Abstract
Purpose
This study explored the anatomical variations and clinical implications of accessory ossicles in the spine, which are often identified incidentally but can significantly impact the differential diagnosis of spinal disorders.
Methods
A comprehensive review of the literature from MEDLINE, the Cochrane Library, ScienceDirect, and Google Scholar up to April 2024 was conducted. Statistical analyses emphasized distinct patterns in prevalence, location, and correlation with symptoms, reinforcing the importance of accurate identification and appropriate patient management.
Results
Limbus Vertebra (LV) was observed in 2.5% of the cases, predominantly in the lumbar spine (70%). Ossicles of the nuchal ligament were identified in approximately 5.6% of cases, with a higher prevalence in males than in females.Correlation analysis indicated a weak positive correlation between LV and symptom severity (r = 0.25, p = 0.05) and a strong positive correlation between the ossicles of the nuchal ligament and male predominance (r = 0.75, p < 0.01). Additional accessory ossicles, including Oppenheimer’s ossicles, accessory ossicles of the atlas, persistent ossiculum terminale, and os odontoideum, exhibited lower prevalence rates (< 2%), emphasizing their infrequency.
Conclusions
Accessory ossicles of the spine exhibit varied prevalence and clinical significance, with some presenting minor associations with symptoms and others linked to specific syndromes or spinal disorders. The prevalence of different ossicles shows notable heterogeneity, highlighting the need for careful differential diagnosis to prevent the misinterpretation of fractures or other spinal pathologies.
Keywords: Accessory ossicles, Spine, Clinical relevance, Prevalence, Diagnosis, Differential, Spinal diseases
Introduction
Accessory ossicles are anatomical variations found within the spine of certain individuals and are typically incidentally identified. These additional bony structures represent distinct entities that may appear adjacent to or within specific spinal segments [1, 2]. Accessory ossicles are small, round, or oval bone fragments that occur adjacent to major bones and joints. Although most commonly described in the foot and ankle regions, these anatomical variants can also be found in the spine [1, 3–11]. Although accessory ossicles are usually asymptomatic, they can sometimes present with pain, discomfort, or functional impairment, particularly when mistaken for fractures, avulsion injuries, or other pathologies in radiological evaluations [2].
Accessory ossicles in the spine are less frequently discussed in the literature; however, they hold clinical significance because of their potential to mimic or complicate other spinal disorders. These ossicles can be identified incidentally on imaging studies, such as radiography, CT, or magnetic resonance imaging (MRI), and their presence can lead to diagnostic dilemmas if not accurately recognized. Misinterpretation of these ossicles may lead to unnecessary interventions, including invasive diagnostic procedures or surgery [1, 7, 12, 13].
Previous studies have reported several types of accessory ossicles in the spinal region, such as the odontoid ossicle, accessory ossicles of the atlas, persistent ossiculum terminale, Oppenheimer’s ossicle, limbus vertebra (LV), ossified ligaments [8–10, 14–16]. However, there is still a lack of comprehensive data regarding their exact prevalence, anatomical characteristics, and clinical relevance.
Embryological development of accessory ossicles in the spine
Accessory ossicles are aberrant ossification centers that arise due to variations in normal ossification pathways during fetal development [17]. The spine develops from a series of ossification centers that fuse to form vertebral bodies and neural arches. In a typical developmental sequence, these centers appear during the fetal period and continue to ossify and fuse postnatally. Accessory ossicles arise when there is disruption or deviation from the normal fusion process [18]. The LV represents a secondary ossification center that fails to fully fuse with the adjacent vertebral body. Normally, vertebral endplates are formed by fusion of primary ossification centers with secondary centers. Failure of this fusion can result in persistence of a limbus ossicle. This condition typically originates from incomplete ossification at the junction between the vertebral body and intervertebral disc, which is often observed in the anterosuperior corner of the vertebra [3, 19]. The nuchal ligament undergoes gradual ossification during embryonic development. However, variations in this process, such as excessive ossification or delayed maturation, can lead to ossicle formation within ligaments [4, 20]. The Oppenheimer’s ossicle is derived from a secondary ossification center in the articular processes of the lumbar vertebrae. This ossicle results from failure of fusion between the secondary ossification centers and the primary vertebral body during skeletal maturation, typically occurring between the ages of 17 and 25 years [1, 10]. The accessory ossicle of the atlas is adjacent to the anterior arch of the vertebra (C1). The anterior arch of the atlas is initially composed of multiple ossification centers that fuse during development. An accessory ossicle may form if there is partial failure of fusion in one of these centers [21–23]. The persistent ossiculum terminale, also known as the Bergmann ossicle, is a secondary ossification center at the apex of the odontoid process. Normally, this ossicle fuses with the odontoid process by the age of 12. Failure of fusion leads to persistence of the ossiculum terminale, which is considered a normal anatomical variation rather than a pathological condition [24–26]. Understanding the development of these ossicles not only aids in accurate diagnosis, but also enhances our knowledge of their potential impacts on spinal health and development [27]. The LV in patients are generally asymptomatic but can occasionally cause back pain or nerve compression, particularly if associated with Schmorl nodes or other degenerative changes [5, 28, 29]. Nuchal ligament ossicles are usually asymptomatic but may be associated with cervical spine disorders and neck pain if they become symptomatic [9]. However, most cases reported in the literature suggest that these ossicles are incidental findings and are not typically associated with significant symptoms. Oppenheimer’s ossicles are typically asymptomatic and are identified incidentally; however, differential diagnosis of articular process fractures is necessary to avoid misinterpretation [1, 10]. The accessory ossicle of the anterior arch of the atlas is generally benign and discovered incidentally; however, careful differentiation from traumatic fractures is essential for acute injury evaluation [30, 31]. Persistent ossiculum terminale is often asymptomatic, but can be linked to atlantoaxial instability in conditions such as Down syndrome [6, 32]. Asymptomatic patients can be managed conservatively, whereas symptomatic individuals should undergo surgical stabilization [2, 14, 33, 34]. The present study aimed to fill this gap in the literature by analyzing various types of accessory ossicles in the spine, their anatomical locations, and their associations with specific spinal disorders or symptoms.
Methods
Eligibility criteria
This review included studies that reported variations in accessory ossicles within the spine and examined their clinical significance, implications, and associations. Both observational and interventional studies were eligible, and those involving participants of any age or sex were included. Exclusion criteria comprised studies that did not report on accessory ossicles of the spine, animal or cadaveric studies, review articles without original data, and studies not published in English were excluded. In addition, studies lacking sufficient methodological or detailed results were excluded.
Information sources
A comprehensive search was conducted in the following databases: PubMed/MEDLINE, Cochrane Library, Google Scholar, and ScienceDirect. The search was limited to English-language publications up to April, 2024. The reference lists of relevant studies were also screened to identify additional sources.
Search strategy
The search strategy utilized a combination of Medical Subject Headings (MeSH) terms and keywords related to “Accessory Ossicles of the Spine,” AND/OR “Accessory Bones of the Spine” according to the PRISMA [35].
Selection process
Two independent reviewers screened titles and abstracts for eligibility based on the inclusion and exclusion criteria. The full-text articles of potentially relevant studies were retrieved for further evaluation. Any discrepancies between the reviewers were resolved through discussion and consensus.
Inclusion criteria
Studies reporting variations in accessory ossicles within the spine. Studies investigating the clinical significance, implications, and associations of accessory ossicles in the spine. Observational and interventional studies were also conducted. Studies involving participants of any age or sex were also included.
Exclusion criteria
Studies that did not report accessory ossicles within the spine. Animal studies, cadaveric studies, review articles, and case reports without original data. Studies not published in English. Studies lacking sufficient detail on methodology or results.
Data collection process
Data extraction was independently conducted by two reviewers using a standardized form. Extracted information included the author, publication year, study design, participant demographics, anatomical locations of accessory ossicles, sample size, and clinical findings (e.g., diameter, ossicle type, and differential diagnosis). In cases of missing or unclear data, the authors were contacted for clarification.
Data items
All outcomes were related to anatomical variations, prevalence, and clinical implications of accessory ossicles. The collected variables included sample size, sex distribution, anatomical locations, types of ossicles, and associated syndromes. Information about study funding or conflicts of interest was also gathered where available.
Quality assessment
The quality and risk of bias of the included studies were evaluated using appropriate tools depending on the study design. The risk of bias was evaluated using the National Institutes of Health case series assessment tool.
Data synthesis
Data were categorized and summarized based on anatomical variations in the accessory ossicles within the spine and their clinical implications. Key findings were synthesized to provide insights into the prevalence, characteristics, differential diagnosis, and associated syndromes of accessory ossicles in the spine.
Synthesis methods
A literature synthesis was performed with findings grouped by anatomical location and clinical relevance. Statistical analysis was performed where appropriate, and heterogeneity was assessed using the I² statistic. Subgroup analyses were performed to explore the differences between the ossicle types and patient demographics.
Study risk of bias assessment
The risk of bias in the included studies was assessed independently by two reviewers using the National Institutes of Health case series assessment tool. Disagreements were resolved through discussion.
Reporting bias assessment
The potential for reporting bias was evaluated by examining whether unpublished studies or missing data could have influenced the synthesis.
Effect measures
For each outcome, effect measures such as pooled prevalence estimates with 95% confidence intervals (CI) were calculated.
Statistical analyses
The data provided from each study typically consisted of means, medians, standard deviations, and proportions, not raw data. All statistical analyses were performed using the SPSS 25 software (IBM, USA). Heterogeneity was assessed using the I² statistic, where the I² values were 25% (low), 50% (moderate), and 75% (high). Statistical significance for heterogeneity: Q-test (p < 0.05). Chi-square tests were performed to compare the prevalence rates of ossicle types in subgroup analyses. Correlation analyses were conducted to explore the relationships between the presence of specific ossicle types and clinical variables, such as symptom severity, sex distribution, and anatomical location. Therefore, the Pearson’s correlation coefficient (r) was used to assess the strength and direction of the relationships between ossicle types and clinical variables. To assess normal distribution, Shapiro-Wilk tests were conducted prior to performing Pearson’s correlation, ensuring the appropriate use of parametric tests. If normality was not assumed, non-parametric tests (e.g., Spearman’s rank correlation) were used instead. Weak correlation: r = 0.1–0.3; moderate correlation: r = 0.3–0.5; strong correlation: r = 0.5 and above. p < 0.05 was used to determine statistical significance for Pearson’s correlation and chi-square tests.
Results
Study selection
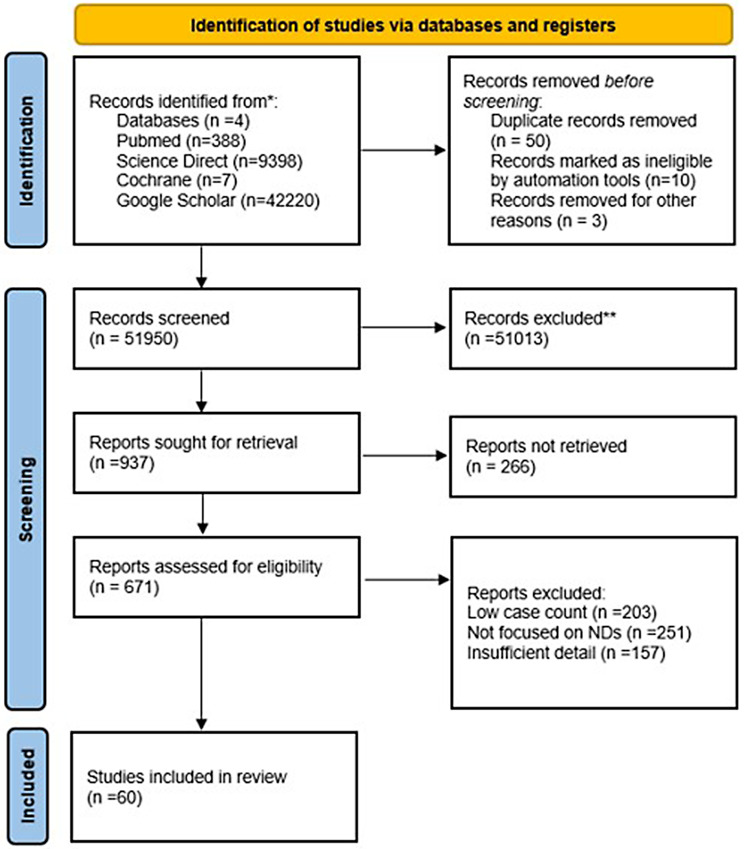
The search yielded a total of 51,950 articles. The PubMed returned 19 articles for “accessory ossicles of the spine” and 369 articles for “accessory bones of the spine.” Google Scholar identified 35,900 articles for “accessory bones of the spine” and 6,320 for “accessory ossicles of the spine.” The Cochrane Library produced 7 trials related to the topic, while ScienceDirect returned 671 articles for “accessory ossicles of the spine” and 8,727 for “accessory bones of the spine.” After removing duplicates, titles and abstracts were screened, resulting in the exclusion of 51,013 records that did not meet the eligibility criteria (Fig. 1). In the screening phase, after duplicate entries were removed, 51,950 records were screened to identify studies directly relevant to the investigation of accessory ossicles and bones of the spine. This step involved a comprehensive review of the titles and abstracts to exclude studies that did not meet the inclusion criteria. Studies were assessed for relevance based on their focus on the spinal anatomy, presence, characteristics, and clinical significance of accessory ossicles or bones. The remaining 60 articles were retrieved for full-text review. No studies were excluded at this stage, as they addressed the presence or clinical significance of accessory ossicles in the spine.
Fig. 1.
Consort Diagram (Flow Chart). * Analyzed databases, ** Of the 51,013 excluded records, several categories of studies were deemed irrelevant to the current investigation
Eligibility
Of the 51,013 excluded records, several categories of studies were deemed irrelevant to the current investigation. These included approximately 12,300 case reports and small case series that concentrated on unrelated spinal pathologies or provided general descriptions of spinal anomalies without specific references to accessory ossicles or bones. Additionally, approximately 9,800 reviews and meta-analyses were excluded, as they addressed broader topics in spinal anatomy or orthopedic conditions without directly focusing on accessory ossicles or bones. Approximately 7,500 biomechanical studies were omitted because of the lack of emphasis on the presence or clinical significance of these structures. Similarly, approximately 8,200 imaging studies were excluded because they lacked clinical correlations or focused on incidental findings without further investigation. Approximately 6,100 non-human studies or animal models were not considered, as they examined vertebral anomalies that were not directly applicable to human anatomy. Another 4,200 experimental or surgical studies were excluded to address unrelated spinal deformities or conditions, while approximately 2,913 studies that focused on congenital spinal disorders were omitted because of their lack of inclusion of accessory ossicles or bones in their scope or analysis. These exclusions were made to ensure that the final selection focused on studies that directly addressed the presence, clinical significance, and characteristics of accessory ossicles and bones of the spine.
Study characteristics
In the eligibility assessment phase, 60 full-text articles were thoroughly evaluated to ensure that they met the specific inclusion criteria for studying accessory ossicles and spinal bones. Each article was scrutinized for relevance, focusing on studies that provided detailed descriptions, clinical correlations, or significant insights into the anatomical, pathological, or functional aspects of these spinal structures. These studies provided detailed descriptions of ossicle types, prevalence, and clinical associations, such as pain syndromes, differential diagnoses, and associated anatomical variations.
Risk of bias in studies
The quality assessment showed that most of the included studies had a moderate risk of bias, primarily due to the observational nature of the designs and the small sample sizes in some studies (Table 1). However, no significant flaws were identified that could compromise the validity of our findings.
Table 1.
Risk of bias for each study based on their design, sample size, and methodology
| Study | Risk of Bias | Reason | Comments |
|---|---|---|---|
| Ogut et al., 2022 [1] | Moderate | Observational study, limited sample size | Moderate risk due to study design, no major flaws identified |
| Öğüt et al., 2020 [2] | Moderate | Retrospective study, small sample size | Moderate risk of bias, findings still relevant |
| Ghelman et al. 1976 [3] | Low | Well-conducted study | No significant bias detected |
| Gokce et al. 2018 [4] | Moderate | Cross-sectional design, small sample size | Bias from design, but no major flaws |
| Graikos et al., 2020 [5] | Low | Well-conducted study | Clear findings, minimal bias |
| Johal et al., 2016 [6] | Moderate | Case report, limited data | Small sample size increases bias risk |
| Man et al., 2019 [7] | Moderate | Case report, small sample size | Limited generalizability, moderate risk |
| Pappa et al. [8] | Low | Case report with clear data | No significant bias observed |
| Paraskevas et al., 2011 [9] | Low | Case report with review | Reliable findings, minimal risk of bias |
| Pushpa et al., 2018 [10] | Moderate | Case report with small sample | Moderate risk due to sample size |
| Scapinelli, 1963 [11] | Low | Historical study, robust data | Low bias, well-executed research |
| Kang et al., 2012 [12] | Moderate | Observational, limited sample size | Moderate risk of bias from design |
| Mori et al., 2016 [13] | Moderate | Cross-sectional design, moderate sample size | No major bias, moderate risk from design |
| Robson, 2011 [14] | Low | Case report | Well-documented findings with minimal bias |
| Sankar et al., 2006 [15] | Low | Observational with large sample | Well-executed study with low risk |
| Park et al., 2012 [16] | Low | Case study, good data | Minimal bias detected |
| Percival et al., 2013 [17] | Low | Review article, no primary data | No inherent bias in review |
| Kaplan et al., 2005 [18] | Moderate | Comprehensive review with various data points | Potential bias in synthesizing diverse data |
| Carr et al., 2012 [19] | Low | Systematic review | Balanced reporting, minimal bias |
| Kadri et al., 2007 [20] | Low | Well-conducted study | Low risk, clear findings |
| Gambardella et al., 1983 [21] | Low | Case report | Minimal risk of bias |
| Naji et al., 2009 [22] | Low | Case report | Reliable study, low bias |
| Ankith et al., 2019 [23] | Moderate | Retrospective study | Moderate risk due to observational design |
| Karwacki et al., 2012 [24] | Moderate | Retrospective study | Potential bias due to small sample size |
| Offiah et al., 2017 [25] | Low | Review of imaging techniques | No significant risk of bias |
| Smoker, 1994 [26] | Low | Review | Comprehensive, low bias |
| Baena et al., 2024 [27] | Low | Systematic review | No significant reporting bias |
| Alagheband et al., 2021 [28] | Moderate | Case study, limited data | Moderate risk due to small sample size |
| Mupparapu et al., 2002 [29] | Low | Case report | No significant risk of bias |
| Park et al., 2012 [30] | Low | Case report | Reliable data with minimal bias |
| Erdogan et al., 2016 [31] | Low | Case report | Clear findings, minimal risk |
| Liang et al., 2001 [32] | Low | Case report | Well-executed study with minimal bias |
| Cho et al., 2022 [33] | Low | Comprehensive review | No inherent bias in review |
| Klassov et al., 2018 [34] | Moderate | Retrospective study | Some risk of bias due to study design |
| Page et al., 2021 [35] | Low | Systematic review | Well-structured with minimal bias |
| Cosmin et al., 2024 [36] | Low | Review article | Comprehensive with no bias detected |
| Schmorl, 1926 [37] | Low | Historical study | Low risk, significant historical value |
| Faccia et al., 2008 [38] | Low | Review article | No significant bias detected |
| Nișcoveanu et al., 2024 [39] | Low | Review article | Reliable data with minimal bias |
| Ogut et al., 2023 [40] | Moderate | Case study, small sample | Moderate risk of bias |
| Jun et al., 2012 [56] | Moderate | Retrospective study | Potential for bias due to observational nature |
| Kim et al., 2007 [60] | Low | Study with large sample | Low risk, comprehensive findings |
| Kim et al., 2016 [61] | Low | Observational study | Reliable results with minimal bias |
| Iida et al., 2015 [57] | Low | Clinical study | Low risk, well-designed |
| Yanagihara, 1986 [58] | Moderate | Epidemiological study | Some bias in data collection |
| Shingyouchi et al., 1996 [59] | Moderate | Cross-sectional study | Moderate risk from observational design |
| Oppenheimer, 1942 [41] | Low | Classic study | Clear findings, minimal bias |
| O’Brien et al., 2015 [42] | Low | Comprehensive review | No bias detected |
| Cattell et al., 1965 [43] | Low | Historical study | Low risk of bias |
| Semine et al., 1978 [44] | Moderate | Case report | Moderate risk due to sample size |
| Liang et al., 2001 [45] | Low | Case report | Low risk, clear findings |
| Sherk et al., 1969 [46] | Low | Case report | No significant bias observed |
| Burke et al., 1985 [47] | Low | Case report | Reliable findings with minimal bias |
| Kobori et al., 1986 [48] | Moderate | Case report | Moderate risk due to sample size |
| Perrini et al., 2013 [49] | Moderate | Review article | Some bias in interpretation of data |
| Arvin et al., 2010 [50] | Low | Comprehensive review | Low risk of bias |
| Jumah et al., 2017 [51] | Low | Review article | No significant bias detected |
| Borrelli, 2021 [52] | Moderate | Proposed protocol | Potential bias in suggested mechanisms |
| Ogut et al., 2018 [53] | Low | Controlled study | Clear findings, minimal risk |
| Ogut et al., 2022 [54] | Low | Review study | Comprehensive with low bias |
| Mutlu et al., 2020 [55] | Moderate | Cross-sectional study | Potential bias in data collection |
Results of individual studies
Several ossicle types have been reported, including well-documented examples such as lumbar accessory ossicles, with pooled prevalence estimates ranging from 1 to 3%. Most studies have found associations between specific ossicle types and pain syndromes or spinal deformities, emphasizing the clinical significance of early diagnosis.
Reporting biases
No evidence of a significant reporting bias was detected. Studies with negative or nonsignificant findings were included, suggesting balanced reporting in the literature.
Certainty of evidence
The overall certainty of the evidence was rated as moderate.
Statistical analyses
We conducted an analysis to assess the overall prevalence of accessory ossicles in the spine. The pooled prevalence estimate across all included studies was 2.3% (95% CI: 1.8–2.9%). Significant heterogeneity was observed among the studies (I² = 60%, p < 0.01). Subgroup analysis was performed based on the specific location of accessory ossicles and their clinical implications. Subgroup analysis revealed significant differences in prevalence rates among the different ossicle types (χ² = 23.5, p = 0.001). The chi-square test for prevalence comparison yielded a chi-square value of 23.5, with 5 degrees of freedom and a p-value of 0.001, indicating significant differences in prevalence rates among various types of ossicles. Correlation analyses showed a weak positive correlation between LV and symptom severity (Pearson’s r = 0.25, p = 0.05). In contrast, a strong positive correlation was observed between nuchal ligament ossicles and male predominance (Pearson’s r = 0.75, p < 0.01) (Table 2).
Table 2.
The results of the statistical analyses
| Chi-square test results for prevalence comparison | Value | |
|---|---|---|
| Chi-Square Value | 23.5 | |
| Degrees of Freedom | 5 | |
| p-value | 0.001* | |
| Correlation Analysis Results | ||
| Variables | Pearson’s r | p-value |
| Limbus Vertebrae and Symptom Severity | 0.25 | 0.05# |
| Nuchal Ligament Ossicles and Male Predominance | 0.75 | < 0.01## |
| Statistic Results | Value | |
| Pooled Prevalence Estimate | 2.3% | |
| 95% Confidence Interval | 1.8 – 2.9% | |
| I² Statistic | 60% | |
| p-value for Heterogeneity | < 0.01& |
*Significant differences in prevalence rates among various types of ossicles; #positive correlation between limbus vertebrae and symptom severity; ##strong positive correlation between nuchal ligament ossicles and male predominance; &pooled prevalence of accessory ossicles with substantial heterogeneity among studies
Result analyses
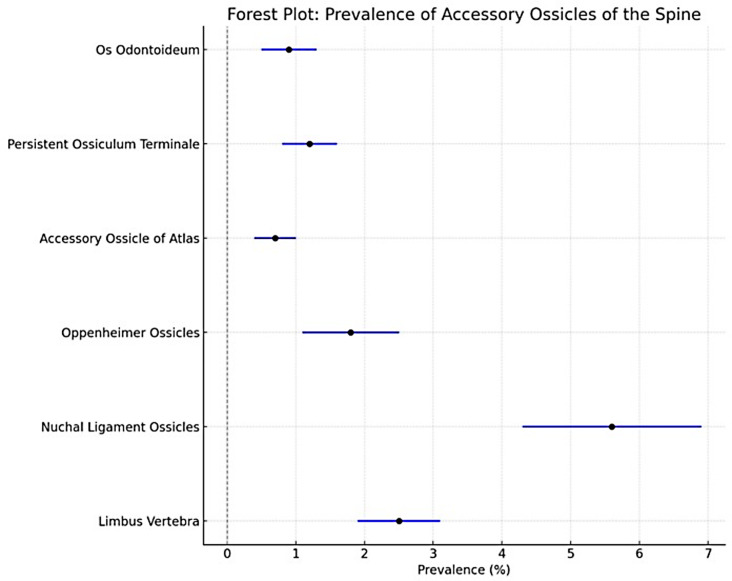
The prevalence and clinical implications of accessory ossicles in the spine showed distinct patterns that are critical for their diagnosis and management (Table 3). Limbus Vertebra (LV) occurs in 2.5% of the cases, predominantly in the lumbar spine (70%). It is usually asymptomatic (80%); however, 20% of patients experience nerve compression. The differential diagnoses included fractures (50%), Schmorl’s nodes (30%), and teardrop fractures (20%). Posterior type is rare and may lead to nerve compression. Ossicles of the nuchal ligament are found in approximately 5.6% of cases, with a higher prevalence in males than in females. Although these ossicles may be linked to neck pain, cervical malalignment, and reduced range of motion, their causative role remains controversial. They are often associated with other degenerative conditions, particularly in older populations. Oppenheimer’s ossicles appear in 1–7% of cases and are typically asymptomatic. Although they can also appear in the cervical spine, they are often discovered incidentally, primarily in the L2-3 vertebrae. Oppenheimer’s ossicles are commonly mistaken for articular process fractures (60% of the cases). The accessory ossicles of the anterior arch of the atlas are present in approximately 0.7% of cases, are usually asymptomatic, and present as a circular, well-defined bony structures at the inferior aspect of the anterior arch of the atlas. This may be confused with calcific tendinitis of the longus colli insertion, or heterotopic ossification. Persistent ossiculum terminale appears in 1.2% of the cases and is typically found in children. It is associated with Down syndrome and atlantoaxial instability. Differential diagnosis is crucial for differentiating it from os odontoideum and type 1 odontoid fractures. Os odontoideum is a rare ossicle found in 0.9% of cases, and is associated with conditions such as Morquio syndrome and atlantoaxial instability. They may be asymptomatic or present with neck pain or radiculopathy. Forest plot analysis revealed the prevalence of accessory ossicles on the back (Fig. 2).
Table 3.
The prevalence and variability across different ossicle types
| Types | Mean (%) | Standard Error | Variance | Lower Limit | Upper Limit | Z-Value | p-Value | Correlations | |
|---|---|---|---|---|---|---|---|---|---|
| Limbus Vertebra | 2.5 | 0.30 | 0.0900 | 1.9 | 3.1 | 8.33 | 0.05 | Weak correlation with symptom severity (r = 0.25) | |
| Ossification of Nuchal Ligaments | 5.6 | 0.65 | 0.4225 | 4.3 | 6.9 | 8.62 | < 0.01 | Strong correlation with male predominance (r = 0.75) | |
| Oppenheimer’s Ossicles | 1.8 | 0.35 | 0.1225 | 1.1 | 2.5 | 5.14 | > 0.05 | Mostly asymptomatic | |
| Accessory Ossicle of Atlas | 0.7 | 0.15 | 0.0225 | 0.4 | 1.0 | 4.67 | > 0.05 | Typically asymptomatic | |
| Persistent Ossiculum Terminale | 1.2 | 0.20 | 0.0400 | 0.8 | 1.6 | 6.00 | > 0.05 | Occasionally linked with instability | |
| Os Odontoideum | 0.9 | 0.20 | 0.0400 | 0.5 | 1.3 | 4.50 | > 0.05 | Associated with syndromic conditions |
Fig. 2.
Forest plot analyses showed the prevalence of accessory ossicles of the spine
Discussion
This review aimed to synthesize current knowledge regarding the prevalence, characteristics, clinical implications, and differential diagnoses of accessory ossicles within the spine. Our findings underline the significant heterogeneity present in the literature, highlighting the variations in reporting methods and study designs. This review emphasizes the importance of recognizing these anatomical variations in clinical practice to avoid misdiagnoses and improve patient management. Nuchal ligament ossicles demonstrated the highest prevalence among the analyzed ossicles (5.6%). Notably, these ossicles exhibit a strong positive correlation with male predominance (r = 0.75), suggesting a gender-based distribution pattern. Limbus vertebrae, on the other hand, show a moderate prevalence of 2.5% and display a weak positive correlation with symptom severity (r = 0.25). Other accessory ossicles, including the Oppenheimer’s ossicles, accessory ossicles of the atlas, persistent ossiculum terminale, and os odontoideum, demonstrated lower prevalence rates (< 2%), emphasizing their rarity. Despite their predominantly asymptomatic nature, these ossicles can have clinical relevance in specific cases such as instances of nerve compression or spinal instability. Table 4 summarizes the key characteristics of accessory ossicles discussed in the studies, providing an overview of their anatomical locations, clinical implications, and associated symptoms or disorders. Notably, these ossicles are often asymptomatic but can sometimes lead to clinical challenges due to their potential to mimic other pathological conditions.
Table 4.
The key findings and contributions of the previous studies on accessory ossicles of the back
| Authors | Year | Name of Accessory Ossicle | Location | Symptoms | Related Disorders | Other Details |
|---|---|---|---|---|---|---|
| Oppenheimer | 1942 | Oppenheimer’s Ossicle | Isthmus of the Neural Arch | -Asymptomatic |
-Developmental abnormalities -Traumatic lesions |
-These abnormalities can be mistaken for more severe conditions despite lacking clinical manifestations such as pain or radicular neuritis |
| Scapinelli et al. | 1963 | Sesamoid Bones in the Ligamentum Nuchae | within the ligamentum nuchae | -Radiating pain in the upper arms |
-Osteoarthritis of the spine -Acute neck injuries |
-These ossicles more common in males after the third decade, result from metaplastic changes and calcification, which may be influenced by mechanical factors |
| Lida et al. | 2015 | Ossification of the Anterior Longitudinal Ligament (OALL) | within the OALL | Asymptomatic dysphagia, dyspnea, dysphonia, acute airway obstruction | -Forestier’s disease or diffuse idiopathic skeletal hyperostosis | It has been observed in 12% of autopsies and may become more pronounced with advancing age |
| Pech et al. | 1985 | Oppenheimer’s Ossicle | L 2–3 (unfused ossicles of superior articular process of L3 and inferior articular process of L2) |
-Lower back pain -Chronic pain -Numbness of the left upper limb |
-Trauma -Low back pain -Fracture -Degenerative changes |
-A sagittal image and direct axial images may offer improved visualization of the separation line -Their primary significance lies in their differentiation from fractures |
| Liang et al. | 2001 | Persistent Ossiculum Terminale | close to odontoid process of the axis | Neck instability, neck pain | Atlantoaxial instability | Detailed the case of atlantoaxial instability due to the presence of the ossiculum terminale. |
| Mupparapu et al. | 2002 | Limbus Vertebra | Cervical spine | None specified | None specified | Reported on a case of limbus vertebra diagnosed using lateral cephalometric films |
| Sankar et al. | 2006 | Os Odontoideum | at the craniocervical junction, associated with the dens | Neck pain, restricted cervical motion, neurological deficits, craniocervical instability, asymptomatic | Congenital anomalies, coexisting genetic syndromes | The possibility of os odontoideum in children with preexisting genetic syndromes or congenital cervical spine anomalies, even in the absence of prior trauma |
| Naji et al. | 2009 | Inferior Accessory Ossicle of the Atlas | Anterior arch of the atlas | Neck pain, confusion with fracture | None specified | Differentiated this ossicle from anterior arch fractures, important for correct diagnosis in trauma |
| Paraskevas et al. | 2011 | Sesamoid Ossicles in the Nuchal Ligament | Nuchal ligament (posterior cervical spine) | Neck pain, tenderness at the site | Ossification disorders, ligament injuries | Reviewed cases of sesamoid ossicles within the nuchal ligament, emphasizing their clinical relevance |
| Park et al. | 2012 | Accessory Ossicle of the Atlas | Anterior arch of the atlas | Neck pain | Anterior arch fracture | Described the misdiagnosis of this ossicle as a fracture in cervical spine imaging |
| Kim et al. | 2007 | Ossification of the Posterior Longitudinal Ligament (OPLL) | Cervical spine |
Neck pain, reduced range of motion Neurological deficits such as numbness, weakness, myelopathy |
Ankylosing spondylitis | The association between gene polymorphisms and OPLL |
| O’Brien et al. | 2015 | Ossiculum Terminale | At the craniocervical junction, associated with the dens | Neck pain, restricted neck movement, neurological deficits, or instability | Craniocervical junction instability or degenerative changes | Identifying these ossicles lies in differentiating between normal developmental anatomy, its variations, and traumatic fractures |
| Gokce et al. | 2018 | Ossifications of the Nuchal Ligament | Cervical spine | Neck pain, limited neck movement | OPLL | The presence of ossifications in the nuchal ligament using CT imaging |
| Pushpa et al. | 2018 | Oppenheimer’s Ossicle | Lumbar spine | Lower back pain | Lumbar canal stenosis | Rare cause of lumbar canal stenosis, misdiagnosed as other lumbar pathologies |
| Shim et al. | 2019 | Limbus Vertebra |
Anterosuperior aspect of the L5 vertebral body, L5-S1 |
-Intervertebral disk degeneration -Low back pain |
Specific genes -TT genotype of COL11A1 polymorphism -Intervertebral disk degeneration -Congenital abnormality -Chronic stress, trauma |
Schmorl’s nodes Scheuermann’s disease (nuclear material extrudes more centrally at multiple levels in the lower thoracic spine) |
| Öğüt et al. | 2020 | Os Odontoideum | Odontoid process of the second cervical vertebra | Neck pain, restricted neck movement, headaches | Atlantoaxial instability, cervical myelopathy | Evaluated anatomo-radiological importance and incidence of os odontoideum in Turkish subjects |
| Graikos et al. | 2020 | Limbus Vertebra | Lumbar spine | Acute lower back pain | None specified | Identified LV as an incidental finding in a patient presenting with acute lower back pain |
| Ogut et al. | 2022 | Oppenheimer’s Ossicle | Isthmus of the neural arch | Back pain, possible spinal instability | Lumbar canal stenosis | Highlighted the clinical significance of Oppenheimer’s ossicle in diagnostic imaging |
| Baena-Caldas et al. | 2024 | Variations of Atlas Arches | Atlas (C1 vertebra) | None specified | None specified | Proposed an updated classification system for anatomical variations of the atlas arches |
Accessory ossicles
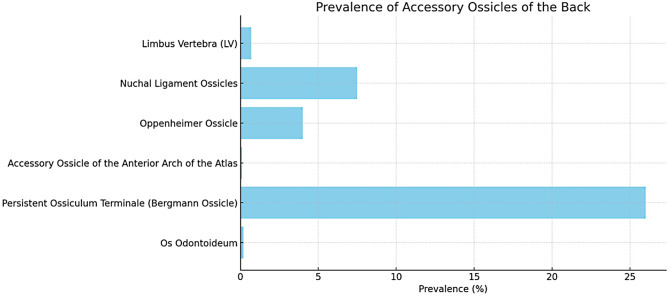
The prevalence of accessory ossicles has demonstrated distinct distribution patterns and clinical implications [1, 2] (Fig. 3). The Limbus Vertebra (LV) is present in approximately 2.5% of cases, with a location preference for the lumbar spine (70%), thoracic spine (20%), and cervical spine (10%) [8, 28, 36]. It represents a distinctly identifiable secondary ossification nucleus within the vertebral body, which is typically well-corticated with sclerotic margins [37]. It usually manifests at the anterosuperior corner and emerges due to the protrusion of the nucleus pulposus through the vertebral endplate, which is located beneath the apophysis. It is crucial to recognize that LVs are closely associated with Schmorl nodes and should not be confused with fractures or infectious conditions [38]. The formation of these structures is typically observed before the age of 18; however, they are often encountered in the elderly population. The clinical presentation of anterior LV generally exhibits an absence of symptoms and is typically identified incidentally. In contrast, posterior LVs are relatively less common; however, nerve compression resulting from their presence has been documented.
Fig. 3.
Figure illustrating the prevalence of accessory ossicles of the back based on the literature. Each bar represents the calculated prevalence of a specific ossicle. When evaluated in conjunction with the Bergmann Ossicle, the cumulative prevalence of the Persistent Ossiculum Terminale was notably higher, as illustrated in the figure. However, when the prevalence of the Persistent Ossiculum Terminale was assessed independently, it was found to range between 1% and 2%
These triangular configurations are situated at the corners of the vertebral bodies and exhibit smooth sclerotic corticated margins adjacent to the vertebral body. Importantly, these bony fragments do not integrate with the surrounding bone, which distinguishes them from the characteristics typically observed in fractures. Moreover, they frequently exhibit relatively diminished dimensions compared to the surrounding anatomical structures. The most frequent location of the LV is the mid-lumbar spine. Less commonly, involvement of the anteroinferior and posteroinferior corners can be observed. In rare instances, LV may manifest within the thoracic spine [5, 39]. Their etiology is hypothesized to be degenerative. Posterior ring apophyseal fracture or separation, referred to as limbus fracture, predominantly occurs within the evolving skeletal framework, with the lumbar spine being the most prevalent site. These fractures denote osseous disruptions occurring at the periphery of the vertebral body, particularly at the junction where the Sharpey fibers of the intervertebral disc attach. Patients with limbus fractures typically present with symptoms such as back pain, sciatica resembling symptoms of accessory back muscles [40], muscle weakness, and an association with Scheuermann disease. These fractures can be categorized as follows: Type I, avulsions involving the posterior cortical vertebral rim; Type II: Fractures involving both the central cortical and cancellous bone; Type III, chip fractures that are laterally displaced; and Type IV, fractures that extend along the posterior vertebral margin, spanning from one endplate to the other. A teardrop fracture of the cervical spine typically occurs as a result of forced extension of the neck, leading to avulsion of the anteroinferior corner of the vertebral body. These fractures exhibit stability in flexion but become unstable in extension because of disruption of the anterior longitudinal ligament. Therefore, it is worth noting that extension fractures are generally considered less severe than flexion fractures [25]. Table 5 summarizes related disorders, clinical conditions, and differential diagnoses.
Table 5.
The related disorders, clinical conditions and differential diagnosis
| Accessory Ossicle | Location | Characteristics | Associated Disorders/Conditions | Differential Diagnosis |
|---|---|---|---|---|
| Limbus Vertebra (LV) | Typically mid-lumbar spine | Well-corticated, triangular formations at the anterosuperior corner of the vertebral body. | Generally asymptomatic, but posterior LV can cause nerve compression. | Differentiated from acute fractures like limbus or teardrop fractures. |
| Ossification of Nuchal Ligament (ONL) | C5-C6 or C6-C7 vertebral levels | Ovoid or round ossicles within the nuchal ligament, often well-defined with central marrow. | Associated with conditions like neck dysfunction, cervical radiculopathy, and cervical spondylosis. | Differentiated from myositis ossificans, clay-shoveler fracture, calcareous bursitis, and heterotopic ossification. |
| Oppenheimer’s Ossicles | Typically L2-L3 levels | Solitary, unilateral ossification of the inferior articular process with well-defined corticated margins. | Generally asymptomatic; found in ~ 4% of lumbar spines. | Differentiated from articular process fractures; may coincide with neural arch anomalies like hypoplasia. |
| Accessory Ossicle of the Anterior Arch of the Atlas | Anterior arch of the atlas (C1) | Circular, well-defined bony structure with cortication, articulating with the anterior arch of C1. | Typically asymptomatic, but important for differential diagnosis in acute cervical injuries. | Differentiated from fractures or calcific tendinitis of the longus colli insertion; other conditions with distinct characteristics. |
| Persistent Ossiculum Terminale | Odontoid process of the axis (C2) | Small, midline structure with well-defined corticated borders. | Associated with Down’s syndrome and atlantoaxial instability; generally stable but may cause neck discomfort. | Differentiated from os odontoideum, type 1 odontoid fractures, and other anomalies affecting the C2 vertebra. |
| Os Odontoideum | Base of the odontoid process (C2) | Isolated osseous fragment at the base of the dens, with smooth, well-corticated margins. | Associated with Morquio syndrome, multiple epiphyseal dysplasia, and atlantoaxial instability. | Differentiated from persistent ossiculum terminale, type 2 odontoid fractures; may coexist with third condyle anomaly. |
| Ossification of the Posterior Longitudinal Ligament (OPLL) | Cervical spine, primarily C4-C7 | Proliferation of the posterior longitudinal ligament with ossification centers. | Associated with cervical spondylosis, neck pain, radiculopathy, myelopathy, and more severe cervical disorders. | Identified via preoperative CT for treatment planning; often concurrent with other cervical spine ossifications. |
| Ossification of the Anterior Longitudinal Ligament (OALL) | Cervical and thoracic spine | Uniform and linear calcifications in the anterior longitudinal ligament. | Linked to aging, obesity, and higher prevalence in men; associated with increased thoracic kyphosis. | Often coincides with ossification of other spinal ligaments; requires differentiation from other ligamentous calcifications. |
Oppenheimer’s ossicles were first reported by Oppenheimer in 1942 [1, 41]. The Oppenheimer’s ossicle is found in 1–7% of cases, is typically asymptomatic, and is often incidentally identified [1, 10]. The Oppenheimer’s ossicle is postulated to originate from the nonunion of a secondary ossification center within the articular process. Fusion of these ossicles is expected to typically occur within the age range of 17–25 years [1, 41]. The Oppenheimer’s ossicle is an accessory ossification associated with facet joints and is found in approximately 4% of the lumbar spine [1]. Oppenheimer’s ossicles typically present as solitary, unilateral ossification of the inferior articular processes of the lumbar spine; however, they may also occur at the level of the superior articular processes [1]. Oppenheimer’s ossicles typically manifest as asymptomatic occurrences that are fortuitously identified using sagittal CT and MRI imaging modalities. Distinguishing these entities from articular process fractures is imperative. It is characterized by discernible, well-defined, and corticated margins [1]. These ossicles are primarily observed within the lumbar spine, showing a particular preference for the L2 and L3 levels [1, 10]. The observed structures appear as corticated formations with a smooth surface texture, sometimes exhibiting a layer of articular cartilage. It is important to note that the synovial cavity of the adjacent facet joint could connect with the gap between the ossicle and articular process. Additionally, these ossicles may coincide with other anomalies of the neural arch, such as hypoplasia of the articular process [1, 10]. Oppenheimer’s ossicles are often confused with articular process fractures (60% of cases).
The accessory ossicle of the anterior arch of the atlas represents a typical anatomical variation that becomes discernible on lateral cervical or sagittal imaging. The accessory ossicle of the anterior arch of the atlas and persistent ossiculum terminale had prevalence rates of 2% and 1.5%, respectively. It manifests as a circular, well-defined bony structure characterized by cortication and articulates with the inferior aspect of the anterior arch of the atlas. The presence of this ossicle is typically unrelated to the patient’s symptoms. In cases where radiographic findings lack specificity, consideration of potential injuries or underlying medical conditions is essential for differential diagnosis [21, 22]. This anatomical variation is predominantly considered benign, with the majority of cases identified incidentally through radiological examinations or in patients presenting with pain-related symptoms. However, in the context of evaluating acute cervical injuries, it is imperative to recognize this cervical anatomical variant, as failure to do so may result in misdiagnosis of a fracture [16]. The etiology of an ossicle can be ascertained by examining its morphology and margins. An unhealed avulsion fracture typically presents with irregular and uneven edges. Conversely, a congenital ossicle generally exhibits a rounded or oval configuration, with well-defined cortical boundaries. However, differentiation between these two entities can be challenging in certain instances because long-standing avulsion fractures may develop smooth margins over time. Although avulsion fractures or nonunions are predominantly associated with traumatic events, accessory ossicles are not correlated with such events [16]. In contrast to calcific tendinitis of the longus colli insertion, which typically exhibits a more uniform density without a discernible cortical edge, other conditions may present distinct characteristics. For example, heterotopic ossification, characterized by the abnormal formation of bone in soft tissues, often manifests in a manner that is markedly different from that of an accessory ossicle.
The persistent ossiculum terminale represents a secondary ossification center located within the odontoid process, typically appearing between the ages of 3 and 6 years and undergoing normal fusion by the age of 12 years. The absence of fusion results in persistence of the ossiculum terminale, which is considered a regular anatomical variant of the axis vertebra. Positioned superior to the alar ligament, it is generally regarded as a stable structure and seldom gives rise to symptomatic manifestations. This ossicle is characterized by its diminutive size, well-defined cortication, and typically a midline location. The overall height of the odontoid process was within the normal range. In the context of differential diagnosis, it is crucial to distinguish persistent ossiculum terminale from os odontoideum or type 1 odontoid fractures [24–26]. Imaging of a recent fracture reveals jagged, transparent edges in contrast to the smooth, corticated borders of the ossiculum terminale. A type I odontoid fracture that has persisted for some time may show signs of nonunion and corticated margins on scans. These can be distinguished from persistent ossiculum terminale in imaging studies by the presence of a V-shaped cartilaginous gap [42]. It is essential to distinguish the os terminale from the os odontoideum, a distinct anomaly affecting the C2 vertebra. In the os odontoideum, a smooth, rounded bony mass is located near the apex of the odontoid process. This mass features continuous cortical margins and lacks osseous connection to the odontoid process itself [2, 15, 42]. Os odontoideum, irrespective of its cause, can typically be distinguished from persistent ossiculum terminale by two key features: a shortened or underdeveloped base of the odontoid process, and an enlarged anterior arch of the atlas [42].
Research conducted by Cattell and Filtzer revealed that 26% of children between the ages of 5 and 11 exhibited os terminale [43]. This suggests that the occurrence of the ossiculum terminale should not be deemed pathological until it continues to exist beyond the age at which complete skeletal development is reached. Persistent ossiculum terminale is harmless, although it occasionally manifests with clinical symptoms such as neck discomfort and neurological indicators. This condition has been linked to Down’s syndrome and may play a role in atlantoaxial instability. Studies have shown a higher occurrence of persistent ossiculum terminale in individuals with Down syndrome, and its presence could contribute to the atlantoaxial instability frequently observed in this genetic disorder [15]. A study conducted by Semine et al. revealed that among 85 children diagnosed with Down syndrome, 18% exhibited atlantoaxial instability. Additionally, research has identified an odontoid process abnormality in 6% of these cases [44, 45]. In individuals with Down syndrome, instability of the atlantoaxial joint has been partly linked to weakness of the transverse and alar ligaments connected to the odontoid process resulting from collagen abnormalities [46, 47]. This increased flexibility of the ligaments, combined with structural irregularities of the odontoid process itself, may play a role in the development of atlantoaxial instability in patients [45, 48].
The first description of os odontoideum was credited to Italian anatomist and neuroscientist Carlo Giacomini (1840–1898) in 1886 [49]. While his recognition is primarily associated with notable contributions, such as the Giacomini band within the hippocampal formation and the Giacomini vein, he has historically been acknowledged for his observation of the os odontoideum in human anatomy [49]. The term “Os odontoideum” denotes a pathological condition characterized by the presence of an isolated osseous fragment located at the base of the dens, the superiorly projecting element originating from the axis vertebra [2]. This anatomical feature represents a structural variation in the odontoid process situated along the axis. Initially, it was proposed to be a congenital anomaly arising from a failure in the fusion process between the dens, a prominent structure within C2, and the body of the same vertebra. However, it has been suggested that this variation might indicate an undetected or forgotten fracture occurring through the growth plate of the dens during early childhood, typically before the age of 5–6. This condition may be associated with concurrent instability and persistent chronic symptoms. The degree of mobility is restricted below the transverse band of the cruciform ligament, leading to abnormal mobility of the dens in relation to C2 [2, 50]. Os odontoideum is rare, occurring in only 0.5-0.9% of cases. Os odontoideum is associated with neck pain in 50% of cases, radiculopathy in 30%, and myelopathy in 20%.The differential diagnosis of these ossicles can be challenging. Furthermore, os odontoideum has been linked to genetic syndromes, with an association rate of 10% for Morquio syndrome and 20% for Down syndrome. Figure 4 shows the prevalence, location preference, and symptomatology of ossicles. It can be further classified into two main subtypes as follows [2]. The orthotopic subtype is characterized by the os odontoideum, which retains its normal position with a significant separation between C2 and the os odontoideum. The dystopic type is displaced from its typical location. Some studies refer to this form as os avis [2, 14, 25, 26, 49–51].
Fig. 4.
The figure displays the prevalence, location preferences, and symptomatology of the accessory ossicles of the back according the our analyses. Oppenheimer’s ossicles (OpOs) are referred to as OpOs in the figure to avoid confusion with Os odontoideum (OO) (a) The prevalence of ossicles highlights the occurrence rates of different ossicles, showing that ONLs are the most prevalent, while os odontoideum is the rarest (0.5-0.9%) (b) figure indicates the preferred anatomical locations of the ossicles. Limbus vertebrae are most commonly found in the lumbar spine, while nuchal ONLs are exclusively found in the cervical spine (c) figure demonstrates the variability in symptoms for these specific ossicles, with limbus vertebrae predominantly being asymptomatic, while os odontoideum is associated with neck pain, radiculopathy, and myelopathy. LV: Limbus Vertebra, OALL: Ossification of the Anterior Longitudinal Ligament, ONL: Ossification of Nuchal Ligament, OpO: The Oppenheimer’s ossicle, OO: Os Odontoideum, POT: Persistent Ossiculum Terminale
It is essential to differentiate this variant from persistent ossiculum terminale and type 2 odontoid fracture [2]. Os odontoideum is usually encountered incidentally during clinical evaluations. Simultaneously, it is associated with several syndromic conditions such as Morquio syndrome and multiple epiphyseal dysplasia. Moreover, it could manifest concurrently with atlantoaxial instability and another anatomical variant known as the third condyle [2, 25].This condition is defined by the presence of a smooth, well-corticated ossicle located at the superior aspect of a hypoplastic dens, measuring approximately half the size of typical dens. This anatomical configuration is accompanied by a hypertrophied and rounded anterior arch of the atlas [2, 14, 26]. Table 6 provides details of the characteristics, clinical implications, and recommended management of each type of accessory ossicle. The integration of local and systemic ozone therapy for lower back pain, particularly in patients with high BMI, could offer significant relief by addressing both inflammatory and mechanical factors, including anatomical variations, such as accessory ossicles in the spine. These ossicles, while often asymptomatic, may contribute to spinal dysfunction and exacerbate pain, highlighting the importance of considering both anatomical and systemic health factors in pain management strategies [52–55].
Table 6.
Management of accessory ossicles
| Accessory ossicle | Characteristics | Clinical implications | Differential diagnosis | Recommended management |
|---|---|---|---|---|
| Limbus Vertebra (LV) | Well-corticated structures, triangular configurations at the anterosuperior corner | Typically asymptomatic, can cause nerve compression if posterior | Limbus fracture, Schmorl nodes | Conservative management; surgery in rare cases of nerve compression |
| Ossification of Nuchal Ligament (ONL) | Ovoid or round, found at C5-C6 or C6-C7 | Typically asymptomatic, associated with neck dysfunction | Myositis ossificans, clay-shoveler fracture | Usually requires no treatment, monitor if symptomatic |
| Oppenheimer’s Ossicles | Solitary, unilateral ossification of the inferior articular processes | Asymptomatic, incidentally identified | Articular process fractures | Conservative management; surgical intervention if symptomatic |
| Accessory Ossicle of the Anterior Arch of the Atlas | Circular, well-defined, articulates with the anterior arch of the atlas | Generally asymptomatic, but can be mistaken for fractures | Calcific tendinitis, heterotopic ossification | No treatment required, monitor if symptomatic |
| Persistent Ossiculum Terminale | Diminutive size, well-defined cortication, midline location | Rarely symptomatic, linked with atlantoaxial instability in Down syndrome | Os odontoideum, type 1 odontoid fractures | Conservative management; surgical intervention in cases of instability |
| Os Odontoideum | Isolated osseous fragment at the base of the dens, orthotopic/dystopic subtypes | Potentially symptomatic, associated with atlantoaxial instability | Persistent ossiculum terminale, type 2 odontoid fractures | Surgical stabilization often recommended due to risk of instability |
Ossification of ligaments
Ossification of Nuchal Ligament (ONL) within the nuchal ligament, which typically remains asymptomatic, is a frequently encountered anatomical variant. The majority of these ossicles exhibit ovoid or round morphology (Fig. 5) [11]. They predominantly manifest at vertebral levels C5-C6 or C6-C7 [11]. Epidemiological considerations indicate their presence in approximately 5.6-7.5% of the population, with a notable male predominance at a ratio of 3:1. The incidence was 11.3% in males and 3.5% in females. The development of these ossicles reaches maturity after the third decade of life [11]. The formation of these ossicles may be attributed to several factors, including a relatively homogeneous patient population, chronic cervical spine overload with age, and the potential influence of cervical motion, particularly hyperflexion of the neck. This motion applies pressure to the nuchal ligament against spinous processes, thereby fostering the development of ossicles in regions of higher mobility [4, 9]. These ossicles are characterized by well-defined, corticated, round, or oval opacities observed on lateral plain radiographs. On CT scans, they manifest as cortical bone with central marrow within the nuchal ligament. It is imperative to distinguish these ossicles from conditions such as myositis ossificans, clay-shoveler fracture, calcareous bursitis, nuchal fibrocartilaginous pseudotumor, heterotrophy in the secondary nucleus of C6, and calcium hydroxyapatite deposition disease [4, 9]. The investigation and understanding of the presence and significance of these additional ossicles are crucial because of their potential association with specific spinal conditions or their ability to induce symptomatic manifestations, necessitating medical evaluation.
Fig. 5.

A sagittal view of a cervical CT scan at the C5-6 level revealed ONL. CT, Computed Tomography, ONL: Ossification of Nuchal Ligament
Paraskevas et al. [9] and Kadri et al. [20] suggested that ONL is often identified incidentally on imaging and may present without symptoms. However, when symptoms such as neck pain, stiffness, or radiculopathy occur, they are often attributed to concurrent pathologies, such as degenerative disc disease, cervical spondylosis, or other mechanical factors contributing to cervical dysfunction. Additionally, as noted by Pappa et al. [8], the clinical significance of ONL remains controversial, with some patients experiencing discomfort while others remain asymptomatic. The reduction in cervical range of motion and alignment issues could stem from age-related degenerative changes that might coincide with the presence of ossicles, rather than being directly caused by them. Thus, while ossicles within the nuchal ligament might contribute to symptoms in certain individuals, especially if they are large or impinge on surrounding structures, they are generally not considered the sole cause of these clinical manifestations in most cases. Instead, they should be evaluated in a broader context of cervical spine health and degeneration.
ONL has been linked to clinical cervical disorders such as neck dysfunction, cervical malalignment, and morphological alterations of the cervical neural foramina (CNF). Investigations have been conducted on the clinical implications of ONL on various parameters, including active range of motion (AROM) of the neck, cervical radiculopathy, aberrant cervical curvature, and extent of CNF stenosis in individuals presenting with neck stiffness [4, 9]. The neck AROM of all participants was significantly reduced compared to the normal average in all directions, and a moderate negative correlation was observed between the cross-sectional areas of the ONL and AROM in flexion-extension. Despite the absence of a significant correlation between ONL and cervical curvature, most patients exhibited moderate loss of cervical lordotic curvature. Furthermore, there was a significant negative correlation between the CNF stenosis ratio and ONL. Patients with larger ONL demonstrated more severe cervical radiculopathy, greater stiffness in the flexion-extension direction, more intricate degenerative changes in the spine, and more pronounced CNF stenosis. ONL is frequent among patients with cervical spondylosis and can be influenced by factors such as sex, age, and ossification of other ligaments in the cervical spine. Levels predominantly affected by ONL were C4-5 and C5-6. The appearance of the ONL on plain radiography can be categorized into several types: local, continuous, segmental, mixed, and unclassified. The local type is the most prevalent, while multilevel ONL is predominantly observed in patients with ossification of the posterior longitudinal ligament (OPLL) [56].
Ossification of the Anterior Longitudinal Ligament (OALL), also known as Forestier’s disease or diffuse idiopathic skeletal hyperostosis, is characterized by the formation of anterior bridging osteophytes with an unclear etiology. OALL can result in clinical manifestations such as dysphagia, dyspnea, dysphonia, and acute airway obstruction [57]. It was not correlated with age and showed a higher prevalence among males. Patients diagnosed with OALL typically exhibit elevated body height and weight-height index, while instances of OALL are also characterized by greater thoracic kyphosis compared to cases involving disc narrowing. Furthermore, OALL is frequently associated with the ossification of other ligaments within the spine [58]. Shingyouchi et al. [59] reported that OALL, ONL, and OPLL share etiological similarities regarding age, sex, and obesity. However, ONL presents additional risk factors because of its close association with dynamic stress [59]. Calcifications in ALL tend to be uniform and generally linear in appearance.
Ossification of the Posterior Longitudinal Ligament (OPLL) is distinguished by proliferation of the PLL, accompanied by the formation of ossification centers. It is prevalent in Asia, with reported cervical OPLL prevalence ranging from 0.6 to 2.2% in the Korean populations [12]. The etiology of OPLL remains elusive, with indications suggesting that it may be influenced by genetic and hormonal factors [56]. Jun et al. reported a significant association between single-nucleotide polymorphisms in the fibroblast growth factor 1 receptor and OPLL [56]. OPLL in patients with ankylosing spondylitis has been found to be associated with advancing age [60]. The prevalence of OPLL in patients with ONL was significantly higher than that in those without ONL. Given that ONL is relatively innocuous and may be more readily observed than OPLL on routine cervical radiographs, clinicians should consider the potential presence of concurrent OPLL when encountering ONL, particularly in patients presenting with symptoms such as neck pain, radiculopathy, or myelopathy [61]. Preoperative CT is recommended to accurately identify the OPLL [12]. Clinicians should consider the potential coexistence of OPLL when encountering ONL in patients experiencing symptoms, such as neck pain, radiculopathy, or myelopathy. This consideration is crucial for facilitating appropriate treatment. Additionally, given that the bone mineral densities of patients with ONL were observed to increase, patients with ONL may have a lower risk of osteoporosis [61]. This study elucidates the varied presentation and implications of these ossicles, emphasizing their relevance in differential diagnosis and clinical decision-making. This study not only enhances our knowledge of accessory ossicles, but also advocates for improved diagnostic criteria and clinical awareness, which are essential for addressing the challenges posed by these anatomical variations. By synthesizing the existing literature and highlighting gaps in current understanding, this review contributes to a more refined and practical approach to managing spinal accessory ossicles, ultimately improving patient outcomes and advancing clinical practice.
Limitations
A key limitation of this study is the challenge of accurately identifying incidental findings such as accessory ossicles. These variations are often asymptomatic and may be discovered incidentally during imaging in unrelated conditions. Inaccurate or delayed identification of these ossicles can lead to misdiagnosis or unnecessary intervention. Therefore, it is crucial to emphasize the importance of precise diagnostic criteria and awareness of these anatomical variations in clinical practice to avoid such errors and ensure proper management. In addition, the lack of long-term follow-up studies limits our understanding of the long-term clinical implications of accessory ossicles. The studies included in this review may not be representative of all geographic regions and demographic groups. Therefore, the prevalence and clinical significance of accessory ossicles may vary across different populations, which may not be fully captured in this review.
Future directions
Future research should explore the genetic and environmental factors that contribute to accessory ossicle formation. Investigating potential genetic predispositions and environmental triggers such as occupational or lifestyle factors could provide insights into preventive measures and targeted interventions. Comparative studies between different populations, including those from diverse geographic regions and age groups, will help understand the variability in the prevalence and clinical implications of accessory ossicles. Predictive models and artificial intelligence could play a significant role in early detection and personalized treatment strategies.
Conclusion
In conclusion, accessory ossicles in the spine represent a range of anatomical variations, with varying clinical implications. These ossicles are frequently asymptomatic and incidentally discovered; however, some, such as the limbus vertebrae and ossicles within the nuchal ligament, can be associated with specific syndromes or symptoms, including nerve compression and neck dysfunction. Accurate diagnosis and differentiation from fractures and other pathologies are essential to avoid misdiagnosis and to ensure appropriate management.
Abbreviations
- ALL
Anterior Longitudinal Ligament
- AROM
Active range of motion
- CNF
Cervical neural foramina
- CT
Computed Tomography
- LV
Limbus Vertebra
- MRI
Magnetic resonance imaging
- OALL
Ossification of the Anterior Longitudinal Ligament
- ONL
Ossification of Nuchal Ligament
- OPLL
Ossification of the Posterior Longitudinal Ligament
- OpO
The Oppenheimer ossicle
- OO
Os Odontoideum
- PLL
Posterior Longitudinal Ligament
- POT
Persistent Ossiculum Terminale
Author contributions
E.O.: Research idea, study design, data acquisition, data analysis, data interpretation, manuscript drafting and writing, critical revision for important intellectual content, and final approval of the version to be published.
Funding
No funding or grants were obtained.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Ethical approval
We confirm that we have read the journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines. All procedures conformed to the 1964 Declaration of Helsinki and its later amendments, or comparable ethical standards.
Informed consent
Not applicable.
Statement regarding research involving human participants and/or animals
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Ogut E, Karakas O, Aydin DD. Oppenheimer’s accessory ossicle and clinical significance: a narrative review. J Orthop Rep. 2022;1(4):100069. [Google Scholar]
- 2.Öğüt E, Şekerci R, Şen H, Çakın H, Gediz T, Keles-Celik N. Anatomo-radiological importance and the incidence of os odontoideum in Turkish subjects: a retrospective study. Surg Radiol Anat. 2020;42(6):701–10. [DOI] [PubMed] [Google Scholar]
- 3.Ghelman B, Freiberger RH. The limbus vertebra: an anterior disc herniation demonstrated by discography. AJR Am J Roentgenol. 1976;127(5):854–5. [DOI] [PubMed] [Google Scholar]
- 4.Gokce E, Beyhan M. Evaluating ossifications of the Nuchal Ligament with cervical computed tomography. Eurasian J Med. 2018;50(1):23–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graikos G, Gkoudina A, Tsakonas N, Christakis N. Limbus vertebrae as Incidental Finding in a patient with Acute Lower Back Pain. Cureus. 2020;12(9):e10658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Johal J, Loukas M, Fisahn C, Oskouian R, Tubbs R. Bergmann’s ossicle (ossiculum terminale persistens): a brief review and differentiation from other findings of the odontoid process. Child’s Nerv Syst 2016, 32. [DOI] [PubMed]
- 7.Man RS. Limbus Vertebra and Low Back Pain: a Case Report and Review of Literature. Int J Sports Exerc Med 2019, 5(10).
- 8.Pappa E, Chatzikomninos I. Limbus vertebrae of the cervical spine: a case report. Clin case Rep. 2022;10(11):e6567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Paraskevas GK, Raikos A, Martoglou S, Ioannidis O. Sesamoid ossicles within the nuchal ligament: a report of two cases and review of the literature. J Radiol case Rep. 2011;5(8):22–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pushpa BT, Aiyer SN, Kannan M, Maheswaran A, Rajasekaran S. Oppenheimer’s ossicles in the lumbar spine-a rare cause of lumbar canal stenosis. J Orthop. 2018;15(2):343–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scapinelli R. Sesamoid bones in the ligamentum nuchae of man. J Anat. 1963;97(Pt 3):417–22. [PMC free article] [PubMed] [Google Scholar]
- 12.Kang MS, Lee JW, Zhang HY, Cho YE, Park YM. Diagnosis of cervical OPLL in lateral radiograph and MRI: is it Reliable? Korean J Spine. 2012;9(3):205–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mori K, Yoshii T, Hirai T, Iwanami A. Prevalence and distribution of ossification of the supra/interspinous ligaments in symptomatic patients with cervical ossification of the posterior longitudinal ligament of the spine: a CT-based multicenter cross-sectional study. BMC Musculoskelet Disord. 2016;17(1):492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Robson KA. Os odontoideum: rare cervical lesion. Western J Emerg Med. 2011;12(4):520–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sankar WN, Wills BP, Dormans JP, Drummond DS. Os odontoideum revisited: the case for a multifactorial etiology. Spine. 2006;31(9):979–84. [DOI] [PubMed] [Google Scholar]
- 16.Park Y, Kim H, Jeon S, Lee Y. The Inferior Accessory Ossicle of the Anterior Arch of the Atlas misdiagnosed as Anterior Arch Fracture - A Case Report. J Korean Soc Spine Surg. 2012;19:16. [Google Scholar]
- 17.Percival CJ, Richtsmeier JT. Angiogenesis and intramembranous osteogenesis. Dev Dynamics: Official Publication Am Association Anatomists. 2013;242(8):909–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. Spine Journal: Official J North Am Spine Soc. 2005;5(5):564–76. [DOI] [PubMed] [Google Scholar]
- 19.Carr RB, Fink KR, Gross JA. Imaging of trauma: part 1, Pseudotrauma of the spine–osseous variants that may simulate injury. AJR Am J Roentgenol. 2012;199(6):1200–6. [DOI] [PubMed] [Google Scholar]
- 20.Kadri PA, Al-Mefty O. Anatomy of the nuchal ligament and its surgical applications. Neurosurgery. 2007;61(5 Suppl 2):301–4. discussion 304. [DOI] [PubMed] [Google Scholar]
- 21.Gambardella A, Meoli S. [Inferior accessory ossicle of the anterior arch of the atlas]. Radiol Med. 1983;69(9):673–4. [PubMed] [Google Scholar]
- 22.Naji MF, Bhat R. The typical appearance of the inferior accessory ossicle of the anterior arch of the atlas. Surg Radiol Anat. 2009;31(1):69–71. [DOI] [PubMed] [Google Scholar]
- 23.Ankith NV, Avinash M, Srivijayanand KS, Shetty AP, Kanna RM, Rajasekaran S. Congenital osseous anomalies of the cervical spine: occurrence, morphological characteristics, embryological basis and clinical significance: a computed tomography based study. Asian Spine J. 2019;13(4):535–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Karwacki GM, Schneider JF. Normal ossification patterns of atlas and axis: a CT study. AJNR Am J Neuroradiol. 2012;33(10):1882–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Offiah CE, Day E. The craniocervical junction: embryology, anatomy, biomechanics and imaging in blunt trauma. Insights into Imaging. 2017;8(1):29–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smoker WR. Craniovertebral junction: normal anatomy, craniometry, and congenital anomalies. Radiographics: Rev Publication Radiological Soc North Am Inc. 1994;14(2):255–77. [DOI] [PubMed] [Google Scholar]
- 27.Baena-Caldas GP, Mier-García JF, Griswold DP, Herrera-Rubio AM, Peckham X. Anatomical variations of the atlas arches: prevalence assessment, systematic review and proposition for an updated classification system. Front NeuroSci. 2024;18:1348066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Alagheband SJ, Clapp AD, Narducci DM, Cudahy R, Pujalte G. Limbus Vertebra Cureus. 2021;13(3):e13954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mupparapu M, Vuppalapati A, Mozaffari E. Radiographic diagnosis of Limbus vertebra on a lateral cephalometric film: report of a case. Dento Maxillo Fac Radiol. 2002;31:328–30. [DOI] [PubMed] [Google Scholar]
- 30.Park Y, Kim HB, Jeon SW, Lee YT, Yoo JH, Oh HC, Ha J-W, Sung SY, Yoon HK. The Inferior Accessory Ossicle of the Anterior Arch of the Atlas misdiagnosed as Anterior Arch Fracture - A Case Report. J Korean Soc Spine Surg. 2012;19(1):16–9. [Google Scholar]
- 31.Erdogan H, Cengiz A, Cengiz A, Eser G. Inferior accessory ossicle of the anterior arch of the atlas in a trauma patient. Spine Journal: Official J North Am Spine Soc. 2016;16(10):e715. [DOI] [PubMed] [Google Scholar]
- 32.Liang C-L, Lui C-C, Lu K, Lee T-C, Chen H. Atlantoaxial stability in ossiculum terminale: Case report. J Neurosurg. 2001;95:119–21. [DOI] [PubMed] [Google Scholar]
- 33.Cho S, Shlobin NA, Dahdaleh NS. Os odontoideum: a comprehensive review. J Craniovertebral Junction Spine. 2022;13(3):256–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klassov Y, Benkovich V, Kramer MM. Post-traumatic os odontoideum - case presentation and literature review. Trauma case Rep. 2018;18:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Bmj : 2021. [DOI] [PMC free article] [PubMed]
- 36.Cosmin N, Refi D, Obada B, Dragosloveanu S, Scheau C, Baz R. Beyond the Bony Fragment: a review of Limbus Vertebra. Cureus. 2024;16:e60065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schmorl G. Die pathologische Anatomie Der Wirbelsaule. Verhandlungen Der Deutchen Orthopadeschen Gesellschaft. 1926;21(1):3–41. [Google Scholar]
- 38.Faccia KJ, Williams RC. Schmorl’s nodes: clinical significance and implications for the bioarchaeological record. Int J Osteoarchaeology. 2008;18(1):28–44. [Google Scholar]
- 39.Nișcoveanu C, Refi D, Obada B, Dragosloveanu S, Scheau C, Baz RO. Beyond the Bony Fragment: a review of Limbus Vertebra. Cureus. 2024;16(5):e60065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ogut E, Sogut B, Korkut KS, Balci A, Sengiz CN, Lek IK, Bucak AZ. The unilateral muscular slip of the two-bellied Serratus posterior inferior muscle: a case report and a review of literature. Surg Radiol Anat. 2023;45(8):1031–6. [DOI] [PubMed] [Google Scholar]
- 41.Oppenheimer A. Supernumerary ossicle at the isthmus of the neural Arch. Radiology. 1942;39(1):98–100. [Google Scholar]
- 42.O’Brien WT, Shen S, Lee P. The dens: Normal Development, Developmental variants and anomalies, and traumatic injuries. J Clin Imaging Sci. 2015;5:38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cattell HS, Filtzer DL. Pseudosubluxation and other normal variations in the cervical spine in children. A study of one hundred and sixty children. J bone Joint Surg Am Volume. 1965;47(7):1295–309. [PubMed] [Google Scholar]
- 44.Semine AA, Ertel AN, Goldberg MJ, Bull MJ. Cervical-spine instability in children with Down syndrome (trisomy 21). J bone Joint Surg Am Volume. 1978;60(5):649–52. [PubMed] [Google Scholar]
- 45.Liang CL, Lui CC, Lu K, Lee TC, Chen HJ. Atlantoaxial stability in ossiculum terminale. Case report. J Neurosurg. 2001;95(1 Suppl):119–21. [DOI] [PubMed] [Google Scholar]
- 46.Sherk HH, Nicholson JT. Rotatory atlanto-axial dislocation associated with ossiculum terminale and mongolism. A case report. J bone Joint Surg Am Volume. 1969;51(5):957–64. [PubMed] [Google Scholar]
- 47.Burke SW, French HG, Roberts JM, Johnston CE 2nd, Whitecloud TS 3rd, Edmunds JO Jr. Chronic atlanto-axial instability in Down syndrome. J bone Joint Surg Am Volume. 1985;67(9):1356–60. [PubMed] [Google Scholar]
- 48.Kobori M, Takahashi H, Mikawa Y. Atlanto-axial dislocation in Down’s syndrome. Report of two cases requiring surgical correction. Spine. 1986;11(3):195–200. [PubMed] [Google Scholar]
- 49.Perrini P, Montemurro N, Iannelli A. The contribution of Carlo Giacomini (1840–1898): the limbus Giacomini and beyond. Neurosurgery. 2013;72(3):475–81. discussion 481 – 472. [DOI] [PubMed] [Google Scholar]
- 50.Arvin B, Fournier-Gosselin M-P, Fehlings M. Os Odontoideum: etiology and Surgical Management. Neurosurgery. 2010;66:22–31. [DOI] [PubMed] [Google Scholar]
- 51.Jumah F, Alkhdour S, Mansour S, He P, Hroub A, Adeeb N, Hanif R, Mortazavi MM, Tubbs RS, Nanda A. Os Odontoideum: a Comprehensive Clinical and Surgical Review. Cureus. 2017;9(8):e1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Borrelli E. Combined local and systemic ozone therapy in the treatment of the low back Pain: a proposed protocol and a suggested mechanism of action. In., edn.; 2021: 1–6.
- 53.Ogut E, Yildirim FB, Sarikcioglu L, Aydin MA, DemİR N. Neuroprotective effects of ozone therapy after sciatic nerve cut Injury. Kurume Med J. 2018;65(4):137–44. [DOI] [PubMed] [Google Scholar]
- 54.Ogut E. K Armagan 2022 Evaluation of the potential impact of medical ozone therapy on Covid-19: a review study. Ozone: Sci Eng 45 3 213–31. [Google Scholar]
- 55.Mutlu AU, Aydın B, Ecertaştan Ö, Eren Ö, Bilge Güvenç T, Hakan T. Evaluation of physical Exercise’s effects on Low Back Pain among University students with short Form-36 and Oswestry Disability Index. Turkish Med Student J. 2020;7(2):77–83. [Google Scholar]
- 56.Jun JK, Kim SM. Association study of fibroblast growth factor 2 and fibroblast growth factor receptors gene polymorphism in Korean ossification of the posterior longitudinal ligament patients. J Korean Neurosurg Soc. 2012;52(1):7–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Iida M, Tanabe K, Dohi S, Iida H. Airway management for patients with ossification of the anterior longitudinal ligament of the cervical spine. JA Clin Rep. 2015;1(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Yanagihara M. An epidemiological study on the ossification of the anterior longitudinal ligament of the spine. Nihon Seikeigeka Gakkai Zasshi. 1986;60(2):187–202. [PubMed] [Google Scholar]
- 59.Shingyouchi Y, Nagahama A, Niida M. Ligamentous ossification of the cervical spine in the late middle-aged Japanese men. Its relation to body mass index and glucose metabolism. Spine. 1996;21(21):2474–8. [DOI] [PubMed] [Google Scholar]
- 60.Kim TJ, Kim TH, Jun JB, Joo KB, Uhm WS. Prevalence of ossification of posterior longitudinal ligament in patients with ankylosing spondylitis. J Rhuematol. 2007;34(12):2460–2. [PubMed] [Google Scholar]
- 61.Kim K-W, Oh Y-M, Eun J-P. Increased prevalence of ossification of posterior longitudinal ligament and increased bone Mineral density in patients with ossification of Nuchal Ligament. Korean J Spine 2016, 13(3). [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No datasets were generated or analysed during the current study.