Abstract
Background
Compared with short-term practices, long-term yoga might promote differential qualitative and quantitative outcomes. Following JBI’s and PRISMA-ScR guidelines, this scoping review followed an apriori and systematic protocol to document the long-term effects of yoga on neural, cognitive, psychological, and physiological outcomes, provide evidence maps for each yoga component, and summarize results identifying knowledge gaps and promising directions.
Methods
Four databases (PubMed, Cochrane, LILACS, and PubPsych) were last searched in March 2023. Studies were included if they evaluated adults with > 1 year of practice, specified yoga-based practice(s) of interest, measured neural, cognitive, psychological, and/or physiological outcomes, were written in English, Spanish, or Portuguese, presented original data, and mentioned search terms in the title/abstract. Evidence maps for each yoga component followed a 4-level structure of outcome category, method, study design and literature size. Qualitative summaries followed the same structure, to facilitate information retrieval.
Results
Out of 2270 screened studies, 65 were included (meditative studies = 36, predominantly postural studies = 25, breathing practice studies = 8). Physiologicaland neural outcomes were the most common, followed by psychological and cognitive outcomes. Although heterogeneous, neural results reveal structural and functional changes related to sensorimotor, interoceptive, emotion regulation, and executive functions. Physiologically, most studies have associated long-term practice with parasympathetic-driven autonomic, hormonal and immune responses, but some studies revealed sympathetic-driven or mixed responses, maybe due to the specific technique or individual differences. Psychological outcomes included lower levels of negative affect, psychopathological symptoms, and emotional reactivity. Cognitive measures have shown improved memory/cognition for older adults, but mixed or null effects for other constructs. Commonly, however, long-term practitioners demonstrated improved neural or physiological efficiency while performing cognitive tasks.
Conclusions
Future research should provide clear descriptions of the investigated yoga practice, employ more experimental paradigms, and refine statistical reports and models. We encourage researchers to work with specific overarching theoretical frameworks to refine research predictions, such as the neurovisceral integration model or predictive coding models; to consider motivational, cultural, and contextual factors that might influence long-term outcomes; and to develop systematic reviews and meta-analyses as next steps of evidence summary.
Keywords: Yoga, Long-term, Experience, Expertise, Scoping review
Background
Historically, yoga philosophy and practices emerged from heterogeneous oral lineages and texts. Most of them framed yoga as a goal achieved by meditative and psychophysical efforts, such as stilling mental fluctuations, experiencing nondual states, or bonding with a chosen deity [1, 2]. Modern yoga-based practices represent a long process of transnational intercultural exchange, traversing colonialist, traditionalist, and secularist pressures [3–5]. They are usually delivered as postural, breathing, and/or meditation practices, with associated neurocognitive, psychological, and physiological effects [6–9]. While yoga-based practices can be delivered in somewhat standardized formats, there are schools and approaches that prioritize individualized deliveries. Commonly, practitioners also incorporate ethical, philosophical or religious prescriptions in their practices and everyday behaviors [10].
Postural training usually synchronizes breath and movement in controlled sequences while creating moderate physical/mental stress to be counteracted through self-regulatory strategies. Different schools can be more energetic, more stable, or not include physical training at all. Most breathing exercises/pranayamas carry slow and controlled qualities (e.g., alternate nostril breathing) but there are also vigorous exercises (e.g., fast effortful exhalations), and these can be performed alone or during postures (e.g., ujjayi, breathing with a slight throat constriction, is largely used in postural practice).
Moreover, the role of meditation can vary depending on styles and stages of practice [11]. It might be the main focus of a tradition, play a complementary role after training another component, or be only implicitly present, built into postural practice. Across components, practitioners are often encouraged to cultivate attentional and meta-cognitive engagement with mental experiences and sensorimotor sensations of interoceptive, proprioceptive, kinesthetic or spatial qualities. Even if no specific meditative technique is employed, beginners might gradually transition from unstable, effortful, closed-focus and object-oriented meditative experiences to more stable, effortless, open and meta-aware experiences [9, 12].
These multiple components constitute a challenge for psychological and neuroscientific research, when trying to describe their unique and synergistic contributions, but theoretical frameworks have sought to describe their associated mechanisms [6, 8, 13]. Yoga-based practices are proposed to strengthen bidirectional communication across high-level brain networks (e.g., the frontoparietal control network, which is linked to behavioral inhibition and executive monitoring; and the central executive network, which is linked to attentional control), low-level networks (e.g., the striatopallidal-thalamocortical network, which is linked to extinction learning; and the dorsal attention network, which is linked to attentional orienting), and interoceptive processes (e.g., the sensorimotor, cardiovascular, respiratory, and visceral systems).
The neurovisceral integration model, although not specifically devoted to yoga-based practices, might also help to derive possible mechanisms. It explains how parasympathetic-driven autonomic inhibitory processes, reflected in vagally-mediated heart rate variability, regulate attention and emotion [14, 15]. Smith et al. [16] expanded the model, outlining eight hierarchical levels of vagal control from the cardiac ganglia and reflex arcs to brainstem nuclei, hypothalamus, amygdala, and cortical networks. Yoga practices may differentially affect these levels, enhancing self-regulation in cognitive, behavioral, and emotional domains through improved parasympathetic tonus.
Several reviews and meta-analyses support that yoga-based practices are associated with changes in brain structure and function across these hierarchical levels [13, 17], emotion regulation [18], cognitive functioning [19], stress-related physiology [20], and neuropsychiatric symptomatology [21, 22], but the empirical scenario is far from complete. It is possible that some of these modifications occur more distinctively over continued practice, but it is hard to distinguish the temporal dynamics of effects without a systematic organization of the literature. For instance, despite a considerable body of evidence linking yoga practice to parasympathetic tonus, drawing firm conclusions has been hindered by systematic methodological limitations. These include heterogeneous samples, small sample sizes, a lack of randomized controlled trials, insufficient experimental control, variability in yoga interventions, and inadequate methodological or statistical reporting [20, 23, 24]. On top of that, mixed results could also come from not accounting for the long-term trajectories of effects.
Few intervention studies have lasted beyond a few months, when the time scale that yoga-based practices require to establish some of its effects might be longer than that [25–28]. For example, prominent systematic reviews reported interventions lasting from 5 weeks to 6 months, when assessing yoga for cognitive functions [19], from 3 days to 8 weeks, for anxiety [29], from 3 days to 12 weeks, for depression [30, 31], from 2 weeks to 6 months, for several neuropsychiatric conditions [21], and from 10 days to 24 weeks for inflammatory processes [32].
Moreover, cross-sectional studies tend to include practitioners with several years of experience, but samples can be heterogeneous not only with respect to experience levels, but also to age, physical and mental health, individual differences, cultural context, etc., such that long-term effects are not easily distinguished from multiple sources of variability. Prolonged exposure to yoga-based practices is likely to lead to differential quantitative and qualitative outcomes [6, 8, 33], and we argue that it should be considered separately for a refined understanding of the mechanisms and impacts of yoga—it can be a meaningful filter for organizing the growing number of studies in the field, contextualizing mixed findings, and guiding future research. At this point, it is unclear what has been done at this intersection, and a preliminary search did not identify any reviews on the topic.
Considering our goals, the state of the literature, and JBI’s guidelines, a scoping review was deemed more appropriate than a systematic review, given that we aim to conduct comprehensive coverage of the literature, examine the available evidence in the field, evaluate how research has been conducted, identify knowledge gaps, and facilitate future systematic reviews [34–36]. In addition, scoping reviews are useful frameworks compared with traditional literature reviews, given that they follow a prespecified protocol, adopt a systematic search strategy, extract and present data in a structured way, and aim to be reproducible and reliable [37]. Applying the PRISMA extension for scoping reviews (PRISMA-ScR) also ensures greater transparency and rigor in this endeavor [38].
Present study
This scoping review aimed to comprehensively identify the available evidence regarding long-term yoga-based practices, assess the main knowledge gaps, explore promising research directions, and present evidence maps of the neural, cognitive, physiological, and psychological outcomes from selected studies. It followed an apriori protocol and a systematic search strategy, according to JBI’s and PRISMA-ScR guidelines ([link removed for blinding]). It was beyond the scope of this work to conduct individual critical appraisals, as usual and recommended by guidelines for scoping reviews with a high volume of included studies. Our aim was to document as much of the literature as possible, having in mind that exposing the current state of the evidence also allows researchers to identify and correct for limitations in the field. To provide some information on general publication quality, however, each map includes journal-level impact factors and rankings. While these indices do not reflect the quality of individual studies, they inform on how long-term yoga publications are situated in relation to the broader psychological and neuroscientific literature. This study’s PCC elements (participants, concept, and context) are described next [35].
Participants
The participants should have been clinical or nonclinical adults (18 + years old), with more than one year of experience in a yoga-based practice, considering prior experience and/or interventions. Long-term experience was operationalized as more than one year of practice, since this period of time is within feasible limits for interventions, and filters out the development of basic skills and functional adjustments [39, 40]. It is an inevitably arbitrary criterion for inspecting the gradual and complex dynamics of continued practice [39–41], and different yoga traditions or cultural contexts can diverge on what constitutes a “long-term” practice. Our attempt was to capture as much of the literature as possible, but relevant studies might have fallen out of operational definitions.
Concept
Modern yoga-based practices, shaped by complex cultural and historical influences, often incorporate physical postures, breathing exercises, and meditation. Physical postures synchronize breath and movement in controlled sequences, ranging from gentle to vigorous. Breathing exercises can be calming or energizing, often practiced independently or integrated into physical postures. Meditation, in turn, involves mental techniques to cultivate particular states of cognitive-affective experience, such as equanimity, focused concentration, or open awareness. A common thread across these practices is the cultivation of attentional-related skills, both of bodily sensations and mental processes, which are often associated to increased self-awareness, emotional regulation, and overall well-being [6, 9, 42].
Context
This scoping review covers neuroscientific and psychological research, so that studies should have measured neural, cognitive, psychological, and/or physiological outcomes. The field has attracted increasing interest in contemplative traditions, but meaningful filters are needed to organize, refine and contextualize findings. We did not identify previous efforts to gather and systematize evidence on the effects of continued practice, despite theoretical predictions of its relevance.
Types of sources
This review considered study designs that presented original data including experimental, quasi-experimental, analytical observational designs and descriptive observational designs. Therefore, no reviews, meta-analyses or opinion papers were included.
Method
Study selection
Four databases (PubMed, Cochrane, LILACS, and PubPsych) were last searched in March 2023, using the following terms: (yoga OR yoga-based OR ioga) AND (neurocog* OR neuropsych* OR neurophys* OR physiolog* OR brain OR cognition OR memory OR working memory OR attention OR executive OR emotion* OR top-down OR bottom-up OR regulation OR inhibit* OR decision). The terms were selected based on previous reviews. Following a prespecified protocol ([link removed for blinding]), studies had to: evaluate practitioners with more than one year of practice; investigate clinical or nonclinical adults; specify yoga-based practice(s) of interest; measure a neurological, cognitive, psychological, or physiological outcome; be in English, Spanish, or Portuguese; present original data (no reviews or meta-analyses); and mention search terms in the title/abstract. No date limits were applied.
We excluded all cases in gray areas, i.e., studies that reported a mean experience greater than one year but included any number of participants with less than one year of practice; and those with a 1-year follow-up where participants did not necessarily maintain their practices throughout this time, since these posteffects would reflect the consequences of a short- and not a long-term practice [43–47]. Studies that presented mixed mind-body practices, or reported insufficient information about the variables of interest, procedures, statistical tests, or results (e.g., not reporting yoga experience, reporting p-values only, not reporting results for all measured variables) were also excluded, after mutual agreement of two reviewers, to increase uniformity and integrity of the included evidence.
The search results were imported into the citation management software Mendeley for duplicate removal. The unique results were subsequently uploaded to SysRev for systematic data curation [48]. Two independent reviewers evaluated whether studies were eligible for full-text reading. After independent study selection of the database results, the reference lists of all the selected articles were also manually searched by the first author. Titles that indicated an evaluation of any yoga-based practice and any outcome of interest (neural, cognitive, psychological, or physiological) were then uploaded to SysRev. The same independent reviewers decided whether reference list articles should be included. Conflicts were resolved in dialog based on the inclusion criteria. Most conflicts arose from studies in gray areas (as described previously), so that conflict resolution took the form of agreements on a consistent application of criteria between reviewers. Even though a third-party mediator was available, in the case of persistent conflict, this was not necessary in any case by following clear and consistent protocols.
Data extraction and summary
The following data were extracted from each article by the first author: authors, publication year, country of origin, objective, sample size, years of yoga experience, specific yoga practices, and key findings. The data extraction tool was a shared online spreadsheet so that it could be edited and double-checked by the other authors. The studies were then summarized in three evidence maps, one for each yoga component. All three evidence maps follow a 4-level structure: (1) Outcome category (i.e., neural, cognitive, psychological, or physiological); (2) Measure category (relevant to the particular outcome); (3) Study design (i.e., baseline or structural correlates of long-term practice, effects of real-time practice, stimulus response, behavioral task or one-year + interventions); and (4) Literature size (i.e., number of identified studies for a given study design). Studies that measured multiple yoga components or outcomes were repeated between or within maps, so that each outcome could be appropriately categorized and counted. Evidence maps were created on the Lucidchart platform (lucid.app).
We have included journal-level metrics of impact on each map, to inform readers about the overall publication quality. Each map displays the average SJR Impact Factor and SCImago Journal Rankings of the included articles [49]. The SJR Impact Factor is a journal-level metric of the citation frequency of the articles published in that journal for a given year, weighted by the importance or prestige of the journals where the citations came from. Moreover, the Scimago Journal Rankings classify journals of a specific field (e.g., Applied Psychology; Behavioral Neuroscience; Complementary and Alternative Medicine) in quartiles based on citation impact. Journals in Q1 are considered top-tier, followed by those in Q2, Q3, and Q4. Because these metrics are only available from 1999 onward, older articles were not included in the average impact factor, and they were counted as N/A in the rankings chart. In addition, we provide a qualitative summary of the results for each study design.
Results
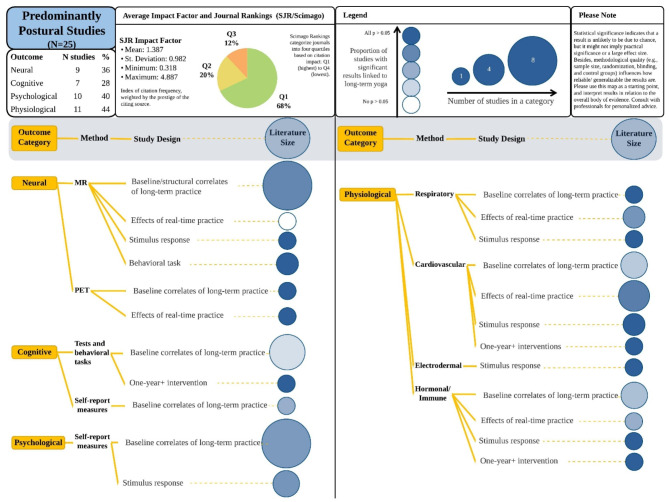
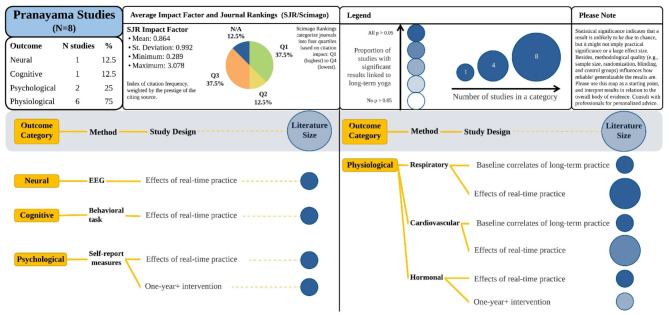
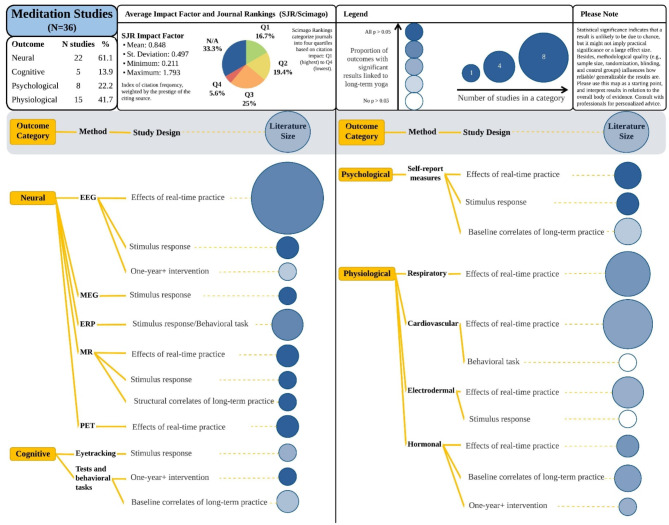
Out of 2270 unique studies, 90 were selected for full-text review by two independent reviewers, and 65 were included after mutual agreement. Figure 1 presents a flowchart of the study selection process. For each yoga component, one evidence map is then presented. Figure 2 shows the evidence map of predominantly postural studies (n = 24); these studies were named “predominantly postural” because practitioners commonly engaged in complementary pranayama or meditative training in addition to their postural practice. Figure 3 shows the evidence map of pranayama studies (n = 8), and Fig. 4 presents meditation studies (n = 36). Each map also includes the number and percentage of studies that measured a certain outcome type, as well as journal-level impact factors and rankings.
Fig. 1.
PRISMA flow diagram of the study selection process
Fig. 2.
Evidence map of postural yoga-based practices
Note: MR = Magnetic resonance, PET = Positron emission tomography. Qualitative summaries for each study design are provided in the Results section
Fig. 3.
Evidence map of breathing yoga-based practices
Note: EEG = Electroencephalography. Qualitative summaries for each study design are provided in the Results section
Fig. 4.
Evidence map of meditative yoga-based practices
Note: EEG = Electroencephalography, MEG = Magnetoencephalography, ERP = Evoked-Response Potentials, MR = Magnetic resonance, PET = Positron emission tomography. Qualitative summaries for each study design are provided in the Results section
Qualitative summary
Next, we provide qualitative summaries of the results for each yoga component, followingthe structure of the evidence maps (i.e., yoga component, outcome category, study design), to facilitate information retrieval. In summary, although somewhat heterogeneous, neural results from long-term meditative and postural studies reveal structural and functional changes in brain regions related to sensorimotor, interoceptive, emotion regulation, and executive functions [27, 28, 50–58]. Pranayama studies were scarce, hindering overarching conclusions about neural patterns. Physiological studies have often associated long-term practice with parasympathetic-driven autonomic, hormonal and immune responses [e.g., 59, 61–66], but some studies revealed sympathetic- or mixed-driven responses [e.g., 67–70] Psychological outcomes included lower levels of negative affect, psychopathological symptoms, and emotional reactivity, and greater levels of mental quietness [e.g., 58, 61, 62, 71], while cognitive measures have shown improved memory, attention and executive function in long-term practitioners [e.g., 58, 60, 72], but also null behavioral effects. Commonly, however, long-term practitioners demonstrated improved neural or physiological efficiency while performing cognitive tasks, even when behavioral differences were absent [55, 57, 59].
Predominantly postural studies
Neural outcomes
Baseline/Structural effects of long-term practice
Functional studies have revealed greater resting-state connectivity in the dorsal attention network [50] and in the anteroposterior default mode network [51]. Moreover, structural changes associated with long-term yoga experience include greater volume in several regions, such as the dorsal medial prefrontal cortex [52], middle, superior and orbital frontal gyri [53, 54], insula [28, 52], frontal operculum, orbitofrontal cortex [28], hippocampus [55], cingulate cortex, supplementary motor area, primary sensorimotor cortex, and middle temporal gyrus [28].
Remarkably, Villemure et al. [28] evaluated how specific yoga components contribute to gray matter volume in aging—combining postures and meditation contributed the most to explaining differences in the hippocampus, precuneus/posterior cingulate cortex, and primary somatosensory cortex/superior parietal lobule, whereas combining meditation and pranayama contributed the most to primary visual cortex size. Such statistical procedures could be replicated. In addition, they reported that years ofexperience correlated mainly with changes in the left hemisphere (i.e., insula, frontal operculum, and orbitofrontal cortex), and that only controls experienced an age-related gray matter decline, demonstrating the neuroprotective effects of long-term yoga.
Another study reported no structural differences between Ashtanga yoga practitioners and controls but found lower resting-state regional glucose metabolism in the hippocampus, parahippocampus, amygdala, insula, anterior midbrain, striatum, and cerebellum, with a peak effect in the left parahippocampus, via 18 F-FDG PET [56]. It is possible that long-term yoga practice could lead to an increased cortical and subcortical inhibition, or that brain regions could chronically present a more efficient glucose metabolism.
The abovementioned studies relate long-term yoga practice to structural and functional modifications of brain regions involved in interoceptive, sensorimotor, motivational and executive functions [13]. Considering lateralized findings, future studies could test whether such asymmetric neuroanatomical substrates in long-term yoga practitioners seem to be linked to parasympathetic tone and positive states, as suggested previously [28].
Effects of real-time practice
Van Aalst et al. [56] acquired PET and fMRI scans of Ashtanga yoga practitioners and matched controls after postural practice or physical exercise, respectively. After practice, yoga practitioners showed a regional relative increase in cerebellar glucose metabolism, whereas controls showed nochanges in glucose metabolism. In turn, the fMRI results demonstrated no group differences.
Stimulus response
Compared with matched controls, practitioners tolerated pain more than twice as long. Insular gray matter volume was positively correlated with increased pain tolerance, and with years of yoga experience. As they tolerated pain, practitioners have also used cognitive strategies focused on parasympathetic regulation and interoceptive awareness, which might be linked to use-dependent enlargement of the insular cortex [52].
Behavioral tasks
In an affective Stroop, practitioners showed lower right dorsolateral prefrontal cortex activity when passively viewing negative stimuli, and greater ventrolateral prefrontal cortex activity when actively responding to trials. In this study, amygdala activity predicted lower positive affect only for controls – the authors suggest an uncoupling between amygdala reactivity and downstream effects on mood states for practitioners, possibly due to frontal executive-dependent emotion regulation processes [57]. In a working memory task, practitioners exhibited lower left dorsolateral prefrontal cortex activity during encoding, but no differences in performance. Considering this region’s sensitivity to task load, the authors suggest an enhanced encoding efficiency in long-term practitioners [55].
Cognitive outcomes
Baseline correlates of long-term practice
Menezes et al. [58] compared more- and less-experienced practitioners in an emotional discrimination task. The more experienced group showed less emotion interference under low attentional demand than did the less experienced group, but group differences disappeared under high attentional demand. Another two studies investigated emotional interference in behavioral tasks and their neurophysiological correlates. During an affective Stroop, the behavioral performance of long-term practitioners was not different from that of controls, but practitioners had lower cardiovascular reactivity during the task [59]. Similarly, another study revealed no differences in affective Stroop performance between practitioners and controls, but identified a greater recruitment of the ventrolateral prefrontal cortex during negative (vs. neutral) distractors, which might suggest the use of frontal executive-dependent regulatory strategies [57].
Another fMRI study replicated this trend with the Sternberg Working Memory Task. Reaction time and accuracy did not differ between practitioners and controls, but practitioners showed less activation in the dorsolateral prefrontal cortex during encoding. Considering this region’s sensitivity to increased task load, decreased activation might reflect increased efficiency in working memory performance [55]. Accordingly, Froeliger et al. found that practitioners reported fewer cognitive failures than matched controls did, and the magnitude of self-reported cognitive health correlated with gray matter volume in several frontal, limbic, temporal, occipital and cerebellar regions [54]. Finally, Santaella et al. reported no differences in the Mini Mental State Examination score between elderly practitioners and matched controls, but practitioners had greater anteroposterior connectivity in the default mode network [51]. Thus, even when behavioral effects were not overtly detected, these studies suggest that long-term yoga influenced cognitive outcomes and their underlying neurophysiology, such as emotion regulation, working memory, and executive functions.
One-year + interventions
A 5-year randomized yoga intervention with nonclinical older adults was conducted in four cities in Asia or Africa. Weekly yoga practice led to improvements on memory and cognitive functions. Self-practice and attendance rate were some of the strongest moderators of these effects [60].
Psychological outcomes
Baseline correlates of long-term practice
With psychological measures as primary outcomes of interest, a number of studies found that practitioners, compared with controls, reported lower self-reported stress [61, 62], anxiety [63], depression [62], negative mood [63], hostility [62], and similar [62] or greater mindfulness levels [61]. Psychological measures have also been used for experimental control (e.g., to ensure that the sample of yoga practitioners had greater self-reported body awareness, and then compare groups with varied body awareness levels on their susceptibility to the rubber hand illusion [73]) and for other secondary purposes (e.g., baseline descriptives in neuroimaging studies with small sample sizes, which often reported no differences between groups [51, 58]).
Stimulus response
When presented with aversive visual stimuli, practitioners have rated them as less unpleasant than controls did [58]. In addition, two studies evaluated pain perception in practitioners vs. controls, revealing that perceptual ratings of pain did not differ between groups, but autonomic responses did differ [64] or that practitioners expected long-term practice to decrease pain reactivity in everyday contexts, and that they have used mental strategies of relaxation, acceptance and nonaversive focus on the pain more frequently than did the control group, who, in turn, engaged in distraction and pain avoidance more frequently [52]. These results suggest that the actual or expected psychological impacts of aversive stimuli are lower in practitioners than in controls.
Physiological outcomes
Baseline correlates of long-term practice
With respect to between-subjects differences, long-term practitioners presented lower heart and respiration rates, greater heart rate variability and aerobic fitness [62], decreased proinflammatory cytokine levels [74], and increased morning cortisol [75]. Other studies, however, found no differences between practitioners and sedentary controls in arterial compliance and endothelium-dependent vasodilation, which indicate cardiovascular risk [76], and in oxidative stress biomarkers [63].
Effects of real-time practice
Hagins et al. [77] found that a beginner-level yoga session performed by experienced practitioners led to metabolic costs below the cardiovascular fitness recommendations, but costs during sun salutations were compatible with moderate levels of exercise intensity (> 3 metabolic equivalents). Accordingly, Lee et al. [78] described metabolic parameters consistent with vigorous physical activity levels during high-intensity hatha yoga, which included fast-paced sun salutations (> 6 metabolic equivalents). Another study reported that more experienced practitioners exhibited greater heart rate variability in an Iyengar yoga session than in a relaxation control condition [65], and lower interleukin-6 and C-reactive protein levels [59].
Stimulus response
Practitioners showed greater skin conductance in anticipation of potentially painful stimuli but similar cardiovascular and respiratory reactions to painful and nonpainful stimuli, whereas controls presented a decreased heart rate in anticipation of nonpainful stimuli and lower respiratory sinus arrhythmia in anticipation of painful stimuli [64]. In another study, more experienced practitioners produced less LPS-stimulated interleukin-6 in response to stress than less experienced practitioners did [59] (for well-conducted emotion reactivity studies where participants had less than one year of experience, see [44, 46]).
One-year + interventions
Two studies conducted one-year randomized yoga interventions for individuals with metabolic syndrome. Compared with passive controls, intervention participants presented decreased proinflammatory and increased anti-inflammatory cytokine levels [79] and a reduced number of diagnostic criteria for metabolic syndrome, such that 44% of the subjects were no longer within the diagnostic threshold after the intervention [80]. More studies could apply long-term interventions in clinical and nonclinical samples to experimentally test the physiological changes associated with continued practice.
Yoga-based breathing techniques
Neural outcomes
Effects of real-time practice
An EEG study investigated the correlates of two blocks of alternate nostril breathing in long-term practitioners, using a 1:4:2 ratio of inhalation-retention-exhalation, in cycles of 30–40 s [81]. Beta power increased during both blocks compared with that at rest, whereas alpha power increased during the second block only. Beta activations might indicate an increased state of arousal or alertness, possibly due to the extended breath retention periods, whereas alpha activation in the second round could represent a state of greater relaxation.
Cognitive outcomes
Effects of real-time practice
Performing ujjayi (a slow diaphragmatic breath through the nostrils, with a slight constriction of the glottis) led to improved selective attention, as measured by the six-letter cancellation test, and both ujjayi and control sessions led to improved speed of information processing, as measured by the digit letter substitution test [72].
Psychological outcomes
Effects of real-time practice
The same study tested whether self-reported state-trait anxiety varied when practicing ujjayi vs. simply sitting [72]. They reported a significant decrease in state-trait anxiety after both session types, but no between-group differences.
One-year + interventions
A one-year randomized intervention of Sudarshan Kriya Yoga, which follows a structured breathing practice, led to improvements in menopausal-related quality of life [82].
Physiological outcomes
Baseline correlates of long-term practice
Long-term practitioners have shown greater respiratory sinus arrythmia at rest, compared with controls, but the effect disappeared during slow-paced breathing of 15 breaths/min [83]. Another study revealed that, compared with controls, experienced practitioners presented reduced chemoreflex sensitivity during spontaneous breathing such that their ventilatory responses to both hypoxia and hypercapnia were considerably lower. Even though these effects were diminished during paced breathing, the long-term effects of yoga also seem to have independently reduced chemoreflex sensitivity [84].
Effects of real-time practice
A couple of studies have investigated chemoreflex sensitivity in long-term practitioners engaged in real-time practice [84, 85]. The first compared chemoreflex sensitivity during spontaneous and paced breathing so that paced breathing attenuated (but did not seem to fully account for) the differences in chemoreflex sensitivity between practitioners and controls [84]. Accordingly, a study inspected the ventilatory responses during one hour of ujjayi pranayama under a 1/min breath rate, suggesting a lower chemosensitivity to hypercapnia in this highly trained practitioner [84].
In within-subject designs, practitioners showed greater respiratory sinus arrhythmia during segmented breathing (eight-step inhalation and exhalation) than during bhastrika (i.e., a fast-breathing technique involving unlabored inhalation and pumping exhalation from the navel) [86] increased oxygen pulse, carbon dioxide output volume, and heart ratein pranayama practice (slow inhalation, retention, and exhalation at a 1:4:2 ratio) compared with rest and open-monitoring meditation [87], and faster physical activity recovery using a slow-paced breathing technique [88].
One-year + interventions
Menopausal women participated in a 1-year randomized intervention of Sudarshan Kriya Yoga, which consists of slow- and fast-paced cyclical breathing techniques, in contrast to walking. Practitioners have shown increased posttest antioxidant enzymes, as well as decreased blood pressure, fasting blood sugar, total red blood cells, and hemoglobin [82].
In summary, these findings suggest that pranayama practice may offer benefits for autonomic regulation and overall health, particularly in terms of reduced chemoreflex sensitivity, increased baseline respiratory sinus arrhythmia, and improved recovery from physical activity. However, drawing firm conclusions about the long-term versus short-term effects of pranayama is challenging owing to the limited number of studies, the prevalence of single-group and single-subject designs, and the general lack of methodological rigor.
Meditative yoga-based practices
Neural outcomes
Structural correlates of long-term practice
An MRI study revealed that experienced meditators had greater gray matter volume overall and in specific regions, such as the insula, ventrolateral prefrontal, ventromedial orbitofrontal, inferior temporal, and parietal cortices, than did matched controls in terms of age, sex, and education level [71]. These areas have been associated with attentional and emotional regulation and interoceptive and autonomic function monitoring.
Effects of real-time practice
EEG studies reported that, compared with rest, meditative states of experienced practitioners led to greater activity in the alpha [66, 89, 90] and theta bands [67, 91, 92] (but also see null results in [90, 93]). Although the functional significance of the alpha and theta bands has been highly debated, they seem to cooccur with states of relaxed alertness in meditative states [94]. Prefrontal, frontal, and central regions are frequently implicated [91–93], and a few studies have reported greater coherence between the anterior-posterior [89, 90], frontal [90], and frontoparietal regions [95]. Thomas et al. compared groups with 4 and 30 years of meditative experience, on average, and reported that less experienced individuals presented greater parietal and frontal cortical activity in theta and alpha, whereas more experienced individuals presented greater temporal and insular cortical activity at higher frequencies, especially gamma, which is thought to facilitate neuroplasticity through the widespread coordination of neural assemblies [27].
The frequency band hypothesis proposes that t increased low-frequency oscillations, mainly in frontal regions, are more prevalent in the initial stages of experience, marked by the learning of internalized attention and enhanced relaxation. In turn, high-frequency oscillations become more frequent in the advanced stages of practice [33]. This hypothesis receives empirical support from Zen [96], Tibetan Buddhist [97, 98], and Yogic meditation practices [43]. Unfortunately, most of the EEG studies we identified filtered out gamma signals [e.g., 66, 67, 89–92] so that the association between meditative expertise and high-frequency oscillations remains unexplored in yoga-based practices.
During meditation, PET studies have revealed an increase in ventral striatal dopamine release associated with reduced reports of readiness for action [99] and greater anterior‒posterior ratios of the metabolic rate linked to states of relaxed concentration [100]. Additionally, (f)MRI studies have correlated self-reported deep meditative states with gray matter volumes in the anterior cingulate cortex; functional connectivity with the bilateral anterior insula [101]; and activation in the right inferior frontal cortex, right insula, right middle/superior temporal cortex [102], thalamus, insula and cingulate cortex [103]. Although somewhat heterogeneous, these results point to the recruitment of regions involved in sensorimotor integration, interoception, and emotion regulation, aligned with other neurobiological findings of yoga [13].
Stimulus response or behavioral tasks
EEG, MEG, and ERP studies that investigated responses to affective [104], aversive [105], or painful stimuli [103, 106] tended to find attenuated reactivity, distress or arousal in long-term practitioners (also see [107], a pioneer study that was excluded for not reporting years of experience), but there were mixed findings when responding to auditory stimuli [108, 109]. A study also compared more experienced, less experienced, and nonpractitioners on contingent negative variation, an ERP index of anticipatory responses between cue and target presentation. More experienced practitioners exhibited greater anticipatory responses and lower distraction interference during tasks [110].
One-year + interventions
A single-group one-year intervention study revealed greater frontal broadband coherence during transcendental meditation than at baseline to 2 months posttest, but no significant differences were detected between 2, 6, and 12 months posttest. Increased coherence also occurred during the rest and reaction-time tasks. No changes in lateral asymmetry were observed from pre- to postintervention [93].
Cognitive outcomes
Baseline correlates of long-term practice
Meditators tended to outperform controls in baseline measures of attention, working memory, and executive function [111, 112] (but see [110] for null behavioral results).
Stimulus response
An eye-tracking study compared experienced Sahaja Yoga meditators and controls in an affective free-viewing paradigm. When presented with displays of four facial expressions (neutral, angry, fearful, and happy), meditators spent less time viewing angry and fearful faces and selectively attended to happy faces, whereas controls reported increased dwell time on both angry and happy faces [113]. A positivity bias may indicate heightened appetitive motivation and may protect practitioners from attention-related vulnerabilities to psychopathology (e.g., threat-related attentional biases in anxious individuals).
One-year + interventions
Compared with a control intervention, a two-year intervention involving transcendental meditation led to improvements in intelligence scores and reaction time performance from pre- to posttraining [114].
Psychological outcomes
Baseline correlates of long-term practice
A study reported greater self-reported emotional stability, inner orientation, moral reasoning, and lower state/trait anxiety when comparing meditators and controls under baseline conditions [93]. Two other studies, interested in stress-related physiology, measured self-reported anxiety for experimental control, not as a main outcome of interest, thus reporting no differences in anxiety levels between practitioners and controls [115, 116].
Effects of real-time practice
More experienced practitioners reported experiencing more intense feelings of bliss, lower thought appearance, and lower restlessness than less experienced practitioners did while meditating [105]. Two studies have also investigated the functional and structural neural correlates of self-reported mental silence so that this psychological measure was not the main outcome of interest but played a key role in their design [101, 102]. In addition, the depth of mental silence in the laboratory has been correlated with age, years of experience, and the reported frequency of mental silence in habitual practice [101]. These results suggest a progressive development of mental quietness as a result of long-term practice.
Stimulus response
Compared with controls, experienced practitioners reported lower emotional reactivity to both types of stimuli after exposure to neutral and aversive movie clips [105]. Kakigi et al. [103] also documented a practitioner who reports feeling pain during nonmeditative states, as evoked by laser stimulation, but claims to feel no pain during meditative states.
Physiological outcomes
Baseline correlates of long-term practice
Compared with nonpractitioners, experienced meditators presented decreased baseline levels of morning beta-endorphin, ACTH [115], norepinephrine, and epinephrine [116]; decreased evening norepinephrine [116]; and decreased daily fluctuations in beta-endorphin, ACTH [115], and catecholamines [116] but no changes in cortisol levels [115]. Another study, however, revealed that more experienced practitioners had increased urine excretion of catecholamines and their metabolites, which indicates heightened sympathetic activity [68]. All three studies investigated transcendental meditation practitioners, so the mixed findings cannot be attributed to the specific technique.
Effects of real-time practice
A number of studies have shown that, compared with rest, meditative states in experienced practitioners lead to parasympathetic-driven autonomic and hormonal responses, such as increased respiratory sinus arrythmia [90], decreased heart rate [68, 69, 87], lower peripheral vascular resistance [69], decreased oxygen consumption [87, 117], increased abdominal breathing [66], increased respiratory amplitude [67], a lower respiration rate [66, 67, 90], lower electrodermal activity [90], increased evening melatonin [118], and decreased cortisol levels [119].
Some studies, however, have associated sympathetic-driven or mixed responses with meditative states in long-term practitioners, including a greater heart rate [67, 70]; a decreased respiratory rate but increased electrodermal activity in more experienced practitioners than in less experienced and nonpractitioners [67]; and increased plasma noradrenaline, diastolic blood pressure, or urinary excretion of catecholamines in more experienced practitioners than in less experienced practitioners [68, 69, 87] (see [69, 70] for null cardiovascular, respiratory and/or electrodermal results).
Stimulus response and behavioral task
When responding to auditory clicks [108] and to reaction-time tasks [110], experienced meditators showed no differences in physiological responses compared with controls.
One-year + interventions
A study investigated hormonal changes before and after 3 years of meditative training, reporting a progressive decrease in thyroid stimulation hormone, growth hormone, and prolactin but no changes in cortisol, T3, or T4 over multiple assessments [120].
While many studies point to parasympathetic-driven states [e.g., 87, 66, 90, 117, 118], several others present mixed or sympathetic-driven activations during meditation [67, 68, 69, 70]. The available evidence suggests that there is no unique physiological signature of yoga-based meditations, and future studies, reviews and meta-analyses could quantitatively assess the extent to which the experience level of the practitioner might lead to parasympathetic or mixed profiles, for a given technique.
Discussion
Methodological limitations and recommendations
Reporting of yoga practice
Frequently, studies did not report how yoga experience was measured. A few different options are available, such as questionnaires, interviews, screenings, or yoga schools’ archives. Clear descriptions can help to critically appraise the provided information, qualify mixed findings, and facilitate replications. In addition, the investigated practices can be more thoroughly detailed, beyond generic descriptors such as “meditation” or “yoga”. Specific practice compositions are likely to have differential long-term effects [9, 28, 121], so that reporting the studied tradition/style, component(s), frequency, and duration of practice for each component would help to refine the research questions and compare results.
Study designs
Cross-sectional studies were highly prevalent in this review, often with single group designs. Using well-matched control groups and multiple pre/posttest measurements are strategies that could be better explored. Comparing groups with progressive levels of experience (e.g., 1–3 years; 3–5 years; 5–10 years; 10 years+) might be helpful to investigate linear and non-linear effects of long-term practice. Studies that have done so revealed not only quantitative changes (e.g., a more intense relaxation response in the more-experienced group), but also qualitative changes as a function of experience (e.g., a mixed- or sympathetic-driven response in the more experienced group vs. a predominantly parasympathetic response in the less experienced group). The field would also benefit from well-designed long-term interventions and randomized controlled trials. Implementing them poses challenges such as financial costs, personnel limitations, and time displacement of publications, but they would largely strengthen the explanatory power of long-term yoga studies.
Reporting of statistical tests and results
A problematic and recurrent limitation was the incomplete reporting of statistical tests or results. For example, reporting means, standard deviations, and p-values only, with no indication of test statistics, degrees of freedom, nor effect sizes; not clearly stating which variables/groups were being tested; or reporting statistically significant results only. When interpreting and communicating results, researchers should also be mindful of confirmatory language. A preference for confirmatory affirmations might lead researchers to overlook important phenomena, such as contradictory, nonsignificant and nonintuitive results, and can compromise the integrity of the field. Pre-registered studies can also be more widely adopted, to increase the reliability and robustness of the findings. We have also identified instances where religious or institutional motives seem to be operating for researchers and/or participants, and potentially biasing their reports and explanatory framings to favor specific schools/techniques. Future research, using critical appraisal and risk of bias tools, could systematically inspect how much risk these factors impose to the integrity of the findings. Some of these points were already brought up by other authors [8, 9, 122], but were also found in our review.
Limitations of this review
Publication biases of positive results cannot be discarded, and language biases are likely to be present insofar as studies in English, Spanish or Portuguese were included, whereas studies in South-Asian or other languages were not. Thus, despite our sincere efforts, this is not an exhaustive review and important evidence might have been missed. Additionally, we did not perform critical appraisals of individual studies. In this way, this review might include studies of low methodological quality, which are likely to be unreliable. We expect, however, that exposing the current state of the evidence also allows researchers to identify and correct systematic limitations in the field.
Future directions
Unpacking yoga’s complexity
Future research should delve deeper into the unique and combined contributions of different yoga components (meditation, pranayama, and postural practice) to specific outcomes. Isolating individual components to investigate their mechanisms is a helpful and valid approach but, beyond that, new experimental designs and statistical techniques can identify and quantify the interactive contributions of yoga components to specific research questions, given that in real-world scenarios they are usually practiced in tandem (e.g., [28]. Additionally, the expertise literature points to many other facets of superior performance, beyond years of experience. Fundamental contributors to skill acquisition and development include deliberate practice, teacher guidance, informative feedback, and situational/contextual characteristics of the training [39, 40, 41]. Individual differences, such as age, physical or mental health, socioeconomic status, and adverse life events, are also promising moderators of continued practice effects, which can be better incorporated into the yoga literature.
Testing specific theoretical models
We encourage researchers to work with specific overarching theoretical models that could shed light on the mechanisms underlying yoga’s effects, instead of focusing on narrowly focused research questions. One promising framework is the neurovisceral integration model, which posits that vagal control regulates the different hierarchical levels of organization in the organism [14, 15, 16]. Other theoretical models, such as predictive coding, also offer valuable avenues for investigation [6, 123, 124]. By grounding research in a specific framework, researchers can more effectively identify common underlying mechanisms and address fundamental explanatory gaps.
Diversifying measures and paradigms
In general, neural and physiological outcomes were the most frequently investigated, while cognitive and psychological variables were less represented. It is crucial to examine how experienced practitioners perform on cognitive tasks, along with their psychological and phenomenological experiences of both real-time practices and their long-term trajectory. Cognitive and psychological assessments can be seamlessly integrated with neural and physiological measures, and future research should explore the intersection of these diverse outcomes to build a more integrated understanding of long-term yoga.
Cultural and contextual factors
In our understanding, long-term yoga effects cannot be abstracted from the social, cultural and contextual factors around them. Traditionally, yoga traditions were situated in South Asian worldviews, and their translocative dynamics to Westernized environments created hybrid frameworks through which practitioners understand their continued commitments to practice. These frameworks seem to influence the motivations behind long-term practice, such as physical health, stress-management, mental health, religious or spiritual reasons, social or community belonging, and they will be embedded in the long-term trajectories of effects. For instance, achieving metabolic recommendations for physical activity would be a priority to design interventions for cardiovascular health, but might not be a priority when proposing interventions for parasympathetic tonus.
Collaborations between the sciences and the humanities can help to analyze the macro-level situatedness of modern yoga practices. Creating context-sensitive interventions is also a pathway worth exploring. For example, Pandya’s multicity intervention study suggests that yoga practices were more effective for Asian, compared to African populations [60]. Interventions that are designed to be more culturally appropriate are likely to have a greater impact on a given local population.
Systematic reviews and meta-analyses
This scoping review represents an initial step of evidence summary, and we suggest, as next steps, that researchers consider conducting systematic reviews with risk of bias assessments and meta-analyses. In this way, our qualitative summaries can be tested against critical, quantitative, and meta-analytic systematizations. Researchers and practitioners are encouraged to use the presented data not as definitive evidence, but as a point of entry for further critical inquiries and creative investigations. Future reviews and meta-analyses also need to be responsive to contextual and motivational factors, and could try to pool results in ways that acknowledge the myriad objectives that practitioners might have (e.g., comparing slower vs. more dynamic practices; cardiovascular/physical health vs. relaxation/mental health motivations). Being able to do that goes back to researchers clearly stating the components of practice they are studying, the goals of their interventions, and the motivations that practitioners express to engage with long-term practices.
In summary, to advance our understanding of yoga’s long-term effects, future research must integrate its inherent complexity by considering the unique and shared effects of yoga components, employing careful experimental paradigms, and applying statistical models that can capture the multifaceted nature of yoga-based practices. Researchers should diversify outcome measures and experimental designs, and consider culturally sensitive interventions that account for individual and community differences. Exploring the motivational and contextual factors that influence long-term outcomes is crucial for developing a situated understanding of long-term yoga effects. Finally, systematic reviews and meta-analyses will be essential for synthesizing findings across diverse studies, offering robust evidence to inform both theory and practice in this evolving field.
Author contributions
GC: Conceptualization, methodology, data selection, extraction and visualization, synthesis, and writing (original draft). JRA: Conceptualization, methodology, data selection, validation, and writing (review and editing). JPA: Validation and writing (review and editing). WCS: Validation, supervision, and writing (review and editing). GMC: Validation, supervision, and writing (review and editing).
Funding
GC and JRA received funding from the Brazilian National Council for Scientific and Technological Development during the execution of this work in the form of postgraduate scholarships.
Data availability
Data is available within the manuscript. Other resources are available from the corresponding author on request.
Declarations
Ethics approval
The research project that led to this review received ethics approval from our local committee (details removed for blinding).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Harimoto K. How yoga became yoga: yoga and meditation up to the classical period. In: Newcombe S, O’Brien-Kop K, editors. Routledge Handbook of Yoga and meditation studies. Routledge; 2020. pp. 65–79.
- 2.Mallinson J, Singleton M. Roots of Yoga. Penguin; 2017.
- 3.De Michelis E. A history of modern yoga: Patanjali and Western esotericism. Continuum; 2005.
- 4.De Michelis E. A preliminary survey of modern yoga studies. Asian Med. 2007;3:1–19. [Google Scholar]
- 5.Newcombe S. The development of modern yoga: a survey of the field. Relig Compass. 2009;3:986–1002. [Google Scholar]
- 6.Gard T, Noggle JJ, Park CL, Vago DR, Wilson A. Potential self-regulatory mechanisms of yoga for psychological health. Front Hum Neurosci. 2014;8:1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Riley KE, Park CL. How does yoga reduce stress? A systematic review of mechanisms of change and guide to future inquiry. Health Psychol Rev. 2015;9:379–96. [DOI] [PubMed] [Google Scholar]
- 8.Schmalzl L, Powers C, Henje Blom E. Neurophysiological and neurocognitive mechanisms underlying the effects of yoga-based practices: towards a comprehensive theoretical framework. Front Hum Neurosci. 2015;9:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Schmalzl L, Jeter PE, Khalsa SBS. The psychophysiology of yoga: characteristics of the main components and review of research studies. In: Newcombe S, O’Brien-Kop K, editors. Routledge Handbook of Yoga and meditation studies. Routledge; 2020. pp. 440–59.
- 10.Campelo G, De Castilho GM, Yoga. Explicit, and implicit emotion regulation: long-term and current yoga practice predicted more attentional focusing and less emotional bias in a go/no-go task. Trends Psychol. 2023. 10.1007/s43076-023-00352-1
- 11.Schmalzl L, Crane-Godreau MA, Payne P. Movement-based embodied contemplative practices: definitions and paradigms. Front Hum Neurosci. 2014;8. [DOI] [PMC free article] [PubMed]
- 12.Lutz A, Jha AP, Dunne JD, Saron CD. Investigating the phenomenological matrix of mindfulness-related practices from a neurocognitive perspective. Am Psychol. 2015;70:632–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van Aalst J, Ceccarini J, Demyttenaere K, Sunaert S, Van Laere K. What has neuroimaging taught us on the neurobiology of yoga? A review. Front Integr Nuerosci. 2020;14:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Thayer JF, Lane RD. A model of neurovisceral integration in emotion regulation and dysregulation. J Affect Disord. 2000;61:201–16. [DOI] [PubMed] [Google Scholar]
- 15.Mather M, Thayer JF. How heart rate variability affects emotion regulation brain networks. Curr Opin Behav Sci. 2018;19:98–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smith R, Thayer JF, Khalsa SS, Lane RD. The hierarchical basis of neurovisceral integration. Neurosci Biobehavioral Reviews. 2017;75:274–96. [DOI] [PubMed] [Google Scholar]
- 17.Gothe NP, Khan I, Hayes J, Erlenbach E, Damoiseaux JS. Yoga effects on brain health: a systematic review of the current literature. Brain Plast. 2019;5:105–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Menezes CB, Dalpiaz NR, Kiesow LG, Sperb W, Hertzberg J, Oliveira AA. Yoga and emotion regulation: a review of primary psychological outcomes and their physiological correlates. Psychol Neurosci. 2015;8:82–101. [Google Scholar]
- 19.Gothe NP, McAuley E. Yoga and cognition: a meta-analysis of chronic and acute effects. Psychosom Med. 2015;77:784–97. [DOI] [PubMed] [Google Scholar]
- 20.Pascoe MC, Thompson DR, Ski CF. Yoga, mindfulness-based stress reduction and stress-related physiological measures: a meta-analysis. Psychoneuroendocrinology. 2017;86:152–68. [DOI] [PubMed] [Google Scholar]
- 21.Balasubramaniam M, Telles S, Doraiswamy PM. Yoga on our minds: a systematic review of yoga for neuropsychiatric disorders. Front Psychiatry. 2013;3 JAN:1–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hofmann SG, Andreoli G, Carpenter JK, Curtiss J. Effect of Hatha yoga on anxiety: a meta-analysis. J Evidence-Based Med. 2016;9:116–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zou L, Sasaki JE, Wei G-X, Huang T, Yeung AS, Neto OB, et al. Effects of mind–body exercises (Tai Chi/Yoga) on heart rate variability parameters and perceived stress: a systematic review with meta-analysis of randomized controlled trials. JCM. 2018;7:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Posadzki P, Kuzdzal A, Lee MS, Ernst E. Yoga for heart rate variability: a systematic review and meta-analysis of randomized clinical trials. Appl Psychophysiol Biofeedback. 2015;40:239–49. [DOI] [PubMed] [Google Scholar]
- 25.Brefczynski-Lewis JA, Lutz A, Schaefer HS, Levinson DB, Davidson RJ. Neural correlates of attentional expertise in long-term meditation practitioners. Proc Natl Acad Sci USA. 2007;104:11483–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dresler M, Sandberg A, Bublitz C, Ohla K, Trenado C, Mroczko-Wasowicz A, et al. Hacking the brain: dimensions of cognitive enhancement. ACS Chem Neurosci. 2019;10:1137–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thomas J, Jamieson G, Cohen M. Low and then high frequency oscillations of distinct right cortical networks are progressively enhanced by medium and long term Satyananda yoga meditation practice. Front Hum Neurosci. 2014;8:1–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Villemure C, Čeko M, Cotton VA, Catherine Bushnell M. Neuroprotective effects of yoga practice: age-, experience-, and frequency-dependent plasticity. Front Hum Neurosci. 2015;9:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cramer H, Lauche R, Anheyer D, Pilkington K, De Manincor M, Dobos G, et al. Yoga for anxiety: a systematic review and meta-analysis of randomized controlled trials. Depress Anxiety. 2018;35:830–43. [DOI] [PubMed] [Google Scholar]
- 30.Cramer H, Anheyer D, Lauche R, Dobos G. A systematic review of yoga for major depressive disorder. J Affect Disord. 2017;213:70–7. [DOI] [PubMed] [Google Scholar]
- 31.Cramer H, Lauche R, Langhorst J, Dobos G. Yoga for depression: a systematic review and meta-analysis. Depress Anxiety. 2013;30:1068–83. [DOI] [PubMed] [Google Scholar]
- 32.Djalilova DM, Schulz PS, Berger AM, Case AJ, Kupzyk KA, Ross AC. Impact of yoga on inflammatory biomarkers: a systematic review. Biol Res Nurs. 2019;21:198–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fell J, Axmacher N, Haupt S. From alpha to gamma: electrophysiological correlates of meditation-related states of consciousness. Med Hypotheses. 2010;75:218–24. [DOI] [PubMed] [Google Scholar]
- 34.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Social Res Methodology: Theory Pract. 2005;8:19–32. [Google Scholar]
- 35.Peters MD, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: scoping reviews. In: Aromataris E, Munn Z, editors. JBI Manual for evidence synthesis. JBI; 2020.
- 36.Peters MDJ, Marnie C, Tricco AC, Pollock D, Munn Z, Alexander L, et al. Updated methodological guidance for the conduct of scoping reviews. JBI Evid Synthesis. 2020;18:2119–26. [DOI] [PubMed] [Google Scholar]
- 37.Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18. [DOI] [PMC free article] [PubMed]
- 38.Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73. [DOI] [PubMed] [Google Scholar]
- 39.Ericsson KA. The Differential influence of experience, practice, and deliberate practice on the Development of Superior Individual Performance of experts. The Cambridge Handbook of Expertise and Expert Performance: Second Edition. Cambridge University Press; 2018. pp. 745–69.
- 40.Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100:363–406. [Google Scholar]
- 41.Hambrick DZ, Oswald FL, Altmann EM, Meinz EJ, Gobet F, Campitelli G. Deliberate practice: is that all it takes to become an expert? Intelligence. 2014;45:34–45. [Google Scholar]
- 42.Lutz A, Slagter HA, Dunne JD, Davidson RJ. Attention regulation and monitoring in meditation. Trends Cogn Sci. 2008;12:163–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Banquet JP. Spectral analysis of the EEG in meditation. Electroencephalogr Clin Neurophysiol. 1973;35:143–51. [DOI] [PubMed] [Google Scholar]
- 44.Gootjes L, Franken IHA, Van Strien JW. Cognitive emotion regulation in yogic meditative practitioners: sustained modulation of electrical brain potentials. J Psychophysiol. 2011;25:87–94. [Google Scholar]
- 45.Khalsa SB, Shorter SM, Cope S, Wyshak G, Sklar E. Yoga ameliorates performance anxiety and mood disturbance in young professional musicians. Appl Psychophysiol Biofeedback. 2009;34(4):279–89. CC-Complementary Medicine CC-Common Mental Disorders. [DOI] [PubMed] [Google Scholar]
- 46.Mocanu E, Mohr C, Pouyan N, Thuillard S, Dan-Glauser ES. Reasons, years and frequency of yoga practice: effect on emotion response reactivity. Front Hum Neurosci. 2018;12:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rhodes A, Spinazzola J, van der Kolk B. Yoga for adult women with chronic PTSD: a long-term follow-up study. J Altern Complement Med (New York NY). 2016;22(3):189–96. CC-Complementary Medicine. [DOI] [PubMed] [Google Scholar]
- 48.Bozada T, Borden J, Workman J, Del Cid M, Malinowski J, Luechtefeld T. Sysrev: a FAIR platform for data curation and systematic evidence review. Front Artif Intell. 2021;4. [DOI] [PMC free article] [PubMed]
- 49.SJR — SCImago. Journal & Country Rank.
- 50.Froeliger B, Garland EL, Kozink RV, Modlin LA, Chen NK, McClernon FJ et al. Meditation-state functional connectivity (msFC): strengthening of the dorsal attention network and beyond. Evidence-based Complementary and Alternative Medicine. 2012;2012. [DOI] [PMC free article] [PubMed]
- 51.Santaella DF, Balardin JB, Afonso RF, Giorjiani GM, Sato JR, Lacerda SS, et al. Greater anteroposterior default mode network functional connectivity in long-term elderly yoga practitioners. Front Aging Neurosci. 2019;10 JUL:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Villemure C, Čeko M, Cotton VA, Bushnell MC. Insular cortex mediates increased pain tolerance in yoga practitioners. Cereb Cortex. 2014;24:2732–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Afonso RF, Balardin JB, Lazar S, Sato JR, Igarashi N, Santaella DF, et al. Greater cortical thickness in elderly female yoga practitioners-A cross-sectional study. Front Aging Neurosci. 2017;9:JUN. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Froeliger B, Garland EL, McClernon FJ. Yoga meditation practitioners exhibit greater gray matter volume and fewer reported cognitive failures: results of a preliminary voxel-based morphometric analysis. Evidence-based Complementary and Alternative Medicine. 2012;2012. [DOI] [PMC free article] [PubMed]
- 55.Gothe NP, Hayes JM, Temali C, Damoiseaux JS. Differences in brain structure and function among yoga practitioners and controls. Front Integr Nuerosci. 2018;12:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.van Aalst J, Ceccarini J, Schramm G, Van Weehaeghe D, Rezaei A, Demyttenaere K et al. Long-term Ashtanga yoga practice decreases medial temporal and brainstem glucose metabolism in relation to years of experience. EJNMMI Res. 2020;10. [DOI] [PMC free article] [PubMed]
- 57.Froeliger BE, Garland EL, Modlin LA, McClernon FJ. Neurocognitive correlates of the effects of yoga meditation practice on emotion and cognition: a pilot study. Front Integr Nuerosci. 2012;6:48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Menezes CB, Dalpiaz NR, Rossi NT, De Oliveira AA. Yoga and the interplay between attentional load and emotion interference. Psychol Rep. 2015;117:271–89. [DOI] [PubMed] [Google Scholar]
- 59.Kiecolt-Glaser JK, Christian L, Preston H, Houts CR, Malarkey WB, Emery CF, et al. Stress, inflammation, and yoga practice. Psychosom Med. 2010;72:113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pandya SP. Yoga education program for improving memory in older adults: a multicity 5-year follow-up study. J Appl Gerontol. 2020;39:576–87. [DOI] [PubMed] [Google Scholar]
- 61.Brisbon NM, Lowery GA. Mindfulness and levels of stress: a comparison of beginner and advanced Hatha yoga practitioners. J Relig Health. 2011;50:931–41. [DOI] [PubMed] [Google Scholar]
- 62.Satin JR, Linden W, Millman RD. Yoga and psychophysiological determinants of cardiovascular health: comparing yoga practitioners, runners, and sedentary individuals. Ann Behav Med. 2014;47:231–41. [DOI] [PubMed] [Google Scholar]
- 63.Yoshihara K, Hiramoto T, Sudo N, Kubo C. Profile of mood states and stress-related biochemical indices in long-term yoga practitioners. Biopsychosoc Med. 2011;5 June. [DOI] [PMC free article] [PubMed]
- 64.Cotton VA, Low LA, Villemure C, Bushnell MC. Unique autonomic responses to pain in yoga practitioners. Psychosom Med. 2018;80:791–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Khattab K, Khattab AA, Ortak J, Richardt G, Bonnemeier H. Iyengar yoga increases cardiac parasympathetic nervous modulation among healthy yoga practitioners. Evidence-Based Complement Altern Med. 2007;4:511–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Arambula P, Peper E, Kawakami M, Gibney KH. The physiological correlates of Kundalini yoga meditation: a study of a yoga master. Appl Psychophysiol Biofeedback. 2001;26:147–53. [DOI] [PubMed] [Google Scholar]
- 67.Corby JC, Roth WT, Zarcone VP, Kopell BS. Psychophysiological correlates of the practice of tantric yoga meditation. Arch Gen Psychiatry. 1978;35:571–7. [DOI] [PubMed] [Google Scholar]
- 68.Lang R, Dehof K, Meurer KA, Kaufmann W. Sympathetic activity and transcendental meditation. J Neural Transm. 1979;44:117–35. [DOI] [PubMed] [Google Scholar]
- 69.Telles S, Nagarathna R, Nagendra HR. Autonomic changes during OM mediation. Indian J Physiol Pharmacol. 1995;39:418–20. [PubMed] [Google Scholar]
- 70.Telles S, Desiraju T. Autonomic changes in Brahmakumaris Raja yoga meditation. Int J Psychophysiol. 1993;15:147–52. [DOI] [PubMed] [Google Scholar]
- 71.Hernández SE, Suero J, Barros A, González-Mora JL, Rubia K. Increased grey matter associated with long-term Sahaja yoga meditation: a voxel-based morphometry study. PLoS ONE. 2016;11:e0150757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Niranjan P, Balaram P. Immediate effect of Ujjayi pranayama on attention and anxiety among university students: a randomised self-control study. J Clin Diagn Res. 2022;16:1–4. [Google Scholar]
- 73.David N, Fiori F, Aglioti SM. Susceptibility to the rubber hand illusion does not tell the whole body-awareness story. Cogn Affect Behav Neurosci 2014;14:297–306. 10.3758/s13415-013-0190-6 [DOI] [PubMed]
- 74.Kiecolt-Glaser JK, Christian LM, Andridge R, Hwang BS, Malarkey WB, Belury MA, et al. Adiponectin, leptin, and yoga practice. Physiol Behav. 2012;107:809–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vera FM, Manzaneque JM, Maldonado EF, Carranque GA, Rodriguez FM, Blanca MJ, et al. Subjective sleep quality and hormonal modulation in long-term yoga practitioners. Biol Psychol. 2009;81:164–8. [DOI] [PubMed] [Google Scholar]
- 76.Hunter SD, Tarumi T, Dhindsa MS, Nualnim N, Tanaka H. Hatha yoga and vascular function: results fromcross-sectional and interventional studies. J Bodyw Mov Ther. 2013;17:322–7. [DOI] [PubMed] [Google Scholar]
- 77.Hagins M, Moore W, Rundle A. Does practicing hatha yoga satisfy recommendations for intensity of physical activity which improves and maintains health and cardiovascular fitness? BMC Complement Altern Med. 2007;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee K-H, Ju H-M, Yang W-H. Metabolic energy contributions during high-intensity hatha yoga and physiological comparisons between active and passive (Savasana) recovery. Front Physiol. 2021;12. [DOI] [PMC free article] [PubMed]
- 79.Supriya R, Yu AP, Lee PH, Lai CW, Cheng KK, Yau SY, et al. Yoga training modulates adipokines in adults with high-normal blood pressure and metabolic syndrome. Scand J Med Sci Sports. 2018;28:1130–8. [DOI] [PubMed] [Google Scholar]
- 80.Siu PM, Yu AP, Benzie IF, Woo J. Effects of 1-year yoga on cardiovascular risk factors in middle-aged and older adults with metabolic syndrome: a randomized trial. Diabetol Metab Syndr. 2015;7:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Stančák A, Kuna M. EEG changes during forced alternate nostril breathing. Int J Psychophysiol. 1994;18:75–9. [DOI] [PubMed] [Google Scholar]
- 82.Swain D, Nanda P, Das H. Impact of yoga intervention on menopausal symptoms-specific quality of life and changes in hormonal level among menopausal women. J Obstet Gynaecol Res. 2021;47:3669–76. [DOI] [PubMed] [Google Scholar]
- 83.Bertisch SM, Hamner J, Taylor JA. Slow yogic breathing and long-term cardiac autonomic adaptations: a pilot study. J Altern Complement Med. 2017;23:722–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Miyamura M, Nishimura K, Ishida K, Katayama K, Shimaoka M, Hiruta S. Is man able to breathe once a minute for an hour? The effect of yoga respiration on blood gases. Jpn J Physiol. 2002;52:313–6. [DOI] [PubMed] [Google Scholar]
- 85.Spicuzza L, Gabutti A, Porta C, Montano N, Bernardi L. Yoga and chemoreflex response to hypoxia and hypercapnia. Lancet. 2000;356:1495–6. [DOI] [PubMed] [Google Scholar]
- 86.Peng CK, Henry IC, Mietus JE, Hausdorff JM, Khalsa G, Benson H, et al. Heart rate dynamics during three forms of meditation. Int J Cardiol. 2004;95:19–27. [DOI] [PubMed] [Google Scholar]
- 87.Danucalov MAD, Simões RS, Kozasa EH, Leite JR. Cardiorespiratory and metabolic changes during yoga sessions: the effects of respiratory exercises and meditation practices. Appl Psychophysiol Biofeedback. 2008;33:77–81. [DOI] [PubMed] [Google Scholar]
- 88.Monnazzi P, Leri O, Guizzardi L, Mattioli D, Patacchioli FR. Anti-stress effect of yoga-type breathing: modification of salivary cortisol, heart rate and blood pressure following a step-climbing exercise. Stress Health 2002;18:195–200. 10.1002/smi.938
- 89.Hebert R, Lehmann D, Tan G, Travis F, Arenander A. Enhanced EEG alpha time-domain phase synchrony during transcendental meditation: implications for cortical integration theory. Sig Process. 2005;85:2213–32. [Google Scholar]
- 90.Travis F, Wallace RK. Autonomic and EEG patterns during eyes-closed rest and transcendental meditation (TM) practice: the basis for a neural model of TM practice. Conscious Cogn. 1999;8:302–18. [DOI] [PubMed] [Google Scholar]
- 91.Aftanas LI, Golocheikine SA. Human anterior and frontal midline theta and lower alpha reflect emotionally positive state and internalized attention: high-resolution EEG investigation of meditation. Neurosci Lett. 2001;310:57–60. [DOI] [PubMed] [Google Scholar]
- 92.Baijal S, Srinivasan N. Theta activity and meditative states: spectral changes during concentrative meditation. Cogn Process. 2010;11:31–8. [DOI] [PubMed] [Google Scholar]
- 93.Travis F, Arenander A. Cross-sectional and longitudinal study of effects of transcendental meditation practice on interhemispheric frontal asymmetry and frontal coherence. Int J Neurosci. 2006;116:1519–38. [DOI] [PubMed] [Google Scholar]
- 94.Lomas T, Ivtzan I, Fu CHY. A systematic review of the neurophysiology of mindfulness on EEG oscillations. Neurosci Biobehav Rev. 2015;57:401–10. [DOI] [PubMed] [Google Scholar]
- 95.Shaw L, Routray A. Topographical assessment of neurocortical connectivity by using directed transfer function and partial directed coherence during meditation. Cogn Process. 2018;19:527–36. [DOI] [PubMed] [Google Scholar]
- 96.Hauswald A, Übelacker T, Leske S, Weisz N. What it means to be Zen: marked modulations of local and interareal synchronization during open monitoring meditation. NeuroImage. 2015;108:265–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Lehmann D, Faber PL, Achermann P, Jeanmonod D, Gianotti LRR, Pizzagalli D. Brain sources of EEG gamma frequency during volitionally meditation-induced, altered states of consciousness, and experience of the self. Psychiatry Res - Neuroimaging. 2001;108:111–21. [DOI] [PubMed] [Google Scholar]
- 98.Lutz A, Greischar LL, Rawlings NB, Ricard M, Davidson RJ. Long-term meditators self-induce high-amplitude gamma synchrony during mental practice. Proceedings of the National Academy of Sciences. 2004;101:16369–73. [DOI] [PMC free article] [PubMed]
- 99.Kjaer TW, Bertelsen C, Piccini P, Brooks D, Alving J, Lou HC. Increased dopamine tone during meditation-induced change of consciousness. Cogn Brain Res. 2002;13:255–9. [DOI] [PubMed] [Google Scholar]
- 100.Herzog H, Lele VR, Kuwert T, Langen K-J, Kops ER, Feinendegen LE. Changed pattern of regional glucose metabolism during yoga meditative relaxation. Neuropsychobiology. 1990;23:182–7. [DOI] [PubMed] [Google Scholar]
- 101.Elías Hernández S, Barros-Loscertales A, Xiao Y, Luis González-Mora J, Rubia K. Gray matter and functional connectivity in anterior cingulate cortex are associated with the state of mental silence during sahaja yoga meditation. Neuroscience. 2018;371:395–406. [DOI] [PubMed] [Google Scholar]
- 102.Hernández SE, Suero J, Rubia K, González-Mora JL. Monitoring the neural activity of the state of mental silence while practicing sahaja yoga meditation. J Altern Complement Med. 2015;21:175–9. [DOI] [PubMed] [Google Scholar]
- 103.Kakigi R, Nakata H, Inui K, Hiroe N, Nagata O, Honda M, et al. Intracerebral pain processing in a yoga master who claims not to feel pain during meditation. Eur J Pain. 2005;9:581. [DOI] [PubMed] [Google Scholar]
- 104.Reva NV, Pavlov SV, Loktev KV, Korenyok VV, Aftanas LI. Influence of long-term sahaja yoga meditation practice on emotional processing in the brain: an ERP study. Neuroscience. 2014;281:195–201. [DOI] [PubMed] [Google Scholar]
- 105.Aftanas L, Golosheykin S. Impact of regular meditation practice on EEG activity at rest and during evoked negative emotions. Int J Neurosci. 2005;115:893–909. [DOI] [PubMed] [Google Scholar]
- 106.Peper E, Wilson VE, Gunkelman J, Kawakami M, Sata M, Barton W, et al. Tongue piercing by a Yogi: QEEG observations. Appl Psychophysiol Biofeedback. 2006;31:331–8. [DOI] [PubMed] [Google Scholar]
- 107.Anand BK, Chhina GS, Singh B. Some aspects of electroencephalographic studies in Yogis. Electroencephalogr Clin Neurophysiol. 1961;13:452–6. [Google Scholar]
- 108.Becker D, Shapiro D. Physiological responses to clicks during Zen, yoga, and TM meditation. Psychophysiology. 1981;18:694–9. [DOI] [PubMed] [Google Scholar]
- 109.Telles S, Naveen KV. Changes in middle latency auditory evoked potentials during meditation. Psychol Rep. 2004;94:398–400. [DOI] [PubMed] [Google Scholar]
- 110.Travis F, Tecce JJ, Guttman J. Cortical plasticity, contingent negative variation, and transcendent experiences during practice of the transcendental meditation technique. Biol Psychol. 2000;55:41–55. [DOI] [PubMed] [Google Scholar]
- 111.Prakash R, Rastogi P, Dubey I, Abhishek P, Chaudhury S, Small BJ. Long-term concentrative meditation and cognitive performance among older adults. Aging Neuropsychol Cognition. 2012;19:479–94. [DOI] [PubMed] [Google Scholar]
- 112.Prakash R, Dubey I, Abhishek P, Gupta SK, Rastogi P, Siddiqui SV. Long-term vihangam yoga meditation and scores on tests of attention. Percept Mot Skills. 2010;110:1139–48. [DOI] [PubMed] [Google Scholar]
- 113.Pavlov SV, Korenyok VV, Reva NV, Tumyalis AV, Loktev KV, Aftanas LI. Effects of long-term meditation practice on attentional biases towards emotional faces: an eye-tracking study. Cogn Emot. 2015;29:807–15. [DOI] [PubMed] [Google Scholar]
- 114.Cranson RW, Orme-Johnson DW, Gackenbach J, Dillbeck MC, Jones CH, Alexander CN. Transcendental meditation and improved performance on intelligente-related measures: a longitudinal study. Pers Indiv Differ. 1991;12:11051116. [Google Scholar]
- 115.Infante JR, Peran F, Martinez M, Roldan A, Poyatos R, Ruiz C, et al. ACTH and β-endorphin in transcendental meditation. Physiol Behav. 1998;64:311–5. [DOI] [PubMed] [Google Scholar]
- 116.Infante JR, Torres-Avisbal M, Pinel P, Vallejo JA, Peran F, Gonzalez F, et al. Catecholamine levels in practitioners of the transcendental meditation technique. Physiol Behav. 2001;72:141–6. [DOI] [PubMed] [Google Scholar]
- 117.Wolkove N, Kreisman H, Darragh D, Cohen C, Frank H. Effect of transcendental meditation on breathing and respiratory control. J Appl Physiol Respiratory Environ Exerc Physiol. 1984;56:607–12. [DOI] [PubMed] [Google Scholar]
- 118.Tooley GA, Armstrong SM, Norman TR, Sali A. Acute increases in night-time plasma melatonin levels following a period of meditation. Biol Psychol. 2000;53:69–78. [DOI] [PubMed] [Google Scholar]
- 119.Jevning R, Wilson AF, Davidson JM. Adrenocortical activity during meditation. Horm Behav. 1978;10:54–60. [DOI] [PubMed] [Google Scholar]
- 120.Werner OR, Wallace RK, Charles B, Janssen G, Stryker T, Chalmers RA. Long-term endocrinologic changes in subjects practicing the transcendental meditation and TM-Sidhi program. Psychosom Med. 1986;48:59–66. [DOI] [PubMed] [Google Scholar]
- 121.Schmalzl L, Powers C, Zanesco AP, Yetz N, Groessl EJ, Saron CD. The effect of movement-focused and breath-focused yoga practice on stress parameters and sustained attention: a randomized controlled pilot study. Conscious Cogn. 2018;65(CC–):109–25. [DOI] [PubMed] [Google Scholar]
- 122.Van Dam NT, van Vugt MK, Vago DR, Schmalzl L, Saron CD, Olendzki A, et al. Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect Psychol Sci. 2018;13:36–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Farb N, Daubenmier J, Price CJ, Gard T, Kerr C, Dunn BD, Klein AC, Paulus MP, Mehling WE. Interoception, contemplative practice, and health. Front Psychol. 2015;6. [DOI] [PMC free article] [PubMed]
- 124.Pagnoni G. The contemplative exercise through the lenses of predictive processing: A promising approach. Progr Brain Res 2019;244:299–322. 10.1016/bs.pbr.2018.10.022 [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available within the manuscript. Other resources are available from the corresponding author on request.