Abstract
Purpose
Aseptic loosening (AL) of prostheses is a complex and multi-factorial consequences characterized by nonspecific hip start-up pain, impaired gait, or ambulation. The AL of acetabular components associated with femur prostheses can lead to challenges in accurate diagnosis and suitable therapy, potentially resulting in disaster consequence. This study reported revision of in four cases with AL of acetabular components associated with or without femur prostheses after underwent primary total hip arthroplasty.
Case Description
We present four cases with aseptic loosening of prostheses with a medical history of total hip arthroplasty who presented obvious clinical features of recurrent hip pain or “start-up” pain, limping gait, and worsening of walking. Basing on preoperative imaging materials, and ruling out prosthetic joint infection, the comprehensive analysis revealed migration and radiolucency line around margin of prosthesis, confirming the diagnosis of prosthetic AL. All patients accepted individual revision surgery and acquired satisfactory results basing on the month telephone follow-up duration.
Conclusion
Our case report suggests long femur stem associated with wires cerclage fixation combined with or without bone graft revision for treatment of aseptic loosening of the acetabular components coupled with femur prostheses is a viable technique for achieving reliable fracture healing and satisfactory clinical results. Besides, it is the critical need for individualized approaches to therapeutic method, uniquely intended to address the complexity of this AL after THA.
Keywords: aseptic loosening, total hip arthroplasty, revision surgery, radiolucency line, periprosthetic fracture
Introduction
As a common cause of revision, total hip arthroplasty (THA), aseptic loosening (AL) of the acetabular components associated with femur prostheses remains a significant challenge for arthroplasty surgeons.1 Moreover, AL lead to present a significant medical or economic burden to both patient and society. While the diagnosis of AL is relatively well defined, the management modality of AL for acetabular components along with femur prostheses following primary THA remains a challenge.2 The purpose of our study aims to report management modality in four cases diagnosed with aseptic loosening of acetabular components along with femur prostheses after THA.
Materials and Methods
Ethical Statement
The subjects in our study are four individuals (Female 3, Male 1) who presented with aseptic loosening of the acetabular components coupled with or without femur prostheses after primary THA (Table 1). This study was approved by the Ethics Committee of Hunan University of Medicine General Hospital. Medical messages were obtained from all patients, and written informed consents were obtained from the patient of this study.
Table 1.
The Details of Cases in Our Study
| Items | Gender | Age (Years) | PMH | CRP (mg/L) | ESR (mm/H) | LL (10^9/L) | NG (%) | IL-6 (pg/mL) | Operation Program | Radiological Features | Clinical Features | Types of Loosening | Analgesic Plan |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 1 | Male | 72 | Femoral head necrosis | 1.7 | 11 | 9.8 | 65.6 | 0.708 | Using of new acetabular cup and femoral stem combined with wires cerclage fixation | Acetabular screw rupture, vertical subsidence and varus angulation of the femoral prostheses | Persistent hip pain; Limping gait | Loosening of acetabular cup and femoral stem | Oral non-steroidal anti-inflammatory drugs and Tramadol tablets |
| Case 2 | Female | 64 | None | 1 | 12 | 7.0 | 75.7 | 0.967 | Using of new acetabular cup and femoral stem combined with additional wires fixation and acetabular screws | Radiolucencies at the bone-implant interface and acetabulum-prostheses interface | The “start-up” pain in hip | Loosening of acetabular cup and femoral stem | Oral non-steroidal anti-inflammatory drugs |
| Case 3 | Female | 57 | Femoral head necrosis | 0.73 | 15 | 6.2 | 66.4 | 4.79 | Using of new acetabular cup and femoral stem, and corticocancellous allograft chips and wires fixation | Cortical osteolysis and medial bone resorption; Pedestal sign | Hip pain; Worsening of walking | Loosening of acetabular cup and femoral stem | Oral Tramadol tablets |
| Case 4 | Female | 65 | Rheumatoid arthritis | 13.56 | 26 | 6.8 | 77.2 | 5.98 | Using of additional wires fixation combined with large size femoral prosthesis, and acetabular screws and cancellous screws along with porous acetabular cup | Migration of acetabular components with acetabular screw fracture, Radiolucency line | Hip pain; Worsening of walking | Loosening of acetabular cup and femoral stem | Oral and intravenous non-steroidal anti-inflammatory drugs |
Abbreviations: CRP, C-Reactive Protein; ESR, Erythrocyte Sedimentation Rate; IL-6, Interleukin-6; LL, Leukocyte Level; NG, Neutrophilic Granulocyte; PMH, Past Medical History.
Cases Presentation
Case 1
The patient was a 72-year-old man who was diagnosed with aseptic loosening of acetabular components along with femur prostheses after ten years of primary total hip arthroplasty. He was admitted to hospital because of persistent left hip pain and limping gait before one year. The patient had no significant other medical history. There was no abnormality in preoperative laboratory test results. A preoperative X-ray showed that osteolysis were around both the left femur prosthesis in Gruen zone 5, 6, and 7, and revealed that the cup migration (acetabular components) representing a definite sign of loosening (Figure 1). Besides, the left femoral component obvious subsidence consistent with loosening was observed by us (Figure 1). On the third day after admission, the patient underwent left hip revision. Femoral instability and cup loosening were found. Moreover, wires cerclage fixation was used to deal with intraoperative periprosthetic femoral fractures. Postoperative X-ray showed that the size and position of the acetabular components and femoral prosthesis were acceptable (Figure 1). Second month telephone follow-up proved that he had stable conditions.
Figure 1.
(a) AP Hip radiographs shows possible medialization of the acetabular cup, acetabular screw rupture, and demonstrates evidence of vertical subsidence (most obvious at the lesser trochanter) and varus angulation of the femoral prostheses, consistent with aseptic loosening and osteolysis in Gruen zone 5, 6, and 7. Additionally, linear radiolucent lytic lines can be seen in bone-prostheses interface (Red arrows). (b) Postoperative hip radiographs shows intraoperative periprosthetic femoral fracture underwent wires cerclage fixation (Yellow arrows).
Case 2
A 64-year-old female patient underwent total hip arthroplasty 8 years ago due to severe left hip osteoarthritis. She was referred to our hospital with a 1-year history of “start-up” pain while standing from a seated position and within the first few steps of walking. The patient had no significant other medical history and had normal laboratory test results. The preoperative X-ray image confirmed aseptic loosening of acetabular components along with femur prostheses due to significantly radiographic signs (Figure 2). On the fourth day after admission, the patient underwent left hip revision. In respective, the additional wires fixation and acetabular screws were used to deal with intraoperative periprosthetic fracture and aseptic loosening of acetabular component (Figure 2). A good pain alleviation and improvement of activity ability were observed by our team based on the second month telephone follow-up duration.
Figure 2.
(a) Radiolucencies at the bone-implant interface (most obvious at the lesser and larger trochanter) and acetabulum-prostheses interface are noted in AP Hip radiographic image, which are defined as signs of loosening (Red arrows). (b) Postoperative hip radiographs shows intraoperative periprosthetic femoral fracture underwent wires cerclage fixation (Yellow arrows) and larger acetabular cup combined with screws fixation.
Case 3
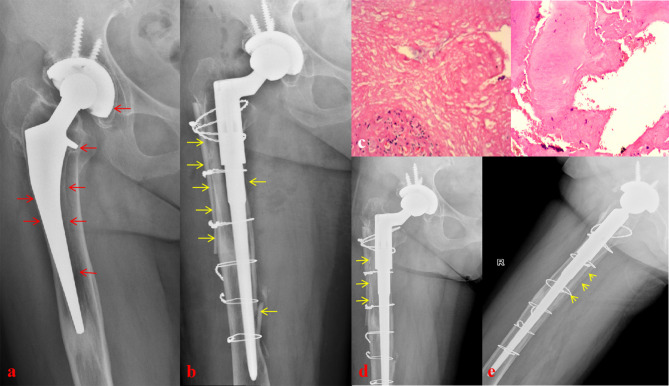
A 57-year-old female patient underwent left total hip arthroplasty 13 years ago because of femoral neck fracture. She was re-admitted to our hospital with a half of year history of right hip pain and worsening of walking. She had no history of alcohol/tobacco use or traditional herbal medicines. The preoperative X-ray image demonstrated radiolucency at the bone-implant interface, and formation of a sclerotic line (Figure 3). At the same time, radiolucency line around margin of acetabular cup was revealed by radiographs. Notably, osteolysis of both cortical bone and cancellous bone was observed in around right femur prosthesis in Gruen zone 1, 2, 3, 5, 6, and 7 (Figure 3). In Gruen zone 4, the pedestal sign was also observed (Figure 3). The suitable corticocancellous allograft chips combine with wires fixation were used to deal with lateral cortical bone defect and intraoperative periprosthetic fracture in her total hip revision surgery (Figure 3). The pathological examination revealed proliferation of aseptic inflammatory granulation tissue (Figure 3). Three months follow-up proved that she had stable conditions (Figure 3).
Figure 3.
(a) AP Hip radiographs show lateral cortical osteolysis and medial bone resorption in Gruen zone 1, 2, 3, 5, 6, and 7, and demonstrate formation of new bone and formation of a sclerotic line known as pedestal sign (Red arrows). (b) Intermediately postoperative hip radiographs show corticocancellous allograft chips combine with wires fixation which are used to deal with lateral cortical bone defect and intraoperative periprosthetic fracture (Yellow arrows). (c) The results of pathological examination reveal proliferation of aseptic inflammatory granulation tissue (Hematoxylin and Eosin Staining, Magnification 40). (d and e) According to radiographic images, the stable condition of acetabular components along with femur prostheses are observed during follow-up time. Anteroposterior and lateral X-ray show the growth of osteotylus and bone resorption (Yellow arrows).
Case 4
A 65-year-old female patient underwent left total hip arthroplasty 8 years ago because of femoral head necrosis. She was re-admitted to our hospital with one year history of left hip pain and worsening of walking. She had a history of rheumatoid arthritis and accepted treatment of oral methylprednisolone tablet. The preoperative X-ray image demonstrated migration of acetabular components with acetabular screw fracture and radiolucency line around margin of acetabular cup (Figure 4). The obvious radiolucency at the bone-implant interface was observed in around around the femoral prosthesis (Figure 4). On the fourth day after admission, the patient underwent left hip revision. In respective, the additional wires fixation combined with large size femoral prosthesis and acetabular screws and full thread cancellous screws along with porous acetabular cup were used to deal with intraoperative periprosthetic fracture and aseptic loosening of acetabular component (Figure 4). Five weeks follow-up proved that she had stable conditions.
Figure 4.
(a) The preoperative X-ray image demonstrated migration of acetabular components with acetabular screw fracture, and radiolucency line around margin of acetabular cup and obvious radiolucency at the bone-implant interface was observed in around around the femoral prosthesis (Red arrows). (b) The additional wires fixation combined with large size femoral prosthesis, and acetabular screws and full thread cancellous screws along with porous acetabular cup were used to deal with intraoperative periprosthetic fracture and aseptic loosening of acetabular component (Yellow arrows).
Discussion
Aseptic loosening of the acetabular components or femur prostheses remains the most common cause for revision of primary and revision total hip arthroplasty, that is defined as failure of the fixation of acetabular components or femur prostheses in the absence of infection.3,4 Many factors finally cause this consequence including inadequate initial fixation, mechanical loss of fixation over time, and biologic loss of fixation caused by particulate-induced osteolysis around the implant.5 These above listed factors usually play a combinatorial role in driving aseptic loosening during the clinical scenario.4–6 The continued progression of loosening can occur as a result of the mechanical loss of fixation over time and particulate-induced loss of biologic fixation driven by osteolysis participate in a positive feedback loop.3,5 This case report explains the conundrum posed by surgeon grappling with aseptic loosening of the acetabular components associated with femur prostheses. It includes diagnosis, Diagnosis of aseptic loosening relies on history, clinical symptoms as well as radiographic image. Radiographic criteria currently used to identify aseptic loosening include measuring acetabular component migration relative to surrounding host bone and identifying radiolucent lines at the bone-implant interface.7,8 Our four cases showed radiolucency at the bone-implant interface, and formation of a sclerotic line in their radiographic images.
Treatment of septic loosening of the acetabular components or femur prostheses after total hip arthroplasty has historically yielded variable results.9 All components both acetabular cup and femur prostheses need to reconstruction based on individual situation. Larger acetabular cup and longer screws often were used to be replacement of loosening acetabular components.10 In our operative duration, we also found that there was a thinner medial wall of the acetabulum in our three cases compared with the primary total hip arthroplasty group. As a margin of safety for medial wall of the acetabulum, surgeon should avoid to acetabular cup exceed Kohler line in intraoperative fluoroscopy.11
For intraoperative femur prosthetic fracture, options of femoral component revision and reconstruction include open reduction and wires fixation with or without bone grafting.9,10 In a meta-analysis of previously published results, Mont and Maar reported satisfactory results in 43% to 77% of fracture locations depending on fracture location and treatment.10,12 Lee GC et al suggested that among the various treatment modalities used, a long cementless femoral revision with cerclage fixation was associated with the most favorable outcomes.10 In response to intraoperative femur prosthetic fracture, our cases accepted long-stem cementless fixation associated with wires cerclage fixation, or long-stem cemented fixation coupled with bone graft, and wires cerclage fixation. Bone grafting was also introduced as a means to restore acetabular and femoral deficits during revision total hip arthroplasty.13
Conclusions
In fact, there are several limitations to this study including the small sample size and lack of a control group, however, we believe that our case report has the potential to address aseptic loosening of the acetabular components coupled with femur prostheses. Cortical bone loss, intraoperative prosthetic fracture, and strategies of fixation are often present in the management of these very difficult situation. Our results show that long femur stem associated with wires cerclage fixation combined with or without bone graft revision for treatment of aseptic loosening of the acetabular components coupled with femur prostheses is a viable technique for achieving reliable fracture healing and satisfactory clinical results.
Funding Statement
This study was supported by The Science and Technology Planning Project of Huaihua, China, NO.2021R3117 and The Scientific and Technological Innovation Platform of Huaihua, China, No. 2022F2701.
Abbreviations
AL, Aseptic Loosening; THA, Total Hip Arthroplasty.
Data Sharing Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
Informed consent was obtained from the patients for drafting the manuscript and the research follows ethical guidelines.
Consent for Publication
This study was approved by the Ethics Committee of Hunan University of Medicine General Hospital. And, the Hunan University of Medicine General Hospital approved publication of the case details. Written informed consent had been provided by the patients to have the case details and any accompanying images published. All authors declared consent for publication in International Medical Case Reports Journal once our study was accepted.
Disclosure
The authors have declared that no competing interest exists in this work.
References
- 1.Koulischer S, Kapanci B, Bloemers N, Charles T, Jayankura M. Aseptic loosening after total hip arthroplasty in an acromegalic patient: a case report. J Orthop Case Rep. 2017;7(2):94–97. doi: 10.13107/jocr.2250-0685.768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tang K, Deng Z, Wang T, Nie M. Aseptic loosening after total hip arthroplasty secondary to the disappearing coating? Asian J Surg. 2022;45(1):535–536. doi: 10.1016/j.asjsur.2021.09.041 [DOI] [PubMed] [Google Scholar]
- 3.Anil U, Singh V, Schwarzkopf R. Diagnosis and detection of subtle aseptic loosening in total hip arthroplasty. J Arthroplasty. 2022;37(8):1494–1500. doi: 10.1016/j.arth.2022.02.060 [DOI] [PubMed] [Google Scholar]
- 4.Melvin JS, Karthikeyan T, Cope R, Fehring TK. Early failures in total hip arthroplasty -- a changing paradigm. J Arthroplasty. 2014;29(6):1285–1288. doi: 10.1016/j.arth.2013.12.024 [DOI] [PubMed] [Google Scholar]
- 5.Abu-Amer Y, Darwech I, Clohisy JC. Aseptic loosening of total joint replacements: mechanisms underlying osteolysis and potential therapies. Arthritis Res Ther. 2007;9(Suppl 1):S6. doi: 10.1186/ar2170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Noordin S, Masri B. Periprosthetic osteolysis: genetics, mechanisms and potential therapeutic interventions. Can J Surg. 2012;55(6):408–417. doi: 10.1503/cjs.003711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillet R, Teixeira P, Bonarelli C, et al. Comparison of radiographs, tomosynthesis and CT with metal artifact reduction for the detection of Hip prosthetic loosening. Eur Radiol. 2019;29(3):1258–1266. doi: 10.1007/s00330-018-5717-3 [DOI] [PubMed] [Google Scholar]
- 8.Guo S, Tang H, Zhou Y, Huang Y, Shao H, Yang D. Accuracy of digital tomosynthesis with metal artifact reduction for detecting osteointegration in cementless hip arthroplasty. J Arthroplasty. 2018;33(5):1579–1587. doi: 10.1016/j.arth.2017.12.037 [DOI] [PubMed] [Google Scholar]
- 9.Barden B, von Knoch M, Fitzek JG, Löer F. Periprosthetic fractures with extensive bone loss treated with onlay strut allografts. Int Orthop. 2003;27(3):164–167. doi: 10.1007/s00264-002-0423-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Migaud H, Common H, Girard J, Huten D, Putman S. Acetabular reconstruction using porous metallic material in complex revision total Hip arthroplasty: a systematic review. Orthop Traumatol Surg Res. 2019;105(1S):S53–S61. PMID: 30138711. doi: 10.1016/j.otsr.2018.04.030 [DOI] [PubMed] [Google Scholar]
- 11.Qian H, Wang X, Wang P, et al. Total hip arthroplasty in patients with Crowe III/IV developmental dysplasia of the hip: acetabular morphology and reconstruction techniques. Orthopaed Surg. 2023;15(6):1468–1476. doi: 10.1111/os.13733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mont MA, Maar DC. Fractures of the ipsilateral femur after hip arthroplasty. A statistical analysis of outcome based on 487 patients. J Arthroplasty. 1994;9(5):511–519. doi: 10.1016/0883-5403(94)90098-1 [DOI] [PubMed] [Google Scholar]
- 13.Wu ES, Cherian JJ, Kapadia BH, Banerjee S, Jauregui JJ, Mont MA. Outcomes of post-operative periprosthetic femur fracture around total hip arthroplasty: a review. Expert Rev Med Devices. 2015;12(1):61–72. doi: 10.1586/17434440.2015.958076 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study available from the corresponding author on reasonable request.