Abstract
Background
Dental caries is one of the most common global childhood diseases and is, for the most part, entirely preventable. Good oral health is dependent on the establishment of the key behaviours of toothbrushing with fluoride toothpaste and controlling sugar snacking. Primary schools provide a potential setting in which these behavioural interventions can support children to develop independent and habitual healthy behaviours.
Objectives
To assess the clinical effects of school‐based interventions aimed at changing behaviour related to toothbrushing habits and the frequency of consumption of cariogenic food and drink in children (4 to 12 year olds) for caries prevention.
Search methods
We searched the following electronic databases: the Cochrane Oral Health Group's Trials Register (to 18 October 2012), the Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library 2012, Issue 4), MEDLINE via OVID (1948 to 18 October 2012), EMBASE via OVID (1980 to 18 October 2012), CINAHL via EBSCO (1981 to 18 October 2012) and PsycINFO via OVID (1950 to 18 October 2012). Ongoing trials were searched for using Current Controlled Trials (to 18 October 2012) and ClinicalTrials.gov (to 18 October 2012). Conference proceedings were searched for using ZETOC (1993 to 18 October 2012) and Web of Science (1990 to 18 October 2012). We searched for thesis abstracts using the Proquest Dissertations and Theses database (1950 to 18 October 2012). There were no restrictions regarding language or date of publication. Non‐English language papers were included and translated in full by native speakers.
Selection criteria
Randomised controlled trials of behavioural interventions in primary schools (children aged 4 to 12 years at baseline) were selected. Included studies had to include behavioural interventions addressing both toothbrushing and consumption of cariogenic foods or drinks and have a primary school as a focus for delivery of the intervention.
Data collection and analysis
Two pairs of review authors independently extracted data related to methods, participants, intervention design including behaviour change techniques (BCTs) utilised, outcome measures and risk of bias. Relevant statistical information was assessed by a statistician subsequently. All included studies contact authors were emailed for copies of intervention materials. Additionally, three attempts were made to contact study authors to clarify missing information.
Main results
We included four studies involving 2302 children. One study was at unclear risk of bias and three were at high risk of bias. Included studies reported heterogeneity in both the intervention design and outcome measures used; this made statistical comparison difficult. Additionally this review is limited by poor reporting of intervention procedure and design. Several BCTs were identified in the trials: these included information around the consequences of twice daily brushing and controlling sugar snacking; information on consequences of adverse behaviour and instruction and demonstration regarding skill development of relevant oral health behaviours.
Only one included study reported the primary outcome of development of caries. This small study at unclear risk of bias showed a prevented fraction of 0.65 (95% confidence interval (CI) 0.12 to 1.18) in the intervention group. However, as this is based on a single study, this finding should be interpreted with caution.
Although no meta‐analysis was performed with respect to plaque outcomes (due to differences in plaque reporting between studies), the three studies which reported plaque outcomes all found a statistically significant reduction in plaque in the intervention groups with respect to plaque outcomes. Two of these trials involved an 'active' home component where parents were given tasks relating to the school oral health programme (games and homework) to complete with their children. Secondary outcome measures from one study reported that the intervention had a positive impact upon children's oral health knowledge.
Authors' conclusions
Currently, there is insufficient evidence for the efficacy of primary school‐based behavioural interventions for reducing caries. There is limited evidence for the effectiveness of these interventions on plaque outcomes and on children's oral health knowledge acquisition. None of the included interventions were reported as being based on or derived from behavioural theory. There is a need for further high quality research to utilise theory in the design and evaluation of interventions for changing oral health related behaviours in children and their parents.
Keywords: Child; Child, Preschool; Humans; Schools; Candy; Candy/adverse effects; Carbonated Beverages; Carbonated Beverages/adverse effects; Cariogenic Agents; Cariogenic Agents/adverse effects; Dental Caries; Dental Caries/etiology; Dental Caries/prevention & control; Dental Plaque; Dental Plaque/etiology; Dental Plaque/prevention & control; Oral Hygiene; Oral Hygiene/methods; Randomized Controlled Trials as Topic; Toothbrushing; Toothbrushing/methods
Plain language summary
Programmes based in primary schools designed to help prevent tooth decay by changing children's behaviour
Improving the dental health of children is a global public health priority. Currently 60% to 90% of 5‐year olds worldwide suffer from tooth decay. Understanding how to intervene early with respect to establishing good dental health habits requires an understanding of the key behaviours which either help prevent decay (toothbrushing, twice a day with a fluoride‐based toothpaste) or encourage decay (sugar snacking) in children's teeth. Primary schools provide a setting in which behavioural interventions designed to encourage and establish good toothbrushing and snacking habits can be tested.
This review examined how successful the interventions in the suitable studies were in improving dental health in children aged from 4 to 12 years. The latest search of relevant studies was carried out on 18th October 2012.
Interventions were programmes that enabled children to.
∙ Making lasting changes to toothbrushing habits. ∙ Reduce the amount and how often food and drink known to cause tooth decay were consumed.
The trials had to include an educational element which taught skills or gave instructions and one or more accepted techniques to change behaviour.
Out of 1518 possible studies found only four were sufficiently relevant and of high enough quality to be included in this review. One small study showed that children who received the behavioural intervention developed fewer caries during the study. Three studies showed that there was less dental plaque (better oral hygiene) in the children in the behavioural intervention groups. More research is needed to confirm these findings.
The dental health of 4 to 12 year olds is an important issue ‐ reducing the amount of decay in this group would have a positive impact on overall health, particularly for those living in the poorest communities. More high quality research with well designed programmes will help to establish which techniques are most effective at changing child and parent behaviour to encourage good toothbrushing and discourage sugar snacking.
Summary of findings
for the main comparison.
| Behavioural intervention compared with control for prevention of caries in children | ||||
|
Patient or population: Children aged 4 to 12 years Settings: Primary school Intervention: Behavioural intervention (both oral hygiene and dietary components) Comparison: No intervention or delayed intervention | ||||
| Outcomes | Relative effect (95% confidence interval (CI)) | No of participants (studies) | Quality of the evidence (GRADE) | Comments |
|
Caries ‐ DMFS (prevented fraction (PF)) Follow‐up: 15 months |
PF = 0.65 (95% CI 0.12 to 1.18) | 60 participants (1 RCT) | ⊕⊕⊝⊝ low1 | Small study of children at high risk of caries |
|
Plaque indices Follow‐up: 3 to 15 months |
All 3 RCTs showed a reduction in plaque in the intervention group compared to control group | 827 participants (3 RCTs) | ⊕⊕⊝⊝ low2 | Data not suitable for meta‐analysis |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 Quality of the evidence was downgraded for risk of bias (unclear allocation concealment) and imprecision.
2 Quality of the evidence was downgraded for risk of bias (1 trial unclear and 2 trials high risk of bias) and inconsistency (heterogeneity due to differences in design, intervention and outcome measurement).
Background
Description of the condition
Oral diseases are common in many societies globally, with dental caries being the most prevalent chronic disease among children (Gussy 2006). Dental caries is present in low‐income, middle‐income and high‐income countries; between 60% and 90% of children in industrialised countries are affected (Petersen 2005). The US Surgeon General report on oral health (Surgeon General 2000) states that oral health problems are five times more likely to occur in children than asthma and seven times more than hay fever. Dental caries is a debilitating condition that can cause a child to suffer a significant degree of pain (Edelstein 2000) and if left untreated the disease may lead to further complications including sepsis (Pine 2006). Severe untreated caries has also been found to have links to general health and well being, affecting young children's body weight and growth (Sheiham 2006). Additionally, good oral health is important in terms of the psychosocial factors which relate to quality of life (Sheiham 2005) and optimum social functioning (Exley 2009) including self expression and communication. The mouth is a highly visible facial feature in most cultures (Goffman 1990). Discoloured and missing teeth have negative connotations in modern culture, being predominantly associated with unhygienic and undesirable lifestyles (Exley 2009) and with severe deprivation (Gibson 2008). Additionally, children who experience dental pain may lose time at school (Jackson 2011) and have difficulties sleeping, eating and playing (Casamassimo 2009). Being prevented from taking part in these and other normal recreational social activities with family and friends may have a detrimental effect on the child's social development and overall well being.
Brought about by dietary factors (such as frequent consumption of sugar) and exacerbated by inadequate oral hygiene routines (lack of brushing with fluoride toothpaste), caries is virtually completely preventable (Edelstein 2006). The impact of dental caries can be extensive and enduring for the child, sometimes impacting on their adult life (Nunn 2006) and potentially, future generations (Amin 2009).
Improving and promoting oral health has become common practice worldwide, both at local and population levels. Oral health is influenced by a myriad of interconnected variables, including socioeconomic status (SES) (Reisine 2001), ethnicity (Shiboski 2003) and attitudes (Blinkhorn 2001) which potentially have a cumulative effect and appear to be most profound in materially and socially deprived populations.
Rates of caries among children in many parts of the world have improved dramatically since the introduction of fluoridated toothpastes in the 1970s (Mullen 2005). Yet while child dental health has improved overall in recent years the gap between the most and least deprived children continues to widen (Armfield 2009; Watt 1999; Watt 2007), suggesting that relative poverty is a moderating factor in terms of rates of dental caries. Children from disadvantaged communities and some ethnic minorities have the highest rates of dental caries. This is particularly significant in light of observed increases in ethnic minorities among some communities and in the interest of halting and reversing the magnification of disparities throughout low SES groups (Pine 2004a).
Description of the intervention
Improving and promoting oral health has become common practice worldwide both at local and population levels. Establishing good routines in childhood is vital for optimum oral health as these behaviours, once established, can endure throughout adulthood (Aunger 2007) and provide lifelong protection against caries (Ramos‐Gomez 2002). Intervention studies related to child oral health have aimed to reduce childhood caries by encouraging children to establish and maintain effective oral health routines (e.g. Worthington 2001). Behaviour change interventions have utilised a number of evidence‐based behavioural change techniques (Michie 2008) including: goal setting, goal review, monitoring specified behaviours, coping planning/strategies, instruction, behavioural rehearsal, homework tasks and reinforcement. The experience of distressing dental treatment in childhood can result in dental fears and phobias which can progress into adulthood (Brukiene 2006). Dental anxiety is a commonly cited reason for adults refusing to attend routine oral health checks with a dentist. Non‐attendance can have a detrimental effect on oral health status (Eitner 2006) and may result in an increased number of patients requiring significant treatment. The cost of treating these patients creates a significant financial burden on the health services, both in terms of the cost of the treatment itself and in dealing with anxious patients. Oral health interventions early on in life could potentially save costs and avoid anxiety among patients later in life.
Patterns of behaviour conducive to positive dental outcomes are not always achieved in the home and this may be attributed to a variety of interconnected variables including SES (Shaw 2009) and cultural factors. For this reason and in the interest of reducing dental health inequalities, it remains necessary to provide effective interventions at the population level.
Primary schools, because of their inclusive nature, provide a suitable environment for dental health behavioural interventions (Kwan 2005). Interventions for preventing caries, which take place in primary schools, are potentially too late to prevent early childhood caries (ECC), particularly in its initial stages. However, targeting interventions at children earlier will reduce the effectiveness of interventions; that is to say, children develop the motor control necessary for effective toothbrushing more fully when they are primary school aged. Additionally children are unlikely to have sufficient control over routines in the home whilst they are very young. It is therefore inappropriate to target interventions for preventing caries (or ECC) at preschool age children (as opposed to targeting their parents).
Behaviours and routines are developed and become established during childhood, and as a result they become more difficult to alter in adulthood due to formed habits and automatic behaviour. Between the ages of 5 and 8 years children progress developmentally in many areas. To facilitate habitual tooth cleaning it is important to ensure the behaviour is established by the end of this life stage. Oral health programmes may be especially relevant at primary school level, particularly for children in their eighth year of life as this is considered to be a latency phase in which the child is more open to absorbing information about how to care for their body (Graham 2005).
Although brushing at home twice a day is optimum, many children do not do this. School‐based interventions not only offer children supervised brushing once a day, they also offer training in a skill that may not be being taught in the home. Although an artificial setting, which may not reproduce individual behavioural triggers for incorporating toothbrushing into a personal morning and evening hygiene routine at home, school‐based interventions facilitate the teaching of toothbrushing as a skill. Additionally, there is potential for translating these behaviours into the home environment on a twice daily basis. In spite of the increase in the number of school‐based oral health programmes in recent years, the majority of school‐based oral health interventions have not produced sustained behavioural change. A systematic review of oral health interventions (Kay 1996; Kay 1998) and a subsequent review by Watt 2001 found there to be an improvement in oral health knowledge but not in the related attitudes, beliefs and behaviours.
Parental habits impact on child behaviour, particularly through modelling actions. However, a parent's perception of their own ability to deliver the behaviour of regular toothbrushing (self efficacy) can also significantly impact on child dental health (Pine 2004b). Primary school‐based interventions rarely target both child and parent behaviour, or parental self efficacy. It remains crucial to the development of effective primary school‐based interventions that specific cultural components around self efficacy are identified so that they can be further refined if necessary and replicated in future interventions.
How the intervention might work
Primary school‐based interventions aiming to improve child oral health may disseminate education and information around developing skills for toothbrushing and managing the consumption of cariogenic foods and drinks. In addition they can provide support to parents and family to facilitate both behaviours occurring at home. This may be achieved through task‐specific behavioural rehearsal and reinforcement and through the application of other documented behaviour change techniques (BCTs). The overall outcome may be to increase child and parental self efficacy for oral health behaviours.
Why it is important to do this review
In many countries, primary schools have a recognised duty to deliver health education of which oral health education and the associated behavioural skills are often components. The purpose of this systematic review is to effectively evaluate research on behavioural interventions delivered in primary schools and to provide an understanding of the components and mechanisms of successful interventions which produce lasting behaviour change concerning toothbrushing and controlling the consumption of cariogenic foods and drinks.
Research has repeatedly found significant associations between SES and caries prevalence. The burden of oral ill‐health is such that it remains crucial to provide every child and their family with the knowledge and behavioural skills necessary to maintain a healthy dental lifestyle in the long term.
Objectives
To assess the clinical effects, in terms of caries prevention, of school‐based interventions aimed at changing behaviour related to toothbrushing habits and the frequency of consumption of cariogenic food and drink in children (4 to 12 year olds).
Methods
Criteria for considering studies for this review
Types of studies
Randomised controlled trials (RCTs) where randomisation occurs at the level of the group (cluster by school and/or class) or individual children were included. All other studies were excluded during the screening process or at the point of data extraction.
Types of participants
Children within the age range of 4 to 12 years at the start of the study and attending a primary/elementary/infant or junior school in any country were included. Inclusion was irrespective of dental caries level at the start of the study, fluoride exposure, both topical (e.g. toothpaste, tablets, milk) and via water (both naturally occurring and added), current dental treatment and attendance levels, and nationality. Studies not predominantly taking place in a school setting were also excluded due to the focus of the current review. The review included studies regardless of whether teaching staff or peers were included in the delivery of the intervention.
For the purposes of this review, a 'school' is defined as a place delivering curricular primary education, to children aged between 4 and 12 years. Primary school encompassed the terms: junior, elementary, infant, kindergarten, community and nursery within the specified age range.
Types of interventions
Test or intervention group
Behavioural interventions (including education and/or skills and/or behaviour change) taking place in a school setting around oral health and/or hygiene and frequency of cariogenic food and drink consumption. Studies were included with or without a follow‐up period after the completion of the intervention.
Interventions for inclusion in this review were required to:
have a focus around toothbrushing and cariogenic foods;
use schools as the focal site for intervention delivery;
contain skills, instructions and educational components.
The intervention may be delivered by teachers, dental health professionals, peers, or other educators and must be delivered principally in the school the children are attending. Elements of the intervention may also occur in the home and in clinical settings. Delivery of intervention components can be written, verbal, web‐based or through electronic devices (e.g. video games).
The aim of the intervention must be to improve child oral health. Studies utilising one or more behaviour change techniques (BCTs) were included in the review. Behavioural interventions were coded using the Coding Manual to Identify Behaviour Change Techniques in Behaviour Change Intervention Descriptions, detailed by Abraham 2008. This provided a pre‐validated method to code specific BCTs in interventions. Examples of BCTs that may be included are: reinforcement (brushing charts), modelling (facilitator demonstration of correct brushing technique) and prompts and cues (visual reminders in appropriate settings).
Control group
The control group should receive usual curriculum‐based health education programmes; these may be defined as standard health information and education offered as part of the school curriculum and independent of the study intervention (non‐intervention control). Control groups may also be waiting list control groups.
Exclusion criteria
Studies were excluded where:
the intervention was a change at the level of the school environment ‐ such as change in foods and drinks available in schools;
the intervention was within a nursery school but targeting only children aged 3 to 5 years old.
Types of outcome measures
Primary outcomes
Changes in caries increment measured by the difference in decayed, missing and filled teeth (dmft/DMFT).
Changes in caries increment on tooth surfaces (dmfs/DMFS).
Changes in plaque scores for permanent and deciduous teeth over the course of the intervention and the follow‐up period.
Primary outcomes for both permanent and deciduous teeth were considered if they measured change from baseline for the same cohort of children. For the purposes of this review, clinical effectiveness is defined as either a change in caries experience (decayed, missing or filled teeth ‐ dmft/DMFT) and/or a change in the amount of dental plaque.
Secondary outcomes
Frequency of toothbrushing: measured using reported data correlated with clinical measures.
Frequency of cariogenic food and drink consumption: reported behaviour.
Behavioural outcomes: reported and/or other measures (e.g. data tracking toothbrushes and collecting food wrappers).
Changes in dental attendance (i.e. frequency of dental check‐ups, increase in dental attendance) during the period of the intervention.
Adverse events were recorded using data extraction forms if they were reported. These were considered by the review team.
Search methods for identification of studies
For the identification of studies included or considered for this review, detailed search strategies were developed for each database searched. These were based on the search strategy for MEDLINE but revised appropriately for each database to take account the differences in controlled vocabulary and syntax rules. No restriction on the language of publication was applied to the inclusion criteria.
The search strategy combined the subject search with the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying reports of randomised controlled trials as published in box 6.4.c in the Cochrane Handbook for Systematic Reviews of Interventions version 5.1.0 (updated March 2011) (Higgins 2011).
Electronic searches
The following databases were searched:
The Cochrane Oral Health Group's Trials Register (to 18 October 2012) (Appendix 1)
The Cochrane Central Register of Controlled Trials (CENTRAL) (The Cochrane Library, 2012, Issue 4) (Appendix 2)
MEDLINE via OVID (1948 to 18 October 2012) (Appendix 3)
EMBASE via OVID (1980 to 18 October 2012) (Appendix 4)
CINAHL via EBSCO (1981 to 18 October 2012) (Appendix 5)
PsycINFO via OVID (1950 to 18 October 2012) (Appendix 6)
Current Controlled Trials (to 18 October 2012) (Appendix 7)
ClinicalTrials.gov (to 18 October 2012) (Appendix 8)
ZETOC (limited to Conference Proceedings) (1993 to 18 October 2012) (Appendix 9)
Web of Science (limited to Conference Proceedings) (1990 to 18 October 2012) (Appendix 10)
Dissertations and Theses via Proquest (1950 to 18 October 2012) (Appendix 11).
Searching other resources
In addition to conducting systematic searches of electronic databases, handsearches of appropriate journals were conducted where these have not already been searched as part of the Cochrane Journal Handsearching Programme. The following journals have all been identified as those in which trials in the field are likely to be reported:
Acta Odontologica Scandinavica (2004 to October 2012)
ASDC Journal of Dentistry for Children (2004 to October 2012)
British Dental Journal (2006 to October 2012)
Caries Research (2004 to October 2012)
Community Dental Health (2003 to October 2012)
Community Dentistry and Oral Epidemiology (2003 to October 2012)
Journal of the American Dental Association (2005 to October 2012)
Journal of Dental Research (2005 to October 2012)
Journal of Public Health Dentistry (2004 to October 2012)
Swedish Dental Journal (2002 to October 2012)
International Journal of Paediatric Dentistry (2000 to October 2012).
Data collection and analysis
Selection of studies
Citations retrieved were screened for relevance by five review authors independently on titles, keywords and abstracts. For studies where there was insufficient evidence in the title, keywords or abstracts, or the review team did not agree on the inclusion/exclusion of the report, the full study/paper was obtained. References screened as relevant for the review were obtained in full and assessed for inclusion in the review. If disagreement arose, other review authors were consulted to resolve this; such occurrences were documented.
All included studies were subject to a cited reference search aimed at identifying any related publications.
Data extraction and management
Four review authors extracted data for all included studies. The review authors worked in pairs and any discrepancies arising were discussed by the team. Prior to use, the data extraction form was piloted on a sample of articles to allow for any necessary modifications. Following Cochrane guidelines, details of why studies failed to meet the review criteria were documented and are presented in the Characteristics of excluded studies table.
For each included study we recorded the following data.
Study identification code.
Number of reports on study.
Year study commenced and finished.
Trial funding, number of sites on which the study has been conducted.
Method: study design, type of randomisation, duration of study.
Participants: recruitment, inclusion/exclusion, demographic characteristics, baseline fluoride exposure and dental health data (dmft, dmfs).
Intervention: description of the programme including intervention facilitator, specific BCTs and components utilised as outlined in the Taxonomy of Behavioural Change Techniques Used in Interventions (Abraham 2008). Information on specific theoretical health models that had been reported to inform the intervention design was also recorded.
Control group(s): number of points of contact with researchers and details.
Outcome measures and outcome data collection time points as reported.
Adverse effects.
Analysis details.
Rates of attrition.
Follow‐ups, including time intervals.
Risk of bias.
Risk of bias specific to cluster randomised trials: recruitment bias, baseline imbalance, loss of cluster, incorrect analyses and comparability with individual randomised trials.
Assessment of risk of bias in included studies
The recommended method for assessing the risk of bias in studies included in Cochrane reviews, set out in chapter 8 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) was applied.
This is a two‐part tool, addressing seven specific domains (namely sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective outcome reporting and 'other bias'). Each domain includes one or more specific entries in a risk of bias table. Within each entry, the first part of the tool involves describing what was reported to have happened in the study. The second part of the tool involves assigning a judgement relating to the risk of bias for that entry. This is achieved by assigning a judgement of 'Low risk' of bias, 'High risk' of bias, or 'Unclear risk' of bias. The risk of bias assessment was undertaken independently and in duplicate by four review authors in total as part of the data extraction process. Where a consensus was not reached, methods experts within the group were consulted.
After taking into account the additional information provided by the authors of the trials, studies were grouped into the following categories.
Low risk of bias (plausible bias unlikely to seriously alter the results) for all key domains.
Unclear risk of bias (plausible bias that raises some doubt about the results) if one or more key domains were assessed as unclear.
High risk of bias (plausible bias that seriously weakens confidence in the results) if one or more key domains were assessed to be at high risk of bias.
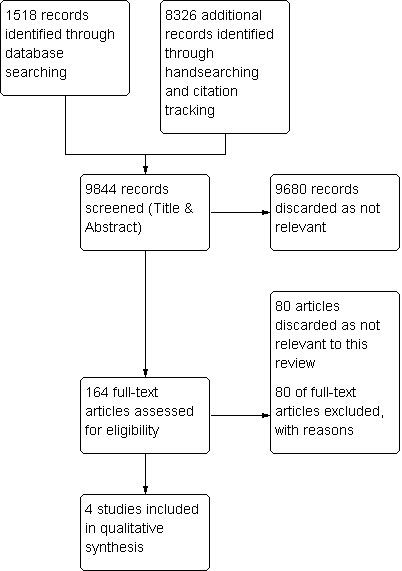
A risk of bias table (Characteristics of included studies) was completed for each included study and the results are presented graphically (Figure 1; Figure 2).
1.

Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
2.
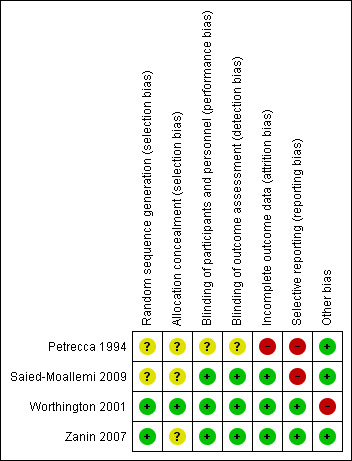
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Measures of treatment effect
Dichotomous data were not reported. Although Zanin 2007 reported on prevalence rates, caries increment was calculated.
In dealing with caries increment data, the mean difference and standardised mean difference were calculated and taken as the summary statistic. If multiple studies reporting a variety of measures (dmft, dmfs etc.) had been included in this review, the prevented fraction (i.e. mean caries increment in the treatment group subtracted from that of the control group and divided by the mean increment in the control group) would have been calculated. Use of prevented fraction allows for a more reliable examination of heterogeneity between trials.
Unit of analysis issues
The review included cluster randomised controlled trials, where schools or classes are the unit subject to randomisation. Where appropriate, intra‐cluster correlation coefficients (ICC) were used to estimate variability between and within clusters as detailed in section 16.3 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). Methods of analysis and reporting were reviewed for appropriateness by a review author expert in these methods (Girvan Burnside (GB)).
Dealing with missing data
If data were unavailable and clarification required (e.g. study characteristics and numerical outcome data), corresponding authors of studies were contacted directly in order to obtain missing information.
Where authors could not be contacted, missing standard deviations were estimated using intention‐to‐treat (ITT) analyses when primary outcome data or participant attrition data are missing.
Assessment of heterogeneity
Where there was poor overlap of confidence intervals of the individual studies, assessments of heterogeneity were carried out using the Chi2 test and the I2 statistic. The I2 statistic was interpreted according to the guide provided in section 9.5 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011), the magnitude and direction of effects and alongside the P value of the Chi2 test. Sources of heterogeneity were explored where the I2 statistic exceeds 25%. If there was unexplained heterogeneity, a meta‐analysis was not conducted.
Assessment of reporting biases
The impact of reporting bias was minimised by undertaking comprehensive searches of multiple sources (including trial registries), increasing efforts to identify unpublished material and including non‐English language publications. Efforts were also made to identify outcome reporting bias in studies by recording all outcomes, planned and reported, and noting where there were missing outcomes. Where evidence of missing outcomes was found, attempts were made to obtain any available data direct from the study authors.
Data synthesis
For the primary outcome variable, the treatment effect was assessed by calculating the relative effect as indicted by the prevented fraction (PF): the mean caries increment in controls minus mean caries increment in the intervention group, divided by the mean caries increment in controls. For the included study, the 95% confidence interval of the PF was calculated.
Each included study was summarised and described according to participant and intervention characteristics and outcomes.
Subgroup analysis and investigation of heterogeneity
Subgroup analyses were planned on the basis of:
age: 4 to 7 years and 8 to 12 years (best practice advice on child age associated competencies for effective toothbrushing; i.e. it is advised that parents undertake or supervise toothbrushing for children under 7 years);
number of BCTs applied as denoted in the Taxonomy of Behavioural Change Techniques Used in Interventions (Abraham 2008);
frequency and duration of exposure to the intervention; and
gender.
A test to determine the interaction between the subgroup estimates was planned.
Sensitivity analysis
Sensitivity analysis was planned on:
risk of bias assessment;
random‐effects modelling;
ICCs estimates where these values were missing in studies.
Only studies at low risk of bias were included in the final analysis.
Results
Description of studies
Further descriptions of the studies can be found in the Characteristics of included studies tables. The following section summarising key aspects of the studies.
Results of the search
The processing of the references identified through electronic searches, handsearches and citation tracking is described in Figure 3. After de‐duplication of the results from electronic searching there were 1518 records. A further 8326 records were identified through handsearching and citation tracking (total 9844). Based on the screening of the title and abstracts (Sarah Elison (SE), Lucy O'Malley (LO), Pauline Adair (PA), Rosemary Armstrong (RA), Anna Cooper (AC)), 9680 records were discarded as irrelevant to this review. Articles were rejected on initial screening if the review author could determine from the title and abstract the article did not meet the inclusion criteria. The review authors assessed full‐text copies of 84 articles (SE, LO, PA, RA, AC). Two review authors (Lindsey Dugdill (LD), AC) independently double screened all citations once the initial screening had been completed. Sixty‐four references were discarded as not relevant. Subsequently, 20 articles were indicated as having potentially met the inclusion criteria and were subjected to full data extraction. During this phase, 16 articles were deemed not to have the distinct elements of the intervention that targeted cariogenic food (in addition to toothbrushing) or the study, upon further examination, was found not to be an RCT. In one case, a study was deemed to be so poorly reported that it could not be included in this review.
3.
Review flow diagram.
Included studies
Characteristics of the trial design and setting
Two studies were cluster randomised at the level of the school (Saied‐Moallemi 2009; Worthington 2001); with the remaining two trials randomised at the level of the individual (Petrecca 1994; Zanin 2007). One study was conducted in South America (Brazil) Zanin 2007, two in Europe, Petrecca 1994 in Italy and Worthington 2001 in the UK and one in Asia, Saied‐Moallemi 2009 in Tehran.
Sample size: In total 2302 children participated in the four studies, of these 1529 children were subject to behavioural interventions and 773 children acted as controls. Sample sizes ranged from 30 (Zanin 2007) to over 400 per group (Petrecca 1994). For a more detailed breakdown of sample size per study please refer to the Characteristics of included studies tables. Two studies reported that power calculations were conducted to inform the sample size (Saied‐Moallemi 2009; Zanin 2007), the remaining two studies did not report how the sample size was arrived at.
Of the included studies, two did not state the source of trial funding, the study by Saied‐Moallemi 2009 was supported by the Iran Centre for Dental Research and the other study by the National Sugar Bureau (Worthington 2001).
Characteristics of the participants
4 to 7 year olds (baseline)
One study was conducted with children aged 4 to 7 years (Zanin 2007). The intervention reported by Zanin 2007, taught an age‐appropriate modified toothbrushing technique to the children. This was done through instruction and demonstration. The technique took into account the limited motor control of children at this age and aimed to improve the children's plaque removal ability. Supervised brushing sessions took place every 3 months. In addition, the intervention involved educational elements which covered dental hygiene and consumption of cariogenic food and drink.
8 to 12 year olds (baseline)
Two studies were conducted with children aged 8 to 12 years (Saied‐Moallemi 2009; Worthington 2001). They were both delivered and monitored by dental professionals, with one involving teachers alongside dental professionals (Saied‐Moallemi 2009). Both linked the school programme to the home with varying levels of parental involvement.
Age at baseline unclear
Petrecca 1994 only reported that children at baseline were within primary school age and specified at baseline they were in primary school years one to three. Based on the current Italian school system, this may indicate that the children were aged between 6 and 9 years at baseline, however it is important to note that this cannot be confirmed. Attempts to make contact with the authors were unsuccessful. The intervention was aimed at children and teachers; diagrams and plastic models were used to explain caries to the children and to teach them oral (including dietary) hygiene. Children were asked every 30 days if they were following the oral (and dietary) hygiene regimen. Teachers were involved in the delivery of the intervention. A second intervention group had the same educational programme plus daily fluoride tablets (1 mg).
The number of boys and girls within each group was not outlined in two studies (Petrecca 1994; Zanin 2007). One study randomised eight boys and eight girls schools separately to include two schools of each gender within each of the four clusters (Saied‐Moallemi 2009 ). The remaining study (Worthington 2001) had an overall equal number of girls and boys in intervention and control groups (based on information from Hill 1999).
One study (Petrecca 1994) excluded children who were either unable to follow the instructions provided or had not taken their fluoride tablets. All children within the research area were given the opportunity to participate in the intervention reported by Worthington 2001. This was facilitated by the design with only those with positive consent being sampled for a clinical examination. One study (Zanin 2007) reported that children were excluded from the study at baseline if they were showing signs of severe fluorosis, hypoplasia, or systemic alteration. Children were also excluded from this study if they had fixed braces. One study did not report any exclusion criteria (Saied‐Moallemi 2009).
Characteristics of the interventions
In all cases, interventions took the form of educational programmes, broken down into a series of classroom‐based lessons. Lessons were designed to fit into the UK national curriculum in one study (Worthington 2001). Details of the design of the interventions of the remaining studies were not reported. All interventions included toothbrushing instruction and skill lessons and information on the use of fluoride toothpaste. Supervised toothbrushing practice sessions with the children were carried out in two of the interventions (Worthington 2001; Zanin 2007). Although all interventions included dietary elements (as per inclusion criteria), the strength of this component varied across the interventions. Information around dietary effects was provided through group discussion (Worthington 2001) or lessons (Zanin 2007), or via instruction (Petrecca 1994) and in one study was provided only through leaflets or worksheets (Saied‐Moallemi 2009). In all studies, it appeared that the dietary elements came secondary to dental hygiene in terms of the strength of delivery.
General dental health information and more detailed information around the behaviour health link was included in all interventions. Interventions were delivered by specifically trained dental nurses (Worthington 2001) and by school health counsellors and teachers (Saied‐Moallemi 2009). For the remaining studies, it is unclear who delivered the interventions. Disclosing tablets were used as part of the interventions in one study as part of a classroom activity (Worthington 2001).
Structures for transition of the intervention into the home were absent in two of the studies (Petrecca 1994; Zanin 2007). Saied‐Moallemi 2009 described one intervention arm that provided parents with leaflets and materials (e.g. brushing charts and worksheets) used in the school with the aim of getting the parents to replicate the intervention at home (these children did not receive an intervention in school). The remaining intervention arm in this study included a combination of home and school elements, each intended to reinforce the other. One study encouraged a link to the home with the provision of oral health related home work tasks (along the same theme as the work in schools) lasting around 1 hour. Parents or grandparents were required to complete these with the children (Worthington 2001).
In three of the studies, control groups were non‐intervention controls; no preventive treatment or instruction was provided (Petrecca 1994; Saied‐Moallemi 2009; Worthington 2001). However in one of these studies half the control schools became active at 4 months (Worthington 2001). In the remaining study (Zanin 2007) treatment, including fillings and extractions, was provided as well as an annual supervised toothbrushing session.
Of the included trials, two did not report that pilot work had been carried out prior to the development of the intervention (Saied‐Moallemi 2009; Zanin 2007). One study conducted pilot work on a population previously examined by the authors (Petrecca 1994) and the remaining study piloted the intervention with children and teachers to test measures, delivery and materials prior to the RCT (Worthington 2001).
In the included studies post‐intervention outcome measures were reported at 3 months (Saied‐Moallemi 2009), 6 months (Zanin 2007) and 1 year after the intervention (Petrecca 1994). Worthington 2001 employed a cross‐over design and as such reported post‐intervention outcome measures at 4 months within phase one and after 3 months for phase two. Only one of the included studies reported having an additional follow‐up time point (Petrecca 1994).
Excluded studies
The search and screening process is summarised in Figure 3. Studies not included in this review (and the reason for exclusion) can be found in the Characteristics of excluded studies table. The most common reason for exclusion was study design. Studies were also excluded where behavioural interventions were provided along side clinical interventions such as sealants or varnish making it impossible to determine the effect of the behavioural intervention alone. Additionally, a substantial number of studies were excluded on the basis that the intervention did not contain the two key components described in the inclusion criteria (oral hygiene and diet) for this review. Most commonly, interventions tended to be based around oral hygiene only.
Risk of bias in included studies
Quality assessment was conducted using The Cochrane Collaboration's 'risk of bias' tool on all included studies. This assesses each study on seven domains: sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessors, incomplete outcome data, selective outcome reporting and any other bias. Across the domains relating to selection, performance and detection bias, the majority of trials scored low or unclear. Selective reporting bias was deemed to be highest risk of bias, being scored as high for half of the included studies (Figure 1 and Figure 2). Overall the risk of bias was assessed as unclear in Zanin 2007, and high in the remaining three studies.
Allocation
Random sequence generation
One of the studies reported that a "lottery" was the method of randomisation (Zanin 2007) and for another included study, details were provided by personal communication (Worthington 2001) confirming that randomisation was achieved by way of a computer generated schedule. Both of these studies were assessed as low risk of bias for this domain. The remaining two studies were assessed at unclear risk of bias here.
Allocation concealment
It was unclear who conducted the "lottery" in the study reported by Zanin 2007, so allocation concealment was assessed as unclear. Personal communication confirmed that allocation to intervention and control groups was undertaken by the statistician and concealed from the dental nurse who conducted the intervention in the other study (Worthington 2001). The remaining two studies reported no information about allocation concealment and were assessed at unclear risk of bias. Within these, two of the studies were cluster randomised controlled trials (Saied‐Moallemi 2009; Worthington 2001) with the unit of allocation being the school.
Blinding
Participants and personnel
Blinding of deliverers and participants in behavioural interventions is problematic and this has been acknowledged in other Cochrane reviews of behavioural interventions (e.g. Waters 2011). Some of the included studies in this review had attempted to minimise the level of information given to children, however it was not always possible to blind the delivery of the intervention for obvious reasons.
Two studies reported that participants were not aware of the treatment group they were allocated to (Saied‐Moallemi 2009; Zanin 2007). Two were cluster randomised hence it was assumed that the risk of performance bias was reduced (Saied‐Moallemi 2009; Worthington 2001).
Outcome assessors
Three studies were judged to be of low risk of performance bias (Saied‐Moallemi 2009; Worthington 2001; Zanin 2007). Lack of information in the remaining study (Petrecca 1994) meant it was not possible to ascertain the level of bias (Petrecca 1994); this was judged to be unclear.
Of the studies that were judged to have low risk of performance bias, three were also judged to have low risk of detection bias, having reported on blinding (Saied‐Moallemi 2009; Worthington 2001; Zanin 2007). For the remaining study (Petrecca 1994) it was not possible to determine the detection bias due to insufficient reporting.
Incomplete outcome data
Three studies included in the review were judged to be of low risk of attrition bias (Saied‐Moallemi 2009; Worthington 2001; Zanin 2007). Low levels of participant drop‐out were reported across these studies meant that attrition was unlikely to impact upon the outcomes of interest.
The study described by Petrecca 1994 was judged to be of high risk of attrition bias as some children were taken out of the sample after the initial phase for not adequately following the oral hygiene and nutrition components of the intervention. Rates of attrition were different in each group over the 2 years of this trial.
Selective reporting
Half of the included studies in this review were judged to have low risk of reporting bias (Worthington 2001; Zanin 2007). However, it is important to note that study protocols could not be obtained; it was clear from the papers that all pre‐specified and expected outcomes were reported.
One study was judged to have high risk of reporting bias (Petrecca 1994) because only point estimates with no estimates of variance were reported, meaning that data could not be interpreted accurately.
Other potential sources of bias
Although the study reported by Worthington 2001 was judged to be of low risk of bias for all other domains, bias may have been introduced regarding the outcome data for plaque. Plaque was measured using a subsample of 10 children in each school, selected based on parental consent. It is possible that the children whose parents did not give consent may have had different mean plaque scores to the subsample measured. It was established through communication with the author that the funder of this study (National Sugar Bureau) had no influence over the data reported.
Effects of interventions
See: Table 1
SeeTable 1.
Primary outcomes
Changes in caries increment measured by the difference in decayed, missing and filled teeth (dmft/DMFT)
One study reported DMFT (Petrecca 1994). While it is unclear as to the precise age of the children in this study, concern about measurement arose from a sentence in the methods section of this paper: "The WHO advises using the same criteria for milk teeth as for permanent dentition, using DMFT but taking into account that teeth lost through caries can be identified only up to the age of 8, since up to that age the absence of a milk molar cannot be due to changeover".
From the DMFT data reported in this study we calculated an estimate of prevented fraction of 0.49 over 2 years, but no standard deviations or standard errors were presented in the paper. Three attempts in total were made to contact the authors of this study for clarification, unfortunately these were unsuccessful. Due to the uncertainty over the measure, this study has not been included in the analysis.
Changes in caries increment on tooth surfaces (dmfs/DMFS)
One study reported on dmfs/DMFS (Zanin 2007). Data presented allowed for the calculation of caries increment, but not standard deviations. This study has been included in the analysis, with estimated standard deviations (SDs) calculated using the regression equation derived by Marinho 2009 in the review of Topical fluorides for preventing dental caries in children and adolescents. This equation was based on a regression analysis of 179 treatment arms. The equation is log (SD caries increment) = 0.64 + 0.55 log (mean caries increment).
This study showed evidence of a reduction in caries increment measured by the difference in decayed missing and filled surfaces (preventive fraction (PF) 0.65, 95% confidence interval (CI) 0.12 to 1.18, 1 RCT, 60 participants) (Analysis 1.1).
1.1. Analysis.
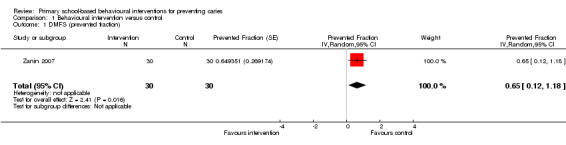
Comparison 1 Behavioural intervention versus control, Outcome 1 DMFS (prevented fraction).
Changes in plaque scores for permanent and deciduous teeth over the course of the intervention and the follow‐up period
Three studies reported plaque outcome data. All plaque indices were based on variations of the Silness and Löe index, with results reported either as post‐treatment plaque score, or change in plaque score from baseline. While the indices differ, they aim to measure a similar outcome and so standardised mean difference (SMD) was used to measure treatment effect.
One study (Zanin 2007) only reported median plaque index (PI). The median PI at the end of the study (15 months) was reported as 0.93 in the control group and 0.60 in the intervention group, with a Mann‐Whitney test reported as significant (P < 0.05). No means were reported, so we were unable to include this outcome in the analysis.
Saied‐Moallemi 2009 reported change in plaque index between pre‐ and post‐intervention examinations. This study had three intervention groups, all of which were judged to meet the inclusion criteria for this review, so the data from these three groups have been combined for analysis here. The study was cluster randomised, with four clusters per group (so 12 clusters in the combined intervention group). No intra‐cluster correlation coefficient (ICC) was reported, although the authors did recognise the cluster design in the analysis of additional outcomes (using generalised estimating equations) the plaque analysis did not adjust for clustering. For the purposes of this review, the ICC has been assumed to be 0.05 (Higgins 2011). After adjustment for clustering, there was a significant difference in change in plaque score, with the intervention groups showing better oral hygiene (SMD ‐0.34, 95% CI ‐0.67 to ‐0.01, cluster adjusted effective sample size 186).
The remaining study, Worthington 2001, was cluster randomised and analysed using generalised estimating equations to allow for the clustering in the analysis. ICC values were also included in the paper, allowing the SMD to be appropriately adjusted for the clustering, by amending the effective sample size. This study presented outcomes at 4 and 7 months, but after the 4‐month examination, the groups were re‐configured, so data from the 4‐month examination have been included here. After adjustment for clustering, there was a significant difference in plaque score, with the intervention group showing a reduction in plaque (SMD ‐0.64, 95% CI ‐0.90 to ‐0.38, cluster adjusted effective sample size 233).
When the Saied‐Moallemi 2009; Worthington 2001 were combined in a meta‐analysis, there was substantial heterogeneity (I2 = 0.50) likely to be due to differences in study design and in the details of the interventions, so meta‐analysis has not been presented (Analysis 1.2).
1.2. Analysis.
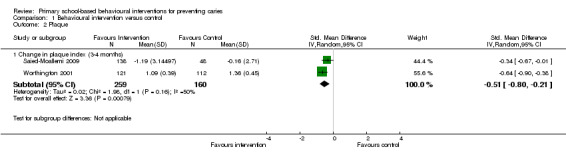
Comparison 1 Behavioural intervention versus control, Outcome 2 Plaque.
Secondary outcomes: Non‐clinical
Of the four included studies, three (Petrecca 1994; Saied‐Moallemi 2009; Zanin 2007) did not measure any secondary outcomes. A variety of non‐clinical measures have been reported in one study (Worthington 2001). These measures relied on self report. The data are described below. There is at present no single reliable method for recording toothbrushing or sugar snacking behaviours.
Children's frequency of toothbrushing
Worthington 2001 reported on children's brushing frequency. Almost all children (99%) at baseline reported twice daily brushing prior to the start of the study, and this level was maintained across all groups throughout the intervention. However, in the baseline focus groups, 'most' children reported that they did not brush their teeth more than once a day.
Children's frequency of cariogenic food and drink consumption
Worthington 2001 reported few children had problems identifying foods containing sugar with only 15% of the intervention and 19% of control participants reporting they routinely consumed sugary snacks when they arrived home from school. However, snack consumption prior to bedtime was reported by approximately a third of participants at baseline, with this figure showing a non‐significant decline across the study period.
Change in oral health knowledge and skills
Worthington 2001 reported changes in oral health knowledge and skills following the intervention. Changes were apparent in both the intervention and control groups at the 4‐month follow‐up (phase one); however, this improvement was greater among the intervention group (34% increase) compared to the control group (15% increase). In phase two, post‐intervention measures showed that the new intervention group had a 10% improvement in knowledge and skill and previous increases found in the intervention and control groups were sustained.
No other behavioural outcomes were measured by the four included studies.
Changes in dental attendance
Worthington 2001 found no change in reported dental visits over the course of the programmes, with 97% of children at baseline reporting visiting the dentist every 2 years. When asked in the focus groups however, most children reported being unsure how often dental visits are recommended.
Adverse events
No study reported any adverse events.
Other analyses
Subgroup and sensitivity analyses were planned, however these were not conducted due to insufficient studies.
Discussion
Summary of main results
This review includes four studies of primary school‐based behavioural interventions aimed at preventing dental caries in children 4 to 12 years of age. Studies were generally less than 2 years in length and there is very limited evidence from these randomised controlled trials (RCTs) on the efficacy of the interventions for dental health. Lack of uniformity in describing the interventions and measuring and reporting outcome variables made accurate pooling of evidence difficult. Only one small study, with 60 participants (Zanin 2007), reported a caries outcome, and showed that the children in the intervention group developed fewer new caries over the study period. Although no meta‐analysis was performed for plaque outcomes, three studies reporting plaque (Saied‐Moallemi 2009; Worthington 2001; Zanin 2007) reported statistically significant reductions in plaque in the intervention groups. This provides some limited evidence that these interventions reduce plaque outcomes over the short term. Short term improvements in plaque scores may arguably not be considered a 'true health outcome' and do not provide useful information on long term effects of these interventions.
In summary the key learning from this review in terms of the efficacy of primary school‐based behavioural interventions on clinical and behavioural outcomes is very limited. The included studies were multifarious in terms of intervention design and clinical and behavioural outcomes. Consequently it is difficult to give any clear evidence‐based recommendations as to the best intervention designs with respect to oral health behaviour change.
Overall completeness and applicability of evidence
This is the first Cochrane review that has examined the use of behaviour change techniques (BCTs) in dental clinical trials. Behaviour change science has progressed rapidly over the last decade and has been applied within various areas of public health research including attempts to change multiple behaviours (e.g. diet and physical activity in obesity interventions) (Michie 2012).
Interventions were subject to high levels of heterogeneity and ways of measuring caries and plaque outcomes varied. Meta‐analysis could not be conducted on caries outcomes as data from only one study were eligible. Nor could a meta‐analysis be conducted on plaque outcomes as we judged heterogeneity to be too high. Additionally, subgroup analysis could not be conducted due to the low number of included studies.
The studies included in this review provide a limited means for answering questions around how best to prevent caries through primary school‐based behavioural interventions. The interventions themselves were not described in detail within published reports, however it is recognised that publication limitations may apply.
Several BCTs could be identified in the included studies; these are recorded in Additional Table 2 (theoretical basis of these BCTs is provided in Appendix 12). These were predominantly around.
1. Behaviour change techniques (BCTs).
| Petrecca 1994 | Saied‐Moallemi 2009 | Worthington 2001 | Zanin 2007 | |
| 1. Provide information about behaviour health link (IMB) | ✓ | ✓ (H&S) | ✓ | ✓ |
| 2. Provide information on consequences (TRA, TPB, SCogT, IMB) | ✓ | ✓ (H) | ✓ | ✓ |
| 3. Provide information about others' approval (TRA, TPB, IMB) | ||||
| 4. Prompt intention formation (TRA, TPB, SCogT, IMB) | ✓ (S) | |||
| 5. Prompt barrier identification (SCogT) | ||||
| 6. Provide general encouragement (SCogT) | ||||
| 7. Set graded tasks (SCogT) | ||||
| 8. Provide instruction (SCogT) | ✓ | ✓ | ||
| 9. Model or demonstrate the behaviour (SCogT) | ✓ | ✓ (S) | ✓ | |
| 10. Prompt specific goal setting (CT) | ||||
| 11. Prompt review of behavioural goals (CT) | ||||
| 12. Prompt self monitoring of behaviour (CT) | ✓ | |||
| 13. Provide feedback on performance (CT) | ✓ | |||
| 14. Provide contingent rewards (OC) | ||||
| 15. Teach to use prompts or cues (OC) | ||||
| 16. Agree on behavioural contract (OC) | ||||
| 17. Prompt practice (OC) | ✓ | ✓ (S) | ✓ | ✓ |
| 18. Use follow‐up prompts | ✓ | |||
| 19. Provide opportunities for social comparison (SCompT) | ✓ | |||
| 20. Plan social support or social change (Social support theories) | ✓ (H) | |||
| 21. Prompt identification as a role model | ||||
| 22. Prompt self talk | ||||
| 23. Relapse prevention (Relapse prevention therapy) | ||||
| 24. Stress management (Stress theories) | ||||
| 25. Motivational interviewing | ||||
| 26. Time management |
Extraction: Saied‐Moallemi 2009 ‐ (H) refers to the home intervention only arm with (S) referring to the school only intervention arm.
The BCTs were extracted from the description of the intervention reported in each paper by 3 authors (Pauline Adair (PA), Lucy O'Malley (LO) and Sarah Elison (SE)). All additional resources (obtained through contact with study authors) were incorporated into this phase of data extraction. The taxonomy of BCTs (Abraham 2008), was used to code all published and unpublished information around the content of each intervention. No assumptions were made that BCTs were present if the available information was unclear. It is important to note that the taxonomy defines discrete BCTs meaning that no one element of an intervention can appear as 2 separate techniques.
Instruction ‐ in most cases referred to promoting toothbrushing or demonstration of brushing but also changing sugar consumption.
Demonstration of toothbrushing ‐ which varied from using models (Petrecca 1994) to supervision of the children's technique on a regular basis, in Saied‐Moallemi 2009 by health counsellors. In the intervention reported by Zanin 2007, it was unclear who supervised the brushing sessions and whether they were trained to do so.
In the case of the intervention described by Zanin 2007, the aetiology of caries was explained in order to provide children with the link between behaviour and consequences. In the intervention described by Worthington 2001, general behaviours were described as resulting in particular dental outcomes. In all cases messages were disseminated either through leaflets or through lessons. One study reported that the interventions involved some form of active learning, such as group discussion (Worthington 2001).
The data presented by Zanin 2007 indicate a large effect on caries as a result of the intervention. It is important to note that the intervention included an age specific toothbrushing technique and toothbrushing was practiced at regular supervised intervals. The evaluation period did not extend beyond the length of the intervention and as such we cannot be certain of the long term impact of this intervention on health behaviours.
Many of these interventions targeted knowledge. It is recognized that knowledge increase or indeed instruction will not necessarily lead to sustained behavioural change (Freeman 2009; Kay 1996; Kay 1998; Stillman‐Lowe 2008). The integration of relevant behavioural components may be important in terms of behavioural outcomes. Such components may benefit from inter‐professional delivery or expertise in the integration of the intervention by an appropriately trained team (Watson 2011).
Quality of the evidence
Based on the evidence gathered by this review (four studies incorporating a total of 2302 children at baseline), it cannot be determined that primary school‐based behavioural interventions are effective at promoting behaviours related to caries prevention.
Methodologically, there were inconsistencies in the use of the terms 'post‐intervention' and 'follow‐up' to describe outcome measurement. No study reported considerations related to exit strategies upon completion of supported intervention delivery hence we cannot make any judgements about the sustainability of interventions.
The interventions reported in this review primarily focused on the toothbrushing component, with the cariogenic dietary component carrying much less weight. Only two of the studies reported that a power calculation had been conducted to determine sample size. There was considerable variation in terms of who delivered the interventions (including variation in the training received). No study reported delivery by dietary professionals. The variation in the responsibility for delivery, reinforcement and maintenance of interventions is likely to impact upon the fidelity and hence efficacy of the interventions. Studies reported frequent supervised toothbrushing sessions and in some interventions parents were encouraged to take an active role in supervising their child's toothbrushing (active reinforcement) however, this intensity of intervention was not replicated for the cariogenic food/drink components.
Based on the evidence for school behavioural interventions for preventing caries presented by the studies included in this review, there are significant knowledge gaps. None of the studies included a cost‐benefit analysis, additionally there was limited analysis of the impact of deprivation. Little can therefore be said about the potential financial implications of providing behavioural interventions in a primary school setting. Further research is also required around the impact of deprivation on behavioural interventions targeting primary school children. Child oral health related quality of life and overall health status are not reported as outcome measures or explanatory variables in any of the included studies.
While some studies have reported behavioural measures alongside clinical outcomes, none have attempted to link the various types of evidence to understand the effects of the interventions in a holistic sense. Complex behavioural interventions require process evaluations to explore, in greater depth, how and why they work or do not. Such evaluations "would improve the science of many randomised controlled trials" (Oakley 2006).
None of the interventions were underpinned by theory. Pilot work to inform intervention design appeared limited, a noteworthy finding in consideration of the recent guidance from the MRC 2000 updated to MRC 2008, NICE 2007 and Intervention Mapping Approaches (Bartholomew 2011) which stress the importance of pre‐testing interventions. Difficulties were encountered in obtaining full intervention manuals (although some intervention materials were provided via contact with authors). This was a limiting factor in understanding the more specific components of the interventions. This also has implications for the repeatability and therefore the reliability of these studies.
A major finding from this review is the lack of consistency in the design of interventions in terms of their intensity and optimum length. Indeed, some studies did not report these parameters. We are not yet at a stage of understanding in oral health research to be able to draw conclusions about the key components needed for effective behavioural interventions for caries prevention in primary school aged children. It may be beneficial to draw on the advances currently being made in the field of behavioural science, largely driven by health psychology. Additionally, the social determinants of health is a key area for all research seeking to reduce disparities in health across socioeconomic strata.
Potential biases in the review process
The number of databases searched electronically and journals handsearched was comprehensive. Through the initial title and abstract screening and the full secondary screening, it is felt that all relevant studies have been included in the review. During the review process, we had greater success in contacting authors of more recent studies. This lead to clarification of studies for the purposes of study screening as well as data extraction. Through contact with authors, some intervention materials were also obtained meaning that we gained a more thorough understanding of these interventions.
Agreements and disagreements with other studies or reviews
This review partially supports reviews which have examined oral health education interventions (Kay 1996; Kay 1998; Watt 2001) in finding short term improvements in the oral health knowledge of children and adults. A recent review conducted by Harris 2012 around chairside interventions for dietary behaviour change found that the reporting of interventions was greatly varied, with "no studies concerned with dietary change aimed at preventing tooth erosion". The primary focus of the interventions was fruit, vegetable and alcohol consumption. Additionally only one study included by Harris 2012 included a cost analysis for the intervention. Cost benefit analysis is highlighted within this review as important and under‐researched in this field.
A review examining interventions aimed at preventing childhood obesity (Waters 2011) also highlighted the difficulty in determining which component of the intervention was most beneficial, although key areas to promote were identified. Waters 2011 concludes that there is a need to strengthen study and evaluation design as well as the reporting of procedures and intervention implementation. Waters 2011 similarly refers to the need to understand the longer term impacts and the cost of interventions.
Authors' conclusions
Implications for practice.
Based on this review there is limited evidence that primary school‐based behavioural interventions that promote twice daily toothbrushing and reduce snacking on sugary foods can prevent caries by improving children's oral hygiene. There is some evidence to suggest that these interventions may have a positive impact upon children's knowledge and on plaque removal.
Recognition of the social determinants of health and the pivotal role of the home environment are likely to be key aspects enhancing design and delivery of future interventions (active involvement of parents was found to impact intervention effectiveness in this review) helping to ensure strong links with the home. The results presented within this review suggest that the home is an important influence on clinical outcomes (plaque) in these types of intervention. Through the inclusion of an 'active' home component, the efficacy of primary school‐based behavioural interventions may be increased. However, due to the small number of included studies, it is not possible to determine the extent of this impact. This is an area recommended for further research.
A greater emphasis should be placed on embedding healthy morning and bedtime routines, focusing on relevant environmental cues within the home. Future intervention design should target development of behavioural transition moving from knowledge acquisition to the adoption of habitual behaviour (i.e. knowledge, skill development, reinforcement and practice behaviours in a relevant setting). As yet it is unclear which BCTs are the most effective for dental health related behaviours. Attention must be paid to theoretical detail regarding behaviour change; failure to do so may limit the potential of interventions to bring about sustained health improvement.
This review highlighted that the dietary component of combined oral health behavioural interventions is less developed and tends to come secondary to oral hygiene. There appears to be a lack of integration between dietary and hygiene messages. Only one study had a more active approach to diet and nutrition. Future practice should ensure a balance between these components. Inter‐professional working may help facilitate such practice.
From a sustainability and cost perspective, programmes should be designed to be integrated into current oral health strategies and school curricula using models such as 'train the trainer'. Such models do not rely on specialist staff and can thus be implemented in future years following the end of the evaluated intervention. The interventions in this review were predominantly delivered by teachers however, it was not reported how these teachers were trained.
Implications for research.
This review highlights that there are questions still to be answered around how to effectively change the behaviour of primary school children and their families to reduce dental caries. In terms of expanding the evidence base, future studies should seek to demonstrate the rigorous standards in the design, implementation, delivery and reporting of these interventions thus aiding subsequent systematic reviews in this area. This should result in a more comprehensive interpretation of the specific behavioural components of interventions. As with intervention components, the same weight should be applied to the measurement and reporting of clinical and behavioural outcomes. Within this review the primary aim of the interventions was to change behaviour; however the focus of measurement was based on clinical outcomes that detect the results of lack of behaviour targeted (e.g. poor gingival health and high plaque levels). Only one study reported behaviour measures (Worthington 2001) being collected as part of the study.
New clinical trials conducted in primary schools aimed at reducing caries should include.
Outcomes that allow assessment of dental caries effect (start age 5 to 6 years to allow effect estimates for first permanent molar teeth) as well as behaviour change.
Cost effectiveness measures.
Recognised staged approach to designing and evaluating complex interventions such as the Medical Research Council (MRC) guidelines for complex intervention.
Theory‐based interventions and incorporate BCTs; reporting of interventions should detail their length.
Multi‐disciplinary teams in addition to dental expertise including health psychologists, dieticians and health economists.
Sample sizes sufficiently powered to measure clinical and behavioural outcomes appropriately.
A significant period of follow‐up (e.g. 2 to 3 years) in order to measure long term impact on caries outcomes.
Data reported according to potentially relevant factors such as age, gender and socio‐economic status allowing for subgroup analysis.
In addition to the Consolidated Standards of Reporting Trials (CONSORT) (CONSORT 2010), reporting should detail.
Intervention length, intensity and frequency as well as specific components.
Intervention deliver(s) and information about the setting.
Statistically, future trials should report mean and standard deviations for each outcome, as well as number of participants at each time point in order to improve the opportunity for meta‐analyses to be performed in future systematic reviews.
Increasingly there is an awareness of the publication of intervention manuals in behavioural research. Journals such as Addiction now publish such materials online to supplement study reports. This could make for a more comprehensive evaluation of behavioural interventions in future systematic reviews.
For all but incomplete outcome data, selective reporting and blinding of participants studies were most commonly assessed to have an unclear risk of bias due to limited reported information. In addition to problems highlighted around the reporting of interventions, there is also an ongoing need to address the reporting of randomisation methods and the details of participant blinding.
Within the measurement of behavioural outcomes, and to a lesser extent, clinical outcomes, there is a lack of standardization around best measures. Future research should look at the need to develop a common core indicator set of behaviour measurements for use in dental public health intervention studies.
Key points
The evidence of effectiveness of primary school‐based behavioural interventions on clinical and behavioural oral health outcomes is limited.
All the included studies contained behavioural interventions which lacked a theoretical basis. They also exhibited limited BCTs; those identified tended to relate to information giving rather than support.
Future delivery of effective oral health interventions may benefit from increased collaboration between relevant dental and dietary professionals to ensure programmes focus on both toothbrushing and dietary practice in an integrated way. Programmes must address the issue of the school‐home interface so that parental involvement is developed as a mechanism to enable future sustainability of children's oral health habits.
Reporting of dental public health trials needs considerable improvement focusing on design, process, impact and outcome of trials, including cost benefit and cost effectiveness.
Future trials are needed to test the impact of better designed and longer‐term oral health behavioural interventions which are designed to sustain behaviour change and should include measures of cost benefit and cost effectiveness.
Acknowledgements
We would like to thank the Cochrane Oral Health Group for the support with the review especially Anne Littlewood for her help in designing and running the search strategy. Val Featherstone was involved in examining search results to support the team. Thank you to www.sel‐uk.com for translating Petrecca 1994 from Italian to English and to Abir Abdel Rahmen for kindly organising the translation of intervention materials pertaining to the study by Saied‐Moallemi 2009. Finally the team would like to thank Louise Robinson and Lucy Fish for their support with the administration of the review.
Appendices
Appendix 1. Cochrane Oral Health Group's Trials Register search strategy
((cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali* or plaque or DMF or "oral hygiene index") AND (mouthwash* or "mouth wash*" or mouth‐wash* or dentifrice* or "oral health" or "oral hygiene" or "oral care" or "mouth care" or "dental care" or "teeth care" or toothbrush* or tooth‐brush* or "tooth brush*" or toothpaste* or tooth‐paste* or "tooth paste*" or mouthrinse* or mouth‐rinse* or "mouth rinse*" or clean* or "sugar intake" or sweet* or candy or candies or gum* or snack* or diet* or food* or drink or beverage*) AND (educat* or instruct* or advice or advis* or teach* or train* or promot* or demonstrat* or supervis*) and (school* or child*))
Appendix 2. The Cochrane Central Register of Controlled Trials (CENTRAL) search strategy
#1 ((teeth near/5 cavit*) or (teeth near/5 caries) or (teeth near/5 carious) or (teeth near/5 decay*) or (teeth near/5 lesion*) or (teeth near/5 deminerali*) or (teeth near/5 reminerali*)) #2 ((tooth near/5 cavit*) or (tooth near/5 caries) or (tooth near/5 carious) or (tooth near/5 decay*) or (tooth near/5 lesion*) or (tooth near/5 deminerali*) or (tooth near/5 reminerali*)) #3 ((dental near/5 cavit*) or (dental near/5 caries) or (dental near/5 carious) or (dental near/5 decay*) or (dental near/5 lesion*) or (dental near/5 deminerali*) or (dental near/5 reminerali*)) #4 ((enamel near/5 cavit*) or (enamel near/5 caries) or (enamel near/5 carious) or (enamel near/5 decay*) or (enamel near/5 lesion*) or (enamel near/5 deminerali*) or (enamel near/5 reminerali*)) #5 ((dentin near/5 cavit*) or (dentin near/5 caries) or (dentin near/5 carious) or (dentin near/5 decay*) or (dentin near/5 lesion*) or (dentin near/5 deminerali*) or (dentin near/5 reminerali*)) #6 ((pulp* near/5 cavit*) or (pulp* near/5 caries) or (pulp* near/5 carious) or (pulp* near/5 decay*) or (pulp* near/5 lesion*) or (pulp* near/5 deminerali*) or (pulp* near/5 reminerali*)) #7 MeSH descriptor Tooth Demineralization explode all trees #8 MeSH descriptor Dental Plaque this term only #9 MeSH descriptor Dental Health Surveys explode all trees #10 ("DMF Index" or "Dental Plaque Index" or "Oral Hygiene Index") #11 (plaque and (teeth or tooth or dental or oral)) #12 (#1 or #2 or #3 or #4 or #5 or #6 or #7 or #8 or #9 or #10 or #11) #13 MeSH descriptor Oral Health explode all trees #14 MeSH descriptor Oral hygiene explode all trees #15 MeSH descriptor Mouthwashes this term only #16 MeSH descriptor Dentifrices explode all trees #17 ((mouth near/6 care) or (oral near/6 care) or (dental near/6 care) or (teeth near/6 care)) #18 ((plaque near/3 control) or (plaque near/3 remov*)) #19 (toothbrush* or tooth‐brush* or "tooth brush*" or toothpaste* or tooth‐paste* or "tooth paste*" or dentifrice*) #20 ((tooth near/3 clean*) or (teeth near/3 clean*) or (interdental near/3 clean*)) #21 (mouthwash* or mouthrinse* or "mouth wash*" or "mouth rinse*" or mouth‐wash* or mouth‐rinse*) #22 ("sugar intake" or sweet* or candy or candies or gum*) #23 (snack* or diet* or food* or drink* or beverage*) #24 ((mouth near/6 health) or (oral near/6 health) or (dental near/6 health) or (teeth near/6 health)) #25 ((mouth near/6 hygien*) or (oral near/6 hygien*) or (dental near/6 hygien*) or (teeth near/6 hygien*)) #26 (#13 or #14 or #15 or #16 or #17 or #18 or #19 or #20 or #21 or #22 or #23 or #24 or #25) #27 MeSH descriptor Health education, dental this term only #28 MeSH descriptor Health promotion this term only #29 ((dental or oral or mouth or teeth) and (instruct* or advice or advis* or educat* or teach* or train* or promot*)) #30 ((demonstrat* or supervis*) and (toothbrush* or "tooth brush*" or tooth‐brush* or floss* or "interdental clean*" or mouthrinse* or mouthwash* or "mouth rinse*" or "mouth wash*" or mouth‐rinse* or mouth‐wash*)) #31 (#27 or #28 or #29 or #30) #32 MeSH descriptor Schools this term only #33 (school* and (primary or elementary or junior or infant*)) #34 "4‐11 year* old*" #35 child* #36 (#32 or #33 or #34 or #35) #37 (#12 and #26 and #31 and #36)
Appendix 3. MEDLINE via OVID search strategy
1. (teeth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 2. (tooth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 3. (dental adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 4. (enamel adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 5. (dentin adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 6. (pulp$ adj5 (cavit$ or caries or carious or decay$ or lesion$)).mp. 7. exp TOOTH DEMINERALIZATION/ 8. Dental plaque/ 9. exp Dental Health Surveys/ 10. ("DMF Index" or "dental plaque index" or "oral hygiene index").mp. 11. (plaque and (teeth or tooth or dental or oral)).mp. 12. or/1‐11 13. exp Oral Health/ 14. exp Oral Hygiene/ 15. Mouthwashes/ 16. Dentifrices/ 17. ((mouth adj6 care) or (oral adj6 care) or (dental adj6 care) or (teeth adj6 care)).mp. 18. ((plaque adj3 control) or (plaque adj3 remov$)).mp. 19. (toothbrush$ or "tooth brush$" or tooth‐brush$ or (toothpaste$ or tooth‐paste$ or "tooth paste$") or dentifric$).mp. 20. ((tooth or teeth or interdental) adj3 clean$).mp. 21. (mouthwash$ or mouthrinse$ or "mouth wash$" or "mouth rinse$" or "mouth‐wash$" or "mouth‐rinse$").mp. 22. ("sugar intake" or sweet$ or candy or candies or gum$).mp. 23. (snack$ or diet$ or food$ or drink$ or beverage$).mp. 24. ((mouth adj6 health) or (oral adj6 health) or (dental adj6 health) or (teeth adj6 health)).mp. 25. ((mouth adj6 hygien$) or (oral adj6 hygien$) or (dental adj6 hygien$) or (teeth adj6 hygien$)).mp. 26. or/13‐25 27. Health education, dental/ 28. Health promotion/ 29. ((dental or oral or mouth or teeth) and (instruct$ or advice or advis$ or educat$ or teach$ or train$ or promot$)).mp. 30. ((demonstrat$ or supervis$) and (toothbrush$ or "tooth brush$" or tooth‐brush$ or floss$ or "interdental clean$" or mouthrinse$ or mouthwash$ or "mouth rinse$" or "mouth wash$" or mouth‐rinse$ or mouth‐wash$)).mp. 31. or/27‐30 32. Schools/ 33. (school$ and (primary or elementary or junior or infant)).mp. 34. Child/ 35. ("school age child$" or "school‐age child$" or "4‐11 year$ old$").mp 36. child$.mp. 37. or/32‐36 38. 12 and 26 and 31 and 37
The above subject search was linked to the Cochrane Highly Sensitive Search Strategy (CHSSS) for identifying randomised trials in MEDLINE: sensitivity maximising version (2008 revision) as referenced in Chapter 6.4.11.1 and detailed in box 6.4.c of the Cochrane Handbook for Systematic Reviews of Interventions, Version 5.1.0 [updated March 2011] (Higgins 2011).
1. randomized controlled trial.pt. 2. controlled clinical trial.pt. 3. randomized.ab. 4. placebo.ab. 5. drug therapy.fs. 6. randomly.ab. 7. trial.ab. 8. groups.ab. 9. or/1‐8 10. exp animals/ not humans.sh. 11. 9 not 10
Appendix 4. EMBASE via OVID search strategy
1. (teeth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 2. (tooth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 3. (dental adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 4. (enamel adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 5. (dentin adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 6. (pulp$ adj5 (cavit$ or caries or carious or decay$ or lesion$)).mp. 7. Dental caries/ 8. Tooth plaque/ 9. ("DMF Index" or "dental plaque index" or "oral hygiene index").mp. 10. (plaque and (teeth or tooth or dental or oral)).mp. 11. or/1‐10 12. exp Mouth hygiene/ 13. Mouthwash/ 14. Toothpaste/ 15. ((mouth adj6 care) or (oral adj6 care) or (dental adj6 care) or (teeth adj6 care)).mp. 16. ((plaque adj3 control) or (plaque adj3 remov$)).mp. 17. (toothbrush$ or "tooth brush$" or tooth‐brush$ or (toothpaste$ or tooth‐paste$ or "tooth paste$") or dentifric$).mp. 18. ((tooth or teeth or interdental) adj3 clean$).mp. 19. (mouthwash$ or mouthrinse$ or "mouth wash$" or "mouth rinse$" or "mouth‐wash$" or "mouth‐rinse$").mp. 20. ("sugar intake" or sweet$ or candy or candies or gum$).mp. 21. (snack$ or diet$ or food$ or drink$ or beverage$).mp. 22. ((mouth adj6 health) or (oral adj6 health) or (dental adj6 health) or (teeth adj6 health)).mp. 23. ((mouth adj6 hygien$) or (oral adj6 hygien$) or (dental adj6 hygien$) or (teeth adj6 hygien$)).mp. 24. or/12‐23 25. Dental health education/ 26. Health promotion/ 27. ((dental or oral or mouth or teeth) and (instruct$ or advice or advis$ or educat$ or teach$ or train$ or promot$)).mp. 28. ((demonstrat$ or supervis$) and (toothbrush$ or "tooth brush$" or tooth‐brush$ or floss$ or "interdental clean$" or mouthrinse$ or mouthwash$ or "mouth rinse$" or "mouth wash$" or mouth‐rinse$ or mouth‐wash$)).mp. 29. or/25‐28 30. School/ 31. (school$ and (primary or elementary or junior or infant)).mp. 32. exp Child/ 33. ("school age child$" or "school‐age child$" or "4‐11 year$ old$").mp. 34. child$.mp. 35. or/30‐34 36. 11 and 24 and 29 and 35
The above subject search was linked to the Cochrane Oral Health Group filter for EMBASE via OVID:
1. random$.ti,ab. 2. factorial$.ti,ab. 3. (crossover$ or cross over$ or cross‐over$).ti,ab. 4. placebo$.ti,ab. 5. (doubl$ adj blind$).ti,ab. 6. (singl$ adj blind$).ti,ab. 7. assign$.ti,ab. 8. allocat$.ti,ab. 9. volunteer$.ti,ab. 10. CROSSOVER PROCEDURE.sh. 11. DOUBLE‐BLIND PROCEDURE.sh. 12. RANDOMIZED CONTROLLED TRIAL.sh. 13. SINGLE BLIND PROCEDURE.sh. 14. or/1‐13 15. ANIMAL/ or NONHUMAN/ or ANIMAL EXPERIMENT/ 16. HUMAN/ 17. 16 and 15 18. 15 not 17 19. 14 not 18
Appendix 5. CINAHL via EBSCO search strategy
S1 (teeth N5 (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*)) S2 (tooth N5 (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*)) S3 (dental N5 (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*)) S4 (enamel N5 (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*)) S5 (dentin N5 (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*)) S6 (pulp* N5 (cavit* or caries or carious or decay* or lesion*)) S7 MH "Tooth Demineralization+" S8 MH "Dental Plaque" S9 ("DMF Index" or "dental plaque index" or "dental health survey*" or "oral hygiene index") S10 (plaque and (teeth or tooth or dental or oral)) S11 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9 or S10 S12 MH "Oral Health+" S13 MH "Oral Hygiene+" S14 MH "Mouthwashes" S15 MH "Dentifrices" S16 ((mouth N6 care) or (oral N6 care) or (dental N6 care) or (teeth N6 care)) S17 ((plaque N3 control*) or (plaque N3 remov*)) S18 ((toothbrush* or "tooth brush*" or tooth‐brush* or toothpaste* or "tooth paste*" or tooth‐paste* or dentifrice*)) S19 ((tooth or teeth or interdental) N3 clean*) S20 (mouthwash* or mouthrinse* or "mouth wash*" or "mouth rinse*" or mouth‐wash* or mouth‐rinse*) S21 ("sugar intake" or sweet* or candy or candies or gum*) S22 (snack* or diet* or food* or drink* or beverage*) S23 ((mouth N6 health) or (oral N6 health) or (dental N6 health) or (teeth N6 health)) S24 ((mouth N6 hygien*) or (oral N6 hygien*) or (dental N6 hygien*) or (teeth N6 hygien*)) S25 S12 or S13 or S14 or S15 or S16 or S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 S26 MH "Dental health education" S27 MH "Health Promotion" S28 ((dental or oral or mouth or teeth) and (instruct* or advice or advis* or educat* or teach* or train* or promot*)) S29 ((demonstrat* or supervis*) and (toothbrush* or "tooth brush*" or tooth‐brush* or floss* or "interdental clean*" or mouthrinse* or mouthwash* or "mouth rinse*" or "mouth wash*" or mouth‐rinse* or mouth‐wash*)) S30 S26 or S27 or S28 or S29 S31 MH "Schools" S32 (school* and (primary or elementary or junior or infant)) S33 MH "Child+" S34 child* S35 S31 or S32 or S33 or S34 S36 S11 and S25 and S30 and S35
The above subject search was linked to the Cochrane Oral Health Group filter for identifying RCTs in CINAHL via EBSCO:
S1 MH Random Assignment or MH Single‐blind Studies or MH Double‐blind Studies or MH Triple‐blind Studies or MH Crossover design or MH Factorial Design S2 TI ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") or AB ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") or SU ("multicentre study" or "multicenter study" or "multi‐centre study" or "multi‐center study") S3 TI random* or AB random* S4 AB "latin square" or TI "latin square" S5 TI (crossover or cross‐over) or AB (crossover or cross‐over) or SU (crossover or cross‐over) S6 MH Placebos S7 AB (singl* or doubl* or trebl* or tripl*) or TI (singl* or doubl* or trebl* or tripl*) S8 TI blind* or AB mask* or AB blind* or TI mask* S9 S7 and S8 S10 TI Placebo* or AB Placebo* or SU Placebo* S11 MH Clinical Trials S12 TI (Clinical AND Trial) or AB (Clinical AND Trial) or SU (Clinical AND Trial) S13 S1 or S2 or S3 or S4 or S5 or S6 or S9 or S10 or S11 or S12
Appendix 6. PsycINFO via OVID search strategy
1. (teeth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 2. (tooth adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 3. (dental adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 4. (enamel adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 5. (dentin adj5 (cavit$ or caries or carious or decay$ or lesion$ or deminerali$ or reminerali$)).mp. 6. (pulp$ adj5 (cavit$ or caries or carious or decay$ or lesion$)).mp. 7. ("DMF Index" or "dental plaque index" or "oral hygiene index").mp. 8. (plaque and (teeth or tooth or dental or oral)).mp. 9. ((mouth adj6 care) or (oral adj6 care) or (dental adj6 care) or (teeth adj6 care)).mp. 10. ((plaque adj3 control) or (plaque adj3 remov$)).mp. 11. (toothbrush$ or "tooth brush$" or tooth‐brush$ or (toothpaste$ or tooth‐paste$ or "tooth paste$") or dentifric$).mp. 12. ((tooth or teeth or interdental) adj3 clean$).mp. 13. (mouthwash$ or mouthrinse$ or "mouth wash$" or "mouth rinse$" or "mouth‐wash$" or "mouth‐rinse$").mp. 14. ("sugar intake" or sweet$ or candy or candies or gum$).mp. 15. (snack$ or diet$ or food$ or drink$ or beverage$).mp. 16. ((mouth adj6 health) or (oral adj6 health) or (dental adj6 health) or (teeth adj6 health)).mp. 17. ((mouth adj6 hygien$) or (oral adj6 hygien$) or (dental adj6 hygien$) or (teeth adj6 hygien$)).mp. 18. Health promotion/ 19. ((dental or oral or mouth or teeth) and (instruct$ or advice or advis$ or educat$ or teach$ or train$ or promot$)).mp. 20. ((demonstrat$ or supervis$) and (toothbrush$ or "tooth brush$" or tooth‐brush$ or floss$ or "interdental clean$" or mouthrinse$ or mouthwash$ or "mouth rinse$" or "mouth wash$" or mouth‐rinse$ or mouth‐wash$)).mp. 21. (school$ and (primary or elementary or junior or infant)).mp. 22. ("school age child$" or "school‐age child$" or "4‐11 year$ old$").mp. 23. child$.mp. 24. or/1‐8 25. or/9‐17 26. or/18‐20 27. or/21‐23 28. 24 and 25 and 26 and 27
Appendix 7. Current Controlled Trials search strategy
(school* AND behavi* AND prevent* AND (caries or carious or "tooth decay"))
Appendix 8. ClinicalTrials.gov search strategy
(school AND prevent* AND (caries or carious or "tooth decay"))
Appendix 9. ZETOC search strategy
(Search limited to Conference Proceedings)
(school* and prevent* and caries) (school* and prevent* and carious) (school* and prevent* and “tooth decay”)
Appendix 10. Web of Science search strategy
(Search limited to Conference Proceedings)
#1 TS=((teeth or tooth or dental or enamel or dentin or pulp*) AND (cavit* or caries or carious or decay* or lesion* or deminerali* or reminerali*)) #2 TS=("DMF Index" or "dental plaque index" or "dental health survey*" or "oral hygiene index") #3 TS=(plaque and (teeth or tooth or dental or oral)) #4 #1 or #2 or #3 #5 TS=(toothbrush* or "tooth brush*" or tooth‐brush* or toothpaste* or tooth‐paste* or "tooth paste*" or interdental or mouthwash* or mouthrinse* or mouth‐wash* or mouth‐rinse* or "mouth wash*" or "mouth rinse*") #6 TS=("sugar intake" or sweet* or candy or candies or snack* or diet* or food* or drink* or beverage* or gum*) #7 TS=((oral or mouth or dental or teeth) AND (hygien* or health or care)) #8 TS="plaque control" #9 TS=(plaque and remov*) #10 TS=(school* or child*) # 11 #5 or #6 or #7 or #8 or #9 # 12 #4 and #10 and #11 # 13 TS=((dental or oral or mouth or teeth) AND (instruct* or advice or advis* or educat* or teach* or train* or promot*)) # 14 TS=((demonstrat* or supervis*) AND (toothbrush* or "tooth brush*" or tooth‐brush* or floss* or "interdental clean*" or mouthrinse* or mouthwash* or "mouth rinse*" or "mouth wash*" or mouth‐rinse* or mouth‐wash*)) # 15 #13 or #14 # 16 #12 and #15
Appendix 11. Dissertations and Theses via Proquest search strategy
ab(caries or carious or "tooth decay" or cavit*) AND ab(school* or child*) AND ab(prevent*) AND ab(random* or trial* or control* or placebo*)
Appendix 12. Explanation of the Taxonomy of Health Behaviour Change Techniques from Abraham & Michie (2008)
| Theoretical framework | Definition | |
| 1 | Information‐Motivation‐Behavioural Skills Theory (Fisher 1994) | This model of behaviour puts forward that change is most likely to occur if individuals have been provided with relevant, effective information, are sufficiently motivated and have social support. Additionally individuals must have the skill to perform the desired behaviour as well as high self efficacy for the task. |
| 2 | Theory of Reasoned Action (Fishbein 1975) | This theory assumes that most socially relevant behaviours are under volitional control, that they are the result of choices made by the individual enacting them. Therefore the intention to enact the behaviour is both the immediate determinant and the single best predictor of that behaviour. Intention to perform the behaviour is influenced by attitudes towards the action. This will include the person's positive or negative beliefs and evaluations of the outcome of the behaviour. Intention is also influenced by subjective norms including the perceived expectations of important others such as family, friends and work colleagues. Behavioural intention results in action. |
| 3 | Theory of Planned Behaviour (Ajzen 1991) | The theory of planned behaviour is an extension of the theory of reasoned action. This theory, in addition to the constructs of reasoned action, allows for the impact of past behaviour and also for the individual not always being in control of their behaviour. The notion of behavioural control is included in this theory. Knowledge of the relevant skills and experience, emotions, past track record and external circumstances are important. Behavioural control is assumed to have a direct influence of intention. |
| 4 | Social Cognitive Theory (Bandura 1986) | A comprehensive theory of behaviour change, social cognitive theory puts forward a multi‐faceted causal structure of motivation and behaviour. It proposes a reciprocal interaction between the individual, the environment and behaviour. Knowledge of health risks, benefits of change social influences and perceived barriers are important components in addition to self influences. Self efficacy is a key component of this theory. This theory proposes that behaviour change can occur if people perceive that they have control over the outcome, that there are few external barriers and people are confident in their ability to enact the behaviour. |
| 5 | Control Theory (Glasser 1985) | Control theory is a theory of motivation which states that behaviour is not a response to external stimuli but that it occurs in response to what the individual most wants at that particular time. Glasser puts forward that all behaviour are a reaction to 1 of 5 internal needs, 1. Survival, 2. The need to belong, 3. In pursuit of power and importance, 4. In pursuit of freedom and independence and 5. To have fun. Interventions guided by this theory stress positive reinforcement and punishment. Developing an environment in which individuals feel safe will reduce negative responses to behaviour change which may be triggered by perceived threats to survival. |
| 6 | Operant Conditioning (Skinner 1953) | A behaviourist theory, operant conditioning puts forward that an individual's behaviour is based on reinforcement and incentives. The process describes how behaviours are acquired and maintained. Behaviour is learned, reinforcement and punishment are key constructs, the consequences of a behaviour once preformed will affect the likelihood of that behaviour being enacted again. |
| 7 | Social Comparison Theory (Festinger 1954) | Social comparison theory posits that individuals look to external sources in order to check and align their behaviour. These sources may be other people or may be environmental. The comparisons people make between themselves and external sources may affect their emotions, motivation and subsequently their behaviour. Comparisons can be 'upward' or 'downward'. 'Upward' comparisons occur when the comparison behaviour (or behavioural outcome) of the external source is more optimal and 'downward' comparisons occur when the external source is less optimal than the individual making the comparison. Upward comparisons tend to elicit greater motivation for change however if the gap between the comparisons is very large, without additional support, the individual may be discouraged from change (Martin 2010). |
| 8 | Social support theories | Social support is a broad concept. Different theories relate to the ways in which social support has been defined. In a review of the literature on social support theories, Hupcey 1998, found there to be 5 categories of theoretical definitions: 1. Type of social support, 2. Recipients perceptions of support, 3. Intentions or behaviours of the providers, 4. Reciprocal support and 5. Social networks. Social support may include emotional support, support with the specific task targeted for change or with overcoming barriers to change as well as support around providing relevant information or tools. The basic premise of theories in this area is that individuals who are supported in the above mentioned ways will be more likely to change their behaviour than individuals who are not. |
| 9 | Relapse Prevention Therapy (Marlatt 1998) | This theory stresses the maintenance of behaviour change, identifying potential steps to prevent relapse. Relapse prevention theory states that relapse is most likely to occur if an individual has low self efficacy, insufficient coping skills. Interventions developed around this theory should prepare individuals for setbacks, these components include, 1. Anticipation of high risk situations, 2. Avoidance of these situations, 3. Working on improving coping responses to these situations, 4. Correctly attributing the cause of the setback and 5. Reframing reactions to the setback. |
| 10 | Stress Theories (Lazarus 1966) | Stress theory relates to how an individual copes with a situation. Upon being confronted with an outside stressor, the individual first assesses the significance of the stressor, then their perceived ability to cope with the stressor. These appraisals direct behaviour in the given stressful situation. |
Data and analyses
Comparison 1. Behavioural intervention versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 DMFS (prevented fraction) | 1 | 60 | Prevented Fraction (Random, 95% CI) | 0.65 [0.12, 1.18] |
| 2 Plaque | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Change in plaque index (3‐4 months) | 2 | 419 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.51 [‐0.80, ‐0.21] |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Petrecca 1994.
| Methods |
Study design: Randomised controlled trial (3‐arm trial) Conducted in: Europe, Italy Unit of randomisation: Individual Unit of analysis: Individual Funded by: Not stated |
|
| Participants |
Inclusion criteria: Children attending primary school in research areas in classes year I, II and III Exclusion criteria: None stated Age at baseline: Unclear ‐only states that the children were of primary school age Gender: Unclear how distributed within study Number of participants randomised: Intervention Group I n = 492, Group II n = 501; Control n = 482 Number of participants evaluated: Group I year 1 n = 479, year 2 n = 477; Group II year 1 n = 472, year 2 n = 466; Control year 1 n = 477, year 2 n = 476 |
|
| Interventions |
Comparison: Series of preventive and corrective measures intended to change and improve oral hygiene and dietary hygiene habits; with constant monitoring and asked to follow these instructions scrupulously versus received all the preventive and corrective instruction aimed at changing their oral and dietary hygiene habits but was also motivated to receive fluoroprophylactic treatment by using fluoride tablets (1 mg per day) versus no type of preventive treatment Group I: Series of preventive and corrective measures intended to change and improve oral hygiene and dietary hygiene habits. This was carried out through meetings with the individual classes using diagrams and plastic models being used to explain the aetiopathogenesis of caries to the children and teach them oral hygiene. Children constantly monitored and asked (approximately every 30 days) to follow these instructions scrupulously Group II: Received all the preventive and corrective instruction aimed at changing their oral and dietary hygiene habits. This group were also motivated to receive fluoroprophylactic treatment by using fluoride tablets (1 mg per day) Control: No type of preventive treatment Duration of intervention: Unclear Post‐intervention: Unclear Duration of follow‐up: 1 and 2 years Behavioural or psychological component: 5 BCTs1 could be identified from the report Dental: Group I: Corrective measure to improve oral hygiene through classroom lessons Group II: Fluoride tables and classroom lesson Nutrition: Dietary hygiene habits in lesson |
|
| Outcomes | Caries ‐ DMFT (mean values, no standard deviations) | |
| Notes |
Design by/Pilot work: Pilot work on a previously examined population was conducted to identify the most important measures to be taken during health education programme evaluation Power calculation: Not reported Language: Paper translated from Italian to English |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Division of the children into 3 groups was "totally random". Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Paper does not specify how children were randomly allocated into groups |
| Blinding of participants and personnel (performance bias) All outcomes | Unclear risk | Not reported |
| Blinding of outcome assessment (detection bias) All outcomes | Unclear risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes | High risk | After first year of study 1% of children were removed from sample due to failure to follow the behavioural instructions around diet and oral hygiene. Over 2 years 15/492 (3%), 35/501 (7%) and 6/482 (1%) were excluded from analysis, this difference in rates may introduce bias |
| Selective reporting (reporting bias) | High risk | Planned outcomes of caries (DMFT) are reported without estimates of variance so data cannot be used in meta‐analysis |
| Other bias | Low risk | No other sources of bias identified |
Saied‐Moallemi 2009.
| Methods |
Study design: Cluster randomised controlled trial (4 clusters) Conducted in: Tehran Unit of randomisation: Schools Unit of analysis: Schools Funded by: Iran Centre for Dental Research (ICDR) |
|
| Participants |
Inclusion criteria: Attending third‐grade class in a boys and girls school within Tehran Exclusion criteria: None reported Age at baseline: 9 year olds Gender: Mixed boys (n = 224) and girls (n = 233) (2 boys and 2 girls schools in each group) Number of participants randomised: Total Intervention n = 340 (Class‐work group (n = 115) 4 schools; Parental‐aid group (n = 114) 4 schools; Combined group (n = 111) 4 schools); Control group (n = 117) 4 schools Number of participants evaluated: Total Intervention n = 331 (Class‐work group (n = 110) 4 schools; Parental‐aid group (n = 112) 4 schools; Combined group (n = 109) 4 schools); Control group (n = 116) 4 schools |
|
| Interventions |
Comparison: Compare the effectiveness in promoting children's gingival health of 3 school‐based interventions versus a no intervention control group Class‐work group: Delivered in class under supervision of school health counsellors during 3 to 4 sessions in 1 month (30‐45 minutes each) by means of 7 various illustrative puzzles printed on A4 sheets, used as learning tools, including oral health messages guiding children to twice‐daily toothbrushing, use of fluoride toothpaste and understanding of cariogenic food. After the completion of each puzzle, the health counsellor explained the oral health message that it conveyed. Intervention delivered by teachers and school health counsellors. Details of the interventions were not explained to the children Parental‐aid group: Provided at home by parents without giving any additional instructions on oral health at school. 2‐page A4‐size oral health leaflet and a brushing diary/chart together were delivered by the health counsellors to the children to take home. Leaflet contained comprehensive oral health information on the aetiology of common oral diseases – gingival disease and dental caries – and their associations with general diseases and quality of life. Emphasizing the preventability of oral diseases and ways to keep the mouth healthy by recommending twice‐daily toothbrushing, use of fluoride toothpaste and restricting sugary snacking. Modelling role of parents was underlined Combined group: Intervention carried out in schools and at home through combination of both groups above Control: No intervention in control group only clinical exam and parental questionnaire Duration of intervention: 3 months Post‐intervention: 3 months Duration of follow‐up: None stated Behavioural or psychological component: School 7 BCTs; home 5 BCTs Dental: Promoting children's gingival health Nutrition: Puzzles about healthy foods and posters on the issues around sugary snacks |
|
| Outcomes | Plaque: Modification of a plaque index (PI). Dental plaque was recorded as no plaque, plaque on gingival margins only, and plaque elsewhere, with scores correspondingly 0, 1, and 2. Acceptable oral hygiene and healthy gingiva were also reported in each group Mothers completed self administered questionnaires at baseline concerning demographic variables (90% reported) |
|
| Notes |
Design by/Pilot work: Unclear how the intervention was designed and if any pilot work was conducted Power calculation: "To detect a 25% reduction in the scores of dental plaque and gingival bleeding with a = 0.05 (2 sided), power = 80%, 1%‐3% attrition, means of 11.00 (SD = 1.4) for plaque and of 4.00 (SD = 1.3) for bleeding, the intra‐cluster correlation coefficients being 0.08 and 0.12, respectively, 1 school/arm with 29 children examined in each school was required. To allow the use of normal distribution critical values and possible effects by gender 16 schools (4 schools/arm) were enrolled" (p 521) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "The clusters were not randomly assigned". Method of sequence generation not described |
| Allocation concealment (selection bias) | Unclear risk | Not reported |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Details of the interventions were not explained to the children |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Dental examiner were blinded to group assignment for post‐intervention but baseline examinations was carried out by a separate examiner who was one of the authors, but it was unclear if they were blinded. Calibration between examiners was carried out |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Numbers excluded from analysis are low and similar in each group. Reasons for missing outcome data unlikely to be related to true outcome |
| Selective reporting (reporting bias) | High risk | Post‐intervention data were not reported clearly only baseline data were presented in the tables |
| Other bias | Low risk | No other sources of bias identified |
Worthington 2001.
| Methods |
Study design: Cluster randomised controlled trial (initial phase 2 clusters, secondary phase 3 clusters) Conducted in: Europe, UK Unit of randomisation: School (32 schools) Unit of analysis: School Funded by: National Sugar Bureau |
|
| Participants |
Inclusion criteria: 10‐year old children in year 5 to 6 attending primary schools in research area took part in programme but only those who were provided with positive consent were sampled for clinical exam Exclusion criteria: None reported Age at baseline: Mean age 10.1 years Gender: Not specified in paper but in original MSc document reports groups being equal in analysis Number of participants randomised: Intervention n = 166; Control n = 144 Number of participants evaluated: Intervention n = 146 (4 months); n = 151 (7 months); Control n = 135 (4 months); n = 137 (7 months n = 57 – new active and 80 remaining control) |
|
| Interventions |
Comparison: A school‐based education programme delivered by dental nurses versus non‐intervention control Intervention: My Mouth Matters. 4 x 1 hour lessons in school. Lessons were designed to fit into the national curriculum. Lessons were conducted by specially trained dental facilitator (qualified dental nurse). The intervention was designed to disseminate dental health knowledge to the children. The lessons incorporated group work and home work (3 x 1 hour projects) which required the participation of parents and grandparents. In phase 1 of the study the lessons were spread over 4 months and in phase 2 over 3 months. Control: Not specified Duration of intervention: Phase 1: 4 months; Phase 2: 3 months Post‐intervention: Phase1: 4 months; Phase 2: 3 months Duration of follow‐up: At 4 months and at Phase 1: 7 months and Phase 2: none Behavioural or psychological component: Group work, active learning, school to home, family involvement, repetition, social norms Dental: Knowledge, behaviour‐health link, toothbrushing instruction and skills consisting of demonstration and instruction and the use of disclosure tablets to provide feedback on performance Nutrition: Knowledge dissemination |
|
| Outcomes | Plaque: Silness and Löe – validated outcome measure (conducted on a sample of children) Oral health knowledge questionnaires (not validated). Children completed questionnaires assessing dental health knowledge; child focus groups were conducted and teacher feedback on the programme obtained |
|
| Notes |
Design by/Pilot work: Pilot work with children and teachers to test programme, method of delivery and evaluation materials Power calculation: None reported |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Paper only states "schools were randomly allocated to active and control groups" (p 23). Further information supplied by author confirmed that "randomisation was done by means of a computer generated schedule" |
| Allocation concealment (selection bias) | Low risk | Further information supplied by author, "Randomisation schedule was held by trial statistician and dental nurse was informed which schools were in the active group" |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | No blinding of schools or participants due to nature of intervention but cluster randomisation at the level of the school is deemed by the authors to account for this and is taken into account during the analysis |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Blinding of assessors conducting dental examinations, 1 examiner conducted all exams throughout the trial |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | Plaque index and oral health knowledge scores reported for each group |
| Selective reporting (reporting bias) | Low risk | Plaque index and oral health knowledge questionnaire responses reported for each group |
| Other bias | High risk | The outcome of plaque index was evaluated on a sample of children whose parents returned consent forms (positive consent). This is likely to have introduced bias. The sugar bureau funded the trial, but funders had no influence over the data and analysis |
Zanin 2007.
| Methods |
Study design: Randomised controlled trial (2 arms) Conducted in: South America, Brazil Unit of randomisation: Individual Unit of analysis: Individual Funded by: Not stated |
|
| Participants |
Inclusion criteria: Children were screened in order to only include those at high risk of caries in the study Exclusion criteria: Children suffering from fluorosis, hypoplasia, systemic alteration or who had fixed braces were excluded Age at baseline: Mean age 6 years Gender: Not reported Number of participants randomised: Intervention n = 30, Control n = 30 Number of participants evaluated: Intervention n = 30, Control n = 30 |
|
| Interventions |
Comparison: Intensive education programme and individual supervised brushing versus once yearly supervised brushing and topical fluoride application Intervention: Interventions every 3 months for the 15 months of the study educational programme including group work (active learning). Age specific technique for brushing was taught in order to maximize manual removal of accumulated plaque deposits. During the first month, oral health education sessions were delivered as 4, 30 minute lectures. The sessions were delivered to small groups (n = 10) of children and involved elements of active learning. It was not clear who delivered the intervention. These sessions included general information regarding physiology of the mouth, function and disease, identification of cariogenic foods, influence on plaque formation and education about the behaviour health link and oral health habits. An age specific skills technique for brushing was taught in order to maximize manual removal of accumulated plaque deposits. Every 3 months after these children received supervised brushing sessions with reinforcement of oral health promotion concepts. No links to parents or the home were made Control: 1 annual supervised toothbrushing and dental hygienist applied topical fluoride Duration of intervention: 15 months Post‐intervention: 3 months, 6 months, 9 months, 12 months, 15 months Duration of follow‐up: None Behavioural or psychological component: Modelling, instruction in method, behaviour‐health link Dental: General information including physiology, function and disease. Education about the behaviour health link. Skills for toothbrushing via instruction and supervised practice Nutrition: Identification of cariogenic foods |
|
| Outcomes | Caries: dmfs/DMFS (prevalence) Plaque: Silness and Löe (median values) |
|
| Notes |
Design by/Pilot work: Unclear how the intervention was designed and if any pilot work was conducted Power calculation: "Estimated sample size was based on an expected mean difference of 0.3 between groups with a standard deviation of 0.3. Assuming a power of 0.8 the sample size was 15 children in each group" (p 246) |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | "Raffle made to allocate volunteers randomly to control and experimental groups" (p 247) |
| Allocation concealment (selection bias) | Unclear risk | Paper does not state who conducted the allocation raffle and whether it was concealed from investigators |
| Blinding of participants and personnel (performance bias) All outcomes | Low risk | Double‐blind trial. However it is unclear how participants could be unaware of their allocated treatment group |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | Double‐blind trial (2 assessors both blinded to intervention allocation) |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | All randomised participants included in outcome evaluation |
| Selective reporting (reporting bias) | Low risk | Published report presents all expected outcomes of interest to the review |
| Other bias | Low risk | No other sources of bias identified |
1 BCTs = behaviour change techniques
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Agerbaek 1979 | Children at baseline span the age limit of the inclusion criteria, with the study being conducted not only in a primary school |
| Al‐Jundi 2006 | No cariogenic food content to intervention |
| Anaise 1976 | No cariogenic food component ‐ toothbrushing only |
| Andruskeviciene 2008 | Children too young at the start of the study for the current review (study begins at 3 years of age) |
| Bagramian 1976 | Not a randomised controlled trial |
| Bagramian 1978 | Not a randomised controlled trial |
| Bagramian 1982 | Not a randomised controlled trial ‐ stratified sampling |
| Belloso 1999 | Not a randomised controlled trial |
| Bentley 1983 | No dental outcome data in study |
| Bordoni 2005 | Children too old for current review |
| Bretz 2004 | No cariogenic food component |
| Buischi 1994 | Study participants too old for current review criteria (13 years old) |
| Culler 2011 | Not a randomised controlled trial |
| Curnow 2000 | No cariogenic food component to intervention |
| Curnow 2002 | No cariogenic food component to intervention |
| Davies 2002 | Intervention only provided free toothpaste |
| Davies 2002a | Intervention only provided free toothpaste |
| de Farias 2009 | Not enough description of intervention to determine inclusion criteria components |
| Ekstrand 2000 | Not a randomised controlled trial |
| Ellwood 2004 | No cariogenic food component ‐ free fluoride toothpaste only |
| Englander 1979 | Study participants too old for current review criteria |
| Esfahanizadeh 2011 | No nutritional component ‐ only toothbrushing instruction |
| Feldens 2010 | Study participants too old for current review criteria |
| Fernández 1988 | Not a randomised controlled trial |
| Fernández 1988a | No cariogenic food component ‐ toothbrushing only |
| Ferrazzano 2008 | No cariogenic food component |
| Fischman 1977 | Has a clinical component to intervention (restorative care) so unable to determine effects of behavioural intervention |
| Frencken 2001 | Non‐random allocation to control and intervention group (self selection into training workshops) |
| Graehn 1984 | Not a randomised controlled trial |
| Graves 1975 | Not a randomised controlled trial |
| Grimoud 2005 | Not a randomised controlled trial |
| Grocholewicz 1999 | Insufficient information to confirm if had cariogenic food component to intervention |
| Harrison 2007 | Children in study were too young for the current review |
| Hartono 2002 | Not a randomised controlled trial |
| Hebbal 2011 | Conducted in secondary school even though children are 12 years old |
| Hietasalo 2009 | Not a school‐based intervention |
| Hochstetter 2007 | Although Hochstetter 2007 appears to meet the inclusion criteria for the review, it was not included. Unfortunately, the reporting of this study was exceptionally poor and we could not rely on the information presented. The intervention appeared to be comprehensive and incorporating parents, children and teachers. Attempts to contact the authors to obtain clarification were unsuccessful |
| Holm 1990a | Children in study were too young for the current review |
| Horowitz 1976 | No cariogenic food component ‐ toothbrushing only |
| Horowitz 1977 | No cariogenic food component ‐ toothbrushing only |
| Huang 1996 | Epidemiological survey |
| Jackson 2005 | No cariogenic food component |
| Julien 1994 | No cariogenic food component ‐ toothbrushing and flossing only |
| Kakudate 2009 | Not a school‐based intervention |
| Kerebel 1985a | No cariogenic food component to study intervention |
| Klimek 1987 | No cariogenic food component ‐ tooth cleaning only |
| Kramer 1990 | No cariogenic food component. Children only took part in supervised tooth cleaning and professional plaque removal and local fluoridation |
| Lena 2001 | No cariogenic food component to study |
| Martinez 2004 | Insufficient information unable to access paper in time frame of review ‐ appears to not be a randomised controlled trial |
| Mazzocchi 1997 | Not a randomised controlled trial ‐ states unable to randomise due to sample size |
| Milejczak 2011 | Not a randomised controlled trial ‐ schools are not randomly allocated to treatment or control but selected in survey manor |
| Moorhead 1991 | No cariogenic food component ‐ supervised brushing |
| Morgan 1998a | Study participants too old for the current review |
| Nyandindi 1996 | Randomisation occurs between "conventional session group" and control group. The "modified session group" were from the following school year, and so there was no randomisation. Cariogenic food component was only included in the modified session intervention, so the study does not satisfy our inclusion criteria for the part that is randomised |
| Peng 2004 | This study was not a randomised controlled trial, random allocation was not reported and therefore could not be assumed |
| Peterson 1979 | No cariogenic food component ‐ supervised brushing |
| Pine 2000 | No cariogenic food component to intervention |
| Pine 2007 | No cariogenic food component to intervention |
| Pujol 1996 | Not a randomised controlled trial |
| Roberts‐Thomson 2010 | Children in study too young for the current review |
| Rodrigues 2003 | No cariogenic food component to study |
| Rodrigues 2009 | Not a randomised controlled trial |
| Sagheri 2009 | Cross‐sectional study |
| Schinder 1992 | Paper could not be accessed by review deadline. Paper reported on 4 different educational approaches in oral health material in kindergartens in Israel |
| Schwarz 1998 | Not a randomised controlled trial ‐ field demonstration trial |
| Secades 1995 | Paper could not be accessed by review deadline. Study of corrective feedback and contingency management in establishing dental hygiene |
| Segal 1967 | No cariogenic food component ‐ supervised toothbrushing |
| Stadtler 1981 | No cariogenic food component ‐ supervised brushing |
| Stadtler 1982 | No cariogenic food component ‐ weekly supervised brushing with a sodium fluoride gel |
| Suomi 1980 | No cariogenic food component ‐ toothbrushing only |
| Tagliaferro 2011 | Unable to determine the impact of behavioural intervention due to the clinical aspects included in intervention |
| Tai 2009 | Unable to determine the impact of behavioural intervention due to the clinical aspects included in intervention |
| Tapias 2001 | Not a randomised controlled trial |
| Toassi 2002 | Not a randomised controlled trial |
| Tolvanen 2009 | No clinical outcome ‐ questionnaire on children's oral health related behaviour, knowledge and attitudes |
| Tolvanen 2010a | Study participants too old for the current review (teachers and parents) |
| van Palenstein 1997 | Not a randomised controlled trial |
| Vanobbergen 2004 | Not a randomised controlled trial ‐ schools are not randomly allocated to treatment or control but selected in survey manor |
| Wierzbicka 2002 | Cross‐sectional survey |
| Yamaguchi 1997 | Not a randomised controlled trial ‐ purpose of this study was to investigate the causes of increasing prevalence of dental caries |
Differences between protocol and review
There were insufficient data to allow planned subgroup analyses to be performed in this review.
Contributions of authors
Co‐ordinating the review: Anna Cooper (AC). Developing search strategy and undertaking search for trials: Anne Littlewood (Trials Search Co‐ordinator and Feedback Editor, Cochrane Oral Health Group), Lindsey Dugdill (LD) and AC. Retrieving trials: AC, Lucy O'Malley (LO) and Sarah Elison (SE). Examining search results and retrieved papers against inclusion criteria: AC, LO, SE, Rosemary Armstrong (RA), LD, Pauline Adair (PA). Data extraction: PA, LD, AC, LO. Contacting trial authors for necessary additional information: AC with support from Lucy Fish. Data management and input into RevMan: LO, AC and Girvan Burnside (GB). Analysis and interpretation of data: GB. Writing the review: AC, LO, SE, LD and GB. Plain language summary: RA. Editing the review: LD, RA, Cynthia Pine (CP) and PA. Providing advice on the review: CP, LD and (PA).
Sources of support
Internal sources
No sources of support supplied
External sources
-
Cochrane Oral Health Group Global Alliance, UK.
All reviews in the Cochrane Oral Health Group are supported by Global Alliance member organisations (British Orthodontic Society, UK; British Society of Paediatric Dentistry, UK; Canadian Dental Hygienists Association, Canada; National Center for Dental Hygiene Research & Practice, USA and New York University College of Dentisry, USA) providing funding for the editorial process (http://ohg.cochrane.org/).
-
National Institute for Health Research (NIHR), UK.
CRG funding acknowledgement: The NIHR is the largest single funder of the Cochrane Oral Health Group.
Disclaimer: The views and opinions expressed therein are those of the authors and do not necessarily reflect those of the NIHR, NHS or the Department of Health.
Declarations of interest
None of the identified review authors have any financial or commercial interest that would present a conflict for this review.
New
References
References to studies included in this review
Petrecca 1994 {published data only}
- Petrecca S, D'Arcangelo C, Esposito P, Marco N. A 2‐year evaluation of different methods of dental caries prophylaxis in a sample school‐aged population. Minerva Stomatologica 1994;43(1‐2):23‐8. [PubMed] [Google Scholar]
Saied‐Moallemi 2009 {published and unpublished data}
- Saied‐Moallemi Z, Virtanen JI, Vehkalahti MM, Tehranchi A, Murtomaa H. School‐based intervention to promote preadolescents' gingival health: a community trial. Community Dentistry and Oral Epidemiology 2009;37(6):518‐26. [DOI] [PubMed] [Google Scholar]
Worthington 2001 {published and unpublished data}
- Hill K. An assessment of a dental health education programme. MSc Thesis 1999; Vol. The University of Manchester.
- Worthington HV, Hill KB, Mooney J, Hamilton FA, Blinkhorn AS. A cluster randomized controlled trial of a dental health education program for 10‐year‐old children. Journal of Public Health Dentistry 2001;61(1):22‐7. [DOI] [PubMed] [Google Scholar]
Zanin 2007 {published data only}
- Zanin L, Meneghim MC, Assaf AV, Cortellazzi KL, Pereira AC. Evaluation of an educational program for children with high risk of caries. Journal of Clinical Pediatric Dentistry 2007;31(4):246‐50. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Agerbaek 1979 {published data only}
- Agerbaek N, Melsen B, Lind OP, Glavind L, Kristiansen B. Effect of regular small group instruction per se on oral health status of Danish schoolchildren. Community Dentistry and Oral Epidemiology 1979;7(1):17‐20. [DOI] [PubMed] [Google Scholar]
- Melsen B, Agerbael N. Effect of an instructional motivation program on oral health in Danish adolescents after 1 and 2 years. Community Dentistry and Oral Epidemiology 1980;8(2):72‐8. [DOI] [PubMed] [Google Scholar]
Al‐Jundi 2006 {published data only}
- Al‐Jundi SH, Hammad M, Alwaeli H. The efficacy of a school‐based caries preventive program: a 4‐year study. International Journal of Dental Hygiene 2006;4(1):30‐4. [DOI] [PubMed] [Google Scholar]
Anaise 1976 {published data only}
- Anaise JZ, Zilkah E. The effectiveness of a dental education program on oral cleanliness for school children of 11 to 14 years old. Israel Journal of Dental Medicine 1976;25(4):23‐7. [PubMed] [Google Scholar]
Andruskeviciene 2008 {published data only}
- Andruskeviciene V, Milciuviene S, Bendoraitiene E, Saldunaite K, Vasiliauskiene I, Slabsinskiene E, et al. Oral health status and effectiveness of caries prevention programme in kindergartens in Kaunas city (Lithuania). Oral Health & Preventive Dentistry 2008;6(4):343‐8. [PubMed] [Google Scholar]
Bagramian 1976 {published data only}
- Bagramian RA, Graves RC, Bhat M. A combined approach to preventing dental caries in schoolchildren: caries reductions after one year. Journal of the American Dental Association 1976;93(5):1014‐9. [DOI] [PubMed] [Google Scholar]
Bagramian 1978 {published data only}
- Bagramian RA, Graves RC, Srivastava S. A combined approach to preventing dental caries in schoolchildren: caries reductions after 3 years. Community Dentistry and Oral Epidemiology 1978;6(4):166‐71. [DOI] [PubMed] [Google Scholar]
Bagramian 1982 {published data only}
- Bagramian RA. A 5‐year school‐based comprehensive preventive program in Michigan, U.S.A. Community Dentistry and Oral Epidemiology 1982;10(5):234‐7. [DOI] [PubMed] [Google Scholar]
Belloso 1999 {published data only}
- Belloso N, Hernández N, Rivera L, Morón A. Effectiveness educational programs for school dental health. Experimental trial. Acta Científica Venezolana 1999;50(1):42‐7. [PubMed] [Google Scholar]
Bentley 1983 {published data only}
- Bentley JM, Cormier P, Oler J. The rural dental health program: the effect of a school‐based, dental health education program on children's utilization of dental services. American Journal of Public Health 1983;73(5):500‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bordoni 2005 {published data only}
- Bordoni N, Squassi A, Bellagamba H, Galarza M. Efficiency of a schoolchildren program for oral care. Acta Odontológica Latinoamericana 2005;18(2):75‐81. [PubMed] [Google Scholar]
Bretz 2004 {published data only}
- Bretz W. School children with a high caries experience benefit from supervised tooth brushing equally with 500 ppm and 1450 ppm sodium fluoride toothpastes after a 9‐month study period. Journal of Evidence‐Based Dental Practice 2004;4(2):138‐9. [Google Scholar]
Buischi 1994 {published data only}
- Buischi YA, Axelsson P, Oliveira LB, Mayer MP, Gjermo P. Effect of two preventive programs on oral health knowledge and habits among Brazilian schoolchildren. Community Dentistry and Oral Epidemiology 1994;22(1):41‐6. [DOI] [PubMed] [Google Scholar]
Culler 2011 {published data only}
- Culler CS. An outcomes evaluation of a comprehensive school‐based oral health program. Dissertation Abstracts International: Section B: The Sciences and Engineering 2011;71(7‐B):4148. [Google Scholar]
Curnow 2000 {published data only}
- Curnow M, Pine CM, Burnside G, Nicholson J, Chesters R, Huntington E. A clinical trial of the efficacy of supervised school toothbrushing in high caries risk children. Caries Research 2000;34(4):349 (Abs No 120). [DOI] [PubMed] [Google Scholar]
Curnow 2002 {published data only}
- Curnow MMT, Pine CM, Burnside G, Nicholson JA, Chesters RK, Huntington E. A randomized controlled trial of the efficacy of supervised toothbrushing in high‐caries‐risk children. Caries Research 2002;36(4):294‐300. [DOI] [PubMed] [Google Scholar]
Davies 2002 {published data only}
- Davies GM, Worthington HV, Ellwood RP, Bentley EM. A randomised controlled trial of the effectiveness of providing free fluoride toothpaste during the pre‐school years on reducing caries in 5‐6‐year old children. Journal of Dental Research 2002;81(Spec Iss A):A385 (Abs No 3103). [PubMed] [Google Scholar]
Davies 2002a {published data only}
- Davies GM, Worthington HV, Ellwood RP, Bentley EM, Blinkhorn AS, Taylor GO, et al. A randomised controlled trial of the effectiveness of providing free fluoride toothpaste from the age of 12 months on reducing caries in 5‐6 year old children. Community Dental Health 2002;19(3):131‐6. [PubMed] [Google Scholar]
de Farias 2009 {published data only}
- Farias IA, Araújo Souza GC, Ferreira MA. A health education program for Brazilian public schoolchildren: the effects on dental health practice and oral health awareness. Journal of Public Health Dentistry 2009;69(4):225‐30. [DOI] [PubMed] [Google Scholar]
Ekstrand 2000 {published data only}
- Ekstrand KR, Kuzmina IN, Kuzmina E, Christiansen ME. Two and a half‐year outcome of caries‐preventive programs offered to groups of children in the Solntsevsky district of Moscow. Caries Research 2000;34(1):8‐19. [DOI] [PubMed] [Google Scholar]
Ellwood 2004 {published data only}
- Ellwood RP, Davies GM, Worthington HV, Blinkhorn AS, Taylor GO, Davies RM. Relationship between area deprivation and the anticaries benefit of an oral health programme providing free fluoride toothpaste to young children. Community Dentistry and Oral Epidemiology 2004;32(3):159‐65. [DOI] [PubMed] [Google Scholar]
Englander 1979 {published data only}
- Englander HR. Supervised deplaquing and improved gingival health in a school program. Journal of Periodontology 1979;50(8):394‐6. [DOI] [PubMed] [Google Scholar]
Esfahanizadeh 2011 {published data only}
- Esfahanizadeh N. Dental health education programme for 6‐year‐olds: a cluster randomised controlled trial. European Journal of Paediatric Dentistry 2011;12(3):167‐70. [PubMed] [Google Scholar]
Feldens 2010 {published data only}
- Feldens CA, Giugliani ER, Duncan BB, Drachler Mde L, Vitolo MR. Long‐term effectiveness of a nutritional program in reducing early childhood caries: a randomized trial. Community Dentistry and Oral Epidemiology 2010;38(4):324‐32. [DOI] [PubMed] [Google Scholar]
Fernández 1988 {published data only}
- Fernández Parra A. Development of dental hygiene skills in children by means of procedures of behavioral intervention. Avances en Psicología Clínica Latinoamericana 1988;6:77‐94. [Google Scholar]
Fernández 1988a {published data only}
- Fernández Parra A, Gil Roales‐Nieto J. Health education and behavioral intervention in the development of dental hygiene habits (toothbrushing) in the elementary school.. Análisis y Modificación de Conducta 1988;14(41):383‐99. [Google Scholar]
Ferrazzano 2008 {published data only}
- Ferrazzano GF, Cantile T, Sangianantoni G, Ingenito A. Effectiveness of a motivation method on the oral hygiene of children. European Journal of Paediatric Dentistry 2008;9(4):183‐7. [PubMed] [Google Scholar]
Fischman 1977 {published data only}
- Fischman SL, English JA, Albino JE, Bissell GD, Greenberg JS, Juliano DB, et al. A comprehensive caries control program‐‐design and evaluation of the clinical trial. Journal of Dental Research 1977;56(Spec Iss):C99‐103. [DOI] [PubMed] [Google Scholar]
Frencken 2001 {published data only}
- Frencken JE, Borsum‐Andersson K, Makoni F, Moyana F, Mwashaenyi S, Mulder J. Effectiveness of an oral health education programme in primary schools in Zimbabwe after 3.5 years. Community Dentistry and Oral Epidemiology 2001;29(4):253‐9. [DOI] [PubMed] [Google Scholar]
Graehn 1984 {published data only}
- Graehn G, Toutenburg H. Health education program for pre‐school children. 2. Effect on caries morbidity. Stomatologie der DDR 1984;34(5):293‐7. [PubMed] [Google Scholar]
Graves 1975 {published data only}
- Graves RC, McNeal DR, Haefner DP, Ware BG. A comparison of the effectiveness of the "Toothkeeper" and a traditional dental health education program. Journal of Public Health Dentistry 1975;35(2):85‐90. [DOI] [PubMed] [Google Scholar]
Grimoud 2005 {published data only}
- Grimoud AM, Verchere AC, Lodter JP, Sudre MC, Remesy MC, Charras P. Caries free smile: a dental health educational programme. Archives de Pédiatrie 2005;12(1):28‐33. [DOI] [PubMed] [Google Scholar]
Grocholewicz 1999 {published data only}
- Grocholewicz K. The effect of selected prophylactic‐educational programs on oral hygiene, periodontium and caries in school children during a 4‐year observation. Annales Academiae Medicae Stetinensis 1999;45:265‐83. [PubMed] [Google Scholar]
Harrison 2007 {published data only}
- Harrison R, Benton T, Everson‐Stewart S, Weinstein P. Effect of motivational interviewing on rates of early childhood caries: a randomized trial. Pediatric Dentistry 2007;29(1):16‐22. [PubMed] [Google Scholar]
Hartono 2002 {published data only}
- Hartono SW, Lambri SE, Palenstein Helderman WH. Effectiveness of primary school‐based oral health education in West Java, Indonesia. International Dental Journal 2002;52(3):137‐43. [DOI] [PubMed] [Google Scholar]
Hebbal 2011 {published data only}
- Hebbal M, Ankola AV, Vadavi D, Patel K. Evaluation of knowledge and plaque scores in school children before and after health education. Dental Research Journal 2011;8(4):189‐96. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hietasalo 2009 {published data only}
- Hietasalo P, Seppa L, Lahti S, Niinimaa A, Kallio J, Aronen P, et al. Cost‐effectiveness of an experimental caries‐control regimen in a 3.4‐yr randomized clinical trial among 11‐12‐yr‐old Finnish schoolchildren. European Journal of Oral Sciences 2009;117(6):728‐33. [DOI] [PubMed] [Google Scholar]
Hochstetter 2007 {published data only}
- Hochstetter AS, Lombardo MJ, D'eramo L, Piovano S, Bordoni N. Effectiveness of a preventive educational programme on the oral health of preschool children. Promotion et Education 2007;14(3):155‐8. [PubMed] [Google Scholar]
Holm 1990a {published data only}
- Holm AK. Education and diet in the prevention of caries in the preschool‐child. Journal of Dentistry 1990;18(6):308‐14. [DOI] [PubMed] [Google Scholar]
Horowitz 1976 {published data only}
- Horowitz AM, Suomi JD, Peterson JK, Voglesong RH, Mathews BL. Effects of supervised daily dental plaque removal by children: first‐year results. Journal of Public Health Dentistry 1976;36(3):193‐200. [DOI] [PubMed] [Google Scholar]
Horowitz 1977 {published data only}
- Horowitz AM, Suomi JD, Peterson JK, Lyman BA. Effects of supervised daily dental plaque removal by children: II. 24 months' results. Journal of Public Health Dentistry 1977;37(3):180‐8. [DOI] [PubMed] [Google Scholar]
Huang 1996 {published data only}
- Huang ST, Chen HS, Yu GW, Tsuang SY. The patterns of dental caries of preschool children in Kaohsiung City Taiwan. Kaohsiung Journal of Medical Sciences 1996;12(7):417‐22. [PubMed] [Google Scholar]
Jackson 2005 {published data only}
- Jackson RJ, Newman HN, Smart GJ, Stokes E, Hogan JI, Brown C, et al. The effects of a supervised toothbrushing programme on the caries increment of primary school children, initially aged 5‐6 years. Caries Research 2005;39(2):108‐15. [DOI] [PubMed] [Google Scholar]
Julien 1994 {published data only}
- Julien MG. The effect of behaviour modification techniques on oral hygiene and gingival health of 10‐year‐old Canadian children. International Journal of Paediatric Dentistry 1994;4(1):3‐11. [DOI] [PubMed] [Google Scholar]
Kakudate 2009 {published data only}
- Kakudate N, Morita M, Sugai M, Kawanami M. Systematic cognitive behavioral approach for oral hygiene instruction: a short‐term study. Patient Education and Counseling 2009;74(2):191‐6. [DOI] [PubMed] [Google Scholar]
Kerebel 1985a {published data only}
- Kerebel LM, Cabellec MT, Daculsi G, Kerebel B. Report on caries reduction in French schoolchildren 3 years after the introduction of a preventive program. Community Dentistry and Oral Epidemiology 1985;13(4):201‐4. [DOI] [PubMed] [Google Scholar]
Klimek 1987 {published data only}
- Klimek J, Prinz H, Hellwig E. Effect of a preventive program on plaque, gingivitis and caries in school children after 3 years. Deutsche Zahnarztliche Zeitschrift 1987;42(2):146‐50. [PubMed] [Google Scholar]
Kramer 1990 {published data only}
- Kramer N, Kunzelmann KH, Hickel R. Middle course between group and individual preventive programs. Deutsche Zahnarztliche Zeitschrift 1990;45(11):706‐9. [PubMed] [Google Scholar]
Lena 2001 {published data only}
- Lena PB, Looi LL, Normala MR, Vijayamanohar K. Effectiveness of supervised daily tooth‐brushing amongst primary school children in Pahang. International Dental Journal 2001;51(5):374. [Google Scholar]
Martinez 2004 {published data only}
- Martinez BM, Sanchez‐Balmisa C, Parga MX. Behavioral intervention in dental health: A preliminary result of a school program. Análisis y Modificación de Conducta 2004;30(129):51‐69. [Google Scholar]
Mazzocchi 1997 {published data only}
- Mazzocchi AR, Moretti R. Effectiveness of a dental preventive program on plaque index results in 8‐year‐old children of Bergamo, Italy. Community Dentistry and Oral Epidemiology 1997;25(4):332‐3. [DOI] [PubMed] [Google Scholar]
Milejczak 2011 {published data only}
- Milejczak CB. The impact of school‐based oral hygiene education on the oral‐health‐related quality of life. Dissertation Abstracts International: Section B: The Sciences and Engineering 2011;72(4‐B):2061. [Google Scholar]
Moorhead 1991 {published data only}
- Moorhead JE, Conti AJ, Marks RG, Cancro LP. The effect of supervised brushing on caries inhibition in school age children. The Journal of Clinical Dentistry 1991;2(4):97‐102. [PubMed] [Google Scholar]
Morgan 1998a {published data only}
- Morgan MV, Campain AC, Adams GG, Crowley SJ, Wright FA. The efficacy and effectiveness of a primary preventive dental programme in non‐fluoridated areas of Victoria, Australia. Community Dental Health 1998;15(4):263‐71. [PubMed] [Google Scholar]
Nyandindi 1996 {published data only}
- Nyandindi U, Milén A, Palin‐Palokas T, Robison V. Impact of oral health education on primary school children before and after teachers' training in Tanzania. Health Promotion International 1996;11(3):193‐201. [Google Scholar]
Peng 2004 {published data only}
- Peng B, Petersen PE, Bian Z, Tai B, Jiang H. Can school‐based oral health education and a sugar‐free chewing gum program improve oral health? Results from a two‐year study in PR China. Acta Odontologica Scandinavica 2004;62(6):328‐32. [DOI] [PubMed] [Google Scholar]
Peterson 1979 {published data only}
- Peterson JK. A supervised brushing trial of sodium monofluorophosphate dentifrices in a fluoridated area. Caries Research 1979;13(2):68‐72. [DOI] [PubMed] [Google Scholar]
Pine 2000 {published data only}
- Pine CM, McGoldrick PM, Burnside G, Curnow MM, Chesters RK, Nicholson J, et al. An intervention programme to establish regular toothbrushing: understanding parents' beliefs and motivating children. International Dental Journal 2000;50(S6_Part1):312‐23. [DOI] [PubMed] [Google Scholar]
Pine 2007 {published data only}
- Pine CM, Curnow MM, Burnside G, Nicholson JA, Roberts AJ. Caries prevalence four years after the end of a randomised controlled trial. Caries Research 2007;41(6):431‐6. [DOI] [PubMed] [Google Scholar]
Pujol 1996 {published data only}
- Pujol MT, Betlla E, Coma C, Cena B, González M, Fernández MA. Evaluation of a 4‐year dental hygiene preventive program of the Les Planes health district in Sant Joan Despi (Barcelona). Atención Primaria 1996;17(8):523‐6. [PubMed] [Google Scholar]
Roberts‐Thomson 2010 {published data only}
- Roberts‐Thomson KF, Slade GD, Bailie RS, Endean C, Simmons B, Leach AJ, et al. A comprehensive approach to health promotion for the reduction of dental caries in remote Indigenous Australian children: a clustered randomised controlled trial. International Dental Journal 2010;60(3 Suppl 2):245‐9. [PubMed] [Google Scholar]
Rodrigues 2003 {published data only}
- Rodrigues JA, dos Santos PA, Garcia PP, Corona SA, Loffredo LC. Evaluation of motivation methods used to obtain appropriate oral hygiene levels in schoolchildren. International Journal of Dental Hygiene 2003;1(4):227‐32. [DOI] [PubMed] [Google Scholar]
Rodrigues 2009 {published data only}
- Rodrigues JA, dos Santos PA, Baseggio W, Corona SA, Palma‐Dibb RG, Garcia PP. Oral hygiene indirect instruction and periodic reinforcements: effects on index plaque in schoolchildren. Journal of Clinical Pediatric Dentistry 2009;34(1):31‐4. [DOI] [PubMed] [Google Scholar]
Sagheri 2009 {published data only}
- Sagheri D, Wassmer G, Hahn P, McLoughlin J. Dental caries experience of schoolchildren of two different oral health care delivery systems. International Dental Journal 2009;59(3):161‐7. [PubMed] [Google Scholar]
Schinder 1992 {published data only}
- Schinder EOM, Rosenberg M, Zangwill L. Educational approach to modifying dental habits in pre‐school children [Ensayo educacional de modificación de los hábitos dentales en niños de edad preescolar]. Revista Asociación Odontológica Argentina 1992;80(4):225‐30. [Google Scholar]
Schwarz 1998 {published data only}
- Schwarz E, Lo EC, Wong MC. Prevention of early childhood caries‐‐results of a fluoride toothpaste demonstration trial on Chinese preschool children after three years. Journal of Public Health Dentistry 1998;58(1):12‐8. [DOI] [PubMed] [Google Scholar]
Secades 1995 {published data only}
- Secades Villa R, Fernandez Rodriguez C. Efficiency of corrective feedback and contingency management in establishing dental hygiene in children. Análisis y Modificación de Conducta 1995;21(77):397‐417. [Google Scholar]
Segal 1967 {published data only}
- Segal AH, Stiff RH, George WA, Picozzi A. Cariostatic effect of a stannous fluoride‐containing dentifrice on children: two‐year report of a supervised toothbrushing study. Journal of Oral Therapeutics and Pharmacology 1967;4(3):175‐80. [PubMed] [Google Scholar]
Stadtler 1981 {published data only}
- Stadtler P. Medical‐educational effect of supervised oral hygiene exercises. Results after a year. Osterreichische Zeitschrift fur Stomatologie 1981;78(6):228‐34. [PubMed] [Google Scholar]
Stadtler 1982 {published data only}
- Stadtler P. Results of a 3‐year clinical, experimental double‐blind study with weekly supervised brushing with a sodium fluoride gel. Osterreichische Zeitschrift fur Stomatologie 1982;79(3):83‐99. [PubMed] [Google Scholar]
Suomi 1980 {published data only}
- Suomi JD, Peterson JK, Matthews BL, Voglesong RH, Lyman BA. Effects of supervised daily dental plaque removal by children after 3 years. Community Dentistry and Oral Epidemiology 1980;8(4):171‐6. [DOI] [PubMed] [Google Scholar]
Tagliaferro 2011 {published data only}
- Tagliaferro EP, Pardi V, Ambrosano GM, Meneghim Mde C, Silva SR, Pereira AC. Occlusal caries prevention in high and low risk schoolchildren. A clinical trial. American Journal of Dentistry 2011;24(2):109‐14. [PubMed] [Google Scholar]
Tai 2009 {published data only}
- Tai BJ, Jiang H, Du MQ, Peng B. Assessing the effectiveness of a school‐based oral health promotion programme in Yichang City, China. Community Dentistry and Oral Epidemiology 2009;37(5):391‐8. [DOI] [PubMed] [Google Scholar]
Tapias 2001 {published data only}
- Tapias MA, Miguel G, Jimenez‐Garcia R, Gonzalez A, Dominguez V. Incidence of caries in an infant population in Mostoles, Madrid. Evaluation of a preventive program after 7.5 years of follow‐up. International Journal of Paediatric Dentistry 2001;11(6):440‐6. [DOI] [PubMed] [Google Scholar]
Toassi 2002 {published data only}
- Toassi RF, Petry PC. Motivation on plaque control and gingival bleeding in school children. Revista de Saude Publica 2002;36(5):634‐7. [DOI] [PubMed] [Google Scholar]
Tolvanen 2009 {published data only}
- Tolvanen M, Lahti S, Poutanen R, Seppa L, Pohjola V, Hausen H. Changes in children's oral health‐related behavior, knowledge and attitudes during a 3.4‐yr randomized clinical trial and oral health‐promotion program. European Journal of Oral Sciences 2009;117(4):390‐7. [DOI] [PubMed] [Google Scholar]
Tolvanen 2010a {published data only}
- Tolvanen M, Lahti S, Hausen H. Changes in toothbrushing frequency in relation to changes in oral health‐related knowledge and attitudes among children ‐ a longitudinal study. European Journal of Oral Sciences 2010;118(3):284‐9. [DOI] [PubMed] [Google Scholar]
Vanobbergen 2004 {published data only}
- Vanobbergen J, Declerck D, Mwalili S, Martens L. The effectiveness of a 6‐year oral health education programme for primary schoolchildren. Community Dentistry and Oral Epidemiology 2004;32(3):173‐82. [DOI] [PubMed] [Google Scholar]
van Palenstein 1997 {published data only}
- Palenstein Helderman WH, Munck L, Mushendwa S, van't Hof MA, Mrema FG. Effect evaluation of an oral health education programme in primary schools in Tanzania. Community Dentistry and Oral Epidemiology 1997;25(4):296‐300. [DOI] [PubMed] [Google Scholar]
Wierzbicka 2002 {published data only}
- Wierzbicka M, Petersen PE, Szatko F, Dybizbanska E, Kalo I. Changing oral health status and oral health behaviour of schoolchildren in Poland. Community Dental Health 2002;19(4):243‐50. [PubMed] [Google Scholar]
Yamaguchi 1997 {published data only}
- Yamaguchi N, Saito T, Oho T, Sumi Y, Yamashita Y, Koga T. Influence of the discontinuation of a school‐based, supervised fluoride mouthrinsing programme on the prevalence of dental caries. Community Dental Health 1997;14(4):258‐61. [PubMed] [Google Scholar]
Additional references
Abraham 2008
- Abraham C, Michie S. A taxonomy of behavior change techniques used in interventions. Health Psychology 2008;27(3):379‐87. [DOI] [PubMed] [Google Scholar]
Ajzen 1991
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes 1991;50(2):179‐211. [Google Scholar]
Amin 2009
- Amin MS, Harrison RL. Understanding parents' oral health behaviors for their young children. Qualitative Health Research 2009;19(1):116‐27. [DOI] [PubMed] [Google Scholar]
Armfield 2009
- Armfield JM, Spencer AJ, Slade GD. Changing inequalities in the distribution of caries associated with improving child oral health in Australia. Journal of Public Health Dentistry 2009;69(2):125‐34. [DOI] [PubMed] [Google Scholar]
Aunger 2007
- Aunger R. Tooth brushing as routine behaviour. International Dental Journal 2007;57 Suppl 5:364‐76. [Google Scholar]
Bandura 1986
- Bandura, A. Social Foundations of Thought and Action: a Social Cognitive Theory. London: Prentice‐Hall, 1986. [Google Scholar]
Bartholomew 2011
- Bartholomew LK, Parcel GS, Kok G, Gottlieb NH, Fernandez ME . Planning Health Promotion Programs: An Intervention Mapping Approach. 3rd Edition. San Francisco: Jossey‐Bass, 2011. [Google Scholar]
Blinkhorn 2001
- Blinkhorn AS, Wainwright‐Stringer YM, Holloway PJ. Dental health knowledge and attitudes of regularly attending mothers of high‐risk, pre‐school children. International Dental Journal 2001;51(6):435‐8. [DOI] [PubMed] [Google Scholar]
Brukiene 2006
- Brukiene V, Aleksejuniene J, Balciuniene I. Is dental treatment experience related to dental anxiety? A cross‐sectional study in Lithuanian adolescents. Stomatologija 2006;8(4):108‐15. [PubMed] [Google Scholar]
Casamassimo 2009
- Casamassimo PS, Thikkurissy S, Edelstein BL, Maiorini E. Beyond the dmft: the human and economic cost of early childhood caries. Journal of the American Dental Association 2009;140(6):650‐7. [DOI] [PubMed] [Google Scholar]
CONSORT 2010
- Schulz KF, Altman DG, Moher D, CONSORT Group. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Medicine 2010;7(3):e1000251. [DOI] [PMC free article] [PubMed] [Google Scholar]
Edelstein 2000
- Edelstein BL. Access to dental care for Head Start enrollees. Journal of Public Health Dentistry 2000;60(3):221‐9. [DOI] [PubMed] [Google Scholar]
Edelstein 2006
- Edelstein BL. The dental caries pandemic and disparities problem. BMC Oral Health 2006;6 Suppl 1:S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eitner 2006
- Eitner S, Wichmann M, Paulsen A, Holst S. Dental anxiety ‐ an epidemiological study on its clinical correlation and effects on oral health. Journal of Oral Rehabilitation 2006;33(8):588‐93. [DOI] [PubMed] [Google Scholar]
Exley 2009
- Exley C. Bridging a gap: the (lack of a) sociology of oral health and healthcare. Sociology of Health & Illness 2009;31(7):1093‐108. [DOI] [PubMed] [Google Scholar]
Festinger 1954
- Festinger L. A Theory of Social Comparison Processes. Indianapolis: Bobbs‐Merrill, 1954. [Google Scholar]
Fishbein 1975
- Fishbein M, Ajzen I. Belief, Attitude, Intention and Behavior: an Introduction to Theory and Research. London: Addison‐Wesley, 1975. [Google Scholar]
Fisher 1994
- Fisher J, Fisher W, Malloy T. Empirical tests of an information‐motivation‐behavioral skills model of AIDS‐preventive behavior with gay men and heterosexual university students. Health Psychology 1994;13:238‐50. [DOI] [PubMed] [Google Scholar]
Freeman 2009
- Freeman R, Ismail A. Assessing patients' health behaviours. Essential steps for motivating patients to adopt and maintain behaviours conducive to oral health. Monographs in Oral Science 2009;21:113‐27. [DOI] [PubMed] [Google Scholar]
Gibson 2008
- Gibson B. Cultural history of the mouth and teeth. Cultural Encyclopaedia of the Body. Westport: Greenwood Press, 2008. [Google Scholar]
Glasser 1985
- Glasser W. Control Theory: A New Explanation of How We Control Our Lives. London: Harper and Row, 1985. [Google Scholar]
Goffman 1990
- Goffman E. Stigma ‐ Notes on the Management of Spoiled Identity. London: Penguin Books, 1990. [Google Scholar]
Graham 2005
- Graham H. Intellectual disabilities and socioeconomic inequalities in health: an overview of research. Journal of Applied Research in Intellectual Disabilities 2005;18(2):101‐11. [Google Scholar]
Gussy 2006
- Gussy MG, Waters EG, Walsh O, Kilpatrick NM. Early childhood caries: current evidence for aetiology and prevention. Journal of Paediatrics and Child Health 2006;42(1‐2):37‐43. [DOI] [PubMed] [Google Scholar]
Harris 2012
- Harris RV, Gamboa A, Dailey Y, Ashcroft A. One‐to‐one dietary interventions undertaken in a dental setting to change dietary behaviour. Cochrane Database of Systematic Reviews 2012, Issue 3. [DOI: 10.1002/14651858.CD006540.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.
Hupcey 1998
- Hupcey J. Clarifying the social support theory‐research linkage. Journal of Advanced Nursing 1998;27:1231‐41. [DOI] [PubMed] [Google Scholar]
Jackson 2011
- Jackson SL, Vann WF Jr, Kotch JB, Pahel BT, Lee JY. Impact of poor oral health on children's schools attendance and performance. American Journal of Public Health 2011;101(10):1900‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kay 1996
- Kay EJ, Locker D. Is dental health education effective? A systematic review of current evidence. Community Dentistry and Oral Epidemiology 1996;24(4):231‐5. [DOI] [PubMed] [Google Scholar]
Kay 1998
- Kay EJ, Locker D. A systematic review of the effectiveness of health promotion aimed at improving oral health. Community Dental Health 1998;15(3):132‐44. [PubMed] [Google Scholar]
Kwan 2005
- Kwan SY, Petersen PE, Pine C, Borutta A. Health‐promoting schools: an opportunity for oral health promotion. Bulletin of the World Health Organization 2005;83(9):677‐85. [PMC free article] [PubMed] [Google Scholar]
Lazarus 1966
- Lazarus R. Psychological Stress and the Coping Process. New York: McGraw‐Hill, 1966. [Google Scholar]
Marlatt 1998
- Marlatt G, George A, William H. Relapse prevention and the maintenance of optimal health. In: Shumaker SA, Schron EB, Ockene JK, McBee WL editor(s). The Handbook of Health Behavior Change. 2nd Edition. New York: Springer Publishing, 1998:33‐58. [Google Scholar]
Martin 2010
- Martin L, Haskard‐Zolnierek K, Dimatteo M. Health Behaviour Change and Treatment Adherence: Evidence Based Guideline of Improving Health Care. New York: Oxford University Press, 2010. [Google Scholar]
Michie 2008
- Michie S, Johnston M, Francis J, Hardeman W, Eccles M. From theory to intervention: mapping theoretically derived behavioural determinants to behaviour change techniques. Applied Psychology 2008;57(4):660‐80. [Google Scholar]
Michie 2012
- Michie S, Johnston M. Theories and techniques of behaviour change: Developing a cumulative science of behaviour change. Health Psychology Review 2012;6(1):1‐6. [DOI] [PubMed] [Google Scholar]
MRC 2000
- Medical Research Council. A Framework for the Development and Evaluation of RCTs for Complex Interventions to Improve Health. Medical Research Council. London, 2000.
MRC 2008
- Medical Research Council. Developing and Evaluating Complex Interventions: New Guidance. Medical Research Council. London, 2008.
Mullen 2005
- Mullen J. History of water fluoridation. British Dental Journal 2005;199(7 Suppl):1‐4. [DOI] [PubMed] [Google Scholar]
NICE 2007
- National Institute for Health and Care Excellence (NICE). Behaviour Change at Population, Community and Individual Levels. Public Health Guidance 6 2007.
Nunn 2006
- Nunn JH. The burden of oral ill health for children. Archives of Disease in Childhood 2006;91(3):251‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Oakley 2006
- Oakley A, Strange V, Bonell C, Allen E, Stepenson J. Process evaluation in randomised controlled trials. BMJ 2006;18(332):413‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petersen 2005
- Petersen PE, Bourgeois D, Ogawa H, Estupinan‐Day S, Ndiaye C. The global burden of oral diseases and risks to oral health. Bulletin of the World Health Organization 2005;83(9):661‐9. [PMC free article] [PubMed] [Google Scholar]
Pine 2004a
- Pine C, Adair PM, Nicoll AD, Burnside G, Petersen PE, Beighton D, et al. International comparisons of health inequalities in childhood dental caries. Community Dental Health 2004;21(1 Suppl):121‐30. [PubMed] [Google Scholar]
Pine 2004b
- Pine C, Adair PM, Petersen PE, Douglass C, Burnside G, Nicoll AD, et al. Developing explanatory models of health inequalities in childhood dental caries. Community Dental Health 2004;21(1 Suppl):86‐95. [PubMed] [Google Scholar]
Pine 2006
- Pine C, Harris RV, Burnside G, Merrett MC. An investigation of the relationship between untreated decayed teeth and dental sepsis in 5‐year‐old children. British Dental Journal 2006;200(1):45‐7. [DOI] [PubMed] [Google Scholar]
Ramos‐Gomez 2002
- Ramos‐Gomez F, Jue B, Bonta CY. Implementing an infant oral care program. Journal of the California Dental Association 2002;30(10):752‐61. [PubMed] [Google Scholar]
Reisine 2001
- Reisine ST, Psoter W. Socioeconomic status and selected behavioral determinants as risk factors for dental caries. Journal of Dental Education 2001;65(10):1009‐16. [PubMed] [Google Scholar]
Shaw 2009
- Shaw D, Macpherson L, Conway D. Tackling socially determined dental inequalities: ethical aspects of Childsmile, the national child oral health demonstration programme in Scotland. Bioethics 2009;23(2):131‐9. [DOI] [PubMed] [Google Scholar]
Sheiham 2005
- Sheiham A. Oral health, general health and quality of life. Bulletin of the World Health Organization 2005;83(9):644. [PMC free article] [PubMed] [Google Scholar]
Sheiham 2006
- Sheiham A. Dental caries affects body weight, growth and quality of life in pre‐school children. British Dental Journal 2006;201(10):625‐6. [DOI] [PubMed] [Google Scholar]
Shiboski 2003
- Shiboski CH, Gansky SA, Ramos‐Gomez F, Ngo L, Isman R, Pollick HF. The association of early childhood caries and race/ethnicity among California pre‐school children. Journal of Public Health Dentistry 2003;63(1):38‐46. [DOI] [PubMed] [Google Scholar]
Skinner 1953
- Skinner B. Science and Human Behaviour. Oxford, England: Macmillan, 1953. [Google Scholar]
Stillman‐Lowe 2008
- Stillman‐Lowe C. Oral health education: What lessons have we learned?. Oral Health Report 2008;2:9‐13. [Google Scholar]
Surgeon General 2000
- U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Dental and Craniofacial Research. Oral Health in America: a Report of the Surgeon General. Office of the Surgeon General 2000; Vol. NIH Publication Number 00‐4713.
Waters 2011
- Waters E, Silva‐Sanigorski A, Hall BJ, Brown T, Campbell KJ, Gao Y, et al. Interventions for preventing obesity in children. Cochrane Database of Systematic Reviews 2011, Issue 12. [DOI: 10.1002/14651858.CD001871.pub3] [DOI] [PubMed] [Google Scholar]
Watson 2011
- Watson PM, Dugdill L, Pickering K, Bostock S, Hargreaves J, Staniford L, et al. A whole family approach to childhood obesity management (GOALS): Relationship between adult and child BMI change. Annals of Human Biology 2011;38(4):445‐52. [DOI] [PubMed] [Google Scholar]
Watt 1999
- Watt R, Sheiham A. Inequalities in oral health: a review of the evidence and recommendations for action. British Dental Journal 1999;187(1):6‐12. [DOI] [PubMed] [Google Scholar]
Watt 2001
- Watt R, Fuller S, Harnett R, Treasure E, Stillman‐Lowe C. Oral health promotion evaluation ‐ time for development. Community Dentistry and Oral Epidemiology 2001;29(3):161‐6. [DOI] [PubMed] [Google Scholar]
Watt 2007
- Watt R. From victim blaming to upstream action: tackling the social determinants of oral health inequalities. Community Dentistry and Oral Epidemiology 2007;35(1):1‐11. [DOI] [PubMed] [Google Scholar]


