Abstract
To show the feasibility of performing human telesurgery robotic-assisted radical prostatectomy (RARP) between two countries using low-latency ultra-long-distance connectivity. This study described the outcomes of performing RARP on a man in his 60’s with localized intermediate-risk prostatic adenocarcinoma located in Kuwait City while the surgeon (SA) was approximately 7000 kilometers (Km) away at Toumai robotic surgical system (TRSS) headquarters in Shanghai. Operative and connectivity details were reported. RARP was performed in December 2024. There were no major clinical or technical problems encountered during the procedure. The average round-trip latency (RTL) was 181.4 milliseconds (ms) using fiber optic broadband network with 5G network as back-up. On the Shanghai end two wired broadband networks were employed as back-up to ensure patient safety. There was an experienced fellowship-trained robotic surgeon (AA) in the operating room in Kuwait capable of taking over in case of clinical or connectivity issues. There were no reported complications. The patient was discharged on postoperative day (POD) 2. Final pathology described Gleason score 7(3 + 4), ISUP 2, and negative surgical margins (pT2Nx). The catheter was removed on POD 9, and the patient was continent a week later. His serum prostate specific antigen (PSA) was undetectable seven weeks post-operatively. This study described the feasibility of human RARP telesurgery between two countries using low-latency, long-distance fiber optic broadband network with 5G network as back-up with successful clinical outcomes. There is a need to establish robust legal and regulatory framework to allow wider international expansion of telesurgery.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11701-025-02274-9.
Keywords: Telesurgery, Robotic surgery, Remote surgery, Prostatectomy
Introduction
The disparity in global healthcare resources is a longstanding and prominent issue [1]. Developed nations typically have advanced medical technology, skilled surgeons, and fully equipped medical facilities, whereas developing countries and remote regions often face scarcity of such resources [2]. This imbalance results in many areas unable to provide timely and high-quality medical services to patients, especially when complex surgical procedures requiring expert surgeons are needed [3]. Telesurgery, where an experienced surgeon performs a surgical intervention on a patient while being away from the operating room, emerges as a promising remedy for such circumstances [4]. It holds promise in overcoming geographical barriers, enabling expert and skilled surgeons to reach patients worldwide, democratizing healthcare access, and ensuring that all patients regardless of location can receive high-quality surgical interventions [5].
Telesurgery provides the context for global medical collaboration and telementoring [6, 7]. Through advanced communication technologies, surgeons from various geographical locations can consult or jointly conduct surgeries in real-time. It enables multidisciplinary teams to work together to improve patient outcomes. This collaborative approach can also provide hands-on training and mentorship opportunities [8]. Ultimately, telesurgery redefines the concept of a surgical team, leveraging global expertise to benefit patients wherever they may be. Laparoscopy requires the surgeon to be scrubbed and perform the procedure at the bedside. In the other hand, Laparoscopic telementoring, where experienced surgeons remotely guide less experienced colleagues during live surgeries, is emerging as a powerful tool to enhance surgical skills [7].
Surgical robots provide the perfect tool for which telesurgery can be performed. They offer exceptional precision with minimal invasiveness facilitated by advanced imaging technologies. Marescaux et al. described the feasibility of transatlantic human cholecystectomy telesurgery in 2001 from New York City (USA) to Strasbourg (France) 6200 kilometers (Km) away [9]. The system at the time consisted of three robotic arms on the patient side as well as a 2D video screen on the surgeon side [10]. The interest declined after that due to increased cost and lack of communication technologies required for high-quality low-latency connectivity. However, with the emergence of new robotic systems with remote connection capabilities, and the evolution of telecommunications and cellular networks, telesurgery resurfaced [11].
The efficacy and performance of robotic technologies and network connections for long distances have been described. In recent years, several groups have described telesurgery in animal models between continents, and humans telesurgery within China and other countries with successful outcomes, with only few reports of country to country cross-border human telesurgery [3, 5, 8, 12, 13]. The purpose of our study was to describe the feasibility of performing Asia to Middle East low-latency robotic-assisted radical prostatectomy (RARP) on a patient located in Kuwait City while the surgeon was located in Shanghai, China approximately 7000 km away. We believe this is the first report of human telesurgery between Asia and the Middle East.
Materials and methods
Patient and hospital details
On December 2024, RARP was performed on a man in his 60’s with localized intermediate risk prostatic adenocarcinoma who progressed on active surveillance from Gleason score 6, international society of urological pathology (ISUP) 1 in 2021, to Gleason score 7(3 + 4), ISUP 2 in 2024. His prostate specific antigen (PSA) was 6.8 ng/dL, clinical stage cT1c, prostate size 55 g, and prostate imaging reporting and data system (PI-RADS) score of 3. His past history was significant for hypertension and hyperlipidemia. His body mass index (BMI) was 21 kg/m2. He was not sexually active and had a sexual health inventory for men (SHIM) score < 7.
The patient was located at the hospital in Kuwait City, a tertiary urology referral center with experience in robotic surgery since 2014 with almost 2000 total robotic procedures performed mostly uro-oncology cases using the Da Vinci Si and Xi robotic surgical system. The main surgeon (SA) was located at Toumai robotic surgical system (TRSS) headquarters in Shanghai. On the patient side of the transmission in Kuwait, there was an experienced local robotic team led by a fellowship trained uro-oncologist and robotic surgeon (AA). The team was capable of inserting trocars, docking the robot, and inserting/exchanging instruments. The contingency plan was set for the local team to take over and finish the case if any of the following were to happen: Patient hemodynamic instability, latency > 300 milliseconds (ms) lasting for > 5 minutes, network failure with loss of video/audio feeds, suspected or proven cyber-attack, intraoperative complications, and/or technical problems with the robotic surgical system. In case there was a need to take-over due to any of the aforementioned criteria, the local surgeon has the ability to immediately assume full control of the TRSS away from the remote surgeon using the local console. In the event of technical problems with the TRSS, the local surgeon can exchange to the local Da Vinci Xi robotic system or convert to laparoscopy or open approach if they deemed necessary.
Informed consent and ethical approval
Before conducting the present study, the research project received institutional review board (IRB) approval. Approvals were also obtained from Kuwait Association of Robotic Surgeons, Kuwait drug and food control administration, Drug and Medical Supplies Sector of Biomedical Administration (Kuwait Ministry of Health), and the Kuwaiti Minister of Health. A detailed informed consent was obtained from the patient including risks and possible complications, benefits, and alternatives. The patient fully understood the procedure being undertaken as well as the remote nature of it and the contingency plan. Since medical malpractice laws typically pertain to the patient’s location, there was an agreement between all involved including the patient that in case of adverse events the responsibility falls on the Kuwaiti team including the remote Kuwaiti surgeon (SA) who was the primary urologist of the patient [13]. Both the remote surgeon (SA) and the local back-up surgeon (AA) were from Kuwait and were licensed to practice uro-oncology and robotic-assisted surgery (RAS) in Kuwait. Additionally, they obtained certification from TRSS headquarters in Shanghai on using the robot for clinical telesurgery application.
Robotic platform
The robot used in our telesurgery RARP was the TRSS. It had national medical products administration (NMPA) and Conformite Europeene (CE) approvals [6]. Both the remote surgeon (SA) and the local surgeon (AA) were certified in using it for clinical telesurgery procedures. The TRSS had three components: (1) A closed console where the surgeon operates the system. It had ergonomically designed hand controls and foot pedals, and was equipped with a stereoscopic screen that provides 3D high resolution view. (2) A single boom, four arm patient cart. (3) A vision cart providing high definition camera and integrated lighting. The robot was compatible with fiber optic and 5G wireless broadband network connections. Multiple carts were able to connect to one surgical console, and vice versa, the ability of multiple consoles to connect to one patient cart was also possible. The hospital in Kuwait was equipped with the Da Vinci Si and Xi robotic surgical systems since 2014. The TRSS was very similar to the Da Vinci Xi in terms of the closed console design, hand controls, foot pedals, and single boom four arm cart making an easy and seamless transition for the surgeons from the Da Vinci Xi. [14–17].
RARP procedure
RARP was performed according to our previously described technique with minor modifications [14]. Four robotic arms were utilized. Six ports were configured as follows: Eleven millimeter (mm) supraumbilical robotic camera port, Three robotic ports (eight mm each), one to the right and two to the left of the camera port a handbreadth apart, 12 mm assistant port just above the right anterior superior iliac spine, and a five mm assistant port superior and halfway between the camera port and right sided robotic port.
The patient was positioned in 25–30 degrees supine Trendelenburg. Access was trans-peritoneal with pneumoperitoneum pressure set at 10–12 mm Hg. A 0° lens was used for the majority of the procedure except during anterior bladder neck dissection where it was replaced with a 30° lens. A posterior approach with dissection of the seminal vesicles was performed. This was followed by dropping the bladder and opening of bilateral endopelvic fascia. Opening of the anterior and posterior bladder neck was followed by control of the prostatic pedicles using powered 60 mm vascular stapler. Dorsal venous complex ligation was performed using 0 polyglactin suture. At our institution, when performing RARP on patients with locally advanced disease or patients with pre-existing sexual dysfunction we control the pedicles using vascular staplers. However, we use Weck Hem-O-Lock clips with avoidance of thermal energy for all our remaining RARPs.
The Rocco stitch was performed using 3–0 absorbable barbed suture, 26 mm taper needle, and the urethro-vesical anastomosis was performed using a double armed 3–0 absorbable barbed suture, 17 mm taper needle. No lymph node dissection was performed as his risk of lymph node metastasis was calculated to be < 4%. The specimen was extracted from the supraumbilical camera port after placing it in a surgical bag. A drain was inserted through the 12 mm assistant port and placed on suction.
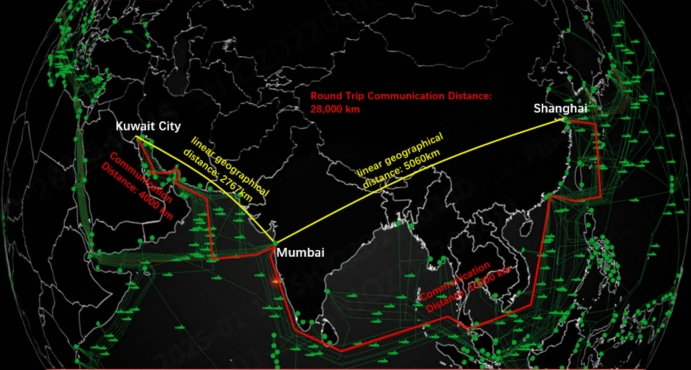
Telesurgery and network details
The execution of the project included collaboration between telecommunication specialists from both countries. We used a dual-network strategy. On the Kuwaiti end, a dedicated internet connection (both wireless 5G and fiber optic broadband network cable) were secured with a local telecom provider with the addition of the on-premise next generation firewall and the high-end load balancer. The operating room was equipped with a combination of fiber optic and Cat7 ethernet cables, outdoor 5G antenna, and 1G network switches. We were prepared to used either, however for our study we used wired broadband network. On the Shanghai end, two wired broadband networks were employed to secure a back-up network [18]. Extensive connectivity testing was performed six weeks before the procedure. Round-trip latency (RTL) within Kuwait was measured at six milliseconds (ms), providing a reliable foundation for remote surgery. The exact linear geographical distance between the hospital in Kuwait and TRSS headquarters in Shanghai was 6935 km (Fig. 1). The average RTL between the two ends was 181.4 ms which was well within the acceptable range not to affect the synchrony between the patient cart and remote surgeon [19, 20].
Fig. 1.
Round trip communication distance from Shanghai to Kuwait showing relay server in Mumbai
A cloud server with a bespoke virtual private network (VPN) service facilitated communication between the two ends, Kuwait and Shanghai. This could have been hosted by amazon, azure or any other cloud service provider. Amazon Web Service (AWS) was the cloud server of choice in the present study and was set up in Mumbai, India (Fig. 2). The communication endpoints of the robotic surgical system were fortified with system firewalls (next-generation firewall from Cisco), allowing only essential connections to go through. In addition, the AWS had its own firewall, which was activated to disable all ports not essential for communication enhancing cybersecurity. Back-up servers for the cloud server were also implemented to ensure continuity if the primary server encountered any faults.
Fig. 2.
Schematic network setup between Kuwait and Shanghai showing ethernet in the hospital connected to the relay server (AWS cloud server) in Mumbai. AWS Amazon Web Services
The internet service used was distinguished by its architecture. It included a single primary cloud server (AWS) and a back-up server, both equipped with public IPs. These servers functioned identically and were dedicated to serving VPN ports and remote debugging ports, with all other ports disabled through the firewall. This setup provided additional enhanced security and streamlined remote access.
In order to prevent telesurgery hijacking during the procedure, communications were encrypted to prevent data leakage and tampering. Multi-factor remote user access was controlled through dynamic user request and authorization protocols from the local surgical team in Kuwait. A control request with the correct access code from the remote surgeon (SA) in Shanghai was required with approval from the local surgeon (AA) in the operating room in Kuwait. The surgical team in Kuwait could also immediately sever remote control at any time if needed to ensure the patient’s safety. In addition, there was continuous traffic monitoring to identify any suspicious activity, and a firewall access control list (ACL) was added to limit the connectivity to only the chosen surgeon consoles.
A separate line of communication between the remote surgeon and the local team in Kuwait was created as an additional interface during the procedure [3]. Bidirectional relay of information with video and audio communication between both ends was seamless. There was clear transmission of the patient’s clinical information to the remote surgeon (Shanghai), and likewise the surgeons demands relayed to the local team (Kuwait) instantaneously. Communication was in the English language as both the remote surgeon (SA) and the local team work together and communicate in the English and Arabic languages (Fig. 3). Having clear, direct, uninterrupted, and understandable communication between both ends was a prerequisite for successful execution of the present study. We believe this should apply to any telesurgery project even if both countries involved speak different languages. There should be peri-operative arrangement to overcome any language barrier and avoid communication errors which may negatively impact the patient’s safety.
Fig. 3.
Operating room setup in Kuwait during surgery and Toumai robotic console in Shanghai controlled by the surgeon
Results
Perioperative data
The procedure started at nine o’clock in the morning Kuwait standard time (equivalent to two o’clock in the afternoon Shanghai standard time). Total operative time was five hours, and console time was approximately three and a half hours. Estimated blood loss was < 100 ml. The patient was ambulating and started on clear liquid diet the evening of the surgery, and his urine was clear. On postoperative day (POD) 2 the patient was started on regular diet, the drain was removed after confirming there was no urine leak by sending fluid from the drain for creatinine level, which was equal to serum creatinine, and he was discharged in stable condition. His catheter was removed on POD 9, required protection pads for one week only, and was continent after that. Final pathology described Gleason 7(3 + 4), ISUP 2, negative surgical margins, and a pathological stage pT2Nx. During his out-patient clinic follow up seven weeks post-operatively, the patient was continent and his serum prostate specefic antigen (PSA) was undetectable.
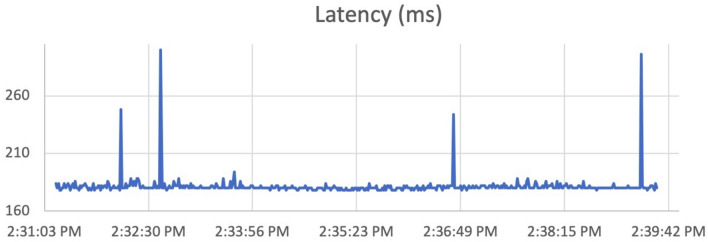
Data transmission and network details
Despite the significant round-trip communication distance of 28,000 km, the system achieved an average RTL of 181.4 ms (minimum 176 ms, maximum 304 ms) with no prolonged latency delays to impact any of the steps in our telesurgery RARP (Fig. 4). There were occasional large delays exceeding 300 ms. However, these delays lasted a second or two and were not noticeable. They were effectively mitigated through instant switching to the redundancy back-up network (Fig. 5) [18]. A supplementary file is included of a second to second log of latency for one hour during the procedure showing the brief duration of the occasional delays that took place during the procedure.
Fig. 4.
Round-trip network latency. ms milliseconds
Fig. 5.
Illustration of the case during dropping the bladder showing RTL of 178 ms. RTL round-trip latency, ms milliseconds
Discussion
The worldwide adoption of robotic surgery has increased exponentially driven by rising demand and technological advancements. The Middle East is emerging as a key player in RAS, fueled by investments in technology and growing expertise [21]. This was paralleled with the emergence of new robotic platforms which offer a more cost-effective and scalable options for healthcare systems [22]. Some of these systems are equipped with telecommunication capabilities allowing remote surgery [6]. This perfectly fits with the expansion of RAS in the Middle East and the Gulf Cooperation Council (GCC) to address disparities in access to advanced surgical care across the region, overcome geographical barriers and resource limitation by connecting surgeons in remote or poorly equipped areas with global experts, and enhance skill and confidence by providing tele-mentoring [23]. Our telesurgery RARP procedure between Kuwait and Shanghai highlights our regions commitment to acquiring state-of-the-art surgical technologies, and its role in advancing global robotic surgical innovations. Such collaboration will contribute in providing readily available robotic surgical care across the Middle East and GCC region.
Since the successful transatlantic “Lindbergh operation” in 2001, high cost and lack of technology were significant limitations for the progression of telesurgery [9]. However, Patel et al. and his group performed multiple trials and remote connections with several centers providing essential information and knowledge about remote surgery in the modern era. They described the feasibility of transpacific telesurgery in live porcine model between Orlando and Shanghai with optimal low-latency connectivity (mean 296 ± 50 ms) and no complications using both 5G and optic fiber networks [13]. Furthermore, they performed a similar animal model study between Sao Paulo and Orlando using fiberoptic network with an average RTL of 120 ms (range between 118–150 ms) [3]. Recently, they reported human RARP telesurgery on a patient with prostate cancer located 1300 km away from the surgeon. Both the patient and surgeon were within China. The surgery was performed using 5G network with successful outcomes [5].
Our human telesurgery experience between Shanghai and Kuwait sets a compelling example of real—time collaboration between teams from different countries, highlighting how remote surgery can overcome geographical imitations (Fig. 6). Our collaborative effort in ensuring a low-latency, secure, and high-quality connection was the result of extensive pre-operative connectivity testing at both ends. Optimal synchrony of audio and video between the remote console in Shanghai and the TRSS in Kuwait were obtained using fiber optic cable with 5G wireless network as back-up. We could not detect prolonged transmission delays or any technological issues that could compromise the optimal quality of the surgery. Our procedure is a significant step forward in telesurgery armamentarium, and a clear continuation of the aforementioned studies into ultra-long distance telesurgery across borders.
Fig. 6.
Remote communication and data exchange
In the present study, a dual-network strategy was used. The decision to alternate between 5G and fiber optic networks was part of a strategy pre-checks to ensure optimal network performance. This strategy aimed to guarantee a seamless, uninterrupted connection throughout the surgery, with swift switching between the two networks if necessary to maintain the required latency threshold [13]. The threshold for switching between the networks was based on latency performance, specifically ensuring that the active link’s latency did not exceed 300 ms which was critical for maintaining real-time communication and system reliability during the procedure. If latency on either network exceeded this threshold, the network team would switch to the other network to restore optimal performance [18]. The rationale behind this approach was to leverage the strengths of both technologies—fiber optic broadband network for stable, high-capacity performance and 5G for its flexibility and rapid deployment—while simultaneously ensuring the lowest possible network latency. Fiber optic network connection was used in the present study and was probably the preferred way to connect both ends in telesurgery. However, it may not be available everywhere, and may be affected by large delays during peak hours, and so, having 5G as back-up would be a safe strategy [24].
In ordinary circumstances, the human reaction time to visual and tactile sensations are 40 ms and one ms, respectively [20, 25]. Based on these values, robotic surgical systems and telecommunication infrastructures should try to mimic these values for safe and smooth remote surgery. Low RTL minimizes the “move and wait” nature of the procedure. The remote surgeon should be able to synchronize command of an action with visualization of the action on the console screen. There is no single value in terms of maximum RTL that is considered acceptable for telesurgery, with a range from 100 ms up to 300 ms being considered safe to perform the procedure [10]. In our experience, with an acceptable average RTL of 181.4 ms, the remote surgeon (SA) adapted well and was not affected by any perceivable delay.
In the present human RARP telesurgery, we demonstrated the feasibility of performing trans-continental Asia to Middle East telesurgery. However, the unique aspect of telesurgery extends beyond only showing its feasibility. Many challenges to its implementation exist especially reimbursement and cost, as regulations and policies pertaining to this are lacking between countries. Implementation of telesurgery may be associated with substantial financial investments, as it requires state-of-the-art robotic systems, high-speed internet infrastructure, and secure communication networks. These costs can be prohibitive for many healthcare systems, particularly in low-resource settings, and this plays a crucial role in determining its financial viability [10, 21]. Additionally, the specialized nature of telesurgery necessitates comprehensive training for surgeons and support staff to effectively utilize the technology. Establishing such training programs requires time and resources, and ongoing education is essential to keep up with technological advancements and ensure proficiency [21]. This combination of high initial costs and the need for specialized expertise may pose a barrier to widespread adoption. Nevertheless, some healthcare systems are capable of investing in remote surgery with the ultimate goal of reducing the overall financial burden. In the Middle East and the GCC for example, telesurgery can help centralize advanced surgical care to reach areas lacking both the expertise and technology and ultimately saving the travel expenses on patients and physicians. Some institutions have robotic surgical systems and are capable of performing basic robotic procedures, but when faced with a complex surgical dilemma requiring remote expertise involvement, the solution used to be boarding the patient to the expert, or inviting the expert to perform the procedure locally. Either way can be cumbersome on the expert, the patient, and healthcare system. Furthermore, the expert may not always be available to travel. By connecting both robotic systems through telesurgery, the patient would get the required surgical care locally next to his family instead of travelling or paying for the expenses of the expert to travel from another city or country [3]. The expert would also avoid losing time at work from travelling. This ultimately saves time, money, and effort. The patient in the present study did not endure any costs and his procedure was covered by Kuwait Ministry of Health as part of free healthcare coverage plan for Kuwaiti citizens. The TRSS used in the present study belonged to the hospital in Kuwait, and it was used by other surgeons on other patients. Connectivity and network coverage plans were part of the hospital’s infrastructure.
Telesurgery has promising potential in transcending geographical barriers and enhancing patient care globally. It can become an essential tool for global humanitarian missions helping to alleviate the burden of surgical diseases in remote and low resource areas [26]. Telementoring and teleproctoring in emergency scenarios especially in areas where access to care is restricted by natural disasters, conflict zones, and resource limited setting is another potential benefit [7]. Additionally, telesurgery holds significant promise in medical education. Traditionally, training has been limited by geographical proximity and expert availability [8]. Telesurgery allows for real-time collaboration and mentorship between surgeons globally. Experts can supervise, guide, and assist in complex procedures remotely without the need for physical relocation allowing for knowledge exchange and skill enhancement, fostering a global community of surgical practices while ultimately saving resources. However, several steps need to be undertaken before applying human telesurgery in a larger cohort. Establishing clear legal frameworks and guidelines to address potential malpractice claims, data privacy concerns, and cross-border practice standards is of paramount importance. This should come from a regulatory organization with international panel members of experts in healthcare, technology, law, and ethics to establish the most effective practice guidelines for telesurgery. This may entail governmental agreements and medical societies involvement to guarantee safe and ethical application of telesurgery. Ensuring rigorous patient safety protocols remains paramount to gaining acceptance and confidence in telesurgical practices [3]. Furthermore, connectivity studies and testing need to be performed across borders with the availability of robust telecommunication infrastructure and advanced surgical technology. A dedicated support team of technical experts specialized in telesurgical communications should be present around the clock for assistance [27]. This team should have remote access to the robotic surgical system software to diagnose and troubleshoot any malfunctions instantly using all communication means necessary (audio, video, and messaging). Emergency protocols should be put in place for situations that endanger patient’s safety including switching to manual operation or aborting the procedure. Challenges related to latency, network stability, and data security must continue to be addressed. Creating a framework to ensure patient autonomy, transparent communication, and the preservation of trust within the surgeon–patient relationship are imperative before embarking on globalization of telesurgery. In that regard, Moschovas and his group published the ten commandments for a safe and ethical exploration of telesurgery [3].
The present study had several limitations. First, the study design with only one patient limits generalizability of the results. Second, the limited follow-up prevents assessment of long-term outcomes and complications. Third, the present study featured a “straight forward” and “standard” RARP procedure done for a patient with no significant surgical history or co-morbidities. The prostate size was 55 g and the patient was diagnosed with localized favorable intermediate-risk prostatic adenocarcinoma. This could have introduced selection bias and limited the comprehensiveness of the findings to patients with more advanced disease. Finally, the outcomes may have been influenced by the experience of the Kuwaiti surgical team and their hospital which is a tertiary urology referral center with almost 2000 uro-oncological RAS procedures performed since 2014, leading to variability in outcomes between studies and hospitals. Despite the aforementioned limitations, the present study achieved an important milestone in telesurgery. We believe the present study demonstrated that cross-border connections are not only feasible but also offer immense potential for future application in several surgical fields. By continuing to explore and refine this technology we have the opportunity to create a more equitable healthcare system. Lessons learned from real-world case studies, including the present study, have provided insights into potential challenges in country to country telesurgery and how to overcome them.
Conclusion
The present study demonstrated the feasibility of human RARP telesurgery executed through carefully planned collaboration between two countries using a robotic surgical system compatible with fiber optic and 5G wireless network connections without intraoperative complications. Highly reliable, low-latency connectivity, and dual network redundancy were essential for the success of our procedure. Nevertheless, telesurgery is still at a young age and one should be cognizant of the complexity and potential challenges of global expansion and application in a larger patient cohort. There are no specific international laws for telesurgery spanning countries, or a unified legal framework for cross-border practices. It is mandatory to establish legal and regulatory guidelines and frameworks set by consensus meetings led by international medical societies to facilitate telesurgery expansion and allow wider international collaboration. Furthermore, informed consent laws might not fully cover telesurgery’s unique challenges, requiring additional disclosures about technology, technical risks, and surgeon’s absence. Integrating these aspects into existing consents requires international collaboration to establish internationally applicable guidelines. Additional efforts are necessary to further guarantee the safety of large-scale telesurgery in the future. Further improvements in telecommunications are required before larger trials can be carried out with longer follow up.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgments
The completion of this project would not have been possible without the dedication and hard work of operating room staff at Sabah Al-Ahmad Urology Center.
Author contributions
[SA] contributed to the study conception and design. Material preparation and data collection were performed by [SA], [AA], [AH], [AS], [SB], and [BB]. Surgeon using the console in Shanghai was [SA]. Surgical team in Kuwait were [AA], [AH], [AS]. The first draft of the manuscript was written by [SA] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
None.
Data availability
No datasets were generated or analysed during the current study.
Declarations
Conflict of interest
Saad Aldousari, Ahmad Almarzouq, Abdulkareem Hassan, Ahmed Shahin, Saleh Bubishate, Basmah Bahbahani: have no conflicts of interest.
Ethical approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000.
Informed consent
Informed consent was obtained from the patient included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Moschovas MC, Saikali S, Rogers T, Gamal A, Perera R, Reddy S, Patel V (2024) Exploring the ethical implications in the telesurgery ERA. Int Braz J Urol 50:375–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Meara JG, Leather AJ, Hagander L, Alkire BC, Alonso N, Ameh EA, Bickler SW, Conteh L, Dare AJ, Davies J et al (2016) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Int J Obstet Anesth 25:75–78 [DOI] [PubMed] [Google Scholar]
- 3.Moschovas MC, Saikali S, Dohler M, Patel E, Rogers T, Gamal A, Marquinez J, Patel V (2025) Advancing telesurgery connectivity between North and South America: the first remote surgery conducted between Orlando and Sao Paulo in animal models. Int Braz J Urol. 10.1590/s1677-5538.ibju.2024.0601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Patel V, Marescaux J, Covas Moschovas M (2024) The humanitarian impact of telesurgery and remote surgery in global medicine. Eur Urol 86:88–89 [DOI] [PubMed] [Google Scholar]
- 5.Moschovas MC, Rogers T, Xu W, Perera R, Zhang X, Patel V (2024) First impressions of Telesurgery robotic-assisted radical prostatectomy using the Edge medical robotic platform. Int Braz J Urol 50:754–763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rocco B, Moschovas MC, Saikali S, Gaia G, Patel V, Sighinolfi MC (2024) Insights from telesurgery expert conference on recent clinical experience and current status of remote surgery. J Robot Surg 18:240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Challacombe B, Kavoussi L, Patriciu A, Stoianovici D, Dasgupta P (2006) Technology insight: telementoring and telesurgery in urology. Nat Clin Pract Urol 3:611–617 [DOI] [PubMed] [Google Scholar]
- 8.Rogers T, Moschovas MC, Saikali S, Reddy S, Gamal A, Li X, Cui L, Patel V (2024) Triple-console robotic telesurgery: first impressions and future impact. J Robot Surg 18:381 [DOI] [PubMed] [Google Scholar]
- 9.Marescaux J, Leroy J, Rubino F, Smith M, Vix M, Simone M, Mutter D (2002) Transcontinental robot-assisted remote telesurgery: feasibility and potential applications. Ann Surg 235:487–492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel V, Saikali S, Moschovas MC, Patel E, Satava R, Dasgupta P, Dohler M, Collins JW, Albala D, Marescaux J (2024) Technical and ethical considerations in telesurgery. J Robot Surg 18:40 [DOI] [PubMed] [Google Scholar]
- 11.Dohler M, Saikali S, Gamal A, Moschovas MC, Patel V (2024) The crucial role of 5G, 6G, and fiber in robotic telesurgery. J Robot Surg 19:4 [DOI] [PubMed] [Google Scholar]
- 12.Zheng J, Wang Y, Zhang J, Guo W, Yang X, Luo L, Jiao W, Hu X, Yu Z, Wang C et al (2020) 5G ultra-remote robot-assisted laparoscopic surgery in China. Surg Endosc 34:5172–5180 [DOI] [PubMed] [Google Scholar]
- 13.Patel V, Dohler M, Marescaux J, Saikali S, Gamal A, Reddy S, Rogers T, Patel E, Oliva R, Satava R et al (2024) Expanding surgical frontiers across the pacific ocean: insights from the first telesurgery procedures connecting Orlando with shanghai in animal models. Eur Urol Open Sci 70:70–78 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aldousari S, Yaiesh S, Alkandari O, Hussein S (2021) Pathological features of prostate cancer in men treated with robot-assisted radical prostatectomy in the Middle East. J Robot Surg 15:125–133 [DOI] [PubMed] [Google Scholar]
- 15.Aldousari SA, Buabbas AJ, Yaiesh SM, Alyousef RJ, Alenezi AN (2021) Multiple perceptions of robotic-assisted surgery among surgeons and patients: a cross-sectional study. J Robot Surg 15:529–538 [DOI] [PubMed] [Google Scholar]
- 16.Azhar RA, Aldousari S, Alghamdi MM, Alotaibi MF, Alkhateeb SS, Nassir AM, Alshaalan A, Yaiesh S, Rabah D (2021) Robot-assisted radical prostatectomy in low-volume regions: should it be abandoned or adopted? A multi-institutional outcome study. J Endourol 35:1013–1019 [DOI] [PubMed] [Google Scholar]
- 17.Buabbas AJ, Aldousari S, Shehab AA (2020) An exploratory study of public’ awareness about robotics-assisted surgery in Kuwait. BMC Med Inform Decis Mak 20:140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Morohashi H, Hakamada K, Kanno T, Tadano K, Kawashima K, Takahashi Y, Ebihara Y, Oki E, Hirano S, Mori M (2023) Construction of redundant communications to enhance safety against communication interruptions during robotic remote surgery. Sci Rep 13:10831 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pandav K, Te AG, Tomer N, Nair SS, Tewari AK (2022) Leveraging 5G technology for robotic surgery and cancer care. Cancer Rep (Hoboken) 5:e1595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nankaku A, Tokunaga M, Yonezawa H, Kanno T, Kawashima K, Hakamada K, Hirano S, Oki E, Mori M, Kinugasa Y (2022) Maximum acceptable communication delay for the realization of telesurgery. PLoS ONE 17:e0274328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mehta A, Cheng Ng J, Andrew Awuah W, Huang H, Kalmanovich J, Agrawal A, Abdul-Rahman T, Hasan MM, Sikora V, Isik A (2022) Embracing robotic surgery in low- and middle-income countries: potential benefits, challenges, and scope in the future. Ann Med Surg (Lond) 84:104803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gamal A, Moschovas MC, Jaber AR, Saikali S, Perera R, Headley C, Patel E, Rogers T, Roche MW, Leveillee RJ et al (2024) Clinical applications of robotic surgery platforms: a comprehensive review. J Robot Surg 18:29 [DOI] [PubMed] [Google Scholar]
- 23.Saikali S, Covas Moschovas M, Gamal A, Reddy S, Rogers T, Patel V (2024) Telesurgery: humanitarian and surgical benefits while navigating technologic and administrative challenges. J Robot Surg 18:393 [DOI] [PubMed] [Google Scholar]
- 24.Barba P, Stramiello J, Funk EK, Richter F, Yip MC, Orosco RK (2022) Remote telesurgery in humans: a systematic review. Surg Endosc 36:2771–2777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li J, Yang X, Chu G, Feng W, Ding X, Yin X, Zhang L, Lv W, Ma L, Sun L et al (2023) Application of improved robot-assisted laparoscopic telesurgery with 5G technology in urology. Eur Urol 83:41–44 [DOI] [PubMed] [Google Scholar]
- 26.Patel V, Moschovas MC, Marescaux J, Satava R, Dasgupta P, Dohler M (2024) Telesurgery collaborative community working group: insights about the current telesurgery scenario. J Robot Surg 18:232 [DOI] [PubMed] [Google Scholar]
- 27.Collins JW, Ghazi A, Stoyanov D, Hung A, Coleman M, Cecil T, Ericsson A, Anvari M, Wang Y, Beaulieu Y et al (2020) Utilising an accelerated delphi process to develop guidance and protocols for telepresence applications in remote robotic surgery training. Eur Urol Open Sci 22:23–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No datasets were generated or analysed during the current study.