Abstract
The objective is to compare the feasibility, safety, and complications of the novel robot-assisted system Hugo™ RAS to the established Intuitive da Vinci Xi system in different gynecologic surgeries. This is a retrospective and propensity score-matching study conducted at a tertiary teaching hospital. The participants were women with various indications for gynecologic surgery who underwent robotic procedures. The results of our first 40 cases of gynecologic procedures performed with Hugo™ RAS were compared to those of a 1:3 propensity-matched cohort using the da Vinci Xi system. Length of hospital stay, blood loss, surgical time, console time, and perioperative complications were the main outcome measures. There were no differences in the length of hospital stay, blood loss, and complication rates between the novel Hugo™ RAS and da Vinci Xi system in different gynecologic procedures. However, the surgical time was longer with Hugo™ RAS in the staging of endometrial cancer. The Hugo™ RAS is a feasible and safe robotic platform for different indications in gynecologic surgery.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11701-025-02255-y.
Keywords: da Vinci Xi, Gynecologic surgery, Hugo™ RAS, Robotic surgery
Introduction
Minimally invasive surgery (MIS) has been the mainstay of surgical procedures for most gynecologic diseases, with increasing application of robotic surgery globally, since the introduction of the Intuitive™ da Vinci system in 2003. The surgical platform provides precise manipulation, tremor filtering effects, magnified surgical fields with less blood loss, shorter hospital stays, and rapid recovery [1, 2]. There is a higher incidence of adhesive disease and morbid obesity, and larger uteri with fewer intraoperative complications in the robotic cohort than in the conventional open abdominal hysterectomy and vaginal hysterectomy cohorts, while shorter hospital stays and fewer postoperative complications than in the laparoscopic-assisted vaginal hysterectomy, vaginal hysterectomy, and abdominal hysterectomy cohorts [3].
By 2024, the da Vinci robotic series has dominated the robotic surgical market for almost 20 years, with nearly 9210 platforms installed in 72 countries worldwide. Innovative surgical platforms were introduced into the market in 2019. The Medtronic Hugo™ RAS first gained EU approval in 2021, and 100 platforms have been installed with more than 10,000 procedures having been performed by July 2024 [4–6]. This novel surgical platform is currently used in only seven centers in East Asia for gynecologic procedures by September 2024, including one in Taiwan and all others in Japan. The procedure has been performed in 51 cases in our institute (TTMHH), 23, 14, 26, 68, 6, and 17 cases in Kitasato Institute, Sapporo Medical University, Tottori University Hospital, Yamanashi Pref. Central Hospital, Fujita Medical University, and Kyoto University Hospital, respectively, by August 2024. Clinical studies were announced in the USA by Medtronic in May 2024.
The innovative open console (Fig. 1) enables surgeons to communicate with operating room personnel effortlessly and effectively during the entire procedure. Furthermore, the ergonomic design is more comfortable and fatigue-free for surgeons compared to an immersive console design, especially during a complicated and long surgery. Another key feature is the four independent arm carts, which enable the adjustment of various configurations adaptable to different clinical scenarios and easy movement between different operating rooms, thereby enhancing the versatility of the platform.
Fig. 1.

The open console facilitates direct communication between the surgeon and the operating room personnel, as well as provides a more comfortable posture for the surgeon per se during a long procedure
Few reports on gynecology [7, 8], except the prolapse of the pelvic organ (POP) procedure, using the new surgical platform have been published in the past 2 years [9]. Herein, we described our first 40 cases of Hugo™ RAS procedure in different gynecologic surgeries and compared it to the established Intuitive da Vinci Xi system to evaluate its feasibility, safety, and perioperative results.
Methods
Study design and participants
Electronic records of patients who underwent Hugo™ RAS for various gynecologic indications between March 2023 and July 2024 were retrospectively analyzed, and the results were compared to those using the da Vinci Xi system with matched demographics and disease characteristics. The study was approved by the Institutional Review Board of Tung’s Taichung Metroharbor Hospital, and the informed consent was waived.
Main outcome measures
To investigate the feasibility of the Hugo™ RAS in different gynecologic diseases, the length of stay, blood loss, surgical time, and perioperative complication rates were compared to those of the established Intuitive da Vinci Xi systems.
Statistical analysis
To reduce treatment discrepancies between the Hugo robotic surgery and da Vinci robotic surgery, propensity score matching was used to pair the two surgical methods based on age, height, weight, and the weight of the excised surgical components. Descriptive statistics were used to describe demographic variables. Continuous variables are presented as mean and range and were compared using Student’s t test. Categorical variables are expressed numerically as percentages and were compared using the Chi-square test or Fisher’s exact test, as appropriate.
Results
Between May 2023 and July 2024, 40 women, including 4, 4, 6, 20, 2, 3, and 1 cases of adenomyosis, cervical cancer, endometrial cancer, uterine leiomyomas, adenomyosis combined with uterine myomas, cesarean scar defect, and ovarian cancer, respectively, underwent hysterectomy (both benign and malignant, n = 25), myomectomy (n = 12), and scar defect repair (n = 3) (Table 1) with mean uterine weight of 338.6 g (62–1975 g). The mean blood loss was 317.68 ml, which was slightly higher in patients undergoing myomectomy (520.83 ml) and hysterectomy with myomas (502.5 ml), but comparable in others. The mean surgical time, docking time, and console time were 279.92 min (137–628), 7 min (2–20), and 131.7 min (25–455), respectively (Table 2).
Table 1.
Surgical characteristics and demographics of the Hugo™ RAS cohort
| No. | Length of hospital stay (days) | Diagnoses | Surgical procedure | Docking time (min) | Console time (min) | Blood loss (ml) | Complications |
|---|---|---|---|---|---|---|---|
| 1 | 4 | Endometrial cancer | Hugo RAS staging | 10 | 215 | 50 | |
| 2 | 3 | Cesarean scar defect with prolonged menses | Hugo RAS scar repair | 5 | 75 | 10 | |
| 3 | 3 |
1. Large subserosal myoma 2. Right paratubal cyst |
Hugo RAS myomectomy/enucleation of paratubal cyst | 5 | 25 | 200 | Ileus |
| 4 | 2 | Uterine myomas | Hugo RAS myomectomy | 14 | 115 | 150 | |
| 5 | 4 | Cervical cancer stage IIIC 1 (p) | Hugo RAS radical hysterectomy + BSO + BPLD | 8 | 272 | 10 | Fever |
| 6 | 2 | Uterine mass with post-menopausal bleeding | Hugo RAS hysterectomy + BSO | 7 | 46 | 50 | |
| 7 | 3 |
1. Left ovarian mucinous cystadenomas 2. Uterine myomas 3. Adenomyosis |
Hugo RAS hysterectomy + LSO + RS | 3 | 178 | 200 | |
| 8 | 3 | Persistent endometrial hyperplasia with atypia (failed medications) | Hugo RAS hysterectomy + BS | 3 | 50 | 10 | |
| 9 | 2 | Cesarean scar defect with prolonged menses | Hugo scar defect repair | 3 | 68 | 2 | |
| 10 | 9 |
1. Post-menopausal bleeding with rule out endometrial cancer 2. Rectal cancer s/p under chemotherapy |
Hugo RAS hysterectomy + BSO | 7 | 38 | 300 | Vomiting, ileus |
| 11 | 3 | Large uterine myomas with compression | Hugo RAS hysterectomy + BSO | 3 | 56 | 350 | |
| 12 | 4 | Multiple huge uterine myomas | Hugo RAS myomectomy | 3 | 129 | 200 | |
| 13 | 4 | Huge uterine myomas with compression | Hugo RAS hysterectomy + BSO | 3 | 167 | 1800 | |
| 14 | 3 |
1. Recurrent multiple myomas 2. Submucosal myomas |
Hugo RAS myomectomy + Tru clear myomectomy | 3 | 370 | 1000 | Spotting |
| 15 | 3 | Adenomyosis with elevated serum Ca-125 | Hugo RAS hysterectomy + BS + adhesiolysis | 8 | 98 | 300 | |
| 16 | 4 | Endometrial cancer | Hugo RAS staging | 5 | 255 | 100 | Hematuria |
| 17 | 2 | Cesarean scar defect with persisted spotting | Hugo scar defect repair | 10 | 70 | 20 | |
| 18 | 3 | Multiple uterine myomas | Hugo RAS hysterectomy + BSO | 5 | 59 | 500 | Dizziness |
| 19 | 2 |
Uterine myomas with degeneration 2 ovarian endometriomas |
Hugo RAS myomectomy + enucleation of ovarian endometriomas | 7 | 32 | 100 | |
| 20 | 4 | Multiple uterine myomas/ovarian endometriomas | Hugo RAS myomectomy + enucleation of ovarian endometriomas | 5 | 202 | 1000 | |
| 21 | 2 |
1. LEGH with post-menopausal bleeding 2. Breast cancer under Tamoxifen |
Hugo RAS hysterectomy + BSO | 5 | 202 | 100 | |
| 22 | 2 | Multiple uterine myomas | Hugo RAS myomectomy | 15 | 101 | 100 | |
| 23 | 3 | Huge uterine myomas | Hugo RAS hysterectomy + BS | 9 | 190 | 1400 | |
| 24 | 2 | Uterine myomas with dysmenorrhea | Hugo RAS myomectomy | 2 | 60 | 100 | |
| 25 | 4 | Large uterine myomas | Hugo RAS myomectomy | 10 | 130 | 600 | |
| 26 | 2 | Adenomyosis with severe dysmenorrhea | Hugo RAS hysterectomy + BS | 12 | 120 | 50 | |
| 27 | 3 | Endometrial cancer | Hugo RAS staging | 3 | 155 | 20 | |
| 28 | 6 | Post-menopausal bleeding with r/o uterine sarcoma | Hugo RAS hysterectomy + BSO | 4 | 182 | 15 | Fever, infection, leg weakness |
| 29 | 2 | large broad ligament’s myomas | Hugo RAS myomectomy | 20 | 80 | 300 | |
| 30 | 52 | Endometrial cancer | Hugo RAS staging | 10 | 190 | 100 | Fever, small intestinal perforation |
| 31 | 5 | Ovarian cancer s/p neoadjuvant chemotherapy | Hugo RAS maximal debulking + hyperthermic intraperitoneal chemotherapy (HIPEC) | 2 | 163 | 100 | |
| 32 | 4 | Multiple large uterine myomas | Hugo RAS myomectomy | 3 | 125 | 1500 | |
| 33 | 3 | Adenomyosis with severe anemia failed Mirena twice | Hugo RAS hysterectomy + BS (single port) | 5 | 65 | 300 | |
| 34 | 3 | Uterine myomas with compression | Hugo RAS myomectomy | 20 | 150 | 1000 | |
| 35 | 3 | Cervical cancer Ib3 s/p neoadjuvant chemotherapy | Hugo RAS radical hysterectomy + BSO | 11 | 455 | 150 | |
| 36 | 2 | Adenomyosis with failed Mirena and persisted dysmenorrhea | Hugo RAS hysterectomy + BS (single port) | 5 | 88 | 200 | |
| 37 | 4 | Cervical cancer s/p CCRT with partial response of tumor | Hugo RAS hysterectomy + BSO | 8 | 77 | 150 | Spotting |
| 38 | 2 | Submucosal myomas | Hugo RAS hysterectomy + BSO | 4 | 90 | 100 | |
| 39 | 3 | CIN3 with margin involved | Hugo RAS hysterectomy + BS | 5 | 85 | 50 | |
| 40 | 3 | Residual endometrial polys/breast cancer under Tamoxifen | Hugo RAS hysterectomy + BS | 10 | 40 | 20 |
BSO, bilateral salpingooophorectomy; BPLD, bilateral pelvic lymph node dissection; LSO, left salpingooophorectomy; RS, right salpingectomy; LEGH, lobular endocervical glandular hyperplasia; CCRT, concurrent chemoradiotherapy; BS, bilateral salpingectomy
Table 2.
Demographics of the Hugo™ RAS cohort
| Parameters | Hugo (n = 40) |
|---|---|
| Age, year | 47.65 (34–84) |
| BMI, kg/m2 | 26.17 (19.52–35.86 |
| Obesity | 8 (20) |
| Uterine weight, gm | 338.6 (62–1975) |
| Myoma, gm | 374.3 (5–1040) |
| Length of hospital stay, day | 4.42 (2–52) |
| Blood loss, ml | 317.68 (2–1800) |
| Hysterectomy + adenomyosis | 212.5 (50–300) |
| Hysterectomy + Cervical cancer | 202.5 (10–500) |
| Hysterectomy + endometrial cancer | 64.17 (15–100) |
| Hysterectomy + leiomyomas and adenomyosis | 175 (50–300) |
| Hysterectomy + myoma | 502.5 (20–1800) |
| Hysterectomy + others | 10 (10–10) |
| Myomectomy + myoma | 520.83 (100–1500) |
| Scar repair | 10.67 (2–20) |
| Surgery time, min | 279.92 (137–628) |
| Hysterectomy + adenomyosis | 209.8 (190–240) |
| Hysterectomy + cervical cancer | 338 (170–628) |
| Hysterectomy + endometrial cancer | 371.3 (290–460) |
| Hysterectomy + leiomyomas and adenomyosis | 203 (154–252) |
| Hysterectomy + myoma | 280.2 (164–607) |
| Hysterectomy + others | 172 (172–172) |
| Myomectomy + myoma | 291.1 (137–627) |
| Scar repair | 155 (141–164) |
| Docking time, min | 7 (2–20) |
| Console time, min | 131.7 (25–455) |
| Surgery type | |
| Hysterectomy | 25 (62.5) |
| Myomectomy | 12 (30) |
| Scar repair | 3 (7.5) |
| Disease | |
| Adenomyosis | 4 (10) |
| Cervical cancer | 4 (10) |
| Endometrial cancer | 6 (15) |
| Leiomyomas and adenomyosis | 2 (5) |
| Myoma | 20 (50) |
| Others | 1 (2.5) |
| Scar repair | 3 (7.5) |
| Complication (7 days) | 9 (22.5) |
| Complication (30 days) | 5 (12.5) |
| Transfusion | 10 (25) |
BMI, body mass index
After propensity score matching, compared to the 111 patients who underwent da Vinci surgery in our series, there were no differences in blood loss [235.42 ml (0–3100) vs. 342.57 ml (10–1800), p = 0.198], incidence of perioperative complications [25 (22.52%) vs. 9 (24.32%), p > 0.99, within 7 days (Table S1); 15 (13.51%) vs. 5 (13.51%), p > 0.99, within 30 days (Table S2)], and length of hospital stay [3.51 days (2–9) vs. 4.59 days (2–52), p = 0.426). However, the surgical time was longer with Hugo™ RAS (228.23 min [84–483] vs. 290.05 min [137–628], p < 0.011), especially in the procedure in the staging of endometrial cancer (381 vs. 324.86 min, p < 0.025) (Table 3).
Table 3.
Comparison between the cohorts using the Hugo™ RAS and da Vinci Xi system
| Parameter | Da Vinci (n = 111) | Hugo (n = 37) | p |
|---|---|---|---|
| Age, year | 48.86 (26–83) | 48.46 (34–84) | 0.836 |
| BMI, kg/m2 | 26.01 (17.8–37.74) | 26.38 (19.52–35.86) | 0.665 |
| Obesity | 42 (37.84) | 15 (40.54) | 0.922 |
| Uterine weight, gm | 335 (5–1990) | 338.6 (62–1975) | 0.972 |
| Myoma, gm | 361.5 (3–1088) | 374.3 (5–1040) | 0.9 |
| Length of hospital stay, day | 3.51 (2–9) | 4.59 (2–52) | 0.426 |
| Blood loss, ml | 235.42 (0–3100) | 342.57 (10–1800) | 0.198 |
| Hysterectomy + adenomyosis | 280 (100–750) | 212.5 (50–300) | 0.664 |
| Hysterectomy + cervical cancer | 118 (20–400) | 202.5 (10–500) | 0.514 |
| Hysterectomy + endometrial cancer | 68.53 (10–300) | 64.17 (15–100) | 0.904 |
| Hysterectomy + leiomyomas and adenomyosis | 164.1 (2–500) | 175 (50–300) | 0.93 |
| Hysterectomy + myoma | 206.43 (0–1700) | 502.5 (20–1800) | 0.14 |
| Myomectomy + myoma | 486.25 (15–3100) | 520.83 (100–1500) | 0.871 |
| Surgery time, min | 228.23 (84–483) | 290.05 (137–628) | 0.011 |
| Hysterectomy + adenomyosis | 190.4 (127–255) | 209.75 (190–240) | 0.523 |
| Hysterectomy + cervical cancer | 271.8 (110–456) | 338 (170–628) | 0.578 |
| Hysterectomy + endometrial cancer | 227.76 (149–483) | 371.33 (290–460) | 0.002 |
| Hysterectomy + leiomyomas and adenomyosis | 199.95 (113–364) | 203 (154–252) | 0.948 |
| Hysterectomy + myoma | 224.36 (84–480) | 280.25 (164–607) | 0.337 |
| Myomectomy + myoma | 261.89 (89–460) | 291.08 (137–627) | 0.47 |
| Surgery type | |||
| Hysterectomy | 83 (74.77) | 25 (67.57) | 0.521 |
| Myomectomy | 28 (25.23) | 12 (32.43) | 0.521 |
| Disease | |||
| Adenomyosis | 5 (4.5) | 4 (10.81) | 0.228 |
| Cervical cancer | 5 (4.5) | 4 (10.81) | > 0.99 |
| Endometrial cancer | 17 (15.32) | 6 (16.22) | 0.067 |
| Leiomyomas and adenomyosis | 20 (18.02) | 2 (5.41) | 0.849 |
| Myoma | 56 (50.45) | 20 (54.05) | > 0.99 |
| Others | 5 (4.5) | 1 (2.7) | 0.573 |
| Ovarian cancer | 3 (2.7) | 0 (0) | 0.234 |
| Complication (7 days) | 25 (22.52) | 9 (24.32) | > 0.99 |
| Complication (30 days) | 15 (13.51) | 5 (13.51) | > 0.99 |
| Transfusion | 27 (24.32) | 10 (27.03) | 0.913 |
BMI, body mass index
Discussion
Main findings
There were no differences in the length of hospital stay, blood loss, and perioperative complication rates between the Hugo™ RAS and the established da Vinci Xi system in our study cohorts. A variety of procedures, including single-port hysterectomy, three-arm setting, and ovarian interval debulking surgery (IDS) combined with HIPEC, were added to conventional simple hysterectomy, radical hysterectomy, endometrial staging procedure, and myomectomy, all resulting in favorable perioperative outcomes. The feasibility of the platform has been clearly demonstrated for almost all common surgical indications in the gynecology field. The main obstacle to be tackled is the limited option of instruments available for procedures performed with only monopolar scissors, bipolar coagulation, and Cadiere forceps to choose from. Although there is a built-in pedal for the ligasure™ (Medtronic), it was not available during the period when this study was carried out. A slight lag time between instrumental shifts sometimes can be a problem for a seamless procedure.
Interpretation of findings
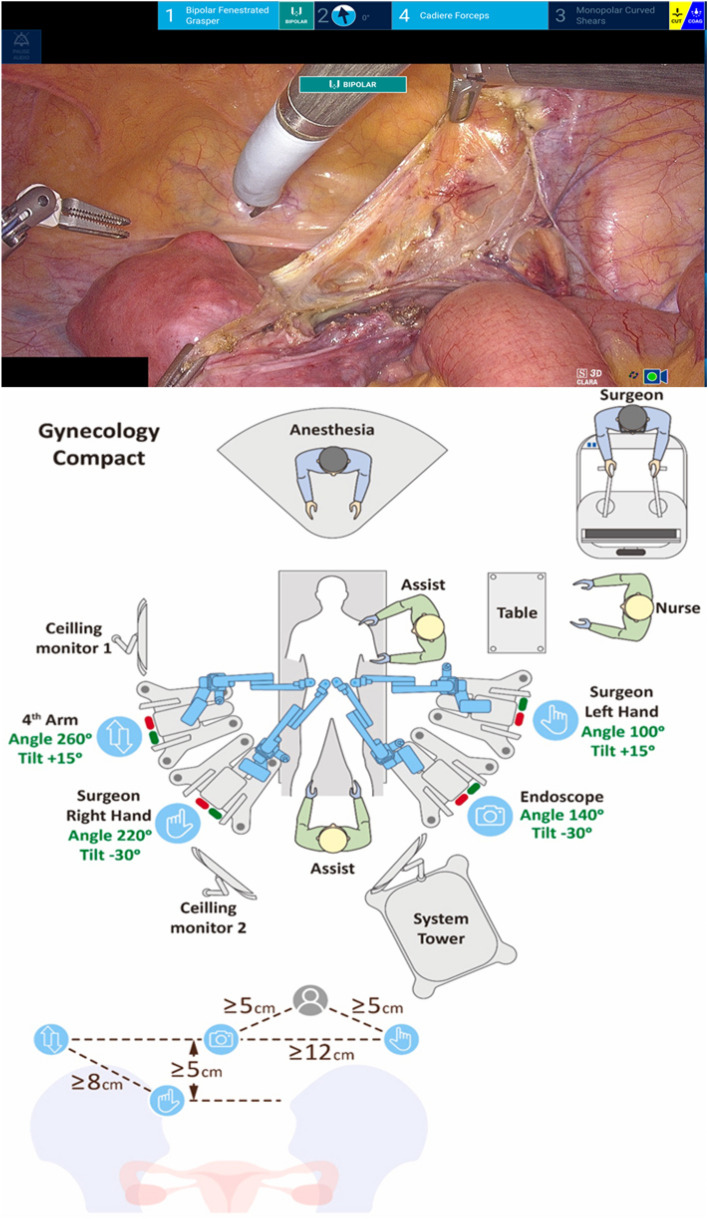
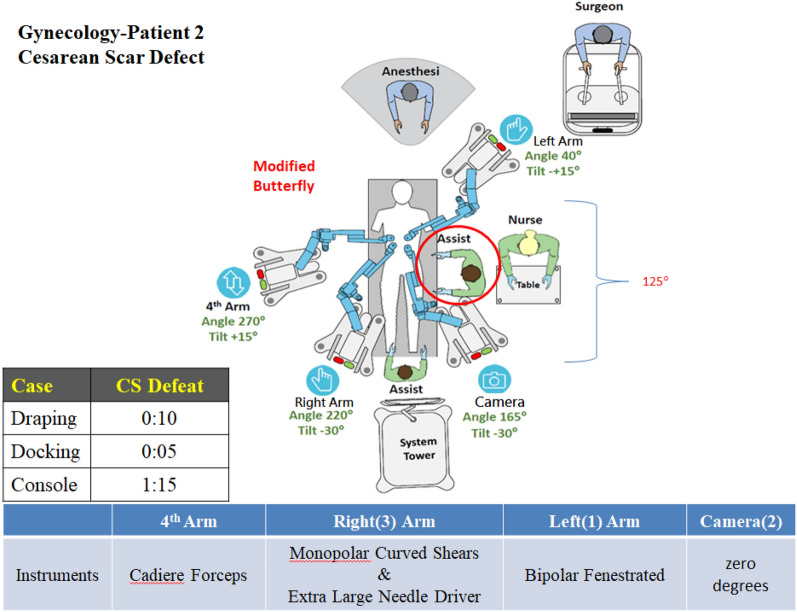
The novel Hugo™ RAS can perform most gynecologic procedures well, and with experience gained in the journey, little modification is required in the configuration of presetting arms to fit different situations. We found that with the compact setting as originally suggested by Gueli Alletti et al. [10] (Fig. 2), a longer instrument and limited space of the assistant through the Palmer point might hinder the smoothness of the procedure, whereas a slight modification of the down placement of the fourth trocar (the straight port placement) coupled with a modified butterfly configuration (Fig. 3) may greatly decrease the incidence of arms collisions during complex procedure. Although its original design is not specifically for single-port applications, we demonstrated the feasibility of single-arm hysterectomy in two cases (Fig. 4). Further evaluation of the modifications of the presetting angles and arm placement is necessary to carry out the procedure smoothly in the future. The procedure of interval debulking with complete resection of the ovarian tumor (R0) in a case of stage IIIB ovarian cancer coupled with intraoperative hyperthermic intraperitoneal chemotherapy (HIPEC) was successfully performed, which is believed to be the first case report using the new surgical platform in this scenario. A slightly longer surgical time is expected when adapting to a new robotic platform, with totally different docking procedure as well as adaptability of limited instrument option, especially for more complicated procedures. However, for more commonly performed surgeries, such as simple hysterectomy and myomectomy, there was no difference in surgical time between our study cohort and the da Vinci cohort.
Fig. 2.
The compact configuration requires the assistants to enter through Palmer’s point, which limits their ability to help due to the longer distance to the target tissue
Fig. 3.
The modified butterfly configuration provides assistants with a more spacious working area
Fig. 4.

Single-port hysterectomy using the Glove Port (Nelis Medical, Korea) and three-arm setting in a single umbilical incisional wound. BS: bilateral salpingectomy
With the introduction of a different setting of surgical console and separate docking arms, a more surgeon-friendly platform will reduce the muscle strains of upper musculoskeletal as well as wrist portion and easy adjustment of angle during operative time will enable the reaching to a wider surgical field.
There is an easy shifting from da Vinci platform to Hugo™ RAS with short learning curve as demonstrated in our study with most of the surgical time, blood loss and hospital stay are comparable to da Vinci platform. With the innovation of different surgical design, it is anticipated there will be more surgeon-friendly and ease to use with comparable results and cost effective in term of unit price.
Strengths and limitations
This is a small retrospective study in a single institution, and the experience in this novel surgical platform of one surgeon inevitably introduced recall bias when retrieving data from previous cases using the da Vinci Xi procedure due to its long-lapsing and retrospective nature. However, every procedure and all demographic details were documented precisely in the first 40 cases using the Hugo™ RAS. The configuration was modified according to different clinical situations and new settings were adapted to various situations, which might provide a more practical and valuable experience compared with the recommendations of in vivo studies, as suggested by Gueli Alletti et al. [10]. The author has been practicing da Vinci surgery since 2013 with a total of 351 different procedures being carried out as of June, 2024 and has been a proctor for TR300 in da Vinci accredited advance course as well as an instructor for IRCAD Taiwan (MIS training center). He is also a sole proctor in Hugo™ RAS in gynecologic surgery in the Greater China since August 2024. There are no single case of conversion to laparotomy both in the da Vinci cohort and Hugo™ RAS during the study period.
Conclusions
The Hugo™ RAS is feasible and safe in most gynecologic procedures with more options of instruments anticipated in the future.
Supplementary Information
Below is the link to the electronic supplementary material.
Author contributions
Kim-Seng Law was responsible for the conception, planning, carrying out, and analysis of the study, as well as writing the manuscript.
Funding
The author received no funding for this study.
Data availability
All data supporting the findings of this study are available within the paper and its Supplementary Information.
Declarations
Conflict of interest
The author reports no conflict of interest.
IRB approval
This study received IRB approval from our institutions (Approval Number 113040 dated 17 July 17, 2024). The requirement for informed consent was waived by the Institutional Review Board.
Prior presentation
Nil.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Rivero-Moreno Y, Echevarria S, Vidal-Valderrama C et al (2023) Robotic surgery: a comprehensive review of the literature and current trends. Cureus 15:e42370. 10.7759/cureus.42370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chuchulo A, Ali A (2023) Is robotic-assisted surgery better? AMA J Ethics 25:E598-604. 10.1001/amajethics.2023.598 [DOI] [PubMed] [Google Scholar]
- 3.Lim PC, Crane JT, English EJ et al (2016) Multicenter analysis comparing robotic, open, laparoscopic, and vaginal hysterectomies performed by high-volume surgeons for benign indications. Int J Gynaecol Obstet 133:359–364. 10.1016/j.ijgo.2015.11.010 [DOI] [PubMed] [Google Scholar]
- 4.Prata F, Ragusa A, Tempesta C et al (2023) State of the art in robotic surgery with Hugo RAS system: feasibility, safety and clinical applications. J Pers Med. 10.3390/jpm13081233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.See Tow HX, Ho ECK, Wong NHP, Tiong HY, So WZ (2024) The Hugo RAS robotic system: a brief overview of current evidence in urological surgery. Robot Rep 2:43–48. 10.1089/rorep.2023.0020 [Google Scholar]
- 6.Ngu JC, Lin CC, Sia CJ, Teo NZ (2024) A narrative review of the Medtronic Hugo RAS and technical comparison with the Intuitive da Vinci robotic surgical system. J Robot Surg 18:99. 10.1007/s11701-024-01838-5 [DOI] [PubMed] [Google Scholar]
- 7.Law KS (2024) Robotic staging procedure performed using Medtronic Hugo™ RAS in an endometrial cancer patient: a case report. Heliyon 10:e23756. 10.1016/j.heliyon.2023.e23756 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Komatsu H, Sawada M, Iida Y et al (2024) New surgery technique combining robotics and laparoscopy using the Hugo™ RAS system. Asian J Endosc Surg 17:e13344. 10.1111/ases.13344 [DOI] [PubMed] [Google Scholar]
- 9.Panico G, Vacca L, Campagna G et al (2023) The first 60 cases of robotic sacrocolpopexy with the novel HUGO RAS system: feasibility, setting and perioperative outcomes. Front Surg 10:1181824. 10.3389/fsurg.2023.1181824 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gueli Alletti S, Chiantera V, Arcuri G et al (2022) Introducing the new surgical robot HUGO™ RAS: system description and docking settings for gynecological surgery. Front Oncol 12:898060. 10.3389/fonc.2022.898060 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data supporting the findings of this study are available within the paper and its Supplementary Information.