Abstract
Background
Acute kidney injury (AKI) is a significant health concern in hospitalized children and is associated with increased mortality. However, the true burden of AKI-associated mortality in pediatric populations remains unclear.
Objective
To determine the pooled incidence of mortality independently associated with AKI in hospitalized children globally.
Data sources
Medline and Embase were searched for studies published by March 2024.
Study eligibility criteria
The inclusion criteria encompassed observational studies involving hospitalized pediatric patients (< 18 years old) with AKI. Only studies that identified AKI as an independent risk factor for increased mortality in multivariate analysis were considered.
Study appraisal and synthesis methods
Studies with at least 100 AKI patients were included in the meta-analysis. Two authors extracted data on the study and patients’ characteristics and mortality across AKI stages and assessed the risk of bias. We used a random-effects meta-analysis to generate pooled estimates of mortality.
Results
Analysis of 60 studies including 133,876 children with AKI revealed a pooled in-hospital mortality rate of 18.27% (95% CI: 14.89, 21.65). Mortality increased with AKI severity; 8.19% in stage 1, 13.44% in stage 2, and 27.78% in stage 3. Subgroup analyses showed no significant differences across geographical regions, income levels, or AKI definition criteria. The pooled post-discharge mortality rate was 6.84% (95% CI: 5.86, 7.82) in a 1–9-year follow-up period.
Conclusions
This meta-analysis demonstrates a substantial global burden of AKI-associated mortality in hospitalized children, with higher mortality rates in more severe AKI stages. These findings highlight the critical need for early detection and intervention strategies in pediatric AKI management.
Clinical trial number
Not applicable.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12882-025-04033-2.
Keywords: Acute kidney injuries; Acute renal injury; Infant; Child, preschool; Cause of death; Child mortality; Acute kidney failures; Fetal outcome; Hospital mortality; Infant, newborn
Introduction
Acute kidney injury (AKI) poses a significant health concern for hospitalized children, leading to adverse outcomes and increased in-hospital and post-discharge mortality rates [1]. In efforts to standardize AKI diagnosis, several classification systems like KDIGO and RIFLE have been introduced to gain better insights into this condition and its effects on children. The lack of consensus on a universally accepted standardized definition for AKI in children has resulted in variations in its incidence and staging [2]. Furthermore, AKI has been significantly associated with short-term adverse outcomes, including prolonged hospital stays and in-hospital mortality [3]. Additionally, AKI has demonstrated links to long-term consequences such as hypertension, proteinuria, and chronic kidney disease in infants and children, potentially leading to post-discharge mortality. This highlights the necessity for comprehensive management strategies [4]. Nevertheless, irrespective of the setting of patients, mortality rates are proved to be higher among patients with AKI compared to those without AKI [1] and there is an ongoing investigation into the incidence of AKI-associated mortality in different pediatric populations.
To devise effective interventions, it is crucial to comprehend the incidence of AKI-associated mortality in diverse groups of children. Studies have indicated that the occurrence of AKI varies, with rates ranging from 5 to 31% in non-critically ill hospitalized children and up to 55% in critically ill hospitalized children [5–8]. Moreover, the burden and causes of AKI vary worldwide, with different resource settings facing distinct challenges. Some studies show low and low-to-middle-income countries experience a higher incidence of AKI due to factors like contaminated water and endemic diseases, such as malaria [4]. In such settings, the mortality of AKI can be worse than high-income countries [4].
Despite the existing literature on AKI mortality, a knowledge gap remains regarding the true burden and mortality rates associated with AKI in children. A previous meta-analysis have reported mortality rates of 11% among hospitalized children with AKI, but these rates have not been statistically proven to be independently associated with AKI via multivariate analysis in many of the included studies [1]. Confounding factors and the complexity of critically ill children contribute to the challenges in attributing mortality solely to AKI. Therefore, our systematic review and meta-analysis aims to determine the overall rate of mortality that is directly linked to AKI in children on a global scale. By synthesizing available evidence, this study intends to enhance our understanding of the impact of AKI on pediatric patients.
Methods
Study design
This review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020) guidelines [9] and was prospectively registered on the International Prospective Register of Systematic Reviews (PROSPERO ID: CRD42024527413). To identify relevant studies, an extensive literature search was performed across Medline (via Pubmed) and Embase in March 18th 2024. In order to optimize search results, tailored search strategies were developed for each database, incorporating pertinent keywords and Medical Subject Headings (MeSH) terms directly related to acute kidney injury (AKI) in the pediatric population (Supplemental material 1). Language restrictions were avoided during the literature search process. Articles in languages other than English were translated using online services such as Doc Translator, and then have them reviewed by an expert translator fluent in both the original language and English to ensure accuracy. Additionally, to enrich our electronic search, we manually scrutinized the bibliographies of eligible studies that met our inclusion criteria.
Study selection
To generate pooled global estimates of AKI mortality, we established rigorous inclusion criteria for selecting relevant studies. Specifically, we only included cohort and cross-sectional studies that reported AKI-related mortality, given that they demonstrated an independent association between AKI and mortality through the application of multivariate analysis. We investigated mortality rates during hospitalization and after discharge, in the pediatric population aged below 18 years. To ensure methodological consistency and the integrity of our analysis, we implemented a series of exclusion criteria. Studies on adults aged over 18 years were excluded from consideration. Additionally, we omitted studies in the form of conference abstracts that did not provide sufficient information for a robust assessment of diagnostic criteria and risk of bias. To achieve an objective screening process, eight authors in pairs independently assessed the titles and abstracts of the electronic records initially. Subsequently, the same authors meticulously evaluated the full texts of relevant articles to determine the final selection of studies for incorporation into our review. In the event of any disagreements between the two authors, a collaborative discussion was undertaken to reach a consensus. This methodological approach guarantees the quality and reliability of our pooled estimates of AKI mortality in the global pediatric population.
Data extraction and quality assessment
The full set of records was divided into four equal parts, with each part independently screened (title/abstract and full-text) by a pair of authors. Each pair reviewed their assigned portion, discussing and resolving any discrepancies between them. Any unresolved conflicts were addressed with the involvement of a third reviewer (MY). This division and screening process ensured that all records were reviewed independently by at least two authors, as recommended by the PRISMA guidelines, while accommodating the high volume of records.
The data extracted included the first author’s name, year of publication, country, data gathering period, study design, clinical setting (e.g., intensive care unit, cardiac surgery, etc.), participants’ age, sample size, number of children with AKI and its severity, in-hospital and post-discharge mortality number in AKI patients among each stage, AKI criteria and definition, and follow-up duration. We also extracted data indicating countries’ development and overall health status including gross domestic income per capita (GDP) [10], % GDP spent on total health expenditure [11], and maternal mortality ratio (MMR) [12] defined as deaths due to complications from pregnancy or childbirth per 100,000 live births.
Based on KDIGO criteria, we equaled the AKI stages in all studies into 3 stages. For RIFLE, pRIFLE, and nRIFLE, “Risk”, “Injury”, and “Failure”, were considered equivalent to KDIGO stage 1, stage 2, and stage 3, respectively. Since many studies had categorized AKI with merged stages, we reported stage-1 and 2, and stage-2 and 3 together for these studies. To assess the risk of bias in the included studies, we utilized the National Heart, Lung, and Blood Institute Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [13].
Statistical analysis
All statistical analyses were conducted using the STATA 18.0 statistical program. To calculate the incidence of mortality among hospitalized patients with AKI, we employed the “meta” package with the random-effect model and reported a pooled incidence with a 95% confidence interval (95% CI). Statistical heterogeneity was assessed using I2 and Chi-square tests. To explore the potential sources of heterogeneity, we performed subgroup analyses as per severity of AKI, clinical setting, study design, and economic groups of countries classified by World Bank.
To better understand and interpret the results with and without small-study effects on the incidence of AKI-associated mortality, we conducted meta-analyses on studies of any sample size and separately on studies with a minimum of 100 AKI patients. Our findings primarily emphasize the results from the latter group, which are presented in the manuscript. For interested readers, the supplementary material includes a table providing subgroup analysis and meta-regressions that incorporate studies without excluding studies with smaller sample sizes.
Meta-regressions were performed to assess the effects of gross domestic product (GDP) per capita in the year 2022 and % of GDP spent on health expenditure (the year 2020), and maternal mortality ratio (2000–2020) on AKI-associated mortality.
Since only five included studies assessed post-discharge mortality, subgroup analysis and meta-regression was not applicable for post-discharge mortality.
Results
Study selection and characteristics of the included studies
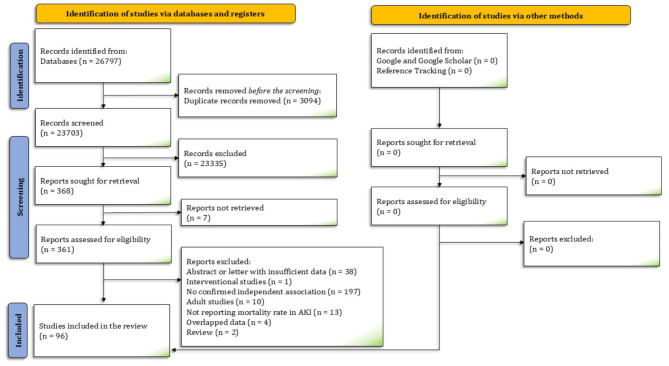
We identified 26,797 records from electronic databases. After screening 363 full-text articles, 96 studies were included in this systematic review [3, 14–108] (Fig. 1). The meta-analysis data comprised 96 in-hospital and 5 post-discharge mortality observations. These studies, from over 24 countries, enrolled a total of 135,448 hospitalized children with AKI. All of these studies reported mortality, which was confirmed to be independently associated with AKI. The characteristics of the included studies are reported in Table 1.
Fig. 1.
The PRISMA flow diagram depicts the flow of the study selection process through the different phases of the present systematic review
Table 1.
Summary characteristics of the included studies
| Author, year | Country | Study Design | Etioology | Neonates/Infants & Children | Admission sites | Aki Criteria | AKI (n) | Mortality (Overall) | Mortality Assessment |
|---|---|---|---|---|---|---|---|---|---|
| Adegboyega, 2022 [109] | USA | Retrospective | LBW | Only neonate | NICU | KDIGO | 116 | 21 | In-hospital |
| Ahn, 2024 [108] | USA | Retrospective | Hypoxic ischemic encephalopathy | Only neonate | NICU | KDIGO | 64 | 10 | In-hospital |
| Akcan-Arikan, 2007 [107] | USA | Prospective | Mixed | Non-neonate | PICU | pRIFLE | 123 | 18 | In-hospital |
| Al Gharabieh, 2023 [106] | USA | retrospective | Sepsis | Only neonate | NICU | KDIGO | 16 | 7 | In-hospital |
| Algadeeb, 2021 [104] | Saudi Arabia | Retrospective | Mixed | Only neonate | NICU | KDIGO | 396 | 122 | In-hospital |
| Al-Mouqdad, 2021 [105] | Saudi Arabia | Retrospective | LBW | Only neonate | NICU | KDIGO | 268 | 79 | In-hospital |
| Alobaidi, 2019 [103] | Canada | Retrospective | Mixed | Non-neonate | PICU | KDIGO | 308 | 21 | In-hospital |
| Alvarez-Hernandez, 2015 [102] | Mexico | Retrospective | Infection | Neonate and non-neonate | PICU, NICU and ward | NR | 14 | 7 | In-hospital |
| Arruda Moraes, 2023 [15] | Brazil | Retrospective | LBW | Only neonate | NICU | KDIGO | 61 | 22 | In-hospital |
| Bakkaloglu, 2024 [101] | Turkey | Retrospective | Crush-AKI | Neonate and non-neonate | Mix | oligo/anuria or serum creatinine level > 2 times the upper limit of age- and sex-referenced normal levels | 314 | 20 | In-hospital |
| Basu, 2021 [100] | multinational | Prospective | Sepsis/Infectious | Non-neonate | PICU | KDIGO | 307 | 37 | In-hospital |
| Bauer, 2023 [99] | USA | Retrospective | Hematopoietic cell transplantation | Non-neonate | PICU and ward | KDIGO | 186 | 47 | In-hospital |
| Bezerra, 2013 [91] | Brazil | Retrospective | Infectious | Only neonate | NICU | pRIFLE | 51 | 19 | In-hospital |
| Bradshaw, 2019 [98] | USA | Retrospective | Diarrheal illness | Neonate and non-neonate | PICU, NICU and ward | ICD-9-CM | 616 | 4 | in-hospital |
| Chen, 2023 [97] | Taiwan | Retrospective | Prematurity | Only neonate | NICU | mKDIGO | 204 | 55 | In-hospital |
| Coggins, 2021 [96] | USA | Retrospective | Sepsis | Only neonate | NICU | mKDIGO | 56 | 17 | In-hospital |
| Conroy, 2019 [95] | Uganda | Prospective | Malaria | Non-neonate | PICU | KDIGO | 168 | 20 | In-hospital and Post-discharge |
| Conroy, 2022 [94] | Uganda | retrospective | Blackwater fever + Malaria | Non-neonate | PICU and ward | KDIGO | 495 | 20 | In-hospital |
| Cui, 2022 [93] | China | Retrospective | Non-Cardiac surgery | Only neonate | NICU | KDIGO | 28 | 9 | In-hospital |
| Dang, 2022 [92] | China | Retrospective | Mixed | Non-neonate | PICU and ward | KDIGO | 419 | 30 | In-hospital |
| Deep, 2018 [90] | UK | Prospective | Septic shock | Non-neonate | PICU | KDIGO | 31 | 9 | In-hospital |
| Demiroz, 2024 [89] | Turkey | Retrospective | Liver transplant | Non-neonate | PICU and ward | KDIGO | 60 | 27 | In-hospital |
| Dos Santos El Halal, 2013 [88] | Brazil | Prospective | Cardiac surgery | Non-neonate | PICU | pRIFLE | 38 | 7 | In-hospital |
| Downes, 2017 [87] | USA | Retrospective | Antibiotic associated AKI | Non-neonate | PICU | KDIGO | 157 | 7 | In-hospital |
| Elgendy,2023 [85] | USA | retrospective | Diaphragmatic hernia | Only neonate | NICU | ICD9,10 | 445 | 239 | In-hospital |
| Elgendy, 2021 [84] | USA | Retrospective | LBW | Only neonate | NICU | NR | 19,603 | 6872 | In-hospital |
| Elgendy, 2024 [86] | USA | retrospective | Hypoxic-ischemic encephalopathy | Only neonate | NICU | ICD9,10 | 2719 | 786 | In-hospital |
| Esmaeili, 2024 [83] | IRAN | Retrospective | Cardiac surgery | Non-neonate | PICU | KDIGO | 58 | 16 | In-hospital |
| Fitzgerald, 2016 [82] | multinational | Prospective | Sepsis/Infectious | Non-neonate | PICU | KDIGO | 102 | 53 | In-hospital |
| Fleming, 2016 [81] | milticenter | Retrospective | ECMO | Neonate and non-neonate | PICU and NICU | KDIGO | 615 | 311 | In-hospital |
| Gil-Ruiz, 2014 [80] | Spain | Retrospective | Cardiac surgery | Non-neonate | PICU | pRIFLE | 107 | 16 | In-hospital |
| Hasson, 2024 [79] | USA | retrospective | Cardiac surgery | Only neonate | NICU | mKDIGO | 205 | 18 | In-hospital |
| Hessey, 2018 [78] | Canada | Retrospective | Non-Cardiac surgery | Non-neonate | PICU | KDIGO | 355 | 34 | Post-discharge |
| Hingorani, 2021 [77] | USA | Prospective | LBW | Only neonate | NICU | KDIGO | 350 | 45 | In-hospital |
| Hirabayashi, 2022 [76] | Japan | retrospective | Prematurity | Only neonate | NICU | nRIFLE | 47 | 12 | In-hospital |
| Hui, 2013 [75] | Hong Kong | Retrospective | Mixed | Non-neonate | PICU | pRIFLE | 71 | 16 | In-hospital |
| Iamwat, 2021 [74] | Thailand | Retrospective | ECMO | Neonate and non-neonate | PICU and NICU | KDIGO | 10 | 7 | In-hospital |
| Ibrahim, 2023 [73] | Nigeria | Retrospective | Malaria | Non-neonate | Mix | KDIGO | 237 | 19 | In-hospital |
| Imani, 2013 [72] | Uganda | Prospective | Infectious | Non-neonate | PICU | pRIFLE | 272 | 68 | In-hospital |
| Jetton, 2017 [71] | multinational | Retrospective | Mixed | Only neonate | NICU | KDIGO | 605 | 59 | In-hospital |
| Kaddourah, 2017 [70] | Asia, AU, EU, NA | Prospective | Mixed | Non-neonate | PICU | KDIGO | 1261 | 82 | In-hospital |
| Kari, 2017 [14] | Saudi Arabia | Prospective | Mixed | Non-neonate | PICU | KDIGO | 511 | 99 | In-hospital |
| Kasililika, 2020 [69] | Tanzania | Prospective | Mixed | Non-neonate | PICU | KDIGO | 53 | 19 | In-hospital |
| Khatana, 2023 [68] | USA | retrospective | Severe Sepsis | Non-neonate | not specified | ICD | 45,463 | 9005 | In-hospital |
| Kriplani, 2016 [67] | USA | Retrospective | Mixed | Non-neonate | PICU | KDIGO | 28 | 8 | In-hospital |
| Kuai, 2022 [17] | China | Prospective | Mixed | Non-neonate | PICU | KDIGO | 22 | 14 | In-hospital |
| Kuai, 2022 [66] | China | Prospective | Mixed | Non-neonate | PICU | KDIGO | 247 | 47 | In-hospital |
| Kumar Sethi, 2024 [65] | multinational | prospective | Continuous kidney replacement therapy | Non-neonate | PICU | KDIGO | 308 | 99 | In-hospital |
| Lazarovits, 2023 [64] | Israel | retrospective | Prematurity | Only neonate | NICU | NIDDK | 32 | 13 | In-hospital |
| Leow, 2022 [63] | Singapore | Retrospective | Acute respiratory distress syndrome | Non-neonate | PICU | KDIGO | 64 | 41 | In-hospital |
| Lobasso, 2021 [62] | USA | retrospective | Cardiac surgery | Neonate and non-neonate | PICU/NICU | KDIGO | 701 | 80 | In-hospital |
| Lu, 2022 [61] | China | retrospective | Cardiac surgery | Only neonate | CICU, NICU | KDIGO | 131 | 38 | In-hospital |
| Medar, 2015 [60] | USA | Retrospective | Heart failure | Non-neonate | Not specified | pRIFLE | 44 | 4 | In-hospital |
| Mengqi, 2020 [59] | China | Retrospective | Malignancy | Non-neonate | Not specified | KDIGO | 1657 | 90 | in-hospital |
| Moffett, 2022 [58] | USA | Retrospective | Mixed | Non-neonate | Not specified | KDIGO | 10,246 | 590 | In-hospital |
| Mohamed, 2023 [57] | USA | retrospective | Non-Cardiac surgery | Only neonate | NICU | ICD-9 and 10 | 2625 | 431 | In-hospital |
| Morgan, 2013 [56] | Canada | Prospective | Cardiac surgery | Only neonate | NICU | AKIN | 163 | 10 | Post-discharge |
| Murdeshwar, 2023 [55] | India | ambispective | Mixed | Non-neonate | PICU/Ward | ADQI | 200 | 37 | In-hospital |
| Nakwan, 2016 [54] | Thailand | Retrospective | Pulmonary hypertension | Only neonate | NICU |
A serum creatinine level of 41.5 mg/dL on two separate occasions at least 12 h apart, while maternal kidney function was normal |
31 | 22 | In-hospital |
| Namazzi, 2022 [53] | Uganda | Prospective | Malaria | Non-neonate | Not specified | KDIGO | 271 | 37 | In-hospital and Post-discharge |
| Özçakar, 2009 [52] | Turkey | Retrospective | Mixed | Non-neonate | Not specified | AKIN | 100 | 33 | In-hospital |
| Patel, 2023 [51] | USA | retrospective | Mixed | Neonate and non-neonate | PICU/NICU/ward | KDIGO | 528 | 138 | In-hospital |
| Pedersen, 2008 [50] | Denmark | Retrospective | Cardiac surgery | Neonate and non-neonate | PICU and NICU | need for dialysis after surgery | 130 | 26 | In-hospital |
| Pillon, 2019 [49] | Italy | Retrospective | Malignancy | Non-neonate | PICU | KDIGO | 17 | 12 | In-hospital |
| Piyaphanee, 2020 [48] | Thailand | Retrospective | Mixed | Non-neonate | PICU | KDIGO | 169 | 53 | in-hospital |
| Plumb, 2023 [47] | UK | retrospective | Mixed | Only neonate | NM | KDIGO | 712 | 59 | In-hospital |
| Plumb, 2023 [47] | UK | retrospective | Mixed | Non-neonate | NM | KDIGO | 4900 | 150 | In-hospital |
| Prodhan, 2012 [46] | USA | Retrospective | Trauma | Non-neonate | PICU | pRIFLE | 52 | 10 | In-hospital |
| Raina, 2022 [45] | USA | retrospective | Covid/infectious | Non-neonate | PICU | KDIGO | 274 | 21 | In-hospital |
| Raina, 2023 [44] | USA | retrospective | Mixed | Neonate and non-neonate | NM | ICD-10 | 2424 | 11 | In-hospital |
| Robinson, 2021 [43] | Canada | Retrospective | Mixed | Neonate and non-neonate | Not specified | ICD-9 and 10 | 1688 | 113 | Post-discharge |
| Rozmiarek, 2004 [42] | USA | Retrospective | Diaphragmatic hernia | Only neonate | NICU | NR | 14 | 10 | In-hospital |
| Sainathan, 2022 [41] | USA | Retrospective | LBW | Non-neonate | Not specified | ICD-10 | 98 | 8 | In-hospital |
| Sainathan, 2022 [41] | USA | Retrospective | Fontan Operation | Non-neonate | PICU and ward | NR | 97 | 8 | In-hospital |
| Sanchez-Pinto, 2015 [40] | USA | Retrospective | Mixed | Non-neonate | PICU | KDIGO | 974 | 246 | in-hospital |
| Schneider, 2010 [39] | USA | Retrospective | Mixed | Non-neonate | PICU | pRIFLE | 339 | 104 | In-hospital |
| Schueller, 2017 [38] | USA | Retrospective | ECMO | Only neonate | NICU | KDIGO | 15 | 7 | In-hospital |
| Selewski, 2014 [37] | USA | Retrospective | Mixed | Non-neonate | PICU and CICU | KDIGO | 737 | 83 | In-hospital |
| Selewski, 2023 [36] | multinational | prospective | mixed | Non-neonate | PICU | KDIGO | 1258 | 78 | In-hospital |
| Shalaby, 2018 [35] | Saudi Arabia | Prospective | Mixed | Only neonate | NICU | nKDIGO | 120 | 34 | In-hospital |
| Sharma, 2022 [34] | India | Retrospective | Covid/infectious | Non-neonate | Not specified | NR | 12 | 9 | In-hospital |
| Singh, 2022 [33] | India | Prospective | Mixed | Non-neonate | PICU | KDIGO | 44 | 14 | In-hospital |
| Slagle, 2021 [32] | USA | Prospective | Non-Cardiac surgery | Only neonate | NICU | mKDIGO | 33 | 8 | In-hospital |
| Smith, 2009 [31] | USA | Retrospective | ECMO | Neonate and non-neonate | PICU and NICU | pRIFLE | 32 | 23 | In-hospital |
| Srinivasan, 2018 [30] | USA | Retrospective | LBW | Only neonate | NICU | mAKIN | 89 | 25 | In-hospital |
| Stanski, 2023 [29] | USA | Prospective | Mixed | Non-neonate | PICU | KDIGO | 77 | 14 | In-hospital |
| Starr, 2020 [28] | USA | Prospective | septic shock | Non-neonate | PICU | KDIGO | 176 | 27 | In-hospital |
| Stojanović, 2017 [27] | Serbia | Retrospective | LBW | Only neonate | NICU | mAKIN | 57 | 35 | In-hospital |
| Umapathi, 2020 [26] | USA | Retrospective | Drowning | Non-neonate | PICU and ward | NR | 752 | 403 | In-hospital |
| Üstün, 2021 [25] | Turkey | Retrospective | LBW | Only neonate | NICU | KDIGO | 102 | 34 | In-hospital |
| Varadarajan, 2022 [24] | India | Prospective | Multisystem Inflammatory syndrome | Non-neonate | PICU and ward | KDIGO | 34 | 22 | In-hospital |
| Vincent, 2023 [23] | USA | Retrospective | Mixed | Only neonate | NICU | KDIGO | 100 | 14 | In-hospital |
| Wang, 2022 [22] | China | Retrospective | Metabolic Acidosis | Non-neonate | PICU and SICU (Surgical ICU) | pROCK | 181 | 22 | In-hospital |
| Wei, 2021 [21] | China | Retrospective | Mixed | Non-neonate | PICU | pROCK | 257 | 32 | In-hospital |
| Wingert, 2021 [20] | USA | Retrospective | Non-Cardiac surgery | Neonate and non-neonate | PICU, NICU and ward | KDIGO | 288 | 23 | in-hospital |
| Xu, 2018 [18] | China | Retrospective | Mixed | Non-neonate | PICU and ward | KDIGO | 19,908 | 842 | In-hospital |
| Xu, 2023 [19] | China | Retrospective | Mixed | Only neonate | NICU | Cys-C based criteria | 6336 | 96 | In-hospital |
| Zwiers, 2013 [16] | Netherlands | Prospective | ECMO | Only neonate | NICU | RIFLE | 153 | 43 | In-hospital |
ADQI: Acute Dialysis Quality Initiative; AKIN: Acute Kidney Injury Network; CICU: Cardiac Intensive Care Unit; Cys-C: Cystatin C; ECMO: Extracorporeal Membrane Oxygenation; ICD-9-CM: International Classification of Diseases, Ninth Revision, Clinical Modification; KDIGO: Kidney Disease: Improving Global Outcomes; LBW: Low Birth Weight; mAKIN: Modified Acute Kidney Injury Network; NICU: Neonatal Intensive Care Unit; NR: Not Reported; nKDIGO: Neonatal Kidney Disease: Improving Global Outcomes; PICU: Pediatric Intensive Care Unit; pRIFLE: Pediatric Risk, Injury, Failure, Loss, End-Stage Renal Disease; pROCK: Pediatric Reference Operative Check for Kidney Dysfunction; SICU: Surgical Intensive Care Unit
Among 101 observations, 13 reported AKI in children with prematurity-related outcomes, 14 with infections, 9 with cardiac surgery, 7 with non-cardiac surgery, 6 with sepsis/septic shock, 5 with ECMO, 33 with mixed conditions, and 14 with miscellaneous conditions. Twenty-seven of the studies were prospective. The geographical distribution of the studies was as follows: 49 from the Region of the Americas (AMR), 15 from the Western Pacific Region (WPR), 12 from the European Region (EUR), 8 from the African Region (AFR), 7 from the South-East Asia Region (SEAR), and 6 from the Eastern Mediterranean Region (EMR). The remaining studies were multinational. Thirty-eight studies included urine output in their AKI diagnostic criteria, and 33 studies enrolled exclusively neonates.
Risk of bias assessment
In the quality control section, it was noted that the majority of studies did not provide justification for the sample size (item 5). Moreover, the blinding status of the outcome observer was not a concern for causing bias since the outcome measured was mortality (item 12). The proportion of patients lost to follow-up could not be determined or was not reported in some studies (item 13). Most studies exhibited a low risk of bias in other domains (Table 2).
Table 2.
Risk of bias assessment by NHLBI tool in included studies
| Study | Item 1 | Item 2 | Item 3 | Item 4a | Item 4b | Item 5 | Item 6 | Item 7 | Item 8 | Item 9 | Item 10 | Item 11 | Item 12 | Item 13 | Item 14 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Adegboyega, 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Ahn, 2024 | Yes | Yes | CD | No | No | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Akcan-Arikan, 2007 | Yes | No | CD | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | NR | Yes |
| Al Gharabieh, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Algadeeb, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Al-Mouqdad, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Alobaidi, 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | NA | Yes | Yes |
| Alvarez-Hernandez, 2015 | Yes | Yes | CD | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Arruda Moraes, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Bakkaloglu, 2024 | Yes | Yes | CD | Yes | CD | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | NR | Yes |
| Basu, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Bauer, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Bradshaw, 2019 | Yes | Yes | Yes | Yes | CD | No | Yes | CD | NR | No | CD | Yes | NA | Yes | No |
| Chen, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Coggins, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Conroy, 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | NA | Yes | Yes |
| Conroy, 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | CD | Yes | NA | Yes | Yes |
| Cui, 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Dang, 2022 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Bezerra, 2013 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Deep, 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Demiroz, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Dos Santos El Halal, 2013 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Downes, 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Elgendy, 2024 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | NR | CD | CD | Yes | NA | Yes | Yes |
| Elgendy,2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | NR | CD | CD | Yes | NA | Yes | Yes |
| Elgendy, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | NR | CD | CD | Yes | NA | Yes | Yes |
| Esmaeili, 2024 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | CD | Yes | NA | Yes | Yes |
| Fitzgerald, 2016 | Yes | No | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes | NA | Yes | Yes |
| Fleming, 2016 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | NA | Yes | Yes |
| Gil-Ruiz, 2014 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Hasson, 2024 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Hessey, 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Hingorani, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Hirabayashi, 2022 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Yes | NA | Yes | Yes |
| Hui, 2013 | Yes | Yes | CD | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Iamwat, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Ibrahim, 2023 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | CD | Yes | NA | Yes | Yes |
| Imani, 2013 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | Yes | Yes | No | Yes | NA | Yes | Yes |
| Jetton, 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Kaddourah, 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes | NA | Yes | Yes |
| Kari, 2017 | Yes | Yes | CD | Yes | Yes | No | Yes | Yes | Yes | Yes | CD | Yes | NA | CD | Yes |
| Kasililika, 2020 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Khatana, 2023 | Yes | Yes | CD | Yes | Yes | No | Yes | CD | CD | CD | CD | Yes | NA | CD | Yes |
| Kriplani, 2016 | Yes | Yes | CD | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | CD | Yes |
| Kuai, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Kuai, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | Yes |
| Kumar Sethi, 2023 | Yes | Yes | CD | Yes | Yes | No | Yes | Yes | Yes | Yes | Yes | Yes | NA | CD | Yes |
| Leow, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Lobasso, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Lu, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Medar, 2015 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | No | Yes | NA | Yes | No | CD | Yes |
| Mengqi, 2020 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Moffett, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Mohamed, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | No | Yes | NA | Yes | No | CD | Yes |
| Morgan, 2013 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Murdeshwar, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Nakwan, 2016 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | Yes | Yes |
| Namazzi, 2022 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Özçakar, 2009 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | Yes | Yes | NA | Yes | No | CD | Yes |
| Patel, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Pedersen, 2008 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Pillon, 2019 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Piyaphanee, 2020 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | No | Yes |
| Plumb, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Prodhan, 2012 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | Yes | Yes | NA | Yes | No | CD | Yes |
| Raina, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Raina, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Robinson, 2021 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Yes | No | Yes | Yes |
| Rozmiarek, 2004 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | No | Yes | NA | Yes | No | CD | Yes |
| Sainathan, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Sanchez-Pinto, 2015 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Schneider, 2010 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Schueller, 2017 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | CD | No | Yes | NA | Yes | No | CD | Yes |
| Selewski, 2014 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Selewski, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Shalaby, 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | Yes | Yes |
| Sharma, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Singh, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Slagle, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | No | Yes | NA | Yes | No | Yes | Yes |
| Smith, 2009 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Srinivasan, 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Stanski, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | No | Yes |
| Starr, 2020 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | No | Yes |
| Stojanović, 2017 | Yes | Yes | Yes | Yes | Yes | No | Yes | CD | Yes | Yes | NA | Yes | No | CD | Yes |
| Umapathi, 2020 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Üstün, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | No | Yes |
| Varadarajan, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Vincent, 2023 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Wang, 2022 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
| Wei, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Wingert, 2021 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Xu, 2023 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | No | Yes | NA | Yes | No | CD | Yes |
| Xu, 2018 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | CD | Yes |
| Zwiers, 2013 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes | NA | Yes | No | Yes | Yes |
CD, cannot determine; NA, Not applicable; NR, not reported
Meta-analysis of the AKI-associated in-hospital and post-discharge mortality
Since the meta-analysis was conducted using a random-effects model, small studies (n < 100) were assigned weights comparable to larger studies (n ≥ 100), leading to a pronounced small-study effect (Supplementary Fig. 1). To provide more robust and generalizable estimates of AKI-associated mortality across diverse patient- and country-level characteristics, we excluded studies with fewer than 100 AKI patients in the main meta-analysis. For comparison, the pooled AKI-associated in-hospital mortality, including small studies (n < 100), is shown in Supplementary Fig. 2.
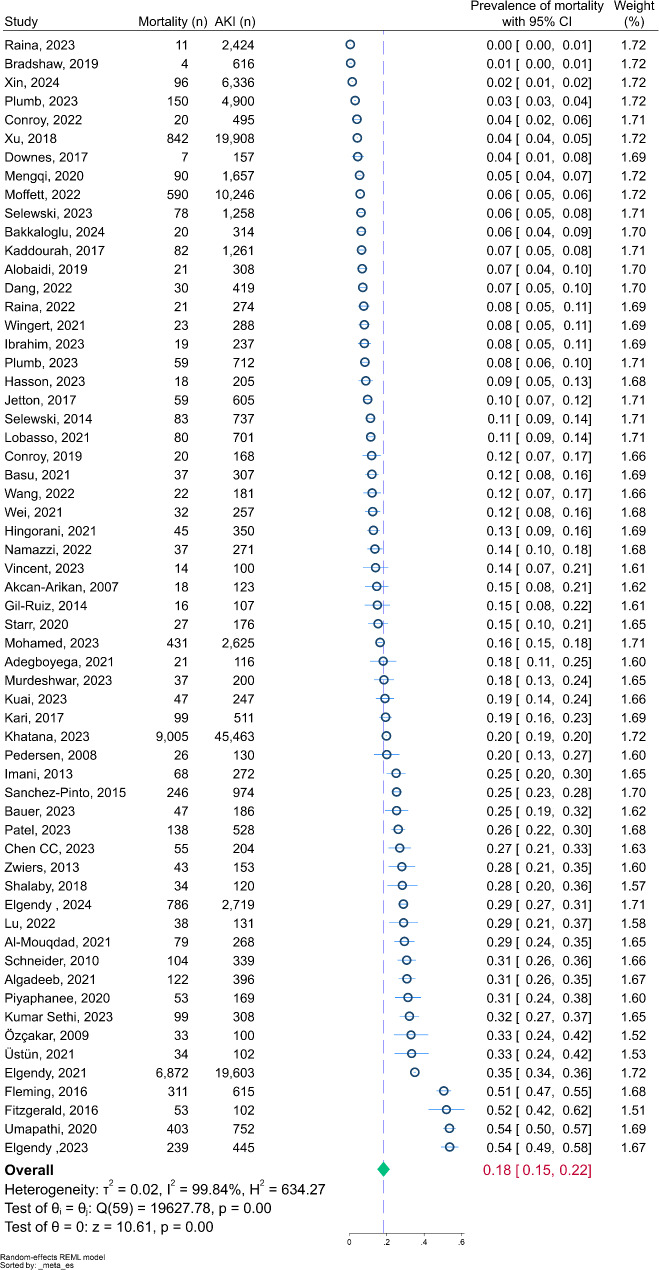
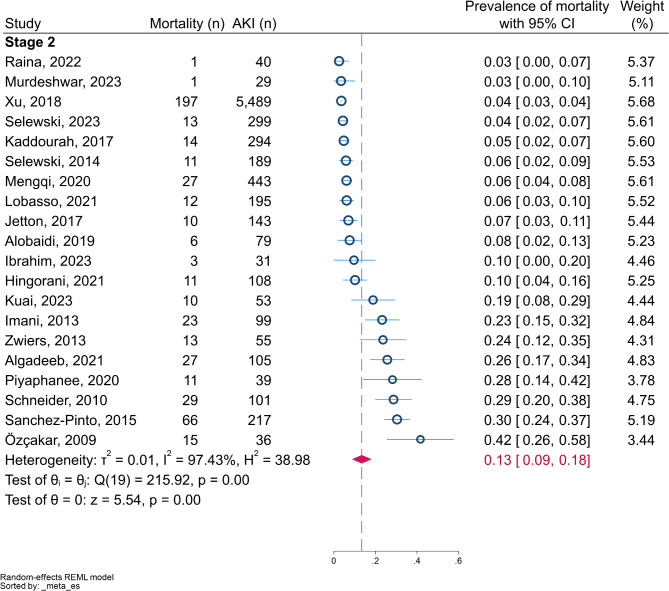
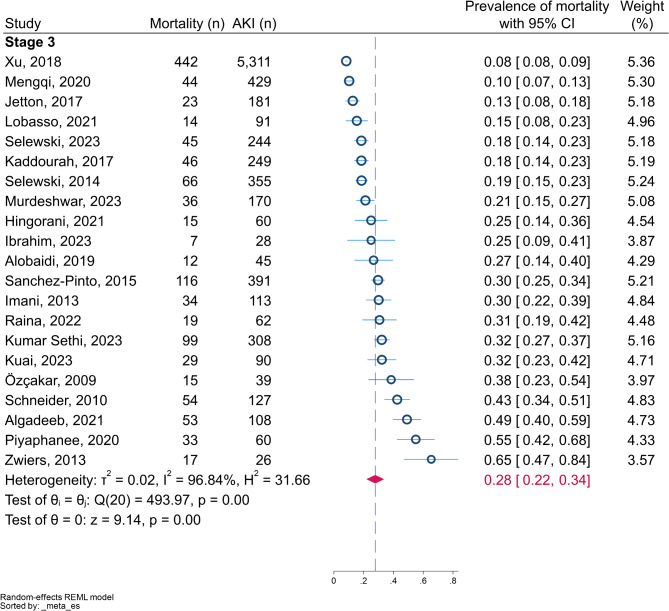
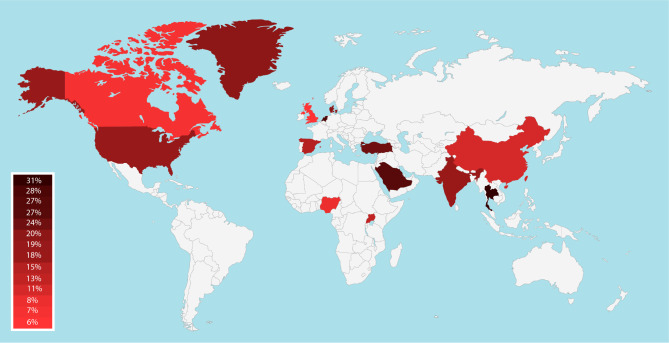
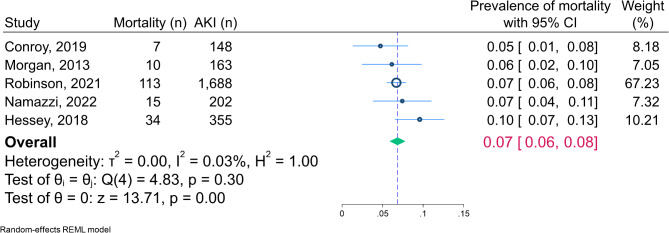
The pooled incidence of AKI-associated in-hospital mortality (60 studies, 133876 participants) was 18.27% (95% CI: 14.89, 21.65) (Fig. 2). Using a KDIGO-equivalent AKI definition, the pooled AKI-associated mortality rate among patients with AKI stage 1, stage 2, and stage 3 was 8.19% (95% CI: 5.65, 10.73), 13.44% (95% CI: 8.69, 18.19), and 27.78% (95% CI: 21.82, 33.74), respectively, as depicted in Figs. 3, 4 and 5. Some studies reported AKI in merged staging of 1 to 2, and 2 to 3. Pooled mortality in AKI stage 1 to 2 and AKI stage 2 to 3 was 12.54% (95% CI: 8.05, 17.02) and 23.50% (95% CI: 18.62, 28.39), respectively (Supplementary Figs. 3–4). We observed significant heterogeneity in the overall in-hospital mortality pooled estimate (I2 = 99.84%). Considering that we pooled data from studies with diverse sample sizes, clinical settings, and severities of AKI, some heterogeneity was expected. To explore potential sources of heterogeneity, we performed subgroup analyses and meta-regressions, as reported in Table 3. Compared to AKI stage 1, the mortality rate was significantly higher in AKI stage 3 (meta-regression coefficient = 0.19 [95% CI: 0.12, 0.25]; p < 0.001), and from AKI stage 2 to stage 3 (meta-regression coefficient = 0.15 [95% CI: 0.09, 0.20]; p < 0.001). The pooled mortality rates were 21.81% (95% CI: 16.84, 80.75) for neonates and 16.56% (95% CI: 12.37, 20.75) for older children. Thirty-nine studies used only a serum creatinine-based definition for AKI, reporting a pooled mortality rate of 18.19% (95% CI: 14.08, 22.30). In comparison, 18 studies using both urine output and serum creatinine-based criteria reported a mortality rate of 17.31% (95% CI: 11.96, 22.66). No differences in the pooled incidence of mortality were observed between prospective and retrospective studies, nor among different geographical regions or countries with different income levels (Fig. 6). AKI-associated mortality rates using KDIGO/mKDIGO and pRIFLE/RIFLE/nRIFLE criteria were 16.76% (95% CI: 13.01, 20.51) and 22.81% (95% CI: 17.46, 33.94), respectively. Meta-regression showed no significant difference (meta-regression coefficient = 0.06 [95% CI: -0.07, 0.19]; p = 0.634). The median sampling period was not significantly associated with the incidence of AKI-associated mortality (meta-regression coefficient = -0.007 [95% CI: -0.014, 0.0004]; p = 0.065). A meta-regression assessing the effects of GDP, its proportion spent on health, and maternal mortality rate (Supplementary Fig. 5) revealed no significant associations with AKI mortality rate (p = 0.491, p = 0.662, and p = 0.308, respectively). The pooled post-discharge mortality rate associated with AKI (from 5 studies including 2,556 participants) was 6.84% (95% CI: 5.86, 7.82) with a median follow-up ranging from 1 to 9 years, as shown in Fig. 7. Subgroup analyses and meta-regressions for all studies including the ones with less than 100 AKI patients are presented in Supplementary Table 1.
Fig. 2.
The forest plot for the incidence of in-hospital mortality among hospitalized children with acute kidney injury
Fig. 3.
The forest plot for the incidence of in-hospital mortality among hospitalized children with stage 1 acute kidney injury
Fig. 4.
The forest plot for the incidence of in-hospital mortality among hospitalized children with stage 2 acute kidney injury
Fig. 5.
The forest plot for the incidence of in-hospital mortality among hospitalized children with stage 3 acute kidney injury
Table 3.
Subgroup analysis and meta-regression for incidence of in-hospital AKI-associated mortality (excluding smaller studies with < 100 AKI patients)
| Subgroups | Studies (participants) | Incidence of mortality (%), (95 CI) | Heterogeneity (I²), P | Coefficient (95 CI) | Subgroup differences (P) | |
|---|---|---|---|---|---|---|
| Severity of AKI | ||||||
| AKI stage 1 | 26 (14843) | 8.19 (5.65, 10.73) | 97.8, < 0.001 | Reference | ||
| AKI stage 2 | 20 (8044) | 13.44 (8.69, 18.19) | 97.4, < 0.001 | 0.049 (-0.015, 0.113) | 0.136 | |
| AKI stage 3 | 21 (8487) | 27.78 (21.82, 33.74) | 96.8, < 0.001 | 0.187 (0.123, 0.252) | < 0.001 | |
| AKI stage 1 and 2 | 20 (21780) | 12.54 (8.05, 17.02) | 99.3, < 0.001 | 0.040 (-0.023, 0.104) | 0.211 | |
| AKI stage 2 and 3 | 28 (17040) | 23.50 (18.62, 28.39) | 98.2, < 0.001 | 0.146 (0.088, 0.205) | < 0.001 | |
| Age | ||||||
| < 1 month | 18 (35190) | 22.81 (16.84, 20.75) | 99.57, < 0.001 | Reference | ||
| > 1 month | 34 (93070) | 16.56 (12.37, 20.75) | 99.78, < 0.001 | -0.062 (-0.138, 0.013) | 0.107 | |
| Study design | ||||||
| Prospective study | 15 (5627) | 19.34 (13.66, 25.03) | 97.67, < 0.001 | Reference | ||
| Retrospective study | 44 (128049) | 17.88 (13.70, 22.07) | 99.90, < 0.001 | -0.016 (-0.096, 0.064) | 0.691 | |
| Country income classification (as per gross national income per capita) | ||||||
| Low income | 5 (1443) | 12.31 (5.44, 19.17) | 94.80, < 0.001 | Reference | ||
| Lower-middle income | 1 (200) | Insufficient data | Insufficient data | Insufficient data | Insufficient data | |
| Upper-middle income | 12 (29821) | 15.65 (8.87, 22.44) | 99.8, < 0.001 | 0.033 (-0.097, 0.163) | 0.623 | |
| High-income | 35 (97956) | 18.88 (14.56, 23.20) | 99.8, < 0.001 | 0.064 (-0.052, 0.181) | 0.279 | |
| Region | ||||||
| AFR | 5 (1443) | 12.31 (5.44, 19.17) | 94.8, < 0.001 | Reference | ||
| AMR | 28 (92635) | 18.66 (13.12, 24.20) | 99.9, < 0.001 | 0.062 (-0.060, 0.184) | 0.320 | |
| EMR | 4 (1295) | 26.69 (21.01, 32.37) | 80.3, < 0.001 | 0.145 (-0.025, 0.315) | 0.095 | |
| EUR | 8 (6518) | 17.77 (9.41, 26.13) | 98.5, < 0.001 | 0.054 (-0.090, 0.199) | 0.462 | |
| SEAR | 2 (369) | 24.73 (12.13, 37.33) | 87.7, < 0.001 | 0.124 (-0.089, 0.337) | 0.255 | |
| WPR | 9 (29340) | 12.64 (6.35, 18.94) | 99.8, < 0.001 | 0.004 (-0.137, 0.145) | 0.956 | |
| AKI criteria | ||||||
| KDIGO/mKDIGO | 40 (50717) | 16.76 (13.01, 20.51) | 99.6, < 0.001 | Reference | ||
| RIFLE/pRIFLE/nRIFLE | 5 (994) | 22.81 (16.28, 29.34) | 83.5, < 0.001 | 0.059 (-0.068, 0.186) | 0.364 | |
| AKIN/mAKIN | 1 (100) | Insufficient data | Insufficient data | Insufficient data | Insufficient data | |
| ICD-9/ICD-10 | 6 (54292) | 19.91 (4.05, 35.77) | 100.0, < 0.001 | 0.030 (-0.085, 0.145) | 0.610 | |
| Miscellaneous | 8 (27773) | 19.96 (8.15, 31.76) | 99.8, < 0.001 | 0.031 (-0.071, 0.134) | 0.549 | |
| AKI criteria based on | ||||||
| SCr | 39 (124124) | 18.19 (14.08, 22.30) | 99.9, < 0.001 | Reference | ||
| SCr + UOP | 18 (6376) | 17.31 (11.96, 22.66) | 98.0, < 0.001 | -0.008 (-0.079, 0.063) | 0.831 | |
| Predisposing condition | ||||||
| Prematurity-related outcomes | 6 (20643) | 25.88 (18.63, 33.13) | 94.9, < 0.001 | Reference | ||
| Sepsis/septic shock | 3 (45946) | 16.06 (11.21, 20.90) | 86.5, < 0.001 | -0.102 (-0.279, 0.076) | 0.262 | |
| Infections | 8 (2435) | 14.94 (4.02, 25.86) | 99.4, < 0.001 | -0.112 (-0.248, 0.024) | 0.108 | |
| Cardiac surgery | 5 (1274) | 16.27 (9.48, 23.06) | 90.0, < 0.001 | -0.093 (-0.246, 0.061) | 0.235 | |
| Non-cardiac surgery | 3 (3358) | 25.98 (-1.48, 53.44) | 99.6, < 0.001 | -0.001 (-0.178, 0.176) | 0.992 | |
| ECMO | 2 (768) | 39.54 (17.53, 61.55) | 96.6, < 0.001 | 0.137 (-0.069, 0.344) | 0.193 | |
| Mixed etiology | 25 (53178) | 14.61 (10.55, 18.67) | 99.8, < 0.001 | -0.112 (-0.227, 0.003) | 0.056 | |
| Miscellaneous a | 8 (6274) | 21.00 (9.03, 32.97) | 99.4, < 0.001 | -0.050 (-0.186, 0.086) | 0.475 | |
CI, confidence interval; AFR, African Region; AMR, Region of the Americas; EMR, Eastern Mediterranean Region; EUR, European Region; SEAR, South-East Asia Region; WHO, World Health Organization; WPR, Western Pacific Region; KDIGO, Kidney Disease: Improving Global Outcomes; mKDIGO, modified KDIGO; RIFLE, Risk, Injury, and Failure; and Loss; and End-stage kidney disease; pRIFLE, pediatric RIFLE; nRIFLE, neonatal RIFLE; AKIN, Acute Kidney Injury Network; mAKIN, modified AKIN; ICD, The International Classification of Diseases; SCr, serum creatinine; UOP, urine output; ECMO, extracorporeal membrane oxygenation
a Miscellaneous predisposing conditions include crush injury, hematopoietic cell transplantation, IV antibiotics, hypoxic-ischemic encephalopathy, continuous kidney replacement therapy, malignancy, drowning, and metabolic Acidosis
Fig. 6.
The map illustrates the incidence of acute kidney injury-associated mortality among hospitalized children across various countries
Fig. 7.
The forest plot depicting the incidence of post-discharge mortality among hospitalized children with acute kidney injury
Discussion
This meta-analysis, encompassing 60 studies and 133,876 hospitalized children with AKI, reveals a substantial global burden of mortality. The pooled in-hospital mortality rate was 18.27% (95% CI: 14.89, 21.65) among studies with at least 100 AKI patients, increasing from 8.19% in stage 1 to 27.78% in stage 3. Subgroup analyses showed no significant differences across geographical regions, income levels, or AKI definition criteria. Meta-regression analyses found no significant associations between AKI-associated mortality and factors such as GDP, healthcare expenditure, or maternal mortality ratio. The pooled post-discharge mortality rate was 6.84% (95% CI: 5.86, 7.82) in a 1–9-year follow-up period. These findings provide crucial insights into the global impact of pediatric AKI mortality and set the stage for discussing potential interventions and policy implications.
To our knowledge, this meta-analysis represents the most comprehensive systematic evaluation of AKI-associated mortality in the pediatric population to date. Our literature review revealed two prior meta-analyses. Notably, Susantitaphong et al.‘s study [109], which searched the Medline database for 2004–2012, included 11 studies employing a KDIGO-equivalent definition of AKI and found a pooled all-cause mortality rate of 13.8% (95% CI, 8.8 to 21.0). However, that analysis lacked studies from low and lower-middle-income countries, limiting its global generalizability. Our study addresses these limitations, providing a more inclusive and globally representative analysis of pediatric AKI mortality.
The second meta-analysis by Meena et al. [1] searched Medline, Embase, and Web of Sciences from March 2012 to January 2022. Analyzing 60 studies using KDIGO criteria and excluding neonates, they found a pooled AKI-associated all-cause hospital mortality of 11% (95% CI: 9–13). Like our study, they restricted analysis to studies with over 100 patients. However, their analysis was limited to studies using KDIGO criteria and excluded neonate patients, potentially limiting its scope and generalizability.
Our systematic review and meta-analysis demonstrate several key methodological strengths that address limitations of previous studies. First, the study rigorously addresses potential confounding factors by exclusively including studies that demonstrated an independent association between AKI and mortality through multivariate analysis. To mitigate the small study effect, the analysis focused on studies with over 100 patients. The comprehensive approach to assessing different AKI criteria, coupled with subgroup analyses, ensured the inclusion of all relevant studies and facilitated valuable comparisons. Notably, the inclusion of neonates and the subsequent age-based subgroup analysis allowed for a nuanced comparison of mortality incidence between neonates and older children, filling an important gap in the literature.
Our analysis demonstrates a clear association between AKI severity and mortality risk. The mortality rates increased progressively from stage 1 AKI to stage 3 AKI, highlighting the critical importance of early intervention to prevent AKI progression. This observation aligns with previous studies that have shown a correlation between AKI severity and adverse outcomes in both adult and pediatric populations [1, 106, 109, 110]. However, our findings highlight the limited availability of data on the utilization of renal replacement therapy (RRT) for severe AKI in pediatric populations. For example, the ASPIRE study reported a mortality rate of 32.1% in children with severe dialysis-dependent AKI, primarily treated with peritoneal dialysis [65]. Unfortunately, such data remain sparse, leaving a significant gap in understanding the specific role of RRT modalities in pediatric AKI mortality.
Our study found neonatal AKI-associated mortality of 21.81% (16.84 to 20.75%), lower than the 30% (27 to 33%) reported in Meena et al.‘s meta-analysis of neonates [111]. Both rates exceed those for pediatric patients older than one month. However, our meta-regression couldn’t establish a statistically significant difference in mortality between neonates and older pediatric patients. The high mortality in neonates with AKI likely reflects their vulnerability to severe illnesses and complications [111].
Our subgroup analyses showed no significant differences in mortality rates across geographical regions or income levels, contrasting with previous reports suggesting worse outcomes in low and middle-income countries [1, 112]. This indicates that AKI-associated mortality in children is a global challenge transcending economic boundaries, emphasizing the need for universal strategies. However, caution is warranted when interpreting results from low-income countries, as reliable epidemiological data on childhood AKI is scarce in these regions [112], and the population samples may be subject to selection bias.
The criteria for defining AKI have evolved from RIFLE to pRIFLE, AKIN, KDIGO, and mKDIGO (neonates). The main differences between these criteria lie in their measurement methods (creatinine, estimated clearance, or GFR), time frames (48 h or 7 days), and use of absolute or relative changes. While these differences can affect the detection of mild AKI cases, the criteria generally align well in identifying more severe cases [61, 106, 113]. Our analysis of different AKI classification systems (KDIGO/mKDIGO vs. pRIFLE/RIFLE/nRIFLE) showed no significant difference in reported mortality rates, supporting the comparability of these widely used classification systems in pediatric populations.
The similar mortality rates observed between studies using only serum creatinine-based AKI definitions (18.19%), and those incorporating both urine output and serum creatinine criteria (17.31%) suggest that serum creatinine alone may be a sufficient marker for identifying high-risk AKI cases in children.
Furthermore, our findings of a 6.84% (95% CI: 5.86, 7.82) post-discharge mortality rate align with Knappett et al.‘s meta-analysis, which reported a 4.4% (95% CI: 3.5–5.4%) six-month post-discharge mortality risk in low and low-middle Sociodemographic index (SDI) countries [114]. These results underscore the importance of long-term follow-up for children who have experienced AKI during hospitalization.
Limitations
This study has several limitations that should be considered when interpreting the results. Firstly, despite comprehensive subgroup analyses and meta-regressions, significant variability persisted among the included studies. This heterogeneity likely reflects differences in study populations, clinical settings, AKI definitions, and healthcare systems across countries. Secondly, limited data on post-discharge mortality restricted our ability to perform subgroup analyses and meta-regressions for this outcome, hindering a deeper understanding of long-term effects. Thirdly, our funnel plot analysis revealed asymmetry around the axis, raising potential concerns about publication bias. However, evidence suggests that conventional funnel plots may not accurately assess publication bias in proportional meta-analyses, as asymmetry can occur even in the absence of true bias [115, 116].
Additionally, by including only studies that reported an independent association between AKI and mortality, our analysis may have been biased toward studies involving higher mortality rates and/or sicker AKI cases. Our intention with this selection criteria was to ensure robust findings by focusing on studies that controlled for confounding variables, strengthening the causal interpretation of AKI-associated mortality. However, we acknowledge that this approach might inflate pooled estimates. Furthermore, while our study incorporated data from multiple countries, some regions—particularly low- and low-middle-income countries—were underrepresented. This underrepresentation limits the global generalizability of our findings and is particularly concerning given that mortality rates in these regions are likely higher.
Lastly, the inclusion of studies that demonstrated a statistical association between AKI and mortality, while methodologically robust, may have introduced selection bias toward studies with higher mortality rates or severe AKI cases. This approach ensures a focus on AKI-specific mortality but may not fully capture the broader spectrum of AKI-associated mortality. Future studies should address this gap by including a wider range of studies, regardless of statistical association, to provide a more comprehensive understanding of AKI-related mortality. Additionally, the heterogeneity in AKI etiologies, which often depend on the child’s or neonate’s age, adds complexity to interpreting the results. Future studies should aim to address these gaps by including diverse populations and systematically reporting long-term outcomes and regional disparities.
Conclusion
This comprehensive systematic review and meta-analysis provides valuable insights into the global incidence of acute kidney injury (AKI)-associated mortality in hospitalized children. Our findings demonstrate that AKI is independently associated with a substantial mortality rate of 18.27% among hospitalized children, with higher mortality rates observed in more severe stages of AKI. This underscores the critical nature of AKI as a significant health concern in pediatric populations worldwide and the crucial need for early detection and intervention strategies. Future research should focus on developing and validating risk prediction models, implementing targeted prevention strategies, and exploring long-term outcomes in pediatric AKI survivors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
Not applicable.
Author contributions
Study design and conceptualization: MY, MH, NA. Data gathering: HZ, AA, AA, AR, HT, SRD, NS, AD. Data analysis: HZ, MY. Interpretation of the results: HZ, AA, MY. Drafting the manuscript: HZ, AA. Revising, editing, and confirming the final version: All authors.
Funding
This research was funded by Tehran University of Medical Sciences (Grant number: 99-1-231-48274).
Data availability
The dataset generated and analyzed during the current study is available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mostafa Hosseini, Email: mhossein110@yahoo.com.
Mahmoud Yousefifard, Email: yousefifard20@gmail.com.
References
- 1.Meena J, Mathew G, Kumar J, Chanchlani R. Incidence of acute kidney injury in hospitalized children: A Meta-analysis. Pediatrics. 2023;151(2). [DOI] [PubMed]
- 2.Luo X, Jiang L, Du B, Wen Y, Wang M, Xi X. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care. 2014;18(4):R144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kaddourah A, Basu RK, Bagshaw SM, Goldstein SL. Epidemiology of acute kidney injury in critically ill children and young adults. N Engl J Med. 2017;376(1):11–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hessey E, Morissette G, Lacroix J, Perreault S, Samuel S, Dorais M, et al. Healthcare utilization after acute kidney injury in the pediatric intensive care unit. Clin J Am Soc Nephrol. 2018;13(5):685–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bhojani S, Stojanovic J, Melhem N, Maxwell H, Houtman P, Hall A, et al. The incidence of paediatric acute kidney injury identified using an AKI E-Alert algorithm in six english hospitals. Front Pediatr. 2020;8:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McGregor TL, Jones DP, Wang L, Danciu I, Bridges BC, Fleming GM, et al. Acute kidney injury incidence in noncritically ill hospitalized children, adolescents, and young adults: A retrospective observational study. Am J Kidney Dis. 2016;67(3):384–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sandokji I, Yamamoto Y, Biswas A, Arora T, Ugwuowo U, Simonov M, et al. A Time-Updated, parsimonious model to predict AKI in hospitalized children. J Am Soc Nephrol. 2020;31(6):1348–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang L, McGregor TL, Jones DP, Bridges BC, Fleming GM, Shirey-Rice J, et al. Electronic health record-based predictive models for acute kidney injury screening in pediatric inpatients. Pediatr Res. 2017;82(3):465–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 10.World Bank. WDI - GDP per capita (current US$) [Available from: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?name_desc=false
- 11.World Bank. WDI - Current health expenditure (% of GDP) [Available from: https://data.worldbank.org/indicator/SH.XPD.CHEX.GD.ZS
- 12.unicef -. Maternal mortality [Available from: https://data.unicef.org/topic/maternal-health/maternal-mortality/
- 13.National Institutes of Health. National Heart Lung aBI. Quality assessment tool for observational cohort and cross-sectional studies 2014 [Available from: https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools
- 14.Kari JA, Alhasan KA, Shalaby MA, Khathlan N, Safdar OY, Al Rezgan SA, et al. Outcome of pediatric acute kidney injury: a multicenter prospective cohort study. Pediatr Nephrol. 2018;33:335–40. [DOI] [PubMed] [Google Scholar]
- 15.Moraes LHA, Krebs VLJ, Koch VHK, Magalhães NAM, de Carvalho WB. Risk factors of acute kidney injury in very low birth weight infants in a tertiary neonatal intensive care unit. Jornal De Pediatria. 2023;99(3):235–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zwiers AJM, De Wildt SN, Hop WCJ, Dorresteijn EM, Gischler SJ, Tibboel D, et al. Acute kidney injury is a frequent complication in critically ill neonates receiving extracorporeal membrane oxygenation: a 14-year cohort study. Crit Care. 2013;17:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuai Y, Huang H, Dai X, Zhang Z, Bai Z, Chen J, et al. In PICU acute kidney injury stage 3 or mortality is associated with early excretion of urinary Renin. Pediatr Res. 2022;91(5):1149–55. [DOI] [PubMed] [Google Scholar]
- 18.Xu X, Nie S, Zhang A, Mao J, Liu H-P, Xia H, et al. Acute kidney injury among hospitalized children in China. Clin J Am Soc Nephrol. 2018;13(12):1791–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Xu X, Nie S, Xu H, Liu B, Weng J, Chen C, et al. Detecting neonatal AKI by serum Cystatin C. J Am Soc Nephrol. 2023;34(7):1253–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wingert T, Grogan T, Cannesson M, Sapru A, Ren W, Hofer I. Acute kidney injury and outcomes in children undergoing noncardiac surgery: a propensity-matched analysis. Anesth Analgesia. 2021;132(2):332–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wei C, Hongxia G, Hui F, Xianhui Q, Danqun J, Haipeng L. Impact of and risk factors for pediatric acute kidney injury defined by the pROCK criteria in a Chinese PICU population. Pediatr Res. 2021;89(6):1485–91. [DOI] [PubMed] [Google Scholar]
- 22.Wang H, Liang R, Liang T, Chen S, Zhang Y, Zhang L, et al. Effectiveness of sodium bicarbonate infusion on mortality in critically ill children with metabolic acidosis. Front Pharmacol. 2022;13:759247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vincent K, Rutledge A, Laney Z, Newman JC, Selewski DT, Steflik HJ. Recurrent neonatal acute kidney injury: incidence, predictors, and outcomes in the neonatal intensive care unit. J Perinatol. 2024;44(3):428–33. [DOI] [PubMed] [Google Scholar]
- 24.Varadarajan P, Elilarasi S, Solomon RS, Subramani S, Subramanian R, Rangabashyam N, et al. Multisystem inflammatory syndrome in children (MIS-C) associated with COVID-19–Single-Center experience. Indian Pediatr. 2023;60(5):389–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Üstün N. Incidence, risk factors, and adverse outcomes of acute kidney injury in very prematureneonates: a single center experience. Turk J Med Sci. 2021;51(5):2641–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Umapathi KK, Thavamani A, Dhanpalreddy H, Khatana J, Roy A. Incidence trends and predictors of in-hospital mortality in drowning in children and adolescents in the united States: a National inpatient database analysis. Clin Pediatr. 2020;59(2):134–41. [DOI] [PubMed] [Google Scholar]
- 27.Stojanović V, Barišić N, Radovanović T, Bjelica M, Milanović B, Doronjski A. Acute kidney injury in premature newborns—definition, etiology, and outcome. Pediatr Nephrol. 2017;32:1963–70. [DOI] [PubMed] [Google Scholar]
- 28.Starr MC, Banks R, Reeder RW, Fitzgerald JC, Pollack MM, Meert KL, et al. Severe acute kidney injury is associated with increased risk of death and new morbidity after pediatric septic shock. Pediatr Crit Care Med. 2020;21(9):e686–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Stanski NL, Krallman KA, Chima RS, Goldstein SL. A risk-stratified assessment of biomarker-based acute kidney injury phenotypes in children. Pediatr Res. 2023;93(5):1354–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Srinivasan N, Schwartz A, John E, Price R, Amin S. Acute kidney injury impairs postnatal renal adaptation and increases morbidity and mortality in very low-birth-weight infants. Am J Perinatol. 2018;35(01):039–47. [DOI] [PubMed] [Google Scholar]
- 31.Smith AH, Hardison DC, Worden CR, Fleming GM, Taylor MB. Acute renal failure during extracorporeal support in the pediatric cardiac patient. ASAIO J. 2009;55(4):412–6. [DOI] [PubMed] [Google Scholar]
- 32.Slagle CL, Goldstein SL, Gavigan HW, Rowe JA, Krallman KA, Kaplan HC, et al. Association between elevated urine neutrophil gelatinase-associated Lipocalin and postoperative acute kidney injury in neonates. J Pediatr. 2021;238:193–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh T, Mahajan V, Kaur J, D’Cruz S, Randev S, Guglani V, et al. Early diagnosis of kidney injury in a paediatric population: a prospective cohort study (E-DRIP STUDY). Pediatr Nephrol. 2022;37(11):2771–9. [DOI] [PubMed] [Google Scholar]
- 34.Sharma AG, Kumar V, Sodani R, Sapre A, Singh P, Saha A, et al. Predictors of mortality in children admitted with SARS-COV‐2 infection to a tertiary care hospital in North India. J Paediatr Child Health. 2022;58(3):432–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Shalaby MA, Sawan ZA, Nawawi E, Alsaedi S, Al-Wassia H, Kari JA. Incidence, risk factors, and outcome of neonatal acute kidney injury: a prospective cohort study. Pediatr Nephrol. 2018;33:1617–24. [DOI] [PubMed] [Google Scholar]
- 36.Selewski DT, Gist KM, Basu RK, Goldstein SL, Zappitelli M, Soranno DE, et al. Impact of the magnitude and timing of fluid overload on outcomes in critically ill children: a report from the multicenter international assessment of worldwide acute kidney injury, renal angina, and epidemiology (AWARE) study. Crit Care Med. 2023;51(5):606–18. [DOI] [PubMed] [Google Scholar]
- 37.Selewski DT, Cornell TT, Heung M, Troost JP, Ehrmann BJ, Lombel RM, et al. Validation of the KDIGO acute kidney injury criteria in a pediatric critical care population. Intensive Care Med. 2014;40:1481–8. [DOI] [PubMed] [Google Scholar]
- 38.Schueller M, Greenberg RG, Smith PB, Laughon MM, Clark RH, Hornik CP. In-hospital outcomes following extracorporeal membrane oxygenation in a retrospective cohort of infants. Am J Perinatol. 2017;34(13):1347–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Schneider J, Khemani R, Grushkin C, Bart R. Serum creatinine as stratified in the RIFLE score for acute kidney injury is associated with mortality and length of stay for children in the pediatric intensive care unit. Crit Care Med. 2010;38(3):933–9. [DOI] [PubMed] [Google Scholar]
- 40.Sanchez-Pinto LN, Goldstein SL, Schneider JB, Khemani RG. Association between progression and improvement of acute kidney injury and mortality in critically ill children. Pediatr Crit Care Med. 2015;16(8):703–10. [DOI] [PubMed] [Google Scholar]
- 41.Sainathan S, Agala CB, Said SM, Mulinari L, Sharma MS. National Fontan operation short-term outcomes at or below 2‐years‐of‐age compared to older than 2‐years‐of‐age. J Card Surg. 2022;37(6):1567–73. [DOI] [PubMed] [Google Scholar]
- 42.Rozmiarek AJ, Qureshi FG, Cassidy L, Ford HR, Hackam DJ. Factors influencing survival in newborns with congenital diaphragmatic hernia: the relative role of timing of surgery. J Pediatr Surg. 2004;39(6):821–4. [DOI] [PubMed] [Google Scholar]
- 43.Robinson CH, Jeyakumar N, Luo B, Wald R, Garg AX, Nash DM, et al. Long-term kidney outcomes following dialysis-treated childhood acute kidney injury: a population-based cohort study. J Am Soc Nephrol. 2021;32(8):2005–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Raina R, Sethi S, Aitharaju V, Vadhera A, Haq I. Epidemiology data on the cost and outcomes associated with pediatric acute kidney injury. Pediatr Res. 2023;94(4):1385–91. [DOI] [PubMed] [Google Scholar]
- 45.Raina R, Mawby I, Chakraborty R, Sethi SK, Mathur K, Mahesh S, et al. Acute kidney injury in COVID-19 pediatric patients in North America: analysis of the virtual pediatric systems data. PLoS ONE. 2022;17(4):e0266737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Prodhan P, McCage LS, Stroud MH, Gossett J, Garcia X, Bhutta AT, et al. Acute kidney injury is associated with increased in-hospital mortality in mechanically ventilated children with trauma. J Trauma Acute Care Surg. 2012;73(4):832–7. [DOI] [PubMed] [Google Scholar]
- 47.Plumb L, Casula A, Sinha MD, Inward CD, Marks SD, Medcalf J, et al. Epidemiology of childhood acute kidney injury in England using e-alerts. Clin Kidney J. 2023;16(8):1288–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Piyaphanee N, Chaiyaumporn S, Phumeetham S, Lomjansook K, Sumboonnanonda A. Acute kidney injury without previous renal disease in critical care unit. Pediatr Int. 2020;62(7):810–5. [DOI] [PubMed] [Google Scholar]
- 49.Pillon M, Sperotto F, Zattarin E, Cattelan M, Carraro E, Contin AE, et al. Predictors of mortality after admission to pediatric intensive care unit in oncohematologic patients without history of hematopoietic stem cell transplantation: A single-center experience. Pediatr Blood Cancer. 2019;66(10):e27892. [DOI] [PubMed] [Google Scholar]
- 50.Pedersen KR, Hjortdal VE, Christensen S, Pedersen J, Hjortholm K, Larsen SH, et al. Clinical outcome in children with acute renal failure treated with peritoneal dialysis after surgery for congenital heart disease. Kidney Int. 2008;73:S81–6. [DOI] [PubMed] [Google Scholar]
- 51.Patel M, Hornik C, Diamantidis C, Selewski DT, Gbadegesin R. Patient level factors increase risk of acute kidney disease in hospitalized children with acute kidney injury. Pediatr Nephrol. 2023;38(10):3465–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Özçakar ZB, Yalçınkaya F, Altas B, Ergün H, Kendirli T, Ateş C, et al. Application of the new classification criteria of the acute kidney injury network: a pilot study in a pediatric population. Pediatr Nephrol. 2009;24:1379–84. [DOI] [PubMed] [Google Scholar]
- 53.Namazzi R, Batte A, Opoka RO, Bangirana P, Schwaderer AL, Berrens Z et al. Acute kidney injury, persistent kidney disease, and post-discharge morbidity and mortality in severe malaria in children: a prospective cohort study. EClinicalMedicine. 2022;44. [DOI] [PMC free article] [PubMed]
- 54.Nakwan N, Pithaklimnuwong S. Acute kidney injury and pneumothorax are risk factors for mortality in persistent pulmonary hypertension of the newborn in Thai neonates. J Maternal-Fetal Neonatal Med. 2016;29(11):1741–6. [DOI] [PubMed] [Google Scholar]
- 55.Murdeshwar A, Krishnamurthy S, Parameswaran N, Rajappa M, Deepthi B, Krishnasamy S, et al. Etiology and outcomes of acute kidney disease in children: a cohort study. Clin Exp Nephrol. 2023;27(6):548–56. [DOI] [PubMed] [Google Scholar]
- 56.Morgan CJ, Zappitelli M, Robertson CMT, Alton GY, Sauve RS, Joffe AR, et al. Risk factors for and outcomes of acute kidney injury in neonates undergoing complex cardiac surgery. J Pediatr. 2013;162(1):120–7. [DOI] [PubMed] [Google Scholar]
- 57.Mohamed TH, Mpody C, Nafiu O. Perioperative neonatal acute kidney injury is common: risk factors for poor outcomes. Am J Perinatol. 2024;41(S 01):e2818–23. [DOI] [PubMed] [Google Scholar]
- 58.Moffett BS, Arikan AA. Trajectory of AKI in hospitalized pediatric patients—impact of duration and repeat events. Nephrol Dialysis Transplantation. 2022;37(8):1443–50. [DOI] [PubMed] [Google Scholar]
- 59.Xiong M, Wang L, Su L, Luo W, Li Y, Li L, et al. Acute kidney injury among hospitalized children with cancer. Pediatr Nephrol. 2021;36:171–9. [DOI] [PubMed] [Google Scholar]
- 60.Medar SS, Hsu DT, Lamour JM, Aydin SI. Acute kidney injury in pediatric acute decompensated heart failure. Pediatr Crit Care Med. 2015;16(6):535–41. [DOI] [PubMed] [Google Scholar]
- 61.Lu C, Lian J, Cao Z, Chen L, Liang J, Wang S. Comparing the pRIFLE, AKIN, KDIGO, and modified KDIGO criteria in neonates after cardiac surgery. Pediatr Nephrol. 2022:1–7. [DOI] [PubMed]
- 62.LoBasso M, Schneider J, Sanchez-Pinto LN, Del Castillo S, Kim G, Flynn A, et al. Acute kidney injury and kidney recovery after cardiopulmonary bypass in children. Pediatr Nephrol. 2022;37(3):659–65. [DOI] [PubMed] [Google Scholar]
- 63.Leow EH, Wong JJM, Mok YH, Hornik CP, Ng YH, Lee JH. Fluid overload in children with pediatric acute respiratory distress syndrome: A retrospective cohort study. Pediatr Pulmonol. 2022;57(1):300–7. [DOI] [PubMed] [Google Scholar]
- 64.Lazarovits G, Ofek Shlomai N, Kheir R, Bdolah Abram T, Eventov Friedman S, Volovelsky O. Acute kidney injury in very low birth weight infants: a major morbidity and mortality risk factor. Children. 2023;10(2):242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Sethi SK, Raina R, Sawan A, Asim S, Khant AK, Matnani M et al. Assessment of South Asian pediatric acute kidney injury: epidemiology and risk factors (ASPIRE)—a prospective study on severe dialysis dependent pediatric AKI. Pediatr Nephrol. 2024:1–10. [DOI] [PubMed]
- 66.Kuai Y, Li M, Chen J, Jiang Z, Bai Z, Huang H, et al. Comparison of diagnostic criteria for acute kidney injury in critically ill children: a multicenter cohort study. Crit Care. 2022;26(1):207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kriplani DS, Sethna CB, Leisman DE, Schneider JB. Acute kidney injury in neonates in the PICU. Pediatr Crit Care Med. 2016;17(4):e159–64. [DOI] [PubMed] [Google Scholar]
- 68.Khatana J, Thavamani A, Umapathi KK, Sankararaman S, Roy A. Increasing incidence of acute kidney injury in pediatric severe sepsis and related adverse hospital outcomes. Pediatr Nephrol. 2023;38(8):2809–15. [DOI] [PubMed] [Google Scholar]
- 69.Kasililika AG. Prevalence, risk factors and immediate outcome of acute kidney injury in critically ill children admitted at Benjamin Mkapa (BMH) and Dodoma regional referral hospitals (DRRH). 2020.
- 70.Jetton JG, Boohaker LJ, Sethi SK, Wazir S, Rohatgi S, Soranno DE, et al. Incidence and outcomes of neonatal acute kidney injury (AWAKEN): a multicentre, multinational, observational cohort study. Lancet Child Adolesc Health. 2017;1(3):184–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Imani PD, Odiit A, Hingorani SR, Weiss NS, Eddy AA. Acute kidney injury and its association with in-hospital mortality among children with acute infections. Pediatr Nephrol. 2013;28:2199–206. [DOI] [PubMed] [Google Scholar]
- 72.Ibrahim OR, Afolayan FM, Alao MA, Mohammed B, Suleiman BM, Adedoyin OT. Impact of methods of estimating baseline serum creatinine (bSCr) on the incidence and outcomes of acute kidney injury in childhood severe malaria. Egypt Pediatr Association Gaz. 2023;71(1):36. [Google Scholar]
- 73.Iamwat W, Samankatiwat P, Lertbunrian R, Anantasit N. Clinical characteristics and outcomes of children with extracorporeal membrane oxygenation in a developing country: an 11-year single-center experience. Front Pead. 2021;9:753708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hui WF, Chan WK, Miu TY. Acute kidney injury in the paediatric intensive care unit: identification by modified RIFLE criteria. Hong Kong Med J. 2013;19(1):13–9. [PubMed] [Google Scholar]
- 75.Hirabayashi M, Yamanouchi S, Akagawa S, Akagawa Y, Kino J, Fujishiro S, et al. Accuracy of diagnosing acute kidney injury by assessing urine output within the first week of life in extremely preterm infants. Clin Exp Nephrol. 2022;26(7):709–16. [DOI] [PubMed] [Google Scholar]
- 76.Hingorani S, Schmicker RH, Brophy PD, Heagerty PJ, Juul SE, Goldstein SL, et al. Severe acute kidney injury and mortality in extremely low gestational age neonates. Clin J Am Soc Nephrol. 2021;16(6):862–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Hessey E, Morissette G, Lacroix J, Perreault S, Samuel S, Dorais M, et al. Long-term mortality after acute kidney injury in the pediatric ICU. Hosp Pediatr. 2018;8(5):260–8. [DOI] [PubMed] [Google Scholar]
- 78.Hasson DC, Alten JA, Bertrandt RA, Zang H, Selewski DT, Reichle G, et al. Persistent acute kidney injury and fluid accumulation with outcomes after the Norwood procedure: report from NEPHRON. Pediatr Nephrol. 2024;39(5):1627–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Gil-Ruiz Gil-Esparza MA, Alcaraz Romero AJ, Romero Otero A, Gil Villanueva N, Sanavia Morán E et al. Rodríguez Sánchez de la Blanca A,. Prognostic relevance of early AKI according to pRIFLE criteria in children undergoing cardiac surgery. Pediatric nephrology. 2014;29:1265-72. [DOI] [PubMed]
- 80.Fleming GM, Sahay R, Zappitelli M, King E, Askenazi DJ, Bridges BC, et al. The incidence of acute kidney injury and its effect on neonatal and pediatric extracorporeal membrane oxygenation outcomes: a multicenter report from the kidney intervention during extracorporeal membrane oxygenation study group. Pediatr Crit Care Med. 2016;17(12):1157–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Fitzgerald JC, Basu RK, Akcan-Arikan A, Izquierdo LM, Olave BEP, Hassinger AB, et al. Acute kidney injury in pediatric severe sepsis: an independent risk factor for death and new disability. Crit Care Med. 2016;44(12):2241–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Esmaeili Z, Asgarian F, Aghaei Moghadam E, Khosravi A, Gharib B. Prevalence, risk factors, and outcomes of acute kidney injury in a pediatric cardiac intensive care unit: A cross-sectional study. Health Sci Rep. 2024;7(1):e1791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Elgendy MM, Othman HF, Younis M, Puthuraya S, Matar RB, Aly H. Trends and Racial disparities for acute kidney injury in premature infants: the US National database. Pediatr Nephrol. 2021;36:2789–95. [DOI] [PubMed] [Google Scholar]
- 84.Elgendy MM, Adisa A, Farghaly M, Ali M, Mohamed MA, Aly H. Acute kidney injury in infants diagnosed with congenital diaphragmatic hernia. Pediatr Res. 2023;94(3):1083–8. [DOI] [PubMed] [Google Scholar]
- 85.Elgendy MM, Cortez J, Saker F, Acun C, Matar RB, Mohamed MA, et al. Acute kidney injury in infants with hypoxic-ischemic encephalopathy. Pediatr Nephrol. 2024;39(4):1271–7. [DOI] [PubMed] [Google Scholar]
- 86.Downes KJ, Cowden C, Laskin BL, Huang Y-S, Gong W, Bryan M, et al. Association of acute kidney injury with concomitant Vancomycin and Piperacillin/tazobactam treatment among hospitalized children. JAMA Pediatr. 2017;171(12):e173219–e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.dos Halal SE, Carvalho MG. Acute kidney injury according to pediatric RIFLE criteria is associated with negative outcomes after heart surgery in children. Pediatr Nephrol. 2013;28:1307–14. [DOI] [PubMed] [Google Scholar]
- 88.Demiroz D, Colak YZ, Ozdes OO, Ucar M, Erdogan MA, Toprak HI, et al. Incidence and risk factors of acute kidney injury in pediatric liver transplant patients: A retrospective study. Indian J Crit Care Medicine: Peer-reviewed Official Publication Indian Soc Crit Care Med. 2024;28(1):75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Deep A, Sagar H, Goonasekera C, Karthikeyan P, Brierley J, Douiri A. Evolution of acute kidney injury and its association with systemic hemodynamics in children with fluid-refractory septic shock. Crit Care Med. 2018;46(7):e677–83. [DOI] [PubMed] [Google Scholar]
- 90.Bezerra CTM, Vaz Cunha LC, Libório AB. Defining reduced urine output in neonatal ICU: importance for mortality and acute kidney injury classification. Nephrol Dialysis Transplantation. 2013;28(4):901–9. [DOI] [PubMed] [Google Scholar]
- 91.Deng Y-H, Yan P, Zhang N-Y, Luo X-Q, Wang X-F, Duan S-B. Acute kidney disease in hospitalized pediatric patients with acute kidney injury in China. Front Pead. 2022;10:885055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Cui Y, Cao R, Deng L. Inadvertent hypothermia and acute kidney injury (AKI) in neonates undergoing Gastrointestinal surgeries: a retrospective study. J Perinatol. 2022;42(2):247–53. [DOI] [PubMed] [Google Scholar]
- 93.Conroy AL, Hawkes MT, Leligdowicz A, Mufumba I, Starr MC, Zhong K, et al. Blackwater fever and acute kidney injury in children hospitalized with an acute febrile illness: pathophysiology and prognostic significance. BMC Med. 2022;20(1):221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Conroy AL, Opoka RO, Bangirana P, Idro R, Ssenkusu JM, Datta D, et al. Acute kidney injury is associated with impaired cognition and chronic kidney disease in a prospective cohort of children with severe malaria. BMC Med. 2019;17:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Coggins SA, Laskin B, Harris MC, Grundmeier RW, Passarella M, McKenna KJ, et al. Acute kidney injury associated with late-onset neonatal sepsis: a matched cohort study. J Pediatr. 2021;231:185–92. [DOI] [PubMed] [Google Scholar]
- 96.Chen C-C, Chu C-H, Lin Y-C, Wang S-T, Huang C-C. Preceding risks and mortality outcomes of different neonatal acute kidney injury in preterm infants. Pediatr Res. 2023;94(4):1530–7. [DOI] [PubMed] [Google Scholar]
- 97.Bradshaw C, Han J, Chertow GM, Long J, Sutherland SM, Anand S. Acute kidney injury in children hospitalized with diarrheal illness in the united States. Hosp Pediatr. 2019;9(12):933–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Bauer A, Carlin K, Schwartz SM, Srikanthan M, Thakar M, Burroughs LM, et al. Risk factors for severe acute kidney injury after pediatric hematopoietic cell transplantation. Pediatr Nephrol. 2023;38(4):1365–72. [DOI] [PubMed] [Google Scholar]
- 99.Basu RK, Hackbarth R, Gillespie S, Akcan-Arikan A, Brophy P, Bagshaw S, et al. Clinical phenotypes of acute kidney injury are associated with unique outcomes in critically ill septic children. Pediatr Res. 2021;90(5):1031–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Bakkaloğlu SA, Delibaş A, Sürmeli Döven S, Taner S, Yavuz S, Erfidan G et al. Pediatric kidney care experience after the 2023 Türkiye earthquake. Nephrol Dialysis Transplantation. 2024:gfae033. [DOI] [PMC free article] [PubMed]
- 101.Alvarez-Hernandez G, Murillo-Benitez C, del Carmen Candia-Plata M, Moro M. Clinical profile and predictors of fatal Rocky mountain spotted fever in children from Sonora, Mexico. Pediatr Infect Dis J. 2015;34(2):125–30. [DOI] [PubMed] [Google Scholar]
- 102.Alobaidi R, Morgan C, Goldstein SL, Bagshaw SM. Population-based epidemiology and outcomes of acute kidney injury in critically ill children. Pediatr Crit Care Med. 2020;21(1):82–91. [DOI] [PubMed] [Google Scholar]
- 103.AlGadeeb K, Qaraqei M, Algadeeb R, Faqeehi H, Al-Matary A. Prediction of risk factors and outcomes of neonatal acute kidney injury. J Nephrol. 2021;34(5):1659–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Al-Mouqdad MM, Huseynova R, Khalil TM, Asfour YS, Asfour SS. Relationship between intraventricular hemorrhage and acute kidney injury in premature infants and its effect on neonatal mortality. Sci Rep. 2021;11(1):13262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Al Gharaibeh FN, Mohan S, Santoro MA, Slagle CL, Goldstein SL. Acute kidney injury and early fluid load in a retrospective cohort of neonatal sepsis. Pediatr Nephrol. 2023;38(6):1971–7. [DOI] [PubMed] [Google Scholar]
- 106.Akcan-Arikan A, Zappitelli M, Loftis LL, Washburn KK, Jefferson LS, Goldstein SL. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71(10):1028–35. [DOI] [PubMed] [Google Scholar]
- 107.Ahn HC, Frymoyer A, Boothroyd DB, Bonifacio S, Sutherland SM, Chock VY. Acute kidney injury in neonates with hypoxic ischemic encephalopathy based on serum creatinine decline compared to KDIGO criteria. Pediatr Nephrol. 2024:1–8. [DOI] [PubMed]
- 108.Adegboyega OO, Singh Y, Bhutada A, Kupferman JC, Rastogi S. Recurrent acute kidney injury in preterm neonates is common and associated with worse outcomes and higher mortality. Pediatr Res. 2022;92(1):284–90. [DOI] [PubMed] [Google Scholar]
- 109.Susantitaphong P, Cruz DN, Cerda J, Abulfaraj M, Alqahtani F, Koulouridis I, et al. World incidence of AKI: a meta-analysis. Clin J Am Soc Nephrol. 2013;8(9):1482–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Lafrance J-P, Miller DR. Acute kidney injury associates with increased long-term mortality. J Am Soc Nephrol. 2010;21(2):345–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Meena J, Kumar J, Kocharlakota JP, Gupta H, Mittal P, Kumar A et al. Acute kidney injury in neonates: A Meta-Analysis. Pediatrics. 2024:e2023065182. [DOI] [PubMed]
- 112.Macedo E, Cerdá J, Hingorani S, Hou J, Bagga A, Burdmann EA, et al. Recognition and management of acute kidney injury in children: the ISN 0by25 global snapshot study. PLoS ONE. 2018;13(5):e0196586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. workgroup A. Acute renal failure–definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Critical care. 2004;8:1–9. [DOI] [PMC free article] [PubMed]
- 114.Knappett M, Nguyen V, Chaudhry M, Trawin J, Kabakyenga J, Kumbakumba E et al. Pediatric post-discharge mortality in resource-poor countries: a systematic review and meta-analysis. EClinicalMedicine. 2024;67. [DOI] [PMC free article] [PubMed]
- 115.Doleman B, Freeman SC, Lund JN, Williams JP, Sutton AJ. Funnel plots May show asymmetry in the absence of publication bias with continuous outcomes dependent on baseline risk: presentation of a new publication bias test. Res Synthesis Methods. 2020;11(4):522–34. [DOI] [PubMed] [Google Scholar]
- 116.Hunter JP, Saratzis A, Sutton AJ, Boucher RH, Sayers RD, Bown MJ. In meta-analyses of proportion studies, funnel plots were found to be an inaccurate method of assessing publication bias. J Clin Epidemiol. 2014;67(8):897–903. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset generated and analyzed during the current study is available from the corresponding author upon reasonable request.