Abstract
Objective
To evaluate the effectiveness of using dorsal toe fibula composite flaps and iliac bone in sequential transplantation for the comprehensive reconstruction of fingers with grade I to III defects.
Methods
Between December 2020 and March 2024, data were collected from 36 patients who received complete finger reconstruction for grade I to III defects using dorsal toe fibula composite flaps and iliac bone in sequential transplantation. Postoperative evaluations included Carroll’s hand function test scores, hand mobility disability assessments, and overall postoperative conditions.
Results
Postoperatively, Carroll’s hand function test scores for patients with grade III finger defects showed a significant improvement (P < 0.05), while hand mobility disability scores significantly decreased (P < 0.05). All 47 finger defects in 36 patients were successfully reconstructed with favorable survival outcomes. Among these, two patients with grade III defects experienced donor site numbness; one reported minor walking difficulties, and the other had restricted mobility. Additionally, one case of infection occurred at the recipient site in a grade I defect patient and another at the donor site in a grade II defect patient. Both infections improved with appropriate dressings and cleaning. Overall, the recipient areas healed well, with 32 patients satisfied with the appearance, 4 finding it average, resulting in an 88.89% satisfaction rate. The donor sites also healed well in 33 cases, with 3 cases showing slow healing—one with a grade II and two with grade III defects—none of which developed hypertrophic scars. Of these, 29 patients were satisfied with the appearance, 5 found it average, and 2 were dissatisfied, leading to an 80.56% satisfaction rate for the donor sites.
Conclusion
The use of dorsal toe fibula composite flaps and iliac bone in sequential transplantation proves effective for fully reconstructing fingers with grade III defects, while minimizing the impact on both the appearance and function of the donor site.
Keywords: Dorsal toe region, Composite tissue flap, Iliac bone graft, Complete finger reconstruction, Grade I–III finger defects
Introductions
Full-shape reconstruction of fingers using free toenail bone flaps is a widely accepted method for repairing finger defects. This technique is well-regarded for its high degree of compatibility with the defect tissue, which facilitates an effective restoration of both the shape and function of the recipient area [1]. However, ongoing clinical research has revealed some significant drawbacks. The removal of the toe segment and toenail from the donor site, particularly the narrow end of the great toe, can have a pronounced impact on the foot’s appearance and functionality. This procedure may result in noticeable cosmetic changes and functional impairment of the toe, which can, in turn, affect overall foot function. These drawbacks are particularly concerning for younger, active patients who rely on full foot function. In contrast, the use of a partial toenail flap preserves the integrity of the great toe while providing sufficient soft tissue coverage for finger reconstruction. Additionally, the reconstructed fingers may retain identifiable characteristics of the toe from which they were derived [2].
One limitation of partial toenail flaps is the lack of sufficient bony or skeletal support, particularly in Grade II and III finger defects. To overcome this, our approach incorporates the use of a non-vascularized iliac bone graft, which provides robust structural support, thereby restoring the phalangeal skeleton. This combined technique avoids the need to harvest large portions of the distal phalanx from the great toe, reducing donor site morbidity and preserving foot function.
Iliac bone grafts are generally employed for reconstructing fingers with grade III defects and higher in contrast. This approach offers several advantages: it typically ensures reliable graft survival, provides ample donor material, maintains stable morphology, and exerts minimal impact on the donor site. By utilizing iliac bone, the excessive cosmetic damage associated with toe segment amputation can be mitigated, leading to a more aesthetically pleasing reconstruction that better aligns with modern aesthetic standards and closely resembles a normal finger [3].
Nonetheless, research [4, 5] indicates that using iliac bone for finger reconstruction may be associated with certain complications, such as bone nonunion. This complication can impair the functionality of the reconstructed finger and potentially increase the risk of requiring additional surgeries, thus imposing a greater economic burden on patients. Furthermore, there is a paucity of clinical studies addressing the efficacy of iliac bone grafts for full reconstruction of finger defects classified as grade I to III.
To address these concerns and better understand the effectiveness of these methods, this article reviews the use of dorsal toe fibula composite flaps combined with iliac bone grafts for full-shape reconstruction of grade I to III finger defects.
Objective
The review covers data collected between December 2020 and March 2024, focusing on assessing the functionality and aesthetic outcomes of both the donor and recipient areas. This analysis aims to provide a comprehensive evaluation of the practical value and effectiveness of these reconstructive techniques.
Materials and methods
Participants and clinical data
From December 2020 to March 2024, data were collected on 36 patients who underwent full-shape reconstruction of grade I to III finger defects using a combination of dorsal toe fibula composite tissue flaps and iliac bone grafts. The cohort included 22 males and 14 females, with a total of 28 and 19 fingers, respectively. The patients ranged in age from 5 to 57 years, with an average age of 26.78 ± 5.32 years. The distribution of finger defects was as follows: 17 cases with grade I defects, 23 cases with grade II defects, and 7 cases with grade III defects.
The iliac bone graft is shaped and positioned to align with the phalangeal bone stump. The graft is secured using K-wires or titanium screws to maintain precise alignment and achieve stability and compression at the bone-to-bone interface. This promotes osteointegration and minimizes the risk of graft displacement. The partial toenail composite flap, which includes the nail bed, soft tissue, and neurovascular pedicle, is transferred to cover the exposed bone and recreate the fingertip anatomy.
To restore joint mobility, particular attention is given to preserving and reconstructing the distal interphalangeal and proximal interphalangeal joints. The articular surfaces are preserved as much as possible, and in cases where the joint is severely damaged, arthrodesis (joint fusion) is performed to restore mechanical strength. In select cases, the use of the second interphalangeal joint as a transplant option is explored.
For Grade II and III defects, distal interphalangeal and proximal interphalangeal joint mobility is prioritized. Where feasible, the joint is preserved, and the phalangeal stumps are aligned to promote joint stability. If severe joint damage is present, arthrodesis is performed, fusing the joint in a functional position. In specific cases, the use of donor interphalangeal joints from the second toe is considered.
Inclusion criteria:
Patients with traumatic finger defects classified as grade I to III, with residual healthy soft tissue coverage on the injured finger.
Patients requiring emergency reconstruction of finger defects were included, provided that the surgical team deemed the patient fit for emergency intervention.
Patients demonstrated a strong commitment to completing the finger reconstruction.
The donor sites (toe bone, soft tissue, and iliac bone) were functionally and morphologically intact and suitable for use.
The affected finger had not previously undergone repair or stump trimming surgery.
Patients were classified as having anesthesia risk ASA I-III, and emergency cases were assessed based on preoperative risk assessment.
All patients provided informed consent, and the study was reviewed and approved by our hospital's medical ethics committee.
Exclusion criteria:
Presence of congenital developmental anomalies, such as syndactyly, toe adhesions, or other congenital finger or toe defects.
Existing infections at the finger stump or systemic infections, bone fractures, or significant scarring.
Patients with conditions affecting motor and sensory functions, such as cerebral palsy, poliomyelitis, or cerebral infarction.
Serious cardiovascular or cerebrovascular diseases, severe liver or kidney dysfunction, significant endocrine or metabolic disorders, or coagulation abnormalities.
Patients who were transferred from other hospitals or had incomplete clinical data.
This comprehensive data collection aims to provide insights into the efficacy and outcomes of using dorsal toe fibula composite flaps in combination with iliac bone grafts for the reconstruction of finger defects across various grades.
Donor site selection criteria
The decision to use the homo-lateral (same-side) or heterolateral (opposite-side) big toe as the donor site was made based on a combination of patient-specific, functional, and anatomical considerations. Preoperative imaging, including CT angiography (CTA) and Doppler ultrasound, was used to assess the vascular anatomy, and the following criteria guided donor site selection:
Patient Preference: If the patient expressed a preference to avoid surgical intervention on both feet, the homo-lateral big toe was selected as the donor site to limit surgical impact to one side.
Functional Requirements: For patients with jobs requiring intensive foot use (e.g., manual laborers, athletes), the heterolateral big toe was preferred to ensure that the ipsilateral foot remained unaffected, thereby preserving its function and weight-bearing capacity.
Foot Symmetry and Aesthetics: In cases where the patient or surgeon prioritized maintaining bilateral foot symmetry, the heterolateral big toe was chosen to ensure that no visual asymmetry occurred between the two feet.
Anatomical Considerations: If the ipsilateral big toe had scars, previous surgical procedures, or other deformities, the heterolateral toe was used to avoid complications with blood supply, scarring, or poor-quality tissue.
Vascular Suitability: Preoperative CTA and Doppler imaging were used to assess the quality and size of the blood vessels on both sides. If the vascular anatomy on the contralateral foot showed superior vessel size and quality, the heterolateral big toe was selected as the donor site.
Surgical Complexity: In situations where minimizing surgical complexity was essential, the homo-lateral big toe was chosen to limit surgical intervention to one side.
By considering these criteria, the surgical team ensured an optimal balance between functional preservation, cosmetic outcome, and patient satisfaction.
Study sesign and setting
Preoperative preparation
The trend of the donor blood vessels and nerves, as well as their distribution on CTA or X-ray, was assessed. Routine cleaning and anti-infection therapy were administered. Based on the examination results and the defect area on the fibular dorsal side of the great toe, the design and marking of the nail bone-composite tissue flap for full reconstruction were carried out.
Surgical technique for full-shape finger reconstruction using dorsal toe composite flap and iliac bone
Under general anesthesia, the patient was placed in a supine position with the affected hand exposed on a sterile table. A pneumatic tourniquet was applied to the upper arm to provide a bloodless surgical field. Preoperative CT angiography (CTA) was performed to assess the vascular anatomy of the donor and recipient sites. The incision line on the plantar surface of the great toe at the stump level was marked using a surgical marker according to the anatomical position of key neurovascular structures, and the phalanx ends were trimmed with bone files.
A linear incision was made along the marked line on the plantar surface of the great toe using a No. 15 scalpel. The incision extended through the epidermis, dermis, and subcutaneous tissue to expose the dorsal digital artery, dorsal digital vein, and the proper digital nerve. One to two superficial veins were identified, carefully dissected, and preserved for later use in vascular anastomosis. The soft tissue was separated to expose the periosteum, which was incised to harvest the cortical bone. The harvested composite flap included the nail bed, subcutaneous soft tissue, vascular pedicle (dorsal digital artery and vein), and proper digital nerve.
After flap harvesting, the donor site was repaired by mobilizing the surrounding soft tissue to cover the exposed area. The incision was closed using 4–0 absorbable sutures in a tension-free manner, and hemostasis was confirmed. A sterile dressing was applied to the donor site.
At the recipient site, necrotic tissues were debrided, and the wound bed was prepared to ensure adequate vascularization. The distal and proximal phalanges were shaped using a bone file to create a flat surface for graft attachment. If a non-vascularized iliac bone graft was required, it was harvested and shaped to match the size and shape of the phalanges. The dorsal digital artery, vein, and nerve at the recipient site were identified and secured using microvascular loops.
The composite flap was transferred to the recipient site. Vascular anastomosis was performed using 10–0 nylon sutures to connect the dorsal digital artery to the first dorsal metatarsal artery and the dorsal digital vein to the superficial venous system. The proper digital nerve of the flap was coated with the recipient's nerve using 8–0 nylon sutures to restore sensory function. Bone fixation was achieved using K-wires or titanium screws, ensuring stable attachment of the bone graft to the phalanges.
Once the flap was secured, vascular patency was confirmed using the empty-and-refill test and Doppler ultrasound. The recipient site was irrigated with saline, and final hemostasis was achieved. The skin was closed with 4–0 non-absorbable sutures, and a sterile dressing was applied. Postoperative care included limb immobilization and monitoring for signs of ischemia, infection, or graft failure. Passive rehabilitation exercises were initiated two weeks postoperatively, and follow-up assessments were conducted at 1, 3, and 6 months to evaluate functional outcomes and donor site morbidity.
For Finger Defect Grade I:
The dorsal aspect of the great toe was incised, and the dorsal vein of the great toe was dissected. The required length for the injured finger was then cut from the toe. The vein was branched to the fibular side of the great toe, and the free vein bundle was dissected to the tip of the great toe. The dorsalis pedis artery, medial and lateral plantar arteries, and first dorsal metatarsal artery, which converge from the web between the second and great toe, were dissected. After identifying the first dorsal metatarsal artery and nerve, the great transverse artery was severed and the distal artery and nerve bundle were freed to the proximal end of the flap.
An incision was made along the marked line on the plantar surface of the great toe, and 1 to 2 superficial veins were dissected and preserved for subsequent use. The subcutaneous tissue was then incised deeply to the fibular side of the toe bone. The tibial side and proximal part of the great toenail were cut to the periosteum along the marking line. Care was taken not to damage the epiphyseal growth plate in children. The cortical bone was separated from the tibiometatarsal bone, and a section including the great toenail, skin composite tissue flap, first dorsal metatarsal artery, and nerve were excised together. The donor material was slightly extended by 1–2 mm beyond the length of the defect. The integrity of the donor nail bed was preserved. Finally, the donor area was repaired and sutured using pedicled flaps from the plantar great toe, plantar base, and plantar second toe.
-
(2)
For Finger Defects Grade II to III:
The surgical procedure began with an incision on the dorsal side of the great toe. One or two thick-caliber dorsal veins were meticulously dissected and severed to provide the necessary length for the defect. Next, the artery and nerve bundles were carefully dissected from the deep layers of the great toe and the fibula. The transverse artery of the great toe was cut and ligated. An incision was made on the tibial side of the great toenail, extending deep to the periosteum. The dorsal bony cortex of the phalanges was then cut, including the long extensor tendon side and the lateral side of the bone cortex. The phalanges, dorsal bony cortex, and some surrounding tissue were removed, preserving the nail bed.
The fibular dorsal composite tissue flap was then connected to the defect finger to ensure precise repair of the toe bone within the flap. Measurements were taken of the defect phalanx length and nail width in comparison to the healthy finger. For cases requiring distal interphalangeal joint reconstruction, the second interphalangeal joint was used as a backup. If the available grafts did not meet the length requirements for the finger bone defect, iliac bone was shaped as needed, and the dorsal fibular composite tissue flap was reconstructed accordingly.
For patients with smaller donor areas, pedicled flaps from the avulsed great toe, plantar base, and plantar second toe were utilized for repair. In cases involving larger wounds, additional flaps were taken from the groin or iliac area, or artificial dermal covers were used to ensure adequate coverage and repair.
Transplantation and reconstruction
The dorsal fibular composite tissue flap was rolled and carefully shaped to match the defect of the finger, ensuring a precise fit with the existing finger stump. The fibular base digital artery and nerve of the great toe were connected to the corresponding artery and nerve at the finger stump. The dorsal digital vein was also anastomosed with the dorsal digital vein, while the stump nail and skin tissue were sutured to the fibular dorsal nail and flap of the great toe.
For Finger Defect Grade I, fixation of the phalanges and residual finger bone was achieved using 0.8 mm sutures. For Finger Defects Grade II to III, iliac bone and phalanges were used in a series, with anastomosis and fixation to the residual finger bone.
During surgery, the flexion tendons were reconstructed based on the knuckle joint fusion, and the C-arm X-ray was used to ensure accurate fixation of the phalanges. Postoperatively, treatments for infection, inflammation, and swelling were administered as needed, with close monitoring of blood supply, skin color, and function at both the donor and recipient sites.
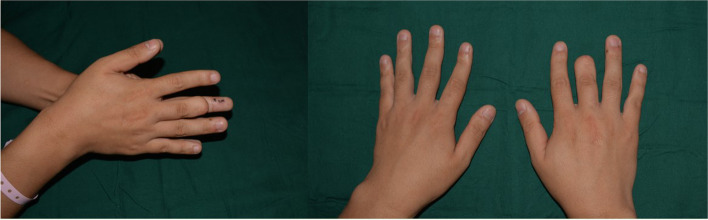
Case 1 (Figures 1, 2, 3, 4, 5 and 6): Right Hand Middle Finger Grade II Defect
Figures 1, 2: Preoperative examination showing a 3 cm defect in the distal phalanx of the middle finger.
Figures 3, 4: Design, incision, and fixation of the plantar and dorsal composite tissue flap from the toe, with successful immediate reconstruction of the defect.
Figure 5: Twelve days post-surgery, showing well-healed bone and finger reconstruction, with no drainage and reduced redness and swelling.
Figure 6: One month postoperative X-ray confirming accurate defect closure and fixation.
Fig. 1.
Preoperative X-ray and CT angiography (CTA) examination of finger defect
Fig. 2.
Appearance of degree II defect in the left middle finger before surgery
Fig. 3.
Design and harvesting of the foot plantar and dorsal composite tissue flap
Fig. 4.
Overall appearance immediately after surgery
Fig. 5.
Removal of sutures 2 weeks after surgery, showing the postoperative effect
Fig. 6.

Postoperative X-ray at 1-month follow-up
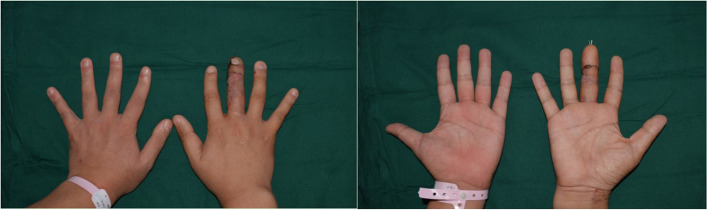
Case 2 (Figures 7, 8, 9, 10, 11 and 12): Left Thumb Grade III Defect
Figure 7: Preoperative display of the second finger defect.
Figures 8, 9: Design and separation of the dorsal composite tissue flap from the toe.
Figures 10, 11: One month post-operation X-ray review showing the reconstructed second finger closely resembles a normal second finger, with accurate internal fixation and partial recovery of sensory function.
Fig. 7.
Preoperative appearance of degree IIIb defect in the right index finger
Fig. 8.
Design, dissection, and preparation of the toe dorsal composite tissue flap
Fig. 9.
Immediate postoperative appearance following intraoperative procedures
Fig. 10.

Preoperative and postoperative X-ray comparison of bone transplantation
Fig. 11.

Recovery of the foot donor site post-transplantation
Fig. 12.

Three-month postoperative appearance showing the results of full shape reconstruction
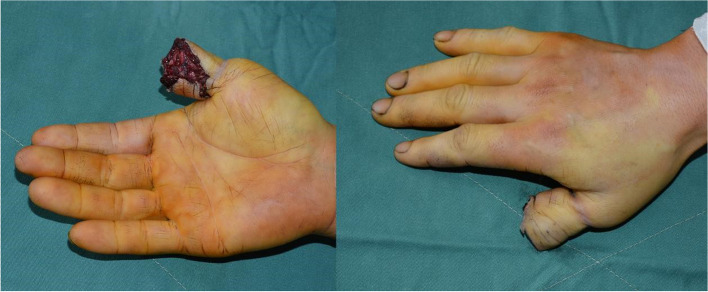
Case 3 (Figures 13, 14, 15, 16, 17, 18): Right Thumb Grade II Defect
Figure 13: Preoperative appearance of the thumb defect.
Figures 14, 15, 16: Thorough debridement of the defect, design and preparation of the dorsal composite tissue flap from the toe, and successful assembly.
Figure 17: Postoperative X-ray and immediate postoperative image showing effective bone transplantation and firm internal fixation.
Figure 18: Three-month follow-up showing the reconstructed thumb closely resembles a normal thumb, partial restoration of sensory function, and good recovery of the foot area with no complications.
Fig. 13.
Preoperative appearance of degree II defect in the right thumb
Fig. 14.

Design of the donor area and surgical excision diagram of the great toe and dorsal fibular composite tissue
Fig. 15.

Intraoperative image showing the free bone and composite tissue flap used for thumb reconstruction
Fig. 16.

Foot donor site on the same side, showing the iliac crest harvest and postoperative arterial perforator flap transplantation for shape repair
Fig. 17.

Comparison of preoperative and postoperative X-rays of the thumb bone defect
Fig. 18.

Three-month postoperative appearance of both the hand and foot following full reconstruction
The evaluation index
Patients were monitored for 3 to 6 months post-operation. Evaluations were carried out using the "Evaluation Standard of Hand Function" [6] and the "Evaluation Method of Hand Function in the Assessment of Human Injury Degree" [7]. The following assessments were conducted:
- Carroll's Hand Function Test: This test comprises 33 items across 6 dimensions: grasp, grip, lateral pinch, pinch, placement, pronation, and supination. Scores range from 0 to 100, with the following interpretations:
- 0–25: Very poor hand function; fine movements may be impossible.
- 26–50: Poor hand function; performing actions is challenging.
- 51–75: Limited hand function; basic movements are possible.
- 76–89: Incomplete hand function; certain movements remain unachievable.
- 90–98: Hand function is near normal; most actions can be performed.
- 99–100: Normal hand function.
Hand Movement Disability Score: This was assessed using the internationally recognized AB compound formula, where the score is calculated as A + B[x](100 - A). Here, A represents the disability degree of the distal interphalangeal joint of a finger, and B represents the disability degree of the proximal interphalangeal joint of the same finger.
Postoperative Outcomes: The survival, healing, and appearance of both donor and recipient sites were evaluated through outpatient visits, telephone follow-ups, and imaging reviews.
Statistical Methods
The data were corrected and processed using SPSS 27.0 software. The measurement data were entered into the system, and the results were analyzed using a paired sample t-test. The comparison results showed statistical significance (P < 0.05).
Results
Carroll hand function test scores for finger I to III defects
For patients with postoperative defects graded I to III, Carroll hand function test scores showed a significant increase (P < 0.05), as presented in Table 1.
Table 1.
Carroll hand function test scores for grade I to III finger defects ( ± s, points)
| The project | Finger I degree defect (n = 17) | Finger II degree defect (n = 23) | Finger III degree defect (n = 7) |
|---|---|---|---|
| Before surgery | 72.58 ± 6.39 | 65.23 ± 6.15 | 62.38 ± 5.46 |
| postoperative | 78.41 ± 5.35 | 74.60 ± 6.82 | 71.18 ± 5.29 |
| T | 2.884 | 4.893 | 3.063 |
| P | 0.007 | < 0.001 | 0.010 |
Hand motor disability scores for finger I to III defects
Following surgery, patients with Grade I-III finger defects exhibited a significant reduction in hand motor disability scores (P < 0.05), as detailed in Table 2.
Table 2.
Hand movement scores for grade I to III finger defects ( ± s, %)
| The project | Finger I degree defect (n = 17) | Finger II degree defect (n = 23) | Finger III degree defect (n = 7) |
|---|---|---|---|
| Before surgery | 22.03 ± 6.22 | 38.79 ± 7.10 | 45.70 ± 7.12 |
| postoperative | 12.35 ± 4.64 | 20.75 ± 5.63 | 25.30 ± 5.75 |
| t | 5.143 | 9.548 | 5.898 |
| P | < 0.001 | < 0.001 | < 0.001 |
Postoperative conditions
Thirty-six patients (47 fingers) underwent successful complete reconstruction. Among them, two patients with Grade III finger defects experienced numbness in the donor area. One patient had minor walking difficulties, and another had limited movement function. There was one case each of recipient site and donor site infections (Grade I and Grade II finger defects, respectively), which improved after dressing changes and cleaning. All recipient sites healed well, with 32 patients satisfied with the appearance and 4 finding it acceptable, resulting in an 88.89% satisfaction rate. Thirty-three cases of donor area healed well, while 3 cases had relatively slow healing (1 with a Grade II finger defect and 2 with Grade III finger defects). There were no hypertrophic scars. The appearance was normal in 29 cases, generally acceptable in 5 cases, and unsatisfactory in 2 cases, with an overall satisfaction rate of 80.56%.
Discussion
When reconstructing defects in fingers I to III degrees, using sections of the foot has been the traditional approach. However, with advances in surgical techniques and increasing patient expectations, particularly among younger individuals, directly using toe material for finger reconstruction is no longer universally preferred [8]. The current challenge is to restore the complete shape of the finger while maintaining the integrity, appearance, and function of the toes, providing a more optimal repair solution for patients.
For a degree I defect, which only involves the distal knuckle, the impact on hand function is relatively minor, and less material is required for repair. Therefore, a dorsal composite tissue flap from the toe can effectively achieve reconstruction [9].
In cases of degree II or III defects, which involve the proximal phalanx, middle phalanx, or phalangeal joint, full reconstruction must consider the flexibility and aesthetics of the finger while conserving the nail, bone, and flap of the toe. To ensure effective repair, clinical practice often involves bone flap transplantation combined with other tissues [10, 11].
This study focused on patients with finger defects I to III degrees who underwent iliac bone transplantation. Postoperative Carroll hand function test scores showed significant improvement due to the following advantages of the iliac bone: [12, 13].
The ilium has a rich blood supply and cancellous structure, making it easy to extract and shape.
The texture of the iliac bone is similar to that of the phalanx, promoting faster healing than cortical bone and ensuring a higher survival rate.
Combining a dorsal composite tissue flap from the toe with iliac bone reduces damage to the toes and meets the demands of the finger defect reconstruction. Additionally, the skin over the ilium is thinner and looser, reducing skin tension and not significantly affecting joint and tendon activity post-surgery [14].
These benefits highlight the effectiveness of using iliac bone in the reconstruction of finger defects, providing patients with better functional and aesthetic outcomes.
Some research [15] suggests using a foot or plantar medial flap with a pedicle skin flap for repair. However, considering that a large flap may increase foot discomfort, affect daily walking, or raise the risk of postoperative infection, the authors still recommend the iliac joint fibular dorsal composite tissue flap of the toe as the first choice. Postoperative hand motor disability scores of patients with I-III degree finger defects significantly improved compared to pre-operation scores. This indicates that the combined use of the toe fibular dorsal and iliac crest composite tissue flap can effectively enhance distal and proximal interphalangeal joint function and improve the motor ability of the reconstructed finger [16].
Additionally, the donor site is designed, decomposed, cut, and then recombined and reshaped according to the degree of finger defect. This approach avoids wasting donor material and preserves the great toe methyl group as much as possible, which is beneficial for regeneration [17]. However, there are still significant clinical differences in the reconstruction of the distal interphalangeal joint, increasing the difficulty, risk, and duration of the surgery and rehabilitation period. Current methods do not show a clear advantage for reconstructing the distal interphalangeal joint [18, 19].
Moreover, Wu C [20] found in a twelve-year postoperative follow-up that patients with finger defects had a significant difference in the motion of the proximal interphalangeal joints, grip strength, and pinch strength compared to the contralateral hand. This suggests that the reconstruction of the interphalangeal joint should consider various factors and prioritize practicality, avoiding the excessive pursuit of complete recovery.
After surgery, two patients experienced numbness in the donor area. This is likely due to reduced blood circulation and impaired nerve and blood vessel function in the toe. To mitigate this, it is recommended to carefully separate the dorsal blood vessels and nerve bundles in the toe, preserving as many arteriovenous branches as possible and considering reconstruction using the second toe or its arteriovenous branches.
The use of the nonvascularized iliac crest bone graft is a widely accepted technique for reconstructing phalangeal defects due to its abundant availability, ease of harvest, and minimal donor site morbidity. However, a notable disadvantage of nonvascularized bone grafts is their susceptibility to bone resorption. Unlike vascularized bone grafts, which maintain their own blood supply, nonvascularized grafts rely on the host site to induce revascularization. Insufficient revascularization can result in reduced metabolic activity within the graft, leading to the activation of osteoclast-mediated bone resorption.
To minimize this risk, we adopted several measures. First, precise bone shaping and press-fit fixation were performed to maximize the bone-to-bone contact, promoting faster revascularization. Additionally, K-wire fixation provided stability, reducing micro-movements at the graft-recipient interface, which is known to promote graft integration. These strategies aimed to enhance osteoconductive processes and limit the extent of resorption. In our study, there were no cases of complete bone resorption, and postoperative X-rays confirmed graft stability and fusion.
Despite these efforts, it is important to recognize that partial bone resorption may still occur, especially in larger grafts or in patients with compromised bone healing potential (e.g., smokers, diabetic patients). Future studies may explore the use of bone morphogenetic proteins (BMPs) or autologous platelet-rich plasma (PRP) to promote bone regeneration and further reduce the risk of resorption.
Previous studies [21, 22] have also reported that nonvascularized iliac bone grafts are prone to resorption compared to vascularized grafts. However, due to the reduced surgical complexity and shorter operating time associated with nonvascularized grafts, this approach remains a viable option for selected patients.
Our findings align with previous research by Kobayashi et al. (2020) [23], who reported favorable outcomes using partial toenail flaps. Similarly, Cai et al. [19] demonstrated the successful reconstruction of soft tissue defects using toenail flaps. Our approach builds on this by integrating the iliac bone graft to restore structural support, particularly for Grade II and III defects, as suggested by Yin et al. (2020). [24] Reconstructing the functionality of a defective finger is a long-term process. This study did not conduct long-term follow-up, included a limited number of cases, and lacked comparative cases. Consequently, the long-term efficacy of using a composite tissue flap from the toe and dorsal series with iliac transplantation for I to III-degree finger defects requires further in-depth analysis with more extensive research data.
Limitations of the study
This study has several limitations that need to be acknowledged. First, the sample size was relatively small, with only 36 patients included, which may limit the generalizability of the findings. Additionally, the study did not include a long-term follow-up period, which is crucial for assessing the sustainability of the surgical outcomes and potential long-term complications. The lack of a control group or comparative cases also limits the ability to draw definitive conclusions about the relative efficacy of the dorsal toe fibula composite flap and iliac bone transplantation technique. Moreover, the study did not account for variations in patient demographics, such as age and underlying health conditions, which could influence the results. Future research with a larger sample size, longer follow-up, and comparative analysis is needed to validate these findings and provide a more comprehensive understanding of the technique's effectiveness and limitations.
Conclusion
In conclusion, the use of dorsal toe fibula composite flaps and iliac bone in sequential transplantation has proven to be an effective method for the complete reconstruction of fingers with grade I to III defects. The technique not only significantly improves hand function, as evidenced by increased Carroll hand function test scores and decreased hand motor disability scores but also maintains high patient satisfaction rates regarding the appearance and functionality of both donor and recipient sites. Despite some minor complications, such as numbness at the donor site and occasional infections, the overall outcomes were favorable. The study highlights the potential of this surgical approach to offer a viable solution for patients requiring comprehensive finger reconstruction, though further research is warranted to address its long-term efficacy and optimize surgical techniques.
Authors’ contributions
Guoshan Li conceived the study and was responsible for the study design and overall direction. Huyu Du and Yuxin Yan contributed to data collection and analysis. Yong Hou and Guangsheng Zhao assisted in the surgical procedures and technical aspects. Xiaolian Lei and Zihan Meng contributed to manuscript drafting and revisions. Linfeng Liu supervised the study and serving as the corresponding author.
Funding
This research was supported by the Taiyuan Bureau of Science and Technology, Science, Technology, and Innovation Program of National Regional Medical Center (Grant No. 202221).
Data availability
he datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
This study was conducted in accordance with the principles of the Declaration of Helsinki and was approved by the Ethical Committee of Taiyuan Hospital of Peking University First Hospital (Taiyuan Central Hospital), under Approval Number 2023041. Informed consent was obtained from all participants and/or their legal guardian(s).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Haolin Sun, Email: dr_sunhaolin@outlook.com.
Linfeng Liu, Email: 18135532659@163.com.
References
- 1.Sahu RK, Kala PC, Dixit PK, Chakraborty SS, K S, Katrolia D. Finger pulp reconstruction with thenar flap: Aesthetic and functional outcome. Chin J Traumatol. 2020;23(5):307–310. 10.1016/j.cjtee.2020.02.004 [DOI] [PMC free article] [PubMed]
- 2.Bregoli C, Biffi CA, Morellato K, et al. Osseointegrated Metallic Implants for Finger Amputees: A Review of the Literature. Orthop Surg. 2022;14(6):1019–33. 10.1111/os.13296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Podolsky DJ, Mainprize J, McMillan C, Binhammer P. Suitability of Using the Hamate for Reconstruction of the Finger Middle Phalanx Base: An Assessment of Cartilage Thickness. Plast Surg (Oakv). 2019;27(3):211–6. 10.1177/2292550319826084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fan X, Zhou Y, Zhou J, Dai S, Liu J, Lao K. The reconstruction of fingertip injury by mini hallux toenail flap pedicled with the hallux transverse artery and toe pulp vein transplantation technique based on the equivalent design theory. BMC Surg. 2023;23(1):231. Published 2023 Aug 11. 10.1186/s12893-023-02097-1 [DOI] [PMC free article] [PubMed]
- 5.Matsusue T. Easy and Simple Techniques to Reconstruct Natural Nailfold with the Wrap-around Flap for Finger Reconstruction. Arch Plast Surg. 2022;49(6):764–768. Published 2022 Dec 13. 10.1055/s-0042-1757573 [DOI] [PMC free article] [PubMed]
- 6.Lee JK, Jung M, Lee HB, Chung HJ, Lee SH. Reliability and Validity of the Martin Vigorimeter for Grip Strength Measurement in Korean Adults. Clin Orthop Surg. 2024;16(4):610–9. 10.4055/cios23383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gopal A, Hsu WY, Allen DD, Bove R. Remote Assessments of Hand Function in Neurological Disorders: Systematic Review. JMIR Rehabil Assist Technol. 2022;9(1):e33157. Published 2022 Mar 9. 10.2196/33157 [DOI] [PMC free article] [PubMed]
- 8.Li X, Zhang L, Sun C, Zhang H, Li W. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2023;37(12):1496–500. 10.7507/1002-1892.202310038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu F, Xiao F, Peng G, et al. Repair of distal finger soft-tissue defects with free fibular great toe neurovascular flaps. BMC Musculoskelet Disord. 2024;25(1):479. Published 2024 Jun 18. 10.1186/s12891-024-07563-2 [DOI] [PMC free article] [PubMed]
- 10.Sơn TT, Việt Dung PT, Nghĩa PT, Hồng Thúy TT. Reconstruction of Finger Soft Tissue Defects With a Thinned Free Anterolateral Thigh Flap. Ann Plast Surg. 2023;91(2):238–44. 10.1097/SAP.0000000000003612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wang T, Wang L, Wang H, Zhang W, Yu Z, Zhang J. Innervated Reconstruction of Fingertip Degloving Injury Using a Dorsal Digital Perforator Flap Combined With a Cross-Finger Flap. Ann Plast Surg. 2022;88(5):500–6. 10.1097/SAP.0000000000003110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aleksandrov NM, Petrov SV, Kuptsov DA, Petrov MS. Reconstruction of Fingers Using Skin-Bone Grafts with Microvascular Anastomoses. Sovrem Tekhnologii Med. 2020;12(1):16–22. 10.17691/stm2020.12.1.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Xu L, Tan J, Wei P, Luo X, Tan H, Mudgal CS. CLINICAL APPLICATION OF 3D PRINTING TECHNOLOGY FOR PREOPERATIVE PLANNING OF THUMB RECONSTRUCTION. Acta Ortop Bras. 2021;29(4):211–8. 10.1590/1413-785220212904235492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Greyson MA, Kinsley S, Talbot SG. Thumb reconstruction by "on-top-plasty" of the long finger. Case Reports Plast Surg Hand Surg. 2021;8(1):87–92. Published 2021 Jul 9. 10.1080/23320885.2021.1935965 [DOI] [PMC free article] [PubMed]
- 15.Langat AS, Wan Sulaiman WA, Mat Johar SFN. Heel Pad Reconstruction With Medial Plantar Flap. Cureus. 2021;13(3):e13987. Published 2021 Mar 19. 10.7759/cureus.13987 [DOI] [PMC free article] [PubMed]
- 16.Zhou KJ, Graham DJ, Lawson RD, Sivakumar BS. Toe-to-Finger Vascularized Joint Transfers for Proximal Interphalangeal Joint Reconstruction: A Systematic Review. Hand (N Y). 2022;17(6):1031–8. 10.1177/1558944720988081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Biesecker LG, Aase JM, Clericuzio C, Gurrieri F, Temple IK, Toriello H. Elements of morphology: standard terminology for the hands and feet. Am J Med Genet A. 2009;149A(1):93–127. 10.1002/ajmg.a.32596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ishiura R, Shiraishi M, Okada Y, et al. Treatment of cold intolerance following finger pulp amputations: a case comparison between immediate finger replantation and delayed pulp and digital arterial arch reconstruction with flow-through free hypothenar flap. Case Reports Plast Surg Hand Surg. 2021;9(1):33–36. Published 2021 Dec 27. 10.1080/23320885.2021.2020656 [DOI] [PMC free article] [PubMed]
- 19.Cai L, Zhang X, Zhang Y, et al. Reconstruction of Composite Soft Tissue Defect in the Distal Finger Using Partial Toenail Flap Transfer. Orthop Surg. 2023;15(10):2716–23. 10.1111/os.13829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wu C, Drake M, Means KR Jr. Total Joint Arthroplasty of a Proximal Interphalangeal Joint with Proximal Metal Surface Replacement and Distal Hemi-Hamate Autograft: A Long-Term Follow-Up. J Hand Surg Glob Online. 2022;4(3):189–193. Published 2022 Mar 3. 10.1016/j.jhsg.2022.02.002 [DOI] [PMC free article] [PubMed]
- 21.Handschel J, Hassanyar H, Depprich RA, Ommerborn MA, Sproll KC, Hofer M, Kübler NR, Naujoks C. Nonvascularized iliac bone grafts for mandibular reconstruction–requirements and limitations. In Vivo Published. 2011;25(5):795–9. [PubMed] [Google Scholar]
- 22.Pogrel MA, Podlesh S, Anthony JP, Alexander J. A comparison of vascularized and nonvascularized bone grafts for reconstruction of mandibular continuity defects. J Oral Maxillofac Surg Published. 1997Nov;55(11):1200–6. 10.1016/s0278-2391(97)90165-8. [DOI] [PubMed] [Google Scholar]
- 23.Kobayashi K, Masuyama N, Nishimura K. Aesthetic Reconstruction of Fingers and Thumbs With the Vascularized Half-Big Toenail Flap With Minimum Donor Site Morbidity. J Hand Surg Glob Online. 2020Jun 29;2(4):203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yin Y, Tao X, Li Y, Bao B, Ying Y, Bao T, Wang J. Cosmetic and functional results of a newly reconstructed thumb by combining the phalanx of second toe and the great toenail flap transplantation. J Orthop Surg Res. 2020Oct 6;15(1):458. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
he datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.