Abstract
Background
Little information is available regarding whether active physical activity lowers mortality risk in individuals with bronchiectasis.
Methods
We used the Korean National Health Insurance Service database from 2010 to 2016 to evaluate the association between changes in physical activity and mortality risk in individuals with bronchiectasis. Of 552,510 individuals with newly diagnosed bronchiectasis, we enrolled 165,842 individuals who had two consecutive health examinations before and after bronchiectasis diagnosis, within two years, as the study aimed to measure changes in exercise habits between the two time points. Active physical activity was defined as engaging in moderate- or vigorous-intensity physical activity at least once a week, either before or after bronchiectasis diagnosis. The outcome measure was all-cause mortality.
Results
During a mean follow-up of 6.2 ± 2.1 years, 10,535 (6.4%) individuals with bronchiectasis died. Individuals with bronchiectasis who were physically active exhibited a lower mortality rate than those who were physically inactive. Mortality reduction was particularly evident in the exercise maintainers group (aHR [adjusted hazard ratio] = 0.69, 95% confidence interval [CI] = 0.64–0.74) and individuals with physical activity ≥1,000 metabolic equivalent of task-min per week (aHR = 0.73, 95% CI = 0.70–0.77) compared to those who were physically inactive.
Conclusion
Engaging in active physical activity is associated with a decreased risk of mortality in individuals with bronchiectasis.
Keywords: bronchiectasis, mortality, exercise, movement, running, sedentary behavior
Introduction
Bronchiectasis is a chronic respiratory disease characterized by abnormal radiological dilation of the bronchi, with respiratory symptoms including chronic cough, purulent sputum, and recurrent chest infections (1). Bronchiectasis-related disease burden is substantial and contributes to increased mortality rates (2, 3). Considering that increased mortality is largely driven by comorbidities such as cardiovascular diseases (3, 4), individuals with bronchiectasis may achieve survival gain through lifestyle modifications, such as exercise intervention. However, this association has not been studied.
Individuals with chronic respiratory diseases, including bronchiectasis, tend to have sedentary lifestyles linked to poorer long-term outcomes (5–7). Appropriate physical activity is recommended for this population, and exercise interventions have shown improvements in exercise capacity, dyspnea, and quality of life (8). Furthermore, enhanced physical activity may prevent the development of cardiovascular disease in individuals with bronchiectasis (4). Hence, our study aimed to assess whether physical activity could reduce the mortality risk in individuals with bronchiectasis.
Methods
Data source and study population
We used data obtained from the Korean National Health Insurance Service (NHIS) database, which encompasses a large-scale nationwide population-based cohort study (9). The NHIS offers detailed reports that include data from health screening exams, sociodemographic data, self-reported survey responses, clinical laboratory results, information on inpatient and outpatient services, prescription details, and diagnoses classified under the International Classification of Diseases, 10th Revision (ICD-10) codes.
During study participant enrollment, the Korean government mandated general health examinations for health insurance subscribers aged ≥40 years, local subscribers aged ≥20 years, job subscribers of all ages, and Medicaid beneficiaries aged 19–64 years, conducted annually or every 2 years. The health examination included various screening items, such as anthropometric measurements (e.g., body mass index [BMI], waist circumference, and blood pressure), laboratory test results, and questionnaires covering smoking habits, alcohol intake, and physical activity. More detailed information on this database is presented in previous studies (4, 10, 11).
Of 552,510 individuals with newly diagnosed bronchiectasis between January 1, 2010, and December 31, 2016, we enrolled 165,842 individuals, meeting the following criteria: (1) aged over 20 years, (2) ICD-10 codes for bronchiectasis (J47, except E84 [cystic fibrosis]), (3) had two consecutive health examinations before and after bronchiectasis diagnosis, within 2 years, as the study aimed to measure changes in exercise habits between the two time points, (4) no history of prior myocardial infarction (I21–I22) (12, 13) or stroke (I63–I64) (14), as cardiovascular diseases are significant causes of mortality in individuals with chronic respiratory diseases and also influence physical activity levels, and (5) no missing data.
Exposure: physical activity
The intensity and frequency of physical activity were evaluated to assess exercise habits through the Korean version of the International Physical Activity Questionnaire (IPAQ) (15), a self-reported survey administered during two health screening examinations conducted before and after the bronchiectasis diagnosis. The IPAQ has been broadly used in several high-quality studies (16, 17). The questionnaire contains the amount of time participants typically spend engaging in various physical activities during a typical week using the 7-day recall method. The survey included three questions addressing the frequency and intensity of the following activities: (1) vigorous physical activity lasting at least 20 min, (2) moderate physical activity lasting at least 30 min, and (3) light physical activity lasting at least 30 min. Vigorous-intensity physical activity is an exercise causing significant shortness of breath, such as running or cycling at high speed. Moderate-intensity physical activity is an exercise inducing mild shortness of breath, including brisk walking or cycling at a regular pace. Light physical activity is walking at a slow or leisurely pace.
We calculated the total metabolic equivalent of task (MET)-minutes per week by summing the standardized intensity levels. Using the Ainsworth et al. compendium, an average MET score was derived for each type of activity: 3.3 METs for walking, 4.0 METs for moderate-intensity activities, and 7.0 METs for vigorous-intensity activities (18). This approach demonstrated validity and reliability in the Korean population when compared to directly measured METs using an omnidirectional accelerometer (19).
Individuals were categorized as either active or inactive, based on their reported physical activity levels. Individuals who reported moderate- or vigorous-intensity physical activity at least once a week, either before or after diagnosis, were categorized as having active activity; individuals who did not meet this criterion were categorized as having inactive activity (20). Active physical activity was further divided into <500, 500–999, and ≥ 1,000 MET-min/week based on the recommendations for physical activity, which has also been widely used for the Korean population (7, 21–23).
Among individuals who engage in active physical activity, changes in exercise habits were assessed and classified into three groups: new exercisers (having inactive physical activity before diagnosis but engaging active physical activity after diagnosis), exercise discontinued (engaging active physical activity before diagnosis changed to having inactive physical activity after diagnosis), and exercise maintainers (engaging active physical activity before and after diagnosis).
Outcome
The outcome was all-cause mortality, excluding accidental deaths, and data were obtained from the National Death Registry (3, 24–30). Individuals were followed up until either the date of death or the last follow-up date (December 31, 2020), depending on whichever occurred earlier.
Covariates
Demographics, anthropometric measurements, personal habits, and socioeconomic status were evaluated using previous health examination data close to the time of bronchiectasis diagnosis, and comorbidities were identified within 1 year preceding the diagnosis. Low income was classified as being in the lowest 20% of income distribution within the Korean population or receiving medical aid (31). Smoking status and alcohol use were determined through a self-reported questionnaire (32). Heavy alcohol consumption was defined as an intake of ≥30 g of alcohol per day (33). Comorbidities were identified using ICD-10 codes, supplemented by specific measurements or medication usage when applicable (34–44).
Statistical analyses
Data are expressed as means with standard deviations or numbers (percentages), as appropriate. Differences in baseline characteristics were assessed using the t-test or χ2 test, as appropriate. The mortality rate was calculated by dividing the number of deaths by the total follow-up duration (per 1,000 person-years). Cox proportional hazards regression analyses were used to evaluate mortality risk based on the levels of physical activity. The multivariate model was adjusted for age, sex, low income, smoking status, alcohol consumption, BMI, and comorbidities (hypertension, diabetes mellitus, dyslipidemia, asthma or chronic obstructive pulmonary disease [COPD], and cancer). Proportional hazard assumptions were evaluated using graphical methods. Kaplan–Meier curves depicting the probability of mortality were plotted based on changes in exercise habits. All analyses were performed using SAS 9.3 (SAS Institute, Cary, NC, United States). All tests were two-tailed, and p-values <0.05 were considered statistically significant.
Results
Baseline characteristics
Baseline characteristics of the study population are shown in Table 1. Of the 165,842 individuals, the majority were aged 40–64 years and 51.6% were women. Individuals with active physical activity were more likely to be old (36.9% vs. 34.7% for ≥65 years, p < 0.001), be male (53.5% vs. 45.9%, p < 0.001), have a higher BMI (mean, 23.7 vs. 23.5 kg/m2, p < 0.001), and a higher possibility of belonging to the low-income group (18.3% vs. 15.6%, p < 0.001) than those who are physically inactive. Physically active individuals were less likely to be current or past smokers compared to those who are physically inactive (12.7% vs. 15.6%, p < 0.001).
Table 1.
Baseline characteristics of the study population.
| Variables | Total (N = 165,842) | Inactive physical activity (n = 110,499) | Active physical activity (n = 55,343) | p-value |
|---|---|---|---|---|
| Age, years | ||||
| <40 years, n (%) | 9,621 (5.8) | 7,215 (6.4) | 2,406 (4.4) | < 0.001 |
| 40–64 years, n (%) | 97,408 (58.7) | 64,907 (58.7) | 32,501 (58.7) | |
| ≥65 years, n (%) | 58,813 (35.5) | 38,377 (34.7) | 20,436 (36.9) | |
| Sex | < 0.001 | |||
| Male, n (%) | 80,336 (48.4) | 50,714 (45.9) | 29,622 (53.5) | |
| Female, n (%) | 85,506 (51.6) | 59,785 (54.1) | 25,721 (46.5) | |
| Body mass index, kg/m2 | 23.5 ± 3.3 | 23.5 ± 3.3 | 23.7 ± 3.1 | < 0.001 |
| Low income, n (%) | 31,365 (18.9) | 21,210 (19.2) | 10,155 (18.3) | < 0.001 |
| Smoking status | ||||
| Current or past smoker, n (%) | 24,294 (14.7) | 17,239 (15.6) | 7,055 (12.7) | < 0.001 |
| Alcohol consumption | ||||
| Heavy drinker, n (%) | 8,402 (5.1) | 5,579 (5.1) | 2,823 (5.1) | 0.657 |
| Comorbidities | ||||
| Hypertension, n (%) | 64,250 (38.7) | 42,287 (38.3) | 21,963 (39.7) | < 0.001 |
| Dyslipidemia, n (%) | 50,422 (30.4) | 32,984 (29.9) | 17,438 (31.5) | < 0.001 |
| Diabetes mellitus, n (%) | 22,762 (13.7) | 14,623 (13.2) | 8,139 (14.7) | < 0.001 |
| Chronic kidney disease, n (%) | 10,948 (6.6) | 7,333 (6.6) | 3,615 (6.5) | 0.426 |
| Asthma or COPD, n (%) | 7,885 (4.8) | 4,871 (4.4) | 3,014 (5.4) | < 0.001 |
| Cancer, n (%) | 57,243 (34.5) | 38,630 (35.0) | 18,613 (33.6) | < 0.001 |
| Amounts of exercise | ||||
| ≥ 500 MET-min/week, n (%) | 80,102 (48.3) | 35,871 (32.5) | 44,231 (79.9) | < 0.001 |
COPD, chronic obstructive pulmonary disease; MET, metabolic equivalent of task.
In terms of comorbidities, physically active individuals showed a higher proportion of hypertension (39.7% vs. 38.3%, p < 0.001), dyslipidemia (31.5% vs. 29.9%, p < 0.001), diabetes mellitus (14.7% vs. 13.2%, p < 0.001), and asthma or COPD (5.4% vs. 4.4%, p < 0.001) than those who were inactive. Physically active individuals engaged in significantly more exercise compared to those who were inactive (79.9% vs. 32.5% for ≥ 500 MET-min/week, p < 0.001). However, no significant differences were observed in alcohol consumption and chronic kidney disease between the two groups (p > 0.05 for both).
Impact of exercise on mortality
During a mean follow-up of 6.2 ± 2.1 years, 10,535 (6.4%) individuals with bronchiectasis died. As shown in Figure 1, the individuals with bronchiectasis who engaged in active physical activity exhibited lower mortality rates than those who engaged in inactive physical activity. The risk reduction of mortality was highest in the exercise maintainers group (adjusted hazard ratio [aHR] = 0.69, 95% CI = 0.64–0.74) and lowest in the exercise discontinued group (aHR = 0.84, 95% CI = 0.79–0.89).
Figure 1.
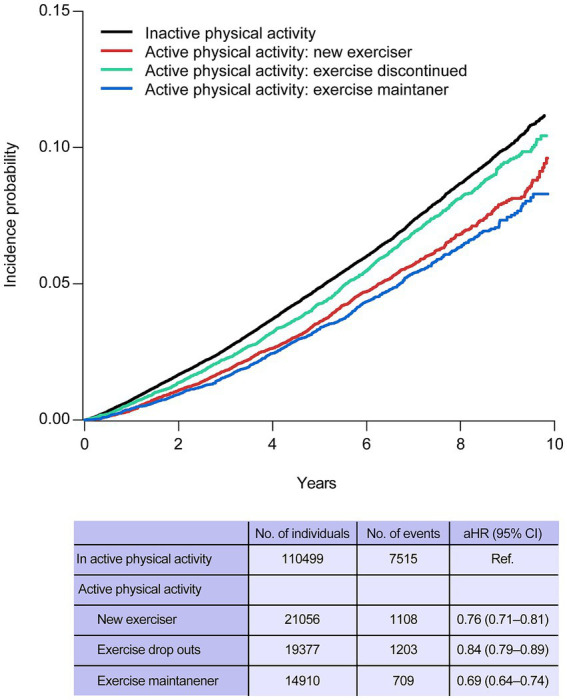
Kaplan–Meier curves of incidence probability of mortality according to the physical activity status. aHR, adjusted hazard ratio; CI, confidence interval.
Regarding the amount of exercise and risk of mortality, the greatest reduction in mortality was observed in individuals who performed exercise ≥1,000 MET-min/week (aHR = 0.73, 95% confidence interval [CI] = 0.70–0.77), followed by 500–999 MET-min/week (aHR = 0.74, 95% CI = 0.68–0.81) and < 500 MET-min/week (aHR = 0.89, 95% CI = 0.83–0.96) (Table 2).
Table 2.
Effect of physical activity on the risk of mortality.
| No. of individuals | Total | ||||
|---|---|---|---|---|---|
| No. of events | IR (/1,000 PY) | aHR (95% CI) | |||
| Overall | Inactive physical activity | 110,499 | 7,515 | 10.8 | 1 (Reference) |
| Active physical activity | |||||
| <500 MET-min/week | 11,112 | 750 | 10.7 | 0.89 (0.83–0.96) | |
| 500–999 MET-min/week | 11,407 | 589 | 8.1 | 0.74 (0.68–0.81) | |
| ≥1,000 MET-min/week | 32,824 | 1,681 | 8.2 | 0.73 (0.70–0.77) | |
| p-value | < 0.001 | ||||
| New exerciser | Inactive physical activity | 110,499 | 7,515 | 10.8 | 1 (Reference) |
| Active physical activity | |||||
| <500 MET-min/week | 457 | 13 | 4.4 | 0.50 (0.29–0.85) | |
| 500–999 MET-min/week | 2,384 | 99 | 6.4 | 0.71 (0.58–0.86) | |
| ≥1,000 MET-min/week | 18,215 | 996 | 8.7 | 0.77 (0.72–0.82) | |
| p-value | < 0.001 | ||||
| Exercise discontinued | Inactive physical activity | 110,499 | 7,515 | 10.8 | 1 (Reference) |
| Active physical activity | |||||
| <500 MET-min/week | 10,377 | 723 | 11.0 | 0.91 (0.84–0.98) | |
| 500–999 MET-min/week | 7,520 | 418 | 8.9 | 0.75 (0.68–0.83) | |
| ≥1,000 MET-min/week | 1,480 | 62 | 6.9 | 0.77 (0.60–0.99) | |
| p-value | < 0.001 | ||||
| Exercise maintainers | Inactive physical activity | 110,499 | 7,515 | 10.8 | 1 (Reference) |
| Active physical activity | |||||
| <500 MET-min/week | 278 | 14 | 7.6 | 0.86 (0.51–1.45) | |
| 500–999 MET-min/week | 1,503 | 72 | 7.5 | 0.74 (0.58–0.93) | |
| ≥1,000 MET-min/week | 13,129 | 623 | 7.7 | 0.68 (0.63–0.74) | |
| p-value | < 0.001 | ||||
IR, incidence rate; aHR, adjusted hazard; CI, confidence interval; MET, metabolic equivalent of task.
Discussion
The significant findings of this study are as follows. First, approximately two-third of individuals with bronchiectasis did not engage in active physical activity. Second, mortality significantly decreased in those who engaged in active physical activity. Third, the reduction in mortality was highest among individuals in the exercise maintainers group and the lowest among exercise discontinued. Fourth, although the amount of active physical activity correlates with the risk reduction of mortality, even a small amount of physical activity can reduce the risk of mortality in individuals with bronchiectasis.
The detrimental effects of physical inactivity are well-documented; however, a significant proportion of individuals continue to fall short of meeting recommended physical activity levels. Recent data indicate that nearly one-third of adults globally, approximately 1.8 billion people, remain physically inactive (45). In patients with bronchiectasis, the prevalence of physical inactivity varies globally, ranging from 40.9 to 73.7% (Table 3) (46–49). Notably, our findings indicate that the proportion of physically inactive individuals with bronchiectasis in Korea is considerably high, far exceeding half of those with bronchiectasis. Recently, physical inactivity has been a significant concern in the Asia-Pacific region, driven by factors such as aging populations, climate change, insufficient infrastructure, and the lingering impacts of the coronavirus 2019 pandemic (50). Considering these circumstances, it is time to focus on the significance of physical inactivity in patients with bronchiectasis, particularly in the Asia-Pacific region.
Table 3.
Summary of studies assessing physical inactivity prevalence in bronchiectasis.
| Study | Country | Data source | Measurement of physical inactivity | Definition of physical inactivity | Prevalence of physical inactivity |
|---|---|---|---|---|---|
| Alcaraz-Serrano et al. (46) | Spain | A tertiary care hospital | A tri-axial accelerometer (SenseWear Armband; BodyMedia Inc., Pittsburgh, PA, United States) | < 6,290 steps per day | 26/53 (49.1%) |
| Bradley et al. (47) | UK | Respiratory clinics at the three selected hospital sites | ActiGraph GT3X+ accelerometer | < 5,000 steps per day | 23/55 (41.8%) |
| de Camargo et al. (48) | Brazil | A tertiary university hospital | Pedometer (Yamax Power Walker, model PW-610; Yamax Corp, Tokyo, Japan) | < 7,500 steps per day | 61/149 (40.9%) |
| Pehlivan et al. (49) | Turkey | Pulmonology outpatient clinics | International Physical Activity Questionnaire (IPAQ) Short Form | Did not meet any of the following criteria: (a) engaging in vigorous activity ≥20 min/day on 3 or more days/week, (b) engaging in moderate-intensity activity or walking for ≥30 min/day on 5 or more days per week, OR (c) achieving a minimum of 600 MET-minutes per week through a combination of walking, moderate-intensity, or vigorous-intensity activities on 5 or more days per week. | 14/19 (73.7%) |
IPAQ, International Physical Activity Questionnaire; MET, Metabolic equivalent of task.
Our findings indicate that active physical activity can effectively decrease mortality risk in individuals with bronchiectasis. Two interesting findings were observed when we assessed physical activity in terms of maintenance and amount. First, although the maintenance of active physical activity showed the highest reduction in mortality, mortality reduction was observed even in individuals in the exercise discontinued group. Second, although there is a correlation between the amount of physical activity and mortality reduction, even individuals who engaged in physical activity below the recommended threshold (approximately more than 600 MET-min/week) showed a significant decrease in mortality (51). Therefore, our study indicates that it is important to encourage individuals with bronchiectasis to maintain physical activity regardless of the amount of exercise because this can yield substantial long-term survival benefits.
This study has several limitations that warrant consideration. First, certain factors not assessed in this study may influence the outcomes. Key variables impacting mortality, such as disease severity—including exacerbation history, lung function, specific treatments, and bacterial colonization—could not be analyzed due to the lack of available data (52–54). Future research should incorporate these variables to understand better the relationship between physical activity and mortality in individuals with bronchiectasis. Second, although we showed that the amount of physical activity is associated with reduced mortality in patients with bronchiectasis, this measure was indirectly assessed. Furthermore, since we used self-reported data, there might be a recall bias. Thus, future studies that directly measure the intensity and duration of exercise, such as using accelerometers, are needed to provide a more comprehensive understanding of the impact of physical activity on the mortality in individuals with bronchiectasis. Third, as this study was conducted in a single Asian country, the generalizability of the results to populations in other regions may be limited.
In conclusion, actively engaging in physical activity is associated with a decreased mortality risk in individuals with bronchiectasis. Therefore, more active physical activity is recommended for this population.
Acknowledgments
This study used data obtained from the National Health Insurance System database, and the results do not necessarily represent the opinions of the National Health Insurance Corporation.
Funding Statement
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Basic Science Research Program through the Korean Ministry of Education (No. 2021R1I1A3052416).
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data that support the findings of this study are available from Korea NHIS but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Requests to access these datasets should be directed to https://nhiss.nhis.or.kr/bd/ab/bdaba001cv.do.
Ethics statement
The study protocol was approved by the Institutional Review Board of Hallym University Kangnam Sacred Heart Hospital (application no. 2022-01-025). The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because The NHIS database was developed after the anonymization of data.
Author contributions
SHK: Visualization, Writing – original draft. HC: Writing – original draft. KH: Data curation, Formal analysis, Writing – review & editing. J-HJ: Data curation, Formal analysis, Writing – review & editing. BY: Writing – review & editing. HL: Conceptualization, Supervision, Validation, Writing – review & editing.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
- 1.Choi H, McShane PJ, Aliberti S, Chalmers JD. Bronchiectasis management in adults: state of the art and future directions. Eur Respir J. (2024) 63:2400518. doi: 10.1183/13993003.00518-2024, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roberts JM, Goyal V, Kularatna S, Chang AB, Kapur N, Chalmers JD, et al. The economic burden of bronchiectasis: a systematic review. Chest. (2023) 164:1396–421. doi: 10.1016/j.chest.2023.06.040, PMID: [DOI] [PubMed] [Google Scholar]
- 3.Choi H, Yang B, Kim YJ, Sin S, Jo YS, Kim Y, et al. Increased mortality in patients with non cystic fibrosis bronchiectasis with respiratory comorbidities. Sci Rep. (2021) 11:7126. doi: 10.1038/s41598-021-86407-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Choi H, Kim SH, Han K, Park TS, Park DW, Moon JY, et al. Association between exercise and risk of cardiovascular diseases in patients with non-cystic fibrosis bronchiectasis. Respir Res. (2022) 23:288. doi: 10.1186/s12931-022-02202-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Emirza C, Tiryaki P, Kara Kaya B, Akyurek E, Kuran AG. Physical activity level and sedentary behavior in patients with bronch iectasis: a systematic review of outcome measures and determinants. Respir Med Res. (2023) 84:101020. doi: 10.1016/j.resmer.2023.101020 [DOI] [PubMed] [Google Scholar]
- 6.Lee H, Ryu J, Chung SJ, Park DW, Park TS, Moon JY, et al. Overall and respiratory mortality reduction with physical activity in subjects with and without asthma. Allergy. (2023) 78:1677–80. doi: 10.1111/all.15638, PMID: [DOI] [PubMed] [Google Scholar]
- 7.Yang B, Lee H, Ryu J, Park DW, Park TS, Chung JE, et al. Impacts of regular physical activity on hospitalisation in chronic obstructive pulmonary disease: a nationwide population-based study. BMJ Open Respir Res. (2024) 11:e001789. doi: 10.1136/bmjresp-2023-001789, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cedeño de Jesús S, Almadana Pacheco V, Valido Morales A, Muñíz Rodríguez AM, Ayerbe García R, Arnedillo-Muñoz A. Exercise capacity and physical activity in non-cystic fibrosis bronchi ectasis after a pulmonary rehabilitation home-based Programme: a randomised controlled trial. Int J Environ Res Public Health. (2022) 19:11039. doi: 10.3390/ijerph191711039, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim SH, Kim Y. Big data research on severe asthma. Tuberc Respir Dis (Seoul). (2024) 87:213–20. doi: 10.4046/trd.2023.0186, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim SH, Han K, Park J, Park DW, Moon JY, Sim YS, et al. Association between non-cystic fibrosis bronchiectasis and the risk of incident dementia: a nationwide cohort study. Chron Respir Dis. (2023) 20:14799731231222282. doi: 10.1177/14799731231222282, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi H, Yoo JE, Han K, Choi W, Rhee SY, Lee H, et al. Body mass index, diabetes, and risk of tuberculosis: a retrospective cohort study. Front Nutr. (2021) 8:739766. doi: 10.3389/fnut.2021.739766, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lee HR, Yoo JE, Choi H, Han K, Lim YH, Lee H, et al. Tuberculosis and the risk of ischemic heart disease: a Nationwide cohort study. Clin Infect Dis. (2023) 76:1576–84. doi: 10.1093/cid/ciac946, PMID: [DOI] [PubMed] [Google Scholar]
- 13.Kim BG, Lee H, Kang MG, Kim JS, Moon JY. Risk of ischemic heart disease in chronic obstructive pulmonary disease: a Nationwide cohort study. J Korean Med Sci. (2023) 38:e344. doi: 10.3346/jkms.2023.38.e344, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lee HR, Yoo JE, Choi H, Han K, Jung JH, Park J, et al. Tuberculosis and risk of ischemic stroke: a Nationwide cohort study. Stroke. (2022) 53:3401–9. doi: 10.1161/STROKEAHA.122.039484, PMID: [DOI] [PubMed] [Google Scholar]
- 15.Chun MY. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. (2012) 33:144–51. doi: 10.4082/kjfm.2012.33.3.144, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park CS, Choi EK, Kyung D, Yoo J, Ahn HJ, Kwon S, et al. Physical activity changes and the risk of incident atrial fibrillation in patients with type 2 diabetes mellitus: a Nationwide longitudinal follow-up cohort study of 1.8 million subjects. Diabetes Care. (2023) 46:434–40. doi: 10.2337/dc22-1655, PMID: [DOI] [PubMed] [Google Scholar]
- 17.Ahn HJ, Lee SR, Choi EK, Han KD, Jung JH, Lim JH, et al. Association between exercise habits and stroke, heart failure, and mortality in Korean patients with incident atrial fibrillation: a nationwide population-based cohort study. PLoS Med. (2021) 18:e1003659. doi: 10.1371/journal.pmed.1003659, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. (2000) 32:S498–516. doi: 10.1097/00005768-200009001-00009, PMID: [DOI] [PubMed] [Google Scholar]
- 19.Oh JY, Yang YJ, Kim BS, Kang JH. Validity and reliability of Korean version of international physical activity questionnaire (IPAQ) short form. J Korean Acad Fam Med. (2007) 28:532–41. [Google Scholar]
- 20.Zimmermann-Sloutskis D, Wanner M, Zimmermann E, Martin BW. Physical activity levels and determinants of change in young adults: a longitudinal panel study. Int J Behav Nutr Phys Act. (2010) 7:2. doi: 10.1186/1479-5868-7-2, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lauer EE, Jackson AW, Martin SB, Morrow JR, Jr. Meeting USDHHS physical activity guidelines and health outcomes. Int J Exerc Sci. (2017) 10:121–7. doi: 10.70252/AZKZ3147, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoon M, Yang PS, Jin MN, Yu HT, Kim TH, Jang E, et al. Association of Physical Activity Level with Risk of dementia in a Nationwide cohort in Korea. JAMA Netw Open. (2021) 4:e2138526. doi: 10.1001/jamanetworkopen.2021.38526, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee SJ, Kim HJ, Kim J, Pyo WK, Kim JH, Ahn JY, et al. Effect of physical activity on risk reduction of infective endocarditis among patients with diabetes: a nationwide cohort study. Sci Rep. (2024) 14:22254. doi: 10.1038/s41598-024-73993-6, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Choi H, Lee H, Ryu J, Chung SJ, Park DW, Sohn JW, et al. Bronchiectasis and increased mortality in patients with corticosteroid-dependent severe asthma: a nationwide population study. Ther Adv Respir Dis. (2020) 14:1753466620963030. doi: 10.1177/1753466620963030, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park HY, Kang D, Lee H, Shin SH, Kang M, Kong S, et al. Impact of chronic obstructive pulmonary disease on mortality: a large national cohort study. Respirology. (2020) 25:726–34. doi: 10.1111/resp.13678, PMID: [DOI] [PubMed] [Google Scholar]
- 26.Lee H, Ryu J, Chung SJ, Park DW, Sohn JW, Yoon HJ, et al. Coexisting COPD increases mortality in patients with corticosteroid-dependent asthma: a nationwide population-based study. Allergy Asthma Immunol Res. (2020) 12:821–31. doi: 10.4168/aair.2020.12.5.821, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Yang B, Choi H, Lee SK, Chung SJ, Yeo Y, Shin YM, et al. Risk of coronavirus disease 2019 occurrence, severe presentation, and mortality in patients with lung cancer. Cancer Res Treat. (2021) 53:678–84. doi: 10.4143/crt.2020.1242, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yeo Y, Lee H, Ryu J, Chung SJ, Park TS, Park DW, et al. Additive effects of coexisting respiratory comorbidities on overall or respiratory mortality in patients with asthma: a national cohort study. Sci Rep. (2022) 12:8105. doi: 10.1038/s41598-022-12103-w, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choi H, Han K, Jung JH, Park SH, Kim SH, Kang HK, et al. Long-term mortality of tuberculosis survivors in Korea: a population-based longitudinal study. Clin Infect Dis. (2023) 76:e973–81. doi: 10.1093/cid/ciac411, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lee H, Kim BG, Jeong CY, Park DW, Park TS, Moon JY, et al. Long-term impacts of COVID-19 on severe exacerbation and mortality in adult asthma: a nationwide population-based cohort study. J Allergy Clin Immunol Pract. (2024) 12:1783–1793.e4. doi: 10.1016/j.jaip.2024.03.035, PMID: [DOI] [PubMed] [Google Scholar]
- 31.Cho SH, Lee H, Kwon H, Shin DW, Joh HK, Han K, et al. Association of underweight status with the risk of tuberculosis: a nationwide population-based cohort study. Sci Rep. (2022) 12:16207. doi: 10.1038/s41598-022-20550-8, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yang B, Han K, Kim B, Kang HK, Kim JS, Kim EG, et al. Association between smoking status and incident non-cystic fibrosis bronchiectasis in young adults: a nationwide population-based study. J Pers Med. (2022) 12:691. doi: 10.3390/jpm12050691, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yeo Y, Yoo JE, Han K, Jung JH, Choi H, Park J, et al. Risk of dementia in survivors of active tuberculosis in Korea: a nationwide cohort study. J Infect Public Health. (2024) 17:286–92. doi: 10.1016/j.jiph.2023.12.006, PMID: [DOI] [PubMed] [Google Scholar]
- 34.Kim SH, Lee H, Jung JH, Kim BG, Park DW, Park TS, et al. Asthma increases long-term risk of death by suicide: a nationwide population-based cohort study. J Allergy Clin Immunol Pract. (2024). doi: 10.1016/j.jaip.2024.11.013, PMID: (Online ahead of print). [DOI] [PubMed] [Google Scholar]
- 35.Lee H, Choi H, Yang B, Lee SK, Park TS, Park DW, et al. Interstitial lung disease increases susceptibility to and severity of COVID-19. Eur Respir J. (2021) 58:2004125. doi: 10.1183/13993003.04125-2020, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Choi H, Park HY, Han K, Yoo J, Shin SH, Yang B, et al. Non-cystic fibrosis bronchiectasis increases the risk of lung cancer independent of smoking status. Ann Am Thorac Soc. (2022) 19:1551–60. doi: 10.1513/AnnalsATS.202111-1257OC, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yoo JE, Kim D, Han K, Rhee SY, Shin DW, Lee H. Diabetes status and association with risk of tuberculosis among Korean adults. JAMA Netw Open. (2021) 4:e2126099. doi: 10.1001/jamanetworkopen.2021.26099, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Choi H, Han K, Yang B, Shin DW, Sohn JW, Lee H. Female reproductive factors and incidence of nontuberculous mycobacterial pulmonary disease among postmenopausal women in Korea. Clin Infect Dis. (2022) 75:1397–404. doi: 10.1093/cid/ciac134, PMID: [DOI] [PubMed] [Google Scholar]
- 39.Jin Z. Does rheumatoid arthritis increase the risk of COPD? Chest. (2024) 166:e126–7. doi: 10.1016/j.chest.2024.03.046, PMID: [DOI] [PubMed] [Google Scholar]
- 40.Choi H, Han K, Jung JH, Park J, Kim BG, Yang B, et al. Impact of rheumatoid arthritis and seropositivity on the risk of non-cystic fibrosis bronchiectasis. Chest. (2024) 165:1330–40. doi: 10.1016/j.chest.2024.01.001, PMID: [DOI] [PubMed] [Google Scholar]
- 41.Kim Y, Yoon JH, Ryu J, Yang B, Chung SJ, Kang HK, et al. Gastroesophageal reflux disease increases susceptibility to nontuberculous mycobacterial pulmonary disease. Chest. (2023) 163:270–80. doi: 10.1016/j.chest.2022.08.2228, PMID: [DOI] [PubMed] [Google Scholar]
- 42.Moon SM, Choi H, Kim SH, Kang HK, Park DW, Jung JH, et al. Increased lung cancer risk and associated risk factors in tuberculosis survivors: a Korean population-based study. Clin Infect Dis. (2023) 77:1329–39. doi: 10.1093/cid/ciad373, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kim BG, Lee H, Jeong CY, Yeom SW, Park DW, Park TS, et al. Risk of newly diagnosed interstitial lung disease after COVID-19 and impact of vaccination: a nationwide population-based cohort study. Front Public Health. (2023) 11:1295457. doi: 10.3389/fpubh.2023.1295457, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lee H, Kim SH, Lee SK, Choi H, Chung SJ, Park DW, et al. Impact of air pollution on healthcare utilization in patients with bronchiectasis. Front Med (Lausanne). (2023) 10:1233516. doi: 10.3389/fmed.2023.1233516, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Strain T, Flaxman S, Guthold R, Semenova E, Cowan M, Riley LM, et al. National, regional, and global trends in insufficient physical activity among adults from 2000 to 2022: a pooled analysis of 507 population-based surveys with 5·7 million participants. Lancet Glob Health. (2024) 12:e1232–43. doi: 10.1016/S2214-109X(24)00150-5, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Alcaraz-Serrano V, Arbillaga-Etxarri A, Oscanoa P, Fernández-Barat L, Bueno L, Amaro R, et al. Exacerbations and changes in physical activity and sedentary behaviour in patients with bronchiectasis after 1 year. J Clin Med. (2021) 10:3628. doi: 10.3390/jcm10061190, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bradley JM, Wilson JJ, Hayes K, Kent L, McDonough S, Tully MA, et al. Sedentary behaviour and physical activity in bronchiectasis: a cross-sectional study. BMC Pulm Med. (2015) 15:61. doi: 10.1186/s12890-015-0046-7, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de Camargo AA, Boldorini JC, Holland AE, de Castro RAS, Lanza FC, Athanazio RA, et al. Determinants of peripheral muscle strength and activity in daily life in people with bronchiectasis. Phys Ther. (2018) 98:153–61. doi: 10.1093/ptj/pzx123, PMID: [DOI] [PubMed] [Google Scholar]
- 49.Pehlivan E, Niksarlıoğlu EY, Balcı A, Kılıç L. The effect of pulmonary rehabilitation on the physical activity level and general clinical status of patients with bronchiectasis. Turk Thorac J. (2019) 20:30–5. doi: 10.5152/TurkThoracJ.2018.18093, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Annear M. Sedentary behavior and physical inactivity in the Asia-Pacific region: current challenges and emerging concerns. Int J Environ Res Public Health. (2022) 19:935. doi: 10.3390/ijerph19159351, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.World Health Organization . Global recommendations on physical activity for health. (2010). Available at: https://www.who.int/publications/i/item/9789241599979 (Accessed February 12, 2025). [PubMed]
- 52.Ellis HC, Cowman S, Fernandes M, Wilson R, Loebinger MR. Predicting mortality in bronchiectasis using bronchiectasis severity index and FACED scores: a 19-year cohort study. Eur Respir J. (2016) 47:482–9. doi: 10.1183/13993003.01312-2015, PMID: [DOI] [PubMed] [Google Scholar]
- 53.Kim SH, Kim C, Jeong I, Lee SJ, Kim TH, Lee CY, et al. Chronic obstructive pulmonary disease is associated with decreased quality of life in bronchiectasis patients: findings from the KMBARC registry. Front Med (Lausanne). (2021) 8:722124. doi: 10.3389/fmed.2021.722124, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Chalmers JD, Goeminne P, Aliberti S, McDonnell MJ, Lonni S, Davidson J, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. (2014) 189:576–85. doi: 10.1164/rccm.201309-1575OC, PMID: [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data analyzed in this study is subject to the following licenses/restrictions: the data that support the findings of this study are available from Korea NHIS but restrictions apply to the availability of these data, which were used under license for the current study, and so are not publicly available. Requests to access these datasets should be directed to https://nhiss.nhis.or.kr/bd/ab/bdaba001cv.do.


