Abstract
Background:
Large-scale power outages (PO) are increasing in the context of climate change. Although some research has been conducted into the adverse health impacts of POs, significant gaps remain regarding whether POs would affect the health of pregnant women. We investigated the association between ED visits due to pregnancy complications and the occurence, intensity, and duration of large-scale POs in eight Sandy-affected counties in New York State (NYS).
Methods:
In this cross-sectional study, daily ED visits for pregnancy complications and large-scale PO data in eight counties in NYS from October to December in 2005–2014 were collected. Using time-series analysis, we estimated the relative increase in ED visits for pregnancy complications during POs compared with non-PO periods at lag 0–7 days. Short-term health impacts of PO intensity and PO duration were investigated. Estimations were also stratified by sociodemographic characteristics and disease subtypes including threatened or spontaneous abortion, threatened or early labor, hypertension complications, infections of genitourinary tract, renal diseases, gestational diabetes mellitus, mental illnesses, and cardiovascular diseases during pregnancy.
Results:
From October to December in 2005–2014, there were 307,739 ED visits for pregnancy complications in the eight counties. We found significant increases in ED visits for overall pregnancy complications (16.6%, 95% confidence interval [CI]: 10.3%, 23.2%) during the Hurricane-PO period at lag 0–7 days. The ED visits increased by 8.8% per level increase in PO intensity and 1.4% per day increase in PO duration. Specifically, threatened/early delivery and gestational diabetes mellitus during the PO period increased by 26.7% (95% CI: 8.2%, 48.4%) and 111.8% (95% CI: 16.7%, 284.4%), respectively. Young adult, Black, Hispanic, and uninsured individuals were at higher risk of complications.
Conclusions:
POs may adversely impact pregnancy, especially for certain pregnancy complications and among low sociodemographic women.
Keywords: Natural disaster, Hurricane, Power outage, Pregnancy health
Graphical Abstract

1. Introduction
The frequency and intensity of extreme weather events, such as heatwaves, floods, and hurricanes have increased in the last 20 years (Stocker, 2014) and are projected to continue to increase worldwide. An increase in severe weather events have caused more frequent large-scale power outages (PO) (Campbell, 2012; Kenward and Raja, 2014; Klinger and Owen Landeg, 2014; Panteli and Mancarella, 2015). Between 2003 and 2012, an estimated 679 widespread POs occurred due to severe weather in the United States (U.S.) (House, 2013).
In October 2012, Hurricane Sandy (Sandy) made landfall and decimated areas along the northeastern U.S. coastline (Casey-Lockyer et al., 2013). Hurricane Sandy caused extensive damage to infrastructure and resulted in one of the largest POs in U.S. history. The outages during and after Hurricane Sandy lasted more than two weeks, with more than 8.5 million households and businesses affected (FEMA, 2013). In September 2017, Hurricane Maria made landfall in Puerto Rico (Orengo-Aguayo et al., 2019), destroying much of the island’s infrastructure and electrical grid, and leaving more than 100,000 Puerto Ricans without power for over seven months (Houser and Marsters, 2018). Understanding how health will be affected by weather-related PO is critical for future planning and intervention (Shultz and Galea, 2017).
Several studies have reported multiple adverse health impacts of PO (Dominianni et al., 2018; Klinger and Owen Landeg, 2014) including increases in rates of both mortality (Anderson and Bell, 2012; Dominianni et al., 2018) and morbidity of respiratory, renal, and mental diseases (Lin et al., 2011; Lin et al., 2016; Lurie et al., 2015), as well as carbon monoxide (CO) poisoning (Lutterloh et al., 2011). Certain people tend to be affected by PO more than others because of their age, health or physical status, and other sociodemographic characteristics (Klinger and Owen Landeg, 2014). Pregnant women undergo great physical and emotional changes throughout their pregnancy, which potentially makes them more vulnerable to extreme weather events (Oni et al., 2015). Previous studies have suggested that environmental hazards (heatwave, hurricane, air pollution) may threaten the health of pregnant women, resulting in adverse pregnancy outcomes, such as preterm delivery (He et al., 2016) and low birth weight (Rylander et al., 2013). Lin et al. (2011) reported that women were more like to be hospitalized during the 2003 Northeast Blackout in New York City (NYC) (Lin et al., 2011). However, little is known about the relationship between large-scale PO and pregnancy complications, such as spontaneous abortion, premature labor, and diseases during pregnancy. In addition, POs vary in terms of coverage and duration, which may affect health (House, 2013). To the best of our knowledge, no prior studies have systematically evaluated the association of the intensity and duration of POs with prenatal health.
In this study, we investigated the relationship between emergency department (ED) visits for pregnancy complications and POs, including intensity and duration, after Sandy in New York State (NYS). We also evaluated potential disease and population vulnerabilities from the PO.
2. Materials and methods
2.1. Study design and study population
Following a time series design, we compared the rate of ED visits due to pregnancy complications on PO days (the case period, in 2012) against the same types of visits on other days (the control period), during the study period from October–December 2005–2014. The health impacts of POs were evaluated in terms of occurrence (Yes/No), intensity (PO coverage tiers), and duration (consecutive days with PO), respectively. This study covered all of the pregnant women living in the following eight Sandy-affected counties during the study period: Bronx, Queens, Kings, Richmond, New York, Nassau, Suffolk, and Westchester (Supplemental Fig. 1). This study was reviewed and approved by the Institutional Review Board at the State University of New York at Albany.
2.2. Data sources
PO data were obtained from the Electric Outage Reporting System (EORS) of the NYS Department of Public Service (DPS). The EORS collects information related to major PO events at the power operating division level, which is defined by the DPS. The system recorded a large-scale and long-lasting PO event in the eight previously identified NYS counties following Hurricane Sandy (2012). Information on the PO event was recorded every half hour from October 29 through November 27 (30 days), 2012. Records for ED visits due to pregnancy complications in the eight counties during 2005–2014 were obtained from the New York Statewide Planning and Research Cooperative System (SPARCS). SPARCS collects information on over 95% of ED visits in NYS, including the principal and up to 24 other diagnoses, date of birth, gender, race, ethnicity, street address, and admission date. Synchronous data on daily temperature and fine particulate matter (PM2.5) were obtained from the U.S. Environmental Protection Agency (EPA).
2.3. Exposure assessment
In this study, we defined three PO indicators including occurrence, intensity, and duration (Fig. 1) for the overall study area, based on the coverage of the PO. PO coverage was calculated as the ratio of daily maximum number of customers affected divided by the total customers. Based on the distribution of daily PO coverage from October 29–November 27, 2012 (Supplemental Fig. 2), we defined days with a PO coverage above the 50th percentile (2.2%) as PO days, and those below the 50th percentile as non-PO days. As a result, each day between October 29 (31.4% of PO coverage) and November 12 (3.4% of PO coverage) was defined as a PO day. Furthermore, we grouped the PO days into four intensity levels to investigate the potential dose-response relationship: Level 1 as 2.2% ≤ PO coverage < 6.1%, level 2 as 6.1% ≤ PO coverage < 9.8%, level 3 as 9.8% ≤ PO coverage < 31.4%, level 4 as PO coverage ≥31.4%. PO duration was calculated as the number of consecutive days with PO prior to a certain day.
Fig. 1.
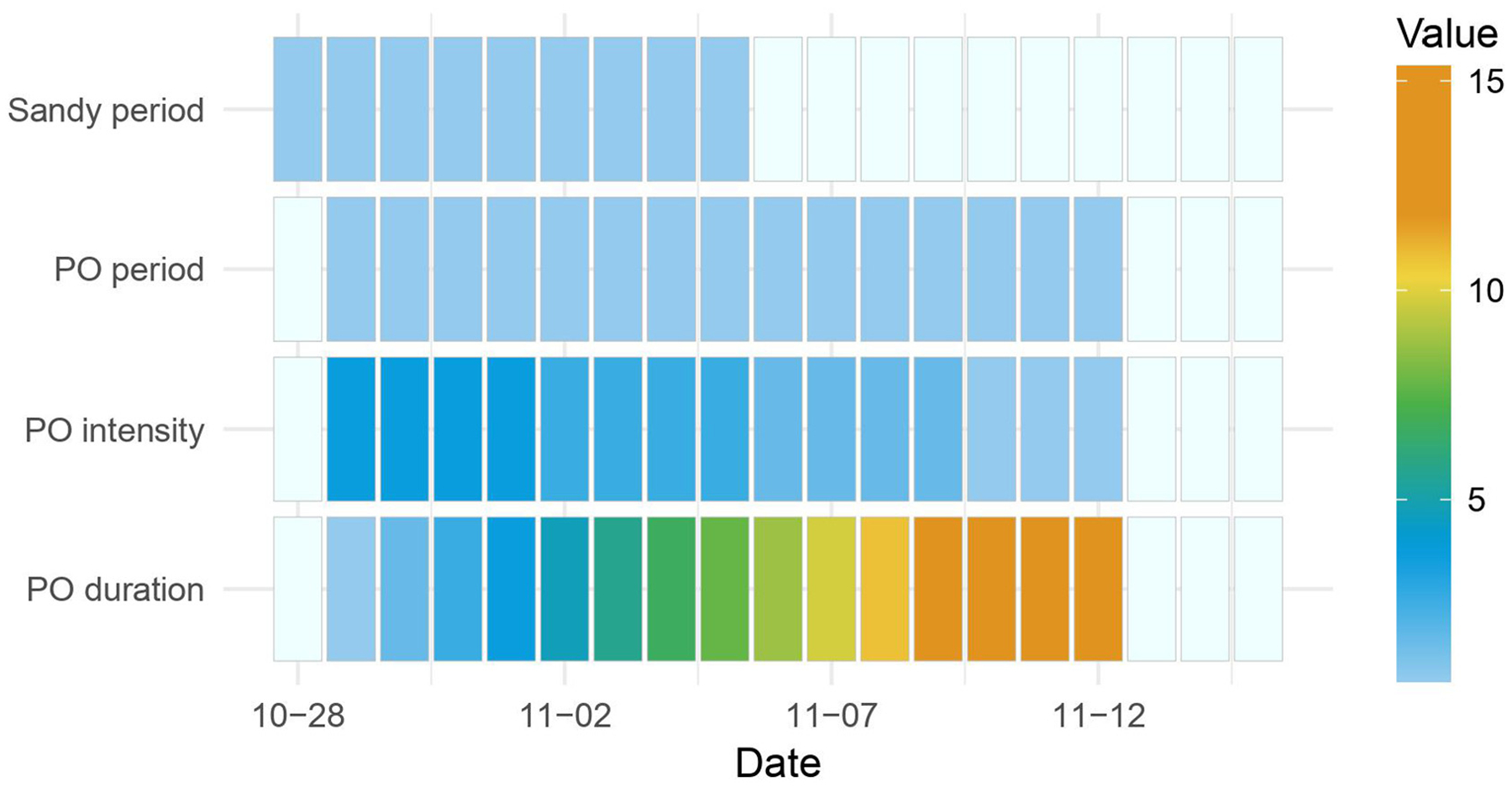
The timelines of Sandy period, PO period, PO intensity, PO duration defined in this study.
2.4. Disease classification
We retained ED visits with a primary diagnosis of pregnancy complications (the International Classification of Diseases, Ninth Revision, ICD-9: 630–649), and focused on both the overall and eight major subtypes (ICD 9 codes described in Supplemental Table 1): threatened or spontaneous abortion, threatened or early labor, hypertension complications, infections of genitourinary tract, renal diseases, gestational diabetes mellitus, mental illnesses, and cardiovascular diseases during pregnancy.
2.5. Statistical analyses
Based on the daily data for the eight counties during the study period, we investigated the association between the daily number of ED visits due to a certain condition and each of the three PO indicators, after controlling for confounders using a Poisson distribution with over-dispersion (Anderson and Bell, 2011; Anderson and Bell, 2012).
First, we used the Generalized Additive Model (GAM) to explore the relationships between PO and the total ED visits for pregnancy complications in the eight affected counties. Since the impact of PO on pregnancy complications may continue over a certain period following the PO, we developed a Distributed Lag Model (DLM) to examine the cumulative impact of the PO period (Gasparrini, 2011). In addition, we also investigated the impact of PO intensity and PO duration on the risk of ED vistis due to pregnancy complications. The potential confounders controlled in the model included Hurricane Sandy, air temperature, PM2.5, and time varying variables (day of week, holidays, seasonality, and long-term trend). We selected these covariates based on related literature identified in our extensive literature review and data used in this study. Specifically, prior studies on this topic observed that hurricane, temperature variation, high concentration of PM2.5, and some time varying variables, such as Monday and holidays were associated with elevated risks of pregnancy complications (Guo et al., 2018; Liang et al., 2018; Liu et al., 2019). Additionally, several studies suggested these factors are confounding factors in PO-health research (Anderson and Bell, 2012; Lin et al., 2011). Furthermore, our preliminary data and published studies using this data observed that Hurricane Sandy, temperature, and time varying variables are associated with pregnancy complications in New York State (Xiao et al., 2019). In time-series analysis, we also adjusted for multiple temporal variables in order to remove the potential time pattern and trend (Bhaskaran et al., 2013; Gronlund et al., 2014).
The cumulative effects were examined up to a lag of 7 days based on the initial analysis, as the short-term effect of POs may last for approximately 7 days (Supplemental Fig. 3). The model used was:
where μ = expected daily ED visits for pregnancy complications in the eight counties; α = model intercept; and β = regression coefficients for PO impact. We incorporated a “cross-basis” function with linear estimation for PO metrics, including occurrence (an indicator with 1 for PO period and 0 for the rest), intensity (an ordinary variable with 1–4 levels of PO coverages during the PO period and 0 for the rest), or duration (PO duration = 0 if non-PO happened that day, otherwise, PO = I to represent the Ith consecutive day with PO); γ = Vector of coefficient for Hurricane Sandy’s impact (Sandy = 1 for Sandy period, Sandy = 0 for non-Sandy period) to control for the confounding effect of the hurricane; f(TM): Natural cubic spline of daily mean temperature with 3 degrees of freedom (df) to control for the confounding effect of cold exposure as previous studies suggested that cold exposure might be significantly associated with elevated risk of pregnancy complications (Ha et al., 2017); f(PM): Natural cubic spline for daily average concentration of PM2.5, the most important air pollutant, with 3 df; f(Time): Natural cubic spline of time, used to model long-term trends, with 1–2 df/year; f(Month): Natural cubic spline of months, used to model monthly trends, with 3 df; δ=Vector of coefficients for day of week and & = Vector of coefficients for holiday, adjusted for the potential temporal patterns in the reporting; offset(POP): with an offset of female population by year. As the female population at reproductive age was not available, we used the total female population as a surrogate. Since the percentage of reproductive females is largely constant and would not change significantly within a few years, using the total female population instead of the reproductive female population would only affect the intercept of the model rather than the regression coefficients (i.e. the RR estimate of POs).
Based on these models, we estimated the percent increase of ED visits for pregnancy complications related to the PO period (versus non-PO period), or to each level increase in PO intensity or each day increase in PO duration on lag 0–7 days. The percentage increase in ED visits was estimated by (exp (β) – 1) * 100%. In the stratified analyses, estimates were stratified by pregnancy complication subtypes and the sociodemographic characteristics of the cases to identify the most vulnerable groups.
Sensitivity analysis was performed to investigate the robustness of our estimates. Specifically, we excluded 2011 data from our study when a large-scale PO was reported following a rare snowstorm in the northeastern U.S. of that year. We also changed the study period from October–December to October–November in the sensitivity analysis to examine if removing a winter month could affect our findings.
All statistical tests were two-sided and we defined statistical significance as P value <0.05 for risk estimation. All analyses were performed using R software (version 3.3.1) (Team, 2014) with the GAM fitted using the “mgcv” package and DLM using the “dlnm” package.
3. Results
3.1. Base information for pregnancy complications
From October to December throughout 2005–2014, there were 307,739 total ED visits for pregnancy complications in the eight counties, with a daily average of 334. Supplemental Table 1 describes the number of visits for each major pregnancy complication subtype. We observed that ED visits for multiple pregnancy complications, such as threatened delivery, renal disease, and gestational diabetes mellitus, increased after PO (i. e. the red curve was higher following PO, Fig. 2) and was higher than the average number of visits reported during 2005–2014 (i. e. the red curve tended to be higher than the blue curve, Fig. 2).
Fig. 2.

The trend of emergency departments (ED) visits for multiple pregnancy complications in eight affected counties from October 1 to December 31 in 2012, compared to the same period in 2005–2014 except 2012. (Black line: October 29, the day power outage begins after Hurricane Sandy made landfall; Blue shadow: the standard deviation of daily ED visits for pregnancy complications during 2005–2014 except 2012).
3.2. ED visits during PO period versus non-PO period
Table 1 shows the percentage increase in ED visits for overall pregnancy complications during different lag periods, during the Hurricane Sandy period, and during PO periods. We found that ED visits for pregnancy complications during the Sandy period significantly increased, with a cumulative increase of 4.1% (95%CI: 0.4%, 8.0%). The ED visits during the PO period were associated with an increase from lag 2 to lag 5 days, with a peak increase on lag 3 days, and a 7-day cumulative increase of 6.0% (95%CI: 2.5%, 9.7%). While adjusting for the Hurricane Sandy period, the cumulative increase in ED visits for total pregnancy complications during PO was 16.6% (95%CI: 10.3%, 23.2%).
Table 1.
Percentage increases (95% CIs) in ED visits for total pregnancy complications during power outage (PO) period and Hurricane Sandy (Sandy) period.
| Lag days | PO period vs. non-PO period | Sandy period vs. non-Sandy period | PO period vs. non-PO period (adjusting Sandy period) |
|---|---|---|---|
| Lag 0 | −0.8 (−5.5, 4.1) | −5.7 (−10.4, −0.7) | −4.1 (−14.2, 7.2) |
| Lag 1 | 3.6 (−1.2, 8.7) | −3.6 (−8.4, 1.5) | 7.4 (2.6, 12.5) |
| Lag 2 | 5.7 (0.8, 10.9) | 2.9 (−2.3, 8.2) | 10.5 (4.2, 17.1) |
| Lag 3 | 5.9 (1.0, 11.1) | 6.9 (1.6, 12.4) | 7.4 (2.9, 12.1) |
| Lag 4 | 5.6 (o.7, 10.8) | 5.8 (0.6, 11.3) | 1.9 (−2.5, 6.4) |
| Lag 5 | 5.3 (0.4, 10.5) | 5.5 (0.3, 11.0) | −3.0 (−8.6, 3.0) |
| Lag 6 | 4.4 (−0.6, 9.5) | 5.4 (0.2, 10.9) | −4.3 (−8.2, −0.2) |
| Lag 7 | 4.7 (−0.1, 9.9) | 4.9 (−0.3, 10.3) | 0.8 (−8.0, 10.4) |
| Lag 0–7 | 6.0 (2.5, 9.7) | 4.1 (0.4, 8.0) | 16.6 (10.3, 23.2) |
Estimates indicating significantly increased health risk were bolded.
3.3. Health impact of PO intensity and PO duration
We observed a nonlinear dose-response relationship between the PO intensity and ED visits for pregnancy complications, with ED visits increasing by 11.3%, 26.3%, 35.9%, and 33.7% for PO intensity level 1 to 4 in comparison with PO intensity level 0, respectively (Fig. 3). ED visits increased by an estimated 8.8% (95%CI: 5.8%, 11.8%) for each level increase in PO intensity. There was an increasing trend of ED visits for pregnancy complications as PO duration increased, especially in the first week of PO. The highest health risk was observed in the first 7 days following PO. Overall, ED visits increased by an estimated 1.4% (95%CI: 0.8%, 2.1%) for each day increase during the 15-day PO duration.
Fig. 3.

The dose-response curve for PO intensity, PO duration and ED visits for total pregnancy complications. Four levels of PO intensity were classified based on the IQR of PO coverage distribution in the 15-day PO period. PO duration was identified was measured as the power outage’s length in the day for PO period, from October 29 to November 12 in 2012.
3.4. Impact of PO by disease
Table 2 shows the cumulative increase in ED visits for multiple pregnancy complications under different PO characteristics. During the PO period, ED visits significantly increased for threatened labor or early delivery (26.7%, 95% CI: 8.2%, 48.4%), especially for threatened labor (23.8%, 95% CI: 5.5%, 45.3%). Gestational diabetes mellitus was estimated to increase by 111.8% (95% CI: 16.7%, 284.4%). No significant increases were observed for other pregnancy complications including threatened or spontaneous abortion, hypertension, infections of genitourinary, renal diseases, mental illnesses, and cardiovascular disease. For PO intensity, we found that the rate of threatened labor or early delivery was significantly associated with PO coverage, with an increase of 13.5% (95% CI: 4.2%, 23.7%) for each level increase in PO intensity. In addition, we found that each day increase in PO duration was associated with a 1.9% (95% CI: 0.7%, 3.2%) and 8.1% (95% CI: 2.4%, 14.0%) increase in threatened labor or early delivery and gestational diabetes mellitus, respectively.
Table 2.
Percentage increase (95% CIs) of ED visits for multiple pregnancy complications under different power outage characteristic.
| Variables | ED visits during the study period | PO period vs. non-PO period | One level increase in PO coverage | One day increase in PO duration |
|---|---|---|---|---|
| 1. Threatened or spontaneous abortion | 70,917 | 8.4 (−5.0, 23.8) | 2.1 (−4.7, 9.3) | 0.9 (−0.1, 2.0) |
| Threatened abortion | 12,513 | 12.4 (−15.7, 49.8) | 3.3 (−11.4, 20.5) | 1.1 (−1.2, 3.4) |
| Spontaneous abortion | 58,404 | 7.7 (−6.6, 24.2) | 1.8 (−5.4, 9.6) | 0.9 (−0.2, 2.0) |
| 2. Hypertension complications | 4124 | −36.8 (−68.4, 26.4) | −11.7 (−34.7, 19.5) | −2.9 (−7.3, 1.7) |
| 3. Threatened labor or early delivery | 44,202 | 26.7 (8.2, 48.4) | 13.5 (4.2, 23.7) | 1.9 (0.7, 3.2) |
| Threatened labor | 44,011 | 23.8 (5.5, 45.3) | 13.0 (3.6, 23.2) | 1.7 (0.5, 3.0) |
| Early onset of delivery | 191 | 112.5 (−16.6, 441.0) | 16.8 (−29.8, 4.3) | 7.9 (−0.7, 17.2) |
| 4. Infections of genitourinary | 18,280 | 14.7 (−11.9, 49.2) | 3.1 (−9.6, 17.6) | 1.3 (−0.8, 3.4) |
| 5. Renal diseases | 269 | −73.6 (−96.5, 97.3) | −66.9 (−83.8, −32.4) | −3.0 (−18.2, 15.1) |
| 6. Diabetes mellitus | 2255 | 111.8 (16.7, 284.4) | 38.6 (−3.2, 98.5) | 8.1 (2.4, 14.0) |
| 7. Mental illness | 948 | 22.3 (−49.7, 197.1) | −7.4 (−44.0, 53.3) | 1.0 (−5.9, 8.6) |
| 8. Cardiovascular diseases | 252 | 78.1 (−81.1, 1581.5) | 118.7 (−68.5, 1419.0) | −33.7 (−59.9, 9.9) |
3.5. Impact of PO by sociodemographic features
Table 3 shows the percentage increase in ED visits for overall pregnancy complications by sociodemographic characteristics. We observed that pregnant women <20 years of age were at the highest risk of complications associated with PO, with an ED visit increase of 27.5% (95% CI: 6.5%, 52.7%) during the PO period. Black and Hispanic individuals had the highest risks, with an ED visit increase of 20.9% and 25.4% respectively. The uninsured group had a higher risk of complications compared to those who are insured (19.1% vs. 15.1%).
Table 3.
Percentage increase (95% CIs) of ED visits for overall pregnancy complications by socio-demographic features under different PO characteristics.
| Variables | ED visits during the study period | PO period vs. non-PO period | One level increase in PO coverage | One day increase in PO duration |
|---|---|---|---|---|
| Age (years) | ||||
| <20 | 33,215 | 27.5 (6.5, 52.7) | 7.4 (−3.2, 19.3) | 2.3 (0.8, 3.9) |
| 20–35 | 229,021 | 16.6 (9.4, 24.2) | 5.2 (0.2, 10.4) | 1.5 (0.8, 2.2) |
| >35 | 45,503 | 10.8 (−3.7, 27.6) | 8.0 (−0.5, 17.1) | 0.4 (−0.8, 1.6) |
| Race | ||||
| White | 77,142 | 5.6 (−5.7, 18.2) | 1.5 (−5.3, 8.9) | 0.1 (−1.0, 1.2) |
| Black | 107,129 | 20.9 (9.9, 33.0) | 6.5 (−0.4, 13.8) | 2.1 (1.1, 3.1) |
| Other | 123,468 | 20.0 (10.3, 30.5) | 7.7 (1.5, 14.2) | 1.6 (0.7, 2.5) |
| Ethnic | ||||
| Hispanic | 117,546 | 25.4 (14.7, 37.2) | 8.0 (1.1, 15.5) | 1.9 (0.9, 2.9) |
| Non-Hispanic | 190,193 | 11.8 (4.3, 19.9) | 4.6 (−0.5, 9.9) | 1.1 (0.4, 1.9) |
| Health insurance | ||||
| Uninsured | 43,430 | 19.1 (2.4, 38.6) | 3.2 (−5.7, 13) | 1.7 (0.4, 3.1) |
| With insurance | 264,309 | 15.1 (8.3, 22.2) | 5.8 (0.6, 11.1) | 1.3 (0.5, 2.0) |
In the sensitivity analysis, we observed that the cumulative increase in ED visits for total pregnancy complications during a PO was 16.0% (95%CI: 9.3%, 23.5%) and 14.6% (95%CI: 8.3%, 25.2%) when excluding 2011 data or shortening the study period separately. These results were similar with previous estimation of 16.6% (95%CI: 10.3%, 23.2%), suggesting results were robust.
4. Discussion
4.1. Association between PO and pregnancy complications
In the present study, we observed that large-scale POs in eight affected counties following Sandy were associated with increased rates of ED visits for pregnancy complications. During the Sandy-related PO period, ED visits for overall pregnancy complications were estimated to increase by 16.6%. Although the association between PO and pregnancy complications remains unclear, some studies focusing on the health impact of weather disasters suggest that psychological stress associated with the consequences of disasters may play an important role in the elevated risk of pregnancy complications (Antipova and Curtis, 2015), (Currie and Rossin-Slater, 2013). Similar mechanisms may be used to interpret the impact of POs. Pregnancy complications may be associated with stress resulting from limited access to safe food or fresh water, and reduction in social interaction (Lin et al., 2016; Zohuri, 2016). Additionally, some power-dependent home medical equipment (e.g. inhalation therapy nebulizer or oxygen conservers) and heating equipment cannot be used during POs. This may exacerbate conditions for pregnant women with certain chronic disease. For instance, people may have limited access to glucose monitoring devices, refrigerated medicine, and food during the PO period, which is important among pregnant women with diabetes mellitus or other diseases. Therefore, during large-scale POs, elevated risk of pregnancy complications could be associated with numerous environmental changes.
In our study, the estimated health impact of PO after controlling for hurricane could accumulate for seven days. The risk of total pregnancy complications elevated from one day following PO, and was highest at the lag 2 day. These lag patterns were consistent with those identified for heatwaves reported in prior studies (Anderson and Bell, 2011; Gasparrini and Armstrong, 2011). This study suggested that PO may have immediate effects on pregnancy complications following the event, and the effect can last for a week. It must be noted that a study by Oni et al. observed that pregnant women exposed to hurricane were more likely to have hypertensive disorders and diabetes mellitus in the following 24 months (Oni et al., 2015). As a result of secondary damage from the hurricane, PO may have a lasting impact on health. Future studies based on longer-term surveillance data would be helpful to clarify this important issue.
A dose-response association was observed between PO coverage and ED visits for pregnancy complications, with a higher risk from higher PO intensity. We found that approximately 39.2% of customers lost power in the eight affected counties on October 30, 2012. It is likely that more people would be affected or seek ED care following more intense POs as compared with the less severe PO events. In this study, there was also evidence supporting the duration effect of PO. The results of the duration effect due to sustained PO were consistent with the findings of the additional effect of heatwave duration (Anderson and Bell, 2011; Gasparrini and Armstrong, 2011). These results suggest that both the coverage and duration of PO events play important roles in PO-related health impacts.
4.2. Impact of PO by disease subtypes
Compared with the non-PO period, the visits for diabetes mellitus during pregnancy increased by 111.8% during the PO period. The association between diabetes and environmental stress, although not specifically POs, has been previously reported (Fonseca et al., 2009; Heptulla et al., 2016; Hopkins, 2017). For example, a study in New Jersey observed that the total ED visits for diabetes increased by 84% following Hurricane Sandy and associated POs the following week (Velez-Valle and Derek Shendell, 2016). A potential interpretation was that pregnant women with diabetes or abnormal glucose tolerance may have limited access to glucose monitoring devices and medicine that needs to be refrigerated (Lee et al., 2016; Velez-Valle and Derek Shendell, 2016). Additionally, they may not have been able to adhere to a normal diet, which is important among pregnant women with diabetes mellitus (Hopkins, 2017).
We found that ED visits significantly increased by 26.7% during the PO period for threatened labor or early delivery. The large-scale PO following Sandy greatly disrupted routine life and health care, which may be associated with an increase in stress and other mental health disorders (Caramanica et al., 2015; Lin et al., 2016; Neria and Shultz, 2012). Therefore, pregnant women in affected areas were potentially more vulnerable to the stress associated with PO and suffered from higher risks of threatened delivery (King and Laplante, 2015; Oni et al., 2015). In addition, heating equipment cannot be used, increased accidental injuries associated with PO (Anderson and Bell, 2012; Casey-Lockyer et al., 2013) may also be a possible interpretation for the elevated risk of threatened labor (Griebel et al., 2005) or early delivery (Goldenberg et al., 2008). Our findings provide evidence that large-scale POs may be associated with elevated risk of severely threaten labor or early delivery.
In this study, we observed slight increases in ED visits for gestational hypertension, renal, mental illness, and cardiovascular disease during a PO, although the increase was not statistically significant. One reason was that ED visit rates for these diseases were relatively low, resulting in decreased statistical power. Another explanation is that the health impacts associated with POs may be delayed. Further studies among a larger population would be needed to confirm our findings regarding the relationship between PO and these subtypes.
4.3. Impact of PO in different population
We observed that the health risk of PO was highest among pregnant women <20 years of age. This finding was consistent with previous reports that pregnant women less than 20 years of age are more likely to have preterm delievery or other pregnacy complications (Jolly et al., 2000). In addition, we observed that Black and Hispanic individuals were at higher risk of health impacts from POs compared with other demographic groups. These findings are consistent with previous studies which suggest that African-Americans and Hispanic individuals in the U.S. are more vulnerable to natural disasters due to English proficiency, housing patterns, community isolation, and experiencing cultural insensitivity including discrimination. (Bolin and Kurtz, 2018; Perilla et al., 2002). When stratified by health insurance, we observed that uninsured women were at higher risk during POs than those who are insured. Low socioeconomic status may be an important reason why health insurance is important (Foundation, 2016).
4.4. Strengths and limitations
To the best of our knowledge, this is the first study to investigate the relationship between POs and pregnancy complications. We estimated the health impacts associated with Sandy-related PO as well as the intensity and duration of PO events. We found that multiple pregnancy complications were associated with the hurricane related PO. During such disasters, health services for pregnant women may need to be prioritized, especially for those of low socioeconomic status (SES).
The present study has several limitations. First, our results may reflect changes in pattern of health service utilization such as a shift from small clinics to emergency departments during POs. Unfortunately, this information is not available to determine whether a patient went to the emergency department due to needing urgent medical care or lack of access to their medical office where they would normally seek care. Nonetheless, this is not likely to be a major issue in the present study as we focused on urgent pregnancy complications, such as threaten labor, which requires immediate emergency medical attention regardless of whether there is a PO. Second, synergistic impacts of multiple events during Sandy, including floods, high winds, and additional storms, may jointly affect the observed impact on prenatal health. Although we have minimized this potential by adjusting for the Sandy period in our model, we may not be able to completely rule out the potentially combined impacts of PO and Sandy, as well as other relevant environmental factors for the results. Third, sample size by disease subtypes and sociodemographic characteristics may be limited, resulting in reduced statistical power. Although we still detected significant signals regarding the impact of PO on overall and certain subtypes of pregnancy complications, more significant findings would be expected when larger sample size is achieved in future studies. Finally, PO may not be county-wide, and only a proportion of women were actually impacted by PO, though all residents in that county have been classified as PO exposed in this study. Therefore, the potential exposure misclassification should be acknowledged. To address this concern, we assessed the coverage and duration of PO in relation to pregnancy complications respectively in addition to the dichotomized indicator of PO exposure (Yes or No). The significant dose-response relationships we observed further validated the positive findings regarding the impact of PO on pregnancy complications.
5. Conclusion
Our results indicate that large-scale POs following a disaster may adversely affect prenatal health, including threatened labor and abnormal glucose with an evident dose-response association. Pregnant women of low SES are more vulnerable to PO. Future public health preparedness and response should consider the healthcare needs of pregnant women based on the predicted possibility of a large-scale weather-related PO. Moreover, pregnant women would benefit from taking additional precautions, given the increasing frequency of weather extremes and associated POs over time due to climate change.
Supplementary Material
HIGHLIGHTS.
Power outage was associated with increased risk of pregnancy complications.
The intensity and duration of power outage play important roles in the health impact.
Young adults, Blacks, Hispanics, and uninsured individuals were the most vulnerable.
Acknowledgement
This work was supported by National Institute of Environmental Health Sciences (NIEHS) [grant R15ES028000]; the United States Centers for Disease Control and Prevention (CDC) [grant TP000566]; the New York State Energy Research and Development Authority (NYSERDA) [grant 28262].
Footnotes
CRediT authorship contribution statement
Dr. Shao Lin has full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Concept and design: Lin, Ma, Meng.
Acquisition, analysis, or interpretation of data: Xiao, Zhang, Huang, Lu.
Drafting of the manuscript: Xiao, Zhang, Huang.
Critical revision of the manuscript for important intellectual content: Huang, Lawrence, Lin, Primeau, Dong, Liu, Tan.
Statistical analysis: Xiao, Zhang.
Supervision: Lin, Ma, Meng.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.scitotenv.2021.145359.
References
- Anderson GB, Bell ML, 2011. Heat waves in the United States: mortality risk during heat waves and effect modification by heat wave characteristics in 43 US communities. Environ. Health Perspect 119, 210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson GB, Bell ML. Lights out: impact of the August 2003 power outage on mortality in New York, NY. Epidemiology (Cambridge, Mass.) 2012; 23: 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antipova A, Curtis A, 2015. The post-disaster negative health legacy: pregnancy outcomes in Louisiana after Hurricane Andrew. Disasters 39, 665–686. [DOI] [PubMed] [Google Scholar]
- Bhaskaran K, Gasparrini A, Hajat S, Smeeth L, Armstrong B, 2013. Time series regression studies in environmental epidemiology. Int. J. Epidemiol 42, 1187–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolin B, Kurtz LC. Race, class, ethnicity, and disaster vulnerability. Handbook of Disaster Research. Springer, 2018, pp. 181–203. [Google Scholar]
- Campbell RJ, 2012. Weather-related Power Outages and Electric System Resiliency. Congressional Research Service, Library of Congress; Washington, DC. [Google Scholar]
- Caramanica K, Brackbill RM, Stellman SD, Farfel MR, 2015. Posttraumatic stress disorder after Hurricane Sandy among persons exposed to the 9/11 disaster. International Journal of Emergency Mental Health 17, 356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Casey-Lockyer M, Heick Rebecca J., Mertzlufft Caitlin E., Yard Ellen E., Wolkin Amy F., Noe Rebecca S., and Murti Michelle. Deaths associated with Hurricane Sandy-October-November 2012. MMWR. Morb. Mortal. Wkly Rep 2013; 62: 393. [PMC free article] [PubMed] [Google Scholar]
- Currie J, Rossin-Slater M, 2013. Weathering the storm: hurricanes and birth outcomes. J. Health Econ 32, 487–503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dominianni C, Lane K, Johnson S, Ito K, Matte T, 2018. Health impacts of citywide and localized power outages in New York City. Environ. Health Perspect 126 (6), 067003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- FEMA. Progress Report: Hurricane Sandy Recovery–One Year Later, 2013.
- Fonseca VA, Smith H, Kuhadiya N, Leger SM, Yau CL, Reynolds K, et al. , 2009. Impact of a natural disaster on diabetes. Diabetes Care 32, 1632–1638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foundation KF, 2016. Key Facts About the Uninsured Population. Kaiser Family Foundation; Washington, DC. [Google Scholar]
- Gasparrini A, 2011. Distributed lag linear and non-linear models in R: the package dlnm. J. Stat. Softw 43, 1. [PMC free article] [PubMed] [Google Scholar]
- Gasparrini A, Armstrong B. The impact of heat waves on mortality. Epidemiology (Cambridge, Mass.) 2011; 22: 68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldenberg RL, Culhane JF, Iams JD, Romero R, 2008. Epidemiology and causes of preterm birth. Lancet 371, 75–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griebel CP, Halvorsen J, Golemon TB, Day AA, 2005. Management of spontaneous abortion. Am. Fam. Physician 72, 1243–1250. [PubMed] [Google Scholar]
- Gronlund CJ, Zanobetti A, Schwartz JD, Wellenius GA, O’Neill MS, 2014. Heat, heat waves, and hospital admissions among the elderly in the United States, 1992–2006. Environ. Health Perspect 122, 1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo T, Wang Y, Zhang H, Zhang Y, Zhao J, Wang Q, et al. , 2018. The association between ambient PM2. 5 exposure and the risk of preterm birth in China: a retrospective cohort study. Sci. Total Environ 633, 1453–1459. [DOI] [PubMed] [Google Scholar]
- Ha S, Liu D, Zhu Y, Kim SS, Sherman S, Mendola P, 2017. Ambient temperature and early delivery of singleton pregnancies. Environ. Health Perspect 125, 453–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He J-R, Liu Y, Xia X-Y, Ma W-J, Lin H-L, Kan H-D, et al. , 2016. Ambient temperature and the risk of preterm birth in Guangzhou, China (2001–2011). Environ. Health Perspect 124, 1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heptulla R, Hashim R, Johnson DN, Ilkowitz JT, DiNapoli G, Renukuntla V, et al. , 2016. Evaluating emergency preparedness and impact of a hurricane sandy in pediatric patients with diabetes. Disaster and Military Medicine 2, 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins POCIT, 2017. South Asian floods and Hurricane Harvey: diabetes in crisis. The Lancet. Diabetes & endocrinology 5, 757. [DOI] [PubMed] [Google Scholar]
- House W, 2013. Economic Benefits of Increasing Electric Grid Resilience to Weather Outages. Executive Office of the President, Washington, DC. [Google Scholar]
- Houser T, Marsters P. The world’s second largest blackout. https://rhg.com/research/puerto-rico-hurricane-maria-worlds-second-largest-blackout/ 2018; April 12.
- Jolly MC, Sebire N, Harris J, Robinson S, Regan L, 2000. Obstetric risks of pregnancy in women less than 18 years old. Obstet. Gynecol 96, 962–966. [DOI] [PubMed] [Google Scholar]
- Kenward A, Raja U, 2014. Blackout: extreme weather, climate change and power outages. Climate Central 1–23. [Google Scholar]
- King S, Laplante DP. Using natural disasters to study prenatal maternal stress in humans. Perinatal Programming of Neurodevelopment. Springer, 2015, pp. 285–313. [DOI] [PubMed] [Google Scholar]
- Klinger C, Owen Landeg VM, 2014. Power outages, extreme events and health: a systematic review of the literature from 2011–2012. PLoS Currents 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee DC, Gupta VK, Carr BG, Malik S, Ferguson B, Wall SP, et al. , 2016. Acute post-disaster medical needs of patients with diabetes: emergency department use in New York City by diabetic adults after Hurricane Sandy. BMJ Open Diabetes Research and Care 4, e000248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang Z, Wang P, Zhao Q, Wang B-Q, Ma Y, Lin H, et al. , 2018. Effect of the 2008 cold spell on preterm births in two subtropical cities of Guangdong Province, Southern China. Sci. Total Environ 642, 307–313. [DOI] [PubMed] [Google Scholar]
- Lin S, Fletcher BA, Luo M, Chinery R, Hwang S-A, 2011. Health impact in New York City during the Northeastern blackout of 2003. Public Health Rep. 126, 384–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin S, Lu Y, Justino J, Dong G, Lauper U, 2016. What happened to our environment and mental health as a result of Hurricane Sandy? Disaster Medicine and Public Health Preparedness 10, 314–319. [DOI] [PubMed] [Google Scholar]
- Liu X, Ye Y, Chen Y, Li X, Feng B, Cao G, et al. , 2019. Effects of prenatal exposure to air particulate matter on the risk of preterm birth and roles of maternal and cord blood LINE-1 methylation: a birth cohort study in Guangzhou. China. Environment International 133, 105177. [DOI] [PubMed] [Google Scholar]
- Lurie N, Finne K, Worrall C, Jauregui M, Thaweethai T, Margolis G, et al. , 2015. Early dialysis and adverse outcomes after Hurricane Sandy. Am. J. Kidney Dis 66, 507–512. [DOI] [PubMed] [Google Scholar]
- Lutterloh EC, Iqbal S, Clower JH, Spiller HA, Riggs MA, Sugg TJ, et al. , 2011. Carbon monoxide poisoning after an ice storm in Kentucky, 2009. Public Health Rep. 126, 108–115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neria Y, Shultz JM, 2012. Mental health effects of Hurricane Sandy: characteristics, potential aftermath, and response. JAMA 308, 2571–2572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oni O, Harville E, Xiong X, Buekens P, 2015. Relationships among stress coping styles and pregnancy complications among women exposed to Hurricane Katrina. J Obstet Gynecol Neonatal Nurs 44, 256–267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orengo-Aguayo R, Stewart RW, de Arellano MA, Suárez-Kindy JL, Young J, 2019. Disaster exposure and mental health among Puerto Rican youths after Hurricane Maria. JAMA Netw. Open 2 (4), e192619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Panteli M, Mancarella P, 2015. Influence of extreme weather and climate change on the resilience of power systems: impacts and possible mitigation strategies. Electr. Power Syst. Res 127, 259–270. [Google Scholar]
- Perilla JL, Norris FH, Lavizzo EA, 2002. Ethnicity, culture, and disaster response: identifying and explaining ethnic differences in PTSD six months after Hurricane Andrew. J. Soc. Clin. Psychol 21, 20–45. [Google Scholar]
- Rylander C, Øyvind Odland J, Manning Sandanger T., 2013. Climate change and the potential effects on maternal and pregnancy outcomes: an assessment of the most vulnerable–the mother, fetus, and newborn child. Glob. Health Action 6, 19538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shultz JM, Galea S, 2017. Preparing for the next Harvey, Irma, or Maria—addressing research gaps. N. Engl. J. Med 377, 1804–1806. [DOI] [PubMed] [Google Scholar]
- Stocker T, 2014. Climate Change 2013: The Physical Science Basis: Working Group I Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change: Cambridge University Press. [Google Scholar]
- Team RC. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing; 2014, 2014. [Google Scholar]
- Velez-Valle EM, Derek Shendell MPHD, 2016. Type II diabetes emergency room visits associated with Hurricane Sandy in New Jersey: implications for preparedness. J. Environ. Health 79, 30. [PubMed] [Google Scholar]
- Xiao J, Huang M, Zhang W, Rosenblum A, Ma W, Meng X, et al. , 2019. The immediate and lasting impact of Hurricane Sandy on pregnancy complications in eight affected counties of New York State. Sci. Total Environ 678, 755–760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zohuri B. Electricity, an essential necessity in our life. Application of Compact Heat Exchangers for Combined Cycle Driven Efficiency in Next Generation Nuclear Power Plants. Springer, 2016, pp. 17–35. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


