Abstract
Aim
Xerostomia is defined as a subjective complaint of dry mouth and is a prevalent condition. The study aims to estimate the cut point of the xerostomia inventory (XI) questionnaire for diagnosing dry mouth based on a saliva test.
Method
This prospective study was conducted in Dentistry School of Kerman University of Medical Sciences. Eligibility criteria included individuals aged 40 and above who were capable of undergoing saliva testing. For each randomly selected participants, a non-stimulating saliva test as a reference test was taken between 9:00 AM and 12:00 PM. Participants were asked to avoid eating, drinking and smoking 60 min before and during the test. For 5 min, the patient poured the accumulated saliva in his mouth every 1 min by bending forward into the container. If the collected saliva was less than 0.1 ml during 1 min, the participant was diagnosed with dry mouth. The Persian version of the XI questionnaire as an index test was used to calculate the xerostomia score, which was determined by summing the scores for each question. The diagnostic power of the questionnaire was assessed using receiver operating characteristic curve, and Youden index was utilized to identify the positivity cut off point.
Results
In this research, 120 people who referred to the Faculty of Dentistry in 2022–2023 who were participated. Of all participants, 50% in the study were women. The average age of the participants in the study was 50.2 ± 7.2 years. Among the participants, 40 experienced dry mouth. The positivity cut-off point for the diagnosis of dry mouth was xerostomia score greater than 23.5, which has a sensitivity of 82.5% and a specificity of 81.5%. The area under curve for the questionnaire was 0.898.
Conclusions
The XI questionnaire cut point of 23.5 demonstrated high sensitivity and specificity for diagnosing dry mouth in individuals over 40 years old. Results for specific age or gender subgroups should be interpreted with caution.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12903-025-05576-4.
Keywords: Xerostomia, Dry mouth, Saliva test, Xerostomia Inventory questionnaire, Receiver operating characteristic, Youden index
Introduction
Individuals may experience Xerostomia, the subjective feeling of dry mouth, even without a significant decrease in salivary volume [1]. This condition can cause to a sensation of burning in the mouth, difficulty in swallowing [2]. Prolonged saliva reduction may cause to dental caries, periodontal disease, oral ulcers, fungal infections (such as candidiasis), and challenges with artificial dentures [3].
Xerostomia prevalence estimates in the general population vary significantly due to differences in measurement, case definitions, and study characteristics, ranging from 5.5% to 46% [4]. A high prevalence of dry mouth has been reported in the elderly, with Johnson et al. estimating it at 33.3% among older adults [5]. Additionally, xerostomia is often a side effect of certain medications, affecting about 30% of users, and is also prevalent in individuals with systemic diseases [6, 7].
Xerostomia is assessed using standard questionnaires, such as the Fox and Xerostomia Inventory(XI) [8, 9]. Recently, Xerostomia Inventory the questionnaire has gained widespread use in studies. There are two versions of the Xerostomia Inventory Questionnaire: the original Xerostomia Inventory [7] and the Summated Xerostomia Inventory [10]. Both tools are designed to assess the severity of dry mouth symptoms, but they differ in structure and application. The original Xerostomia Inventory focuses on evaluating subjective experiences of xerostomia through a series of questions that address the frequency and impact of dry mouth symptoms on daily life. In contrast, the Summated Xerostomia Inventory is a streamlined version that aggregates responses into a single score, enhancing its utility for statistical analysis and clinical assessments. Both inventories have been successfully translated and validated in various languages and cultural contexts, including Portuguese, Turkish, Arabic, Thai, Hindi, Chinese, Indonesian, and Korean [11–17].
Dry mouth is clinically diagnosed based on the patient's description and physical examination, with subjective symptoms often sufficient for diagnosis and treatment initiation, even if there is no measurable decrease in saliva flow. Two primary techniques for measuring dry mouth are sialometry and sialography. Sialography, an imaging technique, can identify salivary stones or masses [18, 19], while three-dimensional sialography offers a promising diagnostic approach for patients exposed to radiation by visualizing salivary gland ducts Three-dimensional sialography is a promising diagnostic approach for patients exposed to radiation, as it can visualize salivary gland ducts [18]. Imaging conducted six weeks before and six months after radiation can assess reductions in saliva flow [20]. In sialometry technique, the stimulated flow is less than 0.5 to 0.7 ml per minute or unstimulated flow is less than 0.1 ml per minute is considered as dry mouth [21]. The stimulated saliva flow rate is normally between 1.5 to 2.0 ml per minute, whereas the unstimulated flow rate ranges from 0.3 to 0.4 ml per minute.
One of less-explored method for measuring dry mouth involves using standardized questionnaires to identify a cutoff point that predicts a decrease in saliva flow. The FOX questionnaire is the first standard questionnaire that has a cutoff point was to predict the dry mouth [9]. Xerostomia inventory questionnaire is now widely used as a valid instrument in research across various countries to assess Xerostomia. To date, no study has been conducted to determine an appropriate cutoff point for the Xerostomia inventory questionnaire based on sialometry testing. The objective of this study is to determine an appropriate cutoff point for the Xerostomia Inventory Questionnaire based on sialometry (saliva testing) to accurately diagnose a reduction in saliva secretion. We hypothesize that the Xerostomia Inventory Questionnaire has a specific cutoff point that can reliably differentiate individuals with reduced saliva secretion from those with normal saliva production, as determined by sialometry testing.
Methods
Study population
This study was prospective research conducted at Kerman city, Kerman Dental School, from March to July 2023. The study protocol was registered and approved by the institutional review board of the Kerman University of Medical Sciences. This study followed the Standards for Reporting of Diagnostic Accuracy Studies guidelines for reporting (Supplementary Table 1). To determine the sample size in this study, considering the sensitivity of the cutoff point to age and gender, it is recommended in the literature that for each variable, 10 individuals with the condition of interest and 10 individuals without the condition should be included in the study [22]. Taking into account interaction effect of age and gender, the sample size in this study is at least 60 individuals. To include 10 cases and 10 non-cases for each variable, the study's sample size was set at 120. Simple random sampling was conducted among all eligible individuals visiting Kerman Dental School. Participants provided informed consent, and their information was kept confidential.
Inclusion criteria:
Individuals aged 40 and above with the ability to undergo saliva testing.
Exclusion criteria:
any systemic disease
Unwillingness to cooperate, inability to undergo saliva testing, inability to read and write.
Data collection
The non-stimulated saliva test was used as a standard reference for diagnosing dry mouth in a previous studies [17, 23–25]. In this study, the non-stimulated saliva test were conducted for each participant between 9 AM and 12 PM. Participants were instructed to abstain from eating, drinking, and smoking 60 min before and during the test. Participants were instructed to abstain from eating, drinking, and smoking for 60 min before and during the test. Saliva was collected by having the patient comfortably seated, spitting accumulated saliva into a pre-weighed disposable container every minute for 5 min, with the patient's code recorded on the container. A saliva volume of 1.0 to 8.0 ml in 1 min is considered normal; if less than 0.1 ml is collected in 1 min, the individual is classified as having dry mouth [21].
The xerostomia questionnaire as an index test used in this study is the Persian version of the Xerostomia Inventory questionnaire, validated by Barkhordari et al. [26]. This questionnaire consists of 11 questions related to dry mouth, and responses are given on a scale of never (score 1), rarely (score 2), sometimes (score 3), most of the time (score 4), and always (score 5). This scoring was use by previous studies [10, 14, 16, 17, 27]. All individuals in this population completed the XI questionnaire, and demographic information, including age and gender, was also collected.
Statistical analysis
Descriptive statistics of participants are presented as mean ± SE and percentages. The association between age and the Xerostomia Inventory questionnaire score was assessed using Pearson correlation. The age and questionnaire scores were compared by gender and dry mouth status using an independent t-test. The maximum value of Youden Index as used to identify the positivity cut off point with high sensitivity and specificity [28]. Among points with similar Youden Index values, the positivity cut off point with sensitivity and specificity above 80% will be selected. The diagnostic power of the questionnaire will be determined using the Receiver Operating Characteristic (ROC) curve, with values above 0.7 indicating acceptable diagnostic power [29]. Sensitivity and specificity will then be calculated overall and for different age and gender subgroups to assess variability in diagnostic accuracy.
Results
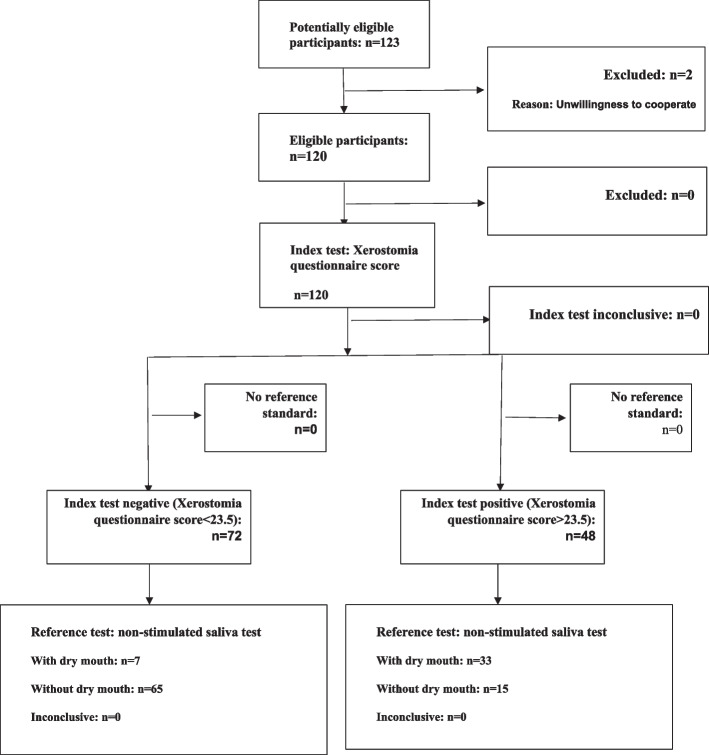
In this study, 123 individuals attending the School of Dentistry in Kerman from 1401 to 1402 were randomly selected, with 120 meeting the inclusion and exclusion criteria. The flow of participants was presented in Fig. 1. Participants' ages ranged from 40 to 69 years, with a mean age of 50.2 ± 7.2 years, and 60.8% were female. The XI questionnaire scores ranged from a minimum of 11 to a maximum of 38, with a mean score of 22.3 ± 6.5. There was no significant difference in XI scores between genders (P = 0.927) Those with dry mouth had a significantly higher XI score, averaging 9.2 units more than those without dry mouth (P < 0.001) (Table 1). No significant correlation was found between XI score and age (r = 0.127, P = 0.921).
Fig. 1.
Flow of participants through the study by Xerostomia questionnaire score as index test and non-stimulated saliva test as reference test
Table 1.
Descriptive statistics of participants characteristics
| Age | P-value |
Xerostomia inventory score |
P-value | |||
|---|---|---|---|---|---|---|
| Gender | Female | 81(67.5%) | 49.7 ± 3.7 | P = 0.323 | 21.2 ± 7.5 | P = 0.927 |
| Male | 39(32.5%) | 51.2 ± 5.7 | 24.5 ± 4.5 | |||
| Dry mouth | Had | 40(33.3%) | 57.7 ± 5.7 | P = 0.135 | 28.4 ± 3.2 | P < 0.001 |
| Not Had | 80(66.6%) | 46.5 ± 3.7 | 19.25 ± 7.2 | |||
| Total | 120 | 50.2 ± 7.2 | 22.3 ± 6.5 |
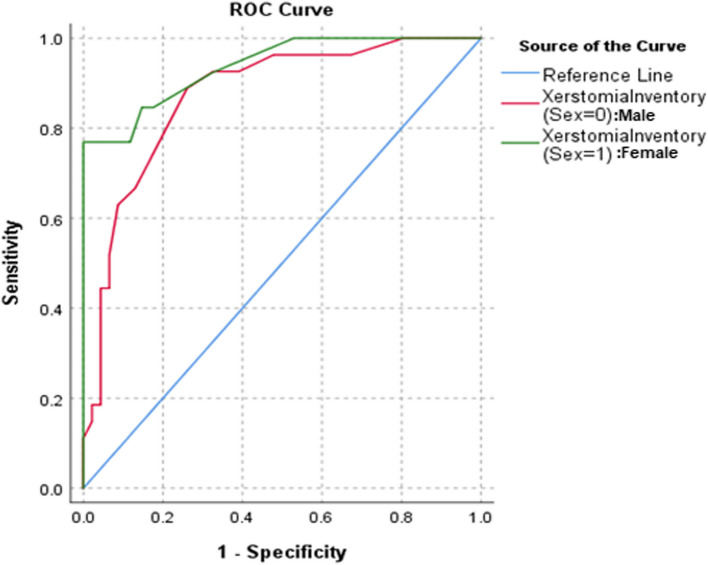
To assess the diagnostic power of the questionnaire, a ROC curve was utilized, yielding an AUC of 0.898 (95% CI = (0.839, 0.958)), indicating a significantly better-than-chance ability to predict disease (Figs. 2 and 3). Sensitivity and specificity for various cutoff points are presented in Table 1. The cutoff point of 22.5 had the highest Youden's index (0.650), with both sensitivity and specificity at 87.5%. The next highest cutoff point, 23.5, had a Youden's index of 0.635, with sensitivity at 82.5% and specificity at 81.5%. Since both sensitivity and specificity at the cutoff point of 23.5 were above 80%, this point was considered optimal (Table 2).
Fig. 2.
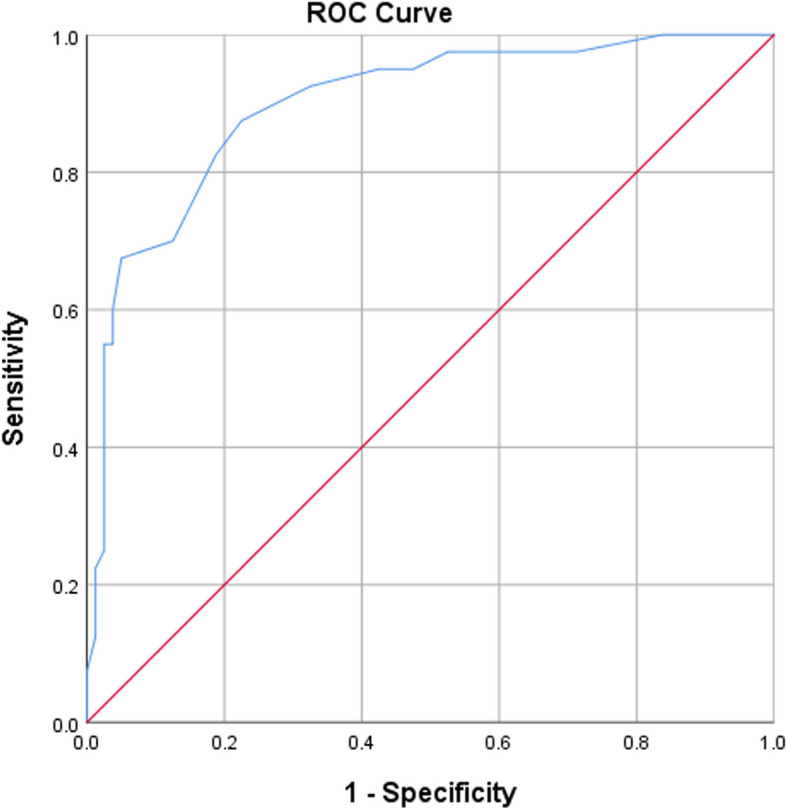
Rock curve of xerostomia inventory questionnaire score for predicting clinical dry mouth
Fig. 3.
Rock curve of xerostomia inventory questionnaire score for predicting clinical dry mouth in males and females
Table 2.
Sensitivity, specificity and Youden index for different cut-off points
| Cut point | Sensitivity | 1—Specificity | Youden Index |
|---|---|---|---|
| 10 | 1 | 1 | 0.000 |
| 11.5 | 1 | 0.988 | 0.012 |
| 12.5 | 1 | 0.95 | 0.050 |
| 13.5 | 1 | 0.888 | 0.112 |
| 14.5 | 1 | 0.838 | 0.162 |
| 15.5 | 0.975 | 0.713 | 0.262 |
| 16.5 | 0.975 | 0.675 | 0.300 |
| 17.5 | 0.975 | 0.575 | 0.400 |
| 18.5 | 0.975 | 0.525 | 0.450 |
| 19.5 | 0.95 | 0.475 | 0.475 |
| 20.5 | 0.95 | 0.425 | 0.525 |
| 21.5 | 0.925 | 0.325 | 0.600 |
| 22.5 | 0.875 | 0.225 | 0.650 |
| 23.5 | 0.825 | 0.188 | 0.637 |
| 24.5 | 0.775 | 0.162 | 0.613 |
| 25.5 | 0.7 | 0.125 | 0.575 |
| 26.5 | 0.675 | 0.05 | 0.625 |
| 27.5 | 0.6 | 0.037 | 0.563 |
| 28.5 | 0.55 | 0.037 | 0.513 |
| 29.5 | 0.55 | 0.025 | 0.525 |
| 30.5 | 0.425 | 0.025 | 0.400 |
| 31.5 | 0.25 | 0.025 | 0.225 |
| 32.5 | 0.225 | 0.012 | 0.213 |
| 33.5 | 0.125 | 0.012 | 0.113 |
| 34.5 | 0.075 | 0 | 0.075 |
| 36 | 0.05 | 0 | 0.050 |
| 37.5 | 0.025 | 0 | 0.025 |
| 39 | 0 | 0 | 0.000 |
The comparison of the area under the ROC curve across age and gender subgroups revealed no statistically significant differences (Table 3). The optimal cutoff points were 28 for men and 24 for women, with men showing a sensitivity of less than 80%. For individuals under 50, the cutoff was 23.5, while for those aged 50 and older, it was 26.5, also with a sensitivity below 80% (Table 3). For individuals under 55, the cutoff was 22.5, and for those 55 and older, it was 25.5. In individuals under 60, the cutoff was 23.5, and for those 60 and older, it was 26.5, both demonstrating a sensitivity and specificity greater than 80% (Table 3).
Table 3.
Sensitivity, specificity, Yuden index, and area under the curve for various cutoff points of the xerostomia inventory questionnaire score in diagnosing dry mouth
| Sub group | Category | cut-off point | Sensitivity | Specificity | YUDEN index | P_value1 |
|---|---|---|---|---|---|---|
| Sex | Male | 28 | 76.9% | 100% | 0.769 | P = 0.260 |
| Female | 24 | 84.60% | 82.40% | 0.699 | ||
| Age | < 50 | 23.5 | 90.90% | 87.50% | 0.759 | |
| > = 50 | 26.5 | 61.10% | 95% | 0.561 | ||
| < 55 | 22.5 | 86.20% | 82.70% | 0.689 | P = 0.821 | |
| > = 55 | 25.5 | 81.80% | 82.10% | 0.692 | ||
| < 60 | 23.5 | 82.90% | 80.90% | 0.667 | P = 0.720 | |
| > = 60 | 26.5 | 80% | 100% | 0.8 |
1P-value calculated for comparing the area under the curve in subgroups
Discussion
In this study, the optimal cutoff point for diagnosing dry Mouth was determined to be 23.5, with a sensitivity and specificity above 80%, respectively. The area under ROC curve for xerostomia inventory questionnaire was found to be high. Importantly, the results revealed that individuals with dry mouth scored significantly higher on the questionnaire, reflecting the tool's effectiveness in distinguishing between xerostomia and non-xerostomia cases. Additionally, the findings suggest that while cutoff points vary by gender and age, the overall area under curve of the questionnaire remains consistent across different demographics. This study highlights the necessity for gender-specific thresholds, as men exhibited higher cutoff points, indicating a more intense perception of dry mouth compared to women. Also, the increase in cutoff points with age suggests that older individuals may be more aware of their symptoms.
Dry mouth is a prevalent challenge for older individuals. Researchers have struggled to accurately measure its prevalence using precise tools. This study utilized the Xerostomia Inventory questionnaire, one of the most widely used instruments in this field, to identify the optimal cutoff point for diagnosing clinical dry mouth. The significance of this study is that the established cutoff point can reliably estimate the prevalence of clinical dry mouth in various populations with minimal cost and time.
The translated Persian version of the xerostomia inventory questionnaire used in this study has been validated by Barkhordari et al. [26]. The Cronbach's alpha coefficient for this questionnaire was 0.84, and the intra-cluster correlation coefficient (ICC) for the total score of the questionnaire was 0.95, indicating good internal consistency and reliability over time. The retest reliability after two weeks yielded a coefficient of 0.95. Concurrent validity of the questionnaire was assessed with a strong significant correlation (0.85) between the total score of the questionnaire and the response to the single question "Do you ever feel oral dryness?” Similar results were obtained in the German [11], Portuguese [12], and Korean [13] versions of the questionnaire.
The ROC curve in this study for the questionnaire was 0.898, indicating excellent diagnostic power. Generally, values between 0.7 to 0.8 are considered acceptable, 0.8 to 0.9 are excellent, and above 0.9 are considered outstanding [4]. Similar studies on this questionnaire have not been conducted to date. The abbreviated Indonesian version achieved an ROC curve of 0.985, consistent with our findings [30].
The optimal cutoff point for diagnosing dry mouth in this study was determined to be 22.5. To date, no study has been conducted to determine the cutoff point for diagnosing oral dryness based on the xerostomia inventory questionnaire. The abbreviated Indonesian version had a cutoff point of 11 [30]. Considering the possible score range for the abbreviated questionnaire is 5–25, the cutoff point of 11 can be considered a median for this questionnaire. In this study, the possible score range for the questionnaire was 11 to 55, and 23.5 was considered the median cutoff point for this questionnaire. Thus, the results of these two studies can be considered consistent. The sensitivity and specificity obtained for the abbreviated Indonesian version with a sample size of 60 were 96% and 100%, respectively. In this study, the sensitivity was 82.5%, and specificity was 81.5%. Higher sensitivity and specificity in the abbreviated Indonesian version may be due to its smaller sample size.
Our findings indicate that although the diagnostic cutoff point may differ by gender, the test's overall ability to distinguish between xerostomia and non-xerostomia cases remains consistent. The higher cutoff point for men suggests they perceive dry mouth more intensely than women. The increased specificity in men at the optimal cutoff may indicate a stricter threshold for identifying true negatives, while the higher sensitivity in women may focus on identifying true positives. This gender variation underscores the necessity for sex-specific thresholds to improve diagnostic accuracy in studies focused on men or women.
In our study the cutoff points increased as age increased. For individuals under 50 years, the optimal cutoff was 23.5, while for those over 50 years, it increased to 25.5. Similarly, for participants under 55 years, the cutoff was 22.5 whereas for those over 55 years, it was 26.5. For individuals under and 60 years, the cutoff remained 23.5 and 26.5. However, no significant differences in AUC were observed between age groups under and over 50, 55, or 60 years. These findings suggest that while age influence the optimal cutoff points, the overall diagnostic accuracy of the XI questionnaire remains consistent across these subgroups. The reason for dependency of age and cutoff points may be that older individuals feel more dry mouth and express it more frequently. This was reflected in the higher sensitivity at younger ages and higher specificity at older ages. Additionally, our study did not have an large sample size for examining the cutoff points in these subgroups. Therefore, it is recommended that future studies repeat this study with larger sample sizes in the age subgroups.
One of the main limitations of our study was the limited sample size. Due to the time-consuming nature of the research and a lack of cooperation from participants, we were unable to include a larger sample. Therefore, future studies are recommended to conduct research with larger sample sizes, particularly in specific age and gender subgroups. It is important to analyze the sensitivity and specificity of individual questions and their combinations in large studies to identify the subset that provides the best results in terms of sensitivity and specificity.
Conclusion
The diagnostic power of the xerostomia inventory questionnaire for diagnosing clinical dry mouth is 89.8%. The cutoff point for the XI questionnaire is 23.5, with a sensitivity and specificity of 82.5% and 81.5%, respectively.
Supplementary Information
Acknowledgements
The authors would like to thank and appreciate everyone who contributed to this research.
Authors’ contributions
Conceptualization, Data curation was done by Shahla Kakooei, Amir H. Nekouei. Data was collected by Donya Pourjahanshah. The data was analyzed and interpreted by Amir H. Nekouei and Ali Akbar Haghdoost. All authors did original Drafting and editing. All authors read and approved the final manuscript.
Funding
Research reported in this manuscript was partially funded through Kerman university of medical sciences.
Data availability
The data that support the findings of this study are available from the Kerman University of Medical Sciences, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Upon reasonable request and and with permission of the Kerman University of Medical Sciences the data will be available from the corresponding author.
Declarations
Ethics approval and consent to participate
This study was carried out in accordance with the Declaration of Helsinki and informed consent was obtained from all study participants. The study was approved by the Research Council of Kerman University of Medical Sciences (Ethical code: IR.KMU.REC.1401.398).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Amir Hossein Nekouei, Email: nekouei.amir@gmail.com.
Shahla Kakoei, Email: skakoei@gmail.com.
References
- 1.López-Pintor RM, Ramírez Martínez-Acitores L, Serrano Valle J, González-Serrano J, Casañas E, de Arriba L, et al. Xerostomia and Hyposalivation. In: Hogue C-M, Ruiz JG, editors., et al., Oral Health and Aging. Cham: Springer International Publishing; 2022. p. 85–108. [Google Scholar]
- 2.Hummelsheim M-Z, Hamacher S, Hagemeier A, Noack MJ, Barbe AG. Care need and dry mouth as risk indicators for impaired taste and smell. Sci Rep. 2021;11(1):20419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nagarajan H, Gunasekaran T. Xerostomia diagnosis and management. 2022.
- 4.Mandrekar JN. Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol. 2010;5(9):1315–6. [DOI] [PubMed] [Google Scholar]
- 5.Pina GdMS, MotaCarvalho R, Silva BSdF, Almeida FT. Prevalence of hyposalivation in older people: a systematic review and meta-analysis. Gerodontology. 2020;37(4):317–31. [DOI] [PubMed] [Google Scholar]
- 6.von Bültzingslöwen I, Sollecito TP, Fox PC, Daniels T, Jonsson R, Lockhart PB, et al. Salivary dysfunction associated with systemic diseases: systematic review and clinical management recommendations. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:S57.e1-S.e15. [DOI] [PubMed] [Google Scholar]
- 7.Thomson WM, Chalmers JM, Spencer AJ, Williams SM. The Xerostomia Inventory: a multi-item approach to measuring dry mouth. Community Dent Health. 1999;16(1):12–7. [PubMed] [Google Scholar]
- 8.Khalid A, Elahi S, Qurban A, Atif S. Xerostomia diagnosis - A narrative review. J Pak Dent Assoc. 2021;31(1):49–54.
- 9.Fox PC, Busch KA, Baum BJ. Subjective reports of xerostomia and objective measures of salivary gland performance. J Am Dent Assoc (1939). 1987;115(4):581–4. [DOI] [PubMed] [Google Scholar]
- 10.Thomson WM, van der Putten GJ, de Baat C, Ikebe K, Matsuda K, Enoki K, et al. Shortening the xerostomia inventory. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;112(3):322–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hohenberger R, Baumann I, Plinkert PK, Brinster R, Krisam J, Affolter A, et al. Validating the Xerostomia Inventory in a radiation-induced xerostomia population in German language. Oral Dis. 2019;25(7):1744–50. [DOI] [PubMed] [Google Scholar]
- 12.da Mata AD, da Silva Marques DN, Freitas FM, de Almeida RatoAmaral JP, Trindade RT, Barcelos FA, et al. Translation, validation, and construct reliability of a Portuguese version of the Xerostomia Inventory. Oral Dis. 2012;18(3):293–8. [DOI] [PubMed] [Google Scholar]
- 13.Lee J, Koh JH, Kwok SK, Park SH. Translation and validation of a Korean version of the Xerostomia Inventory in patients with primary Sjögren’s Syndrome. J Korean Med Sci. 2016;31(5):724–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gupta S, Dhawan P, Tandan P, Jain M. Validity and reliability of the Hindi version of the Summated Xerostomia Inventory-5 among head and neck cancer irradiated patients in Delhi, India. J Cancer Res Ther. 2022;18(Supplement):S165–9. [DOI] [PubMed] [Google Scholar]
- 15.Lapnimitanun C, Wiriyakijja P, Matangkasombut O, Komin O. Cross-cultural adaptation of the Thai Xerostomia Inventory and Summated Xerostomia Inventory. Oral Dis. 2024;30(7):4331–40. [DOI] [PubMed] [Google Scholar]
- 16.Alqaryan S, Almousa H, Almeshari S, Abaalkhail MB, Alabdulkareem AM, Alotaibi S, et al. Translation and Cross-Cultural Adaptation of an Arabic Version of the Summated Xerostomia Inventory. Cureus. 2023;15(10):e47546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wimardhani YS, Rahmayanti F, Maharani DA, Mayanti W, Thomson WM. The validity and reliability of the Indonesian version of the Summated Xerostomia Inventory. Gerodontology. 2021;38(1):82–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nadler C. Standardization of terminology, imaging features, and interpretation of CBCT sialography of major salivary glands: a clinical review. Quintessence Int. 2021;52(8):728. [DOI] [PubMed] [Google Scholar]
- 19.Hu J, Andablo-Reyes E, Mighell A, Pavitt S, Sarkar A. Dry mouth diagnosis and saliva substitutes—A review from a textural perspective. J Texture Stud. 2021;52(2):141–56. [DOI] [PubMed] [Google Scholar]
- 20.Wolff A, Joshi RK, Ekström J, Aframian D, Pedersen AM, Proctor G, et al. A guide to medications inducing salivary gland dysfunction, xerostomia, and subjective Sialorrhea: a systematic review sponsored by the World Workshop on Oral Medicine VI. Drugs R D. 2017;17(1):1–28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kurapati M, Pradusha R, Sajjan MS, Ramaraju A, Nair KC. Management of xerostomia: an overview. Trends Prosthodont Dent Implantol. 2020;10(1 & 2):20–3. [Google Scholar]
- 22.Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9. [DOI] [PubMed] [Google Scholar]
- 23.Zahed M, Azad A, Qapanchi J, Ranjbar Z, Mansourabadi P, Farpour N, et al. Prevalence of Dry Mouth (Xerostomia) and Hyposalivation in Individuals with no Oro-Dental Complications in Shiraz. Iran yums-armaghan. 2021;26(6):969–81. [Google Scholar]
- 24.Grossmann S, de Oliveira G, Teixeira R, do Carmo VM. Stimulated and non-stimulated salivary flows should be tested for the presence of HCV RNA in saliva samples from patients with chronic hepatitis C. Dentistry. 2014;4(5):1. [Google Scholar]
- 25.Carramolino-Cuéllar E, Lauritano D, Silvestre FJ, Carinci F, Lucchese A, Silvestre-Rangil J. Salivary flow and xerostomia in patients with type 2 diabetes. J Oral Pathol Med. 2018;47(5):526–30. [DOI] [PubMed] [Google Scholar]
- 26.Barkhordari Dashtkhaki M, Kakoei S, Larizadeh MH, Nekouei AH. The validity and reliability of the Persian Version of the Xerostomia Inventory Questionnaire. J Dent. 2024;25(1):26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yüce Sarı S, Yılmaz MT, Elmalı A, Kılıç L, Yüce D, Özyiğit G, et al. Turkish translation and validation of the Xerostomia Inventory. Arch Rheumatol. 2022;37(3):351–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Martínez-Camblor P, Pardo-Fernández J. The Youden Index in the Generalized Receiver Operating Characteristic Curve Context. Int J Biostat. 2019;15(1):20180060. [DOI] [PubMed]
- 29.Polo TCF, Miot HA. Use of ROC curves in clinical and experimental studies. J Vasc Bras. 2020;19:e20200186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dwipa L, Wardhani R, Setiani T, Sufiawati I, Susanti Pratiwi Y, Susandi E, et al. Summated Xerostomia Inventory to detect both xerostomia and salivary gland hypofunction. Eur Rev Med Pharmacol Sci. 2023;27(2):517–23. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available from the Kerman University of Medical Sciences, but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Upon reasonable request and and with permission of the Kerman University of Medical Sciences the data will be available from the corresponding author.