Abstract
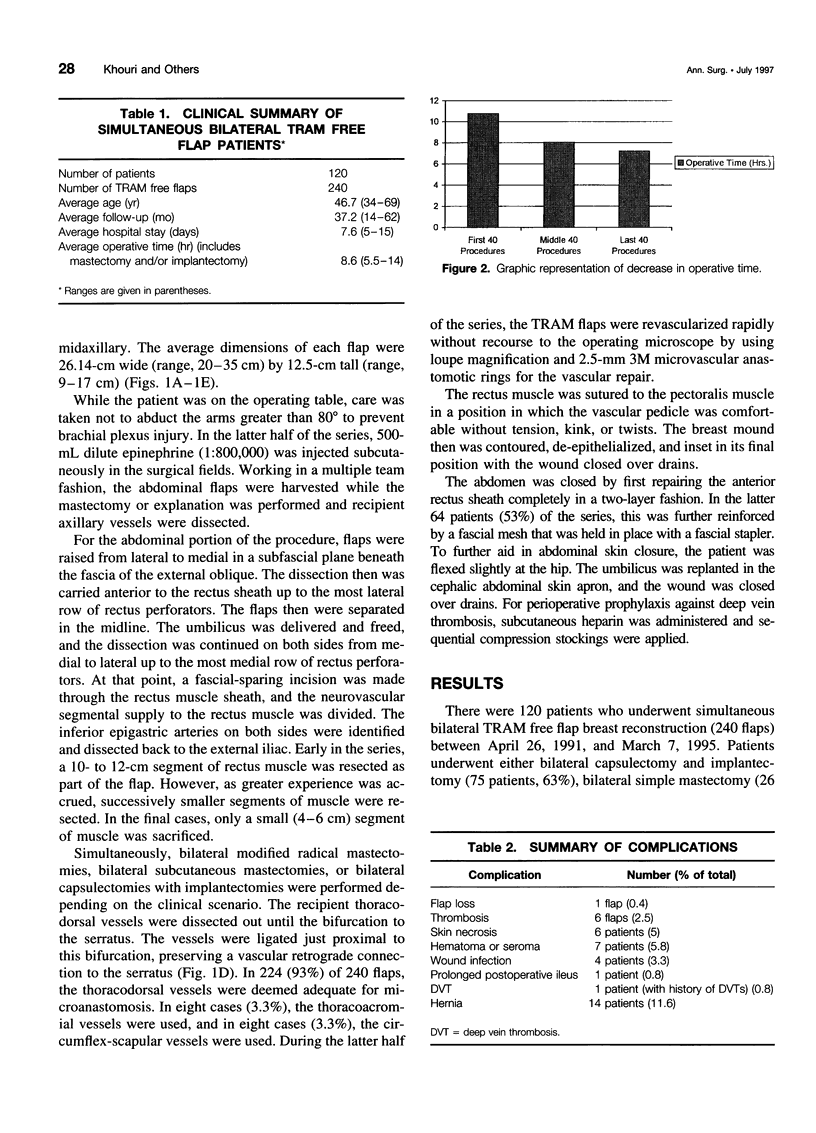
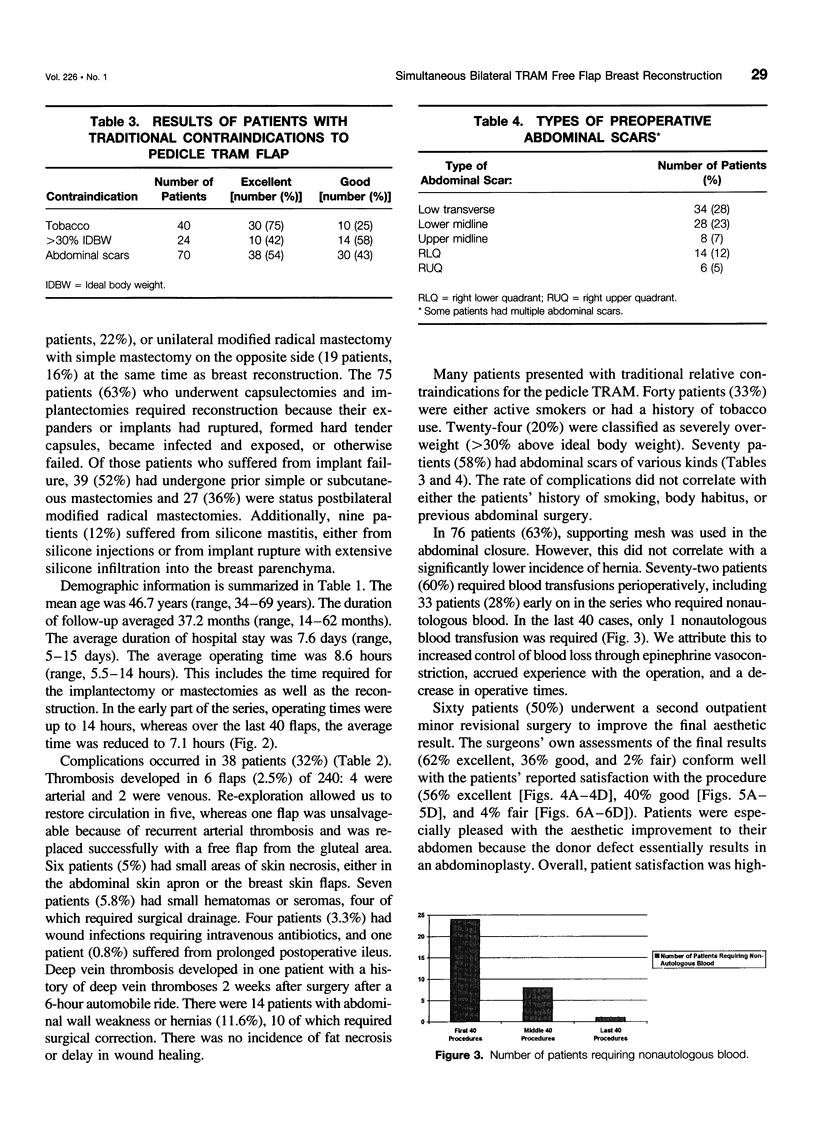
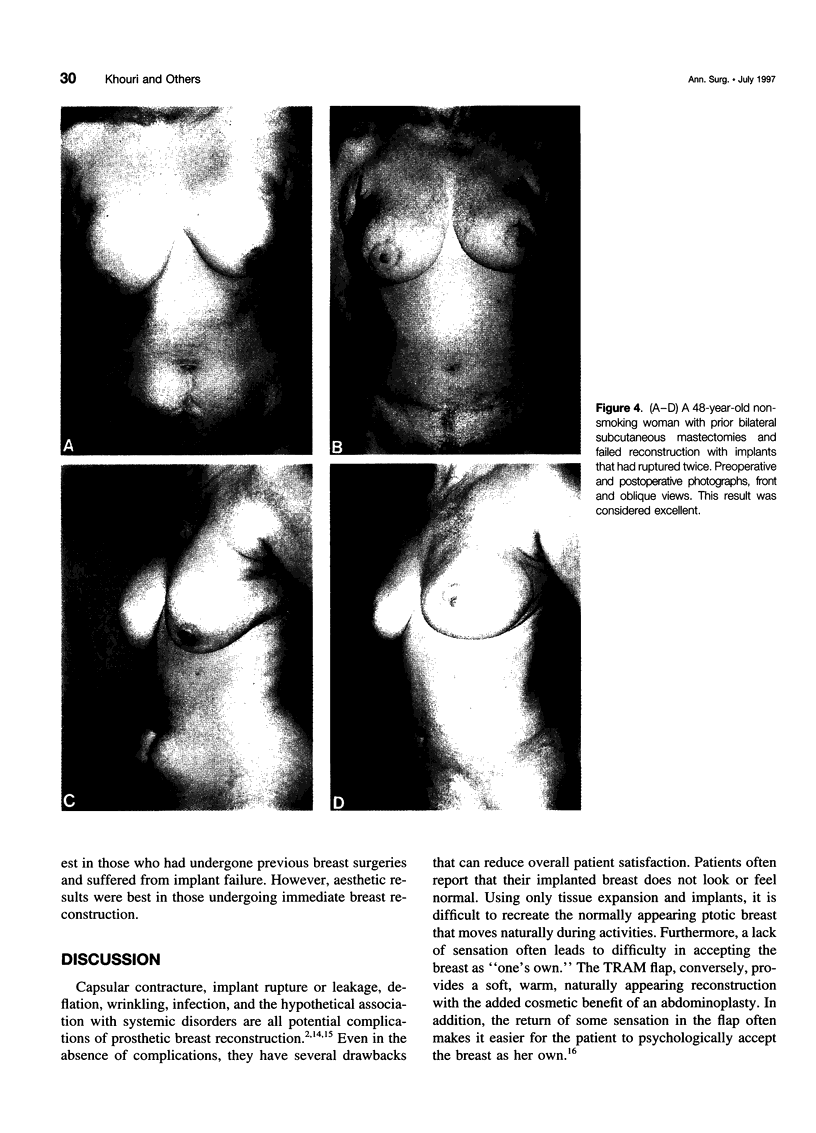
OBJECTIVE: The purpose of the study was to assess the results and morbidity associated with simultaneous bilateral TRAM free flap breast reconstruction and describe refinements in its surgical technique. SUMMARY BACKGROUND DATA: Bilateral prophylactic total mastectomies might be an agreeable option for those patients at highest risk for breast cancer if autogenous tissue breast reconstruction could be performed with reasonable technical ease and acceptable morbidity. However, some surgeons harbor reservations regarding the extensiveness of the surgery, the associated morbidity, and the aesthetic quality of the resulting outcome. METHODS: A multicenter retrospective review of clinical experience with 120 consecutive patients who underwent 240 simultaneous bilateral TRAM free flap breast reconstructions was developed. RESULTS: The average operating time, including the time required for the breast ablative portion of the procedures, was 8.6 hours. The average length of hospitalization was 7.6 days. However, for the last 40 patients, these figures were reduced to 7.1 hours and 6.1 days, respectively. Nonautologous blood transfusions were needed in 33 cases (28%), but only 1 was required in the last 40 patients. Thromboses developed in six of 240 flaps (2.5%): 4 were arterial and 2 were venous. Re-exploration allowed us to restore circulation in five flaps, whereas one flap was unsalvageable and was replaced successfully with an alternate flap. An uncomplicated deep vein thromboses developed in one patient with a history of recurrent deep vein thromboses that had no adverse effect on her outcome. Minor complications developed in 18 patients (15%) (e.g., hematoma, partial wound necrosis, wound infection, or prolonged postoperative ileus) that did not affect the long-term outcome. Fourteen patients (11.6%) had abdominal wall weakness or hernias. Follow-up time averaged 37.2 months (range, 14-62 months). On last follow-up, patients' self-reported overall satisfaction with the procedure was 56% excellent, 40% good, and 4% fair.CONCLUSIONS: Simultaneous bilateral free flap reconstruction is technically feasible with a high rate of success and an acceptable morbidity. When performed by experienced surgeons, bilateral prophylactic total mastectomies combined with simultaneous bilateral TRAM free flap reconstruction may provide an adequate surgical option with aesthetically acceptable results for patients at high risk for breast cancer.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnez Z. M., Bajec J., Bardsley A. F., Scamp T., Webster M. H. Experience with 50 free TRAM flap breast reconstructions. Plast Reconstr Surg. 1991 Mar;87(3):470–482. [PubMed] [Google Scholar]
- Benz C. C., Brandt B. H., Zänker K. S. Gene diagnostics provide new insights into breast cancer prognosis and therapy. Gene. 1995 Jun 14;159(1):3–7. doi: 10.1016/0378-1119(95)00147-x. [DOI] [PubMed] [Google Scholar]
- Bostwick J., 3rd, Jones G. Why I choose autogenous tissue in breast reconstruction. Clin Plast Surg. 1994 Apr;21(2):165–175. [PubMed] [Google Scholar]
- Bostwick J., 3rd Preventive mastectomy. Ann Surg Oncol. 1994 Nov;1(6):455–456. doi: 10.1007/BF02303608. [DOI] [PubMed] [Google Scholar]
- Boyd J. B., Taylor G. I., Corlett R. The vascular territories of the superior epigastric and the deep inferior epigastric systems. Plast Reconstr Surg. 1984 Jan;73(1):1–16. doi: 10.1097/00006534-198401000-00001. [DOI] [PubMed] [Google Scholar]
- Dickson M. G., Sharpe D. T. The complications of tissue expansion in breast reconstruction: a review of 75 cases. Br J Plast Surg. 1987 Nov;40(6):629–635. doi: 10.1016/0007-1226(87)90159-7. [DOI] [PubMed] [Google Scholar]
- Eldar S., Meguid M. M., Beatty J. D. Cancer of the breast after prophylactic subcutaneous mastectomy. Am J Surg. 1984 Nov;148(5):692–693. doi: 10.1016/0002-9610(84)90352-0. [DOI] [PubMed] [Google Scholar]
- Friedman R. J., Argenta L. C., Anderson R. Deep inferior epigastric free flap for breast reconstruction after radical mastectomy. Plast Reconstr Surg. 1985 Sep;76(3):455–460. doi: 10.1097/00006534-198509000-00025. [DOI] [PubMed] [Google Scholar]
- Gardner B. Prophylactic mastectomy: an unnecessary procedure. Ann Surg Oncol. 1994 Nov;1(6):453–454. doi: 10.1007/BF02303606. [DOI] [PubMed] [Google Scholar]
- Grotting J. C., Urist M. M., Maddox W. A., Vasconez L. O. Conventional TRAM flap versus free microsurgical TRAM flap for immediate breast reconstruction. Plast Reconstr Surg. 1989 May;83(5):828–844. doi: 10.1097/00006534-198905000-00009. [DOI] [PubMed] [Google Scholar]
- Hartrampf C. R., Scheflan M., Black P. W. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982 Feb;69(2):216–225. doi: 10.1097/00006534-198202000-00006. [DOI] [PubMed] [Google Scholar]
- Holleb A. I., Montgomery R., Farrow J. H. The hazard of incomplete simple mastectomy. Surg Gynecol Obstet. 1965 Oct;121(4):819–822. [PubMed] [Google Scholar]
- Holmström H. The free abdominoplasty flap and its use in breast reconstruction. An experimental study and clinical case report. Scand J Plast Reconstr Surg. 1979;13(3):423–427. doi: 10.3109/02844317909013092. [DOI] [PubMed] [Google Scholar]
- Jackson C. F., Palmquist M., Swanson J., Wong J., Miller S. H., Demuth R. J., Fletcher W. S. The effectiveness of prophylactic subcutaneous mastectomy in Sprague-Dawley rats induced with 7,12-dimethylbenzanthracene. Plast Reconstr Surg. 1984 Feb;73(2):249–260. doi: 10.1097/00006534-198402000-00017. [DOI] [PubMed] [Google Scholar]
- Jollis J. G., Peterson E. D., DeLong E. R., Mark D. B., Collins S. R., Muhlbaier L. H., Pryor D. B. The relation between the volume of coronary angioplasty procedures at hospitals treating Medicare beneficiaries and short-term mortality. N Engl J Med. 1994 Dec 15;331(24):1625–1629. doi: 10.1056/NEJM199412153312406. [DOI] [PubMed] [Google Scholar]
- Kinne D. W. Management of the contralateral breast. Ann Surg Oncol. 1994 Nov;1(6):454–455. doi: 10.1007/BF02303607. [DOI] [PubMed] [Google Scholar]
- Klamer T. W., Donegan W. L., Max M. H. Breast tumor incidence in rats after partial mammary resection. Arch Surg. 1983 Aug;118(8):933–935. doi: 10.1001/archsurg.1983.01390080041012. [DOI] [PubMed] [Google Scholar]
- Kroll S. S., Baldwin B. A comparison of outcomes using three different methods of breast reconstruction. Plast Reconstr Surg. 1992 Sep;90(3):455–462. doi: 10.1097/00006534-199209000-00015. [DOI] [PubMed] [Google Scholar]
- Lapatto O., Asko-Seljavaara S., Tukiainen E., Suominen E. Return of sensibility and final outcome of breast reconstructions using free transverse rectus abdominis musculocutaneous flaps. Scand J Plast Reconstr Surg Hand Surg. 1995 Mar;29(1):33–38. doi: 10.3109/02844319509048420. [DOI] [PubMed] [Google Scholar]
- Moon H. K., Taylor G. I. The vascular anatomy of rectus abdominis musculocutaneous flaps based on the deep superior epigastric system. Plast Reconstr Surg. 1988 Nov;82(5):815–832. doi: 10.1097/00006534-198811000-00014. [DOI] [PubMed] [Google Scholar]
- Radovan C. Tissue expansion in soft-tissue reconstruction. Plast Reconstr Surg. 1984 Oct;74(4):482–492. doi: 10.1097/00006534-198410000-00005. [DOI] [PubMed] [Google Scholar]
- Schrag D., Kuntz K. M., Garber J. E., Weeks J. C. Decision analysis--effects of prophylactic mastectomy and oophorectomy on life expectancy among women with BRCA1 or BRCA2 mutations. N Engl J Med. 1997 May 15;336(20):1465–1471. doi: 10.1056/NEJM199705153362022. [DOI] [PubMed] [Google Scholar]
- Schusterman M. A., Kroll S. S., Miller M. J., Reece G. P., Baldwin B. J., Robb G. L., Altmyer C. S., Ames F. C., Singletary S. E., Ross M. I. The free transverse rectus abdominis musculocutaneous flap for breast reconstruction: one center's experience with 211 consecutive cases. Ann Plast Surg. 1994 Mar;32(3):234–242. doi: 10.1097/00000637-199403000-00002. [DOI] [PubMed] [Google Scholar]
- Schusterman M. A., Kroll S. S., Weldon M. E. Immediate breast reconstruction: why the free TRAM over the conventional TRAM flap? Plast Reconstr Surg. 1992 Aug;90(2):255–262. [PubMed] [Google Scholar]
- Shaw W. W. Bilateral free flap breast reconstruction. Clin Plast Surg. 1994 Apr;21(2):297–308. [PubMed] [Google Scholar]
- Shenaq S. M., Klebuc M. J., Vargo D. Free-tissue transfer with the aid of loupe magnification: experience with 251 procedures. Plast Reconstr Surg. 1995 Feb;95(2):261–269. doi: 10.1097/00006534-199502000-00005. [DOI] [PubMed] [Google Scholar]
- Stefanek M. E. Bilateral prophylactic mastectomy: issues and concerns. J Natl Cancer Inst Monogr. 1995;(17):37–42. [PubMed] [Google Scholar]
- Temple W. J., Lindsay R. L., Magi E., Urbanski S. J. Technical considerations for prophylactic mastectomy in patients at high risk for breast cancer. Am J Surg. 1991 Apr;161(4):413–415. doi: 10.1016/0002-9610(91)91100-w. [DOI] [PubMed] [Google Scholar]
- Wells S. A., Jr, Chi D. D., Toshima K., Dehner L. P., Coffin C. M., Dowton S. B., Ivanovich J. L., DeBenedetti M. K., Dilley W. G., Moley J. F. Predictive DNA testing and prophylactic thyroidectomy in patients at risk for multiple endocrine neoplasia type 2A. Ann Surg. 1994 Sep;220(3):237–250. doi: 10.1097/00000658-199409000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins E. G., August D. A., Kuzon W. M., Jr, Chang A. E., Smith D. J. Immediate transverse rectus abdominis musculocutaneous flap reconstruction after mastectomy. J Am Coll Surg. 1995 Feb;180(2):177–183. [PubMed] [Google Scholar]
- Wong J. H., Jackson C. F., Swanson J. S., Palmquist M. A., Oyama A. A., Miller S. H., Fletcher W. S. Analysis of the risk reduction of prophylactic partial mastectomy in Sprague-Dawley rats with 7,12-dimethylbenzanthracene-induced breast cancer. Surgery. 1986 Jan;99(1):67–71. [PubMed] [Google Scholar]
- Wooster R., Bignell G., Lancaster J., Swift S., Seal S., Mangion J., Collins N., Gregory S., Gumbs C., Micklem G. Identification of the breast cancer susceptibility gene BRCA2. Nature. 1995 Dec 21;378(6559):789–792. doi: 10.1038/378789a0. [DOI] [PubMed] [Google Scholar]