Abstract
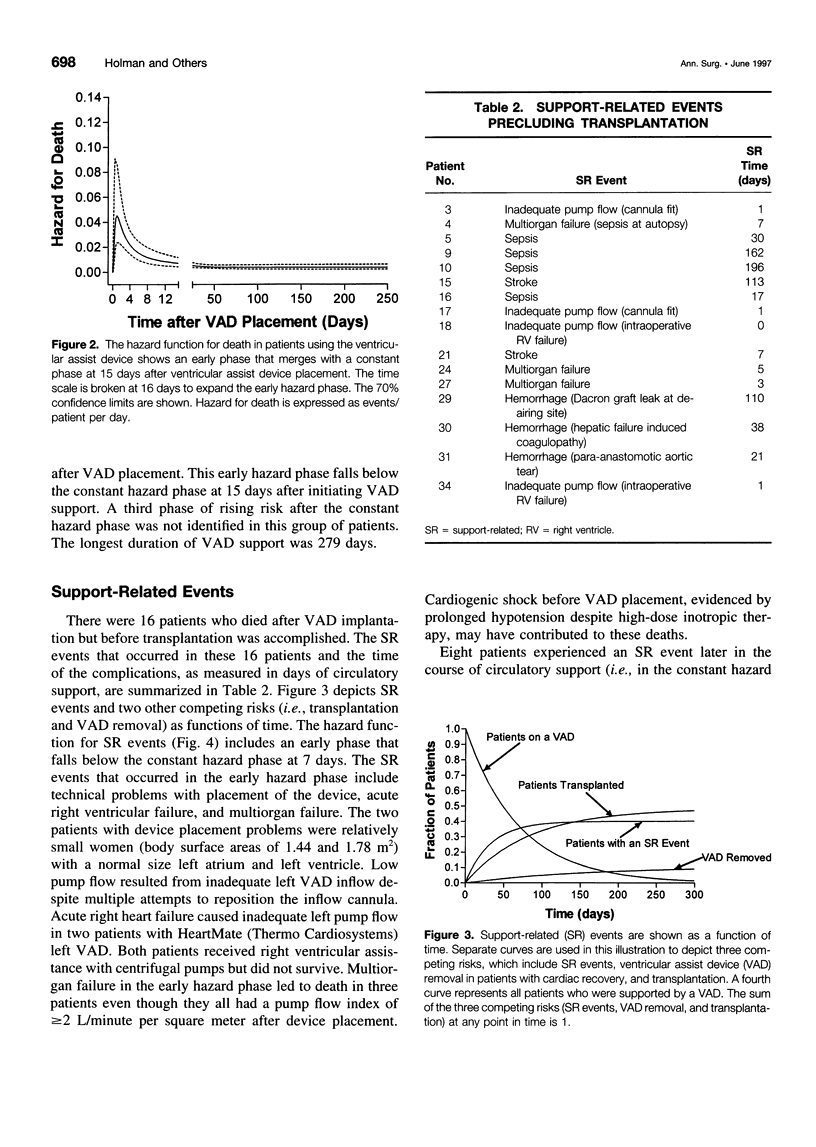
OBJECTIVE AND BACKGROUND: Ventricular assist devices (VADs) have been used for temporary circulatory support pending transplantation or recovery of the native heart. Outcome in 38 patients treated at the authors' institution with VADs pending transplantation was analyzed to provide information relevant to the future use of VADs as permanent implants. METHODS: Thoratec (Thoratec Laboratories, Pleasanton, CA) or HeartMate (Thermo Cardiosystems, Woburn, MA) VADs were used in all cases. Patients were considered for VAD placement if they were candidates for cardiac transplantation and fulfilled the criteria for the Food and Drug Administration investigational Device Exemption trials. The following adverse events were included in the analysis; death during VAD support, device malfunction, bleeding, neurologic events, support-related events that preclude transplantation, and device-related infections. Patient survival and complication rates were quantified using the Kaplan-Meier method, competing risk analysis, and hazard functions. RESULTS: Nineteen patients had transplantation. Three patients had VAD removal after cardiac recovery and 16 died without transplantation. The duration of VAD support ranged from 0 to 279 days. The hazard function for death during VAD support had an early phase that lasted for 2 weeks after VAD placement, and early death was related to the preimplant condition of the patient. Device-related infections were noted in 11 patients. Seven of these patients had transplantation after clearing the infection, whereas four died without transplantation. Neurologic events occurred in seven patients. There were no device malfunctions that led to patient death. CONCLUSIONS: The absence of fatal device malfunctions suggests that longer term support with current VAD designs is feasible. Appropriate patient selection, infection control, and avoidance of thromboembolic neurologic complications will be crucial to the success of permanent VAD use.
Full text
PDF








Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Catanese K. A., Goldstein D. J., Williams D. L., Foray A. T., Illick C. D., Gardocki M. T., Weinberg A. D., Levin H. R., Rose E. A., Oz M. C. Outpatient left ventricular assist device support: a destination rather than a bridge. Ann Thorac Surg. 1996 Sep;62(3):646–653. doi: 10.1016/s0003-4975(96)00456-0. [DOI] [PubMed] [Google Scholar]
- Davis R., Whittington R. Aprotinin. A review of its pharmacology and therapeutic efficacy in reducing blood loss associated with cardiac surgery. Drugs. 1995 Jun;49(6):954–983. doi: 10.2165/00003495-199549060-00008. [DOI] [PubMed] [Google Scholar]
- Dew M. A., Kormos R. L., Roth L. H., Armitage J. M., Pristas J. M., Harris R. C., Capretta C., Griffith B. P. Life quality in the era of bridging to cardiac transplantation. Bridge patients in an outpatient setting. ASAIO J. 1993 Apr-Jun;39(2):145–152. [PubMed] [Google Scholar]
- Didisheim P., Olsen D. B., Farrar D. J., Portner P. M., Griffith B. P., Pennington D. G., Joist J. H., Schoen F. J., Gristina A. G., Anderson J. M. Infections and thromboembolism with implantable cardiovascular devices. ASAIO Trans. 1989 Jan-Mar;35(1):54–70. [PubMed] [Google Scholar]
- Evans R. W., Orians C. E., Ascher N. L. The potential supply of organ donors. An assessment of the efficacy of organ procurement efforts in the United States. JAMA. 1992 Jan 8;267(2):239–246. [PubMed] [Google Scholar]
- Farrar D. J., Hill J. D. Recovery of major organ function in patients awaiting heart transplantation with Thoratec ventricular assist devices. Thoratec Ventricular Assist Device Principal Investigators. J Heart Lung Transplant. 1994 Nov-Dec;13(6):1125–1132. [PubMed] [Google Scholar]
- Farrar D. J., Hill J. D. Univentricular and biventricular Thoratec VAD support as a bridge to transplantation. Ann Thorac Surg. 1993 Jan;55(1):276–282. doi: 10.1016/0003-4975(93)90537-r. [DOI] [PubMed] [Google Scholar]
- Frazier O. H., Rose E. A., Macmanus Q., Burton N. A., Lefrak E. A., Poirier V. L., Dasse K. A. Multicenter clinical evaluation of the HeartMate 1000 IP left ventricular assist device. Ann Thorac Surg. 1992 Jun;53(6):1080–1090. doi: 10.1016/0003-4975(92)90393-i. [DOI] [PubMed] [Google Scholar]
- Frazier O. H., Rose E. A., McCarthy P., Burton N. A., Tector A., Levin H., Kayne H. L., Poirier V. L., Dasse K. A. Improved mortality and rehabilitation of transplant candidates treated with a long-term implantable left ventricular assist system. Ann Surg. 1995 Sep;222(3):327–338. doi: 10.1097/00000658-199509000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein D. J., Seldomridge J. A., Chen J. M., Catanese K. A., DeRosa C. M., Weinberg A. D., Smith C. R., Rose E. A., Levin H. R., Oz M. C. Use of aprotinin in LVAD recipients reduces blood loss, blood use, and perioperative mortality. Ann Thorac Surg. 1995 May;59(5):1063–1068. doi: 10.1016/0003-4975(95)00086-z. [DOI] [PubMed] [Google Scholar]
- Graham T. R., Dasse K., Coumbe A., Salih V., Marrinan M. T., Frazier O. H., Lewis C. T. Neo-intimal development on textured biomaterial surfaces during clinical use of an implantable left ventricular assist device. Eur J Cardiothorac Surg. 1990;4(4):182–190. doi: 10.1016/1010-7940(90)90002-h. [DOI] [PubMed] [Google Scholar]
- Gristina A. G. Biomaterial-centered infection: microbial adhesion versus tissue integration. Science. 1987 Sep 25;237(4822):1588–1595. doi: 10.1126/science.3629258. [DOI] [PubMed] [Google Scholar]
- Gristina A. G., Giridhar G., Gabriel B. L., Naylor P. T., Myrvik Q. N. Cell biology and molecular mechanisms in artificial device infections. Int J Artif Organs. 1993 Nov;16(11):755–763. [PubMed] [Google Scholar]
- Gristina A. G. Implant failure and the immuno-incompetent fibro-inflammatory zone. Clin Orthop Relat Res. 1994 Jan;(298):106–118. [PubMed] [Google Scholar]
- Harasaki H., Fukamachi K., Massiello A., Chen J. F., Himley S. C., Fukumura F., Muramoto K., Niu S., Wika K., Davies C. R. Progress in Cleveland Clinic-Nimbus total artificial heart development. ASAIO J. 1994 Jul-Sep;40(3):M494–M498. [PubMed] [Google Scholar]
- Holman W. L., Murrah C. P., Ferguson E. R., Bourge R. C., McGiffin D. C., Kirklin J. K. Infections during extended circulatory support: University of Alabama at Birmingham experience 1989 to 1994. Ann Thorac Surg. 1996 Jan;61(1):366–373. doi: 10.1016/0003-4975(95)01021-1. [DOI] [PubMed] [Google Scholar]
- Massad M. G., McCarthy P. M., Smedira N. G., Cook D. J., Ratliff N. B., Goormastic M., Vargo R. L., Navia J., Young J. B., Stewart R. W. Does successful bridging with the implantable left ventricular assist device affect cardiac transplantation outcome? J Thorac Cardiovasc Surg. 1996 Nov;112(5):1275–1283. doi: 10.1016/S0022-5223(96)70141-1. [DOI] [PubMed] [Google Scholar]
- McCarthy P. M., Wang N., Vargo R. Preperitoneal insertion of the HeartMate 1000 IP implantable left ventricular assist device. Ann Thorac Surg. 1994 Mar;57(3):634–638. doi: 10.1016/0003-4975(94)90557-6. [DOI] [PubMed] [Google Scholar]
- Menconi M. J., Pockwinse S., Owen T. A., Dasse K. A., Stein G. S., Lian J. B. Properties of blood-contacting surfaces of clinically implanted cardiac assist devices: gene expression, matrix composition, and ultrastructural characterization of cellular linings. J Cell Biochem. 1995 Mar;57(3):557–573. doi: 10.1002/jcb.240570320. [DOI] [PubMed] [Google Scholar]
- Mertes P. M., Pinelli G., Hubert T., Carteaux J. P., Hottier E., Larcan A., Villemot J. P. Impact of nitric oxide inhalation on right ventricular failure after implantation of Novacor left ventricular assist system. J Thorac Cardiovasc Surg. 1995 Jun;109(6):1251–1251. doi: 10.1016/S0022-5223(95)70213-X. [DOI] [PubMed] [Google Scholar]
- Myers T. J., Dasse K. A., Macris M. P., Poirier V. L., Cloy M. J., Frazier O. H. Use of a left ventricular assist device in an outpatient setting. ASAIO J. 1994 Jul-Sep;40(3):M471–M475. doi: 10.1097/00002480-199407000-00044. [DOI] [PubMed] [Google Scholar]
- Pennington D. G., McBride L. R., Swartz M. T., Kanter K. R., Kaiser G. C., Barner H. B., Miller L. W., Naunheim K. S., Fiore A. C., Willman V. L. Use of the Pierce-Donachy ventricular assist device in patients with cardiogenic shock after cardiac operations. Ann Thorac Surg. 1989 Jan;47(1):130–135. doi: 10.1016/0003-4975(89)90254-3. [DOI] [PubMed] [Google Scholar]
- Reedy J. E., Pennington D. G., Miller L. W., McBride L. R., Lohmann D. P., Noedel N. R., Swartz M. T. Status I heart transplant patients: conventional versus ventricular assist device support. J Heart Lung Transplant. 1992 Mar-Apr;11(2 Pt 1):246–252. [PubMed] [Google Scholar]
- Salih V., Graham T. R., Berry C. L., Coumbe A., Smith S. C., Dasse K., Frazier O. H. The lining of textured surfaces in implantable left ventricular assist devices. An immunocytochemical and electronmicroscopic study. Am J Cardiovasc Pathol. 1993;4(4):317–325. [PubMed] [Google Scholar]
- Sasaki T., Takatani S., Shiono M., Sakuma I., Noon G. P., Nosé Y., DeBakey M. E. A biolized, compact, low noise, high performance implantable electromechanical ventricular assist system. ASAIO Trans. 1991 Jul-Sep;37(3):M249–M251. [PubMed] [Google Scholar]
- Winowich S., Nastala C. J., Pristas J. M., Griffith B. P., Kormos R. L. Discharging patients who are undergoing mechanical circulatory support. Ann Thorac Surg. 1996 Jan;61(1):478–479. doi: 10.1016/0003-4975(95)00993-0. [DOI] [PubMed] [Google Scholar]


