Abstract
Background
Life expectancy is a vital indicator of a country’s health and progress. Low-income countries face uncertainty regarding the long-term impact of the COVID-19 pandemic, driven by health expenditure levels, concerns over rising child mortality rates, and decreasing per capita income. These factors challenge life expectancy and demand urgent attention. This study aims to identify patterns, challenges, and opportunities to improve life expectancy in these countries through better health policies and resource allocation.
Methods
The research investigates the impact of the COVID-19 pandemic, health expenditure, per capita income, and child mortality rates on life expectancy in low-income countries. By examining 22 years of data from 20 countries, using a comprehensive dataset from the Our World in Data database, this study employs panel regression and time series analysis to explore how these factors influence life expectancy.
Results
The findings indicate a significant negative effect of COVID-19 on life expectancy, while health expenditure and per capita income show a positive impact. Conversely, child mortality rates exert a negative effect on life expectancy in low-income countries.
Conclusion
This research contributes to the existing body of knowledge by analysing how COVID-19, health expenditure, per capita income, and child mortality collectively affect life expectancy in low-income countries. The insights gained may inform policymakers and health consultants about the need for targeted interventions, prioritising healthcare investment and child health. By addressing these critical areas, it may be possible to improve life expectancy and overall health outcomes, thus contributing to global health equity.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-22109-4.
Keywords: Child Mortality Rate, COVID-19, Health Expenditure, Life Expectancy, Per capita income
Introduction
The COVID-19 outbreak brought an unprecedented global crisis, the loss of millions of lives, a shock to public health systems, and an economic and social disruption disproportionately affecting the most vulnerable. The pandemic has significantly impacted life expectancy (LE) across various income groups [1, 2].
LE represents the average number of years an individual is expected to live given current mortality rates. It is a crucial measure of a population’s health status influenced by factors such as healthcare quality, living conditions, and socio-economic development. LE serves as a standard for measuring the effectiveness of healthcare systems and policies and the more significant impact of factors such as health expenditure (HE), child mortality rates (CMR), per capita income (GDP) and exterior shocks such as pandemics on overall population well-being. The actual death toll caused by COVID-19 is believed to be considerably higher than that given by official statistics because of the limited testing capacities in poorly resourced countries and varying standards and policies in diagnosing and assigning deaths of COVID-19 internationally [3, 4]. Although COVID-19 is no longer a public health emergency. It is still a significant ongoing global health threat posing considerable challenges for humanity. Therefore, it is crucial to understand better the pandemic’s effects on mortality and the relevant patterns and changes over time.
Due to COVID-19, LE can be compared across two periods to compare mortality rates before the pandemic period (2000–2019) and the post-pandemic period (2020–2021) across countries [5, 6]. Existing research indicates that COVID-19 has led to a significant reduction in LE in many countries.
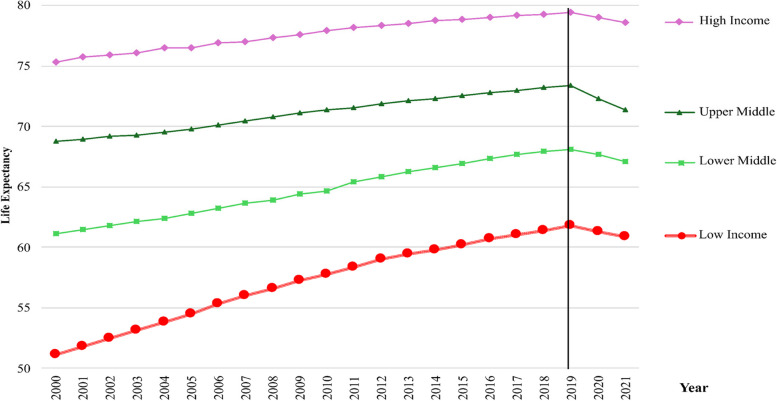
Figure 1 demonstrates the LE rates by the income classification, which was depicted from 2000 to 2021. However, with the onset of COVID-19, there was a decline in LE, especially after 2019. All the incomes shed weight, and the upper middle-income countries (UMICs) had a steeper drop [7]. This decline is due to the pandemic's health impact in these nations, which is far from ordinary, as seen in the following consequences. Lower middle-income countries (LMICs) also reported similar results, demonstrating that COVID-19 reduced LE across all income levels and increased existing gaps in health.
Fig. 1.
Life expectancy trends by income level. Four lines were identified life expectancy from 2000 to 2021. The red colour line with the dots indicates the low-income countries, the light green colour line with square shows lower-middle countries, the dark green colour line with triangles appears upper middle-income countries and the violet colour with diamonds illustrate high income countries. However, after 2019 all the income groups were decline. Source: Authors’ graphics based on World Bank data
High-income countries (HICs) typically exhibit robust healthcare systems, allowing effective responses to health crises like the COVID-19 pandemic [8, 9]. In these countries, increased HE often correlates with improved health outcomes, including higher LE and lower CMR.
In low-income countries (LICs), the situation is even more problematic. These nations face substantial challenges, including limited healthcare infrastructure, insufficient HE, a weak economy and high CMR. The COVID-19 pandemic has further strained their already weak health systems, leading to increased mortality, decreased GDP, and reduced LE [10–14]. Research indicates that LICs have a stronger correlation between HE and health outcomes and GDP, suggesting that even modest increases in spending can significantly impact CMR and LE [15–17]. Previous studies have shown how due to COVID-19, global LE has been extremely reduced in many countries [2, 7, 18, 19].
Figure 2 demonstrates the LE rates by the income classification and the female A and male B, which was depicted from 2000 to 2021. Therefore, this study aims to provide a proper understanding of data gathered from 2000 to 2021 in twenty countries. The research includes the formulation of precise research questions and research and policy interventions. It is the intention of the authors to make minor, though significant, improvements to this deficit in knowledge by identifying the major components of LE in LICs and through better understanding of COVID-19, HE, GDP, and CMR to help inform improved health policy decisions in the allocation of resources [20]. Even though COVID-19 cases continue to be reported, with 890 deaths in the last seven days in September 2024 [21]. This research remains crucial in filling the knowledge gap required to address the health-related challenges faced by LICs during the pandemic and in preparation for future shocks [9, 22–26].
Fig. 2.
Life expectancy trends by income level. Figure 2A shows the female life expectancy using four lines, that were identifies from 2000 to 2021. The red colour line with the dots indicates the low-income countries, the light green colour line with square shows lower-middle countries, the dark green colour line with triangles appears upper middle-income countries and the violet colour with diamonds illustrate high income countries. However, after 2019 all the income groups were decline. Figure 2B respectively shows the male life expectancy using four lines, that were identifies from 2000 to 2021. The red colour line with the dots indicates the low-income countries, the light green colour line with square shows lower-middle countries, the dark green colour line with triangles appears upper middle-income countries and the violet colour with diamonds illustrate high income countries. However, after 2019 all the income groups were decline. Source: Authors’ illustrations based on data
To achieve this, researchers utilised acclaimed electronic research databases such as Emerald Insight, Google Scholar, Science Direct, Wiley Online, PubMed, The BMJ and ResearchGate, ensuring a solid groundwork for the study.
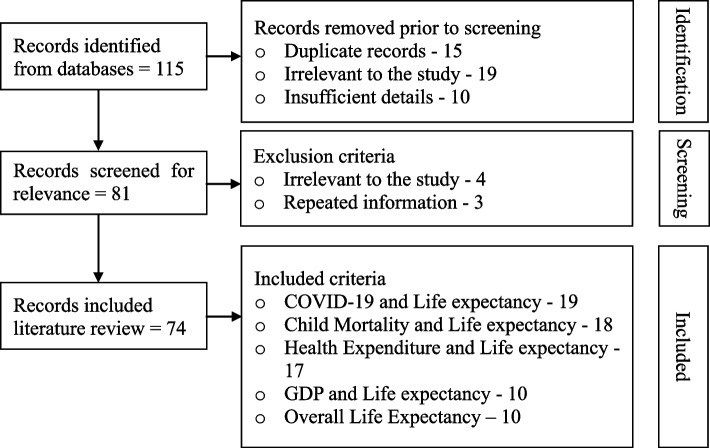
The search strategies identified full-text publications available online. The selection process involved examining both keywords (Child mortality rate and COVID-19 or Pandemic and Health expenditure, and GDP and Life expectancy) and titles to choose articles suitable for the study. Irrelevant articles were excluded, leading to a final selection of 74 articles for the current investigation (Fig. 3).
Fig. 3.
Literature search. The diagram indicates the PRISMA flow, showing the flow of information through the phases of the review. Source: Authors’ compilations
Figure 4 shows the number of research articles over time categorised by critical variables. The chart shows research directions predicting LE for 1998–2024 concerning COVID-19, CMR, HE, and GDP. There was an increased interest in research in the period 2020–2023 because of COVID-19, with most emphasis placed on it. The demise of children, the gross domestic product, and the health expenses continued to be priorities. This visualisation was done by using Python in doing the analysis and Canva when presenting the data.
Fig. 4.
Number of publications by year. This stacked bar chart displays the number of publications from 1998 to 2024 related to each independent variable in relation to the dependent variable. The green colour represents COVID-19 and life expectancy, the yellow colour represents child mortality and life expectancy, the blue colour represents health expenditure and life expectancy, the brown colour represents GDP and life expectancy, and the pink colour represents overall life expectancy with multi-independent variables relationships. Source: Authors’ compilations
Past research in this area does not mostly highlight COVID-19, CMR, GDP, and HE's impact on the LE from COVID-19 together [27, 28]. These factors differ based on the LICs’ usage of LE. The proposed research framework addresses measuring the effects of COVID-19, GDP, HE, and CMR on LE in LICs.
The onset of the COVID-19 pandemic has rapidly changed the LE, CMR, GDP, and HE. Early reports from the onset of COVID-19 show that overall HE, GDP, and CMR with LE in the LICs decreased [29–31]. COVID-19 is a world-shattering step in the history of health and global crises that affected almost all nations globally, especially the LICs, where the interaction between health spending, pandemic response, and CMR with LE has established a significant impact on the health systems [32]. This research paper offers a critical evaluation of the existing literature on these related factors, including the gaps and relevant links for future research.
Considered the effects of other variables with LICs or discussed the policy implications of building future health systems in the wake of pandemics [33, 34]. This points to the fact that little is known regarding the effects of the pandemic in the long run in LICs, as most prior studies have presented short-run models and omitted possibly influential variables. Thus, the challenges in the analysis of income group differences and the future health system policies continue to pose research questions.
Power BI, Canva, and Photoshop were used to create the map in Fig. 5. It gives an overall view of what affects the lifespan of an individual. The first set of pie charts as mentioned earlier looks at the correlation between overall life expectancy, healthcare spending, GDP, child mortality, and COVID-19 effects. As for the countries that published most of the articles, the leaders are the United States, the United Kingdom, and China regarding the excellence of the research. On the other hand, low publication rates are recorded for countries that present few data such as, Chad, Somalia, and Yemen. It also underlines COVID-19’s impact throughout the world and healthcare and socio-economic contributions to differences in life span.
Fig. 5.
Number of publications by research country context. The number of publications relevant to each country is shown in this figure using lines and a pie chart. The black line ending with a red dot highlights countries with publications, while the corresponding pie chart displays article counts. In the pie chart, the green colour represents COVID-19 and life expectancy, the yellow colour represents child mortality and life expectancy, the blue colour represents health expenditure and life expectancy, the brown colour represents GDP and life expectancy, and the pink colour represents overall life expectancy, reflecting relationships with multiple independent variables. Source: Authors’ compilations
COVID-19 and life expectancy
The COVID-19 pandemic led to a reduction in LE in some countries [7]. In 2021, LE fluctuated, with some regions, like Eastern Europe and the U.S., stabilising losses while others faced further declines [35, 36]. This clearly shows the differences that exist in the effects that COVID-19 brought about by geographical and socio-economic differences [6, 37]. Denmark and Australia observed an increase in LE rates in 2020, based on the decrease in the mortality rates other than COVID-19 [1, 38]. The differences in the impact of COVID-19 on LE by region and socioeconomic status since the mortality of children did not increase.
Besides, it did not affect all people similarly. For example, mortality increased significantly during 2020, thereby having a significant role in reducing LE at birth [39–41]. On the other hand, the CMR shows the ability to maintain the levels and report lower deaths of children below five years of age during the pandemic [39, 42, 43]. These studies show that COVID-19 affects people in different ways since the mortality of children did not increase even though adult mortality increased during the pandemic.
The health systems have been exposed to COVID-19 disruptions as inequity in necessary health care leads to higher mortality [21]. Pointed out that global estimated deaths that are directly or indirectly linked with COVID-19 were around 14.9 million in the year 2024, which was higher than the recorded number [44]. These high death rates are the leading causes of the reduction in LE that has been observed to occur at the population level.
While the COVID-19 pandemic has affected the global LE of all people, it is essential to mention that the impact differs, depending on the specific region, vaccinations, and standard demographic indicators [43]. It was established that the CMR had raised an unprecedented level due to COVID-19, and LE reductions were recorded in 29 countries, including the United States and countries in Eastern Europe, which had persisting mortality deficits [45]. Some countries that submitted data had higher vaccination rates and thus had a better record of LE loss, which clearly exhibited the link between vaccination and mortality data [46]. This critical literature establishes the relationship between vaccination and decrease in mortality while presenting countries with better LE and comparing it to COVID-19’s impact on CMR.
Although much research has shown how the COVID-19 pandemic has affected LE in different areas and socioeconomic categories, much research still needs to be undertaken to fully understand the long-term repercussions of these changes. To lessen the long-term effects of such global health crises, future research must examine how health systems' resilience and adaptability may be strengthened, making sure that all populations are better prepared to face comparable difficulties in the future.
Child mortality and life expectancy
According to the literature, studies show that during the COVID-19 period, there has been a raised CMR [47]. This is significant since it plays an important role in determining LE in most populations [48]. High incidences of infant and CMR mean that children are likely to die younger if they are born in such societies, a mirage of bigger social injustice and health inequalities [49]. This part explains the high CMR during these pandemics with LE while bringing out existing social inequality and health disparities that affect societies.
Researchers have analysed the change in average LE that has not considered the huge enhancements in CMR. CMR refers to the probability that a child will die before five years of age [30]. This means that there is a diffusion and an increase of 27 years in the average time that patients take before receiving a malaria diagnosis [30, 50].
Among the studied five LMICs and based on similar reports, the conforming investigations pointed to the COVID-19 control leading to a 22% increase in infant mortality and a 27% rise in neonatal mortality. At the same time, the restrictions of utilisation in health care services were identified as critical predictors of these adverse outcomes [51, 52]. Another study estimated that there were 113,962 additional child mortalities under five years because of cuts in essential health services in the pandemic [52]. This part declares that COVID-19 raised the child and newborn mortality rate in LMICs where health care utilisation was limited.
However, due to the pandemic, there will be substantial indirect CMR due to economic constraints [52]. That is why the literature notes the impact of the pandemic on essential health services, including immunisation and maternal care, which are very important in children’s survival [9, 53]. Some of these shortcomings include the absence of disaggregated data for national levels and death data that exclude or underestimate LICs’ [53, 54]. Lack of sample breakdown and proper mortality statistics thus calls for more concentrated research and intervention to help enhance children’s survival rights in such areas.
Disruptions from COVID-19 are projected to cause an additional 9.3 million children to suffer from wasting and 2.6 million from stunting, potentially leading to significant future productivity losses [55]. Some articles show a CMR that differs from one population group to another among tribes in India, where a CMR of 124 per 1000 live births has been registered [47]. High CMR reduces LE, and very often, it is lower than LE at one year of age [56]. This shows that even in the future, it is hard to determine the CMR increases and effects of such a level, but the study confirms that different population groups have considerably different CMR and that high CMR could be an example of a decrease in LE.
CMR has reduced across the globe with a 44% reduction for children between the ages of 0–5 in the year 2003 as compared to the year 1980 [57]. The death causes in LMICs among children 5–14 years are enteric infections and unintentional injuries whose elimination could add 0.085 years to a lifetime [58]. However, these predictions assume content healthcare delivers across LICs, which is unrealistic [59]. This aspect is important because it points at global progress in the decline of CMR. However, a prediction based on constant healthcare delivery in LMICs is untenable and thus lowers the expectations of LE.
But these predictions are built on expectations that HE delivery and access to appropriate foods will remain constant in all the various environments of LICs, which is unrealistic [60]. In the same time, disruptions in the health system, as well as issues with access to food, are highlighted to have contributed to the increase in maternal deaths as well as deaths of children under five years, without due consideration accorded to the variations in the health services in the local settings, which could impact such outcomes [50, 52]. Despite overall advancements in child health, there have been persisting disparities and specific causes of death that have called into question the gains in LE, therefore urging for more interventions. It has been brought out that expectations on the health outcome predictions do not consider variations and shocks to health care and food by demonstrating how CMR and LE gains have been impacted.
Future studies should concentrate on the relationship between food security, CMR, and healthcare interruptions, especially in LICs, where data is frequently lacking or overestimated. To develop more effective interventions and raise child survival rates and LE predictions in groups that are already at risk, it will be imperative to close these knowledge gaps.
Health expenditure and life expectancy
While HE plays a critical role in the LE. There is nothing as significant when it comes to the research on the effects of HE on COVID-19, CMR, and LE. HE has been proven to have reduced the mortality rate of the people in the LICs. Investment in health systems is important in combating a pandemic [44]. But this assertion brings out a few issues regarding health investment in LICs where budget constraints and resource direction compasses will limit the benefits of increased spending [61, 62]. This is in harmony with the significance of health investment in the current efforts to decrease mortality and increase LE.
The effect of COVID-19 and LE adds to the global realisation of how these diseases shape COVID-19 and LE, given the burden of such diseases, especially in countries like India. There is a need to ensure that health spending is well understood for such illnesses [63]. The positive correlation studies suggest that HE increases LE by promoting healthy spending in various contexts. African nations and those in the European Union [28, 64].This work notes that improved economic expenditures in health lead to a better LE among different regions.
However, factors such as government effectiveness can impact this relationship, hence decreasing LE even as the HE is increased [28, 65]. But pollution with ecological factors reduces the efficacy of increased health spending, a factor that implies the decremental effect of externalities on the health outputs [66, 67]. The costs of environmental degradation negate the gains from healthcare expenditure, highlighting the importance of the relationship between health and environmental measures [68]. From this part, it is evident that enhanced HE enhances LE, other factors, such as government efficiency and ecological degradation, can offset all these gains, thus the need for health and environmental policies.
The overall decrease in the provision and quality of healthcare during the COVID-19 pandemic reveals the weaknesses of HE in LICs. It makes it essential to understand better how health spending leads to better health [69]. In the United States, technological innovation and insurance generosity have fuelled HE, but those forces on their own do not necessarily generate improved health [70].
As can be seen, familiarity with such dynamics is essential in managing public health concerns. This includes the government's capability to manage HE, also known as efficiency [71]. In some of the contexts, poor governance contributes to a situation where increased spending does not enhance the LE of the population [28]. This needs to examine the HE in the growth effects of environmental issues and policy efficacy, which states that the incompetence of policy could negate the positive effects of enhanced health spending.
There is a clear distinction in health funding as well as health status when high-focus and non-high-focus states are analysed in India [72]. States with low levels of health care and literacy rates, with corresponding low levels of HE, also pose a problem for solutions relating to equitable health-based development. Worse still is the high out of pocket expenditure and poor investment in the relevant health infrastructure by the government section. The subsequent sections investigate the main concerns related to this problem [73–75].
There is a noticeable relationship between HE and LE, with several factors playing a vast role. In our analysis, although higher HE was associated with better living standards, some ailment types may negatively affect the longevity of a given population [76]. HE is vital for the improvement of the health of the public, but this depends on dealing with the environmental factors and increasing government efficiency. This complexity indicates that even though it may be possible to improve health budgets to increase LE sufficiently. This may not be enough without significant policy changes [77]. This part underlines that raising HE always leads to improving living standards. However, raising LE significantly is possible only through the consideration of the environmental factors and the improvement of policy effectiveness rather than through the increase in the budget only.
Even though the relationship between HE and LE has been the subject of much research, there is still a significant knowledge gap regarding how environmental degradation, government efficiency, and policy efficacy interact with health spending to affect LE, especially in LICs. Future studies should examine these relationships to offer a more thorough strategy for enhancing LE through healthcare spending.
GDP and life expectancy
The LE and per capita GDP of LICs are neither simple nor basic for development impacts on health. Studies show that there is an increase in LE, with an increase in per head income, meaning that economic improvement will improve health standards [78]. On the other hand, these levels differ about the relationship between GDP and LE, with significant differences in expectations in low-income countries [79–81].
On the positive relationship between GDP and LE, for the one-year increase in an increment of three hundred and fifteen dollars is expected to be achieved once the GDP in low income countries reaches five thousand [82, 83]. Since economic growth encourages spending in health care, education and infrastructure which are important determinants of health status [84]. Health is influenced most by per capita GDP; the aspect has a direct effect on the life span and survival rates among the [85] population. The observed influence of the Gini coefficient testifies to the fact that economic development is insufficient since eradicating inequality remains a significant precondition for enhancing the subject’s health among LICs [86–88]. Different from communicable diseases, infectious diseases are perennial health threats that can suppress the impact of economic development on life period [89].
Despite its importance for international comparative data, economic growth is not the key to an increase in life expectancy. It is, therefore, important to introduce orientation changes at the population level towards broader aspects of health determinants and inequalities.
Overall life expectancy
COVID-19 has especially affected health spending and CMR, leading to affecting LE in LICs [52]. The results concerning the impact of COVID-19 on LE are worrying, especially in terms of indirect effects. Nevertheless, low COVID-19 lethal fatality trends in some LICs, rising CMR, and disruption of HE that endanger improvements in LE can be distinguished [90, 91]. That is an indication that while the proportion of children succumbing to COVID-19 is less, the death rates could be more profound in LICs and LMICs than HICs [32, 92]. This critical section highlights the contradiction addressing the increase of LE in the LICs, which implies that even with low mortality rates. It is necessary to employ data and methods focusing on specific child and health issues.
On the other hand, it would not have considered the socio-economic determinants of those disparities. One gross example from India is the fact that actual LE at birth reduced by 2.6 years from 2019 to 2020, which also coincided with a reduction of 17% in mortality during the pandemic months, can be distinguished [69]. A comprehensive analysis must also consider socioeconomic factors and particular circumstances, such as India's lower LE and shifting mortality rates.
In LICs, about 112 child deaths per thousand births occur before the child reaches the age of five as compared to 8 developed countries, which shows that there is a significant effect on LE [93]. Eliminating leading causes of CMR, such as enteric infections and malaria, could increase LE for children between ages 5–14, and we can predict 0–5 child mortality. However, one question that has not been answered is whether those interventions are feasible in the LICs and LMICs [58]. This point shows significant differences, in and casts doubt on the viability of eradicating primary causes of death, casting doubt on the efficacy of health care interventions in LICs.
However, this study finding suggests a need to explore further the moderating factors that exist in the two contexts as related to governance, healthcare infrastructure, and socio-economic environments, as proposed [94]. This point highlights the need for additional study into moderating factors like governance and socioeconomic conditions while also showing a favourable relationship between HE and LE, particularly in LICs.
Although there are existing studies on COVID-19’s effects on the health front in LICs, some areas remain relatively unexplored, particularly regarding HE, COVID-19, and CMR. Also, COVID-19 effects are not mentioned in using these variables [52]. These findings are still relatively broad and do not have the depth needed for policy interventions or understanding an individual’s choice-making mechanisms. Thus, our further research will address these gaps based on the longitudinal analysis of context specific case studies, including the investigation of the effect of comorbidities as well as the proposed policy recommendations that may regard the problems of LICs during the pandemic period.
Moreover, it is essential to fill these gaps to improve the understanding of the effects of the pandemic as well as to identify measures for the development of strengthened health systems that have the capacity to withstand future shocks [95]. This point highlights the necessity of assessing the effectiveness of health spending, especially for the mortality of children under five years, to create health agendas that are effective and to build resilient systems that can resist shocks in the future.
Higher value of the GDP is linked with lower CMR. For instance, the correlation of economic expansion of renewable energy use and under-5 mortality rate is far lower in the countries [96]. It was also established that in South Asia, per capita GDP and the level of urbanisation reduce the rate of child mortality. However, factors like high fertility rates and environmental degradation were found to increase child mortality [97]. With economic well-being losses that totalled $3.57 trillion, racial groups were not spared by COVID-19 [23].The negative effects of COVID-19 on health care access and lockdowns has been attributed to reduced LE [98].
Despite the body of research on the subject, there are still many unanswered questions about how COVID-19 affects health spending, LE, and CMR in LICs. Future investigations should concentrate on context-specific assessments that consider the socioeconomic circumstances and health infrastructure in LICs, as well as longitudinal studies that look at the pandemic's long-term consequences on healthcare systems and LE.
The study's contribution to the existing body of knowledge comes in four primary ways. First, its significance is important since it explores the combined effects of COVID-19, HE, GDP, and CMR on LE. This area has not been thoroughly investigated in extant literature. While previous research has examined the individual impacts of these variables, the linkage connection of all three factors provides a more comprehensive understanding of their collective influence on LE.
Second, to identify the impact of the COVID-19 pandemic, HE, GDP, and CMR on LE in LICs, from 2000 to 2021 in twenty countries. This comprehensive analysis aims to uncover the interconnections among these variables during a critical period.
Third, a quantitative approach has been used to analyse the impacts of the COVID-19 pandemic, HE, GDP, and CMR on LE in LICs [9, 23–26]. By utilising the time series analysis, the study aims to identify trends and variations in LE, revealing how these factors interact over time and the specific challenges faced by LICs before and after the COVID-19 crisis. This methodological framework allows for an intense examination of the direct and indirect effects of COVID-19 pandemic, HE, and CMR on LE by providing valuable insights for policymakers and health consultants.
Fourth, this paper utilised graphical methods to effectively portray the descriptive statistics results. Such a graphical representation enhances the clarity of data interpretation, allowing for a more intuitive understanding of the COVID-19, HE, GDP, and CMR on LE in LICs.
Studying the interplay of COVID-19, HE, GDP, and CMR in LICs are crucial for understanding how to improve health outcomes in these vulnerable populations. Insights from this research can guide policymakers in resource allocation and health interventions, ultimately aiming to enhance LE and GDP and reduce CMR in LICs.
The remaining sections are organised as follows: “Data and Methodology,” which presents the data and methodology utilised; “Results and Discussion,” which evaluates the empirical results and the discussion; and “Conclusion and Policy Implications,” which presents the recommendations and conclusion, respectively.
Data and methodology
This study develops secondary data sourced from Our World in Data. It is covering 20 LICs from 2000 to 2021.
The variables analysed include LE, COVID-19, HE, GDP, and CMR. shows the analysis of the impact of these variables on LE using a panel regression model for panel data and time series analysis for time series data (Fig. 6). The model relations for the lagged effect of HE to capture its impact over time. Presenting a clear understanding of how these components work together to affect LE in LICs.
Fig. 6.
Overview of the workflow of the study. The diagram indicates the flow of overall research through each phase and step. Source: Authors’ compilations based on the literature
Data
This study uses secondary data sources with the data file presented in S1 Appendix. Data Set.. Data was collected from one database. Five variables are detailed in Table 1.
Table 1.
Variables and sources
| Variable | Measurement | Source |
|---|---|---|
| Life Expectancy | Life expectancy at birth | Our world in data https://ourworldindata.org/grapher/life-expectancy |
| COVID-19 | COVID-19 deaths in per million | Our world in data |
| https://ourworldindata.org/grapher/total-daily-covid-deaths | ||
| Healthcare Expenditure | Percentage of GDP | Our world in data |
| https://ourworldindata.org/grapher/total-healthcare-expenditure-gdp | ||
| Child Mortality Rate | Child deaths before the age of 5 per 100 births | Our world in data |
| https://ourworldindata.org/grapher/child-mortality-igme | ||
| GDP | GDP per capita |
Our world in data |
Summary of each variable's measurement with the sources from, which data were gathered
Source: Compiled by the authors
Model
The panel regression analysis model for panel data to identify the impact of HE, COVID-19, CMR and GDP on LE is given below.
| 1 |
The time series analysis model for time variation data to identify the impact of HE, COVID-19, CMR and GDP on LE is given below. For the time series analysis, 20 separate equations are regressed.
| 2 |
i(country) units at time t (years), with ε accounting for standard errors,
denotes the life expectancy, represents COVID-19 deaths. The coefficient measures the effect of COVID-19 deaths on LE, represents HE. The coefficient measures the effect of HE on LE, the impact of HE over time, a lagged variable for HE was used in the analysis. represents CMR. The coefficient measures the effect of CMR on LE, represents GDP. The coefficient measures the effect of GDP on LE, represents the intercept term and it captures the baseline level of LE when all independent variables are constant.
Results and discussion
Descriptive statistics
Based on the information in S2 Appendix. Summary of Descriptive Analysis Results. Fig. 7 summarises descriptive statistics using a radial bar chart. The radial bar chart presents a detailed visualisation of the data, illustrating the mean values for key variables, including COVID-19, CMR, GDP, and HE. Additionally, it highlights LE and GDP using a colour gradient scale, applied across 20 countries, offering a detailed analysis of regional disparities.
Fig. 7.
Low-income countries radial bar chart. The inner colour ring categorises life expectancy into four groups, ranging from 48–52 years (light brown) to 60–64 years (dark red). The outer colour ring represents GDP per capita in US dollars, with shades from light pink (200–350 USD) to dark purple (650–800 USD). Within each country segment, bars of different colours illustrate the impact of independent variables, green represents COVID-19, blue indicates healthcare expenditure, and yellow signifies the child mortality rate. The diagram visually compares how these factors vary across African nations, helping to understand their relationship with life expectancy and economic conditions. Source: Authors’ illustrations based on data
The red heatmap inside radial bar chart represents the average LE, the purple heatmap outside radial bar chart represents the average GDP. While the green bars indicate COVID-19 deaths, measured as the average number of deaths per million in a year due to the pandemic. HE is depicted using blue bars and is expressed as a percentage of GDP. The CMR is represented by yellow bars, indicating the number of deaths of children under the age of five per 100 live births.
The radial bar chart highlights key indicators across different countries. Eritrea, Gambia, Madagascar, Rwanda, and Sudan have highest LE records. In terms of COVID-19, Gambia exhibits the highest value, at 5.7. Sierra Leone records the highest values for both HE and CMR, with HE at 10.4 and CMR at 16.2. Uganda records the highest value for GDP, with 749.95.
Line chart
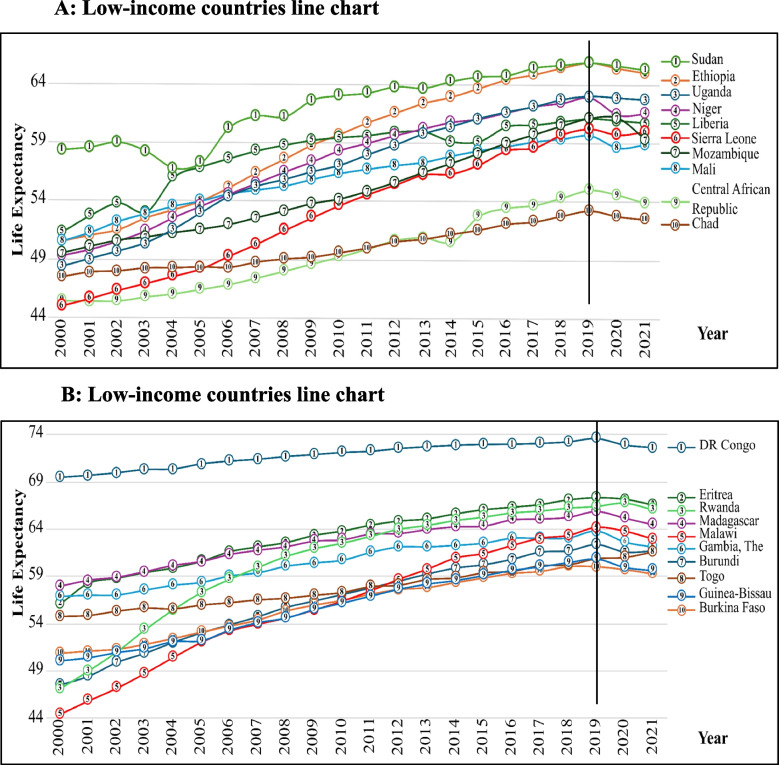
Figure 8 illustrate the LE of countries between 2000 and 2021. After 2000, the LE rate has been on an upward curve. However, the Democratic Republic of Congo retained a higher LE rate from 2000 to 2021. Democratic Republic of Congo might have been less severely affected by some of the epidemics that have plagued other countries such as Ebola [99]. Burundi LE increased rapidly because of the health stability [100]. Furthermore, Sudan showed a similar trend but at a lower value than the Democratic Republic of Congo.
Fig. 8.
Low-income countries line chart. Figure 8A line charts show the 10 low-income countries’ life expectancy, that were identifies from 2000 to 2021. The circle in each line with number indicates the particular country and that explain using the right-side legend inside of the figure. However, after 2019 most of the countries were decline. Figure 8B line charts show the rest of 10 low-income countries’ life expectancy, that were identifies from 2000 to 2021. The circle in each line with number indicates the particular country and that explain using the right-side legend inside of the figure. However, after 2019 most of the countries were decline. Source: Authors’ illustrations based on data
In 2000–2006, Sudan saw a narrow decrease in LE and then was able to increase the rates again in the latter years because The Second Sudanese Civil War was a conflict from 1983 to 2005 between the central Sudanese government and the Sudan People's Liberation Army. The conflict likely disrupted healthcare services and general living conditions, negatively impacting LE [101]. Liberia in 2002–2004 was unstable because the Second Liberian Civil War was a civil war in the West African nation of Liberia that lasted from 1999 to 2003 [102]. Therefore Liberia’ LE was unstable from 2002–2004.
Mozambique experienced cyclone Idai. Although it occurred before 2020, the aftermath of cyclone Idai, one of the worst tropical cyclones to affect Africa and the Southern Hemisphere, could have had lingering effects on health infrastructure and living conditions, worsening the impact of the pandemic conflict in Cabo Delgado [103]. Chad and Central African Republic were Persistent political instability, conflict and poor healthcare infrastructure in both countries could be contributing factors to the stagnation and slow improvement in LE. Central African Republic was during a severe crisis in 2014 due to ongoing civil conflict. The conflict, which began in late 2012, escalated into widespread violence by 2013–2014.
Without exception, all countries went into recession towards 2020 due to the COVID-19 pandemic.
Figure 8 separated into Fig. 8A and Fig. 8B, indicate that LE in the selected countries gradually increased from 2000 to 2021 with slight interjections due to conflicts, natural disasters, and the COVID-19 pandemic, but in DR Congo, LE rates have remained the highest in all years.
Panel regression
Using the panel analysis, this section seeks to establish the effects of COVID-19, HE, CMR, and GDP on LE in LICs. The analysis of the random effects model shows, that several factors deposited the relations between importance and show variations.
According to the panel regression result in Table 2, COVID-19 coefficient is −0.0111 and is statistically significant at the 5% level. It has a negative impact with COVID-19 with LE, when COVID-19 deaths increase, LE decreases. The coefficient for HE is −0.0316, but it is not statistically significant. This means that there is no measurable effect on LE by the HE in LICs. This result shows the insufficiency of delegation of healthcare facilities as well as not need to return in to best health outcomes. The coefficient for CMR is −1.3306, consider as 1% level. This shows that the high value of CMR is highly combined with low LE. That defines the importance of developing maternal and child health services to reduce mortality rate and to enhance total life expectancy. The coefficient for GDP is 0.0013, but it is not statistically significant. If GDP is positively connected with LE, but the result is not adequate to reach statistically important. This result suggest that not affect to increase LE of LICs which the money and the resources not equally divided. VIF value for all variables are comparatively low, defines that multicollinearity is not consider in the structure. The tolerance values are very high and are more advanced contribute for reliability of results of structure.
Table 2.
Random effect models for low-income countries
| REM | VIF | Tolerance | |
|---|---|---|---|
| Intercept |
70.6031*** (1.3929) |
||
| COVID-19 |
−0.0111** (0.0051) |
1.06 | 0.9412 |
| HE |
−0.0316 (0. 0999) |
1.01 | 0.9854 |
| CMR |
−1. 3306*** (0. 0698) |
1.11 | 0.9041 |
| GDP |
0.0013 (0.0011) |
1.05 | 0.9498 |
| R2 Within | 0.9332 | ||
| R2 Between | 0.6376 | ||
| R2 Overall | 0.7674 | ||
This result of a panel regression analysis shows the impact of key independent variables on life expectancy, including COVID-19, healthcare expenditure, child mortality rate, and GDP
Abbreviations: REM Random Effects Model and VIF Variance Inflation Factor
***, **, * represent 1%, 5% and 10% significance level, respectively. Robust standard errors are in parentheses
Source: Authors’ compilation based on the literature and results
Multiple linear regression
The data collected for the five variables LE, HE, COVID-19, GDP and CMR were analysed to observe trends, changes, and regression effects over 22 years for 171 countries. After the analysis, 20 LICs were selected to continue the study comprehensively. The results obtained in the study are discussed in this section. The analysis results are detailed in S3 Appendix. Regression Results.
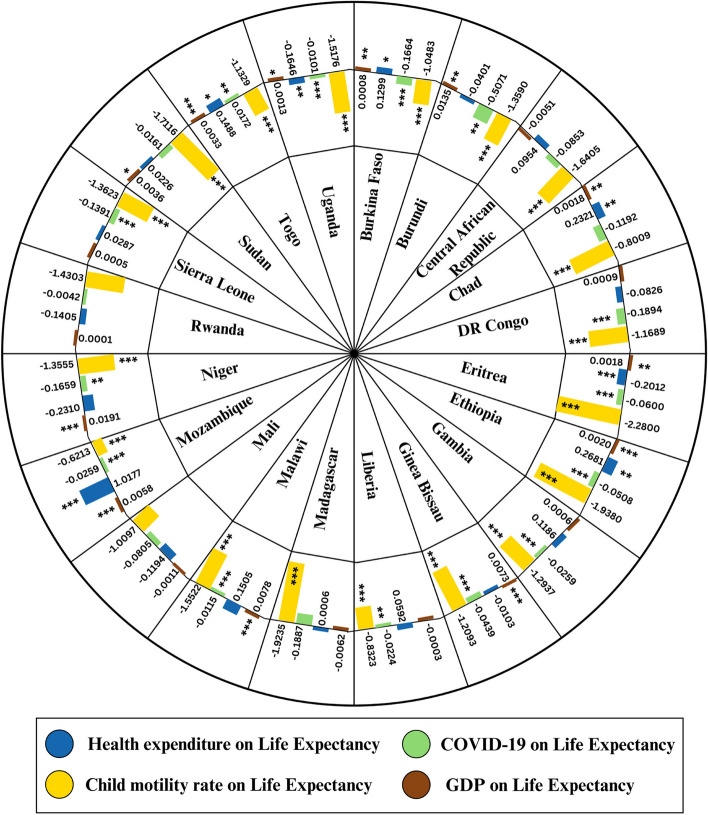
In Fig. 9 chart representing the trends in life expectancy, mortality of children under five years, and per capita GDP throughout the African continent. Fluctuations in these indexes are observed, indicating differences between the states. Some of these trends reveal that low GDP countries are associated with higher child mortality and lower life expectancies. This visualisation was done using Power BI for data processing, Photoshop for image processing, and finally done on Canva.
Fig. 9.
Radial comparative analysis in law-income countries. The figure summarises the impact of independent variables on life expectancy, based on the time series analysis coefficient values, represented using bar charts inside the circle for each country. Health expenditure on life expectancy is indicated by blue bars, while the effect of COVID-19 on life expectancy is represented by green bars. Yellow bars illustrate the impact of the child mortality rate on life expectancy, and brown bars show the influence of GDP on life expectancy. Note: ***, **, * represent 1%, 5% and 10% significance level, respectively. Source: Authors’ illustrations based on analysis results
The Table 3 expected and received impacts of four variables on LE. COVID-19 and CMR negatively impact on LE, GDP positively impact on LE, while HE and COVID-19 can have both positive and negative effects on LE, with the received signs matching expectations.
Table 3.
Summary of variables
| Variable | Description | Expected sign | Received sign |
|---|---|---|---|
| COVID-19 | Impact of COVID-19 on LE | + and - | + and - |
| HE | Impact of HE on LE | + and - | + and - |
| CMR | Impact of CMR on LE | - | - |
| GDP | Impact of GDP on LE | + | + |
This table summarises the expected and observed impact on independent variables on life expectancy
Source: Authors’ compilation based on the literature and results
COVID-19 on life expectancy
In analysed countries, COVID-19 deaths have a negative effect on LE, and it is statistically considerable. In most countries increase in COVID-19 deaths per million was related to the reduction of LE in countries that had weakened healthcare systems. In countries like Burkina Faso, Burundi, Democratic Republic of Congo, Eritrea, Ethiopia, Gambia, Guinea-Bissau, Liberia, Malawi, Mozambique, Niger, Sierra Leone and Uganda, LE has reduced considerably with the increase of COVID-19 deaths. As an example, while Burkina Faso has reduced LE in 0.1664 units with the increased COVID-19 deaths per million in one unit. Similarly, in Burundi the reduction of LE is mostly highlighted as 0.5071 units. These findings urge that the harmful effect of the COVID-19 pandemic to the LE of countries especially with limited healthcare facilities. However, Togo showed a positive effect on LE with COVID-19 deaths and is statistically considerable. It describes the ability of Togo, rather than other nations, to manage the effect of the pandemic most effectively.
Healthcare expenditure on life expectancy
The effect of HE on LE is considerably different in various countries. In some countries increased HE is affected for positive and significant development on LE. As an example, Mozambique showed a strong positive effect while increasing LE from 1.0177 units with the increase of HE in one unit. Chad also showed a positive effect on LE by HE. It shows that the healthcare investments play a vital role in increasing LE. However, not all the countries experienced a positive effect. In Eritrea the coefficient for HE was −0.2012, showing a negative effect on LE, and in Uganda. It also has a negative coefficient for HE, and the increase of HE from one unit is affect for decreasing LE from 0.1646 units.
Child mortality rate on life expectancy
The CMR showed a negative and specific effect of LE in all countries in the study. High CMR had highly effect on the reduction in LE, and it is a clear indicator about the importance of reducing child deaths in developing total overall health results. As an example, in Eritrea the increase of CMR from one unit is caused by reducing LE from 2.2800 units. It is the most important effect observed through all the countries. Similarly, it had observed negative effects on LE in countries like Sierra Leone, Guinea-Bissau, and Malawi. These findings prove that reducing CMR is a priority in increasing LE in LICs.
GDP on life expectancy
The connection between GDP per capita and LE is generally shown a positive effects through countries. In countries like Togo, Sudan, and Mozambique the economic development made a specific and positive effect on LE. As an example in Mozambique, LE is increased from 0.0058 units with the increasing of GDP from one unit and in Togo. The effect was stronger with a coefficient of 0.0033. This means that the economic development with better access for health services, improved living status and the strongest public health infrastructure facilities can make a positive effect on LE. However, the effect of GDP on LE in countries like Liberia and Mali are weakened and unsignificant, suggest that only the development of the economy is not enough for developing health results. This indicates the importance of combining the economic development with targeted investments in healthcare and other social determinants in health.
Discussion
Negative impact of COVID-19 on life expectancy
Our analysis shows a significant negative and positive relationship between COVID-19 deaths and LE in the twenty LICs [20]. The regression results showed that in Burundi, a one-unit increase in COVID-19 deaths corresponded to a 0.5071 unit decrease in LE. Similar trends were observed in other countries, such as Eritrea and the Democratic Republic of Congo, highlighting the significant impact of COVID-19 on LE in countries with limited healthcare infrastructure. This effect of COVID-19 on LE across countries can be attributed to differences in political decisions, healthcare policies and economic factors. Countries with weak healthcare systems and low HE, such as the Niger and Sierra Leone, have faced larger decreases in LE. Where HE was relatively higher, and that country showed a less noticeable reduction. These findings are matched with past research [35] that highlights the role of the healthcare sector and governance in mitigating the COVID-19 impact.
Moreover, the socio-economic context in these LICs further expanded the impact of COVID-19, impact with poor healthcare infrastructure, limited finance capacity and insufficient pandemic preparedness. Many of these countries failed to manage the COVID-19-related deaths, leading to a huge reduction in LE. This highlights the need for targeted interventions to healthcare systems in LICs Particularly in the face of future pandemics.
Positive impact of COVID-19 on life expectancy
While the global consensus is that the increased COVID-19 deaths had negatively affect for LE, and it represents a suspicious exception in that the effect of COVID-19 on LE is positive in Togo. The regression results shows that the increase of LE from 0.0172 units with the increased number of COVID-19 deaths per million from one unit and it is specific in 5% level statistically. According to global priority COVID-19 has harmful impacts for health but this finding shows an opposite meaning. It means in Togo healthcare system had manage the pandemic effectively rather than expected. While most LICs had experienced considerable reduction in LE, Togo takes benefits from better health care access, strong vaccination programme and external support and it helps to minimise the bad effects of the virus. In curfews and lockdown periods restrictions of movements and public gatherings may lead to minimise accidents and injuries and they are mostly relating with alcohol consumption and smoking like bad health habits which caused for high mortality which can be seen mostly in LICs. Lockdown can participate positively for LE in Togo by reducing the deaths by accidental injuries [1]. These findings highlighted the divergence in how the different LICs experienced the pandemic, with the countries like Togo experiencing a little reduction or an even improvement in LE by effective management and minimising strategies. In oppositely the countries with weakened health systems showed a direct reduction in LE. Shows effect of pandemic is not uniform over all LICs.
Impact of healthcare expenditure on life expectancy
This research analysis was able to find out that there were both positive and negative effects of HE on LE in LICs. These findings are matched with past research [28]. Several factors, such as government effectiveness and the efficiency of the health care system, appear to have an impact on the nature of this relationship.
Positive impact of health expenditure on life expectancy
In many LICs, increasing HE has been shown to improve LE. This is consistent with studies conducted across many countries. These findings are matched with past research [104], which determines that high healthcare spending enhances access to medical aid, reduces illness incidence and fosters the adoption of preventive practices in countries that invest more in HE. Persons are more likely to receive their check-ups at the right time and compulsory actions for critical situations. These developments in the healthcare approach result in a direct reduction in mortality rates and increased LE. Such changes in the approach to healthcare bring a direct positive way to reduction in mortality rates and enhancement of the LE. The availability of the proper equipment and medical knowledge means better control the virus. Specially in keeping away and controlling communicable viruses. Besides enhancing the treatment of viruses, HE appears to support new research and technology in medicine that also makes other positive contributions to the quality of health care. These findings are matched with past research [105].
Negative impact of health expenditure on life expectancy
While increasing HE usually has a positive impact on LE, there are a few instances where that can have a negative effect on LE. Specifically, in countries with poor governance and healthcare systems. Many LICs with poor HE and government effectiveness can negatively influence LE. In those cases, even with increased spending, bureaucratic inefficiencies, corruption, and a lack of flexibility in government systems can interrupt the positive outcomes of the healthcare system. During times of essential healthcare needs such as pandemics, inefficient budget allocation and delays in policy implementation can result in low returns on the healthcare system. This inefficiency is popular in countries with ineffective government structures and healthcare systems underfunded. In such environments, additional healthcare expenditure only sometimes leads to the expected improvements in LE. The findings [28] shows that some LICs with better governance can reduce the amount of HE needed to positively affect LE. While weak governance led to inefficiencies. This shows that increasing healthcare spending is insufficient, and the effectiveness of governance and efficient healthcare management are critical to ensuring that funds are appropriately used to improve healthcare outcomes.
Impact of child mortality rate on life expectancy
The negative relationship between LE and CMR is a well-identified phenomenon in global health. These findings are matched with past research [106]. When CMR increases LE tends to decrease reflecting the overall health and socioeconomic conditions of a population. CMR is defined as the number of child deaths before the age of 5 per 100 births. Countries with high CMR always have poor healthcare infrastructure and lack of access to essential services such as clean water and sanitation. These factors not only lead to higher mortality among children but also affect the broader population. That resulted in lower LE in this study. Countries like Eritrea, Sudan, Ethiopia, and Madagascar have experienced the most reduction in LE. Even a slight increase in CMR led to a decrease in LE. As an example, in Eritrea, a one-unit increase in CMR caused a 2.2800-unit decline in LE. This shows that CMR has a significant impact on the overall health and longevity of a population. The findings show the importance of addressing CMR to improve LE in LICs. Reducing CMR through better maternal healthcare improved nutrition and broader access to vaccinations not only save lives but also lead to gain the LE. Countries with high CMR also face broader public health problems and reducing CMR could have a positive effect on the general population’s health and LE.
Impact of GDP on life expectancy
The analysis shows a complex connection between the GDP per capita and LE through 20 low-income countries. It has found a positive connection between the GDP and the LE. But the strength between this connection is different in countries. Some countries like Mozambique, Ethiopia, Togo, and Niger shows a positive and considerable effect on LE by economic development. As an example in Mozambique, the GDP per capita increased from one unit, correspondingly the LE is increased from 0.0058 units. It suggested that the economic development plays a vital role in developing health results including health services, nutrition and total overall living status.
However, the connection between the GDP and LE is universally not strong. In countries like Liberia and Mali, GDP had made a positive and unimportant effect and suggested that only the economic development is not enough to enhance the health results. This finding is aligned with the concept that it should being complementary to economic development trough targeted investments for health services, education and social services to gain a meaningful progress in LE. In these countries, weakened healthcare infrastructure facilities, political instability and inefficient governing like reasons may be a barrier to potential benefits of economic development. According to this there is a connection generally between LE and GDP and it is not the only one indicator of health results and its effect affect by social -political factors and effective governing.
Data scope and limitations
Data availability and consistency allow this study to focus on 20 LICs. Although the World Bank provides data for 37 LICs, many countries lacked complete or inconsistent data available for key variables including LE, HE, COVID-19, CMR and GDP especially, for 2000–2021. To obtain an accurate and reliable analysis, we chose the 20 countries with the best and most consistent data. Although this limits the generalisability of the results, it ensures that analysis is based on reliable data resulting in a robust base from which to draw study conclusions.
Conclusion
The main objective of this research was to investigate the impact of COVID-19, HE, GDP, and CMR on LE in LICs. While previous studies explored these factors separately this study shows a cohesive view of their combined effects, offering critical insights into how pandemics aggravate existing weaknesses in these countries.
Our findings disclose that COVID-19 had a significantly negative effect on LE in a lot of LICs because healthcare systems are already weak. Countries with poor healthcare infrastructures and high CMR show considerable declines in LE. In some cases, increased spending on healthcare shows improved LE, and on the other hand, poor governance and resource allocation reduced its benefits. This shows the need for more strategic healthcare investments addressing structural inefficiencies. The strong impact of CMR on LE shows the urgent need for interventions to reduce CMR. Countries with high CMR need help to improve LE and must consider more healthcare policies, immunisation programmes and access to essential healthcare services.
This study contributes valuable insights for policymakers and healthcare professionals by emphasising the importance of investments in the healthcare system, governance, and child health involvements. Improving healthcare infrastructure, ensuring better management, and increasing access to essential services would be critical to enhancing LE in LICs. Furthermore, pandemic preparedness must become a priority to protect these countries from future global health crises.
Emphasis is made in this study on the efficient allocation of health care resources and strategic investments, which are aimed at reducing the long- term effect of COVID-19 on LE. Improving healthcare literacy on an individual level would be necessary to ensure that it promotes trustworthiness in health systems for more improvements. Future research should focus on the long-term impacts of healthcare system improvements and explore the role of socioeconomic and environmental factors in shaping LE. Investigating how different health policies have influenced outcomes during and after the pandemic will provide deeper insights into how healthcare systems could be more resilient in the face of global health challenges.
This study presents a new perspective on how HE, CMR and pandemics interact to improve LE in LICs. By addressing the challenges identified, policymakers and global health organisations can make informed decisions to improve health outcomes and build more resilient healthcare systems in these countries.
Policy implications
This study outlines the crucial sectors where policy intervention can improve LE in LICs, particularly in response to the challenges posed by the COVID-19 pandemic. The research's key is the urge for better healthcare infrastructure, stronger governance, more preventive care services, and attention to pandemic preparedness in healthcare spending. Those are the essential steps to the prosperity of both maternal and child that focus on reducing the CMR and overall LE improvements in LICs.
Strengthening healthcare infrastructure
Healthcare facilities must be among the priorities of the LICs and should receive vast investments to strengthen the system, thus reducing CMR. Treatment centres should be enhanced, the local populace should have access to essential medical services, the existence of medical equipment should be ensured, and the government should fund them. The first step involves taking concrete steps towards a more robust healthcare system by having the necessary infrastructure. The presence of infrastructure in curative care and in management of outbreaks, will see a better increase in LE in the future.
Improving governance and health system efficiency
Healthcare spending requires a good business environment to produce optimum returns in LICs. This is only possible through better governance, transparency, and accountability in the health sector. The laws with solid monitoring and evaluation systems shall ensure that the healthcare expenditure becomes the actual encryption in public health. Improved governance will reduce resource wastage and promote the efficiency of the healthcare systems, resulting in better health and increased LE.
Increasing healthcare expenditure focused on preventive care
LICs should allocate the budget with a concentration on preventive care in the key areas, specialised in maternity and child healthcare services, vaccination services and regular check-ups for the patients. Thus, the preventive plans will lead to fewer deaths in children, and the health issue will be solved in the long term. Furthermore, teaching health workers prevention will not only strengthen the community’s healthcare, but it will also result in a healthier population.
Targeted interventions for high child mortality rate countries
One of the significant features of the study is the need for targeted interventions geared towards lessening CMR. States need to provide maternal and child health services as well as safe drinking water to their residents. Programmes such as those that offer cost-free or subsidised maternal and infant health care services can make a considerable contribution to reducing CMR and increasing in average LE. Some of those programmes must be oriented in nations that are still at deadly CMR.
Pandemic preparedness and response plans
The COVID-19 pandemic exposed the vulnerabilities in healthcare systems in LICs, which led to a severe decrease in LE. Governments, in coordination with internal and external stakeholders, should develop a detailed plan containing disease warning systems, stockpiling the most crucial medicines, and ensuring that there are enough medical staff and necessary resources to be sent out rapidly during a pandemic. The best way forward is to engage international actors and bring funding to these efforts, besides increasing the capacity of systems to respond to any crisis.
Leveraging international aid and technical assistance
It is the responsibility of the licensor to initiate a commitment to such partners as the World Bank and the World Health Organisation (WHO) to access the payment of financial aid and provide technical assistance. These relationships help healthcare facilities in licensor countries to achieve their goals, such as immunisation, cleaner sanitation, and more convenient access to essential health services by adopting the low-cost, high-impact model. International cooperation is indispensable, which would eventually bridge the gap of health equity and thus increase LE in LICs.
Addressing underlying socioeconomic determinants of health
LICs health policies should be included in the broader socio-economic strategies to cover the root causes of ill health. Better access to education, poverty reduction and improving living conditions, especially about sanitation and clean water, can contribute to the overall health and longer life of the population. The intervention of these essential determinants is not only a rising part of the public health system but also the underlying infrastructure for the long-term resilience of LICs.
Data-driven health policy
The governing bodies in LICs should allocate funds data collection, monitoring, and research to monitor health indicators more accurately and make interventions that cater to specific needs. The government, using data-driven choices, can ensure that healthcare resources are contacted and targeted effectively to the areas with the highest need. This method will not only permit the better use of healthcare funds but will also improve LE.
Expanding child and maternal health programmes
Treating child and maternal health services is instrumental in improving the LE of LICs. Emphasise the provision of bottom-up services to pregnant women and young children, particularly in the case of the underserved countries. Therefore, governments must ensure that these crucial services can reach even the remotest area. This is the only way a country could eliminate cases of child mortality and, at the same time, enhance the health of its population.
Supplementary Information
Additional file 1: S1 Appendix. Data set
Additional file 2: S2 Appendix. Summary of descriptive analysis results
Additional file 3: S3 Appendix. Regression results
Acknowledgements
The authors also would like to thank Mr. Harasha Gunewardene for proof-reading and editing this manuscript.
Authors’ contributions
All authors contributed to the conception and design of the project. MK, AP, PM and ND composed the writing of the manuscript. PB, MK and AP did a lot of statistical work in the manuscript. RJ provided critical knowledge in drafting of the paper and supervised the entire study. The authors have read and approved the final manuscript.
Funding
The authors received no specific funding for this work.
Data availability
The datasets generated and analysed during the current study are publicly available at Our World in Data database: https://ourworldindata.org/. All data generated or analysed during this study are included in this published article and its supplementary information files.
Declarations
Ethics approval and consent to participate
Study used the secondary data and necessary clearance was obtained.
Consent for publication
Not applicable (NA).
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Strozza C, Vigezzi S, Callaway J, Aburto JM. The impact of COVID-19 on life expectancy across socioeconomic groups in Denmark. Popul Health Metrics. 2024;22(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta A, Hathi P, Banaji M, Gupta P, Kashyap R, Paikra V, Sharma K, Somanchi A, Sudharsanan N, Vyas S. Large and unequal life expectancy declines during the COVID-19 pandemic in India in 2020. Seience Advance. 2024;10(29):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aburto JM, Schöley J, Kashnitsky I, Kashyap R. Life expectancy declines in Russia during the COVID-19 pandemic in 2020. Int J Epidemiol. 2022;51(5):1695–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.The Lancet Public H. Public health in China: time to invest in prevention. The Lancet Public Health. 2023;8(12):1–2. [DOI] [PubMed] [Google Scholar]
- 5.Castro MC, Gurzenda S, Turra CM, Kim S, Andrasfay T, Goldman N. Reduction in life expectancy in Brazil after COVID-19. Nat Med. 2021;27(9):1629–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Aburto JM, Schöley J, Kashnitsky I, Zhang L, Rahal C, Missov TI, Mills MC, Dowd JB, Kashyap R. Quantifying impacts of the COVID-19 pandemic through life-expectancy losses: a population-level study of 29 countries. Int J Epidemiol. 2021;51(1):63–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huang G, Guo F, Liu L, Taksa L, Cheng Z, Tani M, Zimmermann KF, Franklin M, Silva SSM. Changing impact of COVID-19 on life expectancy 2019–2023 and its decomposition: Findings from 27 countries. SSM - Population Health. 2024;25:101568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Canudas-Romo V, Houle B, Adair T. Quantifying impacts of the COVID-19 pandemic on Australian life expectancy. Int J Epidemiol. 2022;51(5):1692–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao G, Liu J, Liu M, Liang W. Effects of the COVID-19 pandemic on life expectancy at birth at the global, regional, and national levels: A joinpoint time-series analysis. J Glob Health. 2023;13:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Behera DK, Dash U. Is health expenditure effective for achieving healthcare goals? Empirical evidence from South-East Asia Region. Asia-Pacific Journal of Regional Science. 2020;4(2):593–618. [Google Scholar]
- 11.Rahman MM, Khanam R, Rahman M. Health care expenditure and health outcome nexus: new evidence from the SAARC-ASEAN region. Glob Health. 2018;14(1):113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zulu JM, Silumbwe A, Munakampe M, Chavula MP, Mulubwa C, Sirili N, Zulu W, Michelo C, Tetui M. A scoping review of the roles, challenges, and strategies for enhancing the performance of community health workers in the response against COVID-19 in low-and middle-income countries. Res Squar. 2024;120(1):1–15. [Google Scholar]
- 13.Jones-Esan L, Somasiri N, Lorne K. Enhancing healthcare delivery through digital health interventions: a systematic review on telemedicine and mobile health applications in Low and Middle-Income Countries (LMICs). Res Square. 2024;120(1):1–15. [Google Scholar]
- 14.Yew SQ, Trivedi D, Adanan NIH, Chew BH. Facilitators and barriers of digital health technologies implementation in hospital settings in lower-income and middle-income countries since the COVID-19 pandemic: a scoping review protocol. The Bmj. 2024;14(1):e078508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schumacher AE, Kyu HH, Aali A, Abbafati C, Abbas J, Abbasgholizadeh R, Abbasi MA, Abbasian M, Abd ElHafeez S, Abdelmasseh M, et al. Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. The Lancet. 2024;403(10440):1989–2056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hauck K, Martin S, Smith PC. Priorities for action on the social determinants of health: Empirical evidence on the strongest associations with life expectancy in 54 low-income countries, 1990–2012. Soc Sci Med. 2016;167:88–98. [DOI] [PubMed] [Google Scholar]
- 17.Hasan I, Marra M, To TY, Wu E, Zhang G. COVID-19 Pandemic and Global Corporate CDS Spreads. J Bank Finance. 2023;147:106618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sanderson WC, Scherbov S. The effect of the COVID-19 pandemic on life expectancy in the USA: An application of hybrid life expectancy. Biol Methods Protoc. 2023;8(1):bpad025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Padmaja M, Behera DK. Disruptions in accessing women’s health care services: evidence using COVID-19 health services disruption survey. Matern Child Health J. 2023;27(2):395–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huang G, Guo F, Zimmermann KF, Liu L, Taksa L, Cheng Z, Tani M, Franklin M. The effect of the COVID-19 pandemic on life expectancy in 27 countries. Sci Rep. 2023;13(1):8911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Number of COVID-19 cases reported to WHO https://data.who.int/dashboards/covid19/cases?n=c.
- 22.Cao G, Liu J, Liu M, Liang W. Effects of the COVID-19 pandemic on life expectancy at birth at the global, regional, and national levels: A joinpoint time-series analysis. J Glob Health. 2023;13(12):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Silva S, Goosby E, Reid MJA. Assessing the impact of one million COVID-19 deaths in America: economic and life expectancy losses. Sci Rep. 2023;13(1):3065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ko S, Kim R, Subramanian SV. Patterns in Child Health Outcomes Before and After the COVID-19 Outbreak in India. JAMA Netw Open. 2023;6(6):e2317055–e2317055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Shalitin S, Phillip M, Yackobovitch-Gavan M. Do changes in BMI during the COVID-19 pandemic persist in the post-pandemic period in a pediatric population attending health care clinics? A longitudinal study. Hormone Res Paediatr. 2024;28:1–12. [DOI] [PubMed] [Google Scholar]
- 26.Tomidis Chatzimanouil MK, Rößler S, Nurjadi D, Iakovidis I, Berner R, Toepfner N, Bornstein tDGASSGSR, Aschoff R, Bornhäuser M, Güldner A, et al. Post-COVID-19-pandemic changes and clinical characteristics of invasive group a streptococcal infections from 2015 to 2023. Infection. 2024;12(120):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Park M-B, Hwang B-D, Nam Y-H. Investigating the Role of Social Determinants in Child Mortality and Life Expectancy: Longitudinal Analysis of 200 Countries from 1990 to 2021. Child Indic Res. 2024;17(4):1871–89. [Google Scholar]
- 28.Bunyaminu A, Mohammed I, Yakubu IN, Shani B. Abukari: The effect of health expenditure on average life expectancy: does government effectiveness play a moderating role? International Journal of Health Governance. 2022;27(4):365–77. [Google Scholar]
- 29.Bhattacharyya H, Agarwalla R, Khandelwal A. Impact of COVID-19 on child health and healthcare services. Medical Journal Armed Forces India. 2022;78(1):3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.It’s Not Just About Child Mortality, Life Expectancy Increased at All Ages. https://ourworldindata.org/its-not-just-about-child-mortality-life-expectancy-improved-at-all-ages.
- 31.Miguel E, Mobarak AM. The economics of the COVID-19 pandemic in poor countries. Annual Rev Econ. 2022;14(1):253–85. [Google Scholar]
- 32.Ho JY, Hendi AS. Recent trends in life expectancy across high income countries: retrospective observational study. The Bmj. 2018;362:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Child Mortality and Covid-19. https://data.unicef.org/topic/child-survival/covid-19/.
- 34.Nuwagira E, Muzoora C. Is Sub-Saharan Africa prepared for COVID-19? Tropical Medicine and Health. 2020;48(1):1–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Islam N, Jdanov DA, Shkolnikov VM, Khunti K, Kawachi I, White M, Lewington S. Lacey BJb: Effects of covid-19 pandemic on life expectancy and premature mortality in 2020: time series analysis in 37 countries. The Bmj. 2021;375:1649–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Heuveline P. The COVID-19 pandemic adds another 200,000 deaths (50%) to the annual toll of excess mortality in the United States. Social Sciences. 2021;118(36):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pifarré i Arolas H, Acosta E, López-Casasnovas G, Lo A, Nicodemo C, Riffe T, Myrskylä M. Years of life lost to COVID-19 in 81 countries. Sci Rep. 2021;11(1):1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Adair T, Houle B, Canudas-Romo V. Effect of the COVID-19 pandemic on life expectancy in Australia, 2020–22. Int J Epidemiol. 2023;52(6):1735–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.COVID-19 eliminated a decade of progress in global level of life expectancy. https://www.who.int/news/item/24-05-2024-covid-19-eliminated-a-decade-of-progress-in-global-level-of-life-expectancy.
- 40.Woolf SH, Masters RK. Aron LYJb: Effect of the covid-19 pandemic in 2020 on life expectancy across populations in the USA and other high income countries: simulations of provisional mortality data. The BMJ. 2021;373:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kontis V, Bennett JE, Rashid T, Parks RM, Pearson-Stuttard J, Guillot M, Asaria P, Zhou B, Battaglini M, Corsetti G, et al. Magnitude, demographics and dynamics of the effect of the first wave of the COVID-19 pandemic on all-cause mortality in 21 industrialized countries. Nat Med. 2020;26(12):1919–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hillis SD, Unwin HJT, Chen Y, Cluver L, Sherr L, Goldman PS, Ratmann O, Donnelly CA, Bhatt S, Villaveces A, et al. Global minimum estimates of children affected by COVID-19-associated orphanhood and deaths of caregivers: a modelling study. The Lancet. 2021;398(10298):391–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Av D. Cooney RE, Sabin ML: COVID-19 exacerbating inequalities in the US. The Lancet. 2020;395(10232):1243–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.The World Health Report 2005. Make every mother and child count. https://www.who.int/publications/i/item/9241562900. [DOI] [PubMed]
- 45.Jordan B. Life expectancy and Covid: Setting the record straight. Med Sci (Paris). 2022;38(12):1075–7. [DOI] [PubMed] [Google Scholar]
- 46.Schöley J, Aburto JM, Kashnitsky I, Kniffka MS, Zhang L, Jaadla H, Dowd JB, Kashyap R. Life expectancy changes since COVID-19. Nat Hum Behav. 2022;6(12):1649–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Verma A, Sharma RK, Saha KB. Diversity in Child Mortality and Life Expectancy at Birth Among Major Tribes in Selected States of India. Indian Pediatr. 2021;58(1):20–4. [PubMed] [Google Scholar]
- 48.Liu L, Oza S, Hogan D, Chu Y, Perin J, Zhu J, Lawn JE, Cousens S, Mathers C, Black RE. Global, regional, and national causes of under-5 mortality in 2000–15: an updated systematic analysis with implications for the Sustainable Development Goals. The Lancet. 2016;388(10063):3027–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Marmot M. The health gap: the challenge of an unequal world. The Lancet. 2015;386(10011):2442–4. [DOI] [PubMed] [Google Scholar]
- 50.Hill K, Pebley ARJP. review d: Child mortality in the developing world. JSTOR. 1998;15:657–87. [Google Scholar]
- 51.Wagner Z, Heft-Neal S, Wang Z, Jing R, Bendavid E: Infant and neonatal mortality during the covid-19 pandemic: an interrupted time series analysis from five low- and middle-income countries. medRxiv 2023;N/A:1–17.
- 52.Roberton T, Carter ED, Chou VB, Stegmuller AR, Jackson BD, Tam Y, Sawadogo-Lewis T, Walker N. Early estimates of the indirect effects of the COVID-19 pandemic on maternal and child mortality in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(7):901–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.The State of the Global Education Crisis: A Path to Recovery. https://www.worldbank.org/en/topic/education/publication/the-state-of-the-global-education-crisis-a-path-to-recovery.
- 54.Hogan AB, Jewell BL, Sherrard-Smith E, Vesga JF, Watson OJ, Whittaker C, Hamlet A, Smith JA, Winskill P, Verity R, et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob Health. 2020;8(9):1132–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Osendarp S, Akuoku JK, Black RE, Headey D, Ruel M, Scott N, Shekar M, Walker N, Flory A, Haddad L, et al. The COVID-19 crisis will exacerbate maternal and child undernutrition and child mortality in low- and middle-income countries. Nature Food. 2021;2(7):1–11. [DOI] [PubMed] [Google Scholar]
- 56.Fazle Rabbi AM. Imbalance in Life Table: Effect of Infant Mortality on Lower Life Expectancy at Birth. J Sci Res. 2013;5(3):479–88. [Google Scholar]
- 57.Rutstein SO. Factors associated with trends in infant and child mortality in developing countries during the 1990s. Bull World Health Organ. 2000;78(10):1256–70. [PMC free article] [PubMed] [Google Scholar]
- 58.Liang J, Du Y, Qu X, Ke C, Yi G, Liu M, Lyu J, Ren Y, Xing J. Wang CJFiP: The causes of death and their influence in life expectancy of children aged 5–14 years in low-and middle-income countries from 1990 to 2019. Front Pediatr. 2022;10:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Victora CG, Bahl R, Barros AJD, França GVA, Horton S, Krasevec J, Murch S, Sankar MJ, Walker N, Rollins NC. Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. The Lancet. 2016;387(10017):475–90. [DOI] [PubMed] [Google Scholar]
- 60.U.S. Life Expectancy Increasing, but So Is Child Death Rate. https://www.webmd.com/a-to-z-guides/news/20240321/us-life-expectancy-increasing-but-so-is-child-death-rate.
- 61.Haldane V, De Foo C, Abdalla SM, Jung A-S, Tan M, Wu S, Chua A, Verma M, Shrestha P, Singh S, et al. Health systems resilience in managing the COVID-19 pandemic: lessons from 28 countries. Nat Med. 2021;27(6):964–80. [DOI] [PubMed] [Google Scholar]
- 62.Shahraki M. Public and private health expenditure and life expectancy in Iran. J Payesh. 2019;18(3):221–30. [Google Scholar]
- 63.Singh AK, Misra A. Impact of COVID-19 and comorbidities on health and economics: Focus on developing countries and India. Diabetes Metab Syndr. 2020;14(6):1625–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Railaite R. Ciutiene RJIe: The impact of public health expenditure on health component of human capital. Engineering Economics. 2020;31(3):371–9. [Google Scholar]
- 65.Omar MH, Asmuni NH, Shima SN. Healthy life expectancy vs health expenditure by Sullivan method in Malaysia. Indonesian Journal of Electrical Engineering and Computer Science. 2019;14:402–6. [Google Scholar]
- 66.Sabra MM. Health expenditure, life expectancy, fertility rate, CO 2 emissions and economic growth Do public, private and external health expenditure matter? Theoretical and Applied Economics. 2022;29(3):88–232. [Google Scholar]
- 67.Bayar Y, Gavriletea MD, Pintea MO. Sechel ICJIJoER, Health P: Impact of environment, life expectancy and real GDP per capita on health expenditures: Evidence from the EU member states. Enviromental resarch and public health. 2021;18(24):1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Radmehr M, Adebayo TS. Does health expenditure matter for life expectancy in Mediterranean countries? Environ Sci Pollut Res. 2022;29(40):60314–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Chippaux J-P. COVID-19 impacts on healthcare access in sub-Saharan Africa: an overview. Venomous Animals and Toxins including Tropical Disease. 2023;29:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Galma T. FONSECA, Raquel, MICHAUD, Pierre-Carl, KAPTEYN, Arie Accounting for the Rise of Health Spending and Longevity. J Eur Econ Assoc. 2021;19(1):1–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Fan VY. Savedoff WDJSs, medicine: The health financing transition: a conceptual framework and empirical evidence. Soc Sci Med. 2014;105:112–21. [DOI] [PubMed] [Google Scholar]
- 72.Mohanty RK, Behera DK. Heterogeneity in health funding and disparities in health outcome: a comparison between high focus and non-high focus states in India. Cost Effectiveness and Resource Allocation. 2023;21(1):1–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Kumar D. Reasons and Realities of Health and Geographical Inequality in India: A Study of Inter-State Variations. Regional Economic Development Research. 2021;123(1):38–50. [Google Scholar]
- 74.Dwivedi R, Pradhan J. Does equity in healthcare spending exist among Indian states? Explaining regional variations from national sample survey data. International Journal for Equity in Health. 2017;16(1):15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Farahani M, Subramanian SV, Canning D. Effects of state-level public spending on health on the mortality probability in India. Health Econ. 2010;19(11):1361–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Molassiotis A, Kwok SWH, Leung AYM, Tyrovolas S. Associations between sociodemographic factors, health spending, disease burden, and life expectancy of older adults (70 + years old) in 22 countries in the Western Pacific Region, 1995–2019: estimates from the Global Burden of Disease (GBD) Study 2019. GeroScience. 2022;44(2):925–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Cylus J, Papanicolas I, Smith PC. How to make sense of health system efficiency comparisons? The Bmj. 2017;375:162–266. [PubMed] [Google Scholar]
- 78.Behera DK, Dash U. Healthcare financing in South-East Asia: Does fiscal capacity matter? International Journal of Healthcare Management. 2020;13(sup1):375–84. [Google Scholar]
- 79.Shkolnikov VM, Andreev EM, Tursun-zade R, Leon DA. Patterns in the relationship between life expectancy and gross domestic product in Russia in 2005–15: a cross-sectional analysis. The Lancet Public Health. 2019;4(4):e181–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Rubi MA, Bijoy HI, Bitto AK: Life Expectancy Prediction Based on GDP and Population Size of Bangladesh using Multiple Linear Regression and ANN Model. In: 2021 12th International Conference on Computing Communication and Networking Technologies (ICCCNT): 04th December 2024. 2021;2021:1–6.
- 81.Freeman T, Gesesew H, Bambra C, Giugliani E, Popay J, Sanders D, Macinko J, Musolino C, Baum F. Why do some countries do better or worse in life expectancy relative to income? An analysis of Brazil, Ethiopia, and the United States of America. International Journal for Equity in Health. 2020;19(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.He L, Li N. The linkages between life expectancy and economic growth: some new evidence. Empirical Economics. 2020;58(5):2381–402. [Google Scholar]
- 83.Chen Z, Ma Y, Hua J, Wang Y, Guo H. Impacts from economic development and environmental factors on life expectancy: A comparative study based on data from both developed and developing countries from 2004 to 2016. International Journal of Environmental Research Public Health. 2021;18(16):8559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Thomson R. The Intrinsic Concatenation of Economic Growth and Life Expectancy: How Periods of GDP Expansion Generate Global and National Increases in Average Life Span. Topophilia. 2024;120(1):16–21. [Google Scholar]
- 85.Barfar E, Faramarzi A, Khanijahani A, Alizadeh S, Ashrafi A. Investigation of the Relationship between Health and Economic Indicators in Selected Countries, 2004–2011. Sadra Med J. 2014;2(4):349–60. [Google Scholar]
- 86.Prata PR. Economic development, inequality, and health. Cad Saude Publica. 1994;10(1):387–91. [DOI] [PubMed] [Google Scholar]
- 87.Wang H. The impact of economic development on health: a country-level analysis. Digital Carchulaacth. 2019;120(1):1–15. [Google Scholar]
- 88.Lau EW, Schooling CM. Tin kY, Leung GM: Income Inequality and Cause-Specific Mortality During Economic Development. Ann Epidemiol. 2012;22(4):285–94. [DOI] [PubMed] [Google Scholar]
- 89. Swint JM, Franzini L, Honda C, Murakami Y, Rasu R: Relationships between Economic Growth and Population Health in Low and Middle Income Countries. Osaka Economic Papers 2008:11–32.
- 90.Gmanyami JM, Quentin W, Lambert O, Jarynowski A, Belik V, Amuasi JH. Excess mortality during the COVID-19 pandemic in low-and lower-middle-income countries: a systematic review and meta-analysis. BMC Public Health. 2024;24(1):10–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Tandon A, Roubal T, McDonald L, Cowley P, Palu T, de Oliveira Cruz V, Eozenou P, Cain J, Teo HS, Schmidt M. Economic impact of COVID-19: Implications for health financing in Asia and Pacific: World Bank; 2020.
- 92.Kitano T, Kitano M, Krueger C, Jamal H, Al Rawahi H, Lee-Krueger R, Sun RD, Isabel S, García-Ascaso MT. Hibino HJPo: The differential impact of pediatric COVID-19 between high-income countries and low-and middle-income countries: a systematic review of fatality and ICU admission in children worldwide. PLoS ONE. 2021;16(1):1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sachs JD. Primary Health Care in Low-Income Countries: Building on Recent Achievements. JAMA. 2012;307(19):2031–2. [DOI] [PubMed] [Google Scholar]
- 94.Sheidaei A, Rezaei N, Sharafkhah M, Poustchi H, Mobinizadeh M, Mohammadshahi M, Naghavi M, Olyaeemanesh A, Malekzadeh R, Delavari A et al: Exploring the impact of health expenditure and its allocation on neonatal and child mortality at national level across 188 countries from 2000 to 2019: insights from the Global Burden of Disease Study. medRxiv 2024:1–37.
- 95.Gebremeskel AT, Otu A, Abimbola S. Yaya SJBGH: Building resilient health systems in Africa beyond the COVID-19 pandemic response. BMJ Glob Health. 2021;6(6):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Akter S, Voumik LC, Rahman MH, Raihan A, Zimon G. GDP, health expenditure, industrialization, education and environmental sustainability impact on child mortality: Evidence from G-7 countries. Sustainable Environment. 2023;9(1):2269746. [Google Scholar]
- 97.Zakaria M, Tariq S. ul Husnain MI: Socio-economic, macroeconomic, demographic, and environmental variables as determinants of child mortality in South Asia. Environ Sci Pollut Res. 2020;27(1):954–64. [DOI] [PubMed] [Google Scholar]
- 98.Hong J, Yi S, Yoon T. The impact of the COVID-19 pandemic on life expectancy by the level of area deprivation in South Korea. Front Public Health. 2023;11(1):1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Elston JWT, Cartwright C, Ndumbi P, Wright J. The health impact of the 2014–15 Ebola outbreak. Public Health. 2017;143:60–70. [DOI] [PubMed] [Google Scholar]
- 100.Learning from Burundi’s political pivot on COVID-19 vaccines. https://blogs.worldbank.org/en/nasikiliza/learning-burundis-political-pivot-covid-19-vaccines.
- 101.Civil War in Sudan. https://www.cfr.org/global-conflict-tracker/conflict/power-struggle-sudan.
- 102.Second Liberian Civil War. https://en.wikipedia.org/wiki/Second_Liberian_Civil_War.
- 103.2 years since Cyclone Idai and Mozambique has already faced an additional 3 cyclones.
- 104.Nica E, Poliakova A, Popescu GH, Valaskova K, Burcea SG. Constantin A-LD: The impact of financial development, health expenditure, CO2 emissions, institutional quality, and energy Mix on life expectancy in Eastern Europe: CS-ARDL and quantile regression Approaches. Heliyon. 2023;9(11):1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Zarulli V, Sopina E, Toffolutti V, Lenart AJPO. Health care system efficiency and life expectancy: A 140-country study. PLoS ONE. 2021;16(7):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Djoumessi YF. The impact of malnutrition on infant mortality and life expectancy in Africa. Nutrition. 2022;103–104:1–12. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: S1 Appendix. Data set
Additional file 2: S2 Appendix. Summary of descriptive analysis results
Additional file 3: S3 Appendix. Regression results
Data Availability Statement
The datasets generated and analysed during the current study are publicly available at Our World in Data database: https://ourworldindata.org/. All data generated or analysed during this study are included in this published article and its supplementary information files.