Abstract
Background
Cholera is an acute, severe, illness caused by infection with Vibrio cholerae. Cholera outbreaks are closely linked to armed conflicts and humanitarian emergencies. This study describes the cholera outbreak amidst conflict in Gadaref state, discusses the possible factors mediated its spread and proposes future improvements in preparedness and response measures.
Methods
A retrospective analytical study was conducted using national surveillance records of cholera cases, supported by interviews with key informants involved in preparedness and response, along with a review of state reports, to identify possible factors contributing to the spread and to evaluate the response.
Result
The outbreak was confirmed after the isolation of Vibrio cholerae of O1 serotype, with both Inaba and Ogawa serogroups. A total of 2,047 cholera cases records reviewed. The mean age was 16.8 (SD, 15.8) with an equal gender distribution. The case fatality ratio was 2.4% and the overall attack (AR) rate was 7.38 cases per 10,000 population, with the highest in Medeinat Gadaref locality (21.07/10,000). Interviews and reports review suggest that the outbreak was likely imported to villages near Ethiopian border before spreading to other parts of Gadaref. Atbara seasonal river, was the identified source of infection at the beginning. A disrupted health system due to conflict, delays in response teams’ deployment, and late implementation of control measures were identified as factors contributing to response delay and expansion of the outbreak. Oral cholera vaccine campaign was implemented in five localities, followed by an observable decline in cases.
Conclusion
Cholera remains a recurrent risk that has been further exacerbated by the armed conflict. The reporting of index cases from a border village highlights the need to strengthen surveillance at points of entry. Investment in case management and risk communication is necessary to improve clinical outcomes. The use of Oral Cholera Vaccine was associated with a decline in cases; however, further field studies are recommended to analyze its actual contribution in limiting the outbreak. The government’s primary role in leading and financing preparedness and response interventions has been limited by the conflict, urging investment in community-led interventions, while moving to more strategic outbreak preparedness and response financing mechanisms remains a priority, with partner support being essential in conflict settings.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12889-025-22128-1.
Keywords: Cholera outbreak, Surveillance, Sudan armed conflict, Oral cholera vaccine
Background
Cholera is an acute, severe, and sometimes lethal diarrheal illness that has affected almost the whole world through several outbreaks. It is caused by infection with Vibrio cholerae, a Gram-negative curved bacterium of the small intestine [1]. If left untreated, cholera is associated with very high mortality within a short period of time due to severe dehydration [2]. The actual global burden of cholera is largely unknown as the majority of cases remain unreported. As indicated by the World Health Organization (WHO), only 5–10% of cases occurring annually are officially reported, however, this is still enough to cause considerable mortality [3]. The underreporting of the disease is explained by several factors including the limited capacity of epidemiological services and laboratories, as well as the economic, social, and political discouragement of reporting [4].
The world has experienced several cholera pandemics since the early 19th century with the last one occurring in the late 20th century with both serotypes O1 and O139 identified as responsible, however, the O1 serotype is more strongly linked to these pandemics [5]. Many factors like poverty, poor sanitation, limited access to safe water and collapsed infrastructure are well known to play key role in cholera outbreaks [6–8].
Sudan has experienced many outbreaks during the past 10 years, according to the Federal Ministry of Health (FMOH) records, an outbreak led to 15,000 cases and 279 deaths in 2016, affecting many states in different regions in Sudan [9]. Consequently, in 2017, a traditional gold mining center for many Sudanese people with poor environmental and water sanitation witnessed an outbreak in Northern State. From the 7th to the 36th epidemiological week, the total number of cases reported was 957 with a case fatality ratio (CFR) of 1.9% [10]. The last outbreak reported in Sudan was in 2019, affecting both Sennar and Blue Nile states and causing high mortality with CFR of 4% in Blue Nile and 2.3% in Sennar [11]. During this last outbreak the Oral Cholera Vaccine (OCV) was used for the first time as one of the interventions. The OCV was effective in controlling the outbreak and preventing its expansion as concluded by Mohamed NS et al. [11].
On April 15, 2023, the Sudan armed conflict started causing disruptions in health system across all Sudan states and leading to large displacement. The number of internally displaced persons (IDPs) is estimated to have reached 10 million. Such a humanitarian emergency is associated with poor shelter, decreased water quality, inadequate sanitation and massive population movement, all of which facilitate the emergence and rapid spread of infectious diseases [12, 13]. More specifically, cholera outbreaks are strongly linked to armed conflicts and humanitarian emergencies [14–18]. Cholera outbreak was confirmed and declared in Gadaref state in late August 2023, four months after the armed conflict began. This placed the health authorities under high stress during a very critical time when resources were very limited and health partners were not yet settled.
This study describes the outbreak of cholera in Gadaref state, from August 2023 to January 2024 and discusses the possible factors that contributed to its spread while proposing future improvements in preparedness and response measures.
Methods
A retrospective case study of the cholera outbreak in Gadaref state, Sudan (from August 24, 2023, to January 1,2024).
Case definition: The Sudanese National and State-level epidemiological surveillance system defines a suspected cholera case as any patient aged 5 or older presenting with a sudden onset of watery diarrhea, without abdominal pain, with or without vomiting. The presence of severe dehydration or death from acute watery diarrhea increases the probability of cholera. A confirmed cholera case requires a suspected case with Vibrio cholerae isolated through culture or confirmed by RT-PCR. Rapid diagnostic tests were also used to support detection as confirmatory bacteriological testing conducted on a limited number of suspected cases at the outbreak’s beginning.
Reporting and data flow: Cases were reported from the lower levels—health facilities and communities—to the locality (district) level, where the locality Rapid Response Team (RRT) was deployed for the initial investigation of cases. The investigation covered the collection of full details on cases, contacts, the affected area, the possible source of infection, and the collection of environmental and stool samples for confirmation. The locality level reported to the state level, where validation was done and additional support was provided for investigation. The data then flowed up to the national level, where final validation and compilation done. The stool samples were transported to the National Public Health Laboratory (NPHL) for testing, and feedback on the results was immediately sent back to the lower levels. Environmental sampling, particularly drinking water sampling, is done by the RRT, and samples are tested at the state level at the Directorate of Environmental Health using the Total Coliform and E. coli microbiological test.
Study population: The study used the cholera cases records of Gadaref state, at the national level at the National Surveillance Directorate, in addition to the collection of qualitive data from selected key informants at the state and the national levels.
Inclusion and exclusion criteria: For the case records the study only included confirmed cholera cases records at the national level, validated and compiled at the National Surveillance Directorate. Records missing critical variables like dates, clinical features, and other important demographics were excluded. The key informants were selected purposively based on their direct links to surveillance and response activities during the outbreak. The study included 11 key informants: five from the national response team, four surveillance and response personnel at state level, and two WHO staff involved in the response activities at the state level.
Data collection: Data was collected through obtaining the cases line-list from the national surveillance system for case record analysis, which was done using Epi info 7 software. Cases were described by person, place and time using tables and charts. In addition, state reports were reviewed to identify the potential factors that facilitated the spread of the diseases. An in-depth interview guide was developed and included questions covering specific themes such as; the field investigation findings, the source of infection, potential spread factors, surveillance and reporting, timeliness of the response activities implementation, effect of the conflict on the response. The qualitative data was transcribed into text and analyzed with thematic analysis.
The map demonstrating the geographical distribution of the outbreak, was created using the ArcGIS (Geographical Information System) software.
Ethical approval
was provided by the National Health Emergencies and Epidemic Control General Directorate (HEEC) at Federal Ministry of Health (FMOH). Data from the line-list was used after the removal of personal information like names and contact numbers for each patient’s record.
Results
Outbreak confirmation
The outbreak was declared after the confirmation of the diagnosis through the isolation of the organism, as 66 rectal specimens were cultured, with 22 (36%) of them showing growth of Vibrio Cholerae. The identified serotype was O1 with both Inaba and Ogawa serogroups. The outbreak was confirmed on 28th August 2023, and cases continued to be reported based on the standard case definition, epidemiological link, and rapid diagnostic test (RDT) results.
Epidemiological distribution of cases
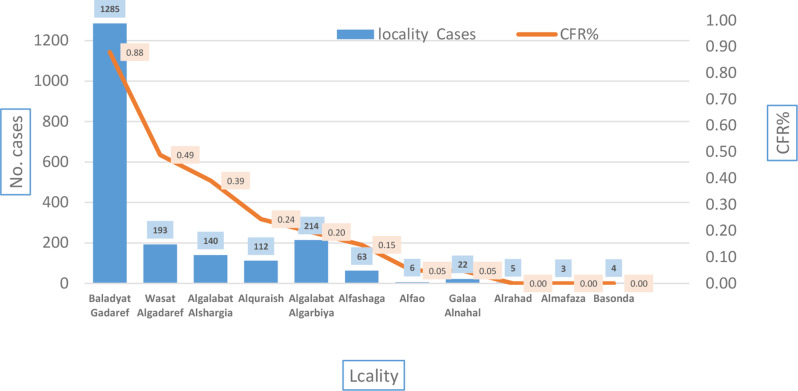
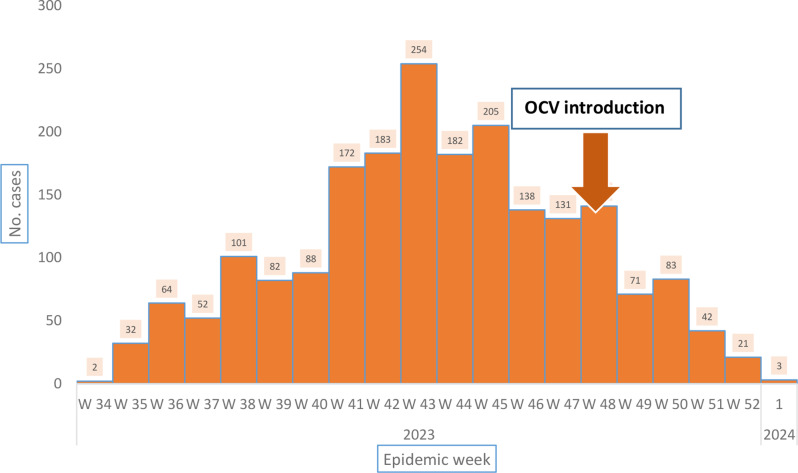
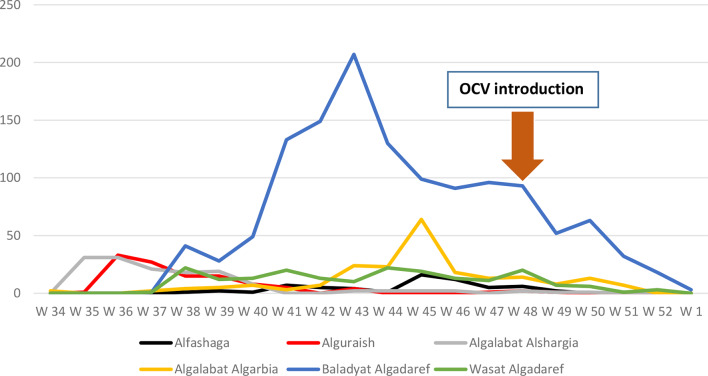
From a total of 2047 cholera cases reported from 28th Aug 2023 to 1st Jan 2024, 50.1% were females. The mean age was 16.8 years (SD 15.8), with 16.6% of cases aged below five years. Regarding patients’ occupation, 28.9% were housewives, 29.3% were unemployed, and only 0.5% were health workers (Table 1). All patients reported acute watery diarrhea; however, 63.4% developed dehydration. There were 50 reported deaths, with a case fatality ratio (CFR) of 2.4%. The overall attack rate (AR) was 7.38 cases per 10,000 population, with the highest AR in Baladyat Algadaref locality (another name, Medeinat Al Gadaref), reaching 21.07/10,000 (Table 2). In addition to reporting the highest number of cases, Baladyat Algadaref locality also had the highest CFR (Fig. 2). The outbreak peaked in epidemic week 43, with the number of reported cases reached 254, and then began to gradually decline in the following weeks (Fig. 1). The direction of spread was from the eastern localities near the Ethiopian borders, starting from Algalabat Alshargia (first in Hilat Khatir village), followed by Alguraisha, then to Baladyat Algadaref, and later expanded to involve the other localities (Figs. 3 and 4). The CFR was highest in Baladyat Algadaref, which includes Algadaref city, the state capital (Fig. 3).
Table 1.
Distribution of cholera cases by person characteristics in Gadaref 2023. (n = 2047)
| Variable | Frequency | % | |
|---|---|---|---|
| Sex (n = 2047) | |||
| Male | 1021 | 49.9 | |
| Female | 1026 | 50.1 | |
| Age group (n = 2047) | |||
| < 5 | 340 | 16.6 | |
| 5–15 | 293 | 14.3 | |
| 15–30 | 544 | 26.5 | |
| 30–45 | 408 | 19.9 | |
| 45–60 | 207 | 10.1 | |
| 60&More | 255 | 12.4 | |
| Occupation (n = 2045) | |||
| Freelance | 313 | 15.3 | |
| Tea seller | 2 | 0.09 | |
| Tradesman | 27 | 1.3 | |
| Housewife | 590 | 28.8 | |
| Student | 307 | 15.0 | |
| Unemployed | 600 | 29.3 | |
| Farmer | 59 | 2.8 | |
| Teacher | 18 | 0.8 | |
| Gov. employee | 118 | 5.7 | |
| Health Worker | 11 | 0.5 | |
| Symptoms (n = 2047) | |||
| Watery diarrhea | 2047 | 100 | |
| Vomiting | 1473 | 71.9 | |
| Nausea | 183 | 8.9 | |
| Dehydration | 1093 | 53.3 | |
| Headache | 34 | 1.6 | |
| Fever | 41 | 2.0 | |
| Dehydration (n = 1723) | |||
| Yes | 1093 | 63.4 | |
| No | 630 | 36.5 | |
| Deaths (n = 2047) | |||
| Yes | 50 | 2.4 | |
Table 2.
Cholera attack rate per locality in Gadaref state for 10,000 population
| Locality | Attack rate/ 10,000 |
|---|---|
| Baladyat Algedaref | 21.07 |
| Al Galabat Al Gharbyah - Kassab | 10.87 |
| Wasat Al Gedaref | 7.38 |
| Al Qureisha | 6.80 |
| Galabat Ash-Shargiah | 5.39 |
| Al Fashaga | 4.75 |
| Gala’a Al Nahal | 1.54 |
| Basundah | 0.27 |
| Al Mafaza | 0.19 |
| Ar Rahad-GD | 0.17 |
| Al Fao | 0.16 |
| Overall state attack rate | 7.38 |
Fig. 2.
The case-load and case fatality rate per each affected locality in Gadaref state
Fig. 1.
Distribution of Cholera cases by epidemic week, Gadaref state, Aug 2023 - Jan 2024 (n = 2047)
Fig. 3.
Distribution of cholera cases and deaths by localities, Gadaref state, 2023–2024
Fig. 4.
Comparison of reported cases in the localities where oral vaccination campaign was implemented
Potential infection source and spread factors
From national and state RRT’s reports and interviews with key informants in the cholera outbreak response, the Ethiopia-bordering village was known for its regular population movement to and from Ethiopia. At the same time there were unofficial media reports of reported acute watery diarrhea (AWD) cases in Ethiopia. In addition, there was a lack of safe drinking water in the affected areas at the beginning of the outbreak. An interviewee stated: “they all use the seasonal river water, the Atbara River”. Water samples collected from the river revealed fecal contamination with uncountable thermotolerant coliform bacteria per 100 ml. This river is a common source of water for drinking, washing, bathing, and swimming for both humans and animals. The river valley was also used as an area for open defecation during dry seasons. A national response field member declared that “there was a delayed deployment of the state and national RRT, which led to delays in case investigation and implementation of control measures, as well as a delayed provision of supplies and technical support at the locality level, which resulted in improper case isolation and management”. These were factors that contributed to the disease’s spread to other villages and even localities. The delay was due to the health system disruption caused by the armed conflict and the insufficient resources to deploy RRT, including a lack of team incentives, transportation costs, and medical supplies, including infection control materials. These also contributed to the delay. The aforementioned factors weakened the role of active cases-finding, which contributed to under-reporting, as “Cases were reported mainly through routine passive surveillance,” said the national response leader. The conflict caused the local health system to collapse; government employees at health institutions ceased their work, healthcare services provision declined, transportation was challenging, and remote areas were difficult to reach. Additionally, there was a shortage of medical supplies. Furthermore, partners like non-governmental organizations (NGOs) were also affected by the conflict, as their systems and logistical mechanisms were disrupted.
Oral cholera vaccine (OCV) introduction
Sudan has received OCV, Euvichol-Plus, for the second time in history, as a reactive response strategy, to be distributed in cholera-affected states. Five localities were targeted in Gadaref state, with a total target population of 1,576,448. The vaccination campaign began in epidemiologic week 48 and lasted for 6 days in all targeted localities. Although the trend of the disease had already started to decline, a further, clearly observable decrease in the weekly reported cases was seen after the OCV campaign (Fig. 4). Two weeks after the campaign, only a few cases were reported in 2 localities, Baladyat Algadaref and Algalabat Algarbiya (Fig. 4).
Discussion
The cholera emerged at a time when the health system was under significant disruption and weakness due to the ongoing armed conflict. The outbreak started in Gadaref state in late August, with the first index cases reported in Hilat Khatir, a border village near Ethiopia. There was active border movement between the neighboring villages of both countries, with a high possibility that the disease was imported from outside the country. This was supported by the travel history of the cases and the recurrent outbreaks in Ethiopia, the last being in 2020, which all support the importation hypothesis [19]. This is not the first time that cholera has been imported from neighboring countries; an overwhelming outbreak in 2016 was imported from South Sudan and affected several states [20]. Strengthening surveillance at points of entry along the borders is highly recommended for early detection and prevention of its spread. As of 1st January 2024, the overall attack rate was 7.38/10,000, which is lower than the average attack rate of cholera during the 2017 outbreak in Sudan, which was 12/100,000 [10]. Cholera cases in this outbreak were mainly reported through routine passive surveillance, which might have contributed to the lower attack rate. Active case finding should be strengthened to address the underreporting issue. A considerable proportion (16.6%) of infections occurred among the under-five, which urges the need to revisit the standard case definition to avoid excluding under-five children. This aligns with the Yemen outbreak, which had a relatively high infection rate among children compared to other age groups [21]. The Crude CFR of this outbreak is significantly high exceeding what is recommended by the WHO as it should not pass 1% [3]. It is slightly higher than that reported in 2016 [9]; however, it is close to the CFR reported in Sennar (2.3%) in 2019, while in the same year, the CFR was 4% in Blue Nile state [22]. The high CFR could be attributed to poor case management and poor risk communication activities leading to delayed medical care-seeking. Intensive efforts should be focused on health promotion and risk communication. Regarding the presenting symptoms, all patients presented with acute watery diarrhea, and most of them had vomiting, while more than half had a degree of dehydration. These symptoms were typical of cholera as described in the standard case definition adopted by Ministry of Health (MoH), as recommended by the WHO [3].
According to the field investigation report, the first villages to be affected by the outbreak shared the same water source, Atbrara River, which was identified as the source of infection based on the biological testing of its water. This is a seasonal river (flowing only during rainy season, July – October) extending from the Ethiopian plateau and running through Gadaref state. In addition, during the dry season, the river bed is a common place for open defecation and waste disposal. The villages along the riverside had no safe water sources, and the communities there carried out all their daily activities in the river, including swimming, doing laundry, and even allowing animals to use the same water.
Additional factors such as the delays in RRTs deployment along with the delayed implementation of control measures, including proper case isolation and treatment were also key factors that contributed to the expansion of the outbreak. It is well documented that a delay in response to detected cholera cases leads to an enlargement of the outbreak size to the point where containment is very difficult [22]. Following the early detected cases in Algalabat Alshargia locality, the preparedness and prevention measures in the other cholera-free localities were very weak due to system disruption and lack of resources. The role of humanitarian partners is crucial to support MoH preparedness in risk areas and also to support field interventions and control measures in this complex context to achieve better response outcomes. It is the government responsibility to lead preparedness and response activities and to finance the interventions. However, in conflict settings where the health system is disrupted and the health authorities have lost significant resources and supplies, the role of partners is critical to support preparedness and response [23]. In addition, empowering local communities and investing in community-based solutions represent a sustainable and resilient approach to combating outbreaks.
OCV has proven its effectiveness in Sudan in 2019 [11]; however, the observation in this campaign needs to be supported by another field study to analyze its actual contribution to the overall outbreak control. Before the OCV campaign, the disease trend had already started to decline, which could be attributed to other interventions such as water and sanitation activities, improved community practices, or even the natural progression of the outbreak. A comprehensive response analysis is recommended for stronger evidence to inform future strategic direction. The current armed conflict poses several factors that are expected to contribute to the spread of cholera to other Sudan states. These include a disrupted health system, limited resources for preparedness and response, massive displacement, and open borders.
Limitations
Despite the important insights from real-ground experience that this study provides, there are still limitations in the design that prevent a more in-depth analysis of the situation, as could be achieved with other designs like a case-control study or implementation research. These are recommended alternatives that future researchers might consider. Additionally, the researchers were unable to reach and include frontline workers at the locality (district) level. Their reflections and field experiences could have enriched the results, strengthened the evidence, and widened the perspectives. This study is limited by potential confounding factors such as healthcare access, population movement, and hygiene practices, which may have influenced the outbreak dynamics and response effectiveness. Additionally, findings are specific to Gadaref state and may not be generalizable to regions with different healthcare infrastructures, conflict conditions, or environmental factors. Variability in surveillance data quality and possible underreporting also pose challenges in accurately estimating the true disease burden.
Conclusion
Cholera remains a recurrent risk that has been further exacerbated by the armed conflict. The reporting of index cases from a border village highlights the need to strengthen surveillance at points of entry. Significant mortality was caused by cholera, urging greater investment in case management and risk communication to improve clinical outcomes. The use of Oral Cholera Vaccine was associated with a decline in cases; however, further field studies are recommended to analyze its actual contribution in limiting the outbreak. The government’s primary role in leading and financing preparedness and response interventions has been limited by the conflict, urging investment in community-led interventions, while moving to more strategic outbreak preparedness and response financing mechanisms remains a priority, with partner support being essential in conflict settings.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Acknowledgements
We would like to thank all the staff at the HEEC general directorate for their facilitation along the process of data collection. Special thanks to Gadaref state MoH staff for their dedication in work and cooperation to provide the required support to document this experience.
Abbreviations
- AR
Attack Rate
- AWD
Acute Watery Diarrhea
- CFR
Case Fatality Ratio
- FMOH
Federal Ministry of Health
- HEEC
Health Emergencies and Epidemics Control
- IDPs
Internally Displaced Persons
- MoH
Ministry of Health
- NGOs
Non-governmental Organization
- OCV
Oral Cholera Vaccine
- RDT
Rapid Diagnostic Test
- RRT
Rapid Response Team
- WHO
World Health Organization
Author contributions
A.I.; conceptualization, methodology, A.I., HA., and M.Mg.; analysis and result formatting, AI and HE; GIS and mapping, M.A., K.E. and A.B.; resources, A.I., M.Mg. B.M. and S.F. development of the original draft, A.H.D., A.A., S.F., K.E., M.A., M.Mo., B.M. and EM; review and editing.
Funding
This research received no external funding.
Data availability
The data is available in data archive of HEEC, FMOH, Republic of Sudan and accessible by researchers upon request. For any queries or requests regarding data, contact Dr. Ahmad Izzoddeen, email: ahmadizzoddeen@gmail.com.
Declarations
Ethics approval and consent to participate
The study used retrospective data after obtaining the ethical approval from the Research Committee under the General Directorate of HEEC at FMOH. The Ethical approval reference number is (1.11.2.23). The signed document for the ethical approval was attached as a supplementary file. The need for the informed consent from participants has been waived by the Research Committee at HEEC, FMOH, and the data provided after removal of personal information (e.g. name and phone number).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare that they have no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Sack DA, Sack RB, Nair GB, Siddique AK, Cholera. Lancet. 2004;363(9404):223– 33. 10.1016/s0140-6736(03)15328-7. PMID: 14738797. [DOI] [PubMed]
- 2.KF Kiple, editor, The Cambridge world history of human disease, Cambridge University Press, Cambridge; 1993. pp. 642–9. [Google Scholar]
- 3.WHO. Cholera surveillance and number of cases. Geneva: World Health Organization; 2014. [Google Scholar]
- 4.Zuckerman JN, Rombo L, Fisch A. The true burden and risk of cholera: implications for prevention and control. Lancet Infect Dis. 2007;7(8):521– 30. 10.1016/S1473-3099(07)70138-X. PMID. [DOI] [PubMed]
- 5.Guerrant RL, Carneiro-Filho BA, Dillingham RA. Cholera, diarrhea, and oral rehydration therapy: triumph and indictment. Clin Infect Dis. 2003;37(3):398–405. 10.1086/376619. Epub 2003 Jul 22. PMID: 12884165. [DOI] [PubMed] [Google Scholar]
- 6.WHO. Children aged < 5 years stunted; Data by country 2018. Available from: http://apps.who.int/gho/data/node.main.CHILDSTUNTED?lang=en
- 7.WHO/UNICEF Joint Monitoring Programme for Water Supply SaH. Yemen 2018. Available from: https://washdata.org/data. Last Accessed 2018 Apr 24].
- 8.Baumann P, Furniss AL, Lee JV. Vibrio Bergey’s manual of systematic bacteriology Kreig N. R. and Holt J. G. 1 1984 518–38. The Williams & Wilkins Co. Baltimore, Md.
- 9.ACAPS, Briefing Note ACAPS. 2017. Jun 16. Last accessed on 2020 Jan 1. Available from: https://reliefweb.int/report/sudan/acaps-briefing-note-sudan-cholera-outbreak-16-june-2017
- 10.Alzain MA, Haruwn MH, Abdelaziz MO, Elsheikh M, Asweto CO, Algahtani FD, Adeboye AA, Elhassan NEE, Itumalla R. Association between cholera outbreak and traditional gold mining in Northern State, Sudan 2017. J Glob Infect Dis. 2021;13(3):115–9. 10.4103/jgid.jgid_47_20. PMID: 34703150; PMCID: PMC8491817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mohamed NS, Ali Y, Abdalrahman S, Ahmed A, Siddig EE. The use of cholera oral vaccine for containment of the 2019 disease outbreak in Sudan. Trans R Soc Trop Med Hyg. 2022;116(9):763–6. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed K, Bukhari MA, Altaf MD, Lugala PC, Popal GR, Abouzeid A, Lamunu M. Development and implementation of electronic disease early warning systems for optimal disease surveillance and response during humanitarian crisis and Ebola outbreak in Yemen, Somalia, Liberia and Pakistan. Online J Public Health Inf. 2019;11(2). [DOI] [PMC free article] [PubMed]
- 13.World Health Organization. Outbreak surveillance and response in humanitarian emergencies: WHO guidelines for EWARN implementation. World Health Organization; 2012.
- 14.Camacho A, Bouhenia M, Alyusfi R, Alkohlani A, Naji MAM, de Radigues X, Abubakar AM, Almoalmi A, Seguin C, Sagrado MJ, et al. Cholera epidemic in Yemen, 2016-18: an analysis of surveillance data. Lancet Glob Health. 2018;6(6):e680–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ingelbeen B, Hendrickx D, Miwanda B, van der Sande MAB, Mossoko M, Vochten H, Riems B, Nyakio JP, Vanlerberghe V, Lunguya O, et al. Recurrent cholera outbreaks, Democratic Republic of the congo, 2008–2017. Emerg Infect Dis. 2019;25(5):856–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lubogo M, Mohamed AM, Ali AH, Ali AH, Popal GR, Kiongo D, Bile KM, Malik M, Abubakar A. Oral cholera vaccination coverage in an acute emergency setting in Somalia, 2017. Vaccine. 2020;38(Suppl 1):A141–7. [DOI] [PubMed] [Google Scholar]
- 17.Lam E, Al-Tamimi W, Russell SP, Islam Butt MOU, Blanton C, Musani AS, Date K. First oral cholera vaccination campaign in Iraq during an outbreak and humanitarian crisis: findings from the coverage survey, 2015. Am J Trop Med Hyg. 2016;95(5):567. [Google Scholar]
- 18.Connolly MA, Gayer M, Ryan MJ, Salama P, Spiegel P, Heymann DL. Communicable diseases in complex emergencies: impact and challenges. Lancet. 2004;364(9449):1974–83. [DOI] [PubMed] [Google Scholar]
- 19.Letta TT, Belay DB, Ali EA. Determining factors associated with cholera disease in Ethiopia using bayesian hierarchical modeling. BMC Public Health. 2022;22(1):1779. 10.1186/s12889-022-14153-1. PMID: 36123680; PMCID: PMC9487065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alhussien SA, Hassan DM, Bashab HM, Mohammednour SA. Public health emergency: review on cholera preparedness and response Sudan, 2015. J Emerg Med Trauma Acute Care. 2016;2:97. [Google Scholar]
- 21.Dureab FA, Shibib K, Al-Yousufi R, Jahn A, Yemen. Cholera outbreak and the ongoing armed conflict. J Infect Dev Ctries. 2018;12(5):397–403. 10.3855/jidc.10129. PMID: 31865306. [DOI] [PubMed]
- 22.Ratnayake R, Finger F, Edmunds WJ, Checchi F. Early detection of cholera epidemics to support control in fragile States: Estimation of delays and potential epidemic sizes. BMC Med. 2020;18:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Spiegel P, Ratnayake R, Hellman N, Ververs M, Ngwa M, Wise PH, Lantagne D. Responding to epidemics in large-scale humanitarian crises: a case study of the cholera response in Yemen, 2016–2018. BMJ Global Health. 2019;4(4):e001709. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data is available in data archive of HEEC, FMOH, Republic of Sudan and accessible by researchers upon request. For any queries or requests regarding data, contact Dr. Ahmad Izzoddeen, email: ahmadizzoddeen@gmail.com.