Abstract
Background
During the vulnerable transition to parenthood, (expectant) parents may be particularly susceptible to the negative effects of adverse working conditions. However, research on the influence of work-related factors on peripartum mental health issues is scarce. This study aims to enhance our understanding of work-related risk factors for the adjustment of parents in the transition to parenthood by investigating the role of prepartum precarious employment, abusive supervision, job insecurity, and job demand on postpartum mental health symptoms in first-time mothers and their partners.
Methods
In the prospective-longitudinal cohort study “DREAM”, N = 1,259 mothers and N = 811 male and female partners were asked about their working conditions during pregnancy and their mental health 14 months postpartum. We conducted several hierarchical multiple regression analyses with prepartum precarious employment, abusive supervision, job insecurity, and job demand (the latter three in joint regression analyses) as predictors of postpartum symptoms of depression, somatization, obsessive-compulsiveness, anxiety, and anger/hostility. In Model 1 we controlled for sociodemographic variables, and in Model 2 we also controlled for pre-existing symptoms of the respective mental health variable during pregnancy. Separate analyses were calculated for mothers and partners, and each mental health outcome.
Results
Multiple regression analyses revealed that prepartum precarious employment and abusive supervision predicted mothers’ and partners’ mental health symptoms 14 months postpartum even after controlling for pre-existing symptoms. Prepartum job insecurity and job demand also predicted mental health symptoms 14 months postpartum but were no longer significant predictors in most models after controlling for pre-existing mental health symptoms. There were only minor differences regarding the considered mental health outcomes and between mothers’ and partners’ results.
Conclusions
Our study demonstrates that adverse working conditions are important risk factors for the adjustment of parents in the transition to parenthood, requiring more attention from research and practice. Precarious employment and abusive supervision appear to be particularly important factors affecting new parents’ mental health. Future research should investigate the mechanisms behind these variables, including comparisons between mothers and their partners, and the role of stress-related biomarkers. Additionally, developing screening methods for clinical use to facilitate targeted preventive interventions is essential.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-21886-2.
Keywords: DREAM study, Peripartum/perinatal mental health, Fathers’ mental health, Postpartum depression, Working conditions, Precarious employment, Abusive supervision, Job insecurity, Job demand, Work stress
Background
Labor work constitutes a major aspect of adult life, exerting a profound and intricate impact on well-being [1, 2]. While employment has been found to be overall beneficial for workers’ mental health [3], poor working conditions, including low levels of control, high job demand, job insecurity, and unfair pay, can have significant adverse effects on mental health [4–7] – potentially even more detrimental than unemployment [4, 8]. Poor mental health in the workplace is not only a major burden for affected individuals and their families, but also for society as a whole, as mental health problems are a leading cause of loss of productivity and reduced work ability [9–12] as well as high global economic costs [13]. Consequently, identifying and mitigating working conditions that impede employees’ mental health represents a public mental health concern and is increasingly a focus of research [5, 6].
A significant proportion of the global workforce consists of parents: In 2023, 34% of prime-aged adults (aged 25 to 54) had at least one child under the age of six [14], and the vast majority of adults (around 80–90% across OECD countries) will eventually transition to parenthood [15]. Furthermore, dual-income families are becoming more common around the world [16], which is increasing the number of working parents. However, as the transition to parenthood is considered a vulnerable period with many challenges [17], expectant parents may be particularly susceptible to developing mental health issues in adverse working environments. Although there is a growing body of research on mental health in the workplace on the one hand and mental health during the transition to parenthood on the other, the two research areas have rarely been combined [18–20]. In order to inform work policies that maintain the mental health and working ability of (expectant) parents [21], it is of central importance to clarify the role of working conditions on the mental health of parents in the transition to parenthood.
Mental health in the transition to parenthood
Despite the joy of welcoming a new baby, the transition to parenthood is a phase with numerous physiological, psychological, economic, and social challenges for new parents [17, 22]. Alongside the (physical) strains of pregnancy and childbirth mostly mothers carry [22–24], both mothers and their partners must fundamentally restructure their lives to adapt to their new roles as parents and adjust to the infants’ needs [25–27]. Sleep disturbances, relationship strain, and heightened emotional concerns compound the experience [25–28]. Whereas many mothers and partners experience personal growth in their new role as parents (e.g., [29]), the added stressors and challenges can surpass available resources and coping mechanisms, hindering successful adjustment [17]. Consequently, the time after childbirth is often accompanied by the onset of mental health problems [17]. Of these, postpartum depression (global estimate of prevalence among mothers: 17.2–27.6%, [30, 31], and among fathers: 5.6–8.8%, [32, 33]) and postpartum anxiety (global estimate of prevalence among mothers: 9.3%–18.0%, [33–36], and among fathers: 9.5% [33],) as the most common mental disorders are of special interest. However, also symptoms of somatization (i.e., physical symptoms like pain or fatigue), obsessive-compulsiveness (i.e., recurring intrusive thoughts such as contamination obsessions and/or repetitive behaviors such as washing), and anger/hostility (i.e., feelings of irritation, rage, and resentment up to aggressiveness) have been reported in the peripartum period [37–41]. These symptoms warrant attention as they occur more frequently during the peripartum period than in the general population and can cause serious suffering for those affected [37, 39]. To illustrate, postpartum intrusive thoughts or repetitive behaviors as well as feelings of irritation often focus on infant-related concerns (e.g., accidental harm to the infant), and can consequently be particularly shameful or distressing for affected parents [37]. Furthermore, when irritation escalates to aggressiveness, this may have serious consequences for involved family members [38]. In addition, structurally assessing somatization symptoms may be particularly crucial in the peripartum period, as they are important indicators of mental distress and might be overlooked or misattributed to normal pregnancy and postpartum physical changes [39, 40]. Including a broader spectrum of symptoms helps to identify individuals whose psychological distress may manifest differently from more common depression and anxiety measures. Importantly, parental mental health symptoms in the peripartum period can have long-term detrimental effects not only on the well-being of the affected individuals but also on the parent-infant relationship and the child’s behavioral and developmental outcomes [38, 42–45]. Consequently, a growing body of research has focused on identifying potential risk factors for poor mental health in the transition to parenthood.
Adverse working conditions as risk factor for postpartum mental health symptoms
Previous investigations have focused on a variety of individual-level factors such as age, chronic/daily stress exposure, (past) stressful or traumatic life events (e.g., abuse, intimate partner violence), prior mental health disorders, obstetric experiences, difficult infant temperament, partnership conflict, and lack of social support as risk factors for postpartum mental health problems [46–50]. Ko et al. [51], for instance, linked stressful life events occurring within the year before birth to postpartum depression. However, studies on the role of work factors as potential specific chronic/life stressors are still lacking [18, 31]. As an example, a study examining the effects of chronic strains on postpartum-onset depression included measures of neighborhood safety, parenting strain, and relationship strain, but neglected strains related to employment, even though listing employment as a potential source of chronic strain in the introduction [50]. This is surprising, given that we already know from previous research (mainly outside the peripartum period) that the work environment is important for adult mental health [6, 52–57] and that (expectant) parents constitute a particularly vulnerable group [17, 45, 58, 59]. Importantly, the influence of working conditions does not diminish in the transition to parenthood: Across OECD countries, (expectant) mothers are entitled to around 18 weeks of maternity leave shortly before and after birth, remaining largely employed during pregnancy [60–62]; new fathers usually only take few months of parental leave after birth [63], and both have to plan and ensure the future compatibility of work and family life. In addition, the new financial responsibility reinforces the importance of a secure income.
According to the stress-associated Conservation of Resources Theory (COR; [64–66]), adverse working conditions can represent a threat to resources (e.g., personal resources such as skills, material resources such as tools for work, condition resources such as seniority, and energy resources such as positive emotions; [67, 68]) and, via increased attention to and appraisal of this threat, consume energy and lead to resource loss (e.g., negative emotions; [66]). This, in turn, reduces available resources to cope with upcoming strains – which are manifold within the transition to parenthood. In a cyclic process, this might lead to poor mental health in the long term. Specifically, in the context of transitioning to parenthood, COR implies that adverse prepartum working conditions reduce the parents’ resources and abilities to cope with the additional strains coming with this period of great changes and thereby might hinder a successful adjustment. Furthermore, this consideration suggests that adverse working conditions might contribute to a general vulnerability and thereby have an impact on overall mental health, including various mental health symptoms.
The limited evidence available suggests that working conditions during the transition to parenthood indeed have an important influence on postpartum mental health (e.g., [69]). For instance, precarious employment (including, e.g., temporary employment, low wages, and authoritarian treatment) during pregnancy predicted symptoms of depression in mothers eight weeks after childbirth [70]. In addition, higher psychosocial work stress (i.e., an imbalance of high effort and low reward at work) during the COVID-19 pandemic was associated with parental symptoms of depression and anger/hostility [38]. Furthermore, perceived pregnancy discrimination in the workplace was found to be indirectly related to maternal postpartum symptoms of depression via perceived stress during pregnancy [71]. In (expectant) fathers, poor job quality was identified as a significant risk factor for symptoms of psychological distress in the first year postpartum [72], and high job burden as well as low job satisfaction predicted birth-related posttraumatic stress disorder symptoms eight weeks postpartum [57].
Interestingly, certain aspects of the work environment appear to be particularly relevant to employees’ mental health, including abusive supervision (i.e., aggressive and hostile behavior by supervisors; [73, 74]), job insecurity (i.e., fear of losing one’s job or important features of it; [75–77]), and high job demand (i.e., high workload and time pressure experienced at work; [78–80]). First evidence from the peripartum period on these aspects suggests that experiencing abusive supervision, as well as vicarious abusive supervision (i.e., witnessing colleagues being abused) in the peripartum period can contribute to job-related emotional exhaustion and postpartum depressive symptoms in mothers [66]. On the contrary, supportive supervisor behaviors, defined as general feelings of emotional and instrumental support, can have a protective effect on parental mental health [81, 82]. Furthermore, cross-sectional studies report perceived job insecurity to be associated with a higher risk of depression and anxiety disorders in mothers [83, 84] and fathers [85] in the first year postpartum. In accordance, a more recent cross-sectional study conducted during the COVID-19 pandemic in the US found that perceived job insecurity was a significant predictor of symptoms of depression during the peripartum period [86]. Moreover, high job demand was linked to mental health problems in mothers and working-class dual-earner couples during the transition to parenthood [81, 87] and in lesbian and gay parents [88]. Supporting this, a Norwegian longitudinal study reported that prepartum work stress including high job demand predicted postpartum depression and anxiety in mothers [89]. In line with this, a recent systematic review on maternal return to work after giving birth identified total workload, which is part of the concept of job demand, as a significant predictor of maternal mental health [69]. Another recent longitudinal study suggests that the adverse working condition time urgency, which is also part of the concept of job demand, may even have both a direct and – via symptoms of postpartum depression and anxiety – indirect detrimental effect on maternal interactions with their child one year after birth [90]. Furthermore, some studies indicate that an increase in total workload (i.e., paid and unpaid work) is related to adverse postpartum mental health outcomes in mothers [91, 92].
Overall, research on the intersection of working conditions and mental health in the peripartum period is limited. The few available studies have mostly focused on mothers [85], whereas postpartum mental health issues are also experienced by fathers and female partners [93–95] – an issue that applies to almost all areas of peripartum mental health research [96, 97]. However, this is a critical gap to address within the work context, as, despite an increase in dual-earner families, it is still mainly mothers who reduce their working hours and take the majority of parental leave [98], while the working conditions of partners – with their potentially detrimental effects on mental health – remain constantly present during the transition to parenthood [14]. Interestingly, a recent study of our group found that only in fathers but not in mothers, lower job satisfaction and higher job burden during pregnancy serve as predictors of birth-related posttraumatic stress disorder symptoms eight weeks postpartum, highlighting the relevance of considering work-related factors in fathers’ postpartum mental health and suggesting that differential investigations of (expectant) mothers and partners could be informative [57]. A further shortcoming in the literature is that evidence mainly stems from cross-sectional studies. While these add valuable knowledge about associations at the time of assessment, it is crucial to consider the long-term effects of working conditions during the transition to parenthood, especially when at least one or both parents take parental leave. Moreover, many studies lack theory-based, validated measures of working conditions, resulting in a wide range of data that are difficult to compare with each other [53, 99, 100]. In addition, while former studies on work and mental health in the peripartum period mostly focused on depression and anxiety as outcomes (e.g., [101–103]), it should be acknowledged that individual reactions to potentially stressful working conditions might manifest themselves in a variety of mental health symptoms such as symptoms of somatization, obsessive-compulsiveness, and anger/hostility. To illustrate, some individuals may primarily exhibit somatic complaints, contamination or infant-related obsessions, or increased irritability rather than depressive or anxiety symptoms. Examining this broader symptom spectrum is crucial to identify and support individuals who might otherwise be overlooked. Finally, many studies on work and parental mental health analyze data gathered more than 20 years ago. In light of the current changes in the labor market, including digitalization and ongoing flexibilization (e.g., teleworking) – which have received another major boost due to the COVID-19 pandemic – and the associated impact on workers’ mental health [45, 104–107], it is imperative to update the results of older studies. In this context, it should also be noted that, due to the increase in dual-earner families [16], (expectant) parents nowadays represent an even more important and vulnerable group within the working population, firstly because of the growing proportion of working parents (especially due to more working mothers), and secondly because the challenge of reconciling work and family life is becoming increasingly prevalent as more and more parents take on a dual role.
Aim of the present study
The aim of this study is to enhance our understanding of work-related risk factors for the adjustment of parents in the transition to parenthood. To address the identified research gaps, we will investigate the predictive value of adverse prepartum working conditions for a variety of mental health outcomes 14 months postpartum in both mothers and their partners. Based on the available literature and theoretical considerations, we hypothesize that higher levels of prepartum precarious employment, abusive supervision, job insecurity, and job demand will predict poorer mental health outcomes (i.e., more symptoms of depression, somatization, obsessive-compulsiveness, anxiety, and anger/hostility) 14 months postpartum in mothers and their male or female partner, controlling for relevant confounders (e.g., employment status, academic degree) and pre-existing symptoms of the respective mental health variable during pregnancy.
Methods
Study design
The study is based on data from the ongoing Dresden Study on Parenting, Work, and Mental Health (DREAM; “DResdner Studie zu Elternschaft, Arbeit und Mentaler Gesundheit”). DREAM is a prospective cohort study that examines the associations between parental work participation, role distribution, perinatal factors, stress factors, and long-term family (mental) health and intra-family relationships with currently seven measurement points from pregnancy (T1) to 7.5 years after childbirth (T7). Between June 2017 and the end of 2020, 3,860 expectant mothers and their male or female partners were recruited mainly at information events of obstetrical clinics in and around Dresden, Germany. Further information on the design, sample, and procedures can be found in the study protocol [108]. For the current analyses, questionnaire data of mothers and male and female partners on prepartum working conditions (T1) and mental health symptoms at 14 months postpartum (T3) were used.
Sample
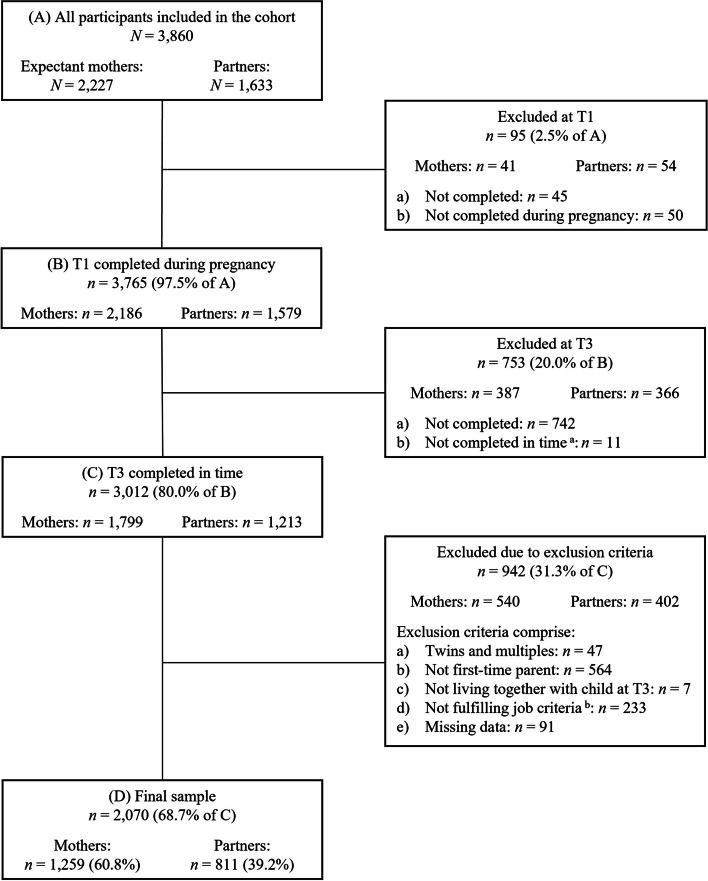
By March 10th, 2023, n = 2,227 expectant mothers and n = 1,633 partners had answered the first questionnaire (T1). Of those, n = 1,799 mothers and n = 1,213 partners completed both the T1 and T3 questionnaire in time (i.e., T1 during pregnancy and T3 within 12–18 months after birth; see flow chart; Fig. 1). For the present study, inclusion criteria comprise 1) giving birth to a single child, 2) being a first-time parent, 3) still living together with the child 14 months after birth, 4) fulfilling relevant job criteria, i.e., being employed at least part-time or marginally at T1 excluding self-employment, 5) being at least 18 years old, and 6) providing data for relevant measures at both timepoints. The final sample consisted of 2,070 participants comprising 1,259 mothers (60.8%) and 811 male and female partners (39.2%).
Fig. 1.
Flowchart of retention rate and exclusion criteria resulting in final sample
Note. T1 = during pregnancy; T3 = around 14 months after the actual birth date. Data for the current study were extracted on March 10, 2023 (version 10 of the quality-assured data files; both T1 and T3 were already completed at the time of data extraction). a Not within 12 and 18 months after the actual birth date. b Job criteria leading to exclusion comprise attending school, working in an apprenticeship or voluntary service, being self-employed, and not being at least in marginal employment at T1 (self-rated)
Measures
Adverse prepartum working conditions as predictors
As predictors, we included the working conditions precarious employment, abusive supervision, job insecurity, and job demand measured during pregnancy (T1). If participants were in pregnancy-related employment ban (see [109]) or had not worked since the pregnancy, participants were asked to answer the questions on working conditions referring to the 6 months prior to pregnancy or employment ban.
Precarious employment was measured with the German version of the Employment Precariousness Scale (EPRES; [110, 111]) that was specifically designed for epidemiological studies among waged workers. In previous investigations, it has shown good acceptability, internal consistency (Cronbach’s α ≥ 0.70), and construct validity [70, 111–113]. The instrument contains six subscales: temporariness (2 items), disempowerment (2 items), vulnerability (5 items), wages (3 items), rights (4 items), and exercise rights (6 items). The subscale disempowerment was excluded in this study due to many different types of employment within the sample. The overall EPRES score, ranging from 0 (not precarious) to 4 (most precarious), is the arithmetic mean of all subscale scores. In our sample, the internal consistency was acceptable (mothers: α = 0.74; partners: α = 0.72).
Abusive supervision was assessed with the EPRES subscale vulnerability [110, 111], which measures defenselessness to authoritarian treatment with five items answered on a 5-point frequency scale from 0 (never) to 4 (always). Example items are “In relation to the way you are treated at work, can you tell me whether…You are defenseless towards unfair treatment by your superiors / … You are made to feel you can be easily replaced” [110]. The items are similar to those used in other studies that identified abusive supervision as relevant for workers’ depression and emotional exhaustion [78]. Total abusive supervision scores are computed as simple averages resulting in a 0–4 range with higher scores indicating more abusive supervision. Internal consistency was acceptable (mothers: α = 0.78; partners: α = 0.73) in the current study.
Job insecurity and job demand were measured via two items of the German version of the Effort-Reward Imbalance Questionnaire (ERI; [114, 115]), respectively. Job insecurity has previously been operationalized this way by Marchand et al. [78]. An example item is “I have experienced or I expect to experience an undesirable change in my work situation”. The two items measuring job demand were selected based on the similarity to items used for this construct in prior studies [81, 116]. An example item is “I have constant time pressure due to a heavy work load”. Responses are based on a 4-point Likert scale from 1 (strongly disagree) to 4 (strongly agree), leading to total sum scores ranging from 2–8 with higher scores indicating more job insecurity/job demand. Internal consistency, measured with the Spearman-Brown coefficient ρ as recommended for two-item scales [117], was acceptable for the two items selected for job insecurity (mothers ρ = 0.61; partners ρ = 0.65) and job demand (mothers ρ = 0.65; partners ρ = 0.61).
Postpartum mental health outcomes
Mental health outcomes were measured at 14 months postpartum (T3) and comprised symptoms of depression, somatization, obsessive-compulsiveness, anxiety, and anger/hostility.
Symptoms of depression were measured by the validated German version of the Edinburgh Postnatal Depression Scale (EPDS; [118]). The EPDS is the gold standard for assessing symptoms of depression throughout the peripartum period in mothers as well as partners [119–121]. The 10 self-report items assess symptom severity in the last seven days. Answers were given on a 4-point scale (0–3), resulting in a sum score ranging from 0–30 with higher scores indicating higher levels of depressive symptoms. Internal consistency was good in the current study (mothers: α = 0.83; partners: α = 0.81).
Symptoms of somatization, obsessive-compulsiveness, anxiety, and anger/hostility were measured with the corresponding subscales of the validated German version of the Symptom-Checklist Revised (SCL-90-R; [122]), including 12, 10, 10, and 6 self-report items, respectively. Answers refer to symptoms experienced within the last seven days and were given on a 5-point Likert scale from 0 (not at all) to 4 (very strong) resulting in scale-length-dependent sum score ranges of 0–48, 0–40, 0–40, and 0–24, respectively, with higher scores indicating more symptom severity. The internal consistency of all subscales was acceptable or good among mothers and partners (0.73 ≤ α ≤ 0.83).
Potential confounding variables
We considered the following variables as potential confounders because associations with the predictor or outcome variables were reported in previous studies: Employment status, academic degree, age, duration of parental leave, and COVID-19 pandemic exposure. Employment status was measured via items on full-time, part-time, and marginal employment, while multiple answers were possible. Employment status was subsequently dichotomized by combining part-time and marginal employment (0 = full-time; 1 = part-time or marginal). If participants chose more than one category, the more time-consuming option was recorded. Academic degree was assessed at T1 with a question based on the German National Cohort Consortium [123] and was subsequently dichotomized as 1 (academic degree) or 0 (no academic degree). Age was measured in years at T1 and duration of parental leave was assessed in months at T3 (i.e., the duration relates to the parental leave taken up to T3). COVID-19 pandemic exposure was considered as a potential confounder to account for possible effects on mental health [124, 125]. Participants were grouped into two categories based on the date of completion at T3 (i.e., when the outcome variable was assessed). Those who completed T3 between March 10th, 2020, and January 15th, 2023 were assigned to the “during pandemic” group, otherwise, they were placed in the “before/after pandemic” group. Finally, we controlled for pre-existing (T1) symptoms of the respective mental health variable, i.e., symptoms of depression at T1 with the EPDS, symptoms of somatization, obsessive-compulsiveness, anxiety, and anger/hostility at T1 with the corresponding subscale of the SCL-90-R.
Statistical analyses
Analyses were performed using SPSS 27 [126]. Participant’s mean values replaced missing items if they filled in at least 80% of the items from psychometric scales. We conducted descriptive analyses for sociodemographic characteristics of the sample and the primary study variables (N, rates in %, M, SD). Furthermore, attrition analyses were conducted for sociodemographic characteristics, predictors, outcomes, and potential confounders, comparing participants who completed T1 and T3 to participants who only completed T1 (see Additional file 1). Potential confounding variables were identified based on theoretical considerations and those significantly correlating with at least one of the mental health outcomes in preliminary correlation analyses (see Additional file 2) were included as confounders in regression analyses (separately for mothers and partners). In the main analyses, Pearson correlations for all study variables were calculated and hierarchical multiple regression analyses were conducted to examine prospective associations between prepartum working conditions and mental health outcomes 14 months postpartum. We calculated separate regression models for each mental health outcome. Regarding working conditions, precarious employment, which reflects a broader, multidimensional construct [53] was investigated separately as predictor to examine its contribution to the outcome among confounders. The more specific adverse working conditions abusive supervision, job insecurity, and job demand were included together as predictors to see if they could explain separate parts of the variance in mental health. In all models, working conditions and sociodemographic confounders were included in the first step to evaluate their contributions to the outcome (Model 1), before entering pre-existing (T1) symptoms of the respective mental health variable in the second step to determine whether working conditions predict the mental health outcome beyond prior symptomatology (Model 2). The Mahalanobis distance was used to identify multivariate outliers considering all relevant study variables [127]. Following, sensitivity analyses for the influence of possible multivariate outliers were conducted (i.e., main analyses were calculated with versus without outliers; see Additional file 4). Due to residuals showing non-normal distributions, bootstrap sampling procedures with 5,000 iterations were applied. For mothers and partners, all analyses were performed separately. A two-tailed p-value < 0.05 was considered significant. To address multiple testing, we applied the Šidák correction , controlling the familywise error rate across our five predicted mental health outcomes (m = 5), resulting in an adjusted significance threshold of p < 0.01. To ensure transparency, we report unadjusted p-values and indicate which findings remain significant after applying the adjusted significance threshold.
Results
Sample characteristics
The sample characteristics and descriptive statistics for working conditions and mental health outcomes are provided in Table 1. Compared to the average population of Dresden [128, 129], the sample consisted mainly of parents with rather high education (58.9% of the mothers and 58.6% of the partners holding an academic degree) and contained fewer inhabitants with birth countries other than Germany (3.2% of the mothers and 1.7% of the partners born in another country than Germany). Of the expectant mothers, 29.0% were in employment ban at T1. Therefore, their answers to working conditions were filled in retrospectively for the 6 months before pregnancy/employment ban. The majority of mothers (77.8%) and partners (90.4%) worked full-time at T1/prior to employment ban. On average, mothers took longer parental leave than partners (12.7 ± 2.00 months versus 3.35 ± 2.69 months).
Table 1.
Descriptive statistics for mothers and partners
| Characteristic |
Mothers n a = 1,259 |
Partners n a = 811 |
|---|---|---|
| M ± SD (Range) or n (%) b | M ± SD (Range) or n (%) b | |
| Age (years) | 29.9 ± 3.60 (20–43) | 32.0 ± 4.36 (21–54) |
| Sex | ||
| Male | - | 799 (98.5) |
| Female | - | 12 (1.5) |
| Gestational week at T1 | 29.0 ± 6.43 (8–41) | 29.4 ± 6.62 (8–41) |
| Age of child in months at T3 | 13.8 ± 0.60 (12–18) | 13.9 ± 0.58 (12–18) |
| County of birth | ||
| Germany | 1,215 (96.8) | 793 (98.3) |
| Other | 40 (3.2) | 14 (1.7) |
| Relationship status | ||
| Permanent relationship | 1,239 (89.4) | 809 (99.9) |
| No permanent relationship | 20 (1.6) | 1 (0.1) |
| Academic degree | ||
| Academic degree | 738 (58.9) | 470 (58.6) |
| No academic degree | 516 (41.1) | 332 (41.4) |
| Employment status at T1 c | ||
| Full-time employment | 979 (77.8) | 733 (90.4) |
| Part-time employment | 237 (18.8) | 56 (6.9) |
| Marginal employment | 43 (3.4) | 22 (2.7) |
| Working hours per week at T1 c | 38.6 ± 7.79 (3–70) | 40.7 ± 7.32 (4–70) |
| Monthly income of main job at T1 c,d | ||
| More than 2,500€ | 186 (14.8) | 200 (24.7) |
| 1,501–2,500€ | 759 (60.4) | 482 (59.5) |
| 851–1,500€ | 255 (20.3) | 98 (12.1) |
| 451–850€ | 21 (1.7) | 10 (1.2) |
| Less than 450€ | 35 (2.8) | 20 (2.5) |
| Employment ban at T1 | ||
| Yes | 364 (29.0) | - |
| No | 891 (71.0) | - |
| Duration of parental leave until T3 (in months) | 12.7 ± 2.00 (0–18) | 3.35 ± 2.69 (0–18) |
| T1 Working conditions | ||
| Precarious employment e (possible range 0–4) | 0.95 ± 0.44 (0–2.86) | 0.77 ± 0.40 (0–2.38) |
| Abusive supervision f (possible range 0–4) | 0.78 ± 0.72 (0–4) | 0.55 ± 0.59 (0–3.6) |
| Job insecurity g (possible range 2–8) | 3.73 ± 1.37 (2–8) | 3.31 ± 1.22 (2–8) |
| Job demand g (possible range 2–8) | 5.87 ± 1.39 (2–8) | 5.78 ± 1.29 (2–8) |
| T3 Symptoms of | ||
| Depression h (possible range 0–30) | 5.47 ± 4.12 (0–27) | 3.97 ± 3.55 (0–19) |
| Somatization i (possible range 0–48) | 3.38 ± 3.60 (0–38) | 2.51 ± 3.01 (0–25) |
| Obsessive-compulsiveness i (possible range 0–40) | 4.06 ± 4.18 (0–29) | 3.33 ± 3.81 (0–25) |
| Anxiety i (possible range 0–40) | 1.80 ± 2.75 (0–28) | 1.26 ± 2.12 (0–20) |
| Anger/hostility i (possible range 0–24) | 2.21 ± 2.60 (0–20) | 1.58 ± 2.20 (0–18) |
a n varies slightly due to missing data of some participants. b Valid percent. Percentages may not sum to 100% due to rounding. c If mothers were in employment ban at T1, employment status/working hours before employment ban was used. d Income after taxes. e Measured with the Employment Precariousness Scale (EPRES). f Measured with the EPRES subscale vulnerability. g Measured with two items of the Effort-Reward Imbalance Questionnaire (ERI). h Measured with the Edinburgh Postnatal Depression Scale (EPDS). i Measured with the corresponding subscale of the Symptom Checklist-90-Revised (SCL-90-R)
Preliminary analyses
Attrition analyses and rates of missing data in the final sample
Attrition analyses were conducted for sociodemographic characteristics, working conditions, mental health variables, and potential confounders, comparing participants who completed T1 and T3 to participants who only completed T1 (see Additional file 1). In both mothers and partners, completers were significantly less precariously employed and among partners, completers were significantly less exposed to abusive supervision. Concerning mental health, completers reported significantly fewer symptoms of depression and anger/hostility during pregnancy in both mothers and partners, as well as fewer symptoms of obsessive-compulsiveness in mothers. Completers in both mothers and partners were significantly more often holding an academic degree and were less often born in another country than Germany. For both mothers and partners there were no significant differences between completers and non-completers regarding any other variables. Rates of missing data in the final sample (N = 2,070) were very low, with less than 1% of items missing per scale (range 0.25–0.88%; see Table S3 in Additional file 1).
Confounding variables
Of the sociodemographic confounders, age, duration of parental leave, academic degree, and employment status were selected for regression analyses of mothers, and academic degree and employment status for regression analysis of partners (for preliminary correlational analyses see Additional file 2). COVID-19 pandemic exposure was not significantly associated with mental health outcomes in neither mothers nor partners and was therefore not included in regression analyses.
Sensitivity analyses
After identifying n = 67 multivariate outliers among mothers and n = 46 among partners using Mahalanobis distance considering all relevant study variables, sensitivity analyses for the influence of possible multivariate outliers were performed (i.e., regression analyses were calculated with versus without outliers). As the sensitivity analyses indicated different significances in at least one of the calculated regression analyses, the final correlation (see Table 2) and regression analyses (see Tables 3 and 4) are reported excluding these outliers, as the results without outliers are assumed to provide more accurate estimates. However, results of correlation and regression analyses with outliers included are provided in Additional file 4.
Table 2.
Correlation matrix of study variables of mothers (above diagonal) and partners (below diagonal) after exclusion of multivariate outliers
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1) | Precarious employment T1 (EPRES) | - | .57** | .36** | .09** | .14** | .16** | .17** | .17** | .13** | −.26** | −.06* | −.18** | .22** | .20** | .16** | .19** | .14** | .12** |
| 2) |
Abusive supervision T1 (EPRES subscale) |
.42** | - | .42** | .31** | .22** | .20** | .21** | .23** | .17** | −.06* | .11** | −.15** | −.05 | .27** | .23** | .28** | .25** | .21** |
| 3) |
Job insecurity T1 (ERI selected items) |
.23** | .35** | - | .16** | .16** | .14** | .13** | .14** | .10** | .04 | .04 | −.05 | −.01 | .20** | .17** | .18** | .15** | .09** |
| 4) | Job demand T1 (ERI selected items) | −.03 | .21** | .17** | - | .08** | .14** | .09** | .12** | .07* | .06* | .06* | −.13** | −.20** | .12** | .11** | .11** | .11** | .04 |
| 5) | Symptoms of depression T3 (EPDS) | .12** | .26** | .19** | .05 | - | .43** | .56** | .53** | .56** | −.07* | −.00 | −.04 | .04 | .50** | .32** | .38** | .35** | .29** |
| 6) | Symptoms of somatization T3 a | .11** | .19** | .06 | .05 | .38** | - | .44** | .44** | .39** | −.04 | −.01 | −.05 | .01 | .31** | .46** | .35** | .32** | .23** |
| 7) | Symptoms of obsessive-compulsiveness T3 a | .14** | .26** | .11** | .00 | .57** | .47** | - | .59** | .57** | −.03 | −.00 | −.01 | .01 | .35** | .28** | .49** | .34** | .25** |
| 8) | Symptoms of anxiety T3 a | .11** | .25** | .10** | .02 | .50** | .44** | .62** | - | .46** | −.05 | −.02 | −.01 | .06* | .33** | .29** | .35** | .42** | .22** |
| 9) | Symptoms of anger/hostility T3 a | .09* | .24** | .08* | .05 | .48** | .37** | .49** | .50** | - | −.06* | −.01 | −.02 | .01 | .32** | .29** | .35** | .29** | .42** |
| 10) | Age | −.26** | −.06 | .09* | .11** | −.02 | −.06 | −.03 | −.00 | −.03 | - | .06* | .23** | −.10** | −.07* | −.11** | −.09** | −.03 | −.11** |
| 11) | Duration of parental leave up to T3 | .04 | .01 | −.01 | −.09* | −.01 | .00 | −.04 | −.07 | .01 | -.02 | - | .01 | .01 | −.02 | .01 | .05 | .04 | .01 |
| 12) | Academic degree b | −.05 | −.13** | .00 | −.04 | −.00 | −.09* | .03 | .01 | −.04 | .04 | .05 | - | −.01 | −.11** | −.11** | −.06 | −.04 | −.04 |
| 13) | Employment status T1 c | .32** | −.06 | .04 | −.16** | .11** | .05 | .07 | .03 | .02 | −.17** | .04 | .05 | - | .04 | .01 | .01 | .01 | .02 |
| 14) | Symptoms of depression T1 (EPDS) | .12** | .30** | .25** | .14** | .52** | .29** | .37** | .37** | .30** | −.03 | −.02 | .00 | .02 | - | .36** | .52** | .52** | .49** |
| 15) | Symptoms of somatization T1 a | .09* | .23** | .10** | .11** | .28** | .50** | .31** | .32** | .27** | −.07* | .01 | −.08* | .03 | .37** | - | .51** | .46** | .37** |
| 16) | Symptoms of obsessive-compulsiveness T1 a | .16** | .31** | .20** | .05 | .37** | .30** | .59** | .41** | .33** | −.02 | −.01 | .03 | .06 | .54** | .47** | - | .59** | .51** |
| 17) | Symptoms of anxiety T1 a | .10** | .27** | .17** | .13** | .38** | .35** | .43** | .51** | .34** | .01 | −.04 | .05 | .02 | .54** | .50** | .59** | - | .45** |
| 18) | Symptoms of anger/hostility T1 a | .09* | .30** | .19** | .13** | .31** | .27** | .33** | .36** | .47** | −.00 | −.03 | −.03 | −.02 | .45** | .37** | .52** | .48** | - |
Note. Pearson correlations for mothers (n ranges from 1,047 to 1,187 due to missing data) are shown above the diagonal. Pearson correlations for partners (n ranges from 598 to 763 due to missing data) are shown below the diagonal. EPRES Employment Precariousness Scale, ERI Effort-Reward Imbalance Questionnaire, EPDS Edinburgh Postnatal Depression Scale
*p < .05; **p < .01
a Measured with subscales of the Symptom Checklist-90-Revised (SCL-90-R). b 0 = no academic degree and 1 = academic degree. c 0 = full-time, 1 = part-time or marginal; if mothers were in employment ban at T1, employment status before employment ban was used
Table 3.
Hierarchical multiple regression analyses for mothers after exclusion of multivariate outliers
| Outcomes | Predictors | Model 1 | Model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms of | B | BCa 95% CI | β | p | R2 | B | BCa 95% CI | β | p | R2 | |
| Depression | Precarious employment a | 1.30 | [0.73,1.88] | .14 | < .001 | .02 | 0.45 | [−0.06,0.98] | .05 | .089 | .25 |
| Abusive supervision | 0.99 | [0.61,1.39] | .18 | < .001 | 0.49 | [0.14,0.83] | .09 | .004 | |||
| Job insecurity | 0.29 | [0.10,0.49] | .10 | .002 | 0.12 | [−0.05,0.30] | .04 | .161 | |||
| Job demand | 0.05 | [−0.12,0.22] | .02 | .577 | .06 | −0.02 | [−016,0.13] | −.01 | .794 | .27 | |
| Somatization | Precarious employment a | 1.04 | [0.60,1.49] | .15 | < .001 | .02 | 0.64 | [0.23,1.06] | .09 | .004 | .20 |
| Abusive supervision | 0.59 | [0.29,0.89] | .14 | < .001 | 0.28 | [0.02,0.56] | .07 | .042 | |||
| Job insecurity | 0.17 | [0.03,0.32] | .08 | .021 | 0.08 | [−0.06,0.21] | .03 | .299 | |||
| Job demand | 0.19 | [0.06,0.31] | .09 | .004 | .05 | 0.14 | [0.02,0.25] | .07 | .017 | .21 | |
| Obsessive-compulsiveness | Precarious employment a | 1.54 | [1.00,2.10] | .18 | < .001 | .03 | 0.73 | [0.22,1.24] | .08 | .005 | .26 |
| Abusive supervision | 1.02 | [0.64,1.40] | .20 | < .001 | 0.46 | [0.12,0.81] | .09 | .009 | |||
| Job insecurity | 0.18 | [0.00,0.35] | .07 | .046 | 0.07 | [−0.09,0.24] | .03 | .366 | |||
| Job demand | 0.05 | [−0.11,0.20] | .02 | .587 | .05 | 0.01 | [−0.13,0.15] | .00 | .924 | .25 | |
| Anxiety | Precarious employment a | 0.76 | [0.42,1.12] | .14 | < .001 | .03 | 0.45 | [0.13,0.79] | .09 | .009 | .18 |
| Abusive supervision | 0.57 | [0.34,0.82] | .19 | < .001 | 0.32 | [0.12,0.54] | .10 | .005 | |||
| Job insecurity | 0.08 | [−0.02,0.19] | .05 | .126 | 0.04 | [−0.06,0.15] | .03 | .430 | |||
| Job demand | 0.10 | [0.01,0.19] | .07 | .037 | .06 | 0.07 | [−0.02,0.15] | .04 | .135 | .19 | |
| Anger/hostility | Precarious employment a | 0.74 | [0.42,1.06] | .14 | < .001 | .02 | 0.45 | [0.17,0.75] | .09 | .003 | .19 |
| Abusive supervision | 0.56 | [0.32,0.81] | .17 | < .001 | 0.26 | [0.03,0.48] | .08 | .026 | |||
| Job insecurity | 0.06 | [−0.06,0.19] | .04 | .300 | 0.05 | [−0.06,0.16] | .03 | .329 | |||
| Job demand | 0.04 | [−0.06,0.14] | .02 | .445 | .04 | 0.04 | [−0.06,0.14] | .02 | .404 | .21 | |
Note. Results of multiple regression analyses with working conditions and sociodemographic confounders age, duration of parental leave, academic degree, and employment status (Model 1) and pre-existing (T1) symptoms of respective mental health variable added in the second step (Model 2). R2 = adjusted. Working conditions were measured during pregnancy (T1) and mental health outcomes 14 months after childbirth (T3). For standardized βs of confounding variables see Additional file 3. BCa 95% CI = Bias-corrected and accelerated 95% bootstrap confidence interval
p-values and BCa CI based on 5,000 bootstrap samples. Significant p-values after applying the Šidák correction (p < .01) are presented in bold. Significances deviating from analyses with multivariate outliers included (see Additional file 4) are presented in italics
a Precarious employment was analyzed in a separate regression model
Table 4.
Hierarchical multiple regression analyses for partners after exclusion of multivariate outliers
| Outcomes | Predictors | Model 1 | Model 2 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Symptoms of | B | BCa 95% CI | β | p | R2 | B | BCa 95% CI | β | p | R2 | |
| Depression | Precarious employment a | 0.81 | [0.18,1.47] | .10 | .015 | .01 | 0.30 | [−0.27,0.87] | .04 | .306 | .25 |
| Abusive supervision | 1.42 | [0.94,1.93] | .24 | < .001 | 0.74 | [0.32,1.17] | .12 | < .001 | |||
| Job insecurity | 0.27 | [0.07,0.47] | .10 | .013 | 0.06 | [−0.12,0.25] | .02 | .556 | |||
| Job demand | 0.01 | [−0.17,0.19] | .00 | .953 | .09 | −0.08 | [−0.24,0.12] | −.03 | .370 | .29 | |
| Somatization | Precarious employment a | 0.69 | [0.18,1.23] | .12 | .012 | .01 | 0.46 | [0.00,0.93] | .08 | .062 | .23 |
| Abusive supervision | 0.85 | [0.44,1.28] | .20 | < .001 | 0.39 | [0.05,0.75] | .09 | .025 | |||
| Job insecurity | 0.00 | [−0.15,0.16] | .00 | .994 | −0.01 | [−0.14,0.13] | −.00 | .927 | |||
| Job demand | 0.04 | [−0.10,0.17] | .02 | .586 | .04 | −0.02 | [−0.14,0.13] | −.01 | .778 | .26 | |
| Obsessive-compulsiveness | Precarious employment a | 1.18 | [0.57,1.83] | .15 | < .001 | .02 | 0.55 | [0.03,1.09] | .07 | .046 | .28 |
| Abusive supervision | 1.62 | [1.12,2.14] | .28 | < .001 | 0.63 | [0.19,1.08] | .11 | .004 | |||
| Job insecurity | 0.04 | [−0.15,0.22] | .01 | .708 | −0.11 | [−0.28,0.06] | −.04 | .195 | |||
| Job demand | −0.12 | [−0.30,0.06] | −.05 | .213 | .07 | −0.08 | [−0.24,0.08] | −.03 | .336 | .34 | |
| Anxiety | Precarious employment a | 0.51 | [0.20,0.85] | .12 | .002 | .01 | 0.29 | [0.02,0.59] | .07 | .045 | .22 |
| Abusive supervision | 0.87 | [0.59,1.20] | .27 | < .001 | 0.46 | [0.21,0.72] | .14 | < .001 | |||
| Job insecurity | 0.03 | [−0.08,0.14] | .02 | .597 | −0.02 | [−0.14,0.09] | −.02 | .663 | |||
| Job demand | −0.04 | [−0.15,0.06] | −.03 | .447 | .07 | −0.08 | [−0.17,0.01] | −.06 | .094 | .28 | |
| Anger/hostility | Precarious employment a | 0.38 | [0.06,0.70] | .09 | .021 | .00 | 0.15 | [−0.13,0.44] | .04 | .313 | .22 |
| Abusive supervision | 0.70 | [0.42,0.98] | .24 | < .001 | 0.35 | [0.09,0.60] | .12 | .007 | |||
| Job insecurity | −0.01 | [−0.13,0.11] | −.01 | .863 | −0.06 | [−0.17,0.06] | −.04 | .304 | |||
| Job demand | −0.02 | [−0.12,0.08] | −.01 | .741 | .05 | −0.04 | [−0.13,0.04] | −.04 | .300 | .22 | |
Note. Results of multiple regression analyses with working conditions and sociodemographic confounders academic degree and employment status (Model 1) and pre-existing (T1) symptoms of respective mental health variable added in the second step (Model 2). R2 = adjusted. Working conditions were measured during pregnancy (T1) and mental health outcomes 14 months after childbirth (T3). For standardized βs of confounding variables see Additional file 3. BCa 95% CI = Bias-corrected and accelerated 95% bootstrap confidence interval
p-values and BCa CI based on 5,000 bootstrap samples. Significant p-values after applying the Šidák correction (p < .01) are presented in bold. Significances deviating from analyses with multivariate outliers included (see Additional file 4) are presented in italics
a Precarious employment was analyzed in a separate regression model
Main analyses
Precarious employment as a predictor of mental health symptoms
Precarious employment during pregnancy significantly correlated with all mental health outcomes 14 months postpartum in mothers (ps < 0.001) and partners (ps < 0.05; see Table 2). In hierarchical regression analyses controlling for relevant sociodemographic confounders (Model 1), precarious employment was a significant predictor for all mental health outcomes in mothers (βs = 0.14 to 0.18, ps < 0.001, Table 3) and partners (βs = 0.09 to 0.15, ps < 0.05, Table 4). Whereas all regression coefficients remained significant after Šidák correction in mothers, this was only the case for symptoms of obsessive-compulsiveness and anxiety in partners (p < 0.001, p = 0.002, respectively).
After controlling for pre-existing symptoms of the respective mental health outcome at T1 in addition to sociodemographic confounders (Model 2), precarious employment remained a significant predictor for symptoms of somatization (β = 0.09, p = 0.004), obsessive-compulsiveness (β = 0.08, p = 0.005), anxiety (β = 0.09, p = 0.009), and anger/hostility (β = 0.09, p = 0.003), all significant at Šidák-adjusted level, but not for symptoms of depression (β = 0.05, p = 0.089) in mothers. In partners, precarious employment remained a significant predictor for symptoms of obsessive-compulsiveness (β = 0.07, p = 0.046) and anxiety (β = 0.07, p = 0.045), although not below the threshold according to the Šidák correction; it also no longer significantly predicted the other mental health outcomes in partners after controlling for their respective pre-existing symptomatology (Model 2; βs = 0.04 to 0.08, ps > 0.062).
Abusive supervision as a predictor of mental health symptoms
Abusive supervision during pregnancy correlated significantly with all mental health outcomes 14 months postpartum in mothers and partners (ps < 0.001, see Table 2). In hierarchical regression analyses controlling for relevant sociodemographic confounders (Model 1), abusive supervision was a significant predictor for all mental health outcomes in mothers (βs = 0.14 to 0.20, ps < 0.001, Table 3) and partners (βs = 0.20 to 0.28, ps < 0.001, Table 4), all significant at Šidák-adjusted level.
After controlling for pre-existing symptoms of the respective mental health outcome at T1 in addition to sociodemographic confounders (Model 2), abusive supervision remained a significant predictor for all mental health outcomes in mothers (βs = 0.07 to 0.10, ps < 0.05) and partners (βs = 0.09 to 0.14, ps < 0.05). At the Šidák-adjusted level, the regression coefficients remained significant for symptoms of depression, obsessive-compulsiveness, and anxiety in mothers (p = 0.004, 0.009, 0.005, respectively) and symptoms of depression, obsessive-compulsiveness, anxiety, and anger/hostility in partners (p < 0.001, p = 0.004, p < 0.001, p = 0.007, respectively).
Job insecurity as a predictor of mental health symptoms
Job insecurity during pregnancy correlated significantly with all mental health outcomes 14 months postpartum in mothers (ps < 0.001) and all mental health outcomes (ps < 0.05) besides symptoms of somatization (p = 0.099) in partners (see Table 2). In hierarchical regression analyses controlling for relevant sociodemographic confounders (Model 1), job insecurity was a significant predictor for symptoms of depression, somatization, and obsessive-compulsiveness in mothers (βs = 0.07 to 0.10, ps < 0.05, Table 3) and symptoms of depression in partners (β = 0.10, p = 0.013, Table 4), but not for the remaining mental health outcomes (βs = −0.01 to 0.05, ps > 0.126). When applying the Šidák-adjusted significance threshold of p < 0.01, only the regression coefficient for symptoms of depression in mothers (p = 0.002) remained significant.
In both mothers and partners, job insecurity no longer significantly predicted any of the mental health outcomes after controlling for the respective pre-existing symptomatology in addition to sociodemographic confounders (Model 2; βs = −0.04 to 0.04, ps > 0.161).
Job demand as a predictor of mental health symptoms
Job demand during pregnancy correlated significantly with all mental health outcomes 14 months postpartum in mothers (ps < 0.05), but none of the mental health outcomes in partners (ps > 0.140, see Table 2). In hierarchical regression analyses controlling for relevant sociodemographic confounders (Model 1), job demand was a significant predictor for symptoms of somatization and anxiety in mothers (βs = 0.09 and 0.07, respectively, ps < 0.05, Table 3) but did not predict the remaining mental health outcomes in mothers (βs = 0.02, ps > 0.445) or any of the mental health outcomes in partners (βs = −0.05 to 0.02, ps > 0.213, Table 4). Thereby, only the predictive relationship with symptoms of somatization in mothers (p = 0.004) remained significant after Šidák correction.
After controlling for pre-existing symptoms of the respective mental health outcome at T1 in addition to sociodemographic confounders (Model 2), job demand remained a significant predictor for symptoms of somatization (β = 0.07, p = 0.017, non-significant at Šidák-adjusted level), but not for symptoms of anxiety (β = 0.04, p = 0.135) in mothers. In both mothers and partners, job demand did not predict any of the (remaining) mental health outcomes after controlling for their respective pre-existing symptomatology (βs = −0.06 to 0.02, ps > 0.094).
Discussion
The present study aimed to enhance our understanding of work-related risk factors for the adjustment of parents in the transition to parenthood by investigating the predictive value of adverse prepartum working conditions for a variety of mental health outcomes 14 months postpartum in both mothers and their partners. Our findings provide evidence for the predictive role of adverse prepartum working conditions (i.e., precarious employment and exposure to abusive supervision, job insecurity, and job demand) for parental mental health (i.e., symptoms of depression, somatization, obsessive-compulsiveness, anxiety, and anger/hostility) 14 months after childbirth when controlling for relevant sociodemographic confounders and symptom levels during pregnancy. Precarious employment and abusive supervision emerged as particularly stable predictors of mental health outcomes, whereas results for the predictive value of job insecurity and job demand were mixed.
Precarious employment significantly predicted all mental health outcomes in mothers and partners, supporting the results from recent systematic/scoping reviews and a meta-analysis [53, 55, 130] that identified precarious employment as an important risk factor for mental health symptoms in diverse worker samples. Moreover, this finding is in line with a recent study by our group that identified precarious employment during pregnancy as a significant predictor of symptoms of depression in mothers eight weeks after childbirth [70]. After controlling for symptoms of the respective mental health variable during pregnancy in our regression analyses, precarious employment remained a significant predictor for mothers’ and partners’ symptoms of obsessive-compulsiveness and anxiety, as well as mothers’ symptoms of somatization and anger/hostility. However, it no longer predicted symptoms of depression in mothers and partners and symptoms of somatization and anger/hostility in partners. Whereas all significant findings survived Šidák correction in mothers, in partners this was only the case for symptoms of obsessive-compulsiveness and anxiety before controlling for prior mental health symptoms. Together, our findings indicate that precarious employment may be crucial for parental, especially maternal, postpartum mental health – for several symptoms independent of pre-existing symptomatology, particularly anxiety-related symptoms. Given that precarious employment is a multidimensional construct encompassing a range of unfavorable objective (e.g., temporary employment, low wages) and subjective (e.g., supervisor behavior) working conditions [53], the prospective associations we found with postpartum mental health point to the necessity of considering diverse aspects of the work environment to gain a comprehensive understanding of their impact on new parents.
Abusive supervision significantly predicted all mental health outcomes in mothers and partners, even after controlling for symptoms of the respective mental health variable during pregnancy. When using Šidák correction, all predictive relationships remained significant before controlling for prior symptoms; after controlling for prior symptoms, all predictive relationships except for symptoms of somatization (in both mothers and partners) and anger/hostility (in mothers) remained significant. Together, these findings are in line with former research that identified abusive supervision as a risk factor for workers’ mental health outside the peripartum period [78, 131, 132]. Furthermore, it is consistent with previous investigations showing that supportive supervisor behaviors can have a protective effect on parental mental health [81, 82], assuming that supportive supervision can be understood as the opposite or absence of abusive supervision. Former research emphasizes that abusive supervision violates the important moral principle of treating people respectfully and can evoke several negative stress-related emotions in employees, such as anger, fear, and shame [133], which may explain the particular detrimental effect on postpartum mental health that we found in our sample. Interestingly, a recent study on mothers during the transition to parenthood found that even witnessing abusive supervision predicted adverse mental health outcomes, beyond their own experience [66], again highlighting the particularly stressful nature of abusive supervision.
Job insecurity significantly predicted symptoms of depression in mothers and partners as well as symptoms of somatization and obsessive-compulsiveness in mothers, which is in line with results from the general working population [76, 77], working parents [45, 58, 134], and former research identifying job insecurity as a risk factor for parental depression and anxiety symptoms in the first year postpartum [83–85]. However, only the predictive relationship with symptoms of depression in mothers survived Šidák correction. Furthermore, after controlling for the respective symptom levels during pregnancy, none of the regression coefficients remained significant in our sample, indicating no additive predictive value above the previous mental health status. Moreover, job insecurity did not predict any of the other mental health outcomes in mothers and partners. These findings appear to contradict the aforementioned studies. However, it should be noted that the cited studies on new parents were cross-sectional and did not include outcomes other than depression and anxiety – an important difference from our study design. Furthermore, a recent meta-analysis, which included only prospective cohort studies, reported inconsistent associations between job insecurity and stress-related mental disorders [6], which is in line with our findings that associations depend on the outcome and may not explain variance beyond the preceding symptomatology. Another reason for our mixed results compared to international studies may be that workers in Germany generally enjoy a comparatively high level of security and can mostly rely on regulations on unemployment benefits after job loss, and therefore may perceive job insecurity as less threatening. Furthermore, at least mothers in our sample can mostly rely on legal protection against dismissal during pregnancy and parental leave, which reduces the objective risk of job loss during this period. In addition, the labor market for well-trained workers in Germany is comparatively good, which could make a potential job loss seem less threatening due to the good chances of finding a new job. Therefore, job insecurity may have less weight in our specific sample of highly educated German workers in the transition to parenthood. As we entered abusive supervision, job insecurity, and job demand simultaneously in one model, the limited effect could also be explained by the overlapping variance of job insecurity with abusive supervision, supported by their significant moderate correlation.
Results for the predictive value of job demand were also mixed. While job demand significantly predicted symptoms of somatization in mothers, even after controlling for pre-existing symptoms of somatization during pregnancy, the significant predictive association with symptoms of anxiety was no longer significant after controlling for pre-existing symptoms of anxiety. Furthermore, job demand did not significantly predict any of the other mental health outcomes in mothers, and none of the mental health outcomes in partners. Moreover, only the predictive relationship with symptoms of somatization in mothers before controlling for prior symptoms remained significant after Šidák correction. While these findings are in line with a study in which job demand was no relevant predictor after controlling for other variables [78, 135], they contradict former literature identifying job demand as an important predictor of parental mental health in the transition to parenthood [81] and the general population [6]. A possible explanation for these mixed findings is provided by the challenge-hindrance framework [136, 137], which suggests that job demands must be distinguished into challenge stressors (i.e., appraised as potentially promoting achievement) and hindrance stressors (i.e., appraised as potentially threatening achievement). Research indicates that challenge appraisals are positively associated with favorable health outcomes, whereas hindrance appraisals are negatively associated with favorable health outcomes [138]. However, the appraisal process of job demands is not straightforward. Gerich and Weber [136] report that it is moderated by perceived job control and social support at work and that job demands can simultaneously incorporate challenge and hindrance components. Furthermore, the relation between demand intensity and challenge appraisal is reported to be curvilinear, suggesting that too low job demands can even deteriorate health outcomes via feelings of frustration or boredom [136, 137]. As we did not assess individual challenge/hindrance appraisals or perceptions of control and social support at work, we could not account for their potential influence. Given the relatively high level of education in our sample, many parents may hold jobs that offer a high degree of control [139]. This perceived job control may facilitate challenge appraisals, which could explain the lack of significant associations between job demand and mental health outcomes. Overall, our results on job demand are in line with the conflicting results of previous studies and the possibility that its influence depends on other mediating/moderating variables, such as job resources (e.g., supervisor support, and job control; [135]).
As reported above, many prospective associations of working conditions remained significant even when controlling for pre-existing symptomatology (i.e., precarious employment as a predictor for mothers’ and partners’ symptoms of obsessive-compulsiveness and anxiety, and mothers’ symptoms of somatization and anger/hostility; abusive supervision as a predictor for all mental health outcomes in mothers and partners; and job demand as a predictor for mothers’ symptoms of somatization). After Šidák correction, this held for: (1) precarious employment predicting mothers’ symptoms of somatization, obsessive-compulsiveness, anxiety, and anger/hostility; and (2) abusive supervision predicting symptoms of depression, obsessive-compulsiveness, and anxiety in both mothers and partners, as well as partners’ symptoms of anger/hostility. This demonstrates so-called “Granger causality” [140], meaning that working conditions have a predictive effect on mental health over time beyond the initial symptom level. Importantly, that some of the relationships were no longer significant when adjusting for pre-existing symptoms does not imply that the working condition is irrelevant. Potential influences could have already manifested at T1 or earlier and thus do not lead to further deterioration.
Our multiple regression analyses showed similar patterns of associations for the different mental health symptoms considered, indicating that adverse working conditions might have an impact on mental health in general and contribute to a general vulnerability [53, 76]. The fact that adverse working conditions also predicted symptoms of somatization, obsessive-compulsiveness, and anger/hostility – which have received much less attention than symptoms of depression or anxiety in the literature – emphasizes the importance of considering a range of symptoms in research and practice so that no affected parents are overlooked. In addition, our results evidence persistent and/or delayed effects (i.e., adverse working conditions measured during pregnancy prospectively predicted mental health many months later). Together, these findings align with the COR Theory [64, 65], which proposes that adverse prepartum working conditions reduce the parents’ resources to cope with upcoming strains and thereby might hinder a successful adjustment in the long term. The consideration that adverse working conditions might unfold their impact on mental health symptoms as a general stressor consuming available coping resources is particularly worrying as the transition to parenthood is already a vulnerable period in terms of mental health with many challenges, and (expectant) parents may therefore be particularly affected by adverse working conditions. For a better understanding of the hereby suggested stress-related mechanisms underlying the influence of adverse working conditions on parental mental health in the transition to parenthood, it is imperative to include stress biomarkers in research. For instance, Julià et al. [56] reported that precarious employment is related to employees’ stress biomarkers of adrenal and gonadal hormone production, including cortisol. So far, research on new parents within this context is lacking.
Research on peripartum mental health in partners is generally scarce. However, this gap might be particularly relevant in the context of work factors, as the work environment usually remains present for partners throughout the transition to parenthood, whereas mothers typically plan for longer periods of parental leave after childbirth. Parental leave may buffer the effects of adverse prepartum working conditions, as they become more distant from the postpartum period. The findings of a recent study indeed support that prepartum work factors might be of greater relevance for paternal than maternal postpartum mental health symptoms [57]. However, in the current study, working conditions predicted mental health symptoms in a similar way in both mothers and partners. Minor differences pertain to precarious employment, job insecurity, and job demand predicting slightly more mental health symptoms in mothers than in partners (98.5% males). This contradictory finding might be explained by differential exposure and/or gender inequalities concerning the perception and appraisal of working characteristics – for instance, women are more likely than men to be employed precariously or have jobs with less prestige and control [53, 141]. In line with the considerations above, whether job demands are rather appraised as a hindrance or challenge might differ between mothers and partners due to differential exposure to jobs with low control or autonomy, which has been found to moderate or mediate the association between adverse working conditions and mental health symptoms [136, 142] as well as gender and depressive symptoms [143]. Overall, the results underscore that we need to take both mothers and their partners into focus when examining work factors influencing peripartum mental health. This need is reinforced by the fact that dyadic effects are to be expected, as partners’ mental health was found to be interdependent [144], meaning that poor working conditions of one partner could indirectly affect the mental health of the other partner. Further dyadic research is needed to study these potential dyadic effects related to working conditions.
Strengths and limitations
This study is the first to examine precarious employment and abusive supervision as prospective risk factors for mothers’ and partners’ mental health in the transition to parenthood. Further strengths include our large sample size, the longitudinal approach, the use of validated measures for work and mental health variables, and the multiple theoretical approaches in assessing working conditions. In addition, we considered a wide range of potential mental health symptoms, including symptoms of depression and anxiety, but also less-often-studied symptoms of somatization, obsessive-compulsiveness, and anger/hostility. Moreover, in the second step of our hierarchical multiple regression analyses, we controlled for pre-existing symptoms of the respective mental health variable during pregnancy, and many of the effects remained significant in these models. Thus, we establish “Granger causality” [140], indicating that working conditions during pregnancy provide information that helps predict mental health outcomes 14 months postpartum, beyond the predictive power of mental health status during pregnancy alone. Another strength is that we considered COVID-19 pandemic exposure as a potential confounder due to the reported pandemic-related burden on peripartum mental health (e.g., [125, 145]). As there were no significant correlations with our outcome measures, COVID-19 pandemic exposure was not included in our main analyses. Finally, our rigorous approach to multivariate outliers (i.e., detecting multivariate outliers using Mahalanobis distance, conducting sensitivity analyses with outliers included to examine their influence, and deciding to exclude them from the main analyses) ensures that the results of the regression analyses, which are not robust to outliers, are not distorted by their influence. As the sensitivity analyses revealed minor differences, particularly in Model 2 and in the direction of additional significant associations, we are confident that our approach provides the most robust estimates for the prospective associations investigated.
Notwithstanding, the current study has some limitations. Firstly, some findings did not remain statistically significant after the Šidák correction and should therefore be interpreted with caution. However, the correction did not alter the overall pattern of predictive relationships, supporting the robustness of our conclusions while addressing multiple testing concerns. Furthermore, changes in the working situation after their assessment during pregnancy were not included in our analyses because a substantial portion of our sample, particularly mothers, had not (yet) returned to work at the time of the postpartum survey (n not working: mothers = 556, 44.2%; partners = 76, 9.4%). Additionally, we did not assess whether participants remained in the same employment contract, which would have been necessary to accurately capture changes in the working conditions over time. Consequently, some participants may have experienced better or worse working conditions or were not working at the time of their mental health assessment. Nevertheless, the significant prospective associations we found emphasize the long-term centrality of working conditions during pregnancy for postpartum mental health, regardless of current working conditions. Moreover, due to the predominantly high educational level of the sample, our results are especially generalizable to a more highly educated population. It can be assumed that education is intertwined with the investigated relationships due to interrelations with occupational position and exposure to precarity in work [146]. Our finding that working conditions play an important role in the adjustment to parenthood, even among highly educated (expectant) parents less exposed to precarious conditions, is nonetheless important and concerns many families and – through the workers’ contribution to the economy – also society as a whole [147]. Attrition analyses revealed that participants with no academic degree, poorer mental health, and higher scores of precarious employment and abusive supervision measured during pregnancy were more likely to drop out of the study, suggesting attrition-related "missing at random" (MAR). While we cannot entirely rule out "missing not at random" (MNAR), as distinguishing MAR from MNAR is inherently impossible, we have no evidence for MNAR and consider it rather unlikely. Nevertheless, our results may even underestimate the true relationships between precarious employment and abusive supervision and mental health. These findings indicate that it is crucial to identify expectant parents who are experiencing particularly adverse working conditions or existing mental health problems at an early stage, in order to prevent them from being overlooked and to ensure that they receive the necessary support. Regarding missing data handling within the final sample, we applied person mean imputation for participants missing up to 20% of items on a scale. While we acknowledge that methods such as multiple imputation or full information maximum likelihood are generally more robust techniques, person mean imputation was deemed appropriate in our case due to the very low overall rates of missing data (< 1%, see Table S3 in Additional file 1), which makes potential bias likely negligible, coupled with its greater practicability.
The use of subjective ratings of working conditions implies that ratings depend on individual expectations and standards (e.g., what authoritarian behavior by supervisors entails or what an increasing workload means personally). However, we did use the recommended multidimensional measure of precarious employment including objective data such as type of contract, permanent vs. temporary employment, or salary [53]. Furthermore, research indicates that both objective aspects as well as perceived dimensions of working conditions can impact workers’ mental health (e.g., [142, 148]), suggesting that a combined approach, as in our study, is indeed most suitable.
Implications
The current study underscores the importance of considering adverse working conditions as significant risk factors for mental health problems during the transition to parenthood. Policymakers should prioritize reducing the prevalence of mental health problems in new parents by implementing stronger protections against adverse working conditions – specifically precarious employment and abusive supervision – during the transition to parenthood. This could prevent adverse outcomes for both parents [149] and, in turn, also children [45, 90, 107]. Moreover, promoting strategies against precarious employment could help reduce health inequalities [143, 150].
Clinicians should consider the findings of this study in prenatal care by inquiring about the working conditions and social environment at work for pregnant women and their partners. Parents who are already vulnerable before the birth of their child may be especially susceptible to adverse working conditions, as their resources to cope with challenges are more limited [86, 151]. In contrast, parents with abundant resources may better manage these additional stressors. Identifying individuals at risk allows for targeted preventive interventions, such as psychological counseling on stress management. Developing screening methods for clinical settings to identify these at-risk individuals is crucial for effective early intervention.
In future research, it would be interesting to explore cross-country comparisons, as government regulations (e.g., regarding parental leave policies) could modulate the effects of adverse working conditions. Additionally, further studies could enhance a more differentiated understanding by comparing the mental health impact of working conditions among new parents, parents with older children, and individuals without children. Examining longitudinal cross-lagged changes in both working conditions and mental health, especially around the birth of a child, would provide valuable insights regarding potential causal directions. Furthermore, studies incorporating biomarkers of stress responses will be beneficial in elucidating the physiological mechanisms underlying the impact of working conditions on parental mental health. Such investigations are part of the DREAM sub-studies DREAMHAIR and DREAMEPI, with the latter also focusing on the stress-related effects on offspring [for further information see study protocol; 108], and related publications currently under review. In addition, further research explicitly examining dyadic couple data, as in the study by Kress et al. [57], will provide a more thorough understanding of how working conditions impact family mental health by considering the interconnected experiences of both partners during the transition to parenthood [152]. Finally, future research could contribute to a deeper understanding of the role of working conditions for (expectant) parents’ mental health by integrating a more comprehensive range of established work-related mediating/moderating protective and risk factors into a model that incorporates our findings and testing hypotheses about potential mechanisms. Among these factors, work-family/family-work conflict, relationships with co-workers, perceptions of control, autonomy, flexibility, and social support [83, 84, 87] could be especially instructive.
Mental health problems in new parents can have profound implications, not only for the affected individuals but also for the healthy development of their offspring [45, 90, 107], as well as for society as a whole, due to the high costs associated with mental health issues [9–13]. Therefore, addressing the work-related factors contributing to these problems is not only critical for individual families but also for broader societal well-being and public mental health.
Conclusions
Our findings provide new evidence that adverse working conditions can act as risk factors for first-time parents’ mental health during the vulnerable transition to parenthood. In particular, precarious employment and abusive supervision before or during pregnancy emerged as important predictors of mental health symptoms 14 months postpartum. These results underscore the urgency of further research into the underlying mechanisms affecting both mothers and their partners. Work policies promoting beneficial working conditions are imperative. Additionally, our study highlights the critical need for targeted preventive measures during pregnancy to mitigate potential adverse effects. Addressing the identified work-related risk factors is essential for promoting the well-being of new parents and their families.
Supplementary Information
Acknowledgements
We want to thank all participating mothers and partners. Data collection and management were facilitated using Research Electronic Data Capture (REDCap), a secure, web-based application for data capture as part of research studies (Harris et al., 2009, 2019), hosted at the “Koordinierungszentrum für Klinische Studien” at the Faculty of Medicine of the Technical University of Dresden.
Abbreviations
- DREAM
DResdner Studie zu Elternschaft, Arbeit und Mentaler Gesundheit; Dresden Study on Parenting, Work, and Mental Health
- OECD
Organisation for Economic Co-operation and Development
- COR
Conservation of Resources
- COVID-19
Coronavirus Disease 2019
- EPRES
Employment Precariousness Scale
- ERI
Effort-Reward Imbalance Questionnaire
- EPDS
Edinburgh Postnatal Depression Scale
- SCL-90-R
Symptom-Checklist Revised
- MAR
Missing at random
- MNAR
Missing not at random
Authors’ contributions
LR, JW, MK, VW, and SGN were responsible for the design and conceptualization of the study and defining the research questions. JTM and VW prepared the study data for statistical analysis. LR and JW performed the statistical analyses and interpreted the data. MK, VW, and SGN supervised data analyses and interpretation of the data. SGN acquired funding for this project and was responsible for the conception, design, and coordination of DREAM. LR and JW wrote the first draft of the manuscript. All authors revised subsequent drafts and read and approved the final manuscript for publication.
Funding
Open Access funding enabled and organized by Projekt DEAL. DREAM is funded by the German Research Foundation (“Deutsche Forschungsgemeinschaft”; DFG; grant numbers GA 2287/4–1, GA 2287/4–2, and GA 2287/4–3). The publication was funded by the Open Access budget of MSH Medical School Hamburg. The founders were not involved in the conceptualization, design, data collection, analysis, decision to publish, or preparation of the manuscript.
Data availability
The dataset presented in this article is not publicly available because of legal and ethical constraints. Public sharing of participant data was not included in the informed consent of the study. Requests to access the datasets should be directed to the project manager and principal investigator Susan Garthus-Niegel.
Declarations
Ethics approval and consent to participate
DREAM was reviewed and approved by the Ethics Committee of the Technical University of Dresden (EK 278062015). During recruitment, participants were informed about the study procedure and its objectives, as well as the pseudonymization of their data and their right to withdraw from the study at any time. Each participant signed a declaration of informed consent to participate. This study was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Lydia Rihm, Email: lydia.rihm@medicalschool-hamburg.de.
Susan Garthus-Niegel, Email: susan.garthus-niegel@ukdd.de.
References
- 1.Niedhammer I, Bertrais S, Witt K. Psychosocial work exposures and health outcomes: a meta-review of 72 literature reviews with meta-analysis. Scand J Work Environ Health. 2021;47:489–508. [DOI] [PMC free article] [PubMed]
- 2.Paul KI, Scholl H, Moser K, Zechmann A, Batinic B. Employment status, psychological needs, and mental health: Meta-analytic findings concerning the latent deprivation model. Front Psychol. 2023;14:1017358. [DOI] [PMC free article] [PubMed]
- 3.Heinz AJ, Meffert BN, Halvorson MA, Blonigen D, Timko C, Cronkite R. Employment characteristics, work environment, and the course of depression over 23 years: Does employment help foster resilience? Depress Anxiety. 2018;35:861–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Butterworth P, Leach LS, Strazdins L, Olesen SC, Rodgers B, Broom DH. The psychosocial quality of work determines whether employment has benefits for mental health: results from a longitudinal national household panel survey. Occup Environ Med. 2011;68:806–12. [DOI] [PubMed] [Google Scholar]
- 5.Duchaine CS, Aubé K, Gilbert-Ouimet M, Vézina M, Ndjaboué R, Massamba V, et al. Psychosocial Stressors at Work and the Risk of Sickness Absence Due to a Diagnosed Mental Disorder: A Systematic Review and Meta-analysis. JAMA Psychiat. 2020;77:842–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van der Molen HF, Nieuwenhuijsen K, Frings-Dresen MHW, de Groene G. Work-related psychosocial risk factors for stress-related mental disorders: an updated systematic review and meta-analysis. BMJ Open. 2020;10: e034849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cortès-Franch I, Puig-Barrachina V, Vargas-Leguás H, Arcas MM, Artazcoz L. Is Being Employed Always Better for Mental Wellbeing Than Being Unemployed? Exploring the Role of Gender and Welfare State Regimes during the Economic Crisis. Int J Environ Res Public Health. 2019;16:4799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Chandola T, Zhang N. Re-employment, job quality, health and allostatic load biomarkers: prospective evidence from the UK Household Longitudinal Study. Int J Epidemiol. 2018;47:47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Oliveira C, Saka M, Bone L, Jacobs R. The Role of Mental Health on Workplace Productivity: A Critical Review of the Literature. Appl Health Econ Health Policy. 2023;21:167–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van Hoffen MFA, Rijnhart JJM, Norder G, Labuschagne LJE, Twisk JWR. Distress, Work Satisfaction, and Work Ability are Mediators of the Relation Between Psychosocial Working Conditions and Mental Health-Related Long-Term Sickness Absence. J Occup Rehabil. 2021;31:419–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hennekam S, Richard S, Grima F. Coping with mental health conditions at work and its impact on self-perceived job performance. Empl Relat. 2020;42:626–45. [Google Scholar]
- 12.Weber J, Hasselhorn HM, Borchart D, Angerer P, Müller A. The moderating role of psychosocial working conditions on the long-term relationship between depressive symptoms and work ability among employees from the Baby Boom generation. Int Arch Occup Environ Health. 2021;94:295–307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Arias D, Saxena S, Verguet S. Quantifying the global burden of mental disorders and their economic value. eClinicalMedicine. 2022;54:101675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.International Labour Organization. Women with young children have much lower labour force participation rates. 2024. https://ilostat.ilo.org/blog/women-with-young-children-have-much-lower-labour-force-participation-rates/. Accessed 11 July 2024.
- 15.OECD. Society at a Glance 2024: OECD Social Indicators. Paris: OECD Publishing; 2024. 10.1787/918d8db3-en. [DOI]
- 16.OECD. Distribution of working hours in couple households (LMF 2.2). 2023. https://www.oecd.org/els/family/LMF-2-2-Distribution-working-hours-couple-households_DRAFT.pdf. Accessed 11 July 2024.
- 17.Saxbe D, Rossin-Slater M, Goldenberg D. The transition to parenthood as a critical window for adult health. Am Psychol. 2018;73:1190–200. [DOI] [PubMed] [Google Scholar]
- 18.Hutchens BF, Kearney J. Risk Factors for Postpartum Depression: An Umbrella Review. J Midwifery Womens Health. 2020;65:96–108. [DOI] [PubMed] [Google Scholar]
- 19.Garthus-Niegel S, Schaber R. The Impact of Working Conditions on Postpartum Depressive Symptoms and Family Relations: Re-evaluated in Light of the COVID-19 Pandemic. In: Pramataroff-Hamburger V, Neises-Rudolf M, editors. Women’s Health and Pandemic Crisis. Cham: Springer Nature Switzerland; 2024. p. 45–60. [Google Scholar]
- 20.Sacks E, Langlois ÉV. Postnatal care: increasing coverage, equity, and quality. Lancet Glob Health. 2016;4:e442–3. [DOI] [PubMed] [Google Scholar]
- 21.Ford MT, Cerasoli CP, Higgins JA, Decesare AL. Relationships between psychological, physical, and behavioural health and work performance: A review and meta-analysis. Work Stress. 2011;25:185–204. [Google Scholar]
- 22.Vogel JP, Jung J, Lavin T, Simpson G, Kluwgant D, Abalos E, et al. Neglected medium-term and long-term consequences of labour and childbirth: a systematic analysis of the burden, recommended practices, and a way forward. Lancet Glob Health. 2024;12:e317–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018;15: e1002494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Weibel S, Neubert K, Jelting Y, Meissner W, Wöckel A, Roewer N, et al. Incidence and severity of chronic pain after caesarean section: A systematic review with meta-analysis. Eur J Anaesthesiol. 2016;33:853–65. [DOI] [PubMed] [Google Scholar]
- 25.Ayers S, Crawley R, Webb R, Button S, Thornton A. What are women stressed about after birth? Birth. 2019;46:678–85. [DOI] [PubMed] [Google Scholar]
- 26.McCarthy M, Houghton C, Matvienko-Sikar K. Women’s experiences and perceptions of anxiety and stress during the perinatal period: a systematic review and qualitative evidence synthesis. BMC Pregnancy Childbirth. 2021;21:811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baldwin S, Malone M, Sandall J, Bick D. Mental health and wellbeing during the transition to fatherhood: a systematic review of first time fathers’ experiences. JBI Evid Synth. 2018;16:2118–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bogdan I, Turliuc MN, Candel OS. Transition to Parenthood and Marital Satisfaction: A Meta-Analysis. Front Psychol. 2022;13:901362. [DOI] [PMC free article] [PubMed]
- 29.Navon-Eyal M, Taubman-Ben-Ari O. A longitudinal perspective of the change in personal growth in the transition to motherhood and predicting factors. Psychol Trauma. 2024. Advance online publication. 10.1037/tra0001653. [DOI] [PubMed]
- 30.Wang Z, Liu J, Shuai H, Cai Z, Fu X, Liu Y, et al. Mapping global prevalence of depression among postpartum women. Transl Psychiatry. 2021;11:543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Al-Abri K, Edge D, Armitage CJ. Prevalence and correlates of perinatal depression. Soc Psychiatry Psychiatr Epidemiol. 2023;58:1581–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rao WW, Zhu XM, Zong QQ, Zhang Q, Hall BJ, Ungvari GS, et al. Prevalence of prenatal and postpartum depression in fathers: A comprehensive meta-analysis of observational surveys. J Affect Disord. 2020;263:491–9. [DOI] [PubMed] [Google Scholar]
- 33.Leiferman JA, Farewell CV, Jewell J, Lacy R, Walls J, Harnke B, et al. Anxiety among fathers during the prenatal and postpartum period: a meta-analysis. J Psychosom Obstet Gynaecol. 2021;42:152–61. [DOI] [PubMed] [Google Scholar]
- 34.Dennis C-L, Falah-Hassani K, Shiri R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br J Psychiatry. 2017;210:315–23. [DOI] [PubMed] [Google Scholar]
- 35.Nielsen-Scott M, Fellmeth G, Opondo C, Alderdice F. Prevalence of perinatal anxiety in low- and middle-income countries: A systematic review and meta-analysis. J Affect Disord. 2022;306:71–9. [DOI] [PubMed] [Google Scholar]
- 36.Fawcett EJ, Fairbrother N, Cox ML, White IR, Fawcett JM. The Prevalence of Anxiety Disorders During Pregnancy and the Postpartum Period: A Multivariate Bayesian Meta-Analysis. J Clin Psychiatry. 2019;80:1181. [DOI] [PMC free article] [PubMed]
- 37.Starcevic V, Eslick GD, Viswasam K, Berle D. Symptoms of Obsessive-Compulsive Disorder during Pregnancy and the Postpartum Period: a Systematic Review and Meta-Analysis. Psychiatr Q. 2020;91:965–81. [DOI] [PubMed] [Google Scholar]
- 38.Koerber MI, Mack JT, Seefeld L, Kopp M, Weise V, Starke KR, et al. Psychosocial work stress and parent-child bonding during the COVID-19 pandemic: clarifying the role of parental symptoms of depression and aggressiveness. BMC Public Health. 2023;23:113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Shiva L, Desai G, Satyanarayana VA, Venkataram P, Chandra PS. Somatic Symptoms in the Postpartum Period and Their Association with Childbirth-related Post Traumatic Stress Disorder and Depression: A Cross-sectional Study. J Psychiatry Spectr. 2023;2:41–5. [Google Scholar]
- 40.Zacher M, Wollanka N, Sauer C, Haßtenteufel K, Wallwiener S, Wallwiener M, et al. Prenatal paternal depression, anxiety, and somatic symptom burden in different risk samples: an explorative study. Arch Gynecol Obstet. 2023;307:1255–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Scroggins JK, Ledbetter LS, Jones-Hepler B, Brandon D, Reuter-Rice K. Postpartum symptom clusters in birthing individuals: A systematic review. J Clin Nurs. 2023;32:4419–40. [DOI] [PubMed] [Google Scholar]
- 42.Howard LM, Khalifeh H. Perinatal mental health: a review of progress and challenges. World Psychiatry. 2020;19:313–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Junge C, Garthus-Niegel S, Slinning K, Polte C, Simonsen TB, Eberhard-Gran M. The Impact of Perinatal Depression on Children’s Social-Emotional Development: A Longitudinal Study. Matern Child Health J. 2017;21:607–15. [DOI] [PubMed] [Google Scholar]
- 44.Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. Lancet. 2014;384:1800–19. [DOI] [PubMed] [Google Scholar]
- 45.Bilodeau J, Quesnel-Vallée A, Poder T. Work stressors, work-family conflict, parents’ depressive symptoms and perceived parental concern for their children’s mental health during COVID-19 in Canada: a cross-sectional analysis. BMC Public Health. 2023;23:2181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Souza JP, Day LT, Rezende-Gomes AC, Zhang J, Mori R, Baguiya A, et al. A global analysis of the determinants of maternal health and transitions in maternal mortality. Lancet Glob Health. 2024;12:e306–16. [DOI] [PubMed] [Google Scholar]
- 47.Guintivano J, Manuck T, Meltzer-Brody S. Predictors of Postpartum Depression: A Comprehensive Review of the Last Decade of Evidence. Clin Obstet Gynecol. 2018;61:591–603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Furtado M, Chow CHT, Owais S, Frey BN, Van Lieshout RJ. Risk factors of new onset anxiety and anxiety exacerbation in the perinatal period: A systematic review and meta-analysis. J Affect Disord. 2018;238:626–35. [DOI] [PubMed] [Google Scholar]
- 49.Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and Health Predictors of National Postpartum Depression Prevalence: A Systematic Review, Meta-analysis, and Meta-Regression of 291 Studies from 56 Countries. Front Psychiatry. 2018;8:248. [DOI] [PMC free article] [PubMed]
- 50.Reid KM, Taylor MG. Stress and Maternal Postpartum Depression: The Importance of Stress Type and Timing. Popul Res Policy Rev. 2015;34:851–75. [Google Scholar]
- 51.Ko JY, Rockhill KM, Tong VT, Morrow B, Farr SL. Trends in Postpartum Depressive Symptoms - 27 States, 2004, 2008, and 2012. MMWR Morb Mortal Wkly Rep. 2017;66:153–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stansfeld S, Candy B. Psychosocial work environment and mental health–a meta-analytic review. Scand J Work Environ Health. 2006;32:443–62. [DOI] [PubMed] [Google Scholar]
- 53.Jaramillo NR, Trillos CE, Julià M. The measure of precarious employment and its impact on the mental health of workers: A systematic review 2007–2020. Work. 2022;73:639–50. [DOI] [PubMed] [Google Scholar]
- 54.Utzet M, Valero E, Mosquera I, Martin U. Employment precariousness and mental health, understanding a complex reality: a systematic review. Int J Occup Med Environ Health. 2020;33:569–98. [DOI] [PubMed] [Google Scholar]
- 55.Irvine A, Rose N. How Does Precarious Employment Affect Mental Health? A Scoping Review and Thematic Synthesis of Qualitative Evidence from Western Economies. Work Employment Soc. 2024;38:418–41. [Google Scholar]
- 56.Julià M, Méndez-Rivero F, Gómez-Gómez Á, Pozo ÓJ, Bolíbar M. Association between Precarious Employment and Chronic Stress: Effect of Gender, Stress Measurement and Precariousness Dimensions—A Cross-Sectional Study. Int J Environ Res Public Health. 2022;19:9099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kress V, von Soest T, Kopp M, Wimberger P, Garthus-Niegel S. Differential predictors of birth-related posttraumatic stress disorder symptoms in mothers and fathers - A longitudinal cohort study. J Affect Disord. 2021;292:121–30. [DOI] [PubMed] [Google Scholar]
- 58.Loughman A, Hedley J, Olsson CA, Berk M, Moylan S, Saffery R, et al. Increased maternal mental health burden in a representative longitudinal community cohort coinciding with COVID-19 lockdown. Aust J Psychol. 2021;73:578–85. [Google Scholar]
- 59.Montgomery SC, Short JR, Ledermann T, Kimmes JG, Longley KE, Manhiri E, et al. Work and Family Transitions Throughout Adulthood and the Impact on Health: A Systematic Review. J Popul Ageing. 2023;16:519–64. [Google Scholar]
- 60.Rocheleau CM, Bertke SJ, Lawson CC, Romitti PA, Desrosiers TA, Agopian AJ, et al. Factors associated with employment status before and during pregnancy: Implications for studies of pregnancy outcomes. Am J Ind Med. 2017;60:329–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.OECD. PF2.1. Parental leave systems. 2024. https://www.oecd.org/content/dam/oecd/en/data/datasets/family-database/pf2_1_parental_leave_systems.pdf. Accessed 21 Aug 2024.
- 62.Vigoureux S, Lorthe E, Blondel B, Ringa V, Saurel-Cubizolles MJ. Women’s occupational status during pregnancy and preventive behaviour and health outcomes between 1998 and 2016 in France. J Gynecol Obstet Hum Reprod. 2023;52: 102545. [DOI] [PubMed] [Google Scholar]
- 63.OECD. PF2.2: Parents’ use of childbirth-related leave. 2022. https://www.oecd.org/content/dam/oecd/en/data/datasets/family-database/pf2-2-use-childbirth-leave.pdf. Accessed 20 Aug 2024.
- 64.Hobfoll SE. Conservation of resources: A new attempt at conceptualizing stress. Am Psychol. 1989;44:513–24. [DOI] [PubMed] [Google Scholar]
- 65.Vander Elst T, Richter A, Sverke M, Näswall K, De Cuyper N, De Witte H. Threat of losing valued job features: The role of perceived control in mediating the effect of qualitative job insecurity on job strain and psychological withdrawal. Work Stress. 2014;28:143–64. [Google Scholar]
- 66.Thompson MJ, Carlson DS, Hackney K, Vogel RM. Vicarious abusive supervision and turnover in expectant working mothers: Does financial dependency trigger emotional disconnect? J Organ Behav. 2022;43:448–64. [Google Scholar]
- 67.Diener E, Thapa S, Tay L. Positive Emotions at Work. Annu Rev Organ Psychol Organ Behav. 2020;7:451–77. [Google Scholar]
- 68.Hobfoll SE, Halbesleben J, Neveu J-P, Westman M. Conservation of Resources in the Organizational Context: The Reality of Resources and Their Consequences. Annu Rev Organ Psychol Organ Behav. 2018;5:103–28. [Google Scholar]
- 69.McCardel RE, Loedding EH, Padilla HM. Examining the Relationship Between Return to Work After Giving Birth and Maternal Mental Health: A Systematic Review. Matern Child Health J. 2022;26:1917–43. [DOI] [PubMed] [Google Scholar]
- 70.Karl M, Schaber R, Kress V, Kopp M, Martini J, Weidner K, et al. Precarious working conditions and psychosocial work stress act as a risk factor for symptoms of postpartum depression during maternity leave: results from a longitudinal cohort study. BMC Public Health. 2020;20:1505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hackney KJ, Daniels SR, Paustian-Underdahl SC, Perrewé PL, Mandeville A, Eaton AA. Examining the effects of perceived pregnancy discrimination on mother and baby health. J Appl Psychol. 2021;106:774–83. [DOI] [PubMed] [Google Scholar]
- 72.Giallo R, D’Esposito F, Cooklin A, Mensah F, Lucas N, Wade C, et al. Psychosocial risk factors associated with fathers’ mental health in the postnatal period: results from a population-based study. Soc Psychiatry Psychiatr Epidemiol. 2013;48:563–73. [DOI] [PubMed] [Google Scholar]
- 73.Martinko MJ, Harvey P, Brees JR, Mackey J. A review of abusive supervision research. J Organ Behav. 2013;34:S120–37. [Google Scholar]
- 74.Tepper B. Abusive Supervision in Work Organizations: Review, Synthesis, and Research Agenda. J Manag. 2007;33:261–89. [Google Scholar]
- 75.Cheng GH-L, Chan DK-S. Who Suffers More from Job Insecurity? A Meta-Analytic Review Appl Psychol. 2008;57:272–303. [Google Scholar]
- 76.De Witte H, Pienaar J, De Cuyper N. Review of 30 Years of Longitudinal Studies on the Association Between Job Insecurity and Health and Well-Being: Is There Causal Evidence? Aust Psychol. 2016;51:18–31. [Google Scholar]
- 77.Blom V, Richter A, Hallsten L, Svedberg P. The associations between job insecurity, depressive symptoms and burnout: The role of performance-based self-esteem. Econ Ind Democr. 2018;39:48–63. [Google Scholar]
- 78.Marchand A, Durand P, Haines V, Harvey S. The multilevel determinants of workers’ mental health: results from the SALVEO study. Soc Psychiatry Psychiatr Epidemiol. 2015;50:445–59. [DOI] [PubMed] [Google Scholar]
- 79.Roelen CAM, Schreuder KJ, Koopmans PC, Groothoff JW. Perceived job demands relate to self-reported health complaints. Occup Med. 2007;58:58–63. [DOI] [PubMed] [Google Scholar]
- 80.Boya FO, Demiral Y, Ergör A, Akvardar Y, De Witte H. Effects of perceived job insecurity on perceived anxiety and depression in nurses. Ind Health. 2008;46:613–9. [DOI] [PubMed] [Google Scholar]
- 81.Perry-Jenkins M, Smith JZ, Goldberg AE, Logan J. Working-Class Jobs and New Parents’ Mental Health. J Marriage Fam. 2011;73:1117–32. [Google Scholar]
- 82.Schwab-Reese LM, Ramirez M, Ashida S, Peek-Asa C. Psychosocial employment characteristics and postpartum maternal mental health symptoms. Am J Ind Med. 2017;60:109–20. [DOI] [PubMed] [Google Scholar]
- 83.Cooklin AR, Canterford L, Strazdins L, Nicholson JM. Employment conditions and maternal postpartum mental health: results from the Longitudinal Study of Australian Children. Arch Womens Ment Health. 2011;14:217–25. [DOI] [PubMed] [Google Scholar]
- 84.Strazdins L, Shipley M, Broom D. What Does Family-Friendly Really Mean? Wellbeing, Time, and the Quality of Parents' Job. Aust Bull Labour. 2007;33:202–25.
- 85.Cooklin AR, Giallo R, Strazdins L, Martin A, Leach LS, Nicholson JM. What matters for working fathers? Job characteristics, work-family conflict and enrichment, and fathers’ postpartum mental health in an Australian cohort. Soc Sci Med. 2015;146:214–22. [DOI] [PubMed] [Google Scholar]
- 86.Kinser PA, Jallo N, Amstadter AB, Thacker LR, Jones E, Moyer S, et al. Depression, Anxiety, Resilience, and Coping: The Experience of Pregnant and New Mothers During the First Few Months of the COVID-19 Pandemic. J Womens Health (Larchmt). 2021;30:654–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Dagher RK, McGovern PM, Alexander BH, Dowd BE, Ukestad LK, McCaffrey DJ. The Psychosocial Work Environment and Maternal Postpartum Depression. Int J Behav Med. 2009;16:339–46. [DOI] [PubMed] [Google Scholar]
- 88.Goldberg AE, Smith JZ. Work Conditions and Mental Health in Lesbian and Gay Dual-Earner Parents. Fam Relat. 2013;62:727–40. [Google Scholar]
- 89.Clayborne ZM, Colman I, Kingsbury M, Torvik FA, Gustavson K, Nilsen W. Prenatal work stress is associated with prenatal and postnatal depression and anxiety: Findings from the Norwegian Mother, Father and Child Cohort Study (MoBa). J Affect Disord. 2022;298:548–54. [DOI] [PubMed] [Google Scholar]
- 90.Herman RJ, Perry-Jenkins M. Low-wage Work Conditions and Mother-Infant Interaction Quality Across the Transition to Parenthood. J Child Fam Stud. 2020;29:3552–64. [Google Scholar]
- 91.Dagher RK, McGovern PM, Dowd BE, Lundberg U. Postpartum depressive symptoms and the combined load of paid and unpaid work: a longitudinal analysis. Int Arch Occup Environ Health. 2011;84:735–43. [DOI] [PubMed] [Google Scholar]
- 92.McGovern P, Dagher RK, Rice HR, Gjerdingen D, Dowd B, Ukestad LK, et al. A longitudinal analysis of total workload and women’s health after childbirth. J Occup Environ Med. 2011;53:497–505. [DOI] [PubMed] [Google Scholar]
- 93.Fisher SD, Cobo J, Figueiredo B, Fletcher R, Garfield CF, Hanley J, et al. Expanding the international conversation with fathers’ mental health: toward an era of inclusion in perinatal research and practice. Arch Womens Ment Health. 2021;24:841–8. [DOI] [PubMed] [Google Scholar]
- 94.Shorey S, Chan V. Paternal mental health during the perinatal period: A qualitative systematic review. J Adv Nurs. 2020;76:1307–19. [DOI] [PubMed] [Google Scholar]
- 95.Howat A, Masterson C, Darwin Z. Non-birthing mothers’ experiences of perinatal anxiety and depression: Understanding the perspectives of the non-birthing mothers in female same-sex parented families. Midwifery. 2023;120: 103650. [DOI] [PubMed] [Google Scholar]
- 96.Garthus-Niegel S, Kittel-Schneider S. Väter und peripartale psychische Erkrankungen: Das übersehene Elternteil? Nervenarzt. 2023;94:779–85. [DOI] [PubMed] [Google Scholar]
- 97.Garthus-Niegel S, Radoš SN, Horsch A. Perinatal Depression and Beyond—Implications for Research Design and Clinical Management. JAMA Network Open. 2022;5:e2218978-e. [DOI] [PubMed] [Google Scholar]
- 98.Schaber R, Simm J, Patella T, Garthus-Niegel S. Practicable strategies parents can apply in their daily routine to successfully implement the 50/50-split-model of paid work, childcare, and housework: a qualitative content analysis. BMC Public Health. 2024;24:2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Rönnblad T, Grönholm E, Jonsson J, Koranyi I, Orellana C, Kreshpaj B, et al. Precarious employment and mental health: a systematic review and meta-analysis of longitudinal studies. Scand J Work Environ Health. 2019;45:429–43. [DOI] [PubMed] [Google Scholar]
- 100.Shields M, Dimov S, Kavanagh A, Milner A, Spittal MJ, King TL. How do employment conditions and psychosocial workplace exposures impact the mental health of young workers? A systematic review. Soc Psychiatry Psychiatr Epidemiol. 2021;56:1147–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Theorell T, Hammarström A, Aronsson G, Träskman Bendz L, Grape T, Hogstedt C, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health. 2015;15:738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Rugulies R, Aust B, Madsen IEH. Effort–reward imbalance at work and risk of depressive disorders. A systematic review and meta-analysis of prospective cohort studies. Scand J Work Environ Health. 2017;43:294–306. [DOI] [PubMed]
- 103.Madsen IEH, Nyberg ST, Magnusson Hanson LL, Ferrie JE, Ahola K, Alfredsson L, et al. Job strain as a risk factor for clinical depression: systematic review and meta-analysis with additional individual participant data. Psychol Med. 2017;47:1342–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Cramarenco RE, Burcă-Voicu MI, Dabija DC. The impact of artificial intelligence (AI) on employees’ skills and well-being in global labor markets: A systematic review. Oecon Copernic. 2023;14:731–67. [Google Scholar]
- 105.Elsamani Y, Kajikawa Y. How teleworking adoption is changing the labor market and workforce dynamics? PLoS ONE. 2024;19: e0299051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Figueiredo E, Margaça C, Hernández-Sánchez B, Sánchez-García JC. Teleworking Effects on Mental Health—A Systematic Review and a Research Agenda. Int J Environ Res Public Health. 2024;21:243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Sattler KMP, Prickett KC, Crosnoe R. Mothers’ work conditions, income, and parenting of young children. Fam Relat. 2024;73:1159–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Kress V, Steudte-Schmiedgen S, Kopp M, Förster A, Altus C, Schier C, et al. The Impact of Parental Role Distributions, Work Participation, and Stress Factors on Family Health-Related Outcomes: Study Protocol of the Prospective Multi-Method Cohort “Dresden Study on Parenting, Work, and Mental Health” (DREAM). Front Psychol. 2019;10:1273. [DOI] [PMC free article] [PubMed]
- 109.BMFSJ. Guide to Maternity Protection. 2021. https://www.bmfsfj.de/bmfsfj/meta/en/publications-en/guide-to-maternity-protection-191578. Accessed 11 July 2024.
- 110.Vives A, González F, Moncada S, Llorens C, Benach J. Measuring precarious employment in times of crisis: the revised Employment Precariousness Scale (EPRES) in Spain. Gac Sanit. 2015;29:379–82. [DOI] [PubMed] [Google Scholar]
- 111.Karl M, Staudt A, Vives A, Kopp M, Weise V, Mack JT, et al. Validation of the Employment Precariousness Scale and its associations with mental health outcomes: results from a prospective community-based study of pregnant women and their partners in Dresden. Germany BMJ Open. 2024;14: e077206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Jonsson J, Vives A, Benach J, Kjellberg K, Selander J, Johansson G, et al. Measuring precarious employment in Sweden: translation, adaptation and psychometric properties of the Employment Precariousness Scale (EPRES). BMJ Open. 2019;9: e029577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Vives A, Amable M, Ferrer M, Moncada S, Llorens C, Muntaner C, et al. The Employment Precariousness Scale (EPRES): psychometric properties of a new tool for epidemiological studies among waged and salaried workers. Occup Environ Med. 2010;67:548–55. [DOI] [PubMed] [Google Scholar]
- 114.Rödel A, Siegrist J, Hessel A, Brähler E. Fragebogen zur Messung beruflicher Gratifikationskrisen: Psychometrische Testung an einer repräsentativen deutschen Stichprobe [Psychometric Test of the Questionnaire Measuring Effort-Reward Imbalance at Work in a Representative German Sample.]. J Individ Differ. 2004;25:227–38. [Google Scholar]
- 115.Siegrist J, Wege N, Pühlhofer F, Wahrendorf M. A short generic measure of work stress in the era of globalization: effort–reward imbalance. Int Arch Occup Environ Health. 2009;82:1005–13. [DOI] [PubMed] [Google Scholar]
- 116.Magee CA, Stefanic N, Caputi P, Iverson DC. The association between job demands/control and health in employed parents: The mediating role of work-to-family interference and enhancement. J Occup Health Psychol. 2012;17:196–205. [DOI] [PubMed] [Google Scholar]
- 117.Eisinga R, Grotenhuis Mt, Pelzer B. The reliability of a two-item scale: Pearson, Cronbach, or Spearman-Brown? Int J Public Health. 2013;58:637–42. [DOI] [PubMed]
- 118.Bergant AM, Nguyen T, Heim K, Ulmer H, Dapunt O. Deutschsprachige Fassung und Validierung der “Edinburgh postpartum depression scale” [German validation of the Edinburgh Postpartum Depression Scale]. Deut Med Wochenschr. 1998;123:35–40. [DOI] [PubMed] [Google Scholar]
- 119.Park S-H, Kim J-I. Predictive validity of the Edinburgh postnatal depression scale and other tools for screening depression in pregnant and postpartum women: a systematic review and meta-analysis. Arch Gynecol Obstet. 2023;307:1331–45. [DOI] [PubMed] [Google Scholar]
- 120.Cockshaw WD, Thorpe KJ, Giannotti M, Hazell-Raine K. Factor structure of the Edinburgh Postnatal Depression Scale in a large population-based sample of fathers. J Affect Disord. 2023;340:167–73. [DOI] [PubMed] [Google Scholar]
- 121.Berg RC, Solberg BL, Glavin K, Olsvold N. Instruments to Identify Symptoms of Paternal Depression During Pregnancy and the First Postpartum Year: A Systematic Scoping Review. Am J Mens Health. 2022;16:15579883221114984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Franke GH. Die Symptom-Checkliste von Derogatis (SCL-90-R) - Deutsche Version - Manual. 2., vollst. überarbeitete Auflage. Göttingen: Beltz Test GmbH; 2002.
- 123.Krause G. The German National Cohort: aims, study design and organization. Eur J Epidemiol. 2014;29:371–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gloster AT, Lamnisos D, Lubenko J, Presti G, Squatrito V, Constantinou M, et al. Impact of COVID-19 pandemic on mental health: An international study. PLoS ONE. 2021;15: e0244809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Wall S, Dempsey M. The effect of COVID-19 lockdowns on women’s perinatal mental health: a systematic review. Women Birth. 2023;36:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.IBM Corp. IBM SPSS Statistics for Windows, Version 27.0. Armonk, NY; 2020.
- 127.Yan Q, Chen J, De Strycker L. An Outlier Detection Method Based on Mahalanobis Distance for Source Localization. Sensors. 2018;18:2186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Statistisches Landesamt Sachsen. Mikrozensusergebnisse: Bevölkerung nach Schulabschluss und Berufsabschluss. 2019. https://www.dresden.de/media/pdf/statistik/Statistik_1601_Ausbildung_Mikrozensus.pdf. Accessed 7 Aug 2024.
- 129.Landeshauptstadt Dresden. Bevölkerungsbestand—Bevölkerungsentwicklung. 2023. https://www.dresden.de/media/pdf/statistik/Statistik_1201_11_E2012-1981-Melderegister.pdf. Accessed 7 Aug 2024.
- 130.Pulford A, Thapa A, Thomson RM, Guilding A, Green MJ, Leyland A, et al. Does persistent precarious employment affect health outcomes among working age adults? A systematic review and meta-analysis. J Epidemiol Community Health. 2022;76:909–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Fischer T, Tian AW, Lee A, Hughes DJ. Abusive supervision: A systematic review and fundamental rethink. Leadersh Q. 2021;32: 101540. [Google Scholar]
- 132.Mackey JD, Frieder RE, Brees JR, Martinko MJ. Abusive Supervision: A Meta-Analysis and Empirical Review. J Manag. 2017;43:1940–65. [Google Scholar]
- 133.Peng AC, Schaubroeck J, Chong S, Li Y. Discrete emotions linking abusive supervision to employee intention and behavior. Pers Psychol. 2019;72:393–419. [Google Scholar]
- 134.Chum A, Kaur S, Teo C, Nielsen A, Muntaner C, O’Campo P. The impact of changes in job security on mental health across gender and family responsibility: evidence from the UK Household Longitudinal Study. Soc Psychiatry Psychiatr Epidemiol. 2022;57:25–36. [DOI] [PubMed] [Google Scholar]
- 135.Minnotte KL. Extending the Job Demands-Resources Model: Predicting Perceived Parental Success Among Dual-Earners. J Fam Issues. 2016;37:416–40. [Google Scholar]
- 136.Gerich J, Weber C. The Ambivalent Appraisal of Job Demands and the Moderating Role of Job Control and Social Support for Burnout and Job Satisfaction. Soc Indic Res. 2020;148:251–80. [Google Scholar]
- 137.Dawson KM, O’Brien KE, Beehr TA. The role of hindrance stressors in the job demand–control–support model of occupational stress: A proposed theory revision. J Organ Behav. 2016;37:397–415. [Google Scholar]
- 138.Gerich J. The relevance of challenge and hindrance appraisals of working conditions for employees’ health. Int J Stress Manage. 2017;24:270–92. [Google Scholar]
- 139.Schieman S, Plickert G. How Knowledge is Power: Education and the Sense of Control. Soc Forces. 2008;87:153–83. [Google Scholar]
- 140.Wysocki AC, Lawson KM, Rhemtulla M. Statistical Control Requires Causal Justification. Adv Methods Pract Psychol Sci. 2022;5:25152459221095824. [Google Scholar]
- 141.Brehm U, Huebner M, Schmitz S. 15 Jahre Elterngeld: Erfolge, aber noch Hanldungsbedarf. Ein Blick auf partnerschaftliche Arbeitsteilung und Karrieren. Bevölkerungsforschung aktuell. 2022;6:3–7.
- 142.Sohn M, Choi M, Jung M. Working conditions, psychosocial environmental factors, and depressive symptoms among wage workers in South Korea. Int J Occup Environ Health. 2016;22:209–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.de Breij S, Huisman M, Boot CRL, Deeg DJH. Sex and gender differences in depressive symptoms in older workers: the role of working conditions. BMC Public Health. 2022;22:1023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Thiel F, Pittelkow M-M, Wittchen H-U. Garthus-Niegel S. A Systematic Review and Meta-Analysis. Front Psychiatry: The Relationship Between Paternal and Maternal Depression During the Perinatal Period; 2020. p. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Penna AL, Aquino CM de, Pinheiro MSN, do Nascimento RLF, Farias-Antúnez S, Araújo DABS, et al. Impact of the COVID-19 pandemic on maternal mental health, early childhood development, and parental practices: a global scoping review. BMC Public Health. 2023;23:388. [DOI] [PMC free article] [PubMed]
- 146.Macmillan R, Shanahan MJ. Explaining the Occupational Structure of Depressive Symptoms: Precarious Work and Social Marginality across European Countries. J Health Soc Behav. 2022;63:446–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Schofer E, Ramirez FO, Meyer JW. The Societal Consequences of Higher Education. Sociol Educ. 2021;94:1–19. [Google Scholar]
- 148.Nigam J, Barker R, Cunningham T, Swanson N, LC C. Vital Signs: Health Worker–Perceived Working Conditions and Symptoms of Poor Mental Health — Quality of Worklife Survey, United States, 2018–2022. Weekly Report 2023. 2023;72:1197–205. [DOI] [PMC free article] [PubMed]
- 149.Suto M, Balogun OO, Dhungel B, Kato T, Takehara K. Effectiveness of Workplace Interventions for Improving Working Conditions on the Health and Wellbeing of Fathers or Parents: A Systematic Review. Int J Environ Res Public Health. 2022;19:4779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Niedhammer I, Lesuffleur T, Coutrot T, Chastang J-F. Contribution of working conditions to occupational inequalities in depressive symptoms: results from the national French SUMER survey. Int Arch Occup Environ Health. 2016;89:1025–37. [DOI] [PubMed] [Google Scholar]
- 151.Liu CH, Tronick E. Re-conceptualising Prenatal Life Stressors in Predicting Post-partum Depression: Cumulative-, Specific-, and Domain-specific Approaches to Calculating Risk. Paediatr Perinat Epidemiol. 2013;27:481–90. [DOI] [PubMed] [Google Scholar]
- 152.Bergunde L, Rihm L, Lange LS, Darwin Z, Iles J, Garthus-Niegel S. Family mental health research – the importance of adopting a family lens in the perinatal period and beyond. J Reprod Infant Psychol. 2024;42:565–8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The dataset presented in this article is not publicly available because of legal and ethical constraints. Public sharing of participant data was not included in the informed consent of the study. Requests to access the datasets should be directed to the project manager and principal investigator Susan Garthus-Niegel.