Summary
Background
The COVID-19 pandemic may have been accompanied by an increased exposure to psychosis risk factors. We used a pre-during-post study design to examine variations in the incidence of First-Episode Psychosis (FEP) before, during, and after the COVID-19 pandemic in South London. We hypothesised that FEP rates rose during the pandemic and subsequently returned to pre-pandemic levels.
Methods
Using the Clinical Record Interactive Search (CRIS) system, we screened individuals referred for FEP to Early Intervention Services for Psychosis (EISs) of the South London and Maudsley NHS Foundation Trust (SLaM) from 1 March 2018 to 29 February 2024. Population data for the SLaM catchment area were obtained from the Office for National Statistics (ONS). We calculated crude incidence rates and used Poisson regression models to estimate age-sex-ethnicity-adjusted variation in incidence by year (March-to-February) expressed as Incidence Rate Ratios (IRR).
Findings
A total of 3752 individuals experienced FEP during 5,487,858 person-years at risk, with a mean crude incidence of 68.4 per 100,000 person-years (95% CI: 66.2–70.6). The Poisson model showed a deviation from this mean at the peak of the COVID-19 pandemic in 2020/21, with FEP rates rising to 77.5 per 100,000 person-years (95% CI: 71.8–83.2) and similar rates in 2021/22. FEP incidence gradually returned to the pre-pandemic levels in the following years. During the COVID-19 pandemic, individuals of Black ethnicity experienced the greatest FEP increase, with an IRR of 1.45 (95% CI: 1.29–1.61) in 2020/21 and similar ratios in 2021/22. An increase was also observed in Asian individuals, with an IRR of 1.54 (95% CI: 1.20–1.88) in 2021/22, whereas no significant changes in incidence were observed for other ethnic groups across the pre-, during-, and post-pandemic periods.
Interpretation
FEP incidence in South London increased during the peak of the COVID-19 pandemic, particularly among Black and Asian individuals.
Funding
None.
Keywords: First-Episode Psychosis, COVID-19 pandemic, Psychosis incidence, Early intervention services, Pre-during-post design
Research in context.
Evidence before this study
On 1 July 2024, we searched PubMed for the incidence of First-Episode Psychosis (FEP) during the COVID-19 pandemic, using the keywords (psychos∗[Title/Abstract] OR psychot∗[Title/Abstract] OR schizophr∗[Title/Abstract] OR delusion∗[Title/Abstract] OR hallucinat∗[Title/Abstract]) AND (inciden∗[Title/Abstract] OR rate∗[Title/Abstract]) AND (SARS-CoV-2[Title/Abstract] OR coronavirus [Title/Abstract] OR COVID∗[Title/Abstract] OR lockdown[Title/Abstract] OR pandemic[Title/Abstract]).
We identified six studies that examined FEP incidence or hospitalised FEP incidence before and in the early stages of the COVID-19 pandemic. However, the available evidence was characterised by relatively short observation periods, and no studies examined post-pandemic FEP incidence, not allowing us to draw conclusions about rate variation throughout the pandemic.
Added value of this study
This study provides the first pre-during-post analysis of FEP incidence conducted over a six-year period across the COVID-19 pandemic, within a well-defined catchment area.
We present novel evidence showing that FEP incidence in South London rose during the COVID-19 pandemic and gradually returned to pre-pandemic levels thereafter.
Implications of all the available evidence
Our findings indicate that the COVID-19 pandemic was accompanied by an increased risk of FEP in South London, supporting the notion that the incidence of psychosis may fluctuate over time. Moreover, this study corroborates previous research reporting higher FEP rates among ethnic minorities compared to White British individuals. This incidence disparity widened during the pandemic years, particularly among Black and Asian ethnic groups.
Introduction
Psychotic disorders are characterised by a constellation of positive (e.g., delusions, hallucinations), negative (e.g., diminished emotional expression, avolition/asociality), and disorganisation (e.g., thought/speech disorder, disorganised behaviour) symptoms.1 These presentations may co-occur with affective symptoms such as depression and mania.1 Much epidemiological research focuses on the initial occurrence of this psychopathology, known as the First Episode of Psychosis (FEP). Examining the risk factors associated with FEP is crucial, as these factors likely contribute to incidence variations by location and time. Recent research demonstrates significant geographical discrepancies. For example, the 3-Center AESOP,2 the 16-Center EU-GEI3 and the 3-Center INTREPID-II4 have reported up to a ten-fold variation in FEP incidence rates across different sites. This variability aligns with the different prevalence of, and exposure to, factors influencing psychosis risk.5 As it has been hypothesised, viral outbreaks can increase the risk of developing psychotic disorders, likely through several mechanisms.
Firstly, consistent with the neurodevelopmental theory of schizophrenia, COVID-19 might increase the risk of developing psychosis through direct biological mechanisms via in-utero exposure. However, potential consequences of this pathway may only become evident in the future as those affected mature.6, 7, 8, 9
Additionally, the affective pathway could have been impacted, as exposure to social isolation, deprivation, and unemployment increased during the pandemic, resulting in a marked increase in affective presentations.10 Furthermore, individuals from ethnic minorities experienced greater social deprivation and faced higher risks of contracting COVID-19 with more severe outcomes, including death.11 These overlapping factors highlight the importance of an intersectionality approach,12 as the pandemic may have exacerbated disparities and exposure to risk factors among populations with a pre-existing vulnerability to psychosis.
Finally, evidence remains mixed regarding whether substance use increased during the COVID-19 pandemic, and consequently whether drug-induced psychosis may have temporarily increased.9,13
A few cross-sectional studies have provided FEP incidence rates during the initial stages of the COVID-19 pandemic. Studies from Australia14 and Catalonia15 reported negligible increases and decreases in FEP incidence, respectively. In a preliminary study that we conducted in the South London boroughs of Southwark and Lambeth, we observed a 45% increase in treated FEP incidence during the first year of the pandemic compared to the previous year.16 Similarly, an increased incidence of acute psychosis presentations and FEP admissions was reported also in crisis centres in France, Israel, and the UK.17, 18, 19 Nonetheless, given their short-term focus on periods just before and shortly during the pandemic, the above-mentioned findings should be treated with caution. Robust epidemiological analyses spanning the pre-during-post periods of the pandemic are necessary to confirm trajectories of FEP incidence.
Our current extended study is the first to examine FEP incidence in South London over six years before, during, and after the COVID-19 pandemic and the associated sociodemographic characteristics of individuals presenting FEP. We hypothesised an increase in FEP incidence during the pandemic peak compared to the pre-pandemic rates, with a gradual return to previous rates post-pandemic. Moreover, given that individuals from ethnic minorities in the UK have historically presented higher rates of psychosis2 and faced greater socio-economic challenges during the COVID-19 pandemic,20 we assumed a more pronounced increase in FEP incidence in these demographic groups compared to the White British individuals, consistent with intersectionality perspectives on pre-existing inequalities.
Methods
Study design
We conducted an observational pre-during-post study to estimate the incidence of FEP across four boroughs in South London before, during, and after the COVID-19 pandemic. Using the Clinical Record Interactive Search (CRIS) system we identified all individuals referred to Early Intervention Services for Psychosis (EISs) from 1 March 2018 to 29 February 2024. CRIS is an established, approved healthcare data platform that has produced about 300 peer-reviewed publications.21
Study setting and participants
The EISs under investigation in this study were the STEP team in Southwark, the LEO team in Lambeth, the Lewisham Early Intervention Team, and the COAST team in Croydon, all of which fall under the direction of the South London and Maudsley NHS Foundation Trust (SLaM). These EISs provide care and treatment for adult individuals who first present symptoms of psychosis in their catchment area, covering a population at risk aged 18–64. Using CRIS, we extracted the list of individuals referred to SLaM EISs within the defined time range.
Individual clinical records were reviewed via the front-end CRIS interface.
Consistent with previous incidence studies,2,3 we defined FEP as the first-ever presentation to psychiatric services due to psychotic symptoms, even if longstanding. Specifically, the inclusion criteria were:
-
(a)
experiencing at least one positive psychotic symptom persisting for a minimum of one day or at least two negative psychotic symptoms sustained for six months or more during the study period, as check listed in the Screening Schedule for Psychosis;22
-
(b)
residing in one of the aforementioned London boroughs;
-
(c)
being aged 18–64 (inclusive).
Exclusion criteria were:
-
(a)
experiencing psychotic symptoms secondary to a medical condition (ICD-10 Diagnoses F00-F09);
-
(b)
experiencing transient psychotic symptoms secondary to intoxication;
-
(c)
having previous contact with psychiatric services due to psychotic symptoms before the study period.
Measures
Sociodemographic measures, including age, sex, and ethnicity, were obtained from CRIS. When this information was missing, we reviewed available records from the CRIS front-end interface to derive it.
The main outcome measure was the incidence of FEP by year of presentation (before, during, and after the COVID-19 pandemic). Consistent with previous studies,3,4,22 we used the Screening Schedule for Psychosis to check the list of FEP symptoms. This procedure involves marking Section A (which requires at least one symptom, such as hallucinations, delusions, thought disorders, psychomotor disorders, or bizarre behaviour) and/or Section B (which requires at least two symptoms, including loss of interest, social withdrawal, severe excitement or aggression, overwhelming fear, or self-neglect) for inclusion.
Statistics
We compared the sociodemographic characteristics of individuals excluded from and included in the FEP sample and between those included in the FEP sample and the reference population at risk, using t-tests and chi-square tests where appropriate.
To estimate the incidence rates of FEP, we built the reference population denominators for Southwark, Lambeth, Lewisham, and Croydon using data from the Census 2021 provided by the Office for National Statistics (ONS).23 This process included acquiring stratified population data by sex, age-band, and ethnicity for the population served by the EISs.
We aggregated the population aged between 18 and 64 and residing in the four boroughs to build the SLaM EISs population at risk. This population was further segmented into ten age-bands (ranging from 18 to 64), two sex categories (males and females), and six high-level ethnic groups as defined by the ONS: White British, White Other, Asian, Mixed, Black, and Other ethnic groups (see Supplemental data for detailed classification information).23 Additionally, we built an ethnic minority variable based on the ONS definition, which includes any ethnic group in England different from White British.23
We estimated the overall and standardised incidence rates per 100,000 person-years (PY) with 95% confidence intervals (CI) overall (by summing the annual population at risk into a six-year risk population) and by year of presentation, further stratifying by sex, age-band, and ethnicity. We used multivariate Poisson regression modelling to examine the association with psychosis risk of 1) sex, age-band, and ethnicity, and 2) year of presentation, further adjusting for the population strata as the exposure variable. Incidence Rate Ratio (IRR) were calculated to measure the effect.
To further examine the time-trend hypothesis, a post-hoc analysis of the predicted values and marginal effects assessed whether the incidence in each year differed from the mean incidence of the six years under investigation. We used Sidak's adjustment to account for the multiple comparison.
Finally, to investigate the intersectionality hypothesis that being an individual of other ethnicities was associated with a higher FEP risk during the pandemic than being an individual of White British ethnicity, we introduced an “ethnic group x year” interaction term in the Poisson model. This interaction term examined how the effect of ethnicity on FEP risk changed over different years throughout the pandemic.
Ethics
The CRIS system has received full ethical approval from the Oxfordshire Research Ethics Committee (current reference 23/SC/0257). The CRIS Oversight Committee granted local ethical approval to examine the data used in this study, under reference 20-061: ‘Changes in the Incidence of Psychosis in South London’.
This study used anonymised data extracted from the CRIS database, which does not contain any identifiable personal information. In accordance with ethical guidelines and regulatory requirements, explicit individual consent was not required, as all data were fully de-identified prior to analysis. The procedures followed comply with the Declaration of Helsinki.
Role of funding sources
This study received no specific funding.
Results
Study sample and reference population
We screened 5191 individuals referred to SLaM EISs from 1 March 2018 to 29 February 2024. According to our criteria, 3752 cases were identified as experiencing FEP (Supplementary Figure S1 presents the flow chart of the screening process). Individuals excluded from the FEP sample (M = 33.8, SD = 12.9) were slightly older [t(5187) = 3.4 P < 0.001] and more likely to be White British (χ2(5) = 17.3; P < 0.01) than those included. There were no sex differences between these two groups (χ2(1) = 0.22; P = 0.63).
The FEP cohort comprised 2 176 male patients (58%) and had a mean age of 32.5 years (SD = 12.1), as reported in Table 1. The initial extracted data contained 10% missing ethnicity values, which we completed using the CRIS front-end interface for all except 1.4% of our sample. The majority of the dataset (77.4%) was composed of individuals from ethnic minorities (defined according to the ONS definition as all ethnic groups except White British).23 The ethnic breakdown (Table 1) showed that the sample was composed of individuals identifying themselves as Black (43.2%), followed by White British (21.2%), White Other (12.2%), Asian (9.3%), Other ethnicity (7.1%), and Mixed (5.5%).
Table 1.
Sociodemographic characteristics at FEP.
| FEP (N = 3 752) | |
|---|---|
| Age | |
| Mean (SD) | 32.5 (12.1) |
| Median (IQR) | 29 (22–40) |
| Age band, N (%) | |
| 18–19 | 363 (9.7) |
| 20–24 | 912 (24.3) |
| 25–29 | 631 (16.8) |
| 30–34 | 480 (12.8) |
| 35–39 | 372 (9.9) |
| 40–44 | 261 (7) |
| 45–49 | 250 (6.7) |
| 50–54 | 220 (5.9) |
| 55–59 | 171 (4.6) |
| 60–64 | 92 (2.4) |
| Sex, N (%) | |
| Female | 1 576 (42) |
| Male | 2 176 (58) |
| Ethnicity, N (%) | |
| White British | 795 (21.2) |
| White Other | 459 (12.2) |
| Asian | 350 (9.3) |
| Mixed | 208 (5.5) |
| Black | 1 622 (43.2) |
| Other | 266 (7.1) |
| Not reported | 52 (1.4) |
Note: N, number; SD, Standard Deviation; IQR, Interquartile Range.
The at-risk population, aged 18–64, pooling together individuals living in the four boroughs under consideration, amounted to 914,643, resulting in a summed population at risk of 5,487,858 over six years.
When compared against this population, the incident cases were more likely to be male (58% vs 48%–χ2(1) = 111.3; P < 0.001), younger (χ2(9) = 1068.3; P < 0.001), and from ethnic minorities (77.4% vs 39%, χ2(3) = 11.3; P < 0.001).
Overall incidence rates and changes throughout the COVID-19 pandemic
The overall incidence rate over an at-risk population of 5 487,858 from 1 March 2018 to 29 February 2024 was 68.4 (95% CI 66.2–70.6) per 100,000 person-year (PY).
The incidence rate peaked at 77.51 per 100,000 PY (95% CI 71.81–83.22) in 2020/21, marking a 32% increase (IRR 1.32, 95% CI 1.18–1.48) in FEP presentations compared to the initial year under examination (Table 2). This elevated rate remained stable in the subsequent year. Incidence rates decreased, compared to these peak years, in 2022/23, although the rate remained 14% higher (IRR 1.14, 95% CI 1.02–1.28) than the baseline year. By 2023/24, the IRR further reduced and returned to the baseline (IRR 1.00, 95% CI 0.89–1.12) (Table 2).
Table 2.
FEP Crude Incidence Rates and adjusted Incidence Rate Ratios, overall and stratified by year, sex and ethnicity.
| Reference population (18–64) | Cases | Incidence rates | IR (95% CI) | IRR (95% CI) | |
|---|---|---|---|---|---|
| Year | |||||
| 2018/19 | 914,643 | 537 | 58.71 | 53.75–63.68 | 1.00 |
| 2019/20 | 655 | 71.61 | 66.13–77.10 | 1.22 (1.09–1.37) | |
| 2020/21 | 709 | 77.51 | 71.81–83.22 | 1.32 (1.18–1.48) | |
| 2021/22 | 705 | 77.07 | 71.39–82.77 | 1.31 (1.17–1.47) | |
| 2022/23 | 611 | 66.80 | 61.51–72.10 | 1.14 (1.02–1.28) | |
| 2023/24 | 535 | 58.49 | 53.54–63.44 | 1.00 (0.89–1.12) | |
| 6-year total | 5,487,858 | 3752 | 68.40 | 66.20–70.60 | 1.16 (1.06–1.27) |
| Sex: Females | |||||
| 2018/19 Females | 477,137 | 213 | 44.64 | 38.65–50.64 | 1.00 |
| 2019/20 Females | 290 | 60.78 | 53.78–67.77 | 1.36 (1.20–1.52) | |
| 2020/21 Females | 307 | 64.34 | 57.14–71.54 | 1.44 (1.28–1.60) | |
| 2021/22 Females | 301 | 63.08 | 55.96–70.21 | 1.41 (1.25–1.57) | |
| 2022/23 Females | 250 | 52.40 | 45.9–58.89 | 1.17 (1.03–1.32) | |
| 2023/24 Females | 215 | 45.06 | 39.04–51.08 | 1.01 (0.87–1.14) | |
| 6-year Females | 2,862,822 | 1576 | 55.05 | 52.33–57.77 | 1.23 (1.17–1.29) |
| Sex: Males | |||||
| 2018/19 Males | 437,506 | 324 | 74.06 | 65.99–82.12 | 1.00 |
| 2019/20 Males | 365 | 83.43 | 74.87–91.99 | 1.13 (1.01–1.24) | |
| 2020/21 Males | 402 | 91.88 | 82.9–100.87 | 1.24 (1.12–1.36) | |
| 2021/22 Males | 404 | 92.34 | 83.34–101.35 | 1.25 (1.13–1.37) | |
| 2022/23 Males | 361 | 82.51 | 74–91.03 | 1.11 (1.00–1.23) | |
| 2023/24 Males | 320 | 73.14 | 65.13–81.16 | 0.99 (0.88–1.10) | |
| 6-year Males | 2,625,036 | 2176 | 82.89 | 79.41–86.38 | 1.12 (1.07–1.17) |
| Ethnicity: White British | |||||
| 2018/19 White British | 337,245 | 126 | 37.36 | 30.84–43.89 | 1.00 |
| 2019/20 White British | 145 | 42.99 | 36–49.99 | 1.15 (0.96–1.34) | |
| 2020/21 White British | 157 | 46.55 | 39.27–53.84 | 1.25 (1.05–1.44) | |
| 2021/22 White British | 128 | 37.95 | 31.38–44.53 | 1.02 (0.84–1.19) | |
| 2022/23 White British | 121 | 35.88 | 29.49–42.27 | 0.96 (0.79–1.13) | |
| 2023/24 White British | 118 | 34.99 | 28.68–41.30 | 0.94 (0.77–1.11) | |
| 6-year White British | 2,023,470 | 795 | 39.48 | 36.56–42.02 | 1.06 (0.98–1.12) |
| White Other | |||||
| 2018/19 White Other | 154,070 | 68 | 44.13 | 33.65–54.56 | 1.00 |
| 2019/20 White Other | 74 | 48.03 | 37.09–58.97 | 1.09 (0.84–1.34) | |
| 2020/21 White Other | 90 | 58.42 | 46.35–70.48 | 1.32 (1.05–1.60) | |
| 2021/22 White Other | 89 | 57.77 | 45.76–69.77 | 1.31 (1.04–1.58) | |
| 2022/23 White Other | 68 | 44.14 | 33.65–54.63 | 1.00 (0.76–1.24) | |
| 2023/24 White Other | 70 | 45.43 | 34.79–56.08 | 1.03 (0.79–1.27) | |
| 6-year White Other | 924,420 | 459 | 49.65 | 45.11–54.20 | 1.13 (1.02–1.23) |
| Asian | |||||
| 2018/19 Asian | 106,556 | 52 | 48.80 | 35.54–62.06 | 1.00 |
| 2019/20 Asian | 55 | 51.62 | 37.97–65.26 | 1.06 (0.78–1.34) | |
| 2020/21 Asian | 50 | 46.92 | 33.92–59.93 | 0.96 (0.70–1.23) | |
| 2021/22 Asian | 80 | 75.08 | 58.63–91.53 | 1.54 (1.20–1.88) | |
| 2022/23 Asian | 65 | 61 | 46.17–75.83 | 1.25 (0.95–1.55) | |
| 2023/24 Asian | 48 | 45.05 | 32.30–57.79 | 0.92 (0.66–1.18) | |
| 6-year Asian | 639,336 | 350 | 54.74 | 49.01–60.48 | 1.12 (1.00–1.24) |
| Black | |||||
| 2018/19 Black | 212,075 | 214 | 100.91 | 87.39–114.43 | 1.00 |
| 2019/20 Black | 293 | 138.16 | 122.34–153.98 | 1.37 (1.21–1.53) | |
| 2020/21 Black | 311 | 146.65 | 130.35–162.94 | 1.45 (1.29–1.61) | |
| 2021/22 Black | 309 | 145.70 | 129.46–161.95 | 1.44 (1.28–1.61) | |
| 2022/23 Black | 259 | 122.13 | 107.25–137.00 | 1.21 (1.06–1.36) | |
| 2023/24 Black | 236 | 111.28 | 97.08–125.48 | 1.10 (0.96–1.24) | |
| 6-year Black | 1,272,450 | 1622 | 126.19 | 120.01–132.37 | 1.25 (1.19–1.31) |
| Mixed | |||||
| 2018/19 Mixed | 55,760 | 37 | 66.36 | 44.97–87.74 | 1.00 |
| 2019/20 Mixed | 34 | 60.98 | 40.48–81.47 | 0.92 (0.61–1.23) | |
| 2020/21 Mixed | 37 | 66.36 | 44.97–87.74 | 1.00 (0.68–1.32) | |
| 2021/22 Mixed | 37 | 66.36 | 44.97–87.74 | 1.00 (0.68–1.32) | |
| 2022/23 Mixed | 39 | 69.94 | 47.99–91.89 | 1.05 (0.72–1.38) | |
| 2023/24 Mixed | 24 | 43.04 | 25.82–60.26 | 0.65 (0.39–0.91) | |
| 6-year Mixed | 334,560 | 208 | 62.17 | 53.72–70.62 | 0.94 (0.81–1.06) |
| Other | |||||
| 2018/19 Other | 48,520 | 34 | 70.07 | 46.52–93.63 | 1.00 |
| 2019/20 Other | 50 | 103.05 | 74.49–131.61 | 1.47 (1.06–1.88) | |
| 2020/21 Other | 51 | 105.11 | 76.26–133.96 | 1.50 (1.09–1.91) | |
| 2021/22 Other | 52 | 107.17 | 78.04–136.30 | 1.53 (1.11–1.95) | |
| 2022/23 Other | 48 | 98.93 | 70.94–126.92 | 1.41 (1.01–1.81) | |
| 2023/24 Other | 31 | 63.89 | 41.40–86.38 | 0.91 (0.59–1.23) | |
| 6-year Other | 291,120 | 266 | 91.37 | 80.39–102.35 | 1.30 (1.15–1.46) |
Note: IR, Incidence Rate; IRR, Incidence Rate Ratio; CI, Confidence Interval.
The incidence rates for the years 2020/21 and 2021/22 were higher than the mean incidence rate, as indicated by their confidence intervals not overlapping with the mean (Fig. 1, green line).
Fig. 1.
FEP Crude Incidence Rates by year: Crude (unadjusted) FEP Incidence rates overall (in green) and by sex (in blue and pink) over year with 95% Confidence Intervals.
The independence assumption of the Poisson model was not violated by residual autocorrelation or residual partial autocorrelation.
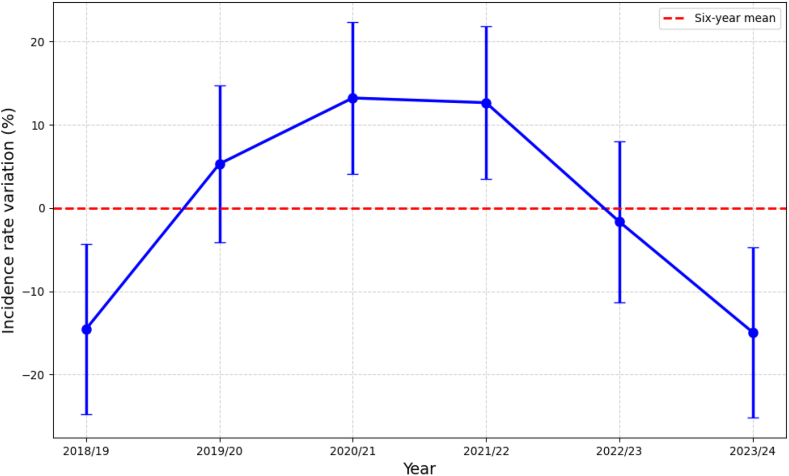
Fig. 2 shows the post-hoc analysis, plotting the Poisson model's mean predicted margins for each year against the average IRR over the entire period, confirming the observed increase in 2020/21 and 2021/22.
Fig. 2.
Contrast from the mean FEP incidence by year: The plot illustrates the contrast of the mean predicted margins (expressed as Incidence Rate Ratio, IRR with 95% CI) for each year from the mean IRR across the years. The Poisson regression model was adjusted for sociodemographic characteristics.
Incidence rates by sex
Throughout the entire period under examination, the crude incidence rate was 55.1 per 100,000 PY in females (95% CI 52.3–57.8) and 82.9 per 100,000 PY in males (95% CI 79.4–86.4) (Table 2). Thus, males had a higher incidence rate than females (IRR 1.56, 95% CI 1.46–1.66) (Table 3). This difference remained consistent throughout the COVID-19 pandemic.
Table 3.
Incidence Rate Ratios of demographic variables for overall FEP risk.
| Variable | IRR (95% CI) | z-value |
|---|---|---|
| Sex | ||
| Females | 1 | |
| Males | 1.56 (1.46–1.66)∗∗∗ | 13.32 |
| Age band | ||
| 18–19 | 1 | |
| 20–24 | 0.82 (0.73–0.93)∗∗ | −3.14 |
| 25–29 | 0.43 (0.37–0.49)∗∗∗ | −12.7 |
| 30–34 | 0.34 (0.29–0.39)∗∗∗ | −15.4 |
| 35–39 | 0.3 (0.26–0.35)∗∗∗ | −16.1 |
| 40–44 | 0.23 (0.2–0.27)∗∗∗ | −17.8 |
| 45–49 | 0.23 (0.2–0.28)∗∗∗ | −17.3 |
| 50–54 | 0.2 (0.17–0.23)∗∗∗ | −18.8 |
| 55–59 | 0.17 (0.14–0.2)∗∗∗ | −19.1 |
| 60–64 | 0.12 (0.09–0.15)∗∗∗ | −17.7 |
| Ethnicity | ||
| White British | 1 | |
| White other | 1.31 (1.17–1.47)∗∗∗ | 4.62 |
| Asian | 1.36 (1.2–1.54)∗∗∗ | 4.8 |
| Black | 3.31 (3.04–3.6) ∗∗∗ | 27.37 |
| Mixed | 1.32 (1.13–1.54)∗∗∗ | 3.56 |
| Other | 2.31 (2.01–2.66)∗∗∗ | 11.8 |
Significance: (P < 0.05), ∗∗ (P < 0.01), and ∗∗∗ (P < 0.001).
Note: IRR, Incidence Rate Ratio; CI, Confidence Interval.
The highest incidence rates for both males and females were observed during the peak pandemic years of 2020/21 and 2021/22 (Table 2), when incidence rates departed from the mean, as indicated by their non-overlapping confidence intervals (Fig. 1, pink and blue lines).
Incidence rates by age
The incidence of FEP was highest in the youngest age band and gradually decreased with increasing age among the FEP group (Table 3, Fig. 3), with a quantified decline in risk starting from an IRR of 0.82 (95% CI 0.73–0.93) in the 20–24 band and reaching the lowest level of 0.12 (95% CI 0.09–0.15) in the 60–64 band (Table 3). These age-related differences remained consistent throughout the COVID-19 pandemic.
Fig. 3.
FEP Incidence Rates by age-band and sex over years: Crude (unadjusted) FEP Incidence Rates with 95% confidence intervals by age-band over years, stratified by sex.
The highest incidence increase, with departure from the mean, was for the age bands 25–29 and 30–34 during the peak pandemic years of 2020/21 and 2021/22 (Supplementary Table S2).
Incidence rates by ethnicity
Across ethnic groups, we observed the highest crude incidence in people of Black ethnicity at 126.1 (120–132.3) per 100,000 PY and the lowest in White British at 39.5 (95% CI 36.6–42) per 100,000 PY (Table 2). The Poisson model showed an IRR of 3.31 (95% CI 3.04–3.6) for Black compared to White British individuals throughout the entire period under examination (Table 3, Fig. 4). Pre-during-post analysis showed the highest incidence rate for Black and White British individuals in 2020/21 at 146.65 (95% CI 130.35–162.94) and 46.55 (39.27–53.84), respectively.
Fig. 4.
FEP Incidence Rates by ethnicity over years: Crude (unadjusted) FEP Incidence Rates with 95% Confidence Intervals by ethnicity over years.
The increase in FEP incidence for Black individuals in the years of the pandemic peak accounted for an IRR of 1.45 (95% CI 1.29–1.61) in 2020/21 and 1.44 (95% CI 1.28–1.61) 2021/22, as evident from the Supplementary Figure S2 illustrating the departure from the mean. Conversely, no such deviation from the mean was observed in White British individuals, with an IRR of 1.25 (95% CI 1.05–1.44) in 2020/21, declining to 1.02 (95% CI 0.84–1.19) in 2021/22.
Thus, the gap in incidence rates between Black and White British individuals widened during the pandemic peak, as evidenced by the difference in the IRR, which was higher in Black individuals by 0.20 in 2020/21 and increased by 0.42 in 2021/22.
The incidence rates for White Other and Other ethnicities slightly increased during the pandemic years, but these increases were not sizeable with precision; the incidence rates for Asian individuals rose more significantly in 2021/22 (IRR 1.54, 95% CI 1.20–1.88) (Table 2, Fig. 4 and Supplementary Figure S2).
Incidence rates by “ethnicity x year”
The model including the “ethnicity x year” interaction term showed an interaction for Black individuals in 2021/22 (IRR 1.42, 95% CI 1.05–1.92), indicating a multiplicative effect of being Black and the pandemic year in increasing FEP risk. A marginal interaction was observed for Asian individuals in the same year, 2021/22, accounting for an IRR of 1.51 (95% CI 0.99–2.32).
Supplementary Table S3 further computes the IRR of Black compared to White British individuals by the year of presentation, showing that this ratio increased from 2.73 (95% CI 2.19–3.41) in 2018/19 up to 3.96 (95% CI 3.22–4.88) in 2021/22.
Discussion
The annual treated FEP incidence diverged from the six-year mean during the COVID-19 pandemic, with subsequent rates returning to pre-pandemic levels. Specifically, treated FEP incidence in South London was ∼58 per 100,000 PY in 2018/19 and 2023/24, peaking at ∼77 per 100,000 PY in 2020/21 and 2021/22.
The increase in incidence rates during the pandemic's peak years occurred in both males and females and across all age-bands. This rise in incidence was greater in Black and Asian than in White British individuals.
To our knowledge, this is the first pre-during-post examination of FEP incidence before, during and after the COVID-19 pandemic, drawn from a well-defined catchment area, encompassing a population at risk of more than five million over six years.
A limitation is that we could only screen individuals referred to SLaM EISs, yet there may be individuals living in the catchment area with psychosis who may not have been referred specifically to these services. Consistently, our pre- and post-pandemic incidence rates are slightly lower (i.e., by about 3 cases per 100,000 PY) than those reported in a comparable catchment area in the EU-GEI study,3 which screened individuals in contact with any secondary psychiatric services. Nonetheless, we avoided differential ascertainment bias over time using the same ascertainment methods throughout the six years.
Furthermore, we cannot rule out the possibility that the observed increase in FEP cases in EISs was due to limited access to primary care services during the first stage of the pandemic, as a ten-year time trend analysis of general practitioner records may suggest.24 If a shift from primary to secondary services occurred, this may have contributed to some of the excess of people accessing EISs during the first stages of the pandemic.
Potential sources of random error in this study include variability in estimates from small subgroups, particularly when stratifying by ethnicity, such as White Other, Mixed, and Other, where smaller sample sizes reduced the precision of our estimates.
Potential sources of systematic error include relying on a population from a specific area of London, characterised by higher levels of social deprivation, crime, and psychosis incidence than other boroughs of the city and the broader UK. This may limit the generalisability of the findings to the wider population, and their applicability to other large-scale traumatic events or natural disasters remains also uncertain.25
Furthermore, given the relatively short duration of the three lockdown measures in the UK (i.e., 23 March 2020 to 1 June 2020, 5 November 2020 to 2 December 2020, 6 January 2021 with gradual easing beginning in March 2021 and restriction lifted by July 2021), we could not reliably measure the putative role of lockdown on the development of psychosis, as individuals who might have developed symptoms during the lockdown could have been referred to EISs shortly after the lockdown windows ended.
Finally, given the observational nature of the study, causal inference cannot be drawn from our data, and we cannot eliminate residual confounders. While the natural pre-during-post quasi-experiment design strengthens causal models by accounting for the temporal introduction and removal of the COVID-19 pandemic and the pre-existing FEP incidence trends, causality cannot be inferred without experimental manipulation or randomisation.
Three previous studies estimated variation in FEP incidence for a shorter duration at the beginning of the COVID-19 pandemic compared with the period just before.14, 15, 16 These studies reported different results that may be explained by differences in the geographic impact of the COVID-19 pandemic, national lockdown measures, cultural and family contexts, or and psychiatric services.26 Specifically, in the early months of the COVID-19 pandemic, non-significant changes were reported in Australia and Catalonia.14,15
In contrast, our findings are consistent with a preliminary report, indicating a 45% increase in FEP incidence in the first pandemic year compared with the year before.16 In the current study, we expanded the catchment area and for the first time we conducted a pre-during-post analysis over a six-year period to ensure sufficient statistical power to validate our previously reported increase in FEP incidence at the onset of the COVID-19 pandemic. The large sample size and extended follow-up period enhanced the precision of our estimates, resulting in narrower confidence intervals, suggesting that the increase in FEP incidence occurred at a slightly smaller magnitude than initially estimated.
Our present study also provides the first evidence that FEP incidence returned to the pre-pandemic levels in 2023/24, consistent with our hypothesis. This finding supports the notion that developing FEP is not a stable phenomenon over time and may fluctuate in response to socioenvironmental and contextual changes.27
Our findings are partially consistent with an interrupted time-series analysis examining extensive data on schizophrenia incidence in Israel. This study showed an initial reduction in schizophrenia risk during the early phase of the COVID-19 pandemic, followed by a projected increase in rates over the subsequent 10 months.25 While we report a consistent FEP rise, our findings confirm their projection. Moreover, we examined the full range of non-affective and affective psychotic disorders, and one possibility is that the COVID-19 pandemic intensified the affective pathway to psychosis. Indeed, social isolation and loneliness may have increased due to the lockdown measures and restricted social opportunities at the beginning of the COVID-19 pandemic,28 and there is evidence of a considerable contextual increase in anxiety and depression conditions.29 On top of that, there could have been a change in the pattern of use of substances associated with psychosis, such as cannabis. There is no evidence of arise in the proportion of people using cannabis; however, some data suggest that individuals already using cannabis increased their frequency of use.9,30 Our stratified incidence rates by sex, age and ethnicity are in line with established literature, specifically reporting that men are more likely to develop psychosis than women.3 Our IRRs also confirm a progressive decrease in FEP risk as age increases, with the highest rates observed in individuals aged 18–19.
This initial risk decreases to 84% in those aged 20–24, progressively declines to 43% in those aged 24–29, and continues to decrease so that by age 60–64 it drops to 12%. The smaller secondary peak in women after age 45 may be consistent with the reported protective role of oestradiol before menopause.31
Our findings by ethnicity are also consistent with previous studies in the UK showing that Black individuals have higher rates of psychosis than White British.2,32 Besides, the interaction in 2021/22 suggests that the pandemic had a higher impact on FEP risk in this demographic. Thus, the incidence gap widened during the pandemic, potentially correlated with social disparities and intersectionality.11 A qualitative interview study conducted in South London and other UK sites suggested several areas of poor mental and physical health experiences for ethnic minority groups during the COVID-19 pandemic.33
Overall, the higher increased psychosis risk among Black and Asian individuals during the interruption across trends may be tentatively explained by structural inequalities, including differential exposure to stressors (e.g., discrimination, social defeat, substandard living and work conditions, financial difficulties, isolation and loneliness) or disparities in access to health services.
The observed FEP incidence increase can therefore be interpreted in the context of intensified exposure to psychosis risk factors during the COVID-19 pandemic, especially among demographics with a pre-existing higher psychosis risk.5 In addition, a direct effect of the COVID-19 infection on the development of psychosis symptoms might have potentially accounted for some of the new cases, given the neurotropism of the virus.34
Finally, the psychological impact of the COVID-19 pandemic might have led to a change in people's beliefs and processing of uncertainty. This shift in prior beliefs has been proposed as an underlying mechanism for developing hallucinations and delusions.35 Indeed, empirical evidence indicated that individuals in the general population experienced more paranoia during the COVID-19 pandemic,26 while those with high levels of paranoia exhibited erratic belief updates in computer-based tasks and were more likely to share pandemic-related conspiracy theories.26
Our findings show an increase in FEP incidence treated by EISs during the COVID-19 pandemic in South London, followed by a gradual return to pre-pandemic levels.
The incidence increase was particularly concerning in individuals of Black ethnicity, who already faced a higher risk of psychosis and COVID-19. Asian also experienced an increase in the incidence of FEP.
These findings may further support that ethnic minorities were more impacted by the COVID-19 pandemic than the rest of the population, consistent with the intersectionality theory.12
The widening incidence gap suggests the pandemic exacerbates social and health inequalities, highlighting the need for context-specific social prevention measures.
Importantly, no previous studies have examined such a long-term period of six years; considering the variability in lockdown measures and the diverse impacts of the COVID-19 pandemic globally, further research from other countries is required to generalise the findings of this study.
Although the longer-term consequences of the COVID-19 pandemic remain uncertain, our findings emphasise that such events may increase the likelihood of developing psychosis in the short term.
Hence, these results may guide policymakers and clinicians in preparing crisis plans for the primary and secondary prevention of psychosis for future pandemics. Social policies should incorporate intersectionality and support groups at higher psychosis risk while ensuring that EISs are adequately resourced to manage increased patient numbers.
Contributors
AQ: Conceptualisation, Investigation, Writing; EP: Conceptualisation, Supervision, Editing, Review; ES: Editing, Review; PBML: Editing, Review; ZL: Editing, Review; RS: Editing, Review; DQ: Conceptualisation, Investigation, Editing, Review; MDF: Conceptualisation, Editing, Review; RMM: Conceptualisation, Editing, Review; MPC: Conceptualisation, Supervision, Editing, Review.
AQ and DQ accessed and verified the data underlying this study.
All authors approved the final version of the manuscript.
Data sharing statement
The data used in this study were obtained through the Clinical Record Interactive Search (CRIS) system.
The CRIS platform provides researchers affiliated with the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre (BRC) access to de-identified electronic health records for approved research projects. Access to CRIS data is restricted to approved researchers who meet the eligibility criteria and have obtained the required ethical and institutional approvals, as the source data are derived from patient records. All applications for data access are subject to review and approval by the CRIS Oversight Committee. Information about the CRIS system and its data access policies is available at the following website: https://www.maudsleybrc.nihr.ac.uk/facilities/clinical-record-interactive-search-cris/.
Declaration of interests
RS reports receiving an educational grant from Takeda to support a PhD studentship and serving as a staff member for PhD supervision with GSK, all outside the submitted work.
DQ reports receiving payments or honoraria for non-promotional lectures from Rovi, outside the submitted work.
MDF reports receiving payments or honoraria for non-promotional lectures from Recordati, outside the submitted work.
RMM reports consultancy roles on advisory boards for Merck, AbbVie, and Boehringer, and payments or honoraria for non-promotional lectures from Recordati and Viatris, all outside the submitted work.
All other authors report no disclosures.
Acknowledgement
DQ is supported by MRC/UKRI CARP (MRC CARP grant MR/W030608/1).
MDF is supported by MRC SRF Fellowship (MRC MR/T007818/1).
RS is part-funded by: i) the NIHR Maudsley Biomedical Research Centre at the South London and Maudsley NHS Foundation Trust and King’s College London; ii) the National Institute for Health Research (NIHR) Applied Research Collaboration South London (NIHR ARC South London) at King’s College Hospital NHS Foundation Trust; iii) UKRI – Medical Research Council through the DATAMIND HDR UK Mental Health Data Hub (MRC reference: MR/W014386); iv) the UK Prevention Research Partnership (Violence, Health and Society; MR-VO49879/1), an initiative funded by UK Research and Innovation Councils, the Department of Health and Social Care (England) and the UK devolved administrations, and leading health research charities.
DQ, RMM, MDF, RS, MPC are supported by NIHR BRC at SLaM and KCL.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2025.103086.
Appendix A. Supplementary data
References
- 1.American Psychiatric Association . American psychiatric association; Washington, DC: 2013. Diagnostic and statistical manual of mental disorders: DSM-5. [Google Scholar]
- 2.Kirkbride J.B., Fearon P., Morgan C., et al. Heterogeneity in incidence rates of schizophrenia and other psychotic syndromes: findings from the 3-center AeSOP study. Arch Gen Psychiatry. 2006;63(3):250–258. doi: 10.1001/archpsyc.63.3.250. [DOI] [PubMed] [Google Scholar]
- 3.Jongsma H.E., Gayer-Anderson C., Lasalvia A., et al. Treated incidence of psychotic disorders in the Multinational EU-GEI Study. JAMA Psychiatr. 2018;75(1):36–46. doi: 10.1001/jamapsychiatry.2017.3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morgan C., Cohen A., Esponda G.M., et al. Epidemiology of untreated psychoses in 3 diverse settings in the global South: the International Research Program on Psychotic Disorders in Diverse Settings (INTREPID II) JAMA Psychiatr. 2023;80(1):40–48. doi: 10.1001/jamapsychiatry.2022.3781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Murray R.M., Mondelli V., Stilo S.A., et al. The influence of risk factors on the onset and outcome of psychosis: what we learned from the GAP study. Schizophr Res. 2020;225:63–68. doi: 10.1016/j.schres.2020.01.011. [DOI] [PubMed] [Google Scholar]
- 6.Kotsiri I., Resta P., Spyrantis A., et al. Viral infections and schizophrenia: a comprehensive review. Viruses. 2023;15(6) doi: 10.3390/v15061345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ayesa-Arriola R., Castro Quintas A., Ortiz-Garcia de la Foz V., et al. Exploring the impact of COVID-19 on newborn neurodevelopment: a pilot study. Sci Rep. 2023;13(1):2983. doi: 10.1038/s41598-023-29680-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kepinska A.P., Iyegbe C.O., Vernon A.C., Yolken R., Murray R.M., Pollak T.A. Schizophrenia and influenza at the centenary of the 1918-1919 Spanish influenza pandemic: mechanisms of psychosis risk. Front Psychiatry. 2020;11:72. doi: 10.3389/fpsyt.2020.00072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spinazzola E., Quattrone D., Quattrone A., Murray R.M., Forti M.D. The increased incidence of psychosis during the COVID-19 pandemic in South London: the role of heavy cannabis use. Psychiatry Res. 2024;336 doi: 10.1016/j.psychres.2024.115869. [DOI] [PubMed] [Google Scholar]
- 10.Ahmed N., Barnett P., Greenburgh A., et al. Mental health in Europe during the COVID-19 pandemic: a systematic review. Lancet Psychiatr. 2023;10(7):537–556. doi: 10.1016/S2215-0366(23)00113-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vai B., Mazza M.G., Delli Colli C., et al. Mental disorders and risk of COVID-19-related mortality, hospitalisation, and intensive care unit admission: a systematic review and meta-analysis. Lancet Psychiatr. 2021;8(9):797–812. doi: 10.1016/S2215-0366(21)00232-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Holman D., Salway S., Bell A., et al. Can intersectionality help with understanding and tackling health inequalities? Perspectives of professional stakeholders. Health Res Policy Syst. 2021;19(1):97. doi: 10.1186/s12961-021-00742-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tang Y., Kirk B., Olanrewaju F., et al. Cannabis use among adolescents and young adults during the COVID-19 pandemic: a systematic review. Drug Alcohol Depend Rep. 2024;11 doi: 10.1016/j.dadr.2024.100232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.O'Donoghue B., Collett H., Boyd S., et al. The incidence and admission rate for first-episode psychosis in young people before and during the COVID-19 pandemic in Melbourne, Australia. Aust N Z J Psychiatry. 2022;56(7):811–817. doi: 10.1177/00048674211053578. [DOI] [PubMed] [Google Scholar]
- 15.Casanovas F., Trabsa A., Berge D., et al. Incidence rate and distinctive characteristics of first episode psychosis during the COVID-19 pandemic: a multicenter observational study. Sci Rep. 2022;12(1) doi: 10.1038/s41598-022-26297-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spinazzola E., Meyer Z., Gray Z.I., et al. The effect of the COVID-19 pandemic on the treated incidence of psychotic disorders in South London. Psychiatry Res. 2023;329 doi: 10.1016/j.psychres.2023.115483. [DOI] [PubMed] [Google Scholar]
- 17.Danan L.N., Poulle J., Bannay A., Baillot S., Laprevote V., Dobre D. COVID-19 crisis and the incidence of hospital admissions for psychosis in France. Encephale. 2024;50(4):386–390. doi: 10.1016/j.encep.2023.08.003. [DOI] [PubMed] [Google Scholar]
- 18.Kelbrick M., da Silva K., Griffiths C., et al. The impact of COVID-19 on acute psychiatric admissions for first and repeated episode psychosis. Int J Soc Psychiatry. 2023;69(8):2042–2047. doi: 10.1177/00207640231188031. [DOI] [PubMed] [Google Scholar]
- 19.Segev A., Hirsch-Klein E., Kotz G., et al. Trends of new-onset psychosis or mania in psychiatric emergency departments during the COVID19 pandemic: a longitudinal comparative study. Sci Rep. 2021;11(1) doi: 10.1038/s41598-021-00310-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.England. PH . 2020. Understanding the impact of COVID-19 on BAME groups. [Google Scholar]
- 21.Stewart R., Soremekun M., Perera G., et al. The South London and Maudsley NHS foundation trust biomedical research centre (SLAM BRC) case register: development and descriptive data. BMC Psychiatr. 2009;9:1–12. doi: 10.1186/1471-244X-9-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jablensky A., Sartorius N., Ernberg G., et al. Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study. Psychol Med Monogr Suppl. 1992;20:1–97. doi: 10.1017/s0264180100000904. [DOI] [PubMed] [Google Scholar]
- 23.Office for National Statistics, Census 2021 Ethnic group by sex by age. 2023. https://www.ons.gov.uk/datasets/RM032/editions/2021/versions/1
- 24.Carr M.J., Steeg S., Webb R.T., et al. Effects of the COVID-19 pandemic on primary care-recorded mental illness and self-harm episodes in the UK: a population-based cohort study. Lancet Public Health. 2021;6(2):e124–e135. doi: 10.1016/S2468-2667(20)30288-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Travis-Lumer Y., Kodesh A., Goldberg Y., Reichenberg A., Frangou S., Levine S.Z. Biopsychosocial exposure to the COVID-19 pandemic and the relative risk of schizophrenia: interrupted time-series analysis of a nationally representative sample. Eur Psychiatry. 2022;65(1) doi: 10.1192/j.eurpsy.2021.2245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suthaharan P., Reed E.J., Leptourgos P., et al. Paranoia and belief updating during the COVID-19 crisis. Nat Hum Behav. 2021;5(9):1190–1202. doi: 10.1038/s41562-021-01176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Murray R.M., Quattrone D. The Kraepelian concept of schizophrenia: dying but not yet dead. Schizophr Res. 2022;242:102–105. doi: 10.1016/j.schres.2021.12.005. [DOI] [PubMed] [Google Scholar]
- 28.Su Y., Rao W., Li M., Caron G., D'Arcy C., Meng X. Prevalence of loneliness and social isolation among older adults during the COVID-19 pandemic: a systematic review and meta-analysis. Int Psychogeriatr. 2023;35(5):229–241. doi: 10.1017/S1041610222000199. [DOI] [PubMed] [Google Scholar]
- 29.Santomauro D.F., Mantilla Herrera A.M., Shadid J., et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. Lancet. 2021;398(10312):1700–1712. doi: 10.1016/S0140-6736(21)02143-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lake S., Assaf R.D., Gorbach P.M., Cooper Z.D. Changes in secondary substance use after the onset of the COVID-19 pandemic among people who use cannabis: findings from a web-based sample of adults in the United States. Exp Clin Psychopharmacol. 2023;31(2):482–490. doi: 10.1037/pha0000572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Riecher-Rössler A., Häfner H. Gender aspects in schizophrenia: bridging the border between social and biological psychiatry. Acta Psychiatr Scand. 2000;102(s407):58–62. doi: 10.1034/j.1600-0447.2000.00011.x. [DOI] [PubMed] [Google Scholar]
- 32.Coid J.W., Kirkbride J.B., Barker D., et al. Raised incidence rates of all psychoses among migrant groups: findings from the East London first episode psychosis study. Arch Gen Psychiatry. 2008;65(11):1250–1258. doi: 10.1001/archpsyc.65.11.1250. [DOI] [PubMed] [Google Scholar]
- 33.Ocloo J., Stuart R., Dasch H.K., et al. Living less safely through the pandemic in England for people with serious mental and physical health conditions: qualitative interviews with service users and carers of Black African, Caribbean, and South-Asian descent. BMC Publ Health. 2024;24(1):2718. doi: 10.1186/s12889-024-20107-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Taquet M., Skorniewska Z., De Deyn T., et al. Cognitive and psychiatric symptom trajectories 2-3 years after hospital admission for COVID-19: a longitudinal, prospective cohort study in the UK. Lancet Psychiatr. 2024;11(9):696–708. doi: 10.1016/S2215-0366(24)00214-1. [DOI] [PubMed] [Google Scholar]
- 35.Corlett P.R., Horga G., Fletcher P.C., Alderson-Day B., Schmack K., Powers A.R. 3rd. Hallucinations and strong priors. Trends Cogn Sci. 2019;23(2):114–127. doi: 10.1016/j.tics.2018.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.