Abstract
Introduction:
Although most children with unilateral cerebral palsy can achieve independent mobility levels with or without assistive devices, they remain susceptible to decreased participation. This study aimed to explore the potential factors affecting participation of children with unilateral cerebral palsy.
Method:
Fifty children with unilateral cerebral palsy were enrolled. The degree of spasticity in the upper limb muscles was assessed using the Modified Ashworth Scale, active range of motion of the upper limb joints was assessed using a universal goniometer, and activity performance was measured using the ABILHAND-Kids and Gross Motor Function Measure. Environmental factors and mental health were evaluated using the European Child Environment Questionnaire and Strength and Difficulties Questionnaire. The Child and Adolescent Scale of Participation was used to assess participation.
Results:
Path analysis showed that upper limb impairment had both direct (β = −0.41; p < 0.05) and indirect (β = 0.64; p < 0.001) effects on participation. Most importantly, it was found that the participation of children with unilateral cerebral palsy was notably influenced by environmental factors and mental health (β2 = −0.42; p < 0.05, and β2 = −0.36; p < 0.05).
Conclusion:
Participation of children with unilateral cerebral palsy is affected by a combination of functioning and contextual factors.
Keywords: Unilateral cerebral palsy, children, participation, structural equation modeling
Introduction
Cerebral Palsy (CP) is a lifelong condition resulting from a non-progressive yet permanent lesion in the developing brain, leading to impairments in body function, activity limitations, and participation restrictions (Cans, 2000). Despite a changing panorama worldwide, CP remains a prevalent contributor to physical disabilities in infancy, early childhood, middle childhood, and adolescence (Dar et al., 2023). Unilateral CP, characterized as unilateral involvement, is the most prevalent subtype of CP (Novak, 2014) and is highly associated with children born term (Wiklund and Uvebrant, 1991). Children with unilateral CP often exhibit more pronounced impairments, such as spasticity, reduced joint movements, muscular weakness, and sensory deficits in the affected upper limbs than in the lower limbs (Wiklund and Uvebrant, 1991). This results in developmental disregard, reduced unimanual capacity and bilateral performance, and impaired hand function in the affected upper limb. Prior research has firmly established relationships between upper limb impairments, activity limitations, and participation restrictions in children with CP (Klingels et al., 2012). Furthermore, studies have indicated the significant contributions of mental health (Ramstad et al., 2012) and environmental factors (van der Kemp et al., 2022) to the participation of children with CP. Therefore, the participation of children with CP should not be attributed solely to the outcomes of CP but should also be considered within contextual factors (i.e., environmental factors and mental health/psychological factors). In other words, the participation of children with CP is shaped by the interaction between disability, functioning, and contextual factors.
Children with CP, including those with unilateral CP, are more likely to have limited participation in home, community, and school settings compared to their typically developing peers (Imms et al., 2008). Considering that participation significantly influences the cognitive, social, physical, and emotional development of a child, acquiring a thorough comprehension of its concept in children with CP becomes imperative. The World Health Organization’s International Classification of Functioning, Disability and Health (ICF) defines participation as an individual’s “involvement in a life situation” and as the “societal viewpoint on functioning.” Therefore, participation has garnered significant attention in the ICF and has been identified as the ultimate objective of intervention approaches. Despite the absence of a universally accepted definition for participation in the literature, a systematic review conducted by Imms et al. (2016) recently revealed five interrelated themes of participation construct: preference, attendance, involvement, activity competence, and sense of self. The study also identified five key environmental factors: availability, accessibility, affordability, accommodability, and acceptability. Then they proposed that a significant relationship might exist between participation themes and environmental factors. As per the recommendation of the review’s authors, it is essential to conduct additional research on the potential relationship between participation construct and contextual factors (i.e. environmental and personal factors). Several studies have explored the predictors of participation in the general CP population via both linear and nonlinear statistical methods (Abu-Dahab et al., 2021; Chiarello et al., 2016; Palisano et al., 2011). Collectively, it has been reported that participation of children with CP is multidimensional and influenced by various child and contextual factors. More specifically, Palisano et al.’s (2011) study using structural model reported that factors of family (e.g., structure and relationships), child (e.g., gross motor function), and service (e.g., processes of service) predicted intensity of participation of children with CP. The study conducted by Abu Dahab et al. (2021) utilized regression analysis showed that manual ability was the only predictor of participation of children with CP. Finally, Chiarello et al. ’s (2016) study using structural model revealed that child factors, such as spasticity, gross motor function, and adaptive behaviors, family factors, including family relationships and social integration, and service factors, including the intensity of therapy and family-centeredness, were all significant predictors of participation in family and recreational activities. Although these findings are valuable, our understanding of the determinants of participation specific to children with unilateral CP is still lacking. Therefore, factors influencing the participation of children with unilateral CP through advanced analytical techniques, such as structural equation modeling (SEM) remain to be determined. SEM differs from regression analysis as it combines path analysis, regression, and factor analysis, enabling the simultaneous examination of the direct and indirect effects of multiple variables (Palisano et al., 2011). Therefore, in the current study, we investigated the potential factors influencing the participation of children with unilateral CP using SEM.
Material and methods
The study protocol was approved by the Ethical Board of the Mus Alparslan University for Non-Invasive Scientific Research (No. 26.11.2021-30766). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. To conduct this study, the authors adhered to the Recommendations for the Conduct, Reporting, Editing, and Publication of Scholarly Work in Medical Journals established by the International Committee of Medical Journal Editors.
Participants
A convenience sample size of 50 children with unilateral CP aged 5–18 years (mean 10.46 y, SD 3.1 y; 27 males and 23 females) were enrolled. All participating children were born in the city of Ankara, located in the middle of Turkey. This sample size was the same as that of an earlier study that performed a path analysis (Kim and Park, 2011). In addition, it adhered to the recommended range of 5–10 participants per predictor variable in SEM (Palisano et al., 2011). Inclusion criteria were being diagnosed with congenital unilateral CP by a physician and having the intellectual capacity to comprehend test items or instructions (moderate- to normal-based on the evaluator’s observation of the child’s behaviors, communication level, and comprehension ability). The exclusion criteria were the presence of severe comorbidities that significantly limited participation in everyday activities (such as visual or hearing impairments or uncontrolled seizures), recent surgical operations that interfered with participation within the last 6 months, and a lack of voluntary consent to participate in the study. After providing detailed information about the study objectives and procedures, written informed consent was obtained from participants aged 7 years and older, as well as from their primary caregivers. For those aged less than years of age, written informed consent was obtained from their primary caregivers only.
Assessment
Classification tools
Fine and gross motor functions of the children in the study were described using the Manual Ability Classification System (MACS) and Gross Motor Function Classification System (GMFCS), while communication performance was defined using the Communication Function Classification System (CFCS).
Factors that may impact the participation of children with unilateral CP and ways to measure them
Spasticity and range of motion
In the assessment of upper limb impairments, the test protocols reported by Klingels et al.(Klingels et al., 2010) were followed. Spasticity was unilaterally evaluated in the muscles of the affected upper limb. The degree of spasticity in the elbow flexor, forearm pronator, and wrist flexor muscles was defined using the Modified Ashworth Scale (MAS). MAS is a prominent and reliable instrument for assessing increased muscle tone in children with CP, utilizing a six-point ordinal scale that ranges from 0 to 4 (Mutlu et al., 2008). An experienced physiotherapist with 8 years of specialization in the CP field quantified spasticity for each child. Additionally, prior to conducting the actual assessment, a workshop was held to enhance the assessor’ accuracy in assessing spasticity. During the assessment of spasticity, each child was asked to lie in a supine position on a therapy bed in a relaxed state. To prevent the asymmetric tonic neck reflex, the child’s head was maintained in midline. Muscle tone was evaluated by manually moving the joint through its entire range of motion and recording the resistance to passive movements while a physiotherapist sat on a chair with a height equal to the therapy bed. The active range of motion (AROM) of elbow extension, forearm supination, and wrist extension with finger extension was assessed using a universal goniometer. When assessing AROM, a dual-physiotherapist approach was employed, with one physiotherapist stabilizing the arm to prevent compensatory movements and the other measuring the joint’s range of motion. Assessment of Range of Motion (ROM) was carried out in a relaxed and comfort position to allow for accurate measurement. For this reason, the position for measuring the ROM in the upper limb joints varied depending on both the joint being assessed and child’s preference. Commonly, assessments were carried out in supine, sitting, and standing positions. In all assessment positions, the children were instructed to extend or rotate actively their joints, depending on the measurement being taken.
Gross motor function
Gross motor function of the participants was assessed using the Turkish Gross Motor Function Measure-88 (GMFM-88). It measures gross motor activities in five dimensions (lying and rolling, sitting, crawling and kneeling, standing, walking, running, and jumping), using a four-point Likert scale. The GMFM-88 was initially designed to assess gross motor function in children with all subtypes of CP (i.e., those with mild-to-severe involvement: hemiplegic, diplegic, and quadriplegic) aged 5 months to 16 years (Russell et al., 1989). Then, it has been demonstrated to be applicable for children aged 3.2–18.1 years with CP (Bjornson et al., 1998) The GMFM-88 has been reported to have good measurement properties in assessing gross motor function in children with CP (Nordmark et al., 1997).
Manual ability
The ABILHAND-Kids questionnaire was employed to assess manual ability, relying on the perspective of families or caregivers regarding their children’s capacity to use their hands for daily activities (i.e., perceived performance). It comprises 21 items designed to assess a child’s performance in managing daily activities outside clinical settings, necessitating the use of one or both hands. The ABILHAND-Kids questionnaire was found to be reliable for assessing the manual ability of Turkish children with CP (good item and model fit) (Şahin et al., 2020).
Mental health
The Strengths and Difficulties Questionnaire (SDQ) was used to describe the availability of mental health problems. The SDQ comprises 25 items that are equally distributed across five subtests: emotional symptoms, conduct problems, hyperactivity inattention, peer problems, and prosocial behavior. The SDQ has been reported to be reliable in identifying the mental health of Turkish children aged 4–17 years (Güvenir et al., 2008).
Environmental factors
Environmental factors were evaluated using the European Child Environment Questionnaire (ECEQ). The ECEQ was developed by the SPARCLE group (Study of Participation of Children with CP) to quantify the availability of essential environmental features in the physical, social, and attitudinal aspects of the home, school, and community environments. The Turkish version of the ECEQ has good psychometric properties, including validity and reliability, in children with CP (Çankaya et al., 2022).
Participation
The Child and Adolescent Scale of Participation (CASP) was utilized to assess the degree of children’s participation in activities within the home, school, and community settings CASP has been validated for Turkish individuals with different types of disabilities and has been shown to be reliable (Atasavun Uysal et al., 2018).
Structural equation modeling
SEM is a sophisticated statistical technique that integrates correlation, bivariate, and multiple linear regression, factor analysis, and path analysis, enabling the examination and assessment of multivariate models. SEM facilitates the estimation of the relationships among multiple interrelated variables within a unified analytical framework. Therefore, SEM is a combination of measurement and structural models. The measurement model indicates associations between observed variables and the construct variables and is tested via Confirmatory Factor Analysis (CFA). In contrast, the structural/path model describes the interrelationships between the construct variables and is tested using path analysis (Weston and Gore Jr, 2006).
Identification of measurement and structural models
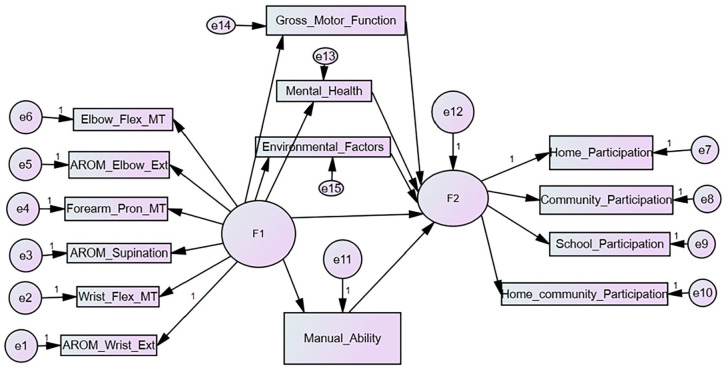
In this study, two distinct measurement models were identified within the SEM: one for upper limb impairment and the other for participation. Figure 1 illustrates the conceptual model of determinants of participation of children with unilateral CP. The measurement model of upper limb impairment incorporated the following indicators: the degree of spasticity in the muscles of the elbow flexors, forearm pronators, wrist flexors, and AROM of elbow extension, forearm supination, and wrist extension. The measurement model of participation consisted of home, community, school, and home and community participation variables. Following the construction of the measurement model, a preliminary structural/path model was created based on the theoretical framework in the literature (Abu-Dahab et al., 2021; Beckung and Hagberg, 2002; Braendvik et al., 2010; Chiu et al., 2010; Kim and Park, 2011; King et al., 2003; Klingels et al., 2012; Park and Kim, 2013; Park et al., 2011; van der Kemp et al., 2022) (Figure 2). When performing path analysis, we found that the paths from the upper limb impairment construct variable to gross motor function, mental health, and environmental factor variables were not significant. Hence, a definitive structural/path model was formulated after the removal of nonsignificant paths (i.e., the proposed path model) (Figure 3).
Figure 1.
Structural model of determinants of participation of children with unilateral cerebral palsy. Ovals represent the latent variables/constructs that could not be measured directly. Dashed rectangles are the observable variables/indicators of the latent variables/construct. Solid rectangles specify the construct that could be measured directly. Arrows represent the direction of direct and indirect effects.
Figure 2.
The preliminary path model of variables.
AROM_Elbow_Ext: Active Range of Motion of the Elbow Extension; AROM_Supination: Active Range of Motion of the Forearm Supination; AROM_Wrist_Ext: Active Range of Motion of the Wrist Extension; Elbow_Flex_MT: Elbow Flexor Muscle Tone; F1: Upper Limb Impairment; F2: Participation; Forearm_Pron_MT: Forearm Pronator Muscle Tone; Wrist_Flex_MT: Wrist Flexors Muscle Tone.
Figure 3.
The proposed path model of variables.
AROM_Elbow_Ext: Active Range of Motion of the Elbow Extension; AROM_Supination: Active Range of Motion of the Forearm Supination; AROM_Wrist_Ext: Active Range of Motion of the Wrist Extension; Elbow_Flex_MT: Elbow Flexor Muscle Tone; F1: Upper Limb Impairment; F2: Participation; Forearm_Pron_MT: Forearm Pronator Muscle Tone; Wrist_Flex_MT: Wrist Flexors Muscle Tone.
Data analysis
IBM SPSS version 25.0 (SPSS Statistics for Windows, Version 25.0. IBM Corporation, Armonk, New York, United States) software package program was used to summarize the demographic data. SEM was executed in two steps using IBM SPSS AMOS version 20.0 (SPSS AMOS for Windows, Version 20.0. IBM Corporation, Armonk, New York, United States). Initially, measurement models of upper limb impairment and participation were established through the application of CFA. The proposed structural/path model of upper limb impairment, manual ability, gross motor function, mental health, environmental factors, and participation was tested using path analysis. Goodness-of-fit indices were investigated to determine whether the proposed path model fitted the collected data. Although there is still no consensus on which types of goodness-of-fit indices should be used to report model fit in the SEM, we chose to use the following goodness-of-fit indices in accordance with Brown’s (Brown, 2015) triad classification: absolute fit indices (X2/df and Standardized Root Mean Square Residual (SRMR), Goodness-of-Fit Index (GFI), Adjusted Goodness-of-Fit Index (AGFI)), parsimony fit indices (Root Mean Square Error of Approximation (RMSEA)), and incremental fit index (CFI). The following threshold values were defined for goodness-of-fit indices to determine if the proposed path model fitted the data collected from children with unilateral CP: X2/df: 3 < X2/df < 5, RMSEA < 0.08, SRMR: <0.08, CFI: >0.90, GFI: >0.90, AGFI: >0.90.
Results
Demographic and clinical characteristics of the study participants were presented in Table 1.
Table 1.
Demographic and clinical characteristics of the study participants (N = 50).
| Variable | M ± SD | Range |
|---|---|---|
| Age | 10.46 ± 3.1 | 5–18 |
| n | % | |
| Gender, n (%) | ||
| Male | 27 | 54 |
| Female | 23 | 46 |
| Affected side | ||
| Right | 27 | 54 |
| Left | 23 | 46 |
| School status | ||
| Special education | 19 | 38 |
| Mainstream/regular school | 31 | 62 |
| Intellectual disability | ||
| Moderate | 11 | 22 |
| Mild | 17 | 34 |
| No | 22 | 44 |
| MACS | ||
| I | 24 | 48 |
| II | 17 | 34 |
| III | 9 | 18 |
| GMFCS | ||
| I | 26 | 52 |
| II | 20 | 40 |
| III | 4 | 8 |
| CFCS | ||
| I | 26 | 52 |
| II | 12 | 24 |
| III | 12 | 24 |
CFCS: Communication Function Classification System; GMFCS: Gross Motor Function Classification System; M: Mean; MACS: Manual Ability Classification System; SD: Standard Deviation.
Results of measurement model
The estimates of the standardized regression weights in the proposed model are presented in Table 2 and illustrated in Figure 2. The regression weights from indicators to upper limb impairment construct were found to be significant (p < 0.001). The results of the study showed that increased active elbow extension (β = 0.83), active elbow supination (β = 0.97), and active wrist extension (β = 0.78), along with reduced wrist flexor spasticity (−0.68), forearm pronator spasticity (β = −0.73), and elbow flexor spasticity (β = −0.44) were necessary for greater upper limb functions. That is, the measurement model of upper limb impairment indicated that the AROM of wrist extension, forearm supination, elbow extension, as well as degree of wrist flexor spasticity, forearm pronator spasticity, and elbow flexor spasticity were all significant indicators of upper limb impairment. Among these, limitations in the AROM of forearm supination (β = 0.97) and elbow extension (β = 0.83) emerged as the most significant indicators of upper limb impairment.
Table 2.
Standardized regression weights of the indicators of the upper limb impairment and participation construct/latent variables.
| Indicator | Construct/latent variable | Estimate (β) | S.E. | C.R. | p | |
|---|---|---|---|---|---|---|
| Active wrist extension | ← | Upper limb impairment | 0.78 | 0.045 | −2345 | *** |
| Wrist flexor spasticity | ← | Upper limb impairment | −0.68 | 0.067 | −6637 | *** |
| Active forearm supination | ← | Upper limb impairment | 0.97 | 0.024 | 35,778 | *** |
| Forearm pronator spasticity | ← | Upper limb impairment | −0.73 | 0.191 | −7562 | *** |
| Active elbow extension | ← | Upper limb impairment s | 0.83 | 0.167 | 10,575 | *** |
| Elbow flexor spasticity | ← | Upper limb impairment | −0.44 | 0.004 | −3449 | *** |
| Home Participation | ← | Participation | 0.85 | 0.065 | 10,768 | *** |
| Community Participation | ← | Participation | 0.87 | 0.095 | 7808 | *** |
| School Participation | ← | Participation | 0.91 | 0.086 | 8252 | *** |
| Home and community Participation | ← | Participation | 0.50 | 0.224 | 3655 | *** |
C.R: Critical Ratio; S.E: Standard Error.
p < 0.001.
Result of structural/path model
Path analysis revealed that upper limb impairment, manual ability, mental health, and environmental factors would all influence the participation of children with unilateral CP. Standardized β weights were significant (p < 0.001) for direct paths between upper limb impairment (β = −0.41), manual ability (β = 0.69), gross motor function (β = 0.24), mental health (β = −0.36), environmental factors (β = −0.42), and participation. Less upper limb impairment, higher manual ability, greater gross motor function, better mental health, and reduced environmental barriers have all been found to correlate with increased participation outcomes. Additionally, upper limb impairment had both direct (β = −0.41; p < 0.001) and indirect (β = 0.64; p < 0.001) effects on participation (Table 3). This suggests that the manual ability variable partially mediates the relationship between upper limb impairment and participation. Collectively, upper limb had a total effect of 0.93 (p < 0.001) on participation.
Table 3.
Standardized direct, indirect, and total effects of the variables.
| Predictor variable | Endogenous/dependent variable | Direct effect (β) | Indirect effect (β) | Total effect (β) |
|---|---|---|---|---|
| Upper limb impairment | Manual ability | 0.93 | — | 0.93 |
| Upper limb impairment | Participation | −0.41 | 0.64 | 0.23 |
| Manual ability | Participation | 0.69 | — | 0.69 |
| Gross motor function | Participation | 0.24 | — | 0.24 |
| Mental health | Participation | −0.36 | — | −0.36 |
| Environmental factors | Participation | −0.42 | — | −0.42 |
Model fit
As outlined in Table 4, the proposed path model of potential factors affecting the participation of children with unilateral CP showed a good model fit (X2/df = 3.543), indicating that the proposed path model fitted the data collected from the study sample (RMSEA = 0.053; SRMR = 0.024; CFI = 0.93; GFI = 0.96; AGFI = 0.91).
Table 4.
Goodness of fit indices of the structural equation modeling.
| Goodness of fit indices | Good fit | Acceptable value | Model fit |
|---|---|---|---|
| X2/df | <3 | 3 < X2/df<5 | 3.543 |
| RMSEA | <0.05 | <0.08 | 0.053 |
| SRMR | <0.05 | <0.08 | 0.024 |
| CFI | >0.95 | >0.90 | 0.93 |
| GFI | >0.95 | >0.90 | 0.96 |
| AGFI | >0.95 | >0.90 | 0.91 |
AGFI: Adjusted Goodness-of-Fit Index; CFI: Comparative Fit Index; GFI: Goodness-of-Fit Index; RMSEA: Root Mean Square Error of Approximation; SRMR: Standardized Root Mean Square Residual.
Discussion
This study employed SEM to investigate potential factors affecting the participation level of children with unilateral CP. The measurement model revealed that the degrees of active forearm supination and elbow extension were the most significant indicators of upper limb impairments. Subsequently, path analysis showed that upper limb impairment accounted for a significant portion of the variance in manual ability. Path analysis showed that upper limb impairment had both direct and indirect impacts on participation, while gross motor function had only direct effects on participation. Most importantly, contextual factors, including mental health and environmental factors, considerably predicted the participation of children with unilateral CP.
It is well established that spasticity in the upper extremities is prevalent in CP (Chaleat-Valayer et al., 2017) and is strongly associated with decreased joint movements (Hedberg-Graff et al., 2019), thus leading to reduced upper limb functions (Klingels et al., 2012). A study by Braendvik et al. (2010) documented that spasticity in the elbow flexors and forearm supinator, and active supination and elbow extension ranges were effective body function measures of the upper limb, corroborating our findings. Previous cross-sectional studies have reported that limitations in AROM of elbow extension, wrist extension, and forearm supination are common in the CP population (Klingels et al., 2012) and that each of these parameters is closely related to upper limb functions (Park et al., 2011). Moreover, some studies have demonstrated that contractures, especially in elbow and wrist flexion, are prevalent in children with CP and typically manifest around the age of 10 years (Hedberg-Graff et al., 2019; Makki et al., 2014).
Path analysis revealed a strong positive correlation between ICF’s activity domain (manual ability and gross motor function) and participation, implying that children with higher manual ability and gross motor function were more likely to participate in a wider range of daily activities. This result was expected. The relationship between gross motor function and participation was unexpectedly weaker than the relationship between manual ability and participation, despite the fact that gross motor function has been reported to be a crucial factor for participation in children with CP (Kim and Park, 2011). This result can be attributed to the fact that most items in the CASP require upper limb and hand use. The close relationship between ICF’s personal factors (i.e., mental health) and participation suggests that children with better mental health tend to have greater participation outcomes. Our findings were consistent with the study by Ramstad et al. (2012) reporting that mental health issues of a severe nature are associated with decreased participation outcomes. Additionally, the current study indicated that ICF’s environmental factors exert a substantial direct influence on the participation, highlighting the need for environmental adjustments to improve participation outcomes of children with unilateral CP. This was substantiated by prior systematic reviews (Mihaylov et al., 2004; van der Kemp et al., 2022), documenting a close linear correlation between environmental factors and the participation.
The ICF enables researchers or clinicians to consider beyond the disability and functioning of the child, while examining the factors affecting participation of children with CP. This is in line with the ICF model that participation is influenced by multiple factors, such as individual, family, environmental, and services received. The interrelationship between outcomes at ICF’ disability and functioning components (i.e., body function, activity, and participation) has been comprehensively established in previous studies (Sakzewski et al., 2010; Wright et al., 2008). However, as indicated in this study, the participation of children with CP is influenced also by ICF’s contextual factors, including mental health and environmental factors. This is consistent with the ICF model, emphasizing the significant role of environmental factors in the participation of children with CP. Thus, modifying environmental factors may potentially enhance participation levels. That is, environmental adjustments could be particularly beneficial in promoting greater participation in various activities. Therefore, establishing an enriched and accessible environment is important for better participation outcomes in children with CP. Likewise, mental health was found to considerably influence the participation of children with unilateral CP. As mental health issues are prevalent in the CP population (Downs et al., 2018), it is imperative to recognize and address mental health issues in children with unilateral CP as a means to enhance their participation outcomes. Although it has been reported previously that there was not a collective consensus of what participation construct is and that the concept of participation is challenging to define and evaluate, Imms et al. (2016) recently established a language to describe participation. They developed five interrelated participation themes and nine subthemes. Among them, environmental factors, activity competence (i.e., gross motor function and manual ability) and sense of self (i.e., mental health well-being) were found to be significantly related to the participation of children with unilateral CP. As a result, active participation in home, school, and community settings plays a crucial role in fostering cognitive, social, physical, and emotional development in children with unilateral CP (Ramstad et al., 2012). Therefore, it is important to consider what is needed to optimize participation outcomes in children with unilateral CP.
Limitations and future research
Although our study’s sample size was consistent with some prior SEM studies and adhered to the recommended guideline of 5–10 participants per estimated parameter, it is important to note that a sample size of 50 participants may be considered relatively small compared to the sample sizes used in other studies. This may be ascribed to the restricted study population and precise inclusion criteria designed exclusively for children with unilateral CP. Therefore, one of the limitations of our study may be primarily related to the sample size. The second limitation may be evaluation of gross motor function using GMFM-88. Although the GMFM-88 was developed to assess gross motor function in children with all subtypes of CP, it is not challenging for children with unilateral CP above the age of 5 to perform the items on the GMFM-88. Consequently, future studies in this area need employ larger sample sizes and utilize more suitable measures of gross motor function, such as the Test of Gross Motor Development.
Conclusion and implications for practice
The measurement model of upper limb impairment showed that spasticity in the wrist flexors, forearm pronators, and elbow flexors, along with limitations in AROM of wrist extension, forearm supination, and elbow extension, were significant impairments of the affected upper limb in children with unilateral CP. Among these, limitations in the AROM of elbow extension and forearm supination were identified as predominant impairments of the affected upper limb. Path analysis revealed the interrelationship between upper limb impairment and manual ability, as well as their relationship with participation. This implies that upper limb impairment has both direct and indirect effects on participation. Furthermore, gross motor function had a direct effect on participation outcomes.
Most importantly, contextual factors, including environmental factors and mental health, had significant direct effects on the participation of children with unilateral CP. This suggests that the participation of children with unilateral CP is influenced not only by the child’s disability and functioning but also by contextual factors. Prior studies have established intercorrelations between body functions/impairments, activity limitations, and participation in the CP population. We also highlighted the significance of mental health and environmental factors in the participation of children with hemiplegia using SEM. Thus, enhancing the participation outcomes of children with unilateral CP also necessitates both improving their mental health and optimizing their physical environments. As a result, children with CP have the same right as their typically developing peers to fully participate in different life situations for their cognitive, social, physical, and emotional development. Therefore, it is imperative for physical and occupational therapists to collaborate with psychologists, psychiatrists, families, and municipal administrators to improve the participation outcomes of children with CP.
Key findings
Environmental factors and mental health exerted a substantial impact on the participation of children with unilateral CP.
Participation of children with unilateral CP is intricately associated with ICF’s main components.
What the study has added
To improve the participation of children with unilateral CP, it is essential for physical and occupational therapists to collaborate with psychologists or psychiatrists, and local government agencies.
Acknowledgments
The authors extend their heartfelt gratitude to the families, service providers, and their respective organizations, whose unwavering commitment and participation in this study were indispensable for its successful completion.
Footnotes
Research ethics: The study protocol was approved by the Ethical Board of the Mus Alparslan University for Non-Invasive Scientific Research (No. 26.11.2021-30766).
Consent: After providing detailed information about the study objectives and procedures, written informed consent was obtained from participants aged 7 years and older, as well as from their primary caregivers. For those aged less than years of age, written informed consent was obtained from their primary caregivers only.
Patient and public involvement data: During the development, progress, and reporting of the submitted research, Patient and Public Involvement in the research was included in the conduct of the research.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) declared no financial support for the research, authorship, and/or publication of this article.
Contributorship: HB and MKG conceived study and wrote the manuscript. HB developed study protocol, gained ethical approval, and conducted statistical analysis. SAS, HF, and EB worked in the field to collect data required. All co-authors examined and revised the manuscript, and then approved the final form of the manuscript.
ORCID iD: Hasan Bingol  https://orcid.org/0000-0003-3185-866X
https://orcid.org/0000-0003-3185-866X
References
- Abu-Dahab SM, Alheresh RA, Malkawi SH, et al. (2021) Participation patterns and determinants of participation of young children with cerebral palsy. Australian Occupational Therapy Journal 68: 195–204. [DOI] [PubMed] [Google Scholar]
- Atasavun Uysal S, Dülger E, Bilgin S, et al. (2018) Investigation of the validity and reliability of the Turkish Child and Adolescent Participation Questionnaire (CASP). Turkish Journal of Physiotherapy and Rehabilitation. Available at: https://dergipark.org.tr/tr/download/issue-full-file/38875 (accessed 15 May, 2022).
- Beckung E, Hagberg G. (2002) Neuroimpairments, activity limitations, and participation restrictions in children with cerebral palsy. Developmental Medicine and Child Neurology 44: 309–316. [DOI] [PubMed] [Google Scholar]
- Bjornson KF, Graubert CS, Buford VL, et al. (1998) Validity of the gross motor function measure. Pediatric Physical Therapy 10: 43–47. [Google Scholar]
- Braendvik SM, Elvrum AKG, Vereijken B, et al. (2010) Relationship between neuromuscular body functions and upper extremity activity in children with cerebral palsy. Developmental Medicine & Child Neurology 52: e29–e34. [DOI] [PubMed] [Google Scholar]
- Brown TA. (2015) Confirmatory Factor Analysis for Applied Research: Guilford Publications. [Google Scholar]
- Cans C. (2000) Surveillance of cerebral palsy in Europe: A collaboration of cerebral palsy surveys and registers. Developmental Medicine & Child Neurology 42: 816–824. [DOI] [PubMed] [Google Scholar]
- Chiarello LA, Bartlett DJ, Palisano RJ, et al. (2016). Determinants of participation in family and recreational activities of young children with cerebral palsy. Disability and Rehabilitation 38: 2455–2468. [DOI] [PubMed] [Google Scholar]
- Chaleat-Valayer E, Bard-Pondarre R, Bernard J, et al. (2017) Upper limb and hand patterns in cerebral palsy: Reliability of two new classifications. European Journal of Paediatric Neurology 21: 754–762. [DOI] [PubMed] [Google Scholar]
- Chiu H-C, Ada L, Butler J, et al. (2010) Relative contribution of motor impairments to limitations in activity and restrictions in participation in adults with hemiplegic cerebral palsy. Clinical Rehabilitation 24: 454–462. [DOI] [PubMed] [Google Scholar]
- Çankaya Ö, Kerem Günel M, Özdemir P. (2022) Construct-concurrent validity and reliability of the European Child Environment Questionnaire (ECEQ) in a sample of Turkish children with cerebral palsy. Disability and Rehabilitation 44: 2104–2112. [DOI] [PubMed] [Google Scholar]
- Dar H, Stewart K, McIntyre S, et al. (2023) Multiple motor disorders in cerebral palsy. Developmental Medicine & Child Neurology 66: 317–325. [DOI] [PubMed] [Google Scholar]
- Downs J, Blackmore AM, Epstein A, et al. (2018) The prevalence of mental health disorders and symptoms in children and adolescents with cerebral palsy: A systematic review and meta-analysis. Developmental Medicine & Child Neurology 60: 30–38. [DOI] [PubMed] [Google Scholar]
- Güvenir T, Özbek A, Baykara B, et al. (2008) Psychometric properties of the Turkish version of the Strengths and Difficulties Questionnaire (SDQ). Turkish Journal of Child and Adolescent Mental Health 15: 65–74. [Google Scholar]
- Hedberg-Graff J, Granström F, Arner M, et al. (2019) Upper-limb contracture development in children with cerebral palsy: A population-based study. Developmental Medicine & Child Neurology 61: 204–211. [DOI] [PubMed] [Google Scholar]
- Imms C, Adair B, Keen D, et al. (2016) ‘Participation’: A systematic review of language, definitions, and constructs used in intervention research with children with disabilities. Developmental Medicine & Child Neurology 58: 29–38. [DOI] [PubMed] [Google Scholar]
- Imms C, Reilly S, Carlin J, et al. (2008) Diversity of participation in children with cerebral palsy. Developmental Medicine & Child Neurology 50: 363–369. [DOI] [PubMed] [Google Scholar]
- Kim WH, Park EY. (2011) Causal relation between spasticity, strength, gross motor function, and functional outcome in children with cerebral palsy: A path analysis. Developmental Medicine & Child Neurology 53: 68–73. [DOI] [PubMed] [Google Scholar]
- King G, Lawm M, King S, et al. (2003) A conceptual model of the factors affecting the recreation and leisure participation of children with disabilities. Physical & Occupational Therapy in Pediatrics 23: 63–90. [PubMed] [Google Scholar]
- Klingels K, De Cock P, Molenaers G, et al. (2010) Upper limb motor and sensory impairments in children with hemiplegic cerebral palsy. Can they be measured reliably? Disability and Rehabilitation 32: 409–416. [DOI] [PubMed] [Google Scholar]
- Klingels K, Demeyere I, Jaspers E, et al. (2012) Upper limb impairments and their impact on activity measures in children with unilateral cerebral palsy. European Journal of Paediatric Neurology 16: 475–484. [DOI] [PubMed] [Google Scholar]
- Makki D, Duodu J, Nixon M. (2014) Prevalence and pattern of upper limb involvement in cerebral palsy. Journal of Children’s Orthopaedics 8: 215–219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mihaylov SI, Jarvis SN, Colver AF, et al. (2004) Identification and description of environmental factors that influence participation of children with cerebral palsy. Developmental Medicine and Child Neurology 46: 299–304. [DOI] [PubMed] [Google Scholar]
- Mutlu A, Livanelioglu A, Gunel MK. (2008) Reliability of Ashworth and modified ashworth scales in children with spastic cerebral palsy. BMC Musculoskeletal Disorders 9: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nordmark E, Hägglund G, Jarnlo G. (1997) Reliability of the gross motor function measure in cerebral palsy. Scandinavian Journal of Rehabilitation Medicine 29: 25–28. [PubMed] [Google Scholar]
- Novak I. (2014) Evidence-based diagnosis, health care, and rehabilitation for children with cerebral palsy. Journal of Child Neurology 29: 1141–1156. [DOI] [PubMed] [Google Scholar]
- Palisano RJ, Chiarello LA, Orlin M, et al. (2011) Determinants of intensity of participation in leisure and recreational activities by children with cerebral palsy. Developmental Medicine & Child Neurology 53: 142–149. [DOI] [PubMed] [Google Scholar]
- Park E-Y, Kim W-H. (2013) Structural equation modeling of motor impairment, gross motor function, and the functional outcome in children with cerebral palsy. Research in Developmental Disabilities 34: 1731–1739. [DOI] [PubMed] [Google Scholar]
- Park ES, Sim EG, Rha D-W. (2011) Effect of upper limb deformities on gross motor and upper limb functions in children with spastic cerebral palsy. Research in Developmental Disabilities 32: 2389–2397. [DOI] [PubMed] [Google Scholar]
- Ramstad K, Jahnsen R, Skjeldal OH, et al. (2012) Parent-reported participation in children with cerebral palsy: The contribution of recurrent musculoskeletal pain and child mental health problems. Developmental Medicine & Child Neurology 54: 829–835. [DOI] [PubMed] [Google Scholar]
- Russell DJ, Rosenbaum PL, Cadman DT. (1989) The gross motor function measure: A means to evaluate the effects of physical therapy. Developmental Medicine & Child Neurology 31: 341–352. [DOI] [PubMed] [Google Scholar]
- Sakzewski L, Ziviani J, Boyd R. (2010) The relationship between unimanual capacity and bimanual performance in children with congenital hemiplegia. Developmental Medicine & Child Neurology 52: 811–816. [DOI] [PubMed] [Google Scholar]
- Şahin E, Dilek B, Karakaş A, et al. (2020) Reliability and validity of the Turkish version of the ABILHAND-kids survey in children with cerebral palsy. Turkish Journal of Physical Medicine and Rehabilitation 66: 444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van der Kemp J, Ketelaar M, Gorter JW. (2022) Environmental factors associated with participation and its related concepts among children and youth with cerebral palsy: A rapid review. Disability and Rehabilitation 44: 1571–1582. [DOI] [PubMed] [Google Scholar]
- Weston R, Gore PA., Jr (2006) A brief guide to structural equation modeling. The Counseling Psychologist 34: 719–751. [Google Scholar]
- Wiklund LM, Uvebrant P. (1991) Hemiplegic cerebral palsy: Correlation between CT morphology and clinical findings. Developmental Medicine & Child Neurology 33: 512–523. [DOI] [PubMed] [Google Scholar]
- Wright FV, Rosenbaum PL, Goldsmith CH, et al. (2008) How do changes in body functions and structures, activity, and participation relate in children with cerebral palsy? Developmental Medicine & Child Neurology 50: 283–289. [DOI] [PubMed] [Google Scholar]