ABSTRACT
Background and Aims
Catheter‐based renal denervation (RDN) is a safe and effective alternative treatment for hypertension. However, data on patient preferences are limited. This study sought to delineate preferences for RDN among Veterans with difficult‐to‐control hypertension at an urban VA Medical Center with the goal of optimizing management and referral practices in hypertensive Veterans.
Methods
Patients on 3+ antihypertensive medications and a measured creatinine < 2.5 mg/dL were identified from the pharmacy database. A total of 100 randomly selected patients were telephoned for the administration of a survey assessing patient preferences for RDN, expectations for RDN, as well as medication adherence using the Medication Adherence Report Scale (MARS‐5). Additional chart review was performed to gather demographic and clinical data of survey respondents.
Results
A total of 51 Veterans completed the survey. While 29 (56.9%) Veterans indicated a preference against RDN, 22 (43.1%) indicated a preference for this procedure, and 33 (64.7%) expressed that if their blood pressure were uncontrolled, they would prefer RDN over additional medication. A history of congestive heart failure (p = 0.017) and lower MARS‐5 score (p = 0.007) were associated with a preference for RDN. Age, reported medication side effects, and hypertension treatment satisfaction ratings were not associated with preference for or against RDN.
Conclusions
A considerable portion of Veterans with difficult‐to‐control hypertension at an urban VA Medical Center expressed a preference for RDN if their blood pressure were to be uncontrolled or if recommended by their doctor. These survey results should be considered in shared decision‐making discussions for hypertension management in this population.
Keywords: hypertension, renal denervation, Veterans
Abbreviations
- ACEi
angiotensin‐converting enzyme inhibitor
- aHTN
antihypertensive
- ARB
angiotensin receptor blocker
- CCB
calcium channel blocker
- CHF
congestive heart failure
- DBP
diastolic blood pressure
- HTN
hypertension
- MARS‐5
Medication Adherence Report Scale
- RDN
renal denervation
- SBP
systolic blood pressure
- VA
Veterans Affairs
- VHA
Veterans Health Administration
1. Introduction
Hypertension is a leading cause of mortality and a major modifiable risk factor for cardiovascular and kidney disease [1]. Among Veterans receiving care through the Veterans Health Administration (VHA), it is the predominant chronic condition, diagnosed in 48.2% of all Veterans [2]. Despite advancements in pharmacotherapies for hypertension, this disease remains difficult to control. In the Veteran population, 66% of Veterans with known hypertension were uncontrolled [3]. With evidence supporting even more stringent blood pressure control, the number of Veterans with known hypertension necessitating intensification of treatment is estimated to be well over 1 million individuals [3, 4].
Optimal hypertension management can be limited by pill burden, medication adherence, medication side effects, and consistent 24‐h blood pressure control. Poor medication adherence may intrinsically and subconsciously be an expression of treatment preference alone. Renal denervation (RDN) offers a potential alternative treatment option, where a one‐time procedure offers sustained, consistent blood pressure control without ongoing adherence or side‐effect concerns. This treatment strategy may provide an attractive alternative to pharmacotherapies for many patients. Multiple sham‐controlled randomized clinical trials have demonstrated significant reductions in blood pressure and reassuring safety with low adverse event rates, reinvigorating interest in this treatment modality [5, 6, 7, 8].
Despite the safety and effectiveness of this catheter‐based treatment option, patient preferences for the procedure and the circumstances under which they will choose to proceed with it remain unclear. An understanding of patient preferences has become increasingly necessary given the importance of shared decision‐making and patient‐centered care. Specifically, shared decision‐making in treatment decisions can lead to better adherence and subsequently better health outcomes [9].
In this study, we sought to characterize and evaluate preference for RDN among Veterans at our center with difficult‐to‐control hypertension. Preference for RDN has not previously been evaluated in a Veteran population.
2. Methods
This quality assurance study received Jesse Brown Veterans Affairs (JBVA) IRB exemption. Patients with at least three current prescriptions of antihypertensive (aHTN) medications and a measured creatinine < 2.5 were identified from the VA pharmacy database. Creatinine was used to identify patients likely to have chronic kidney disease stage IV (CKD IV) or higher. All patients were on at least an angiotensin‐converting enzyme inhibitor (ACEI) or angiotensin receptor blocker (ARB), a calcium channel blocker (CCB), and a diuretic. Combination pill prescriptions were included and counted as individual separate medications.
Inclusion criteria were: receiving aHTN medication prescriptions through JBVA pharmacy, prescribed at least 3 (3+) aHTN medications, and age 18–80. We excluded Veterans with Cr > 2.5 mg/dL, as patients with CKD IV or worse have typically been excluded from RDN trials. A total of 1161 patients were identified as meeting these criteria. A random number generator was used to select a sample of 100 patients from this list to call to administer the survey. After random selection, all 100 were screened to ensure available contact information, not currently admitted to the hospital, and no history of cognitive impairment, dementia, or Alzheimer's disease. Baseline demographic characteristics, comorbidities, and medication prescription data were collected only on patients who completed the survey (Figure 1).
Figure 1.

Flow diagram of methods. *The 100 patients were screened to ensure available contact information, not currently admitted to the hospital, and no history of cognitive impairment, dementia, or Alzheimer's disease.
The survey questionnaire was adapted from prior surveys of patient preference for RDN [10, 11, 12]. The survey collected data on current treatment, including number of pills, perceived side effects, and satisfaction with hypertension treatment, preference to receive alternative treatment with RDN, and determinants of preferences for their choice. The survey was administered over the phone. A preference for RDN was defined as a response indicating either “I want to undergo RDN” or “I'd rather undergo RDN,” while a preference against RDN was defined as answering survey questionnaire was adapted “I don't want to undergo RDN” or “I'd rather not undergo RDN.” Medication adherence was also assessed by the Medication Adherence Report Scale (MARS‐5) questionnaire, a medication adherence self‐reporting tool, validated in hypertension [13].
Demographic and survey data were analyzed and compared between patients with a preference for RDN and against RDN as defined above. A Shapiro–Wilk test was used to test the normality of the data. Age, body mass index (BMI), systolic (SBP) and diastolic blood pressures (DBP), and total aHTN medications were compared with the independent t‐tests. Fisher's exact and χ 2 tests were used to compare medical comorbidities, medication adherence, and treatment satisfaction. Survey responses were also stratified by MARS‐5 score = 25 versus MARS‐5 score < 25, consistent with prior study definitions of good versus poor adherence, respectively [13, 14], again utilizing Fisher's exact and χ 2 tests. Statistical analyses were conducted with the following assumptions: β 0.8, α < 0.05. All analyses were conducted with SPSS software version 29.1 (IBM Corporation, Armonk, NY).
3. Results
3.1. Demographics
A total of 51 Veterans completed the survey. The mean age was 69.6 ± 8.4 years old, and mean BMI was 31.1 kg/m2. In total, 49 (96.1%) respondents were male, and 32 (62.7%) were Black. The most common comorbidities were diabetes mellitus (68.6%), obstructive sleep apnea (39.2%), CKD (41.2%), coronary artery disease (21.6%), congestive heart failure (CHF) (7.8%), and stroke (7.8%). Based on most recent clinic blood pressure measurements, the mean SBP and DBP were 135.1 ± 14.0 mmHg and 76.7 ± 8.5 mmHg, respectively. The average number of aHTN medications was 3.43 ± 0.5 with lisinopril, amlodipine, and hydrochlorothiazide being the most common medications. The average MARS‐5 score was 23.0 ± 2.3. Only 8 (15.7%) reported experiencing any side effects to their aHTN medications, and only 9 (17.6%) reported a treatment satisfaction rating < 4 (Table 1).
Table 1.
Demographics.
| Overall | |
|---|---|
| N = 51 | |
| Age (y) | 69.6 ± 8.4 |
| Sex | |
| Female | 2 (3.9%) |
| Male | 49 (96.1%) |
| Race | |
| White/Caucasian | 18 (35.3%) |
| Black | 32 (62.7%) |
| Other | 1 (2.0%) |
| BMI (kg/m2) | 31.1 ± 6.6 |
| Active or recent tobacco use | 10 (19.6%) |
| Diabetes mellitus | 35 (68.6%) |
| OSA | 20 (39.2%) |
| PAD | 2 (3.9%) |
| CAD | 11 (21.6%) |
| MI | 2 (3.9%) |
| Stroke | 4 (7.8%) |
| CHF | 4 (7.8%) |
| CKD | 21 (41.2%) |
| SPB (mmHg) | 135.1 ± 14.0 |
| DPB (mmHg) | 76.7 ± 8.5 |
| No. of aHTN medications | 3.43 ± 0.5 |
| MARS‐5 score | 23.0 ± 2.3 |
| HTN/medication characteristics | |
| SBP > 129 mmHg | 32 (62.7%) |
| DBP > 89 mmHg | 4 (7.8%) |
| Experienced medication side effects | 8 (15.7%) |
| aTreatment satisfaction rating < 4 | 9 (17.6%) |
| MARS‐5 < 25 | 35 (68.6%) |
Note: Averages are expressed as the mean ± SD.
Abbreviations: aHTN, antihypertensive; BMI, body mass index; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; DBP, diastolic blood pressure; MI, myocardial infarction; OSA, obstructive sleep apnea; PAD, peripheral artery disease; SBP, systolic blood pressure.
Hypertension treatment satisfaction rated on a scale of 0–5.
3.2. Preferences
All 51 survey responses were counted and included in the subsequent analysis (Table 2). Overall, 43.1% reported a preference for RDN by answering either “I'd rather undergo RDN” or “I want to undergo RDN,” while 56.9% reported a preference against RDN by answering either “I don't want to undergo RDN” or “I'd rather not undergo RDN” (Figure 2). However, if their blood pressure were to be uncontrolled, 64.7% of respondents specified that they would prefer RDN over additional medication (Figure 3).
Table 2.
Survey responses.
| Count | |
|---|---|
| N = 51 | |
| Which statement best describes your preference for RDN? | |
| I don't want to undergo RDN | 8 (15.7%) |
| I'd rather NOT undergo RDN | 21 (41.2%) |
| I'd rather undergo RDN | 13 (25.5%) |
| I want to undergo RDN | 9 (17.6%) |
| Would you be treated with RDN if after you still had to take how many pills after? | |
| 0 | 18 (35.3%) |
| 1 | 18 (35.3%) |
| 2 | 10 (19.6%) |
| 3 | 5 (9.8%) |
|
What percentage of success in lowering your blood pressure 10 mmHg would make you want to undergo RDN? | |
| 100% | 18 (35.3%) |
| 90% | 17 (33.3%) |
| 70% | 13 (25.5%) |
| 50% | 3 (5.9%) |
| If your blood pressure was uncontrolled and your doctor recommended either an additional pill or RDN, which would you prefer? | |
| RDN | 33 (64.7%) |
| Pill | 18 (35.3%) |
| I would be more likely to choose RDN if: (multiple response allowed) | |
| Recommended by my doctor | 21 |
| It reliably lowers my blood pressure | 21 |
| I am certain it will be effective | 22 |
| I need to take fewer pills as a result | 25 |
| It is only a one‐time medical procedure and not additional pills | 12 |
| I get closer to ideal systolic blood pressure of 120 | 12 |
| Blood pressure fluctuates less after | 4 |
| I will tolerate it better than pills | 4 |
| I am not interested in treatment with RDN no matter what. | 8 |
Figure 2.
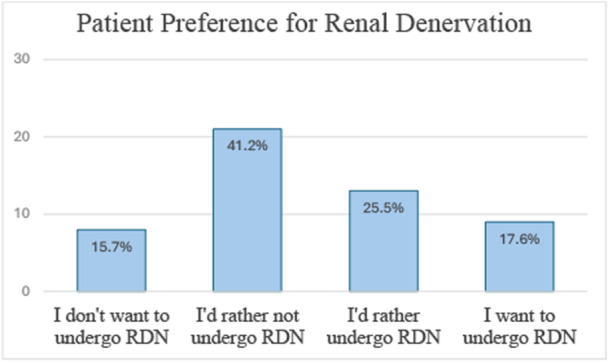
Response to “Which statement best describes your preference for RDN?”.
Figure 3.

Responses to “If your blood pressure were uncontrolled and your doctor recommended either an additional pill or RDN, which would you prefer?”.
Patients were asked several questions about RDN expectations and what factors would make them choose this treatment option. When asked “What percentage of success of RDN in lowering blood pressure by > 10 mmHg would make you want to be treated with it,” 69% answered either 90% or 100%. In total, 35% percent would prefer RDN if they were able to take no pills after. The factors that were most frequently indicated as most important in respondent's hypertension treatment and consideration of RDN were doctor's recommendation, the number of pills needed, the reliability of RDN, and the effectiveness of RDN (Figure 4).
Figure 4.
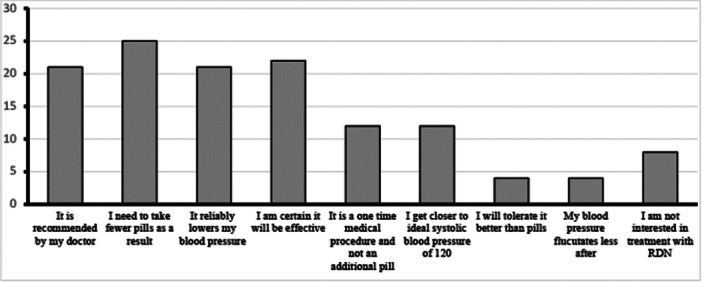
Responses to “What factors most impact your choice related to RDN?”.
There was an association between respondents with a preference for versus against RDN and several factors (Table 3). A comorbid diagnosis of CHF was associated with a preference for RDN (18.2% vs. 0.0%, p = 0.017). Comorbid diabetes mellitus was associated with a preference against RDN (40.9% vs. 72.4%, p = 0.024). More patients who had preference against RDN had uncontrolled SBP (defined as SBP > 129 mmHg) based on most recent clinic measurements (40.9 vs. 79.3%, p = 0.005). Patients who had lower MARS‐5 scores, indicating worse medication adherence, were significantly more likely to prefer RDN than not (p = 0.007). There was no association between those for or against RDN based on age, race, BMI, tobacco use, a reported history of side effects to aHTN medications, or satisfaction with their hypertension treatment.
Table 3.
Association with preference for renal denervation.
| Preference for renal denervation | |||
|---|---|---|---|
| No | Yes | ||
| N = 29 | N = 22 | p value | |
| Age | 70.2 ± 8.4 | 68.6 ± 8.5 | 0.504 |
| Sex | |||
| Female | 1 (3.4%) | 1 (4.5%) | 0.842 |
| Male | 28 (96.6%) | 21 (95.5%) | |
| Race | |||
| White/Caucasian | 12 (41.4%) | 6 (27.3%) | 0.332 |
| Black | 17 (58.6%) | 15 (68.2%) | |
| Other | 0 (0.0%) | 1 (4.5%) | |
| BMI (kg/m2) | 30.8 ± 7.0 | 31.5 ± 6.2 | 0.725 |
| Active or recent tobacco use | 5 (17.2%) | 5 (22.7%) | 0.625 |
| Diabetes mellitus | 21 (72.4%) | 9 (40.9%) | 0.024 |
| OSA | 10 (34.5%) | 10 (45.5%) | 0.427 |
| PAD | 1 (3.4%) | 1 (4.5%) | 0.842 |
| CAD | 8 (27.6%) | 3 (13.6%) | 0.23 |
| MI | 1 (3.4%) | 1 (4.5%) | 0.842 |
| Stroke | 1 (3.4%) | 3 (13.6%) | 0.18 |
| CHF | 0 (0.0%) | 4 (18.2%) | 0.017 |
| CKD | 10 (34.5%) | 11 (50.0%) | 0.256 |
| SPB (mmHg) | 138.4 ± 12.4 | 130.9 ± 15.2 | 0.114 |
| DPB (mmHg) | 75.9 ± 8.4 | 77.7 ± 8.7 | 0.504 |
| No. of aHTN medications | 3.55 ± 0.6 | 3.27 ± 0.5 | 0.066 |
| MARS‐5 score | 23.7 ± 1.4 | 22.0 ± 2.9 | 0.007 |
| HTN/medication characteristics | |||
| SBP > 129 | 23 (79.3%) | 9 (40.9%) | 0.005 |
| DBP > 89 | 2 (6.9%) | 2 (9.1%) | 0.773 |
| Experienced medication side effects | 3 (10.3%) | 5 (22.7%) | 0.228 |
| aTreatment satisfaction rating < 4 | 4 (13.8%) | 5 (22.7%) | 0.407 |
| MARS‐5 < 25 | 18 (62.1%) | 17 (77.3%) | 0.246 |
Note: Averages are expressed as the mean ± SD, categorical data are expressed as frequency (%).
Abbreviations: aHTN, antihypertensive; BMI, body mass index; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; DBP, diastolic blood pressure; MI, myocardial infarction; OSA, obstructive sleep apnea; PAD, peripheral artery disease; SBP, systolic blood pressure.
Hypertension treatment satisfaction rated on a scale of 0–5.
3.3. Adherence
As noted above, patients with lower adherence scores were significantly more likely to prefer RDN. When stratified by MARS‐5 scores = 25 versus MARS‐5 scores < 25, there was no difference in preference for or against RDN in the good versus poor adherence groups (31.3% vs. 48.6%, p = 0.246) (Table 4). However, patients with poor adherence were more likely to select RDN over an additional medication if their blood pressure were uncontrolled and they were given the option of choosing between the two (74% vs. 43.8%, p = 0.034) (Table 4).
Table 4.
MARS‐5 and renal denervation preference and expectations.
| Overall | MARS = 25 | MARS < 25 | ||
|---|---|---|---|---|
| N = 51 | N = 16 | N = 35 | p value | |
| Age | 69.6 ± 8.4 | 70.2 ± 8.4 | 68.6 ± 8.5 | 0.504 |
| Sex—F | ||||
| Female | 2 (3.9%) | 0 (0.0%) | 2 (9.1%) | 0.329 |
| Male | 49 (96.1%) | 16 (100%) | 33 (90.9%) | |
| Race | ||||
| White/Caucasian | 18 (35.3%) | 6 (37.5%) | 12 (34.3%) | 0.783 |
| Black | 32 (62.7%) | 10 (62.5%) | 22 (62.9%) | |
| Other | 1 (2.0%) | 0 (0.0%) | 1 (2.9%) | |
| BMI (kg/m2) | 31.1 ± 6.6 | 30.8 ± 7.0 | 31.5 ± 6.2 | 0.725 |
| Active or recent tobacco use | 10 (19.6%) | 4 (25.0%) | 6 (17.1%) | 0.801 |
| Diabetes mellitus | 35 (68.6%) | 9 (56.3%) | 21 (60.0%) | 0.512 |
| OSA | 20 (39.2%) | 7 (43.8%) | 13 (37.1%) | 0.654 |
| PAD | 2 (3.9%) | 0 (0.0%) | 2 (5.7%) | 0.329 |
| CAD | 11 (21.6%) | 3 (18.8%) | 8 (22.9%) | 0.741 |
| MI | 2 (3.9%) | 1 (6.3%) | 1 (2.9%) | 0.562 |
| Stroke | 4 (7.8%) | 1 (6.3%) | 3 (8.6%) | 0.775 |
| CHF | 4 (7.8%) | 2 (12.5%) | 2 (5.7%) | 0.403 |
| CKD | 21 (41.2%) | 9 (56.3%) | 12 (34.3%) | 0.139 |
| SPB (mmHg) | 135.1 ± 14.0 | 139.8 ± 12.2 | 133.0 ± 14.5 | 0.114 |
| DPB (mmHg) | 76.7 ± 8.5 | 77.9 ± 5.5 | 76.1 ± 9.6 | 0.504 |
| No. of aHTN medications | 3.43 ± 0.5 | 3.44 ± 0.6 | 3.43 ± 0.5 | 0.957 |
| Preference for RDN | 22 (43.1%) | 5 (31.3%) | 17 (48.6%) | 0.246 |
| Rather undergo RDN than add additional aHTN medication | 33 (64.7%) | 7 (43.8%) | 26 (74.3%) | 0.034 |
| HTN/medication characteristics | ||||
| SBP > 129 | 32 (62.7%) | 13 (81.3%) | 19 (54.3%) | 0.065 |
| DBP > 89 | 4 (7.8%) | 0 (0.0%) | 4 (11.4%) | 0.159 |
| Experienced medication side effects | 8 (15.7%) | 1 (6.3%) | 7 (20.0%) | 0.210 |
| aTreatment satisfaction rating < 4 | 9 (17.6%) | 1 (6.3%) | 8 (22.9%) | 0.149 |
Note: Averages are expressed as the mean ± SD, categorical data are expressed as frequency (%).
Abbreviations: aHTN, antihypertensive; BMI, body mass index; CAD, coronary artery disease; CHF, congestive heart failure; CKD, chronic kidney disease; DBP, diastolic blood pressure; MI, myocardial infarction; OSA, obstructive sleep apnea; PAD, peripheral artery disease; SBP, systolic blood pressure.
Hypertension treatment satisfaction rated on a scale of 0–5.
4. Discussion
This study is the first to investigate patient preferences for RDN in the management of hypertension in a Veteran population. The VHA is one of the largest integrated healthcare systems in the United States. Veterans exhibit a markedly high prevalence of hypertension, with a substantial number of patients having uncontrolled blood pressure [3, 15]. RDN offers a promising treatment option, particularly in this population with a high prevalence of overall and uncontrolled hypertension. Utilization of a shared decision‐making model that aligns treatment options, whether lifestyle, pharmaceutical, or interventional therapies, with patient preferences is crucial to improving hypertension control. Previously, little was known of this patient population's preferences for RDN or willingness to undergo procedural treatment for hypertension.
A sizable portion of patients expressed a preference for RDN. The proportion found in our study is similar to studies of other populations, which demonstrated preferences for RDN around roughly 30%–40% [11, 12, 16]. Of particular interest, 62.7% of our respondents were Black. While this is in line with our center's overall demographics, it is much larger than the VHA population and overall US population [17, 18, 19]. This is a much larger proportion of Black patients than has been previously evaluated for preferences in RDN treatment [10, 11, 12, 16]. Importantly, there was no difference in preference for or against RDN based on race. Given well‐described racial disparities in cardiovascular care and evidence of Black patients in the VHA system less likely to undergo evidence‐based cardiovascular procedures, we must be diligent to avoid such disparities in RDN as this new treatment becomes increasingly available [20, 21]. Our study would suggest if such disparities were to arise in referral practices for RDN or treatment with RDN at our center, they would be less likely due to differences in patient preferences.
Similar to other populations, Veterans with comorbid CHF were significantly more likely to prefer RDN [11]. The underpinnings of this association are unclear, but it has been suggested that this may be related to the symptomatic nature of CHF as well as increased motivation to control blood pressure due to a better understanding of the negative effects of hypertension [11]. A shared decision‐making model could lean more favorably toward RDN for patients with CHF given evidence for the therapeutic potential of RDN in this disease process and these patient preference data [11, 22, 23]. This may be a subset of the difficult‐to‐control hypertension population that warrants targeted referral efforts for RDN.
While other studies found male sex, younger patients, and patients who had experienced side effects as predictors of a preference for RDN, these factors were not associated with RDN preference in our study [11, 12, 16]. However, our population was older, much more predominately male, and less likely to have experienced side effects, which likely contributes to our findings.
Comorbid diabetes mellitus and uncontrolled SBP (> 129 mmHg) on most recent clinic measurements were associated with a preference against RDN. Prior studies are mixed as to the role and predictability of uncontrolled blood pressure measurements on preference for or against RDN [10, 11, 12, 16, 24]. Further investigation is needed to elucidate this association and understand a preference against RDN.
Understanding patient preferences may improve efficiency of use and access for procedural treatment options such as RDN [25]. When escalation of treatment is indicated in patients with uncontrolled hypertension, there is an opportunity for investigating patient preferences, patient choice, and creating space in the hypertension treatment pathway for RDN [10, 12, 26, 27]. Respondents in our study indicated a higher preference for RDN (64.7%) over an additional medication (35.3%) if their blood pressure were uncontrolled, compared to ~30%–40% preference for RDN seen in prior studies. We hypothesize higher rates of poor medication adherence in our population as well as high levels of patient trust and satisfaction in the VHA system among other factors may contribute to this difference [28, 29, 30].
This study identified an association between medication adherence and RDN preference. Respondents with a preference for RDN had significantly lower MARS‐5 scores indicating worse adherence than respondents with a preference against RDN. Additionally, those with poor medication adherence were more likely to select RDN over an additional pill. Prior studies demonstrated a similar link, however had not utilized MARS‐5 as a simple, quick, and validated measure of adherence [11, 12, 16, 31]. These data provide further evidence of the opportunity for RDN in patients who struggle with adherence to daily medication regimens [32, 33, 34, 35]. Medication adherence measures, such as MARS‐5, may help inform and predict patient preference and improve efficiency in referral practices for RDN.
4.1. Limitations
This study was limited to a small sample of patients with difficult‐to‐control hypertension from a single VA medical center with uniquely diverse demographics. The preferences of patients at other centers or with hypertension on less or no medications may differ. Patient preferences may differ when decisions and treatment options are no longer theoretical. Telephone survey administration does have some shortcomings, such as time constraints, sample biases, lower response rates, and inability to provide visual aid. As a telephone call does not replace patient–physician discussions, explanation, or the consent process regarding procedures such as RDN, this study is limited to evaluation of initial preferences and factors associated with preferences regarding RDN and hypertension care, not data or definitive conclusions on whether these patients would undergo the procedure or not. There was no health literacy test, knowledge test, or confirmation of understanding of risks and benefits of RDN or risks of uncontrolled hypertension included in this survey study. Surveys were not administered to patients by their medical provider; trustworthiness and, therefore, responses and preferences may differ if information is presented by the provider managing their care or with whom they have an established relationship. As noted above, the sample size was small with 51 respondents and did have significant sex differences with 49 male and only 2 female respondents. Therefore, this study is limited by potential bias by sex differences and conclusions are limited to a predominantly male sample given male sex was a factor associated with a preference for RDN in prior study [11, 12]. Further research with a larger sample size and increased female representation would be beneficial.
5. Conclusion
In this study, we observed a sizable portion of Veterans with difficult‐to‐control hypertension would prefer RDN if their blood pressure were uncontrolled or if recommended by their doctor. In addition, we noted CHF and medication adherence as associated with a preference for RDN. Patient preferences are informative in shared decision‐making for the treatment of hypertension. Understanding patient preferences may help to improve efficiency, access, and potentially outcomes of RDN. Further study is warranted to explore these findings in broader Veteran populations. Additionally, in‐depth investigation is needed to elucidate the causal processes underlying the observed associations and the factors influencing Veterans' treatment preferences.
Author Contributions
Benjamin L. Magod: conceptualization, data curation, formal analysis, investigation, methodology, project administration, writing – original draft, writing – review and editing. Peter A. Glynn: supervision, writing – review and editing. Wesley J. Manz: formal analysis, methodology. Pal V. Shah: investigation, methodology, project administration, writing – review and editing. Mladen I. Vidovich: conceptualization, formal analysis, investigation, methodology, project administration, resources, supervision, writing – original draft, writing – review and editing.
Ethics Statement
This study received IRB exemption.
Conflicts of Interest
The authors declare no conflicts of interest.
Transparency Statement
The lead author Mladen I. Vidovich affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained.
Acknowledgments
The authors have nothing to report.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
- 1. Mills K. T., Stefanescu A., and He J., “The Global Epidemiology of Hypertension,” Nature Reviews Nephrology 16 (2020): 223–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Washington D. L., ed., National Veterans Health Equity Report 2021. Focus on Veterans Health Administration Patient Experience and Health Care Quality (Washington, DC: VHA Office of Health Equity, 2022). [Google Scholar]
- 3. Yamada M., Wachsmuth J., Sambharia M., et al., “The Prevalence and Treatment of Hypertension in Veterans Health Administration, Assessing the Impact of the Updated Clinical Guidelines,” Journal of Hypertension 41 (2023): 995–1002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. J. T. Wright, Jr. , Whelton P. K., and Reboussin D. M., “A Randomized Trial of Intensive Versus Standard Blood‐Pressure Control,” New England Journal of Medicine 374 (2016): 2294. [DOI] [PubMed] [Google Scholar]
- 5. Azizi M., Sanghvi K., Saxena M., et al., “Ultrasound Renal Denervation for Hypertension Resistant to a Triple Medication Pill (RADIANCE‐HTN TRIO): A Randomised, Multicentre, Single‐Blind, Sham‐Controlled Trial,” Lancet 397 (2021): 2476–2486. [DOI] [PubMed] [Google Scholar]
- 6. Azizi M., Schmieder R. E., Mahfoud F., et al, “Endovascular Ultrasound Renal Denervation to Treat Hypertension (RADIANCE‐HTN SOLO): A Multicentre, International, Single‐Blind, Randomised, Sham‐Controlled Trial,” Lancet 391 (2018): 2335–2345. [DOI] [PubMed] [Google Scholar]
- 7. Kandzari D. E., Böhm M., Mahfoud F., et al., “Effect of Renal Denervation on Blood Pressure in the Presence of Antihypertensive Drugs: 6‐Month Efficacy and Safety Results From the SPYRAL HTN‐ON MED Proof‐of‐Concept Randomised Trial,” Lancet 391 (2018): 2346–2355. [DOI] [PubMed] [Google Scholar]
- 8. Mahfoud F., Kandzari D. E., Kario K., et al., “Long‐Term Efficacy and Safety of Renal Denervation in the Presence of Antihypertensive Drugs (SPYRAL HTN‐ON MED): A Randomised, Sham‐Controlled Trial,” Lancet 399 (2022): 1401–1410. [DOI] [PubMed] [Google Scholar]
- 9. Hess E. P., Coylewright M., Frosch D. L., and Shah N. D., “Implementation of Shared Decision Making in Cardiovascular Care: Past, Present, and Future,” Circulation: Cardiovascular Quality and Outcomes 7 (2014): 797–803. [DOI] [PubMed] [Google Scholar]
- 10. Kandzari D. E., Weber M. A., Poulos C., et al., “Patient Preferences for Pharmaceutical and Device‐Based Treatments for Uncontrolled Hypertension: Discrete Choice Experiment,” Circulation: Cardiovascular Quality and Outcomes 16 (2023): e008997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kario K., Kagitani H., Hayashi S., Hanamura S., Ozawa K., and Kanegae H., “A Japan Nationwide Web‐Based Survey of Patient Preference for Renal Denervation for Hypertension Treatment,” Hypertension Research 45 (2022): 232–240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Schmieder R. E., Högerl K., Jung S., Bramlage P., Veelken R., and Ott C., “Patient Preference for Therapies in Hypertension: A Cross‐Sectional Survey of German Patients,” Clinical Research in Cardiology 108 (2019): 1331–1342. [DOI] [PubMed] [Google Scholar]
- 13. Chan A. H. Y., Horne R., Hankins M., and Chisari C., “The Medication Adherence Report Scale: A Measurement Tool for Eliciting Patients' Reports of Nonadherence,” British Journal of Clinical Pharmacology 86 (2020): 1281–1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sandy R. and Connor U., “Variation in Medication Adherence Across Patient Behavioral Segments: A Multi‐Country Study in Hypertension,” Patient Preference and Adherence 9 (2015): 1539–1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Assari S., “Veterans and Risk of Heart Disease in the United States: A Cohort With 20 Years of Follow Up,” International Journal of Preventive Medicine 5 (2014): 703–709. [PMC free article] [PubMed] [Google Scholar]
- 16. Lin S.‐I., Li S. H.‐W., Lan W.‐R., Liao F.‐C., Tsai C. T., and Lee Y.‐H., “Understanding the Patient Preference for Catheter‐Based Hypertension Therapy: A Pilot Study for Physician Awareness of Patients' Behavior in Taiwan,” Journal of the American College of Cardiology 75 (2020): 3586. [Google Scholar]
- 17. Conner C. J., Khan B., Laragh A., et al., Health Equity for Black Veterans (Jesse Brown Veterans Affairs Medical Center, 2022).
- 18. Wong M. S., Hoggatt K. J., Steers W. N., et al., “Racial/Ethnic Disparities in Mortality Across the Veterans Health Administration,” Health Equity 3 (2019): 99–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Vespa J. E., Armstrong D. M., and Medina L., Demographic Turning Points for the United States: Population Projections for 2020 to 2060 (US Department of Commerce, Economics and Statistics Administration, US Census Bureau, 2018).
- 20. Capers Q. and Sharalaya Z., “Racial Disparities in Cardiovascular Care: A Review of Culprits and Potential Solutions,” Journal of Racial and Ethnic Health Disparities 1 (2014): 171–180. [Google Scholar]
- 21. Peterson E. D., “Racial Variation in Cardiac Procedure Use and Survival Following Acute Myocardial Infarction in the Department of Veterans Affairs,” JAMA 271 (1994): 1175–1180. [PubMed] [Google Scholar]
- 22. Fukuta H., Goto T., Wakami K., and Ohte N., “Effects of Catheter‐Based Renal Denervation on Heart Failure With Reduced Ejection Fraction: A Systematic Review and Meta‐Analysis,” Heart Failure Reviews 22 (2017): 657–664. [DOI] [PubMed] [Google Scholar]
- 23. Kresoja K.‐P., Rommel K.‐P., Fengler K., et al., “Renal Sympathetic Denervation in Patients With Heart Failure With Preserved Ejection Fraction,” Circulation: Heart Failure 14 (2021): e007421. [DOI] [PubMed] [Google Scholar]
- 24. Schmieder R. E., Kandzari D. E., Wang T.‐D., Lee Y.‐H., Lazarus G., and Pathak A., “Differences in Patient and Physician Perspectives on Pharmaceutical Therapy and Renal Denervation for the Management of Hypertension,” Journal of Hypertension 39 (2021): 162–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. US Food and Drug Administration , ed., Patient Preference Information ‐ Voluntary Submission, Review in Premarket Approval Applications Humanitarian Device Exemption Applications, and De Novo Requests, and Inclusion in Decision Summaries and Device Labeling (US Food and Drug Administration, 2016). [Google Scholar]
- 26. Mancia G., Kreutz R., Brunström M., et al., “2023 ESH Guidelines for the Management of Arterial Hypertension The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension: Endorsed by the International Society of Hypertension (ISH) and the European Renal Association (ERA),” Journal of Hypertension 41 (2023): 1874–2071. [DOI] [PubMed] [Google Scholar]
- 27. Wang T.‐D., “Patient Preference: Messages for the Wider Adoption of Renal Denervation in the Real World,” Hypertension Research 45 (2022): 244–245. [DOI] [PubMed] [Google Scholar]
- 28. Center for Medicare & Medicaid Services , Survey of Patients' Experiences (HCAHPS). Hospital Consumer Assessment of Healthcare Providers and Systems (Center for Medicare & Medicaid Services, 2024), data.cms.gov. [Google Scholar]
- 29. US Department of Veterans Affairs , ed., Serving America's Veterans Trust Report (US Department of Veterans Affairs, 2023), va.gov. [Google Scholar]
- 30. O'Hanlon C., Huang C., Sloss E., et al., “Comparing VA and Non‐VA Quality of Care: A Systematic Review,” Journal of General Internal Medicine 32 (2017): 105–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Lin S.‐I., Li S. H.‐W., Lan W.‐R., Liao F.‐C., Tsai C. T., and Lee Y.‐H., “Subtypes of Patient Preference for Catheter‐Based Hypertension Therapy: A Pilot Study Based on Taiwan Consensus on Renal Denervation (RDNI2),” Journal of the American College of Cardiology 75 (2020): 3507. [Google Scholar]
- 32. Barbato E., Azizi M., Schmieder R. E., et al., “Renal Denervation in the Management of Hypertension in Adults. A Clinical Consensus Statement of the ESC Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI),” European Heart Journal 44 (2023): 1313–1330. [DOI] [PubMed] [Google Scholar]
- 33. Fisher N. D. L. and Mahfoud F., “Medication Adherence in Hypertension: Lessons Learned From Renal Denervation Trials,” European Journal of Preventive Cardiology 30 (2023): 34–36. [DOI] [PubMed] [Google Scholar]
- 34. Schmieder R. E., Mahfoud F., Mancia G., et al., “European Society of Hypertension Position Paper on Renal Denervation 2021,” Journal of Hypertension 39 (2021): 1733–1741. [DOI] [PubMed] [Google Scholar]
- 35. Swaminathan R. V., East C. A., Feldman D. N., et al., “SCAI Position Statement on Renal Denervation for Hypertension: Patient Selection, Operator Competence, Training and Techniques, and Organizational Recommendations,” Journal of the Society for Cardiovascular Angiography & Interventions 2 (2023): 101121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


