Abstract
Background
The factors that cause children to become smokers in adolescence remain unclear. Although parental smoking and peer pressure may play a role, physiological factors such as lung volume have also been identified.
Methods
To investigate these and other possible childhood predictors of teenage smoking, we gathered follow-up data on 191 Montréal schoolchildren, aged 5–12 years (average 9.2 yr) when first examined. At an average age of 13.0 years, they answered further questions on their health and smoking behaviour and provided a second set of spirometric measurements.
Results
At the second survey, 80% of the children had entered high school and 44% had become smokers. Reaching puberty between the surveys was the most significant determinant of becoming a smoker: 56.4% of the 124 children postpubertal at the second survey had taken up smoking, versus 17.9% of the 67 who were still prepubertal (p = 0.001). We found salivary cotinine level, a measure of uptake of environmental tobacco smoke, to be an independent predictor of becoming a teenage smoker; even after adjustment for sex, socioeconomic status of parents, a crowding index, and the numbers at home of siblings, adult smokers and cigarettes smoked, it remained significant for both groups: postpubertal (odds ratio [OR] 1.2, 95% confidence interval [CI] 1.2–3.0) and prepubertal (OR 2.1, 95% CI 1.0– 4.5). The influence of forced vital capacity was marginally significant only in the postpubertal group (OR 5.0, 95% CI 0.88–28.3).
Interpretation
The proportion of nicotine absorbed from that available in environmental tobacco smoke during childhood is associated with subsequent smoking in adolescence. The more efficient absorption of nicotine seen in some children may be related to physiological factors such as lung capacity.
One striking failure in the campaign against smoking is the continuing number of adolescents who take up the habit. Parental smoking during childhood and adolescent peer pressure are commonly cited as predictors of teenage smoking;1,2 an association with larger lung volumes has also been reported.3,4,5 We decided to compare these and other associations directly by following up on data we had gathered in a previous community-based survey.6
Methods
For our first survey (1990–1992), we made a random selection of 18 Montréal schools after a stratification of all school boards in central Montréal. They were ranked within school boards by socioeconomic status, as described in that report.6 In each school, all the children in 1 class in each of grades 1, 3 and 5 (corresponding to ages 5–7, 8–9 and 10–12 years, respectively) were invited to take part through a questionnaire addressed to and answered by their parents. Each child in grade 5 who participated was also asked, in private, if he or she smoked. With parental permission, we visited the homes of a random sample of children (31%) to gather additional information on housing conditions and to collect a sample of the children's saliva to analyze for cotinine concentration as a measure of their individual uptake of environmental tobacco smoke.7,8,9,10 Satisfactory cotinine measurements were available for 191 of 309 children, who composed the present study population. At the time of the second survey (1994–1996), all 191 children (80% of whom had since entered high school) answered a questionnaire about their health and smoking habits and performed spirometry.
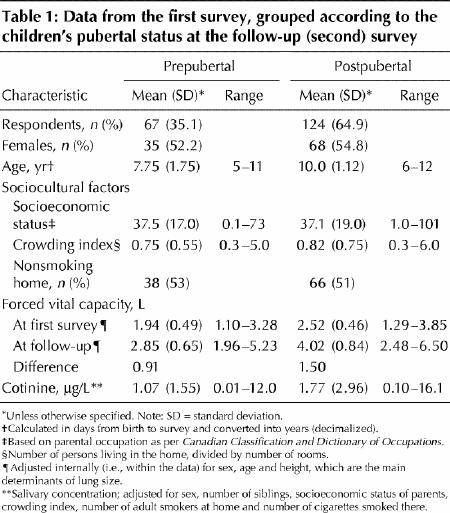
The outcome of interest was having become a smoker by the second survey, defined as an answer of “Yes” to the question, “Have you ever smoked as much as 1 cigarette a week for a month?” Social and cultural factors that may affect levels of environmental tobacco smoke in the home and physiologic data from the first survey are shown in Table 1. During the second survey, we recorded pubertal status (defined as a “yes” answer to the survey question “Have you started your menstruations?” for girls or “Has your voice changed?” for boys), the high school currently attended (a composite marker of peer pressure to smoke and the scholastic and sporting expectations attributed to each school) and changes in family smoking behaviours since the first survey, which we interpreted as indications of parental attitudes toward smoking (negative, if an increase in the number of adult smokers in the home had been allowed; and positive, if smoking cessation in the home appeared to have been encouraged). Univariate analysis was used to select potential explanatory factors, based on 2-tailed p values of 0.10 or less. Independent predictors were determined by multivariate logistic regression analyses.
Table 1
Results
Of the 191 study subjects with data on cotinine levels, 103 (54%) were girls and 88, boys. Their average age at the time of the first survey was 9.2 years, and at the second, 13.0 years. None of the grade 5 children reported being a smoker, although 14 children (7.3%) did not answer the question. Four children at the first survey had concentrations of salivary cotinine that were markedly elevated, but in only 1 child did the level approach 20 μg/L, the usual cutoff for defining a smoker.8 At the time of the second survey, 84 children (44.0%) had become smokers; of these, 10 boys and 10 girls smoked more than 10 cigarettes per week. Attaining puberty between surveys was the most significant determinant of becoming a teenage smoker (56.4% of postpubertal children compared with 17.9% of those still prepubertal when the follow-up survey was administered, p = 0.001). Subsequent analyses were therefore stratified by the children's pubertal status at the second survey (Table 2).
Table 2
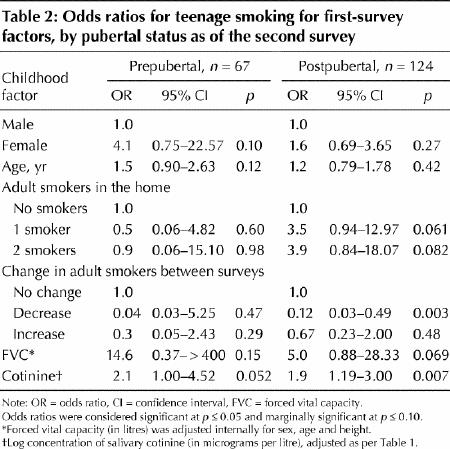
The only factor associated with becoming a teenage smoker in both pre- and postpubertal children was salivary cotinine concentration (adjusted in the analysis for sex, number of siblings, socioeconomic status of the parents, crowding index, number of smokers at home and total number of cigarettes smoked in the home). In prepubertal children, a marginally significant childhood factor was female sex; in postpubertal children, forced vital (lung) capacity and the presence of adult smokers in the home, whether single (i.e., 1 smoker) or multiple. The specific high school currently attended, which was recorded at the second survey, also showed marginal significance (p = 0.09; data not shown).
Interpretation
Our study population was small, and multiple comparisons were made; our results must therefore be interpreted with caution. Moreover, salivary cotinine levels may reflect current smoking by the child as well as environmental tobacco smoke; given the low rates in the first survey both of salivary cotinine and of reported smoking, however, this effect is likely to have been small.
An unexpected finding in the multivariate analysis was the lack of any significant association between becoming a teenage smoker and the number of smokers in the home in childhood (p = 0.99). Also unexpected was the association between a decrease in the number of adult smokers in the home between surveys (thought to indicate a positive parental attitude toward smoking cessation) and a decrease in the number of adolescents becoming smokers (the reduction in risk is shown in Table 2). This could have been caused not only by parental disapproval but alternatively by nonsmoking teenagers pressuring their parents to quit.8,9,10 It nonetheless shows the importance of a dynamic attitude at home against smoking.
As for the anatomic and physiologic findings, the most important observation was that salivary cotinine in childhood (a measurement of the nicotine actually entering the bloodstream) was an independent predictor of adolescent smoking, after adjustment in the analysis for amount smoked at home and other relevant factors (see final footnote, Table 1). Given also the association (admittedly not strong) between forced vital capacity and adolescent smoking, we suggest that lung size (or some associated characteristic) increases the uptake of environmental tobacco smoke, maximizes the influence of passive smoking in childhood and induces smoking in adolescence. In this context, the recently reported reduced density of dopamine D1 receptors in the ventral striatum of the brains of adult smokers of cigarettes led those investigators11 to speculate that a hypodopaminergic state may play an important role in sustaining “nicotine-seeking” behaviour and future addiction.
In conclusion, we hypothesize that enhanced susceptibility to environmental tobacco smoke in childhood increases the risk of nicotine-seeking behaviour in adolescence. If proved correct, this would be valuable information to use in the ongoing campaign against smoking in teenagers.
β See related article page 382
Acknowledgments
The study was funded by the Medical Research Council (Canada) in a grant to the Respiratory Health Network of Centres of Excellence (Principal Investigator, P.T. Macklem). Pierre Ernst was a Chercheur Boursier (Fonds de la recherché en Santé du Québec) and Margaret Becklake was a Career Investigator (Medical Research Council, Canada) during the original study. Dr. Maurice McGregor provided a critical review of the text.
Footnotes
This article has been peer reviewed.
Contributors: Pierre Ernst and Margaret Becklake were responsible for data collection. Heberto Ghezzo designed this study and carried out the statistical analysis. All authors contributed equally to the writing and revision of the manuscript.
Competing interests: None declared.
Correspondence to: Dr. Margaret R. Becklake, Respiratory Epidemiology and Clinical Research Unit, Montreal Chest Institute, Rm. K1.33, 3650 St Urbain Street, Montréal QC H2X 2P4; margaret.becklake@mcgill.ca
References
- 1.Pierce JP, Choi WS, Gilpin EA, Farkas AJ, Merritt RK. Validation of susceptibility as a predictor of which adolescents take up smoking in the United States. Health Psychol 1996;15(5):355-61. [DOI] [PubMed]
- 2.Cook DG, Whincup PH, Jarvis MJ, Strachan DP, Papacosta O, Bryant A. Passive exposure to tobacco smoke in children aged 5–7 years: individual, family, and community factors. BMJ 1994;308(6925):384-9. [DOI] [PMC free article] [PubMed]
- 3.Tashkin DP, Clark VA, Coulson AH, Bourque LB, Simmons M, Reems C, et al. Comparison of lung function in young nonsmokers and smokers before and after initiation of the smoking habit: a prospective study. Am Rev Respir Dis 1983;128(1):12-6. [DOI] [PubMed]
- 4.Leech JA, Ghezzo H, Stevens D, Becklake MR. Respiratory pressures and function in young adults. Am Rev Respir Dis 1983;128(1):17-23. [DOI] [PubMed]
- 5.Becklake MR, Lalloo U. The “healthy smoker”: a phenomenon of health selection? [review]. Respiration 1990;57(3):137-44. [DOI] [PubMed]
- 6.Ernst P, Demissie K, Joseph L, Locher U, Becklake MR. Socioeconomic status and indicators of asthma in children. Am J Respir Crit Care Med 1995;152(2):570-5. [DOI] [PubMed]
- 7.Ernst P, Ghezzo H, Becklake MR. Risk factors for bronchial hyperresponsiveness in late childhood and early adolescence. Eur Respir J 2002;20:635-9. [DOI] [PubMed]
- 8.Coultas DB, Howard CA, Peake GT, Skipper BJ, Samet JM. Salivary cotinine levels and involuntary tobacco smoke exposure in children and adults in New Mexico. Am Rev Respir Dis 1987;136(2):305-9. [DOI] [PubMed]
- 9.Jarvis MJ, McNeill AD, Bryant A, Russell MAH. Factors determining exposure to passive smoking in young adults living at home: quantitative analysis using saliva cotinine concentrations. Int J Epidemiol 1991;20(1):126-31. [DOI] [PubMed]
- 10.Jaakkola MS, Jaakkola JJ. Assessment of exposure to environmental tobacco smoke [review]. Eur Respir J 1997;10(10):2384-97. [DOI] [PubMed]
- 11.Dagher A, Bleicher C, Aston JA, Gunn RN, Clarke PB, Cumming P. Reduced dopamine DF1 receptor binding in the ventral striatum of cigarette smokers. Synapse 2001;42(1):48-53. [DOI] [PubMed]


