Abstract
Thoracic outlet syndrome (TOS) is a group of disorders characterized by the compression of neurovascular structures at the thoracic outlet. Arterial TOS, the least common but most severe form, carries significant thromboembolic risks and has a known association with cervical ribs. Synostosis of a complete first and second rib, termed the Srb anomaly, is rare and occurs in approximately 0.2% of the population. Here, we present a unique case of a 17-year-old boy with right upper extremity claudication owing to arterial TOS from an Srb anomaly. This case emphasizes the successful management of an uncommon condition, the importance of accurate diagnosis and timely intervention.
Keywords: Thoracic outlet, Rib resection, Anomalous rib
Arterial thoracic outlet syndrome (TOS) is a rare condition, affecting less than 1% of patients with TOS, but it carries significant risks of life- and limb-threatening thromboembolic complications.1,2 This form of TOS is most commonly associated with bone abnormalities that compress the subclavian artery, with cervical ribs being the most frequent anomaly, found in nearly 80% of affected patients.2
Other bone abnormalities include an anomalous first rib, a prominent C7 transverse process, or callus formation from previous fractures of the clavicle or first rib.3 Srb anomaly, characterized by synostosis of the first and second ribs is very rare4 and can also lead to significant compression of the subclavian artery, resulting in aneurysmal degeneration and subsequent thromboembolic events, such as upper extremity ischemia.
Diagnosis can be challenging, and treatment typically involves the removal of the bony abnormality via a supraclavicular or paraclavicular approach, along with managing the aneurysmal arterial segment. However, given that these patients are often young, deferring arterial reconstruction in appropriate cases can reduce the need for this reconstruction altogether.
We present the successful management of a 17-year-old boy with right upper extremity claudication owing to arterial TOS caused by Srb anomaly, where the bony abnormality was removed via a transaxillary approach without need for arterial reconstruction. The patient has provided written consent for publication of their case.
Case Report
A 17-year-old male baseball player presented with a 2-month history of right upper extremity hypersensitivity to cold weather, right forearm cramping during exercise, and absent radial and ulnar pulses. His only prior medical history was an endovascular repair for a ventricular septal defect at age 1.
A computed tomography angiogram of the chest and right upper extremity revealed a right brachial artery occlusion above the elbow with reconstitution into the radial artery, compression of the subclavian artery between the first rib and clavicle, and synostosis of the first and second ribs in the form of a Srb anomaly (Fig 1). Based on symptoms and computed tomography angiogram findings, a two-stage approach was performed: first, a right upper extremity angiogram with brachial artery thrombectomy; and second, a first rib resection.
Fig 1.
Preoperative computed tomography (CTA) chest and right upper extremity show a right subclavian artery compression between the first rib and the clavicle and a synostosis of the right first and second rib consistent with Srb anomaly.
Operative technique
Right upper extremity angiogram
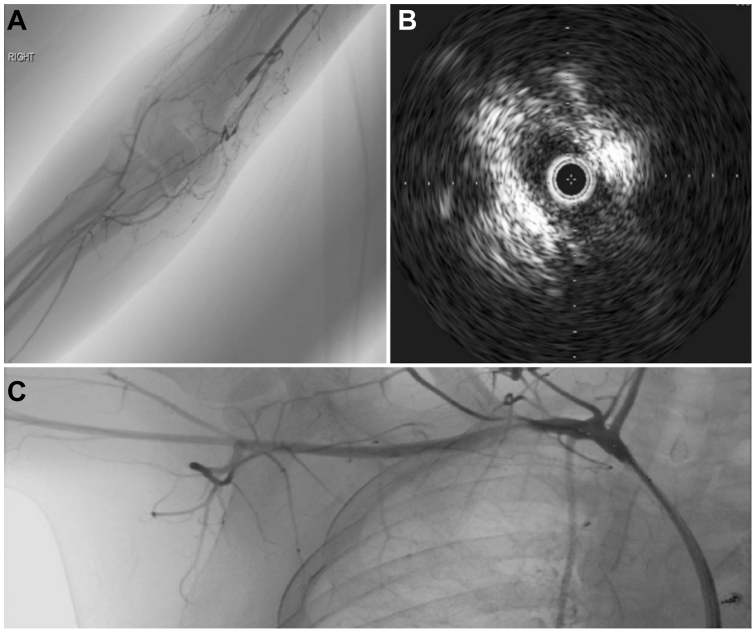
Via a left common femoral approach, a right upper extremity dynamic angiogram was performed demonstrating occlusion of the right brachial artery just above the elbow with distal reconstitution shortly beyond. In addition, there was significant compression of the subclavian artery between the first rib and the clavicle with near complete obliteration of flow with provocative maneuvers (abduction of the arm).
Intravascular ultrasound (IVUS) was performed demonstrating very small aneurysm degeneration distal to the costoclavicular junction with mural thrombus and complete collapse of the artery around the IVUS catheter with provocative maneuvers (Fig 2). Finally, thrombectomy using a lightening 7 penumbra suction thrombectomy device (Penumbra Inc., Alameda, CA) was performed of the brachial artery with significant improvement.
Fig 2.
(A) Right upper extremity angiogram show an occlusion of the brachial artery just above the elbow with distal reconstitution. (B) Intravascular ultrasound (IVUS) show complete collapse of the artery with provocative maneuvers. (C) Right upper extremity angiogram with provocative maneuvers.
Transaxillary first rib resection
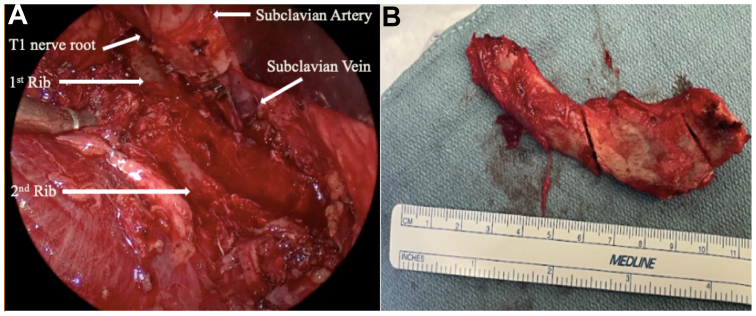
Subsequently, the patient returned to the operating room for a planned transaxillary first rib resection. Owing to minimal aneurysmal dilation and the specific nature of the bony abnormality, we opted for a transaxillary approach.
The patient was positioned laterally using a bean bag for stabilization. An incision was made in the deepest part of the axilla, and blunt dissection was carried out until the subclavian vein was identified. Significant adhesions were found between the abnormal first rib and the artery. The subclavius tendon was divided, and using a combination of a Kerrison rongeur, osteotome, and mallet, we separated the fused first rib from the second rib, leading to its complete removal (Fig 3 A and B).
Fig 3.
(A) Intraoperative image taken with laparoscope showing the patients anatomy. (B) An image of removed first rib.
The patient had an uncomplicated recovery and was discharged on postoperative day 1 with a 3-month course of anticoagulation. At the 3-month follow-up, the patient had returned to baseline function with the aid of physical therapy. He continued with follow-up with serial arterial duplex monitoring to rule out aneurysmal degeneration. At the 15-month follow-up, he reported working out six times a week with no restrictions, and the arterial duplex examination showed no mural thrombus or aneurysmal degeneration of the subclavian artery or signs of residual compression.
Discussion
Arterial TOS, although the least common form of TOS, is the most severe, accounting for less than 1% of all cases. Despite its rarity, arterial TOS poses significant risks, including life- and limb-threatening thromboembolic events, making early recognition and intervention essential. It typically occurs in younger, physically active patients and is often linked to congenital bony anomalies that compress the subclavian artery, leading to arterial intimal damage, thrombosis, distal embolism, or aneurysm formation.5
Accurate diagnosis of this pathology is critical to prevent irreversible complications. Although plain radiography of the neck and chest often demonstrates bone abnormalities that may aid in the diagnosis of TOS, computed tomography angiography not only provides detailed visualization of the vascular structures, but also allows for the use of three-dimensional reconstructive software to better understand patient anatomy, ensuring that no rib abnormalities are overlooked.6 Once the diagnosis is confirmed, IVUS examination is invaluable in identifying aneurysmal changes, mural thrombus, and dynamic compression during provocative maneuvers.7
Regarding management, in cases where patients present with embolic events, performing an angiogram followed by thrombectomy is essential to try to restore perfusion to the hand. Additionally, as mentioned, IVUS examination should be used to confirm arterial compression during provocative maneuvers and evaluate the subclavian artery. After restoring blood flow, removal of the first rib and decompression of the thoracic outlet are crucial steps to prevent further episodes. In cases of arterial TOS caused by the presence of a cervical rib, both the first rib and the cervical rib must be excised surgically. In our case, we successfully separated the fused first and second rib, thereby avoiding the need to remove the second rib.
The supraclavicular or paraclavicular approach has been the gold standard treatment of arterial TOS. These approaches provide superior access to the subclavian artery, enabling effective decompression and, if necessary, arterial reconstruction. The supraclavicular approach, in particular, offers enhanced vascular control and is especially advantageous for facilitating reconstruction when indicated.2,3,5, 6, 7, 8 However, in patients with minimal arterial damage who do not require vascular reconstruction, a transaxillary approach has been also been described.9
The presented case describes one of the first reported case of a patient with arterial TOS owing to Srb anomaly. Several key considerations are worth noting. First, although a supraclavicular approach with vascular reconstruction is typically preferred for treating arterial TOS, a transaxillary approach also provides an effective alternative in cases that do not mandate arterial reconstruction. This approach offers excellent visualization of the thoracic outlet anatomy, facilitating the separation of the first and second ribs, and allowing for the removal of the first rib.
In our case, owing to the minimal aneurysmal degeneration or arterial damage, and the patient’s age, we opted not to perform vascular reconstruction. However, if reconstruction becomes necessary, the axillary incision can be closed, and the patient can be repositioned supine to continue with that portion of the surgery. Additionally, given the presence of intraluminal thrombus detected by IVUS, we decided to place the patient on a 3-month course of anticoagulation to prevent future embolic events. There was no residual mural thrombus noted on follow-up ultrasound examination at 3 or 15 months. We will continue to follow the patient with serial duplex ultrasound examinations and plan to perform a vascular reconstruction if the aneurysm segment degenerates.
Conclusions
Arterial TOS-linked Srb anomaly is an unusual condition with potential limb-threatening thromboembolic complications. Early recognition, accurate diagnosis, and timely surgical intervention are critical in preventing these outcomes. This case highlights successful management, stressing accurate diagnosis and intervention keeping the option open for future vascular reconstruction via a supraclavicular approach if needed.
Funding
None.
Disclosures
None.
Footnotes
The editors and reviewers of this article have no relevant financial relationships to disclose per the Journal policy that requires reviewers to decline review of any manuscript for which they may have a conflict of interest.
References
- 1.Sanders R.J., Hammond S.L., Rao N.M. Diagnosis of thoracic outlet syndrome. J Vasc Surg. 2007;46:601–604. doi: 10.1016/j.jvs.2007.04.050. [DOI] [PubMed] [Google Scholar]
- 2.Vemuri C., McLaughlin L.N., Abuirqeba A.A., Thompson R.W. Clinical presentation and management of arterial thoracic outlet syndrome. J Vasc Surg. 2017;65:1429–1439. doi: 10.1016/j.jvs.2016.11.039. [DOI] [PubMed] [Google Scholar]
- 3.Chang K.Z., Likes K., Davis K., Demos J., Freischlag J.A. The significance of cervical ribs in thoracic outlet syndrome. J Vasc Surg. 2013;57:771–775. doi: 10.1016/j.jvs.2012.08.110. [DOI] [PubMed] [Google Scholar]
- 4.Oner Z., Oner S., Sahin N.E., Cay M. Evaluation of congenital rib anomalies with multi-detector computed tomography in the Turkish population. Folia Morphol (Warsz) 2024;83:182–191. doi: 10.5603/FM.a2023.0006. [DOI] [PubMed] [Google Scholar]
- 5.Aljabri B., Al-Omran M. Surgical management of vascular thoracic outlet syndrome: a teaching hospital experience. Ann Vasc Dis. 2013;6:74–79. doi: 10.3400/avd.oa.12.00081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Moriarty J.M., Bandyk D.F., Broderick D.F., et al. ACR appropriateness criteria imaging in the diagnosis of thoracic outlet syndrome. J Am Coll Radiol. 2015;12:438–443. doi: 10.1016/j.jacr.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 7.Kim T.I., Sarac T.P., Orion K.C. Intravascular ultrasound in venous thoracic outlet syndrome. Ann Vasc Surg. 2019;54:118–122. doi: 10.1016/j.avsg.2018.08.077. [DOI] [PubMed] [Google Scholar]
- 8.Duwayri Y.M., Thompson R.W. In: Atlas of vascular surgery and endovascular therapy. Chaikof E.L., Cambria R.P., editors. Elsevier Saunders; 2014. Supraclavicular approach for surgical treatment of thoracic outlet syndrome; pp. 172–192. [Google Scholar]
- 9.Akkuş M., Kose S., Sönmezoğlu Y. Transaxillary first rib resection for treatment of the thoracic outlet syndrome. J Vis Exp. 2020;13 doi: 10.3791/59659. [DOI] [PubMed] [Google Scholar]