Abstract
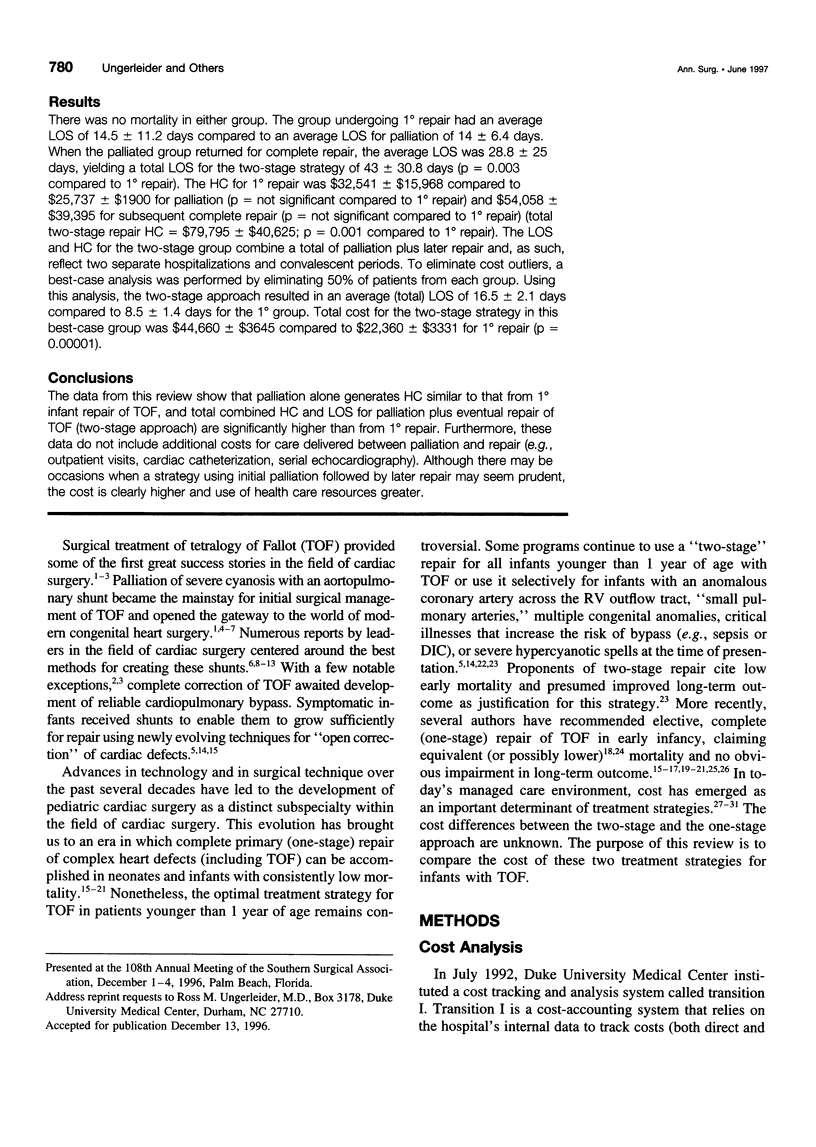
OBJECTIVE: This study compares the total hospital cost (HC) for one-stage versus "two-stage" repair of tetralogy of Fallot (TOF) in infants younger than 1 year of age. SUMMARY BACKGROUND DATA: Total (one-stage) correction of TOF is now being performed with excellent results in infancy. Alternatively, a two-stage approach, with palliation of infants in the first year of life, followed by complete repair at a later time can be used. In some institutions, the two-stage approach is standard practice for infants younger than 1 year of age or is used selectively in patients with an anomalous coronary artery across the right ventricular outflow tract (RVOT), "small pulmonary arteries," multiple congenital anomalies, critical illnesses (CI), which increase the risk of bypass (e.g., sepsis or DIC), or severe hypercyanotic spells (HS) at the time of presentation. The cost implications of these two approaches are unknown. METHODS: The authors reviewed 22 patients younger than 1 year of age who underwent repair of TOF at their institution between 1993 and 1995. Eighteen patients had one-stage (1 degree) repair (mean age, 3.4 +/- 3.1 months; range, 3 days-9 months) and 4 patients were treated by a staged approach with initial palliation (1.6 +/- 0.4 month; range, 1.5-2 months) followed by later repair (14.75 +/- 1.5 months; range, 13-16 months). The reasons for palliation were severe HS at time of presentation (two patients), anomalous coronary artery (one patient) and CI (one patient). In the 18 patients undergoing 1 degree repair, 3 (16.6%) presented with HS, 6 (33.3%) had a transanular repair, and 6 (33.3%) were able to be repaired through an entirely transatrial approach (youngest patient, 1.5 months). The HC (1996 dollars) and hospital length of stay (LOS; days) were evaluated for all patients. The HCs were calculated using transition I, which is a cost accounting system used by our medical center since July 1992. Transition I provides complete data on all direct and indirect hospital-based, nonprofessional costs. RESULTS: There was no mortality in either group. The group undergoing 1 degree repair had an average LOS of 14.5 +/- 11.2 days compared to an average LOS for palliation of 14 +/- 6.4 days. When the palliated group returned for complete repair, the average LOS was 28.8 +/- 25 days, yielding a total LOS for the two-stage strategy of 43 +/- 30.8 days (p = 0.003 compared to 1 degree repair). The HC for 1 degree repair was $32,541 +/- $15,968 compared to $25,737 +/- $1900 for palliation (p = not significant compared to 1 degree repair) and $54,058 +/- $39,395 for subsequent complete repair (p = not significant compared to 1 degree repair) (total two-stage repair HC = $79,795 +/- $40,625; p = 0.001 compared to 1 degree repair). The LOS and HC for the two-stage group combine a total of palliation plus later repair and, as such, reflect two separate hospitalizations and convalescent periods. To eliminate cost outliers, a best-case analysis was performed by eliminating 50% of patients from each group. Using this analysis, the two-stage approach resulted in an average (total) LOS of 16.5 +/- 2.1 days compared to 8.5 +/- 1.4 days for the 1 degree group. Total cost for the two-stage strategy in this best-case group was $44,660 +/- $3645 compared to $22,360 +/- $3331 for 1 degree repair (p = 0.00001). CONCLUSIONS: The data from this review show that palliation alone generates HC similar to that from 1 degree infant repair of TOF, and total combined HC and LOS for palliation plus eventual repair of TOF (two-stage approach) are significantly higher than from 1 degree repair. Furthermore, these data do not include additional costs for care delivered between palliation and repair (e.g., outpatient visits, cardiac catheterization, serial echocardiography). Although there may be occasions when a strategy using initial palliation followed by later repair may seem prudent, the cost is clearly higher and use of health care resources greater.
Full text
PDF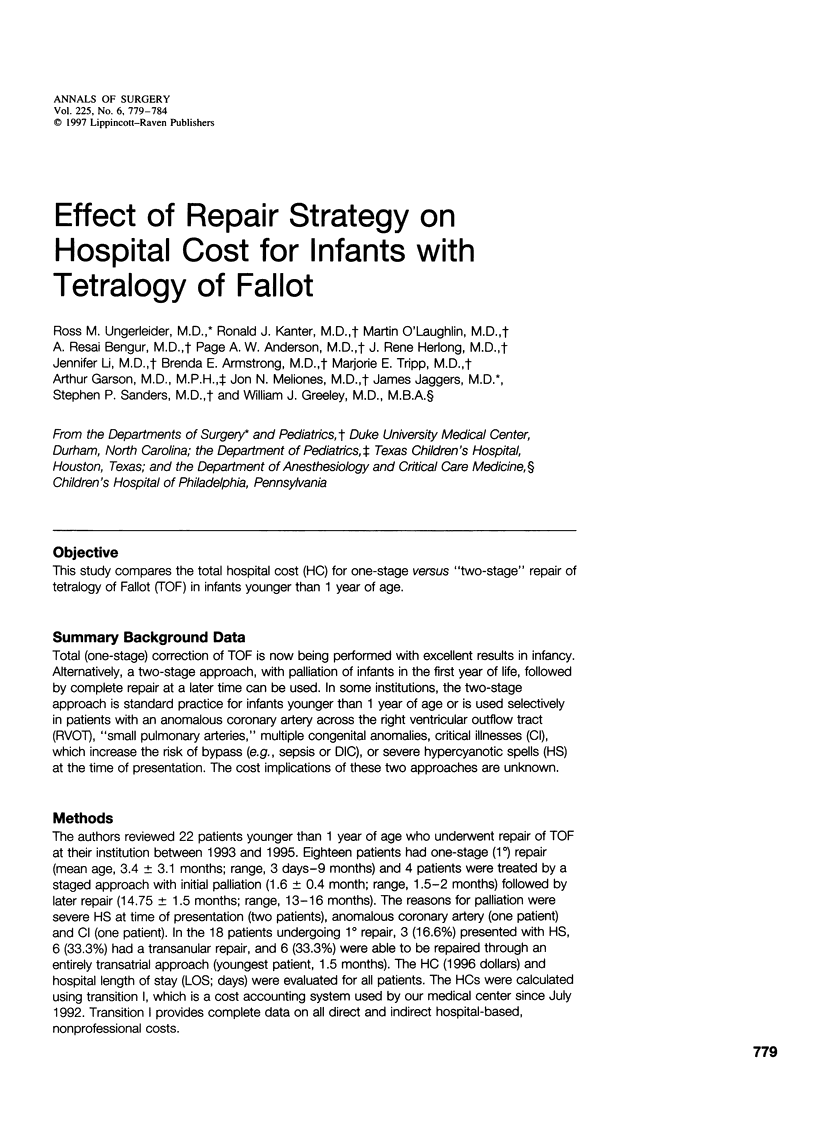

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Amato J. J., Marbey M. L., Bush C., Galdieri R. J., Cotroneo J. V., Bushong J. Systemic-pulmonary polytetrafluoroethylene shunts in palliative operations for congenital heart disease. Revival of the central shunt. J Thorac Cardiovasc Surg. 1988 Jan;95(1):62–69. [PubMed] [Google Scholar]
- Arciniegas E., Blackstone E. H., Pacifico A. D., Kirklin J. W. Classic shunting operations as part of two-stage repair for tetralogy of Fallot. Ann Thorac Surg. 1979 Jun;27(6):514–518. doi: 10.1016/s0003-4975(10)63360-7. [DOI] [PubMed] [Google Scholar]
- Arciniegas E., Farooki Z. Q., Hakimi M., Green E. W. Results of two-stage surgical treatment of tetralogy of Fallot. J Thorac Cardiovasc Surg. 1980 Jun;79(6):876–883. [PubMed] [Google Scholar]
- Barragry T. P., Ring W. S., Blatchford J. W., Foker J. E. Central aorta-pulmonary artery shunts in neonates with complex cyanotic congenital heart disease. J Thorac Cardiovasc Surg. 1987 May;93(5):767–774. [PubMed] [Google Scholar]
- Berwick D. M. Continuous improvement as an ideal in health care. N Engl J Med. 1989 Jan 5;320(1):53–56. doi: 10.1056/NEJM198901053200110. [DOI] [PubMed] [Google Scholar]
- Dudley R. A., Harrell F. E., Jr, Smith L. R., Mark D. B., Califf R. M., Pryor D. B., Glower D., Lipscomb J., Hlatky M. Comparison of analytic models for estimating the effect of clinical factors on the cost of coronary artery bypass graft surgery. J Clin Epidemiol. 1993 Mar;46(3):261–271. doi: 10.1016/0895-4356(93)90074-b. [DOI] [PubMed] [Google Scholar]
- Ebert P. A. Past, present, and future of palliative shunts. Adv Cardiol. 1979;26:127–128. doi: 10.1159/000402399. [DOI] [PubMed] [Google Scholar]
- Gustafson R. A., Murray G. F., Warden H. E., Hill R. C., Rozar G. E., Jr Early primary repair of tetralogy of Fallot. Ann Thorac Surg. 1988 Mar;45(3):235–241. doi: 10.1016/s0003-4975(10)62455-1. [DOI] [PubMed] [Google Scholar]
- Ilbawi M. N., Grieco J., DeLeon S. Y., Idriss F. S., Muster A. J., Berry T. E., Klich J. Modified Blalock-Taussig shunt in newborn infants. J Thorac Cardiovasc Surg. 1984 Nov;88(5 Pt 1):770–775. [PubMed] [Google Scholar]
- Karl T. R., Sano S., Pornviliwan S., Mee R. B. Tetralogy of Fallot: favorable outcome of nonneonatal transatrial, transpulmonary repair. Ann Thorac Surg. 1992 Nov;54(5):903–907. doi: 10.1016/0003-4975(92)90646-l. [DOI] [PubMed] [Google Scholar]
- Kirklin J. K., Kirklin J. W., Blackstone E. H., Milano A., Pacifico A. D. Effect of transannular patching on outcome after repair of tetralogy of Fallot. Ann Thorac Surg. 1989 Dec;48(6):783–791. doi: 10.1016/0003-4975(89)90671-1. [DOI] [PubMed] [Google Scholar]
- Kirklin J. W., Blackstone E. H., Jonas R. A., Shimazaki Y., Kirklin J. K., Mayer J. E., Jr, Pacifico A. D., Castaneda A. R. Morphologic and surgical determinants of outcome events after repair of tetralogy of Fallot and pulmonary stenosis. A two-institution study. J Thorac Cardiovasc Surg. 1992 Apr;103(4):706–723. [PubMed] [Google Scholar]
- Kirklin J. W., Blackstone E. H., Pacifico A. D., Brown R. N., Bargeron L. M., Jr Routine primary repair vs two-stage repair of tetralogy of Fallot. Circulation. 1979 Aug;60(2):373–386. doi: 10.1161/01.cir.60.2.373. [DOI] [PubMed] [Google Scholar]
- LILLEHEI C. W., COHEN M., WARDEN H. E., READ R. C., AUST J. B., DEWALL R. A., VARCO R. L. Direct vision intracardiac surgical correction of the tetralogy of Fallot, pentalogy of Fallot, and pulmonary atresia defects; report of first ten cases. Ann Surg. 1955 Sep;142(3):418–442. doi: 10.1097/00000658-195509000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Laks H., Castaneda A. R. Subclavian arterioplasty for the ipsilateral Blalock-Taussig shunt. Ann Thorac Surg. 1975 Mar;19(3):319–321. doi: 10.1016/s0003-4975(10)64025-8. [DOI] [PubMed] [Google Scholar]
- Lamberti J. J., Carlisle J., Waldman J. D., Lodge F. A., Kirkpatrick S. E., George L., Mathewson J. W., Turner S. W., Pappelbaum S. J. Systemic-pulmonary shunts in infants and children. Early and late results. J Thorac Cardiovasc Surg. 1984 Jul;88(1):76–81. [PubMed] [Google Scholar]
- Lillehei C. W., Varco R. L., Cohen M., Warden H. E., Patton C., Moller J. H. The first open-heart repairs of ventricular septal defect, atrioventricular communis, and tetralogy of Fallot using extracorporeal circulation by cross-circulation: a 30-year follow-up. Ann Thorac Surg. 1986 Jan;41(1):4–21. doi: 10.1016/s0003-4975(10)64489-x. [DOI] [PubMed] [Google Scholar]
- Sabiston D. C., Jr Editorial: Role of the Blalock-Taussig operation in the hypoxic infant with tetralogy of Fallot. Ann Thorac Surg. 1976 Sep;22(3):303–304. doi: 10.1016/s0003-4975(10)64922-3. [DOI] [PubMed] [Google Scholar]
- Sousa Uva M., Lacour-Gayet F., Komiya T., Serraf A., Bruniaux J., Touchot A., Roux D., Petit J., Planché C. Surgery for tetralogy of Fallot at less than six months of age. J Thorac Cardiovasc Surg. 1994 May;107(5):1291–1300. [PubMed] [Google Scholar]
- Starnes V. A., Luciani G. B., Latter D. A., Griffin M. L. Current surgical management of tetralogy of Fallot. Ann Thorac Surg. 1994 Jul;58(1):211–215. doi: 10.1016/0003-4975(94)91102-9. [DOI] [PubMed] [Google Scholar]
- Touati G. D., Vouhé P. R., Amodeo A., Pouard P., Mauriat P., Leca F., Neveux J. Y. Primary repair of tetralogy of Fallot in infancy. J Thorac Cardiovasc Surg. 1990 Mar;99(3):396–403. [PubMed] [Google Scholar]
- Turley K., Tyndall M., Roge C., Cooper M., Turley K., Applebaum M., Tarnoff H. Critical pathway methodology: effectiveness in congenital heart surgery. Ann Thorac Surg. 1994 Jul;58(1):57–65. doi: 10.1016/0003-4975(94)91072-3. [DOI] [PubMed] [Google Scholar]
- Turley K., Tyndall M., Turley K. M., Roge C., Cooper M., Tarnoff H. Cardiovascular-radical outcome method is effective in complex congenital cardiac lesions. Ann Thorac Surg. 1996 Aug;62(2):386–392. [PubMed] [Google Scholar]
- Vobecky S. J., Williams W. G., Trusler G. A., Coles J. G., Rebeyka I. M., Smallhorn J., Burrows P., Gow R., Freedom R. M. Survival analysis of infants under age 18 months presenting with tetralogy of Fallot. Ann Thorac Surg. 1993 Oct;56(4):944–950. doi: 10.1016/0003-4975(93)90361-k. [DOI] [PubMed] [Google Scholar]
- Watson D. C., Jr, Bradley L. M., Midgley F. M., Scott L. P. Costs and results of cardiac operations in infants less than 4 months old. Are they worthwhile? J Thorac Cardiovasc Surg. 1986 May;91(5):667–673. [PubMed] [Google Scholar]
- de Leval M. R., McKay R., Jones M., Stark J., Macartney F. J. Modified Blalock-Taussig shunt. Use of subclavian artery orifice as flow regulator in prosthetic systemic-pulmonary artery shunts. J Thorac Cardiovasc Surg. 1981 Jan;81(1):112–119. [PubMed] [Google Scholar]


