Abstract
Background
Individuals in rural areas consistently demonstrate higher mortality and morbidity rates, and poorer access to healthcare, compared to their metropolitan counterparts. Optimizing the implementation of evidence-based interventions can reduce these inequities. Existing literature outlines numerous barriers and facilitators to the implementation of healthcare interventions, but these are generally not specific to rural areas. This rapid review aims to synthesize barriers and facilitators to the implementation of healthcare interventions in regional and rural healthcare services as reported by healthcare staff, including clinicians, managers, and administrators.
Methods
A systematic search for peer-reviewed publications was conducted using CINAHL, PsycINFO, Medline, and Embase databases (1/1/2000–29/08/2023). Eligible publications were primary research articles published in English, assessing staff-reported barriers and facilitators to implementing healthcare interventions within regional and rural areas of high-income countries. Qualitative, quantitative, and mixed-methods designs were included. Eligible healthcare settings encompassed acute, sub-acute, primary care, community health, and aged care. Barrier and facilitator data were coded and grouped into sub-themes and broader themes, with results presented narratively.
Results
Thirty-nine publications met the inclusion criteria. Most studies were conducted in Australia or the USA (both n = 18, 46%), within primary care (n = 13, 33%) or hospital settings (n = 12, 31%) in rural (n = 22, 56%) or regional (n = 9, 23%) locations. Implementation barriers and facilitators were grouped into four overarching themes: intervention-level (intervention feasibility and fit; complexity; privacy and confidentiality); staff-level (staff attitudes and beliefs; knowledge, skills, and confidence; staff roles and professional identity), patient-level (patient characteristics; attitudes), and system-level (leadership support; environmental resources and context; geographic vastness; networks and communication).
Conclusions
These findings provide essential guidance for policymakers, healthcare leaders, and researchers in planning and designing future implementation efforts in regional and rural healthcare settings. By considering factors across intervention, staff, patient, and system levels, stakeholders can address challenges and leverage local strengths to enhance implementation success and reduce health disparities.
Trial registration
PROSPERO registration number: CRD42023470736. Registered 19/10/2023.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12913-025-12480-8.
Keywords: Rural health, Implementation science, Barriers, Facilitators, Review, Healthcare
Background
The persistent gap in health outcomes between rural and metropolitan areas represents a significant challenge for healthcare systems globally [1]. Individuals living in rural areas, which are generally characterized by geographical vastness and sparse population distribution [2], consistently experience higher mortality and morbidity rates, along with poorer access to healthcare services, compared to their metropolitan counterparts [3, 4]. These disparities in provision and access of care are influenced by a complex interplay of social, economic, geographical, and system-related factors [5].
Optimizing the implementation of evidence-based interventions (EBIs) has emerged as vital to addressing the health inequities experienced by key population groups, such as those living in regional and rural areas [6]. EBIs are broadly defined as practices, programs, policies, processes, or guideline recommendations that have been proven effective in improving health outcomes [7]. When implemented as intended, EBIs have significant potential to enhance the quality of care and outcomes for people living in regional and rural settings [8]. Yet, integrating EBIs into routine healthcare practice is challenging and complex, with many healthcare interventions not routinely adopted, delivered or sustained [9].
To support the uptake and sustainability of EBIs, the identification of context-specific barriers and facilitators (i.e. determinants) to implementation is recommended as an important step that enables the design of tailored, theory-informed implementation strategies [10]. While existing implementation research has extensively documented various determinants to implementation across a range of healthcare contexts [11–13], there remains a significant gap in understanding the unique experiences of regional and rural areas. Healthcare services in these areas are required to leverage strengths and overcome challenges such as geographic spread, low population density, limited infrastructure, and workforce retention to effectively implement EBIs [14]. A nuanced understanding of the factors influencing implementation in regional and rural healthcare services will be essential for bridging the health disparities between rural and metropolitan populations.
To address this gap, we aimed to synthesize barriers and facilitators to the implementation of healthcare interventions in regional and rural healthcare services as reported by healthcare staff, including clinicians, managers, and administrators. Given the significant differences between high- and low-income healthcare settings [15]—such as resources, infrastructure, health system structure, workforce, disease burden, and policy environments—this rapid review specifically focused on healthcare staff working in high-income countries. Healthcare staff are uniquely positioned to provide valuable insights into the practical realities of implementing healthcare interventions in their settings. By focusing on their lived experiences, this review will inform future implementation efforts in regional and rural areas and contribute to the design of more effective and equitable healthcare solutions.
Methods
Design
This study adopted a rapid review design, a form of knowledge synthesis that accelerates the process of conducting a traditional systematic review through streamlining or omitting various methods to produce evidence for stakeholders in a resource-efficient manner [16]. This approach met the practical need of informing the authors’ broader research program, funded by the Medical Research Future Fund in Australia under the Rapid Applied Research Translation initiative. In this review, streamlining of methods included applying limiters to the systematic search (English-language, year of publication 2000 +), using single data extraction (checked for accuracy), and omitting the critical appraisal step. Additionally, knowledge users, specifically clinicians based in regional and rural areas, were included as part of the authorship team, and participated in all stages of the review process. The Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) [17] statement and the interim guidance for the reporting of rapid reviews [18] guided the reporting of this review (See Supplementary File 1); the protocol was prospectively registered in PROSPERO (CRD42023470736).
Search strategy
A literature search was conducted on 29/08/2023 using four electronic databases (Medline, Embase, PsycINFO and CINAHL); additional studies were identified by searching the reference lists of included papers. The search was limited to articles published after 1 January 2000, aligning with the emergence of implementation science as a distinct discipline [19]. While healthcare interventions have advanced rapidly in the past decade, this broader timeframe ensured the inclusion of both foundational implementation research and recent developmentsrelevant to contemporary healthcare practices. Preliminary literature searches and key terms from relevant literature [11, 20] guided the development of a comprehensive list of search terms. The search strategy used key terms and synonyms related to the following concepts: the regional/rural context, implementation, healthcare setting, barriers and facilitators (Supplementary File 2). To increase the sensitivity of the search, key terms that mapped to specific subject headings (e.g., MeSH) were included and adapted according to each database. Additionally, truncations and expansions were applied to selected search terms.
Inclusion and exclusion criteria
A summary of the eligibility criteria for this review is provided in Table 1. Barriers and facilitators were broadly conceptualized as any factor that either hindered or promoted the implementation process of healthcare interventions and included synonymous terms, such as challenges and enablers. The designations of factors as barriers and facilitators within primary research studies were accepted as reported. Classifications of regional and rural were also accepted as reported; authors did not have to explicitly refer to a geographical classification system (e.g., Rural–Urban Continuum Codes (RUCC) [21] or Modified Monash Model [22] (MMM)) for a study to be considered eligible, although this information was extracted from included papers. Inclusion was limited to studies conducted in high-income countries, as defined by the World Bank classification [23] (as at 11 August 2023). Importantly, papers that only assessed intervention effectiveness e.g., clinical or health outcomes, rather than factors influencing the implementation process, were excluded.
Table 1.
Summary of eligibility criteria for the review
| Criteria | Included | Excluded |
|---|---|---|
| Population | Healthcare staff in eligible context. Includes clinicians, managers, and administrators | Non-healthcare staff, or healthcare staff based in an ineligible context |
| Context | Acute, sub-acute, primary, community health, and residential aged care settings | Non-healthcare settings (e.g., workplaces, schools) |
| Regional and rural areas (e.g., MMM 2–5) | Major cities/metropolitan areas (e.g. MMM 1) & remote areas (e.g., MMM 6–7); with regional and/or rural areas not separated in analysis | |
| High-income countries, according to The World Bank rankings [23] (excluded at full-text stage only) | Low- and middle-income countries (excluded at full-text stage only) | |
| Intervention of focus | Healthcare interventions encompassing direct patient interventions (e.g., clinical or therapeutic practices or programs) or interventions with an intended benefit on health outcomes or quality of care (e.g., guidelines, processes, models of care) | Non-healthcare interventions/interventions with a primary focus on administrative outcomes, rather than quality of care or health outcomes. (e.g., management interventions, staff rostering interventions, referral only interventions) |
| Outcomes | Healthcare staff-reported barriers and facilitators to the implementation process. Could be collected during any stage of implementation (i.e., pre-implementation, during implementation, or post-implementation) | Not healthcare staff-reported barriers and facilitators to implementation (i.e., patient-reported barriers) |
| Publication type | Original research, including case-studies, qualitative, quantitative, and mixed method research | Theses, conference abstracts, reviews, commentaries, editorials, published books, protocols |
| English language full-text articles only | Articles not published in English | |
| Publication date | Published from 1 January 2000-August 29 2023 | Published prior to 1 January 2000 |
Study selection and data analysis
Database search results were imported into Endnote X9 to remove duplicates; remaining records were then uploaded to Covidence. All records were independently screened in duplicate by title and abstract; potentially relevant full-text articles were then dual-screened against pre-specified eligibility criteria. Any screening conflicts were resolved through discussion or by involving the senior author. Only full-text articles that met all inclusion criteria progressed to data extraction.
Data extraction was performed using REDCap, with each paper undergoing single data extraction. A broad team of reviewers extracted data on study characteristics, including year and country of study, description of rurality, participant characteristics, description of intervention, and methodological approaches. Two authors (AC & DM) concurrently extracted barrier and facilitator data; these data were extracted in narrative form as per the explicit reporting within each article. Following single extraction, the first author reviewed data for completeness.
A narrative synthesis approach was employed to integrate and interpret the extracted barrier and facilitator data [24]. Relevant data fields were exported from REDCap into Excel and organized into a summary table that included the name, description, illustrative quotes, and the designation of whether each item was categorized as a barrier or a facilitator within each study. This summary table was then imported into NVivo software, where two authors (AC & AB) independently coded data, applying an inductive approach to identify key concepts. These concepts were first organized into sub-themes and then grouped into overarching themes. Given most included studies did not formally use an implementation framework to collect, analyze, or present their findings, data were not coded according to a specific implementation framework. To enhance the rigor of synthesis, themes and sub-themes were discussed among the broader author team, allowing the incorporation of diverse perspectives, including input from clinicians with lived experience in implementing healthcare interventions in rural and regional areas. In addition to the narrative synthesis, summary statistics were generated to describe the study characteristics.
Results
Search results
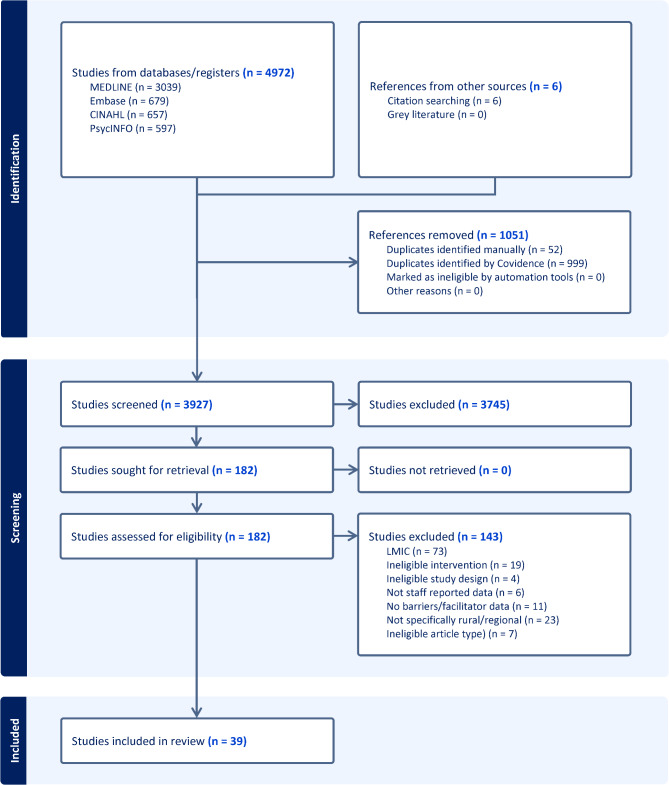
After removing duplicates, the search yielded 3,927 citations, from which 182 full texts were examined. Ultimately, 39 publications met the inclusion criteria. The PRISMA flow diagram details the search process and reasons for exclusion (Fig. 1).
Fig. 1.
PRISMA Flow chart
Characteristics of included studies
Characteristics of included studies are provided in Table 2. Most studies were published within the previous five years (2019–2023: n = 27, 69%) and were conducted in Australia or the United States of America (USA) (n = 18 each, 46%). The majority described their context as rural (n = 22, 56%), followed by regional (n = 9, 23%) and mixed rural/regional (n = 8, 21%). Only seven (18%) studies explicitly used a geographical classification system to define the context (Australian Statistical Geography Standard: n = 2, Urban Influence Codes: n = 2, MMM n = 1, Accessibility/Remoteness Index of Australia n = 1, RUCC n = 1). Primary care (n = 13, 33%), hospital (n = 12, 31%), and mixed healthcare settings (n = 8, 21%) were the most common healthcare settings, followed by community health (n = 3, 8%), and residential aged care (n = 3, 8%).
Table 2.
Summary table of included articles (n = 39)
| First author, citation | Year | Country | Health service | Intervention of focus (classification type) | Staff sample characteristics | Rurality | Data collection approachb | Use of implementation TMF |
|---|---|---|---|---|---|---|---|---|
| Andrilla [25] | 2017 | USA | Primary care | Buprenorphine maintenance treatment– prescription of buprenorphine to treat opioid use disorder. (Clinical Practice/ Program) | (N = 1,124). Physicians | Rural, as defined by an Urban Influence Code designation | Quantitative (surveys) | No |
| Beks [26] | 2022 | Australia | Community health |
Tulku wan Wininn primary health mobile clinic using an Aboriginal Community-Controlled Health Organization model of service delivery (Model of Care) |
(N = 19). Included health service personnel and key informants (n = 12), and Aboriginal and/or Torres Strait Islander clients (n = 7) | Rural, as defined by the Modified Monash Model | Qualitative (interviews) | No |
| Berends [27] | 2012 | Australia | Hospital |
Screening and brief intervention for risky alcohol use and referral to treatment (Screening & Assessment) |
(N = 149). Survey participants (nurses; n = 142); Interview participants (stakeholders; n = 7) | Regionala | Mixed methods (surveys, interviews) | No |
| Chatterton [28] | 2022 | Australia | Community health, public mental health service with tertiary education provider |
Telehealth mental health response in a regional public mental health provider. Targeted to healthcare providers and patients (Digital Health Intervention) |
(N = 32). Medical, nursing and allied health staff | Regionala | Qualitative (interviews, focus groups) | No |
| Daugherty [29] | 2021 | USA | Hospital, Primary care |
Clinical Recommendations in the CDC Paediatric Mild Traumatic Brain Injury Guideline– targeted to healthcare providers and patients (Guideline/ Recommendation) |
(N = 9). Healthcare providers, including physicians (n = 5); physician assistant (n = 2); nurse practitioners (n = 2) | Rurala | Qualitative (interviews) | No |
| DeHart [30] | 2021 | USA | Hospital, Primary care |
Telehealth modalities including live videoconferencing, store-and-forward, remote patient monitoring and mobile health (Digital Health Intervention) |
(N = 17). Health providers, including administrators (n = 7); nurses (n = 3); physicians (n = 2); dieticians (n = 2); counsellors (n = 1); social workers (n = 1); educator (n = 1) | Mixed rural/regionala | Mixed methods (surveys, interviews, focus groups) | No |
| Delaforce [31] | 2023 | Australia | Hospital |
Concentric Care fall prevention platform– digital intervention targeted to nursing staff in inpatient settings. Consists of speech-enabled nurse call system, location services and digital dashboards to assist with care provision for high-risk fall patients (Digital Health Intervention) |
(N = 12). Nursing staff, including nurses (n = 8); nurse managers (n = 4) | Rurala | Qualitative (interviews, focus groups) |
Yes (CFIR) |
| Druskin [32] | 2022 | USA | Range of healthcare settings | Parent–Child Interaction Therapy targeted to patients, families, and healthcare providers– opioid crisis-related emotional and behavioural intervention for children, teaches positive and appropriate strategies for parents. (Clinical Practice/ Program) | (N = 34). Therapists at doctoral level and masters level, and doctoral student trainees | Rurala | Qualitative (interviews) | No |
| Dwyer [33] | 2020 | Australia | Hospital |
Australian Commission on Safety and Quality in Health Care's Acute Stroke Clinical Care Standard (Guideline/ Recommendation) |
(N = 11). Clinicians; including interview participants (n = 3; pharmacist, senior nurse, physiotherapist); focus group participants (n = 8; neurologists, a general medical physician) | Regional, using the Accessibility/Remoteness Index for Australia 2011 system | Qualitative (interviews, focus groups) | No |
| Ervin [34] | 2019 | Australia | RAC |
Older person's nurse practitioner role and extended scope of practice in residential aged care (Model of Care) |
(N = 58). Health service management, care managers, nursing and care staff, and GPs | Mixed rural/regionala | Qualitative (interviews, focus groups) |
Yes (May’s Implementation Theory) |
| Findholt [35] | 2013 | USA | Primary care |
Implementation of the American Medical Association Expert Committee recommendations for assessment, treatment and prevention of childhood obesity (Guideline/ Recommendation) |
(N = 13). Clinicians | Rural, using Urban Influence Code designations | Qualitative (interviews) | No |
| Fletcher [36] | 2016 | Australia | Hospital, primary care |
Advanced Care Planning– discussion exploring issues of end-of-life experience for patients in aged care facilities. Targeted to healthcare providers and patients (Care Planning) |
(N = 55). GPs, general practice registrars, practice nurses, community nurses, hospital nurses | Mixed rural/regional, as defined by ASGC– Remoteness Area | Qualitative (focus groups) | No |
| Harrod [37] | 2014 | USA | Hospital |
Effort to prevent healthcare-associated infections for patients—included data on the local safety culture, administrative support for infection prevention, and hospital's infection prevention program (Clinical Practice/ Program) |
(N = 72). Lead infection preventionists at rural veterans’ affairs hospitals | Rurala | Mixed methods (surveys, interviews) | No |
| Henderson [38] | 2018 | Australia | Range of healthcare settings |
Integrated care for older people with mental health problems (Model of Care) |
(N = 31). Healthcare providers; included NGO (n = 3); social support services (n = 3); mental health (n = 4); aged care (n = 4); primary care (n = 9); community health (n = 6); local government (n = 1); hospital (n = 1) | Mixed rural/regionala | Qualitative (interviews) | No |
| Hill [39] | 2022 | Australia | RAC |
Provision of prescribed texture-modified food and fluids for residents with dysphagia (Guideline/ Recommendation) |
(N = 11). Included nurses (n = 6) and food services staff (n = 5) in aged care facility | Rurala | Qualitative (focus groups) | No |
| Howland [40] | 2021 | USA | Primary care |
Telepsychiatric Collaborative Care (support to providers treating patients at FQHCs) or telemental health referral (videoconferencing patient assessment and treatment at FQHC) (Digital Health Intervention) |
(N = 14). Including off-site telepsychiatrists (n = 10); telepsychologists (n = 4) | Rurala | Qualitative (interviews) |
Yes (CFIR) |
| Khoong [41] | 2014 | USA | Primary Care |
Clinical preventive service guidelines (Guideline/ Recommendations) |
(N = 29). Primary care physicians | Mixed rural/regionala | Qualitative (interviews) | No |
| Kilcullen [42] | 2017 | Australia | Hospital |
Delivery of neonatal palliative care by neonatal ICU nurses (Clinical Practice/ Program) |
(N = 8). Neonatal ICU nurses with experience providing neonatal palliative care | Mixed rural/regionala | Qualitative (interviews) | No |
| Kirstman-Valente [43] | 2022 | USA | Primary care |
Cannabis use reduction screening, brief intervention, and referral to treatment model for adolescent cannabis users (Model of Care) |
(N = 11). Patient-engaged providers/staff from Seattle Children’s Care Network Includes paediatricians (n = 7); paediatric nurse practitioners (n = 2); registered nurse (n = 1); practice manager (n = 1) |
Regionala | Qualitative (focus groups) | No |
| Kruse-Diehr [44] | 2022 | USA | Primary care |
Colorectal Cancer Screening (Screening & Assessment) |
(N = 7). Medical providers, primarily nurses from 4 primary care clinics | Rurala | Qualitative (interviews) | No |
| Lam [45] | 2018 | Australia | RAC |
Advanced Care Planning– discussion exploring issues of end-of-life experience for patients in aged care facilities (Care Planning) |
(N = 114). Nurses, care managers, occupational therapists, medical doctors. Includes survey participants (n = 109; interview participants (n = 5) | Rurala | Mixed methods (surveys, interviews) | No |
| Lillebuen [46] | 2020 | Canada | Hospital |
Peritoneal dialysis provided by ED nurses (Clinical Practice/ Program) |
(N = 7). Nurse managers and clinical nurse educators employed at participating sites | Rurala | Qualitative (interviews) | No |
| Littlewood [47] | 2019 | Australia | Primary care |
Advanced Care Planning—supporting adults to understand and share values, goals, and future medical care preferences during serious and chronic illnesses (Care Planning) |
(N = 13). General practice registrars and recently fellowed GPs | Rural, as defined by the Australian Statistical Georgraphical Classification– Remoteness Area | Qualitative (interviews) | No |
| Maxwell [48] | 2021 | Australia | Community health |
Reablement-focused program for older people in regional Australia. Intervention included training for community-based organisational staff to incorporate and reflect on reablement into practice (Clinical Practice/ Program) |
(N = 17). Included care coordinators (n = 13, focus groups); direct care staff (n = 4, interviews) | Regionala | Qualitative (interviews, focus groups) | No |
| Morgan [49] | 2019 | Canada | Primary care |
Evidence-based interdisciplinary primary healthcare memory clinic for dementia (Model of Care) |
(N = 25). Included primary healthcare team members, managers, office staff | Rurala | Qualitative (interviews, focus groups) |
Yes (CFIR) |
| Muir-Cochrane [50] | 2014 | Australia | Community health, RAC |
Mental health care for older people through health and social services (Clinical Practice/ Program) |
(N = 19). Key informants from 16 local government and non-government health and social care agencies | Rurala | Qualitative (interviews) | No |
| Nelson-Brantley [51] | 2021 | USA | Primary care |
Cancer screening practices in rural primary care practices (Screening & Assessment) |
(N = 28). Physicians, nurses, osteopath, medical assistant, care coordinator and administrators in primary care practices | Rural, as defined by Rural–Urban Continuum Codes | Qualitative (focus groups) |
Yes (CFIR) |
| Paliadelis [52] | 2005 | Australia | Hospital |
'Family centred care'– paediatric nurses’ involvement of parents in the care of hospitalized children (Model of Care) |
(N = 14). Paediatric nurses | Regionala | Qualitative (interviews) | No |
| Parchman [53] | 2020 | USA | Primary care |
The Six Building Blocks program—management of patients using long-term opioid therapy. Includes leadership support, revision and alignment of policies, tracking and monitoring patients, planned, patient-centred visits, identifying and connecting to resources for complex patients, and measuring success (Model of Care) |
(N not specified). Staff and clinicians, including opiod improvement team members, from six organisations | Rurala | Qualitative (interviews, focus groups) | No |
| Porter [54] | 2021 | USA | Primary care |
Three evidence-based intensive weight management programs: (1) Calcium Weighs-In (2) TOURS, and (3) diaBEAT-it! (Clinical Practice/ Program) |
(N = 51). Included physicians (n = 15); nurses (n = 11); clinic managers/ administrators (n = 9); physical assistants/nurse practitioners (n = 7), clinic staff (n = 7); health coach /coordinator (n = 2) | Mixed rural/regionala | Qualitative (focus groups) |
Yes (PARiHS Framework) |
| Rosado [55] | 2023 | USA | Primary care |
Adverse childhood experiences screening protocol (Screening & Assessment) |
(N = 12). Paediatricians; survey participants (n = 6); focus group participants (n = 6) | Rurala | Mixed methods (surveys, focus groups) |
Yes (EPIS Framework) |
| Rosenberg [56] | 2022 | USA | Hospital |
ED-initiated buprenorphine for patients presenting with OUD (Clinical Practice/ Program) |
(N = 11). ED Directors from Critical Access Hospital EDs | Rurala | Qualitative (interviews) | No |
| Saunders [57] | 2019 | USA | Primary care |
Substance use screening (alcohol/drug) (Screening & Assessment) |
(N = 43). Primary care providers and medical assistants, including medical assistants (n = 22); nurse practitioners (n = 9); physician assistants (n = 8); medical doctors (n = 6); doctor of osteopathy (n = 1); and other (n = 2) | Rurala | Qualitative (interviews, focus groups) |
Yes (Knowledge to Action Framework) |
| Seidel [58] | 2022 | Germany | Hospital, Primary care |
Dementia Care Management– multimodal and multiprofessional model of care for people with dementia. Comprises of management of treatment and care, medication management, and caregiver support and education (Model of Care) |
(N = 22). Healthcare providers, including doctors (n = 2); nurses and care providers (n = 7); palliative care providers (n = 1); regional networks (n = 1); hospitals (n = 4); counselling services (n = 4); self-help services (n = 3) | Regionala |
Qualitative (interviews) |
Yes (CFIR) |
| Shreck [59] | 2020 | USA | Community health |
Telemental health delivered in Veteran's Health Administration through secure, real-time, interactive clinical videoconferencing systems (Digital Health Intervention) |
(N = 9). Psychologists | Mixed rural/regionala | Qualitative (document review) | No |
| Shulver [60] | 2016 | Australia | Hospital |
Telehealth into mainstream healthcare services in the care of older people (Digital Health Intervention) |
(N = 44). Clinicians and care workers | Rurala | Qualitative (focus groups) |
Yes (Normalisation process theory) |
| Stanford [61] | 2019 | Australia | Hospital |
Patient-practitioner communication and education with Aboriginal and Torres Strait Islanders within inpatient/outpatient cardiac or coronary care units (Model of Care) |
(N = 17). Included nursing staff (n = 11); cardiologists (n = 5); Aboriginal health worker (n = 1) | Regionala | Qualitative (interviews) | No |
| Watson [62] | 2022 | USA | Hospital |
Recovery Coach and Peer Support Initiative– aims to implement peer support services within EDs, targeting patients with OUD, linking them to treatment and services (Model of Care) |
(N not specified). 4 ED vendors participated. Interviewees included primary leader of implementation, peers, and supervisors of peers | Rurala | Qualitative (interviews) |
Yes (CFIR) |
| Wilkinson [63] | 2019 | Australia | Hospital |
Evidence-based model of care for GDM care in dietetics, specifically Medical Nutrition Therapy (Model of Care) |
(N = 8). Practitioners, including GDM dietitian, site project champion, dietetics project lead, and key stakeholders | Regionala | Qualitative (interviews) | No |
CDC Centres for Disease Control and Prevention, CFIR Consolidated Framework for Implementation Research, ED Emergency Department, EPIS Exploration, Preparation, Implementation, Sustainment, FDHQ Federally Qualified Health Centre, GDM Gestational Diabetes Mellitus, GP General Practitioner, ICU Intensive Care Unit, OUD Opioid Use Disorder, PARiHS Promoting Action on Research Implementation in Health Services, RAC Residential Aged Care, TMF Theory, Model or Framework, USA United States of America
aIndicates the article did not use a geographical classification system to define rurality
bData collection approach refers to the approach used to collect barrier and facilitator data only
Most studies exclusively used qualitative methods to collect barrier/facilitator data (n = 33, 85%) via interviews (n = 18), focus groups (n = 6), document review (n = 1), or multiple qualitative approaches (n = 8; e.g. interviews and focus groups). Five studies (13%) used mixed-methods, while one study (3%) exclusively used a quantitative approach (survey). Less than one third of studies (n = 11, 28%) reported using an implementation theory, model or framework to guide an aspect of implementation; the most common was the Consolidated Framework for Implementation Research [64] (CFIR; n = 6, 15%).
The interventions studied were diverse. Models of care were most common (n = 11, 28%). Other intervention types included clinical practices/programs (n = 9, 23%), digital health interventions (n = 6, 15%), screening/assessment (n = 5, 13%), guidelines/recommendations (n = 5, 13%), and care planning (n = 3, 8%). Furthermore, only limited priority populations were specifically targeted in these interventions. For instance, only two studies specifically focused on Aboriginal populations [26, 61], while a single study targeted a culturally and linguistically diverse group (Latino children living in the USA) [55].
Key barriers and facilitators to implementation
Key barriers and facilitators as perceived by healthcare staff, are presented below within four overarching themes: intervention-level, staff-level, patient-level, and system-level (Fig. 2). While a patient-level theme emerged from the findings, it is important to note that this theme reflects staff-reported perceptions of patient-related factors, rather than direct patient input. Specific barriers and facilitators reported in each study are detailed in Supplementary File 3.
Fig. 2.
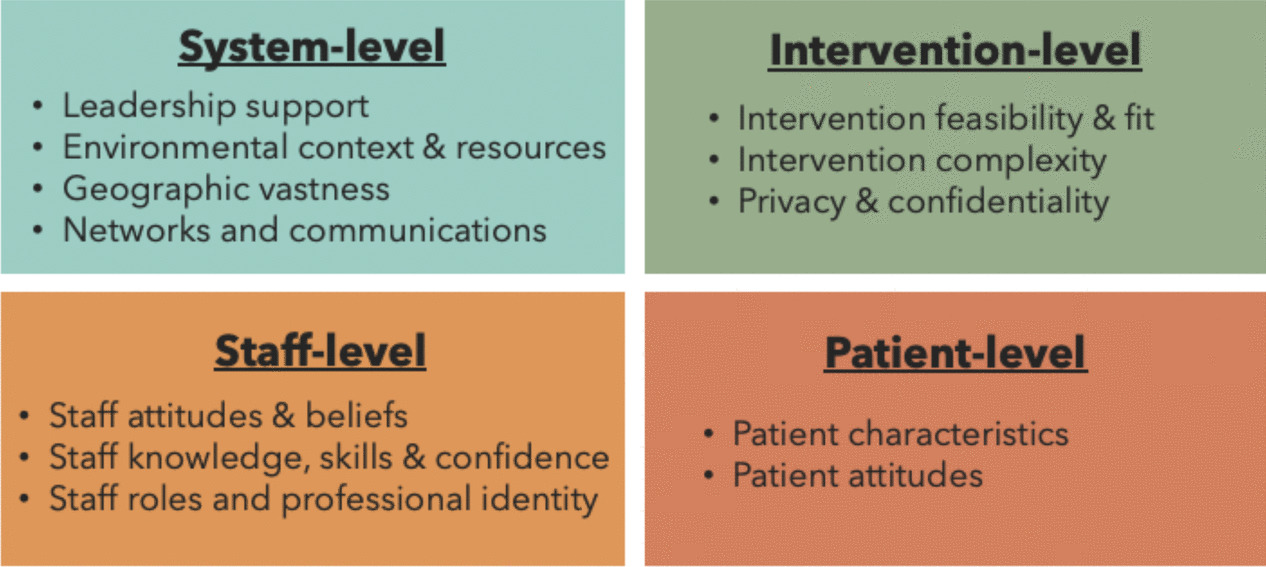
Visual depiction of themes
Intervention-level
Intervention feasibility and fit
One major barrier related to the implementation of healthcare interventions in regional and rural areas was a lack of intervention feasibility. Some interventions did not align with existing workflows, systems and resources, which limited their practical implementation [29, 31]. In particular, integrating digital interventions (e.g., telehealth/those involving electronic medical records (EMR)) within organizational/systems processes posed a challenge for regional and rural healthcare professionals, as it required software compatibility across different organizations, healthcare settings and platforms [30, 49, 60]. Another perceived challenge was a lack of fit or need for a given intervention. In some instances, interventions were seen as unnecessary, incompatible or irrelevant to the needs of regional or rural healthcare providers, patients, or settings [31, 37, 58, 62]. Additionally, some healthcare professionals described having limited opportunities to implement certain interventions due to a lack of presenting patients in regional and rural areas [35, 42, 46]. While this was perceived to impact intervention feasibility and utility [35], some perceived the lack of experience with an intervention and/or specific patient population to affect staff confidence and competence [42, 46].
Conversely, the adaptability of interventions, such as cancer screening programs, that were tailored to the unique context of rural primary care practices, was determined to be a key factor that enhanced adoption [51]. Example adaptations included changing EMR functions and nurse workflows [51]. Additionally, interventions that had a high perceived need among stakeholders [49, 58], and were easily integrated into existing systems/processes [27, 58] were believed to facilitate implementation. Other enabling strategies included raising awareness and need for an intervention at a community level, including other health services and organisations [26].
Intervention complexity
Complexity of interventions also posed substantial challenges to their implementation in regional and rural areas. Interventions considered overly cumbersome or detailed were perceived to negatively impact the motivation of healthcare professionals [58]. Even when interventions were considered useful, their complexity was viewed as making implementation a lengthy and challenging process [58]. Rural healthcare professionals also cited the length of guidelines/recommendations as a barrier [29]. To alleviate these problems, several facilitator strategies were suggested, including the development of clear guidelines and providing healthcare professionals with summaries (or laminated copies) of clinical recommendations/checklists [29].
Confidentiality and privacy
Staff concerns related to the confidentiality and privacy of patients were noted as a barrier to the implementation of some healthcare interventions. This was particularly evident for interventions focused on potentially stigmatizing issues, such as mental health treatment [28] or substance use screening and/or treatment [27, 43, 57], including those that involved the sharing or storage of personal information via digital platforms [27, 30, 57]. Specifically, some staff held reservations about whether patients in rural areas would be willing to engage with an intervention due to a potential risk to their privacy [57].
Staff-level
Staff attitudes and beliefs
Several studies identified staff attitudes and beliefs as crucial factors affecting the implementation process. When healthcare professionals held positive attitudes and perceived the intervention as valuable, they were more likely to engage with and support its adoption and implementation [31, 63]. While a willing and engaged healthcare workforce was highlighted as an enabler, the lack of such a workforce was posed as a barrier [58]. Challenges in engaging staff to modify professional behaviors and adhere to intervention processes were most apparent for studies focused on the management of patients with substance use disorders in rural areas [53, 56, 62]. Additionally, staff in some studies reported that healthcare professionals held negative beliefs about the potential increase in numbers of challenging patients (e.g., people who use illicit drugs) presenting to their rural health service, which diminished healthcare professionals’ motivation to adopt the intervention [25, 56]. Conversely, personal experience was observed to be an internal motivator for some rural clinicians, leading them to support and even champion an intervention [56]. Several studies also highlighted that the identification and formal appointment of champions facilitated implementation and motivated healthcare professionals to engage with the process through positive role modelling [31, 49, 51, 53].
Staff knowledge, skills, and confidence
Lack of confidence among healthcare professionals emerged as a significant barrier to the implementation process, with confidence closely tied to knowledge and skill levels. Staff who reported lower knowledge and/or skills related to the intervention often felt less prepared and capable of effectively implementing interventions, which led to a reluctance to adopt new practices [39, 46]. This lack of confidence typically stemmed from limited familiarity with the intervention or inadequate training on the intervention itself and its integration into existing organizational processes [31, 33, 48]. Addressing these barriers through enhanced training and upskilling of health professionals was frequently cited as key for optimizing implementation [27, 31, 34, 35, 42, 48, 49, 57]. Participants from rural sites, who commonly reported facing workforce recruitment and retention challenges, highlighted the need for educational opportunities to be offered at orientation and repeated at intervals to ensure that new staff, including locums, are adequately informed about intervention processes [37, 46]. Supplementing training with easily accessible resources, such as manuals and checklists (digital/physical), was also suggested to facilitate improved staff knowledge and skills [31]. Additionally, providing culturally appropriate training and employing an Aboriginal Health Liaison Officer were emphasized to support staff knowledge for healthcare interventions targeting patients of Aboriginal and Torres Strait Islander descent [42, 61].
Staff roles and professional identity
In regional and rural settings, staff roles and professional identity influenced the implementation of healthcare interventions. Reluctance emerged when staff viewed new intervention processes as outside their primary roles or were uncertain about shifting responsibilities [57, 58]. The introduction of new roles sometimes led to staff feeling undermined, especially when role changes, and the need for them, were poorly communicated [34]. Acceptance and integration of new roles were particularly compromised if staff felt there was potential to deskill a certain profession [34, 52] (e.g., potential deskilling of rural aged care nurses with the introduction of a specialist nurse practitioner role) [34]. Conversely, a well-defined framework for staff to understand role responsibilities and clear communication channels were perceived to enhance motivation and willingness to implement [45].
Patient-level
Patient characteristics
Healthcare staff reported a range of sociodemographic characteristics to profoundly influence patients' access and interaction with healthcare interventions in regional and rural areas, which hindered the implementation ability of staff due to fewer opportunities or resources to provide effective care. In the rural context, economic constraints, including lower income levels, lack of health insurance, and increased travel costs due to geographic remoteness and limited availability of local healthcare providers, were perceived to hinder engagement with follow-up care and referral to specialist services [35, 56]. Long work hours and shift work were also highlighted as prevalent in rural communities, which limited patients' availability to attend appointments, particularly in primary care [54]. Technology-related barriers, such as inadequate telehealth infrastructure within patient homes and varying levels of technological proficiency (noted as particularly challenging among older people or those with lower educational attainment) [30] were seen to impede the effective implementation of digital health interventions [28]. To overcome barriers related to patient characteristics, the implementation of targeted strategies was recommended, including tailored patient education and support [30] and practical elements such as the provision of data SIM cards for telehealth [28].
Patient attitudes
Staff perceived that patient attitudes played a significant role in patients’ engagement with healthcare interventions, with a lack of engagement impacting staff opportunities to implement. One study found that rural patients' reluctance to seek healthcare was due to a cultural mindset of only addressing health issues if severe [44]. Additionally, challenges were noted in motivating patients to adopt healthier lifestyles, specifically in relation to the management of childhood obesity [35]. The reluctance of older adults to address mental health issues also emerged as a barrier, largely driven by fear of stigma in rural communities and the belief that others were more deserving of services [50]. Conversely, staff recognized that positive patient receptivity played a crucial role in facilitating the implementation of healthcare interventions. When patients engaged with and demonstrated understanding and appreciation for an intervention, it motivated health professionals to persist with their implementation efforts [53]. Furthermore, patient education and clear information materials [29], and strong patient/provider relationships [45], were seen as key factors in fostering positive patient attitudes and improving engagement with healthcare interventions in rural and regional areas.
System-level
Leadership support
Leadership support and buy-in were commonly cited as key to driving the successful implementation and sustainability of healthcare interventions in regional and rural areas. Engaged leaders were seen as essential for ensuring adequate resourcing, clearly communicating the importance of an intervention, and fostering staff buy-in [49, 53]. Leaders were also perceived to be pivotal in supporting staff attendance at meetings and education sessions [46], addressing implementation resistance within organisations [28], and securing the appropriate skill mix of personnel required for successful intervention delivery [42]. Maintaining consistent leadership across a region was also considered crucial for ensuring sustained implementation [49]. The absence of engaged leaders and internal support was also noted as a barrier in some studies [37, 42, 56, 58]. In one study, health professionals suggested this issue was more pronounced in rural hospitals, where a small number of key individuals can impact the broader staff group [56].
Environmental resources and context
Several barriers related to environmental resources and context were emphasized by staff in regional and rural areas. For example, budget constraints and insufficient funding for staff and services notably hindered implementation efforts [34, 38, 62, 63]. Additional challenges were highlighted concerning the reimbursement of healthcare professionals for the delivery of specific services, such as childhood obesity management [35]. High staff turnover rates and shortages in regional and rural areas were commonly perceived to exacerbate heavy workloads, time pressures, and competing priorities [33, 39, 49, 52, 53]. These factors made it challenging for staff to attend educational opportunities [46] and balance routine clinical duties with the added demands of implementing new interventions and processes [63]. In one study, researchers observed that the formal designation of a person to support staff with implementation effectively mitigated workload issues [49]. Telehealth was additionally proposed to alleviate the time pressures experienced by staff in regional and rural areas by reducing the need for travel [30].
Challenges were also noted in relation to physical and technological infrastructure. Staff reported difficulties obtaining adequate physical space [30, 63] and, in some cases, highlighted the absence of specialized care units in rural areas, such as acute stroke units [33], which hindered alignment with guidelines. Inadequate technological infrastructure, including a lack of high-speed internet, suitable hardware, and compatible software, particularly impacted the implementation of telehealth interventions [28, 30, 59]. However, investment in robust, effective, and user-friendly digital platforms was recognized to enhance the adoption of telehealth interventions [28].
Geographic vastness
The implementation of healthcare interventions across geographically vast areas posed notable challenges. Infrequent healthcare visits, combined with sporadic communication between patients and clinicians, as well as clinicians themselves, were cited as barriers to consistent implementation [37]. These issues were particularly highlighted by staff in rural areas, where transportation barriers and distance to local services impacted patient access and clinician adherence to guidelines [41, 54]. Furthermore, the lack of local resources and specialist services often required patients to travel long distances to urban centers for necessary care, which staff described as especially burdensome for frail older individuals without access to personal or public transportation [50].
Despite these challenges, several facilitators emerged. The use of telehealth [30] and long-standing positive patient-provider relationships [45, 47] were perceived to improve communication, coordination, and continuity of care. The sense of community in rural areas was also considered crucial, as familiarity between clinicians and patients fostered rapport and strengthened staff commitment to their communities [38, 45]. Additionally, staff noted that regional and rural services often had the flexibility to adopt new programs and practices, leading to innovative solutions tailored to their unique contexts [42, 54].
Networks and communication
Staff identified external communication and collaboration between services and staff as a challenge to the implementation of healthcare interventions in regional and rural areas [58, 62]. Additionally, the absence of academic affiliations was noted in one study to affect a rural hospital’s ability to access new knowledge, resources, and recruit clinicians [37]. In contrast, respected and well-connected implementers within organizations were seen as instrumental in driving implementation efforts by leveraging their social networks to identify and secure resources [37]. Informal networking in smaller communities also played a crucial role in information sharing, referrals and identifying service gaps; however, reliance on informal networks was noted to create difficulties for staff new to an area [38]. Lastly, staff in one study reported that joining a collaborative network of healthcare providers (e.g., an Accountable Care Organization) facilitated benchmarking between organizations that drove performance improvements through data comparisons [51].
Discussion
This rapid review uniquely identified barriers and facilitators to the implementation of healthcare interventions in regional and rural healthcare services, as reported by healthcare staff working in high-income countries. The findings reveal a complex interplay of factors across four overarching themes: intervention-level, staff-level, patient-level, and system-level. While many identified barriers and facilitators align with those reported in other healthcare contexts [11, 12], this review highlights that some factors are amplified in regional and rural areas. Importantly, the review findings also emphasize that regional and rural healthcare services possess distinct strengths that can be leveraged to support the effective implementation of healthcare interventions.
Workforce shortages were found to be a critical system-level barrier and were perceived to significantly impact the implementation of healthcare interventions in regional and rural settings. Difficulties in recruiting and retaining healthcare professionals, alongside the lack of specialist services, were perceived to exacerbate workload pressures and time constraints for staff. This aligns with global concerns about the maldistribution of healthcare workers in rural areas, as highlighted by the World Health Organization (WHO) [65], where healthcare professionals are often required to cover a wide range of roles with insufficient support or resources. A shortage of specialists, such as mental healthcare providers, limits the availability of specialist care in regional and rural areas, placing an additional burden on generalists [66]. Programs like the Australian Government's Rural Health Multidisciplinary Training Program [67]. which offers healthcare students the opportunity to train in rural and remote communities, are valuable initiatives aimed at addressing these workforce gaps. This review underscores the ongoing imperative to sustain such programs to bridge the workforce divide (refer to Table 3 for summary of discussion key messages and potential actions).
Table 3.
Discussion key messages and potential actions
| Key Messages | Supporting Findings | Potential Actions |
|---|---|---|
| Workforce shortages and retention issues hinder implementation and sustainability | - Regional and rural healthcare providers face high workloads, limited specialist support, and high attrition, making implementation challenging |
- Invest in rural workforce training and retention programs - Support multidisciplinary team models to optimize workforce distribution - Explore financial incentives for rural healthcare staff |
| Intervention feasibility and fit are essential for implementation success | - Rigid interventions that do not align with local workflows and resources hinder implementation |
- Conduct pre-implementation needs assessments to tailor interventions to regional and rural settings - Engage healthcare leaders, frontline staff and local communities in the co-design and adaptation of interventions |
| Strong leadership and organizational support drive implementation | - Leadership buy-in facilitates staff engagement and access to resources |
- Develop leadership training programs for regional and rural healthcare managers - Foster organizational buy-in through transparent communication - Designate implementation champions to drive change within regional and rural healthcare organizations |
| Digital health interventions show promise but require long-term investment | - Telehealth has the potential to improve implementation and alleviate access issues associated with geographic vastness but is limited by infrastructure gaps, digital literacy, and confidentiality concerns |
- Invest in rural broadband and digital health infrastructure - Provide digital literacy training for healthcare providers and patients - Address privacy and confidentiality concerns through secure platforms |
| Regional and rural healthcare settings have strengths that should be leveraged to support implementation | - Strong community links, flexible healthcare services that can adapt to local needs, long-term patient-provider relationships, and informal peer networks all facilitate implementation |
- Engage trusted local leaders in healthcare initiatives to foster long-term community buy-in - Foster regional collaboration networks to share resources and knowledge, building on existing community ties |
| Implementation science frameworks and geographic classification systems are underutilized | - Most studies did not use structured implementation frameworks to assess barriers and facilitators or use standardized geographic classification systems to define their context |
- Build capacity of the rural health workforce relating to implementation science - Encourage the use of geographical classification reporting (e.g., Modified Monash Model, Rural–Urban Continuum Codes) |
| Limited focus on priority populations | - Few studies targeted priority populations, such as Indigenous or culturally diverse groups |
- Engage priority populations in research through participatory methodologies - Apply equity-focused frameworks (e.g., Health Equity Implementation Framework) |
While a patient-level theme emerged in the synthesis, these findings reflect staff-reported perceptions rather than direct patient input. Many of the identified patient-level barriers, such as attitudes toward healthcare and economic constraints, stem from broader systemic inequities rather than individual choices [68]. Factors such as lower income levels, lack of health insurance, and high travel costs for medical care disproportionately impact rural populations and limit healthcare access. Addressing these challenges requires policy and structural reforms to improve healthcare access and equity in rural settings.
Digital health interventions, particularly telehealth, were identified as potential solutions to address some of the barriers associated with environmental resources and context and geographic vastness. Telehealth reduces the need for patients and healthcare providers to travel long distances, which is particularly valuable in rural areas [69]. However, this review also identified several barriers to the effective implementation of telehealth in regional and rural settings, including inadequate digital infrastructure, limited digital literacy among healthcare staff and patients, and concerns over confidentiality and privacy. These barriers reflect findings from other studies [70, 71]. While telehealth holds promise for improving access to care, its success depends on significant investment in digital infrastructure, workforce training, and equitable access to technology, as emphasized in WHOs Global Strategy on Digital Health 2020–2025 [72]. The strategy highlights the need for robust digital health systems, increased digital literacy for healthcare providers and patients, and efforts to bridge the digital divide to ensure that telehealth benefits are accessible to all populations, particularly in low-resource settings.
At the intervention level, this review emphasizes the importance of ensuring that healthcare interventions are feasible and fit with the local context. Interventions perceived as overly complex or incompatible with existing workflows and resources were seen to have limited implementation capacity. Implementation science frameworks, such as the Implementation in Context (ICON) Framework [73] and the CFIR [64], provide guidance to implementers on the elements of context that should be considered when planning for successful implementation. Additional guidance further emphasizes the importance for interventions to be tailored to local contexts, rather than attempting to directly translate interventions developed for other settings [74]. In regional and rural settings, this may involve simplifying processes and ensuring interventions are aligned with available resources, infrastructure and staff capabilities. The adaptation of interventions and the pursuit of equity-centered implementation hinge on the authentic and meaningful participation of the community. Engaging local stakeholders, such as healthcare professionals and patients, in the co-design and adaptation of healthcare interventions is an important step that may enhance intervention relevance and acceptance, improving implementation, adoption and overall effectiveness [75]. Adaptation guidance provides structured approaches for adapting interventions to new contexts [76, 77], while practical tools like the Hexagon tool [78], and the APEASE criteria [79] can help to evaluate an intervention’s fit with the local context.
This review also highlights several strengths of regional and rural healthcare settings, that if effectively leveraged, may offset some of the identified barriers, contributing to more effective implementation of healthcare interventions. For instance, strong community relationships and flexible healthcare services that can adapt to local needs were identified as valuable assets in regional and rural areas. Long-term relationships between healthcare providers and patients in these communities can also serve as a driver to enhance patient trust and engagement with new interventions. Additionally, leadership support was seen as key to the implementation of healthcare interventions. Regional and rural healthcare services should focus on fostering strong leadership and building internal capacity to drive implementation efforts and ensure that healthcare staff are adequately supported throughout the implementation process [80].
A notable strength of this review is the comprehensive search and selection process that yielded a sizeable number of included studies published since 2000. Furthermore, data synthesis and interpretation were strengthened by an author team highly engaged in rural health research, many of whom are clinicians embedded within regional and rural healthcare services. The diversity of healthcare interventions can be seen as both a strength and a limitation of this review. While the consistency of common implementation barriers and facilitators suggests broad relevance to regional and rural healthcare settings, this diversity also limited the depth of understanding for each specific intervention type. Additionally, gaps in the available literature may limit the generalizability of the findings to certain healthcare settings or interventions not addressed in the included studies. For example, few studies were conducted outside of Australia or the USA, and aged care and community health settings were underrepresented, limiting insights into implementation factors in these contexts. Furthermore, research focusing on priority populations, such as culturally and linguistically diverse or Indigenous groups was limited. Future research should prioritise an equity-focused approach to better understand and address the unique factors influencing implementation in these populations. This may involve the use of participatory methodologies that actively engage communities, while ensuring research upholds principles of self-determination [81]. Applying equity-focused implementation frameworks, such as the Health Equity Implementation Framework [82], may also enhance the cultural responsiveness and effectiveness of healthcare interventions.
While the omission of a formal critical appraisal step is common and accepted in rapid reviews, it introduces some potential for bias, particularly regarding the strength and reliability of reported barriers and facilitators. However, the consistency of themes across studies and their alignment with existing literature [11, 12] suggest that the key findings remain robust. Future research incorporating formal risk-of-bias assessments could further enhance the reliability of synthesized evidence.
Another important finding from this review is the limited application of implementation theories, models, and frameworks in rural healthcare research. The majority of studies did not report using structured frameworks, such as the CFIR [64] or the Theoretical Domains Framework [83], to guide their assessment of barriers and facilitators. This gap highlights the need for further research to understand the feasibility, relevance, and potential impact of applying these frameworks to the implementation of healthcare interventions in non-urban settings. Future studies should also consistently apply geographical classification systems to define rurality, e.g., MMM [22] or RUCC [21]. The lack of consistent use of these classifications in the studies included in this review made it difficult to compare findings across different contexts.
Lastly, although healthcare settings differ significantly between high- and low-income countries, many of the barriers and facilitators identified in this review, such as lack of intervention fit and the importance of stakeholder engagement, have also been observed in low-income healthcare contexts [84]. Future research should explore the relevance of these factors in rural low-income healthcare settings to better understand their impact on healthcare implementation.
Conclusion
This review provides valuable insights into the barriers and facilitators associated with implementing healthcare interventions in regional and rural settings, as perceived by healthcare staff in high-income countries. Addressing the challenges faced in these contexts while leveraging their inherent strengths has the potential to significantly enhance implementation outcomes and contribute to reducing the health disparity gap between rural and metropolitan populations. Policymakers, healthcare leaders, and researchers tasked with designing and implementing healthcare interventions in regional and rural areas should systematically consider barriers and facilitators across the four overarching themes: intervention-, staff-, patient-, and system-level. Conducting context-specific assessments that utilize established implementation frameworks will enable stakeholders to design tailored implementation strategies that have the capacity to effectively support healthcare staff and optimize service delivery.
Supplementary Information
Acknowledgements
The authors wish to acknowledge Sharina Riva for their assistance in preparing the tables for the manuscript.
Abbreviations
- EBI
Evidence-based intervention
- PRISMA
Preferred Reporting Items for Systematic reviews and Meta-Analysis
- RUCC
Rural-Urban Continuum Codes
- MMM
Modified Monash Model
- USA
United States of America
- CFIR
Consolidated Framework for Implementation Research
- EMR
Electronic Medical Records
- WHO
World Health Organization
- ICON
Implementation in Context
Authors’ contributions
AC and AU conceptualized the study. AC and DM developed the review protocol, which was refined with input from all authors. DM conducted the database searches, and AB, DM, AC, and AU screened the records. Data extraction was led by AC and DM, with contributions from AB, AU, LA, AWS, and KH. Analysis was led by AC and AB, with interpretation supported by all authors. AC drafted the manuscript, with assistance from DM. All authors critically revised the manuscript and have read and approved the final version.
Funding
This study was conducted as part of the DELIVER research program that is supported by an Australian Commonwealth funded MRFF Rapid Applied Research Translation Grant (RARUR000072). AU is supported by a Victorian Cancer Agency fellowship. AP is supported through an NHMRC Investigator Grant. SY is supported by a Heart Foundation Future Leader Fellowship (ref no:106654). LA and AWS are supported by the Rural Health Multidisciplinary Training Program (RHMT) from the Australian Federal Government’s Department of Health and Aged Care.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests. HB is an editorial board member of BMC Health Services Research but was not involved in the peer review or decision-making process for this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.International Labour Office. Global evidence on inequities in rural health protection: new data on rural deficits in health coverage for 174 countries. Geneva: ILO, Social Protection Department; 2015. [Google Scholar]
- 2.Beks H, Walsh S, Alston L, et al. Approaches Used to Describe, Measure, and Analyze Place of Practice in Dentistry, Medical, Nursing, and Allied Health Rural Graduate Workforce Research in Australia: A Systematic Scoping Review. Int J Environ Res Public Health. 2022;19(3):1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Australian Institute of Health and Welfare. Rural and remote health [Internet]. 2024. https://www.aihw.gov.au/reports/rural-remote-australians/rural-and-remote-health. Accessed 31 July 2024.
- 4.Cross SH, Califf RM, Warraich HJ. Rural-Urban Disparity in Mortality in the US From 1999 to 2019. JAMA. 2021;325(22):2312–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Reid S. The rural determinants of health: using critical realism as a theoretical framework. Rural Remote Health. 2019;19(3):5184. [DOI] [PubMed] [Google Scholar]
- 6.Shelton RC, Brownson RC. Enhancing Impact: A Call to Action for Equitable Implementation Science. Prev Sci. 2024;25(1):174–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pinnock H, Barwick M, Carpenter CR, et al. Standards for Reporting Implementation Studies (StaRI): explanation and elaboration document. BMJ Open. 2017;7(4):e013318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shelton RC, Adsul P, Emmons KM, Linnan LA, Allen JD, Chambers D. Fidelity and Its Relationship to Effectiveness, Adaptation, and Implementation. In: Brownson RC, Colditz GA, Proctor EK, eds. Dissemination and Implementation Research in Health: Translating Science to Practice, 3rd edn. Oxford University Press; 2023. p. 147–171. 10.1093/oso/9780197660690.003.0007
- 9.Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: the 60–30–10 Challenge. BMC Med. 2020;18(1):102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolfenden L, Foy R, Presseau J, et al. Designing and undertaking randomised implementation trials: guide for researchers. BMJ. 2021;372:m3721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Geerligs L, Rankin NM, Shepherd HL, Butow P. Hospital-based interventions: a systematic review of staff-reported barriers and facilitators to implementation processes. Implement Sci. 2018;13(1):36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Correa VC, Lugo-Agudelo LH, Aguirre-Acevedo DC, et al. Individual, health system, and contextual barriers and facilitators for the implementation of clinical practice guidelines: a systematic metareview. Health Res Policy Syst. 2020;18(1):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Webb R, Uddin N, Ford E, et al. Barriers and facilitators to implementing perinatal mental health care in health and social care settings: a systematic review. Lancet Psychiatry. 2021;8(6):521–34. [DOI] [PubMed] [Google Scholar]
- 14.Mullan L, Armstrong K, Job J. Barriers and enablers to structured care delivery in Australian rural primary care. Aust J Rural Health. 2023;31(3):361–84. [DOI] [PubMed] [Google Scholar]
- 15.Pantoja T, Opiyo N, Lewin S, et al. Implementation strategies for health systems in low-income countries: an overview of systematic reviews. Cochrane Database Syst Rev. 2017;9(9):Cd011086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garritty C, Gartlehner G, Nussbaumer-Streit B, et al. Cochrane Rapid Reviews Methods Group offers evidence-informed guidance to conduct rapid reviews. J Clin Epidemiol. 2021;130:13–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stevens A, Hersi M, Garritty C, et al. Rapid review method series: interim guidance for the reporting of rapid reviews. BMJ Evid-Based Med. 2024. 10.1136/bmjebm-2024-112899. [DOI] [PMC free article] [PubMed]
- 19.Eccles MP, Mittman BS. Welcome to Implementation Science. Implement Sci. 2006;1(1):1. [Google Scholar]
- 20.Bach-Mortensen AM, Lange BCL, Montgomery P. Barriers and facilitators to implementing evidence-based interventions among third sector organisations: a systematic review. Implement Sci. 2018;13(1):103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.United States Department of Agriculture. Rural-Urban Continuum Codes [Internet]. Updated 22 January 2024. https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Accessed 23 Jan 2024.
- 22.Australian Government Department of Health and Aged Care. Modified Monash Model [Internet]. Updated 12 December 2023. https://www.health.gov.au/topics/rural-health-workforce/classifications/mmm. Accessed 23 Jan 2024.
- 23.The World Bank. World Bank Country and Lending Groups [Internet]. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed 11 Aug 2023.
- 24.Popay J, Roberts H, Sowden A, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A Prod ESRC Meth Prog Version. 2006;1(1):b92. [Google Scholar]
- 25.Andrilla CHA, Coulthard C, Larson EH. Barriers Rural Physicians Face Prescribing Buprenorphine for Opioid Use Disorder. Ann Fam Med. 2017;15(4):359–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beks H, Mitchell F, Charles JA, McNamara KP, Versace VL. An Aboriginal Community-Controlled Health Organization model of service delivery: qualitative process evaluation of the Tulku wan Wininn mobile clinic. Int J Equity Health. 2022;21(1):163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Berends L, Roberts B. Implementation Effectiveness of an Alcohol-Screening and Intervention Project at Two Hospitals in Regional Victoria. Australia Contemporary Drug Problems. 2012;39(2):289–309. [Google Scholar]
- 28.Chatterton ML, Marangu E, Clancy EM, et al. Telehealth service delivery in an Australian regional mental health service during COVID-19: a mixed methods analysis. Int J Ment Health Syst. 2022;16(1):43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Daugherty J, Waltzman D, Popat S, Groenendaal AH, Cherney M, Knudson A. Rural Primary Care Providers’ Experience and Usage of Clinical Recommendations in the CDC Pediatric Mild Traumatic Brain Injury Guideline: A Qualitative Study. J Rural Health. 2021;37(3):487–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.DeHart D, King LB, Iachini AL, Browne T, Reitmeier M. Benefits and Challenges of Implementing Telehealth in Rural Settings: A Mixed-Methods Study of Behavioral Medicine Providers. Health Soc Work. 2021;47(1):7–18. [DOI] [PubMed] [Google Scholar]
- 31.Delaforce A, Li J, Grujovski M, et al. Creating an Implementation Enhancement Plan for a Digital Patient Fall Prevention Platform Using the CFIR-ERIC Approach: A Qualitative Study. Int J Environ Res Public Health. 2023;20(5):3794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Druskin LR, Han RC, Phillips ST, et al. The Dissemination of Parent-Child Interaction Therapy in West Virginia during the Opioid Epidemic and COVID-19 Pandemic: A Qualitative Study. Int J Environ Res Public Health. 2022;19(22):15085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dwyer M, Peterson GM, Gall S, Francis K, Ford KM. Health care providers’ perceptions of factors that influence the provision of acute stroke care in urban and rural settings: A qualitative study. SAGE Open Med. 2020;8:2050312120921088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ervin K, Reid C, Moran A, Opie C, Haines H. Implementation of an older person’s nurse practitioner in rural aged care in Victoria, Australia: a qualitative study. Hum Resour Health. 2019;17(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Findholt NE, Davis MM, Michael YL. Perceived Barriers, Resources, and Training Needs of Rural Primary Care Providers Relevant to the Management of Childhood Obesity. J Rural Health. 2013;29(s1):s17–24. [DOI] [PubMed] [Google Scholar]
- 36.Fletcher S, Sinclair C, Rhee J, Goh D, Auret K. Rural health professionals’ experiences in implementing advance care planning: a focus group study. Aust J Prim Health. 2016;22(5):423–7. [DOI] [PubMed] [Google Scholar]
- 37.Harrod M, Manojlovich M, Kowalski CP, Saint S, Krein SL. Unique factors rural Veterans’ Affairs hospitals face when implementing health care-associated infection prevention initiatives. J Rural Health Winter. 2014;30(1):17–26. [DOI] [PubMed] [Google Scholar]
- 38.Henderson J, Dawson S, Fuller J, et al. Regional responses to the challenge of delivering integrated care to older people with mental health problems in rural Australia. Aging Ment Health. 2018;22(8):1025–31. [DOI] [PubMed] [Google Scholar]
- 39.Hill C, Clapham RP, Buccheri A, Field M, Wong Shee A, Alston L. Assessing adherence and exploring barriers to provision of prescribed texture modifications for dysphagia in a residential aged care facility in rural Australia. Int J Speech Lang Pathol. 2022;24(1):67–76. [DOI] [PubMed] [Google Scholar]
- 40.Howland M, Tennant M, Bowen DJ, et al. Psychiatrist and Psychologist Experiences with Telehealth and Remote Collaborative Care in Primary Care: A Qualitative Study. J Rural Health. 2021;37(4):780–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Khoong EC, Gibbert WS, Garbutt JM, Sumner W, Brownson RC. Rural, suburban, and urban differences in factors that impact physician adherence to clinical preventive service guidelines. J Rural Health Winter. 2014;30(1):7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kilcullen M, Ireland S. Palliative care in the neonatal unit: neonatal nursing staff perceptions of facilitators and barriers in a regional tertiary nursery. BMC Palliat Care. 2017;16(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kristman-Valente AN, McCarty CA, Walker DD, Walker-Harding L. Barriers to Implementing a Cannabis Focused SBIRT in Adolescent Primary Care. Subst Abuse. 2022;16:11782218221111836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kruse-Diehr AJ, Dignan M, Cromo M, et al. Building Cancer Prevention and Control Research Capacity in Rural Appalachian Kentucky Primary Care Clinics During COVID-19: Development and Adaptation of a Multilevel Colorectal Cancer Screening Project. J Cancer Educ. 2022;37(5):1407–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lam L, Ansari AS, Baquir PJ, Chowdhury N, Tran K, Bailey J. Current practices, barriers and enablers for advance care planning among healthcare workers of aged care facilities in western New South Wales, Australia. Rural Remote Health. 2018;18(4):4714. [DOI] [PubMed] [Google Scholar]
- 46.Lillebuen L, Schick-Makaroff K, Thompson S, Molzahn A. Facilitators and Barriers to Care in Rural Emergency Departments in Alberta for Patients on Peritoneal Dialysis (PD): An Interpretive Descriptive Study. Can J Kidney Health Dis. 2020;7:2054358120970098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Littlewood J, Hinchcliff R, Lo W, Rhee J. Advance care planning in rural New South Wales from the perspective of general practice registrars and recently fellowed general practitioners. Aust J Rural Health. 2019;27(5):398–404. [DOI] [PubMed] [Google Scholar]
- 48.Maxwell H, Bramble M, Prior SJ, et al. Staff experiences of a reablement approach to care for older people in a regional Australian community: A qualitative study. Health Soc Care Community. 2021;29(3):685–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morgan D, Kosteniuk J, O’Connell ME, et al. Barriers and facilitators to development and implementation of a rural primary health care intervention for dementia: a process evaluation. BMC Health Serv Res. 2019;19(1):709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Muir-Cochrane E, O’Kane D, Barkway P, Oster C, Fuller J. Service provision for older people with mental health problems in a rural area of Australia. Aging Ment Health. 2014;18(6):759–66. [DOI] [PubMed] [Google Scholar]
- 51.Nelson-Brantley H, Ellerbeck EF, McCrea-Robertson S, et al. Implementation of cancer screening in rural primary care practices after joining an accountable care organisation: a multiple case study. Fam Med Community Health. 2021;9(4):e001326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paliadelis P, Cruickshank M, Wainohu D, Winskill R, Stevens H. Implementing family-centred care: an exploration of the beliefs and practices of paediatric nurses. Aust J Adv Nurs. 2005;23(1):31–6. [PubMed] [Google Scholar]
- 53.Parchman ML, Ike B, Osterhage KP, Baldwin LM, Stephens KA, Sutton S. Barriers and facilitators to implementing changes in opioid prescribing in rural primary care clinics. J Clin Transl Sci. 2020;4(5):425–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Porter GC, Schwab R, Hill JL, et al. Examining the feasibility and characteristics of realistic weight management support for patients: Focus groups with rural, micropolitan, and metropolitan primary care providers. Prev Med Rep. 2021;23:101390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Rosado JI, Reyes E, Montgomery J, Wang Y, Malloy C, Simpson-O’Reggio AM. From planning to implementation: Developing an ACE screening protocol in a rural integrated primary care clinic serving Latino children. Clin Pract Pediatr Psychol. 2024;12(1):36–47. [Google Scholar]
- 56.Rosenberg NK, Hill AB, Johnsky L, Wiegn D, Merchant RC. Barriers and facilitators associated with establishment of emergency department-initiated buprenorphine for opioid use disorder in rural Maine. J Rural Health. 2022;38(3):612–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Saunders EC, Moore SK, Gardner T, et al. Screening for Substance Use in Rural Primary Care: a Qualitative Study of Providers and Patients. J Gen Intern Med. 2019;34(12):2824–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Seidel K, Quasdorf T, Haberstroh J, Thyrian JR. Adapting a Dementia Care Management Intervention for Regional Implementation: A Theory-Based Participatory Barrier Analysis. Int J Environ Res Public Health. 2022;19(9):5478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Shreck E, Nehrig N, Schneider JA, et al. Barriers and facilitators to implementing a U.S. Department of Veterans Affairs Telemental Health (TMH) program for rural veterans. J Rural Mental Health. 2020;44(1):1–15. [Google Scholar]
- 60.Shulver W, Killington M, Crotty M. “Massive potential” or “safety risk”? Health worker views on telehealth in the care of older people and implications for successful normalization. BMC Med Inform Decis Mak. 2016;16(1):131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Stanford J, Charlton K, McMahon A-T, Winch S. Better cardiac care: health professional’s perspectives of the barriers and enablers of health communication and education with patients of Aboriginal and Torres Strait Islander descent. BMC Health Serv Res. 2019;19(1):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Watson DP, Staton MD, Gastala N. Identifying unique barriers to implementing rural emergency department-based peer services for opioid use disorder through qualitative comparison with urban sites. Addict Sci Clin Pract. 2022;17(1):41. 10.1186/s13722-022-00324-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wilkinson SA, O’Brien M, McCray S, Harvey D. Implementing a best-practice model of gestational diabetes mellitus care in dietetics: a qualitative study. BMC Health Serv Res. 2019;19(1):122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Damschroder LJ, Reardon CM, Widerquist MAO, Lowery J. The updated Consolidated Framework for Implementation Research based on user feedback. Implement Sci. 2022;17(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.World Health Organization. Retention of the health workforce in rural and remote areas: a systematic review. Human Resources for Health Observer Series. Vol 25. Geneva: World Health Organization; 2020.
- 66.Cyr ME, Etchin AG, Guthrie BJ, Benneyan JC. Access to specialty healthcare in urban versus rural US populations: a systematic literature review. BMC Health Serv Res. 2019;19(1):974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Stewart R, McMillan AMF. Australia’s Rural Health Multidisciplinary Training program: Preparing for the rural health workforce that Australia needs. Aust J Rural Health. 2021;29(5):617–9. [DOI] [PubMed] [Google Scholar]
- 68.Placzek H, Cruz S, Chapdelaine M, Carl M, Levin S, Hsu C. Intersecting systemic and personal barriers to accessing social services: qualitative interviews in northern California. BMC Public Health. 2021;21(1):1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Butzner M, Cuffee Y. Telehealth Interventions and Outcomes Across Rural Communities in the United States: Narrative Review. J Med Internet Res. 2021;23(8):e29575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zhang T, Mosier J, Subbian V. Identifying Barriers to and Opportunities for Telehealth Implementation Amidst the COVID-19 Pandemic by Using a Human Factors Approach: A Leap Into the Future of Health Care Delivery? JMIR Hum Factors. 2021;8(2):e24860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kruse CS, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare. 2018;24(1):4–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.World Health Organization. Global strategy on digital health 2020–2025. Geneva: World Health Organization; 2021. [Google Scholar]
- 73.Squires JE, Graham ID, Santos WJ, et al. The Implementation in Context (ICON) Framework: A meta-framework of context domains, attributes and features in healthcare. Health Research Policy Syst. 2023;21(1):81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Skivington K, Matthews L, Simpson SA, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ. 2021;374:n2061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vargas C, Whelan J, Brimblecombe J, Allender S. Co-creation, co-design and co-production for public health: a perspective on definitions and distinctions. Public Health Res Pract. 2022;32(2):3222211. 10.17061/phrp3222211. [DOI] [PubMed] [Google Scholar]
- 76.Moore G, Campbell M, Copeland L, et al. Adapting interventions to new contexts—the ADAPT guidance. BMJ. 2021;374:n1679. 10.1136/bmj.n1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Escoffery C, Lebow-Skelley E, Udelson H, et al. A scoping study of frameworks for adapting public health evidence-based interventions. Transl Behav Med. 2019;9(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Metz A, Louison L. The Hexagon Tool: Exploring Context. Chapel Hill: National Implementation Research Network, Frank Porter Graham Child Development Institute, University of North Carolina at Chapel Hill; 2019.
- 79.Michie S, Atkins L, West R. The Behaviour Change Wheel: A Guide to Designing Interventions: Silverback Publishing; 2014.
- 80.Aarons GA, Ehrhart MG, Moullin JC, Torres EM, Green AE. Testing the leadership and organizational change for implementation (LOCI) intervention in substance abuse treatment: a cluster randomized trial study protocol. Implement Sci. 2017;12(1):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Victorian Aboriginal Community Controlled Health Organisation. marra ngarrgoo, marra goorri: the Victorian Aboriginal Health, Medical and Wellbeing Research Accord 2023.
- 82.Woodward EN, Matthieu MM, Uchendu US, Rogal S, Kirchner JE. The health equity implementation framework: proposal and preliminary study of hepatitis C virus treatment. Implement Sci. 2019;14(1):26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7(1):37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Bradley EH, Curry LA, Taylor LA, et al. A model for scale up of family health innovations in low-income and middle-income settings: a mixed methods study. BMJ Open. 2012;2(4):e000987. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.