Abstract
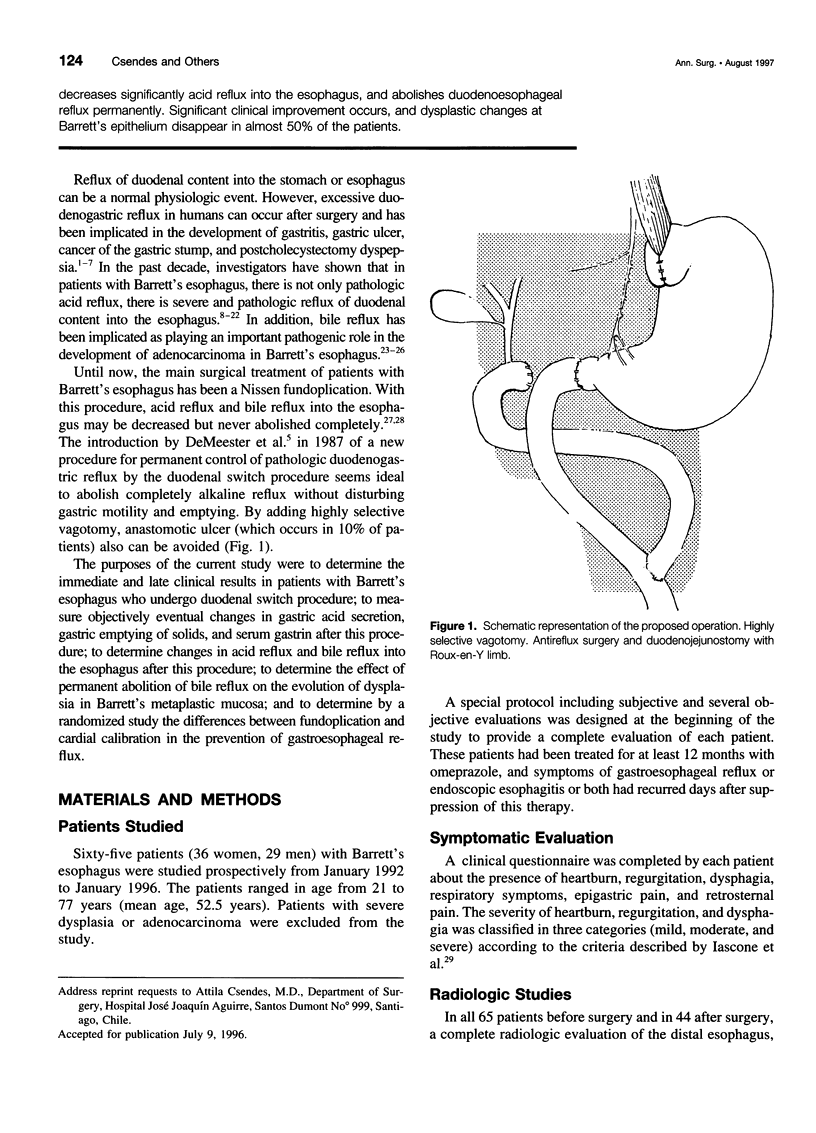
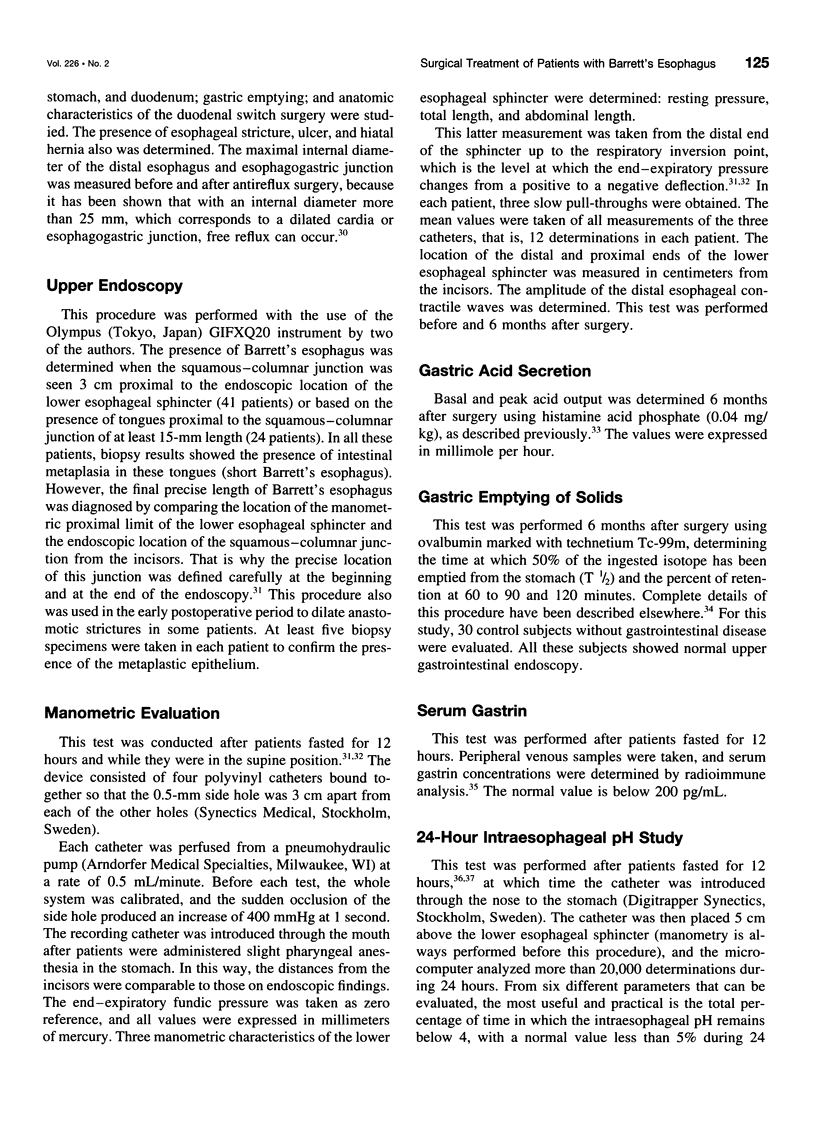
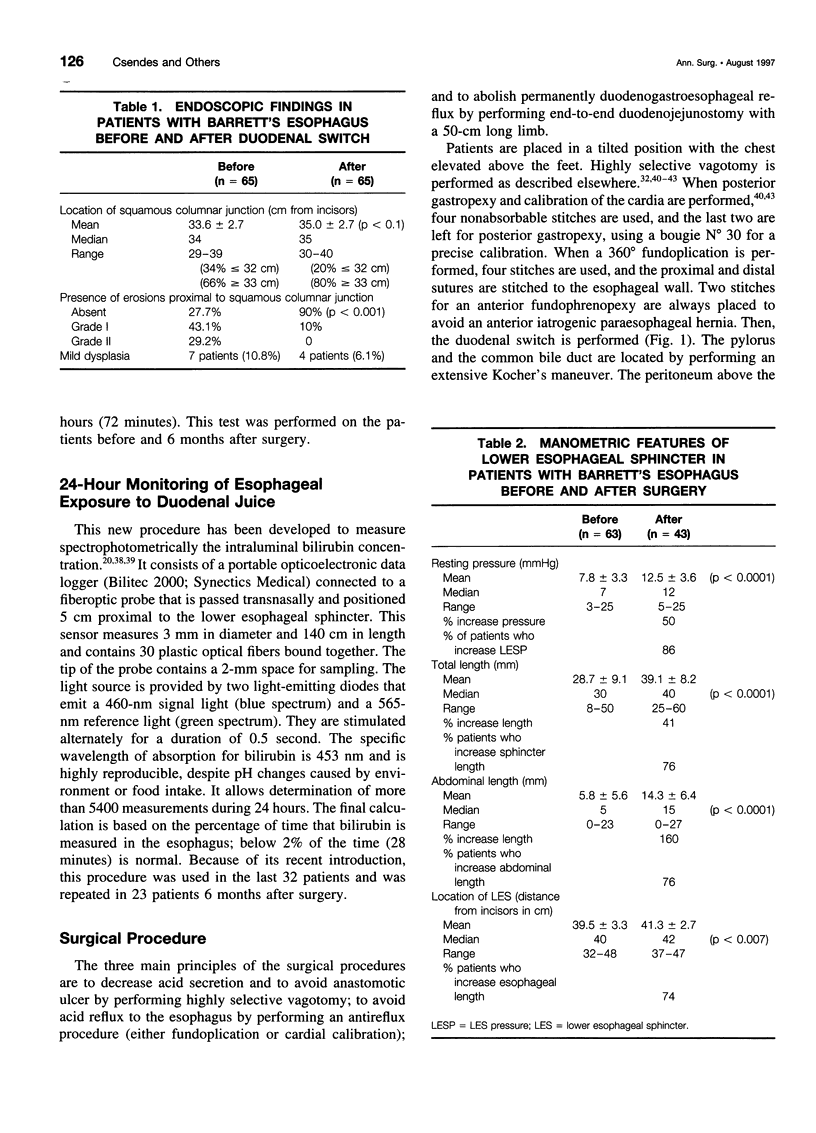
OBJECTIVE: To determine the results of a new surgical procedure for patients with Barrett's esophagus. SUMMARY BACKGROUND DATA: In addition to pathologic acid reflux into the esophagus in patients with severe gastroesophageal reflux and Barrett's esophagus, increased duodenoesophegeal reflux has been implicated. The purpose of this study was to establish the effect of a new bile diversion procedure in these patients. METHODS: Sixty-five patients with Barrett's esophagus were included in this study. A complete clinical, radiologic, endoscopic, and bioptic evaluation was performed before and after surgery. Besides esophageal manometry, 24-hour pH studies and a Bilitec test were performed. After surgery, gastric emptying of solids, gastric acid secretion, and serum gastrin were determined. All patients underwent highly selective vagotomy, antireflux procedure (posterior gastropexy with cardial calibration or fundoplication), and duodenal switch procedure, with a Roux-en-Y anastomosis 60 cm in length. RESULTS: No deaths occurred. Morbidity occurred in 14% of the patients. A significant improvement in symptoms, endoscopic findings, and radiologic evaluation was achieved. Lower esophageal sphincter pressure increased significantly (p < 0.0001), as did abdominal length and total length of the sphincter (p < 0.0001). The presence of an incompetent sphincter decreased from 87.3% to 20.9% (p < 0.0001). Three of seven patients with dysplasia showed disappearance of this dysplasia. Serum gastrin and gastric emptying of solids after surgery remained normal. Basal and peak acid output values were low. Twenty-four hour pH studies showed a mean value of 24.8% before surgery, which decreased to 4.8% after surgery (p < 0.0001). The determination of the percentage time with bilirubin in the esophagus was 23% before surgery; this decreased to 0.7% after surgery (p < 0.0001). Late results showed Visick I and II gradation in 90% of the patients and grade III and IV in 10% of the patients. CONCLUSIONS: This physiologic approach to the surgical treatment of patients with Barrett's esophagus produces a permanent decrease of acid secretion (and avoids anastomotic ulcer), decreases significantly acid reflux into the esophagus, and abolishes duodenoesophageal reflux permanently. Significant clinical improvement occurs, and dysplastic changes at Barrett's epithelium disappear in almost 50% of the patients.
Full text
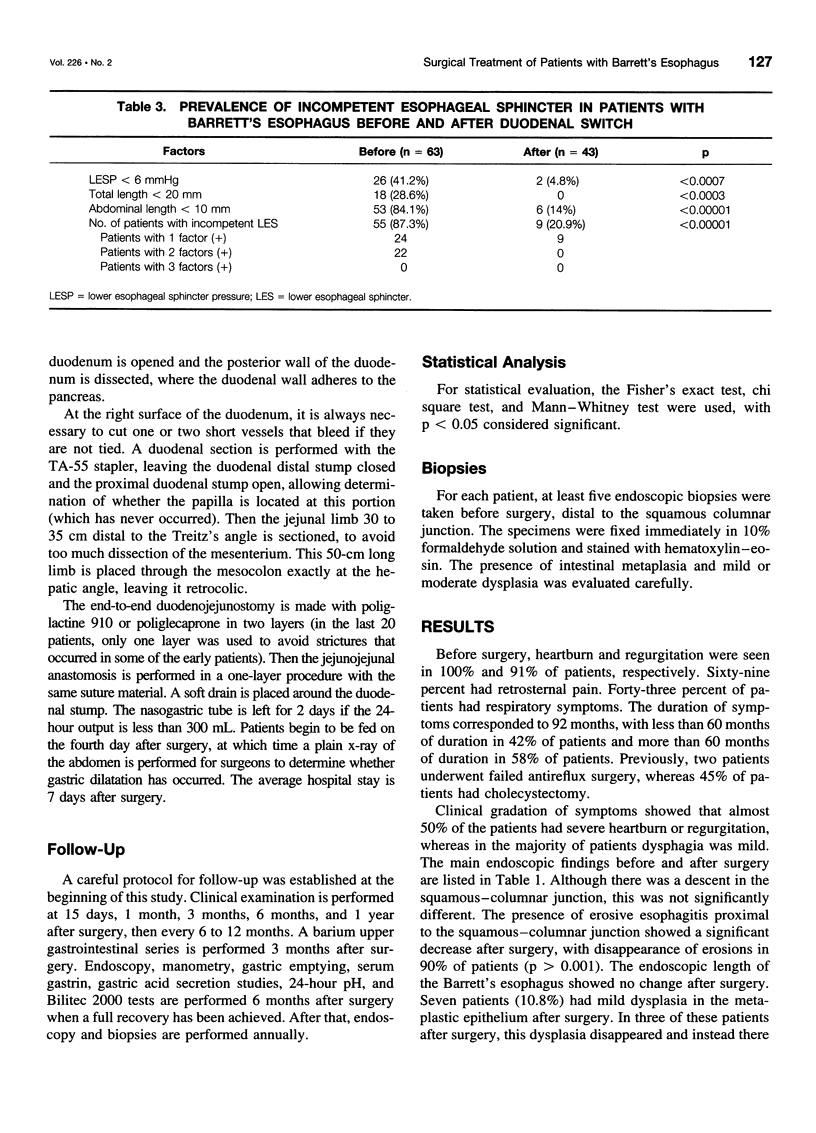
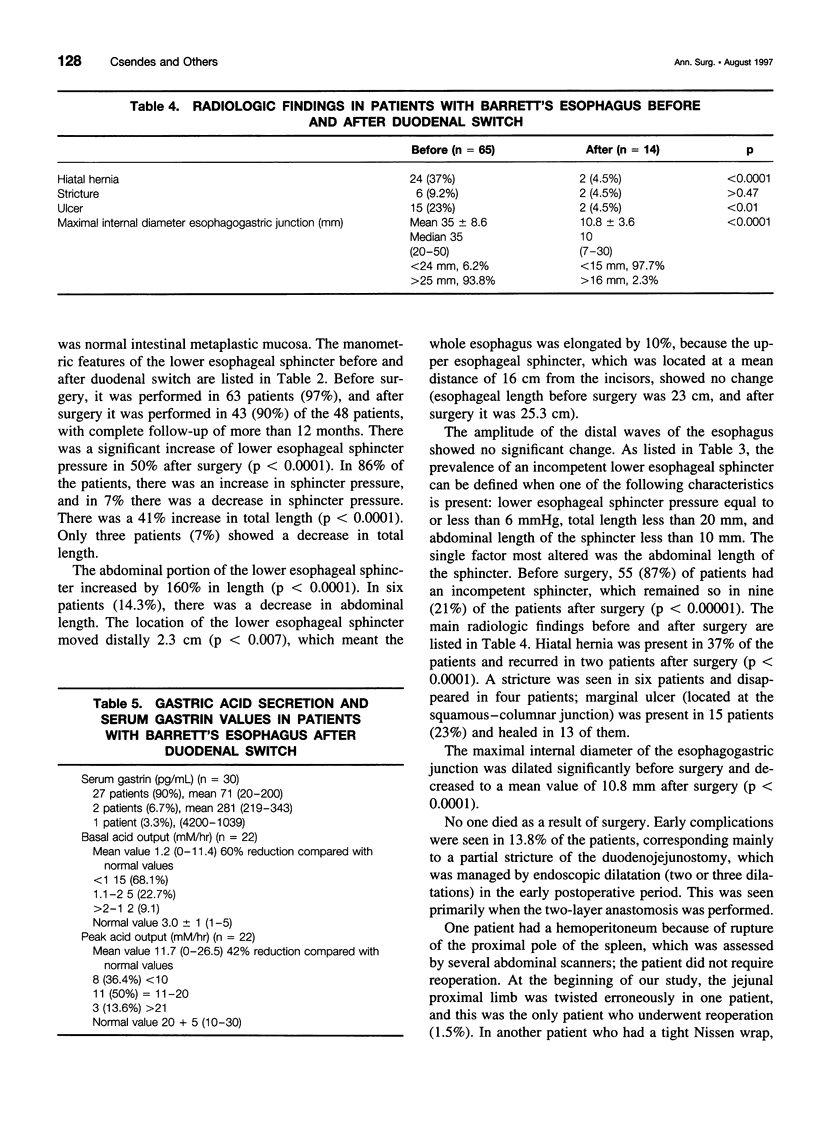
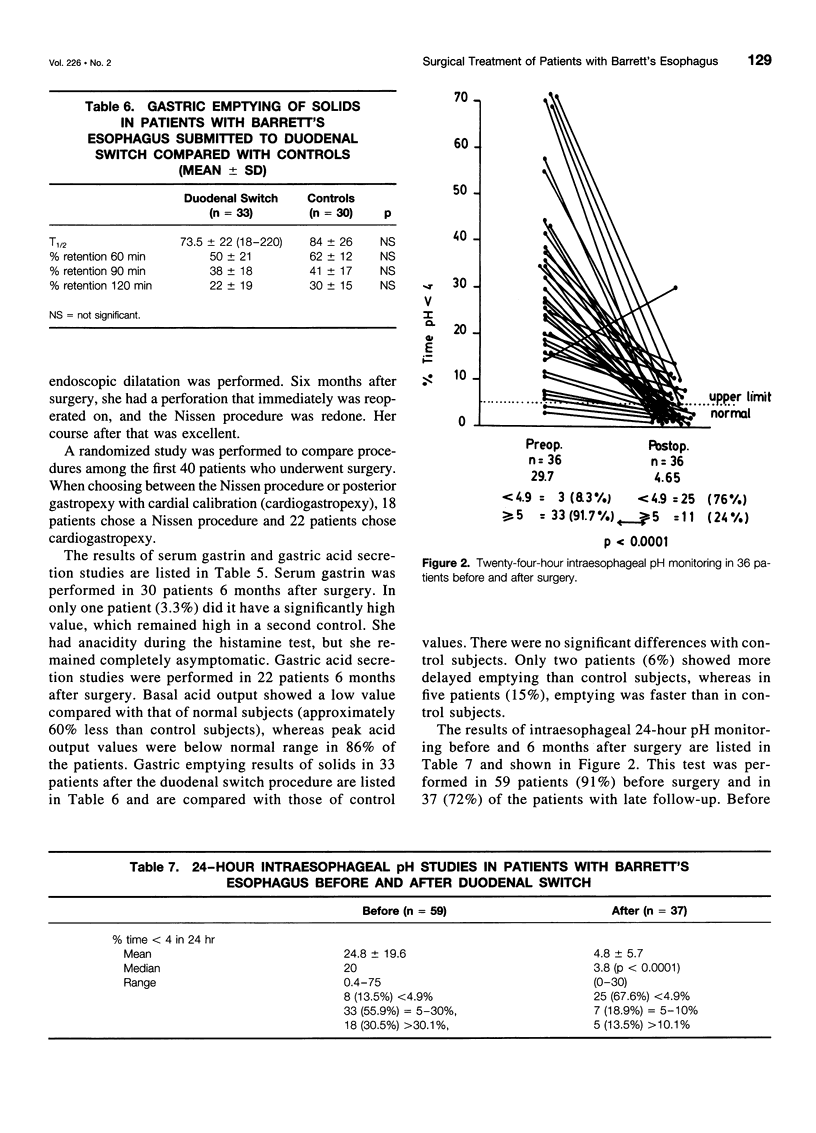
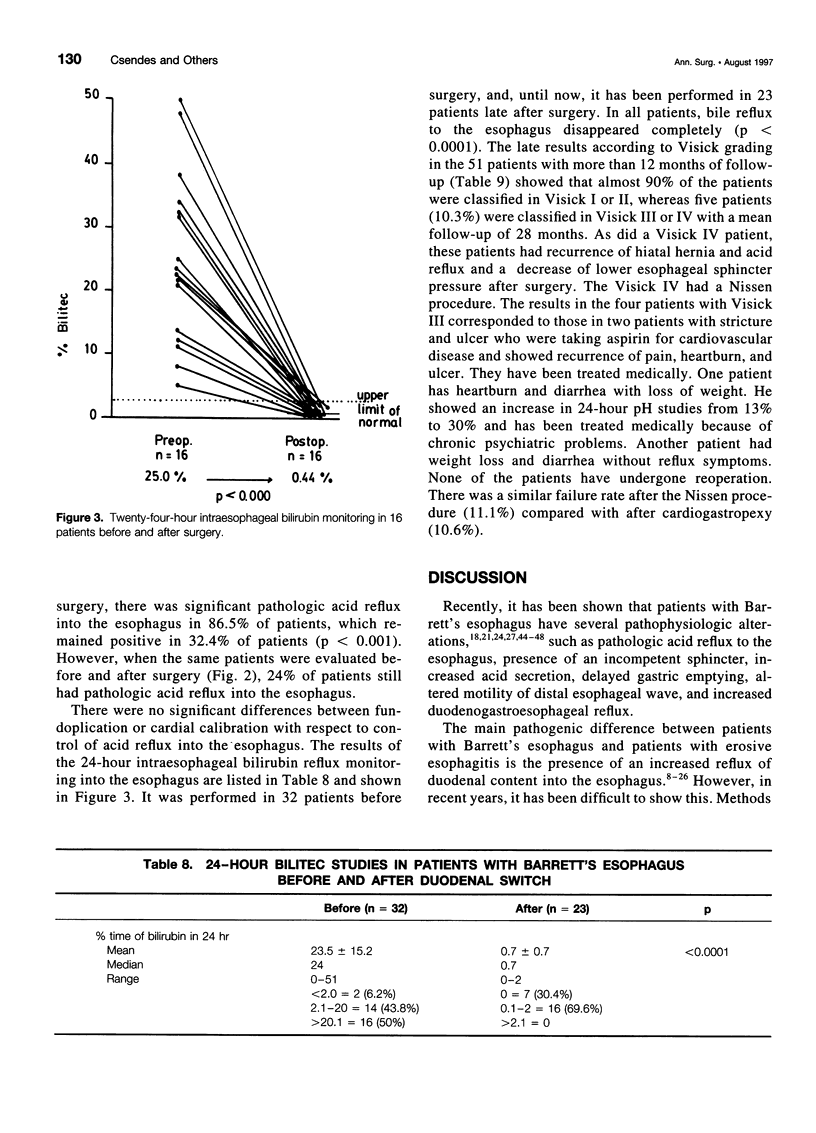
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Attwood S. E., Ball C. S., Barlow A. P., Jenkinson L., Norris T. L., Watson A. Role of intragastric and intraoesophageal alkalinisation in the genesis of complications in Barrett's columnar lined lower oesophagus. Gut. 1993 Jan;34(1):11–15. doi: 10.1136/gut.34.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attwood S. E., DeMeester T. R., Bremner C. G., Barlow A. P., Hinder R. A. Alkaline gastroesophageal reflux: implications in the development of complications in Barrett's columnar-lined lower esophagus. Surgery. 1989 Oct;106(4):764–770. [PubMed] [Google Scholar]
- Attwood S. E., Smyrk T. C., DeMeester T. R., Mirvish S. S., Stein H. J., Hinder R. A. Duodenoesophageal reflux and the development of esophageal adenocarcinoma in rats. Surgery. 1992 May;111(5):503–510. [PubMed] [Google Scholar]
- Bechi P., Pucciani F., Baldini F., Cosi F., Falciai R., Mazzanti R., Castagnoli A., Passeri A., Boscherini S. Long-term ambulatory enterogastric reflux monitoring. Validation of a new fiberoptic technique. Dig Dis Sci. 1993 Jul;38(7):1297–1306. doi: 10.1007/BF01296082. [DOI] [PubMed] [Google Scholar]
- Brand D. L., Ylvisaker J. T., Gelfand M., Pope C. E., 2nd Regression of columnar esophageal (Barrett's) epithelium after anti-reflux surgery. N Engl J Med. 1980 Apr 10;302(15):844–848. doi: 10.1056/NEJM198004103021506. [DOI] [PubMed] [Google Scholar]
- Bremner C. G., Mason R. J. 'Bile' in the oesophagus. Br J Surg. 1993 Nov;80(11):1374–1376. doi: 10.1002/bjs.1800801105. [DOI] [PubMed] [Google Scholar]
- Caldwell M. T., Byrne P. J., Brazil N., Crowley V., Attwood S. E., Walsh T. N., Hennessy T. P. An ambulatory bile reflux monitoring system: an in vitro appraisal. Physiol Meas. 1994 Feb;15(1):57–65. doi: 10.1088/0967-3334/15/1/005. [DOI] [PubMed] [Google Scholar]
- Cameron A. J., Ott B. J., Payne W. S. The incidence of adenocarcinoma in columnar-lined (Barrett's) esophagus. N Engl J Med. 1985 Oct 3;313(14):857–859. doi: 10.1056/NEJM198510033131404. [DOI] [PubMed] [Google Scholar]
- Champion G., Richter J. E., Vaezi M. F., Singh S., Alexander R. Duodenogastroesophageal reflux: relationship to pH and importance in Barrett's esophagus. Gastroenterology. 1994 Sep;107(3):747–754. doi: 10.1016/0016-5085(94)90123-6. [DOI] [PubMed] [Google Scholar]
- Csendes A., Alvarez F., Burdiles P., Braghetto I., Henríquez A., Quesada S., Csendes P. Magnitud del reflujo gastroesofágico ácido cuantificado por medición de pH de 24 horas segun el grado de esofagitis endoscópica. Rev Med Chil. 1994 Jan;122(1):59–67. [PubMed] [Google Scholar]
- Csendes A., Braghetto I., Korn O., Cortés C. Late subjective and objective evaluations of antireflux surgery in patients with reflux esophagitis: analysis of 215 patients. Surgery. 1989 Mar;105(3):374–382. [PubMed] [Google Scholar]
- Csendes A., Larrain A., Uribe P. Gastric acid secretion in patients with a symptomatic gastroesophageal reflux and patients with esophageal strictures. Ann Surg. 1974 Jan;179(1):119–122. doi: 10.1097/00000658-197401000-00023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csendes A., Maluenda F., Braghetto I., Csendes P., Henriquez A., Quesada M. S. Location of the lower oesophageal sphincter and the squamous columnar mucosal junction in 109 healthy controls and 778 patients with different degrees of endoscopic oesophagitis. Gut. 1993 Jan;34(1):21–27. doi: 10.1136/gut.34.1.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csendes A., Oster M., Brandsborg O., Möller J., Brandsborg M., Amdrup E. Gastroesophageal sphincter pressure and serum gastrin studies following food intake before and after vagotomy for duodenal ulcer. Scand J Gastroenterol. 1978;13(4):437–441. doi: 10.3109/00365527809181918. [DOI] [PubMed] [Google Scholar]
- DUPLESSIS D. J. PATHOGENESIS OF GASTRIC ULCERATION. Lancet. 1965 May 8;1(7393):974–978. doi: 10.1016/s0140-6736(65)91214-6. [DOI] [PubMed] [Google Scholar]
- DeMeester T. R., Attwood S. E., Smyrk T. C., Therkildsen D. H., Hinder R. A. Surgical therapy in Barrett's esophagus. Ann Surg. 1990 Oct;212(4):528–542. doi: 10.1097/00000658-199010000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester T. R., Bonavina L., Albertucci M. Nissen fundoplication for gastroesophageal reflux disease. Evaluation of primary repair in 100 consecutive patients. Ann Surg. 1986 Jul;204(1):9–20. doi: 10.1097/00000658-198607000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester T. R., Fuchs K. H., Ball C. S., Albertucci M., Smyrk T. C., Marcus J. N. Experimental and clinical results with proximal end-to-end duodenojejunostomy for pathologic duodenogastric reflux. Ann Surg. 1987 Oct;206(4):414–426. doi: 10.1097/00000658-198710000-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeMeester T. R., Wang C. I., Wernly J. A., Pellegrini C. A., Little A. G., Klementschitsch P., Bermudez G., Johnson L. F., Skinner D. B. Technique, indications, and clinical use of 24 hour esophageal pH monitoring. J Thorac Cardiovasc Surg. 1980 May;79(5):656–670. [PubMed] [Google Scholar]
- Gillen P., Keeling P., Byrne P. J., Healy M., O'Moore R. R., Hennessy T. P. Implication of duodenogastric reflux in the pathogenesis of Barrett's oesophagus. Br J Surg. 1988 Jun;75(6):540–543. doi: 10.1002/bjs.1800750612. [DOI] [PubMed] [Google Scholar]
- Gillen P., Keeling P., Byrne P. J., Hennessy T. P. Barrett's oesophagus: pH profile. Br J Surg. 1987 Sep;74(9):774–776. doi: 10.1002/bjs.1800740906. [DOI] [PubMed] [Google Scholar]
- Gillen P., Keeling P., Byrne P. J., West A. B., Hennessy T. P. Experimental columnar metaplasia in the canine oesophagus. Br J Surg. 1988 Feb;75(2):113–115. doi: 10.1002/bjs.1800750208. [DOI] [PubMed] [Google Scholar]
- Gotley D. C., Morgan A. P., Ball D., Owen R. W., Cooper M. J. Composition of gastro-oesophageal refluxate. Gut. 1991 Oct;32(10):1093–1099. doi: 10.1136/gut.32.10.1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gotley D. C., Morgan A. P., Cooper M. J. Bile acid concentrations in the refluxate of patients with reflux oesophagitis. Br J Surg. 1988 Jun;75(6):587–590. doi: 10.1002/bjs.1800750632. [DOI] [PubMed] [Google Scholar]
- Graziani L., De Nigris E., Pesaresi A., Baldelli S., Dini L., Montesi A. Reflux esophagitis: radiologic-endoscopic correlation in 39 symptomatic cases. Gastrointest Radiol. 1983;8(1):1–6. doi: 10.1007/BF01948078. [DOI] [PubMed] [Google Scholar]
- Haggitt R. C., Tryzelaar J., Ellis F. H., Colcher H. Adenocarcinoma complicating columnar epithelium-lined (Barrett's) esophagus. Am J Clin Pathol. 1978 Jul;70(1):1–5. doi: 10.1093/ajcp/70.1.1. [DOI] [PubMed] [Google Scholar]
- Iascone C., DeMeester T. R., Little A. G., Skinner D. B. Barrett's esophagus. Functional assessment, proposed pathogenesis, and surgical therapy. Arch Surg. 1983 May;118(5):543–549. doi: 10.1001/archsurg.1983.01390050027005. [DOI] [PubMed] [Google Scholar]
- Jazrawi S., Walsh T. N., Byrne P. J., Hill A. D., Li H., Lawlor P., Hennessy T. P. Cholecystectomy and oesophageal reflux: a prospective evaluation. Br J Surg. 1993 Jan;80(1):50–53. doi: 10.1002/bjs.1800800119. [DOI] [PubMed] [Google Scholar]
- Johansson J., Johnsson F., Joelsson B., Florén C. H., Walther B. Outcome 5 years after 360 degree fundoplication for gastro-oesophageal reflux disease. Br J Surg. 1993 Jan;80(1):46–49. doi: 10.1002/bjs.1800800118. [DOI] [PubMed] [Google Scholar]
- Kauer W. K., Burdiles P., Ireland A. P., Clark G. W., Peters J. H., Bremner C. G., DeMeester T. R. Does duodenal juice reflux into the esophagus of patients with complicated GERD? Evaluation of a fiberoptic sensor for bilirubin. Am J Surg. 1995 Jan;169(1):98–104. doi: 10.1016/s0002-9610(99)80116-0. [DOI] [PubMed] [Google Scholar]
- Lillemoe K. D., Johnson L. F., Harmon J. W. Alkaline esophagitis: a comparison of the ability of components of gastroduodenal contents to injure the rabbit esophagus. Gastroenterology. 1983 Sep;85(3):621–628. [PubMed] [Google Scholar]
- Lorusso D., Misciagna G., Mangini V., Messa C., Cavallini A., Caruso M. L., Giorgio P., Guerra V. Duodenogastric reflux of bile acids, gastrin and parietal cells, and gastric acid secretion before and 6 months after cholecystectomy. Am J Surg. 1990 Jun;159(6):575–578. doi: 10.1016/s0002-9610(06)80069-3. [DOI] [PubMed] [Google Scholar]
- Mason R. J., Bremner C. C. Gastric emptying and acid-output patterns following a suprapapillary duodenojejunostomy reconstruction with differing lengths of the afferent limb in the baboon. Am J Surg. 1994 Mar;167(3):322–326. doi: 10.1016/0002-9610(94)90209-7. [DOI] [PubMed] [Google Scholar]
- Mittal R. K., Reuben A., Whitney J. O., McCallum R. W. Do bile acids reflux into the esophagus? A study in normal subjects and patients with gastroesophageal reflux disease. Gastroenterology. 1987 Feb;92(2):371–375. doi: 10.1016/0016-5085(87)90130-2. [DOI] [PubMed] [Google Scholar]
- Moffat R. C., Berkas E. M. Bile esophagitis. Arch Surg. 1965 Dec;91(6):963–966. doi: 10.1001/archsurg.1965.01320180097021. [DOI] [PubMed] [Google Scholar]
- Oster M. J., Csendes A., Funch-Jensen P., Casalnuovo C. A., Sørensen F. H., Amdrup E. PCV and modified hill procedure as surgical treatment of reflux esophagitis: results in 108 patients. World J Surg. 1982 Jul;6(4):412–417. doi: 10.1007/BF01657669. [DOI] [PubMed] [Google Scholar]
- Ritchie W. P., Jr Alkaline reflux gastritis. Late results on a controlled trial of diagnosis and treatment. Ann Surg. 1986 May;203(5):537–544. doi: 10.1097/00000658-198605000-00014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seto Y., Kobori O. Role of reflux oesophagitis and acid in the development of columnar epithelium in the rat oesophagus. Br J Surg. 1993 Apr;80(4):467–470. doi: 10.1002/bjs.1800800420. [DOI] [PubMed] [Google Scholar]
- Starnes V. A., Adkins R. B., Ballinger J. F., Sawyers J. L. Barrett's esophagus. A surgical entity. Arch Surg. 1984 May;119(5):563–567. doi: 10.1001/archsurg.1984.01390170059012. [DOI] [PubMed] [Google Scholar]
- Stein H. J., Hoeft S., DeMeester T. R. Functional foregut abnormalities in Barrett's esophagus. J Thorac Cardiovasc Surg. 1993 Jan;105(1):107–111. [PubMed] [Google Scholar]
- Waring J. P., Legrand J., Chinichian A., Sanowski R. A. Duodenogastric reflux in patients with Barrett's esophagus. Dig Dis Sci. 1990 Jun;35(6):759–762. doi: 10.1007/BF01540180. [DOI] [PubMed] [Google Scholar]
- Warshaw A. L. Bile gastritis without prior gastric surgery: contributing role of cholecystectomy. Am J Surg. 1979 Apr;137(4):527–531. doi: 10.1016/0002-9610(79)90125-9. [DOI] [PubMed] [Google Scholar]
- Welch N. T., Yasui A., Kim C. B., Barlow A. P., Hinder R. A., DeMeester T. R., Polishuk P. V., Clark G. W., Adrian T. E. Effect of duodenal switch procedure on gastric acid production, intragastric pH, gastric emptying, and gastrointestinal hormones. Am J Surg. 1992 Jan;163(1):37–45. doi: 10.1016/0002-9610(92)90250-u. [DOI] [PubMed] [Google Scholar]



