed] [Google Scholar]
- 9.Bachmaier S., Smith P.A., Argintar E.H., Chahla J., Higgins L.D., Wijdicks C.A. Independent suture augmentation with all-inside anterior cruciate ligament reconstruction reduces peak loads on soft-tissue graft. A biomechanical full-construct study. Arthroscopy. 2022;38:88–98. doi: 10.1016/j.arthro.2021.09.032. [DOI] [PubMed] [Google Scholar]
- 10.Bachmaier S., Smith P.A., Bley J., Wijdicks C.A. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: A biomechanical full construct model. Arthroscopy. 2018;34:490–499. doi: 10.1016/j.arthro.2017.10.037. [DOI] [PubMed] [Google Scholar]
- 11.Daniel A.V., Wijdicks C.A., Smith P.A. Reduced incidence of revision anterior cruciate ligament reconstruction with internal brace augmentation. Orthop J Sports Med. 2023;11 doi: 10.1177/23259671231178026. [published online July 24, 2023] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Daniel A.V., Smith P.A. Less subsequent revision anterior cruciate ligament (ACL) reconstruction following primary bone-patellar tendon-bone ACL reconstruction with suture tape augmentation—A retrospective comparative therapeutic trial with 5-year follow-up. Arthroscopy. 2024;40:2455–2464. doi: 10.1016/j.arthro.2024.01.019. [DOI] [PubMed] [Google Scholar]
- 13.Daniel A.V., P.A, Smith Primary all-soft tissue quadriceps tendon autograft anterior cruciate ligament reconstruction with suture tape augmentation resulted in satisfactory patient outcomes and a low graft failure rate in high school and collegiate athletes. Arthroscopy. 2025;41:95–105. doi: 10.1016/j.arthro.2024.02.047. [DOI] [PubMed] [Google Scholar]
- 14.Marieswaran M., Jain I., Garg B., Sharma V., Kalyanasundaram D. A review on biomechanics of anterior cruciate ligament and materials for reconstruction. Appl Bionics Biomech. 2018;2018 doi: 10.1155/2018/4657824. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
This technique describes a primary anterior cruciate ligament (ACL) reconstruction with a full-thickness all-soft-tissue quadriceps tendon autograft with additional suture tape augmentation. Here are our pertinent instructions. With the patient supine and the knee flexed to 100°, a marking pen is used to delineate a 3-cm vertical incision line starting from the suprapatellar pole extending proximally. Initial incision is done using a 10 blade, followed by further subcutaneous and peritenon dissection done with electrocautery, ultimately exposing the quad tendon. A 10-mm-wide double-knife blade, with a depth of 7 mm, is used starting at the suprapatellar pole and extending 65 mm proximally for initial graft width demarcation. A 10 blade is subsequently used to tease the distal portion of the quadriceps tendon off the suprapatellar pole. The teased-off portion of the tendon is tagged with a No. 2 suture. With tension on the suture limbs, a 10 blade is used to release the quadriceps tendon graft further both medially and laterally. This is also done to release the quad tendon graft further from the suprapatellar pole. The suture limbs are then passed through a “cigar cutter” device, which is then extended 65 mm proximally along the graft, ultimately amputating it. After thorough irrigation, the residual tendinous defect is closed using 5-6 No. 1 Vicryl sutures placed in an interrupted horizontal mattress fashion. The subcutaneous tissue is closed using No. 2-0 Monocryl, and a running subcuticular No. 2-0 Prolene suture is used for skin closure. With the knee flexed at 120°, a 7-mm offset guide is used to drill a pilot hole within the anteromedial bundle femoral footprint through the AM portal.
After inspection of the pilot hole, a calibrated measuring pin is drilled across the joint from the AM portal to measure intraosseous distance, and a low-profile 10-mm reamer is passed through the AM portal and drilled over the pin, exceeding the expected graft length in the femur by 4 to 5 mm. The pin is later used to pass a shuttle suture to the aperture of the femoral socket for later graft shuttling.
With the knee flexed to 80°, a tibial aiming device is positioned within the native ACL footprint. After tibial dissection, the guide sleeve is placed down to the bone and a FlipCutter is drilled through the center of the guide for optimal position within the joint. The FlipCutter is then opened to 10 mm in the tibial socket and is retro-cut to a depth exceeding the distal graft length by 4 to 5 mm to allow enough tunnel distance for graft re-tensioning to prevent the graft from “bottoming out.” A suture passer is passed through the tibial tunnel, and both the tibial and femoral shuttle sutures are retrieved through the AM portal. A measuring device is used to measure the intra-articular distance from the aperture of the femoral to the tibial socket. After obtaining the intraosseous and intra-articular distances, the graft, which has been prepared with a button-equipped femoral adjustable loop device (ALD) and a buttonless tibial ALD, is then marked accordingly. Importantly, the femoral shortening strands are marked distal to the button as the expected distance for the ALD button to flip on the femur, potentially to obviate the need for intraoperative fluoroscopy. The proximal graft is usually marked at 21 to 22 mm in the femoral socket with an intra-articular measurement of 20 to 21 mm, generally leaving 22 to 23 mm distally.
The femoral shuttle suture is used to pass the blue passing suture and the white shortening strands of the femoral ALD through the femoral tunnel. The femoral button is pulled with steady and even tension on all suture strands until it flips on the outer femoral cortex. The button is further seated by distally pulling on the free suture tape limbs. The graft is then hoisted to the measured femoral depth with the ALD’s femoral shortening strands, ensuring equal length of each shortening strand limb. The distal ALD, along with the free suture tape limbs, is shuttled distally through the tibial tunnel. The graft is then pulled into the tibial tunnel. On the tibial side, a 14-mm button is applied to the buttonless distal ALD, and the 2 distal tape limbs are passed through the 2 closed unoccupied holes of the distal button. The button is then brought down to the tibia with the knee held in hyperextension but the tibial end of the graft is not tightened at this time.
A 4.5-mm hole is drilled 1 cm distal to the button, which is subsequently tapped. The 2 tape ends are passed through a 4.75-mm anchor, and with the knee held in hyperextension, the suture-tape–loaded anchor is fixed in the distal hole. It is important to ensure that the 2 shortening strands are free between the tapes so that they can be used for retensioning later. After final suture tape fixation, attention is directed to tibial graft fixation. Tensioning handles are placed on the tibial shortening strands, which are then tensioned with the knee held in full hyperextension. The knee is then cycled 20 times to eliminate any residual creep in the final construct. Tensioning handles are placed on the femoral shortening strands, which are tensioned with the knee held again in full hyperextension. The tibial shortening strands are retensioned with the knee in full hyperextension. The tibial shortening strands are then tied over the button for backup fixation. After final construct fixation, stability testing is performed, followed by inspection of final graft positioning and tautness. The suture tape can be seen running posterior to the graft and is noted to be slightly lax in flexion. The knee is brought into hyperextension to assess for notch impingement. Additional notchplasty is usually unnecessary.