Abstract
Purpose of review
Technological innovations and clinical research in SEEG have dramatically increased with its worldwide dissemination. In this review, we summarize the main advances in the field from the last 5 years.
Recent findings
Several large series and meta-analyses have provided consistent data regarding a lower risk of serious complications with SEEG as compared to sub-dural grids, while some studies also suggest a greater diagnostic value. The safety and precision of SEEG partly depends on the type of vascular imaging and method of implantation, with some series suggesting that MR angiography might not provide an optimal delineation of electrode–vessel conflicts and that frameless stereotaxy lacks precision. Noninvasive frame coupled with robot-guided implantation might offer the best precision/invasiveness tradeoff. Small series suggest that SEEG can be safely performed from the age of 16 months, and that adding electrodes during SEEG often prove beneficial. Transhemispheric electrodes targeting the mesial frontal structures, bilaterally, proved safe and informative. Several interictal and ictal biomarkers of the epileptogenic zone have been investigated. Although high-frequency oscillations (HFOs) remain a biomarker of interest, a randomized controlled trial failed to demonstrate its diagnostic value against spikes. Furthermore, other interictal biomarkers proved to better correlate with the epileptogenic zone than HFOs rate, including spike-gamma and spike-ripples. Ictal biomarkers of interest include the so-called chirp and epileptogenic zone fingerprint. Overall, recent data suggest that high-frequency activities are not a mandatory feature of interictal and ictal biomarkers of the epileptogenic zone. Radiofrequency thermocoagulation (RFTC) performed during SEEG investigation have also progressed, with some authors reporting spectacular rates of seizure freedom in patients with localized epileptogenic lesion but also mesial temporal sclerosis. However, a systematic assessment of memory and mental health demonstrated the presence of altered memory and psychiatric complications in a significant proportion of mesial temporal lobe RFTC.
Summary
Progress has been made in the technology and methods used to perform SEEG and RFTC, with the view to increase safety and effectiveness. Several interictal and ictal biomarkers appear promising but still face challenges in their validation and implementation in clinical practice. Future research requires harmonization in the concepts of the seizure onset and epileptogenic zones, and prospective pathology-specific studies.
Keywords: biomarker, epilepsy, epileptogenic zone, radiofrequency thermocoagulation, safety, seizure onset zone, stereoelectroencephalography, stereotaxy, surgery
INTRODUCTION
Stereo-electroencephalography (SEEG), originally developed in the 1950s by Talairach and Bancaud in Paris, has largely remained confined to a few European epilepsy surgery centers for half of a century before rapidly disseminating worldwide during the last 15 years. Accordingly, a 2022 survey of 192 United States tertiary referral epilepsy Centers, 104 of whom responded, showed that 92% of these centers used SEEG, and 76% used it more frequently than sub-dural grids (SDE) [1]. This major expansion of an otherwise old method has promoted technological and methodological innovations as well as SEEG-based clinical research as illustrated in Fig. 1. This review aims at summarizing the main advances and findings reported in the field during the last 5 years, while keeping in sight its remaining challenges and limitations.
FIGURE 1.
Evolution over time of the number of yearly PubMed publications with SEEG or stereo-EEG or stereoelectroencephalography in title.
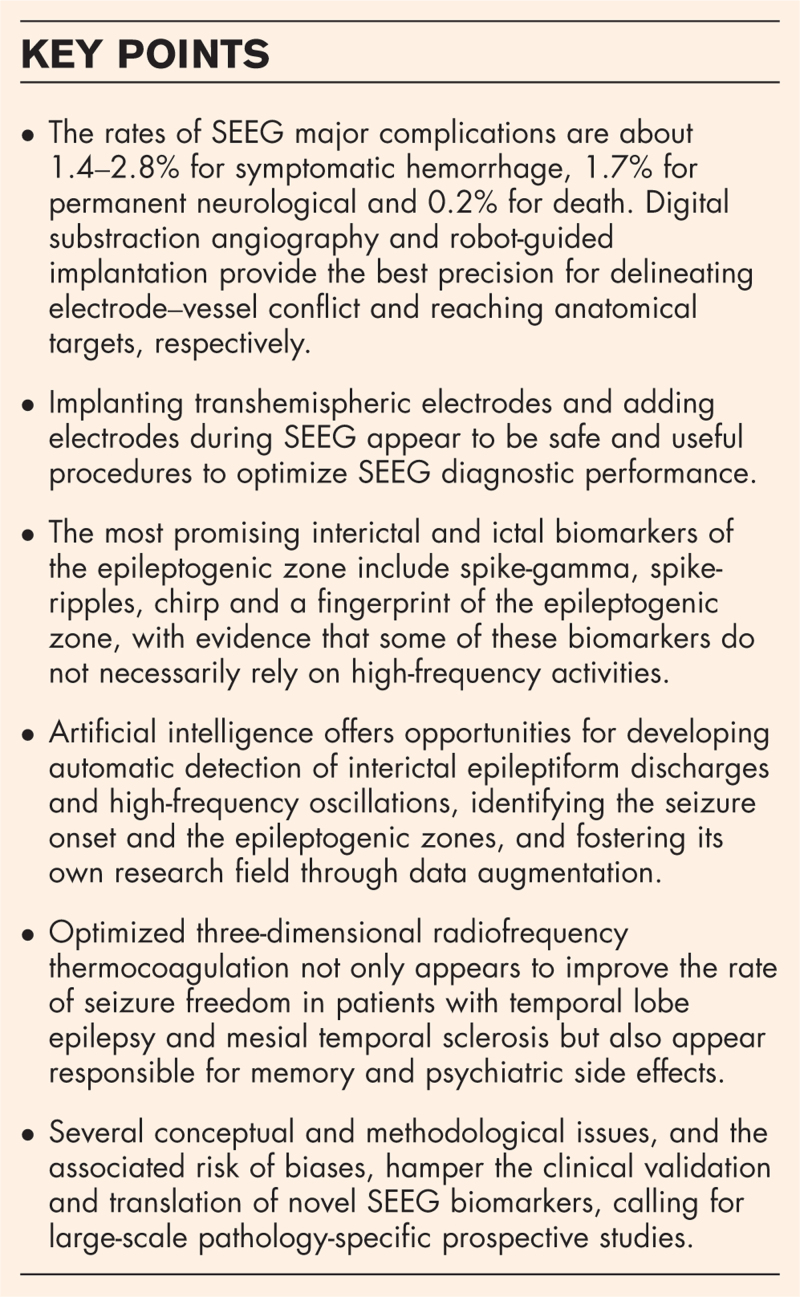
Box 1.
no caption available
STEREO-ELECTROENCEPHALOGRAPHY VERSUS SUB-DURAL GRIDS AND STRIPS ELECTRODES
Several series have compared the rates of complications with SEEG versus sub-dural electrodes (Table 1). None of these were randomized, limiting the robustness of their conclusion, but the largest available study used propensity score matching to mitigate this issue [2]. The series involved 1468 patients from 10 centers and seven countries and found significantly more complications with SDE (9.6%) than SEEG (3.3%) [odds ratio OR = 2.24, 95% confidence interval (CI) 1.34–3.74] [2]. Two smaller series, involving 500 and 176 patients, respectively, reported comparable findings, yet not reaching statistical significance [3,4]. Overall, the risk of symptomatic hemorrhage ranges between 1.4 and 2.8% with SEEG [2,3–8], and between 1.4 and 3.7% with SDE [2,4,9], while that of infection ranges between 0 and 0.9% with SEEG [2,3–6], and between 2.2 and 7% with SDE [2,4,9]. Incidence of transient neurological deficit is more variable across series but can raise up to 2.9% with SEEG [6] and 11.9% with SDE [4,6]. Similar rates of permanent neurological deficit were reported in the largest series comparing SEEG (1.7%) and SDE (1.6%) [2], whereas a previous meta-analysis of SEEG complications reported a 0.4% rate of such deficit [5]. Pediatric series have also reported more transfusion with SDE (13–20%) than with SEEG (0%) [10,11]. The risk of death with both methods can be estimated at 0.2% (see Table 1) [5,9].
Table 1.
Risks of complications of stereo-electroencephalography versus subdural grids and strips according to the largest and most recent series and meta-analyses
| Number of patients | Symptomatic hemorrhage | Infection | Transient deficit | Permanent deficit | Death | |||||||
| SDE | SEEG | SDE | SEEG | SDE | SEEG | SDE | SEEG | SDE | SEEG | SDE | SEEG | |
| Largest noncomparative meta-analyses | ||||||||||||
| Arya et al. 2013 [9] | 2452 (G) | – | 1.4% | – | 5.3% | – | 4.6% | – | NA | – | 0.2% | – |
| Mullin et al., 2016 [5] | – | 2624 | – | 1.5% | – | 0.8% | – | 0.4% | – | 0.4% | – | 0.2% |
| Large studies comparing SDE versus SEEG (N > 150) | ||||||||||||
| Jehi et al., 2021 [2]a | 942 (G) | 526 | 1.8% | 1.6% | 7,0% | 0.9% | NA | NA | 1.6% | 1.7% | 0.1%a | |
| Joswig et al., 2020 [3] | 355 (S) | 145 | 1.4% | 2.8% | 2,3% | 0.0% | 1.1% | 0.7% | 0.6% | 1.4% | 0 | 0.7% |
| Remick et al., 2022 [4] | 134 (G) | 42 | 3.7% | 2.4% | 2,2% | 0.0% | 11.9% | 2.4% | 0.0% | 0.0% | 0 | 0 |
| Other recent large SEEG studies (N > 50) | ||||||||||||
| McGovern et al., 2019 [6] | – | 549 | – | 2.2% | – | 0.7% | – | 2.9% | – | 0.4% | – | 0.2% |
| Agashe et al., 2023 [7] | – | 201 | – | 2.0% | – | NA | – | NA | – | 0 | – | 0 |
| Stefanelli et al., 2022 [8] | – | 72 | – | 1.4% | – | NA | – | NA | – | 0 | – | 1.1% |
NA, not available; SDE, sub-dural grids (G) and strips (S); SEEG, stereo-electroencephalography.
This study used propensity score matching to mitigate potential bias due to the lack of randomization between groups and pooled mortality data from both groups.
Although the proportion of patients undergoing epilepsy surgery is lower following SEEG than grids [2], that of postoperative seizure freedom was reported to be significantly higher with SEEG, with an OR of 1.66 (95% CI 1.21–2.26) in propensity-matched resected patients [2]. Smaller series did not report such significant findings, but numerical differences always favored SEEG over SDE [3,4,10,12].
STEREOTACTIC METHODS
Various methods are being used to visualize intracranial vessels and implant SEEG electrodes, with some differences reported in their respective safety and precision.
Although gadolinium-enhanced MRI has replaced angiography in many SEEG centers, with data showing similar rates of hemorrhage with both methods [13], some recent series suggests that magnetic resonance imaging (MR) angiography might not offer an optimal delineation of intracranial vessels. One such series found that Cone Beam CT Angiography/Venography (CBCT A/V) was superior to MRI in identifying electrode–vessel conflicts, including in patients suffering from a symptomatic hemorrhage at a site where the distance between the electrode and the vessel was less than 1.5 mm [14]. Another series found digital substraction angiography to be superior to both MR angiography and computed tomography angiography (CTA) for detecting such conflicts [15]. DSA-identified electrode–vessel conflicts were also found to be highly predictive of the risk of hemorrhagic complications, with a 94.7% sensitivity [8]. Although the overall rate of hemorrhage was 0.6% per electrode implanted, it raised to 7.2% for electrodes colliding or near-miss a vessel, whereas only 0.37% otherwise [8]. Authors advocating DSA emphasize that its rate of significant complications is currently close to 0, in particular when using a radial artery access [8].
Various methods are being used to implant SEEG electrodes, including the traditional frame-based hand-guided implantation and more recently developed robot-guided and frameless approaches. A 2017 systematic review reported that the mean entry point error (EPE) and target point error (TPE) were, respectively, 1.43 and 1.93 mm for frame-based, 1.17 and 1.71 mm for robot-guided and 2.45 and 2.89 mm for frameless SEEG [16]. A more recent meta-analysis of robot versus manually guided SEEG showed a significantly reduced EPE (mean difference −0.57 mm) and operative time with robotic assistance, while no difference was observed in TPE and complication rate [17▪]. Several new studies have evaluated frameless solutions, including the VarioGuide (BrainLAB AG, Munich, Germany) and StealthStation (Medtronic, Minneapolis, USA) technologies. Using the VarioGuide, two series reported mean EPE of 1.96 and 2.7 mm, and mean TPE of 2.47 and 4.6 mm [18,19]. Another series compared frame-based and StealthStation-assisted procedure, showing a greater average Euclidean distance between actual and ideal electrode tip coordinates for the latter, up to 12.5 mm in the hippocampus [20]. Overall, frameless stereotaxy appears less precise than frame-based and robot-guided SEEG, with the advantage of being less invasive [21]. The novel noninvasive Leksell G frame-based fiducial attachment system coupled with robot-guided implantation might offer the best of the two worlds, providing fixed reference points without the need for additional scalp incisions [22▪]. Using this approach in 25 patients with an average of 18 electrodes per patient, the authors reported a mean EPE of 1.03 mm, a mean TPE of 2.26 mm and a mean angular error of 0.03 radian [22▪]. Other technical aspects of electrode implantation can promote its precision. The use of an external stylet enabled to reduce the target radial error and angular deviation as compared with an internal stylet [23]. Optimal skull angle also helps minimizing the entry radial error and TPE, and depends on the method used for implantation, with an optimal angle of 9° for frame-based hand-guided and 16° for robot-assisted SEEG [24].
Other progress in electrodes implantation include expanding the age limit to younger patients, transhemispheric electrodes and two-step SEEG. Two series have reported uncomplicated SEEG in a total of nine children younger than 2 years and as young as 16 months, with accurate mean TPE of 1 and 1.73 mm [25,26]. These findings suggest that the small skull thickness of very young patients might not be a contraindication to SEEG [25,26]. Two series have reported the use of transhemispheric electrodes crossing the midline to explore mesial frontal regions, bilaterally [27▪,28]. One of these series placed 126 such electrodes in 53 patients without any complication [27▪], whereas the other used 19 electrodes in six patients with an average trajectory error of only 0.1–0.17 mm [28]. In patients with suspected mesial frontal lobe seizures of uncertain lateralization, this novel approach enables to optimize symmetrical bilateral spatial sampling while limiting the number of implanted electrodes. Another interesting strategy to improve spatial sampling consists in adding electrodes during the SEEG investigation, based on preliminary recordings. This strategy was tested in two series of 14 patients each, both reporting that 64% of the added electrodes proved clinically useful in delineating the final epileptogenic zone [29▪,30].
INTERICTAL BIOMARKERS OF THE EPILEPTOGENIC ZONE
The quest for interictal biomarkers other than spikes that might enable to delineate the epileptogenic zone remains very active in SEEG, taking advantage of artificial intelligence as discussed in detail farther.
A systematic review of 13 studies focusing on high-frequency oscillations confirmed the potential interest of fast-ripples to delineate the epileptogenic zone, with a pooled sensitivity of 0.8, a pooled specificity of 0.72 and an area under the curve (AUC) of 0.82 [31]. Ripples proved less informative with pooled sensitivity, specificity and AUC of 0.38, 0.9 and 0.75, respectively [31]. However, the first and currently sole randomized controlled trial (RCT) that tested the clinical usefulness of HFOs in guiding epilepsy surgery, proved negative [32▪▪]. In this study, HFOs and spikes were detected during peri-operative electrocorticography and used to guide the extent of surgical resection [32▪▪]. The primary endpoint was the proportion of patients who achieved postoperative seizure freedom [32▪▪]. The study failed to demonstrate that HFOs were not inferior to spikes in guiding surgery towards this objective [32▪▪]. This result raises the possibility that the bulk of studies suggesting that HFOs help delineating the epileptogenic zone might suffer from biases due to their retrospective design. This issue is further discussed in the challenge and limitation section of this article. Yet, because this RCT had some limitations that could account for its negative findings, it does not firmly exclude the potential diagnostic value of HFOs [32▪▪].
Other HFO-related biomarkers have been developed and tested. One series compared relative entropy in the ripple band to the normalized rate of ripples in 39 patients with Engel class 1 postoperative outcome, showing that the former achieved a higher AUROC (0.85) than the latter (0.75) to delineate the epileptogenic zone while being easier to compute [33]. Another multicenter international study that included 109 patients reported that spike-ripples (a combination of epileptiform spikes and ripples) was a more potent biomarker than spikes, spike-gamma, wideband HFOs, ripples and fast-ripples [34▪▪]. The majority of regions displaying spike-ripples were removed in 79% of ILAE class I patients, versus only 69% for spikes and spike-gamma, 45% for ripples and 36% for fast-ripples [34▪▪]. In contrast, spike-gamma (corresponding to spike preceded by gamma activity) were reported as the most reliable biomarker of the epileptogenic zone in another series of 83 patients, with an AUC of 0.75 compared to 0.54 for ripples and 0.56 for the clinically defined seizure onset zone (SOZ) [35▪▪]. Fast-ripples and spike-ripples were not analyzed in this study [35▪▪]. Finally, one study compared the diagnostic value of various frequency bands on a 30 min non-rapid-eyes movements (REM) sleep recording in 50 patients [36]. The area under the precision-recall curve (AUPRC) was comparable for the 1–500 Hz broadband (0.6), frequencies < 45 Hz (0.58) and those > 65 Hz (0.52), suggesting the lack of additional value of HFOs in that context [36].
ICTAL BIOMARKERS OF THE EPILEPTOGENIC ZONE
In contrast to some of the findings reported above, one series reported that ictal biomarkers, and more specifically the epileptogenicity index, outperformed interictal biomarkers in delineating the visually defined epileptogenic zone (precision of 0.70 for epileptogenicity index versus 0.48 for spikes and 0.29 for HFOs) and predicting surgical outcome (P < 0.001 for epileptogenicity index versus nonsignificant for spikes and HFOs) [37]. A nonsignificant improvement in performance was observed when associating spike to the epileptogenicity index analysis [37]. Finally, epileptogenicity index proved superior to connectivity index [37]. Another small series corroborated this latter finding by showing that the normalized ictal power activation of the EEG signal better delineated the SOZ than the ictal mean functional connectivity of every contact with the rest [38]. A detailed review on connectivity biomarkers is published in this edition of the Current Opinion in Neurology[39].
Two specific ictal biomarkers deserved to be emphasized. Firstly, a so-called chirp pattern, corresponding to a high-power fast activity (>80 Hz) that gradually decreased in frequency within 5–10 s, thus resembling the sonographic pattern recorded during birds’ vocalization described as chirp [40]. In a new study of consecutive 176 patients with various causes, computer-assisted spectrographic analysis detected the presence of chirp in 95.4% of patients and showed that this biomarker correlated with the visually defined epileptogenic zone and predicted surgical outcome [41▪]. Second, a fingerprint of the epileptogenic zone has been identified as a combination of preictal spikes, fast oscillatory activity at seizure onset and concurrent suppression of lower frequencies [42]. A follow-up evaluation of that fingerprint in an independent population of 24 patients showed that this pattern could be extended to lower frequency oscillatory activity (e.g. beta frequencies) with comparable diagnostic value [43]. In patients rendered seizure-free by surgery, 89% of contacts showing the fingerprint were resected, whereas in patients with postoperative seizures, only 27% of these contacts were resected [43].
Finally, one series evaluated a peri-ictal biomarker based on permutation entropy and its evolution between the ictal and postictal period [44]. At each recording site and in each brain region, an index was calculated from the maximal ictal permutation entropy and the minimal postictal permutation entropy [44]. This permutation entropy index proved to be maximal in the epileptogenic zone, to correlate with the connectivity epileptogenicity index methods and to best perform in patients with slow seizure-onset patterns [44].
RADIOFREQUENCY THERMOCOAGULATION
Radiofrequency thermocoagulation (RFTC), typically performed at the end of SEEG investigations, has gained popularity during the last decade, leading to the publication of several new series.
A 2018 systematic review of six studies and 296 patients has reported an overall 50% responder rate of 58% and seizure-free rate of 23% at 1 year [45]. The greater seizure-free rate (38%) was observed in periventricular neuronal heterotopia (PVNH), while the worst results were reported in temporal lobe epilepsy (TLE) [45–47]. Accordingly, one recent series of 62 RFTC reported a global seizure-free rate of 19% and found that response to RFTC predicted the success rate of temporal lobe surgery [48].
Interestingly, most other recent series have reported significantly higher rates of seizure freedom, in particular in PVNH (up to 75%), focal cortical dysplasia (FCD) (up to 67%) and for SOZ that could be fully coagulated (50%) [49,50]. More surprisingly, three series, totaling 72 patients, have reported high seizure-freedom rates of 70–76% at 1 year, in patients with TLE and mesial temporal sclerosis [49,51,52]. However, it should be noted that the proportion of Engel class I outcome dropped from 72,4% at 12 months to 42,9% at 5 years in one of these series [52]. Interestingly, two of these three studies used novel procedures likely to increase the volume of thermocoagulated tissue within the hippocampus, which could account for the improved outcome. In one study, both orthogonal electrodes and a longitudinal electrode parallel to great axis of the hippocampus were implanted in the mesial temporal region and thermocoagulated [51]. Another series used a two-step procedure by performing RFTC at both 2 and 3 weeks following the implantation [52]. The second procedure included a 3D thermocoagulation performed between contacts of adjacent electrodes [52]. RFTC also appears appropriate for the difficult to operate insular epilepsies, with 40% patients achieving an ILAE class 1 outcome, and another 30% an ILAE class 2 outcome in a small series of 10 patients [53].
Although RFTC carries less risks than open surgery, it can still be associated with some complications. A systematic review reported the occurrence of a neurologic deficit in 2.5% of 296 patients [45]. With one exception, these deficits were anticipated and accepted, in order to thermocoagulate an epileptogenic zone localized in an eloquent brain region [45]. However, one series reported a higher rate of neurological deficit (12%), including one permanent, the majority of which were not anticipated [48]. Recent data also point to the possibility of cognitive and psychiatric adverse events [54▪,55▪]. In one series, RFTC in the temporal lobe was associated with decreased verbal memory performance in 20% of patients when performed on the dominant side, and 7% when performed on the nondominant side, with both procedures resulting in altered visual memory performance in 10% of patients [55▪]. Another series of 164 patients reported not only the occurrence of altered memory following RFTC of the amygdala or hippocampus but also significant psychiatric side-effects in 4.2% of patients [54▪]. Finally, most patients appear to experience discomfort during RFTC procedures, which might at times culminate into pain [49].
ARTIFICIAL INTELLIGENCE FOR STEREO-ELECTROENCEPHALOGRAPHY DATA ANALYSIS
Artificial intelligence is particularly well adapted to the analysis of SEEG data and their complex spatiotemporal characteristics. Accordingly, artificial intelligence-based SEEG research is rapidly expanding, offering opportunities to tackle the many challenges still faced in the interpretation of SEEG data.
Machine learning has demonstrated significant effectiveness in detecting spikes in SEEG recordings, particularly through convolutional neural networks (CNNs) [56–58]. For instance, one study involving 46 patients and 13 959 annotated mesial temporal epileptiform discharges reported an AUC of 0.996, a sensitivity of 84%, and a false-positive rate of 1/min [57]. Notably, approximately one-third of false-positive detections were later confirmed as true interictal epileptiform discharges (IEDs) that had been overlooked during expert annotation [57]. Another study utilized 2490 2 s SEEG epochs (with and without IEDs) from 307 patients, transforming these into spectrograms before training a CNN model combined with a template-matching algorithm [58]. This approach detected 100% of all high-amplitude IEDs and 66.15% of atypical morphology IEDs in an external test set [58]. Other machine learning algorithms, including convolutional nonnegative matrix factorization (NNMF) and long short-term memory (LSTM) neural networks, have also achieved high sensitivity and specificity for SEEG spike detection [59–61]. To address clinical needs, automated spike detection algorithms must ultimately differentiate and quantify the diverse types and localizations of IEDs observed in SEEG recordings, a functionality that remains under development and requires validation.
A critical goal of artificial intelligence-based interictal SEEG analysis is to detect HFOs and distinguish between physiological and pathological types [62–65]. Criteria for classifying HFOs as pathological include the presence of associated spikes and the beneficial effect of removing such HFOs on postoperative seizure outcomes [63]. In contrast, HFOs generated by eloquent cortex are often physiological [62]. Studies using weakly supervised deep-learning algorithms on subdural recordings from pediatric patients have addressed these issues [62,63,65]. For example, a model trained on 12 958 annotated HFOs achieved 86.5% accuracy in distinguishing HFOs with or without spikes, facilitating extensive automatic annotation for further analysis [63]. Among patients achieving postoperative seizure freedom, HFOs in the epileptogenic zone were frequently associated with spikes (79%) and exhibited distinct time–frequency characteristics [63], unlike HFOs from eloquent cortex, which were rarely associated with spikes (23%) [62]. These insights improved models predicting postoperative seizure outcomes based on the volume of HFO-generating tissue removed [62,63,65].
Artificial intelligence has emerged as a promising tool for identifying the SOZ and the epileptogenic zone, leveraging hidden EEG features associated with epileptogenic regions. Various methods, including wavelet transformations and support vector machines (SVM), have analyzed ictal and interictal SEEG data and corticocortical-evoked potentials (CCEPs). This has led to the discovery of the previously discussed fingerprint of epileptogenic zone fingerprint, through the identification of a specific interictal-to-ictal transitions [42]. Using only interictal SEEG data, machine learning classifiers (primarily SVMs) have reported AUCs ranging from 0.73 to 0.95, with non-REM sleep providing the most informative data in some studies [66–69]. In CCEP studies, logistic regression applied to features from 50 SEEG patients achieved AUCs of 0.88–0.93.16 Similarly, CNNs trained on 500 000 poststimulation epochs from 10 TLE patients reported 78% sensitivity and 75% specificity in localizing SOZ [70].
Machine learning has also been used to characterize seizure spread across SEEG channels, revealing patterns linked to postoperative outcomes [71]. Furthermore, machine learning techniques, such as data augmentation, have enriched artificial intelligence research datasets by reducing the need for manual annotations and balancing normal versus abnormal epochs [72–74]. For instance, one method (EEGAug) generated new minority-class epochs by combining frequency bands from different samples [73]. Among various oversampling and undersampling strategies, random undersampling (RUS) emerged as the most robust for improving classifier performance [74].
PENDING CHALLENGES AND LIMITATIONS IN STEREO-ELECTROENCEPHALOGRAPHY-BASED RESEARCH
Although SEEG-based research has dramatically expanded during the last decade, progress in its clinical practice has remains limited, in particular regarding the delineation of the epileptogenic zone. Systematic issues and biases in the methods used to develop and validate novel SEEG biomarkers might be responsible for a lack of translation in clinical practice.
The foremost issue pertains to SEEG spatial sampling. A single SEEG contact captures field potentials generated within a volume of approximately 30 mm3. Thus, 12 electrodes with 150 contacts located in the grey matter will sample a total volume of 4.5 cm3, corresponding to roughly 75 million neurons. This accounts for merely 0.5% of the total human cortical brain volume (900 cm3) and neuron count (16 billion). One thus needs to consider the possibility that none of the implanted electrodes are situated within the SOZ, despite being guided by noninvasive presurgical investigations, in particular when dealing with small-size MRI-negative FCD type 2. This necessitates to distinguish the ‘apparent’ SOZ delineated by SEEG from the ‘true’ SOZ. One sophisticated method has been developed to help tackling this issue, based on a previously discussed interictal biomarker, spikes preceded by gamma activity (spike-gamma) [75▪▪]. The model assumes an exponentially decaying rate of spike-gamma with the distance separating recording contacts from the electrode showing the maximal rate, provided that the latter is located in the SOZ [75▪▪]. Its validity was tested by virtually removing each electrode and assessing how the model reacts to this perturbation [75▪▪]. As hypothesized, the model was most strongly altered when removing electrodes from the SOZ [75▪▪]. The authors further used this model to define whether a given SEEG implantation scheme offered an appropriate coverage of the SOZ and found that the model correlated with postoperative outcome [75▪▪].
Another important issue, which directly relates to SEEG spatial sampling and whether the true SOZ was identified, is the definition of the epileptogenic zone. The two primary definitions of the epileptogenic zone suggest that the latter is often larger than the SOZ. Munari and Bancaud [76] have defined the epileptogenic zone as ‘the site of the beginning and the primary organization of the epileptic seizures’. They did not define the term ‘primary organization’, but a general view from SEEG experts is that it encompasses areas of early propagation from the SOZ [77,78]. In contrast, Lüders et al. has defined the epileptogenic zone as ‘the minimum amount of cortex that must be resected (inactivated or completely disconnected) to produce seizure freedom’, further suggesting that it includes the actual SOZ and a potential SOZ [79]. Lüders et al. [79] also stressed that we lack biomarkers of the potential SOZ and evidence that it could correspond to the areas of early seizure propagation. Two recent surveys emphasize the lack of consensus regarding the definition of the epileptogenic zone and SOZ [80,81▪]. The first one collected responses from 321 experts from 39 countries, 68.5% of whom agreed with Lüders's definition of the epileptogenic zone [80]. They were more divided regarding the SOZ, with 55.8% restricting the SOZ to ictal onset proper, while 42.1% included the region of early propagation [80]. The second study was a Delphi survey involving 22 experts from 18 countries who were asked to rate their confidence in the localization of the epileptogenic zone across 42 theoretical scenarios that included MRI and SEEG findings with or without postoperative outcome [81▪]. The overall interrater agreement was poor (0.347), with a substantial level of agreement observed for only 17% of the 42 proposed scenarios [81▪]. Eventually, a consensual rating system could be agreed upon in order to evaluate the robustness of findings in epileptogenic zone-related publication [81▪].
The last issue that likely affects clinical translation of novel SEEG biomarkers is the fact that most studies pool findings from population harboring heterogeneous lesions without providing specific results for each of them. The volume and organization of the epileptogenic tissue, its capacity to generate the various interictal and ictal epileptiform discharges, and its associated postoperative seizure freedom rate vary substantially between pathologies. At one end of the spectrum, FCD type 2 are usually small and well circumscribed lesions with intrinsic epileptogenicity and excellent surgical outcome [82,83]. These lesions typically display the hallmarks of interictal and ictal epileptiform discharges, including spikes, HFOs, spike-ripples, spike gamma, LFVA, and Chirp, with little extension of these abnormalities outside the FCD [83]. Such lesions will necessarily demonstrate a highly significant association with all above biomarkers and the epileptogenic zone, but the latter are not needed to achieve surgical success, which primarily requires a complete resection of the MRI abnormality. Furthermore, there is a trend to avoid SEEG in patients with typical MRI features of FCD type 2 [83,84]. At the other end of the spectrum, very large FCD type 1 and nonlesional extra-temporal epilepsies pose the greatest presurgical and surgical challenges, with greater likelihood of multifocal and/or network organization of the epileptogenic zone and postoperative seizures. This is thus the population where we most need reliable biomarkers of the epileptogenic zone. Although specific data are lacking in the field, personal experience suggest that FCD type 1 and nonlesional extra-temporal epilepsies are unlikely to display well localized interictal and ictal biomarkers of the epileptogenic zone. Accordingly, pooling these pathologies with FCD type 2 would result in a significant association between the presence of any given biomarkers and their complete removal by surgery with postoperative seizure freedom, but this association would merely reflect the difference in pathology and not necessarily help achieving better surgical results. At the era of large-scale data sharing, we now need to expand SEEG research to very large datasets that will offer sufficient sample size for each specific pathology.
CONCLUSION
With the rapid worldwide dissemination of SEEG, notable innovations and progress have been made in the methods used for implantation, delineation of the epileptogenic zone and radiofrequency thermocoagulation, with the potential to improve safety and seizure outcome. Yet, most of these methods remain to be further tested and validated in larger cohorts while addressing the pending challenges and limitations of SEEG.
Acknowledgements
None.
Financial support and sponsorship
Philippe Ryvlin received funding which contributed to this work by the European Unioni's Horizon Europe programme, grant agreement 101147391 (EBRAINS 2.0 project)
Conflicts of interest
There are no conflicts of interest.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▪ of special interest
▪▪ of outstanding interest
REFERENCES
- 1.Gavvala J, Zafar M, Sinha SR, et al. American SEEG Consortium, supported by The American Clinical Neurophysiology Society. Stereotactic EEG practices: a survey of United States Tertiary Referral Epilepsy Centers. J Clin Neurophysiol 2020; 39:474–480. [DOI] [PubMed] [Google Scholar]
- 2.Jehi L, Morita-Sherman M, Love TE, et al. Comparative effectiveness of stereotactic electroencephalography versus subdural grids in epilepsy surgery. Ann Neurol 2021; 90:927–939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Joswig H, Lau JC, Abdallat M, et al. Stereoelectroencephalography versus subdural strip electrode implantations: feasibility, complications, and outcomes in 500 intracranial monitoring cases for drug-resistant epilepsy. Neurosurgery 2020; 87:E23–E30. [DOI] [PubMed] [Google Scholar]
- 4.Remick M, Akwayena E, Harford E, et al. Subdural electrodes versus stereoelectroencephalography for pediatric epileptogenic zone localization: a retrospective cohort study. Neurosurg Focus 2022; 53:E4. [DOI] [PubMed] [Google Scholar]
- 5.Mullin JP, Shriver M, Alomar S, et al. Is SEEG safe? A systematic review and meta-analysis of stereo-electroencephalography-related complications. Epilepsia 2016; 57:386–401. [DOI] [PubMed] [Google Scholar]
- 6.McGovern RA, Butler RS, Bena J, Gonzalez-Martinez J. Incorporating new technology into a surgical technique: the learning curve of a single surgeon's stereo-electroencephalography experience. Neurosurgery 2020; 86:E281–E289. [DOI] [PubMed] [Google Scholar]
- 7.Agashe S, Brinkmann BH, Cox BC, et al. Implications of intracranial hemorrhage associated with stereo-EEG. Clin Neurophysiol 2023; 155:86–93. [DOI] [PubMed] [Google Scholar]
- 8.Stefanelli A, Sabourin V, Hines K, et al. Digital subtraction angiography may reduce the rate of radiographic hemorrhage in stereoelectroencephalography. World Neurosurg 2022; 164:e964–e969. [DOI] [PubMed] [Google Scholar]
- 9.Arya R, Mangano FT, Horn PS, et al. Adverse events related to extraoperative invasive EEG monitoring with subdural grid electrodes: a systematic review and meta-analysis. Epilepsia 2013; 54:828–839. [DOI] [PubMed] [Google Scholar]
- 10.Talai A, Eschbach K, Stence NV, et al. Comparison of subdural grid and stereoelectroencephalography in a cohort of pediatric patients. Epilepsy Res 2021; 177:106758. [DOI] [PubMed] [Google Scholar]
- 11.Larrew T, Skoch J, Ihnen SKZ, et al. Comparison of outcomes after stereoelectroencephalography and subdural grid monitoring in pediatric tuberous sclerosis complex. Neurosurg Focus 2022; 53:E5. [DOI] [PubMed] [Google Scholar]
- 12.Tandon N, Tong BA, Friedman ER, et al. Analysis of morbidity and outcomes associated with use of subdural grids vs stereoelectroencephalography in patients with intractable epilepsy. JAMA Neurol 2019; 76:672–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McGovern RA, Ruggieri P, Bulacio J, et al. Risk analysis of hemorrhage in stereo-electroencephalography procedures. Epilepsia 2019; 60:571–580. [DOI] [PubMed] [Google Scholar]
- 14.Szmidel M, Hunn M, Neal A, et al. Vascular imaging for stereoelectroencephalography: a safety and planning study. J Clin Neurosci 2024; 127:110762. [DOI] [PubMed] [Google Scholar]
- 15.Delgado-Martínez I, Serrano L, Higueras-Esteban A, et al. On the use of digital subtraction angiography in stereoelectroencephalography surgical planning to prevent collisions with vessels. World Neurosurg 2021; 147:e47–e56. [DOI] [PubMed] [Google Scholar]
- 16.Vakharia VN, Sparks R, O’Keeffe AG, et al. Accuracy of intracranial electrode placement for stereoencephalography: a systematic review and meta-analysis. Epilepsia 2017; 58:921–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17▪.Gomes FC, Larcipretti ALL, Nager G, et al. Robot-assisted vs. manually guided stereoelectroencephalography for refractory epilepsy: a systematic review and meta-analysis. Neurosurg Rev 2023; 46:102. [DOI] [PubMed] [Google Scholar]; This meta-analysis compared the precision of robot-assisted versus hand-guided implantation of SEEG electrodes, showing a greater precision for the former.
- 18.Song S, Dai Y, Chen Z, Shi S. Accuracy and feasibility analysis of SEEG electrode implantation using the VarioGuide Frameless Navigation System in patients with drug-resistant epilepsy. J Neurol Surg A Cent Eur Neurosurg 2021; 82:430–436. [DOI] [PubMed] [Google Scholar]
- 19.Brimley C, Shimony N. Accuracy and utility of frameless stereotactic placement of stereoelectroencephalography electrodes. World Neurosurg 2023; 180:e226–e232. [DOI] [PubMed] [Google Scholar]
- 20.Girgis F, Ovruchesky E, Kennedy J, et al. Superior accuracy and precision of SEEG electrode insertion with frame-based vs. frameless stereotaxy methods. Acta Neurochir (Wien) 2020; 162:2527–2532. [DOI] [PubMed] [Google Scholar]
- 21.Parrott A, Tavakol SA, Zieles K, et al. The evolution of stereoelectroencephalography: symbiotic progress in medical imaging and procedural technologies. J Neurosurg Pediatr 2023; 32:545–552. [DOI] [PubMed] [Google Scholar]
- 22▪.Sharma A, Song R, Sarmey N, et al. Validation and safety profile of a novel, noninvasive fiducial attachment for stereotactic robotic-guided stereoelectroencephalography: a case series. Oper Neurosurg (Hagerstown) 2024; 27:440–448. [DOI] [PubMed] [Google Scholar]; This study tested a novel noninvasive frame for robot-guided SEEG, and showed that it offers an excellent precision, comparable to that of invasive frame.
- 23.Lee SJ, Lee PS, Faraji AH, et al. Implantation accuracy and operative variables in robot-assisted stereoelectroencephalography. J Neurosurg 2023; 139:1598–1603. [DOI] [PubMed] [Google Scholar]
- 24.Du C, Wang L, Yan J, et al. The association between trajectory-skull angle and accuracy of stereoelectroencephalography electrode implantation in drug-resistant epilepsy. World Neurosurg 2024; 184:e408–e416. [DOI] [PubMed] [Google Scholar]
- 25.Rahman RK, Tomlinson SB, Katz J, et al. Stereoelectroencephalography before 2 years of age. Neurosurg Focus 2022; 53:E3. [DOI] [PubMed] [Google Scholar]
- 26.Muh CR, Dorilio JR, Beaudreault CP, et al. Feasibility and safety of stereoelectroencephalography in young children. Childs Nerv Syst 2024; 40:1331–1337. [DOI] [PubMed] [Google Scholar]
- 27▪.Restrepo CE, Balaguera P, Thompson SA, et al. Safety and efficacy of bihemispheric sampling via transmidline stereoelectroencephalography. J Neurosurg 2023; 139:229–237. [DOI] [PubMed] [Google Scholar]; This study assesses the safety and usefulness of transhemispheric electrodes, primarily used to sample the mesial frontal regions, bilaterally, with a single electrode. One hundred and twenty-six transhemispheric trajectories were performed in 53 patients without complications or significant target point error.
- 28.Sharma N, Mallela AN, Abou-Al-Shaar H, et al. Trans-interhemispheric stereoelectroencephalography depth electrode placement for mesial frontal lobe explorations in medically refractory epilepsy: a technical note and case series. Oper Neurosurg (Hagerstown) 2023; 24:582–589. [DOI] [PubMed] [Google Scholar]
- 29▪.Ilyas A, Vilella L, Restrepo CE, et al. The value of additional electrodes when stereo-electroencephalography is inconclusive. Epilepsia 2024; 65:641–650. [DOI] [PubMed] [Google Scholar]; This study tested the diagnostic value of adding electrodes during SEEG and showed that this strategy often improves its diagnostic value.
- 30.Whiting AC, Bulacio J, Whiting BB, et al. Difficult-to-localize epilepsy after stereoelectroencephalography: technique, safety, and efficacy of placing additional electrodes during the same admission. Oper Neurosurg (Hagerstown) 2020; 20:55–60. [DOI] [PubMed] [Google Scholar]
- 31.Wang Y, Xu J, Liu T, et al. Diagnostic value of high-frequency oscillations for the epileptogenic zone: a systematic review and meta-analysis. Seizure 2022; 99:82–90. [DOI] [PubMed] [Google Scholar]
- 32▪▪.Zweiphenning W, Klooster MAV, van Klink NEC, et al. Intraoperative electrocorticography using high-frequency oscillations or spikes to tailor epilepsy surgery in the Netherlands (the HFO trial): a randomised, single-blind, adaptive noninferiority trial. Lancet Neurol 2022; 21:982–993. [DOI] [PMC free article] [PubMed] [Google Scholar]; This is the only randomized controlled trial that tested the capacity of per-operative HFO-guided resection to improve surgical outcome. The study was negative and failed to demonstrate noninferiority as compared to spike-guided resection.
- 33.Travnicek V, Klimes P, Cimbalnik J, et al. Relative entropy is an easy-to-use invasive electroencephalographic biomarker of the epileptogenic zone. Epilepsia 2023; 64:962–972. [DOI] [PubMed] [Google Scholar]
- 34▪▪.Shi W, Shaw D, Walsh KG, et al. Spike ripples localize the epileptogenic zone best: an international intracranial study. Brain 2024; 147:2496–2506. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study compared a number of interictal SEEG biomarkers, and found that spike-ripples best identified the epileptogenic zone.
- 35▪▪.Thomas J, Kahane P, Abdallah C, et al. A subpopulation of spikes predicts successful epilepsy surgery outcome. Ann Neurol 2023; 93:522–535. [DOI] [PubMed] [Google Scholar]; This study compared a number of interictal SEEG biomarkers, and found that spike-gamma resection rate best predict surgical outcome.
- 36.Klimes P, Nejedly P, Hrtonova V, et al. Interictal stereo-electroencephalography features below 45 Hz are sufficient for correct localization of the epileptogenic zone and postsurgical outcome prediction. Epilepsia 2024; 65:2935–2945. [DOI] [PubMed] [Google Scholar]
- 37.Makhalova J, Madec T, Medina Villalon S, et al. The role of quantitative markers in surgical prognostication after stereoelectroencephalography. Ann Clin Transl Neurol 2023; 10:2114–2126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vila-Vidal M, Corominas FC, Gilson M, et al. A comparative study between a power and a connectivity sEEG biomarker for seizure-onset zone identification in temporal lobe epilepsy. J Neurosci Methods 2024; 411:110238. [DOI] [PubMed] [Google Scholar]
- 39.Makhoul GS, Doss DJ, Englot DJ. Can brain network analyses guide epilepsy surgery? Curr Opin Neurol 2025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Gnatkovsky V, Pelliccia V, de Curtis M, Tassi L. Two main focal seizure patterns revealed by intracerebral electroencephalographic biomarker analysis. Epilepsia 2019; 60:96–106. [DOI] [PubMed] [Google Scholar]
- 41▪.Di Giacomo R, Burini A, Chiarello D, et al. Ictal fast activity chirps as markers of the epileptogenic zone. Epilepsia 2024; 65:e97–e103. [DOI] [PubMed] [Google Scholar]; This large study of 176 consecutive SEEG confirmed that a chirp pattern of ictal fast activity best identified the epileptogenic zone and predict surgical outcome.
- 42.Grinenko O, Li J, Mosher JC, et al. A fingerprint of the epileptogenic zone in human epilepsies. Brain 2018; 141:117–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Li J, Grinenko O, Mosher JC, et al. Learning to define an electrical biomarker of the epileptogenic zone. Hum Brain Mapp 2020; 41:429–441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bratu IF, Makhalova J, Garnier E, et al. Permutation entropy-derived parameters to estimate the epileptogenic zone network. Epilepsia 2024; 65:389–401. [DOI] [PubMed] [Google Scholar]
- 45.Bourdillon P, Cucherat M, Isnard J, et al. Stereo-electroencephalography-guided radiofrequency thermocoagulation in patients with focal epilepsy: a systematic review and meta-analysis. Epilepsia 2018; 59:2296–2304. [DOI] [PubMed] [Google Scholar]
- 46.Bourdillon P, Isnard J, Catenoix H, et al. Stereo electroencephalography-guided radiofrequency thermocoagulation (SEEG-guided RF-TC) in drug-resistant focal epilepsy: Results from a 10-year experience. Epilepsia 2017; 58:85–93. [DOI] [PubMed] [Google Scholar]
- 47.Moles A, Guénot M, Rheims S, et al. SEEG-guided radiofrequency coagulation (SEEG-guided RF-TC) versus anterior temporal lobectomy (ATL) in temporal lobe epilepsy. J Neurol 2018; 265:1998–2004. [DOI] [PubMed] [Google Scholar]
- 48.Shields JA, Greven ACM, Shivamurthy VKN, et al. Stereoelectroencephalography-guided radiofrequency ablation of the epileptogenic zone as a treatment and predictor of future success of further surgical intervention. Epilepsia 2023; 64:2081–2093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Liu Q, Cai Y, Mao Z, et al. SEEG-RFTC in patients with refractory focal epilepsy: real-world outcomes from 121 cases. Ann Clin Transl Neurol 2024; 11:1999–2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kreinter H, Espino PH, Mejía S, et al. Disrupting the epileptogenic network with stereoelectroencephalography-guided radiofrequency thermocoagulation. Epilepsia 2024; 65:e113–e118. [DOI] [PubMed] [Google Scholar]
- 51.Fan X, Shan Y, Lu C, et al. Optimized SEEG-guided radiofrequency thermocoagulation for mesial temporal lobe epilepsy with hippocampal sclerosis. Seizure 2019; 71:304–311. [DOI] [PubMed] [Google Scholar]
- 52.Li K, Shi J, Wei P, et al. Stereo-electroencephalography-guided three-dimensional radiofrequency thermocoagulation for mesial temporal lobe epilepsy with hippocampal sclerosis: a retrospective study with long-term follow-up. Epilepsia Open 2024; 9:918–925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Dai Y, Zhang H, Fan X, et al. Optimized SEEG-guided three-dimensional radiofrequency thermocoagulation for insular epilepsy. Acta Neurochir (Wien) 2023; 165:249–258. [DOI] [PubMed] [Google Scholar]
- 54▪.Bregianni M, Pizzo F, Lagarde S, et al. Psychiatric complications following SEEG-guided radiofrequency thermocoagulations in patients with drug-resistant epilepsy. Epilepsy Behav 2024; 156:109806. [DOI] [PubMed] [Google Scholar]; This study found that radiofrequency thermocoagulations in the hippocampus or amygdala can be responsible for memory and psychiatric side effects.
- 55▪.Cockle E, Malpas CB, Coleman H, et al. Neuropsychological outcomes after stereo-EEG radiofrequency thermocoagulation. Neurology 2024; 103:e209815. [DOI] [PubMed] [Google Scholar]; This study performed a systematic assessment of memory performance prior to and following temporal lobe radiofrequency thermocoagulation, and found altered verbal memory in 20% of RFTC performed on the side dominant for language.
- 56.Antoniades A, Spyrou L, Martin-Lopez D, et al. Detection of interictal discharges with convolutional neural networks using discrete ordered multichannel intracranial EEG. IEEE Trans Neural Syst Rehabil Eng 2017; 25:2285–2294. [DOI] [PubMed] [Google Scholar]
- 57.Abou Jaoude M, Jing J, Sun H, et al. Detection of mesial temporal lobe epileptiform discharges on intracranial electrodes using deep learning. Clin Neurophysiol 2020; 131:133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Quon RJ, Meisenhelter S, Camp EJ, et al. AiED: artificial intelligence for the detection of intracranial interictal epileptiform discharges. Clin Neurophysiol 2022; 133:1–8. [DOI] [PubMed] [Google Scholar]
- 59.Baud MO, Kleen JK, Anumanchipalli GK, et al. Unsupervised learning of spatiotemporal interictal discharges in focal epilepsy. Neurosurgery 2018; 83:683–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Medvedev AV, Agoureeva GI, Murro AM. A long short-term memory neural network for the detection of epileptiform spikes and high frequency oscillations. Sci Rep 2019; 9:19374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Geng D, Alkhachroum A, Melo Bicchi MA, et al. Deep learning for robust detection of interictal epileptiform discharges. J Neural Eng 2021; 18:abf28e. [DOI] [PubMed] [Google Scholar]
- 62.Zhang Y, Chung H, Ngo JP, et al. Characterizing physiological high-frequency oscillations using deep learning. J Neural Eng 2022; 19:aca4fa. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zhang Y, Lu Q, Monsoor T, et al. Refining epileptogenic high-frequency oscillations using deep learning: a reverse engineering approach. Brain Commun 2022; 4:fcab267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zhao X, Peng X, Niu K, et al. A multihead self-attention deep learning approach for detection and recommendation of neuromagnetic high frequency oscillations in epilepsy. Front Neuroinform 2022; 16:771965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Monsoor T, Zhang Y, Daida A, et al. Optimizing detection and deep learning-based classification of pathological high-frequency oscillations in epilepsy. Clin Neurophysiol 2023; 154:129–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cimbalnik J, Klimes P, Sladky V, et al. Multifeature localization of epileptic foci from interictal, intracranial EEG. Clin Neurophysiol 2019; 130:1945–1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Klimes P, Cimbalnik J, Brazdil M, et al. NREM sleep is the state of vigilance that best identifies the epileptogenic zone in the interictal electroencephalogram. Epilepsia 2019; 60:2404–2415. [DOI] [PubMed] [Google Scholar]
- 68.Conrad EC, Revell AY, Greenblatt AS, et al. Spike patterns surrounding sleep and seizures localize the seizure-onset zone in focal epilepsy. Epilepsia 2023; 64:754–768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Varatharajah Y, Berry B, Cimbalnik J, et al. Integrating artificial intelligence with real-time intracranial EEG monitoring to automate interictal identification of seizure onset zones in focal epilepsy. J Neural Eng 2018; 15:046035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Johnson GW, Cai LY, Doss DJ, et al. Localizing seizure onset zones in surgical epilepsy with neurostimulation deep learning. J Neurosurg 2023; 138:1002–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pattnaik AR, Ghosn NJ, Ong IZ, et al. The seizure severity score: a quantitative tool for comparing seizures and their response to therapy. J Neural Eng 2023; 20:aceca1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Nejedly P, Kremen V, Lepkova K, et al. Utilization of temporal autoencoder for semi-supervised intracranial EEG clustering and classification. Sci Rep 2023; 13:744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Zhao X, Sole-Casals J, Sugano H, Tanaka T. Seizure onset zone classification based on imbalanced iEEG with data augmentation. J Neural Eng 2022; 19:aca04f. [DOI] [PubMed] [Google Scholar]
- 74.Varotto G, Susi G, Tassi L, et al. Comparison of resampling techniques for imbalanced datasets in machine learning: application to epileptogenic zone localization from interictal intracranial EEG recordings in patients with focal epilepsy. Front Neuroinform 2021; 15:715421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75▪▪.Jaber K, Avigdor T, Mansilla D, et al. A spatial perturbation framework to validate implantation of the epileptogenic zone. Nat Commun 2024; 15:5253. [DOI] [PMC free article] [PubMed] [Google Scholar]; This study developed and tested a framework to evaluate the quality of the coverage of the seizure onset zone by the implanted electrodes. The output of the model correlated with the postoperative seizure outcome
- 76.Munari C, Bancaud J, Porter RJ, Morselli PL. The role of stereo-electroencephalography (SEEG) in the evaluation of partial epileptic seizures. The epilepsies. London: Butterworths; 1985. 267–306. [Google Scholar]
- 77.Kahane P, Landre E, Minotti L, et al. The Bancaud and Talairach view on the epileptogenic zone: a working hypothesis. Epileptic Disord 2006; 8 Suppl 2:S16–S26. [PubMed] [Google Scholar]
- 78.Jehi L. The epileptogenic zone: concept and definition. Epilepsy Curr 2018; 18:12–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Lüders HO, Najm I, Nair D, et al. The epileptogenic zone: general principles. Epileptic Disord 2006; 8 Suppl 2:S1–S9. [PubMed] [Google Scholar]
- 80.Thomas J, Abdallah C, Cai Z, et al. Investigating current clinical opinions in stereoelectroencephalography-informed epilepsy surgery. Epilepsia 2024; 65:2662–2672. [DOI] [PubMed] [Google Scholar]
- 81▪.Ryvlin P, Barba C, Bartolomei F, et al. Grading system for assessing the confidence in the epileptogenic zone reported in published studies: a Delphi consensus study. Epilepsia 2024; 65:1346–1359. [DOI] [PubMed] [Google Scholar]; This Delphi study developed and tested a framework to grade the confidence in the epileptogenic zone reported in scientific publications, in order to harmonize and weigh their outputs in systematic reviews.
- 82.Lamberink HJ, Otte WM, Blümcke I, Braun KPJ. European Epilepsy Brain Bank writing group, study group, European Reference Network EpiCARE. Seizure outcome and use of antiepileptic drugs after epilepsy surgery according to histopathological diagnosis: a retrospective multicentre cohort study. Lancet Neurol 2020; 19:748–757. [DOI] [PubMed] [Google Scholar]
- 83.Chassoux F, Landré E, Mellerio C, et al. Type II focal cortical dysplasia: electroclinical phenotype and surgical outcome related to imaging. Epilepsia 2012; 53:349–358. [DOI] [PubMed] [Google Scholar]
- 84.Chassoux F, Mellerio C, Laurent A, et al. Benefits and risks of epilepsy surgery in patients with focal cortical dysplasia type 2 in the central region. Neurology 2022; 99:e11–e22. [DOI] [PubMed] [Google Scholar]