Abstract
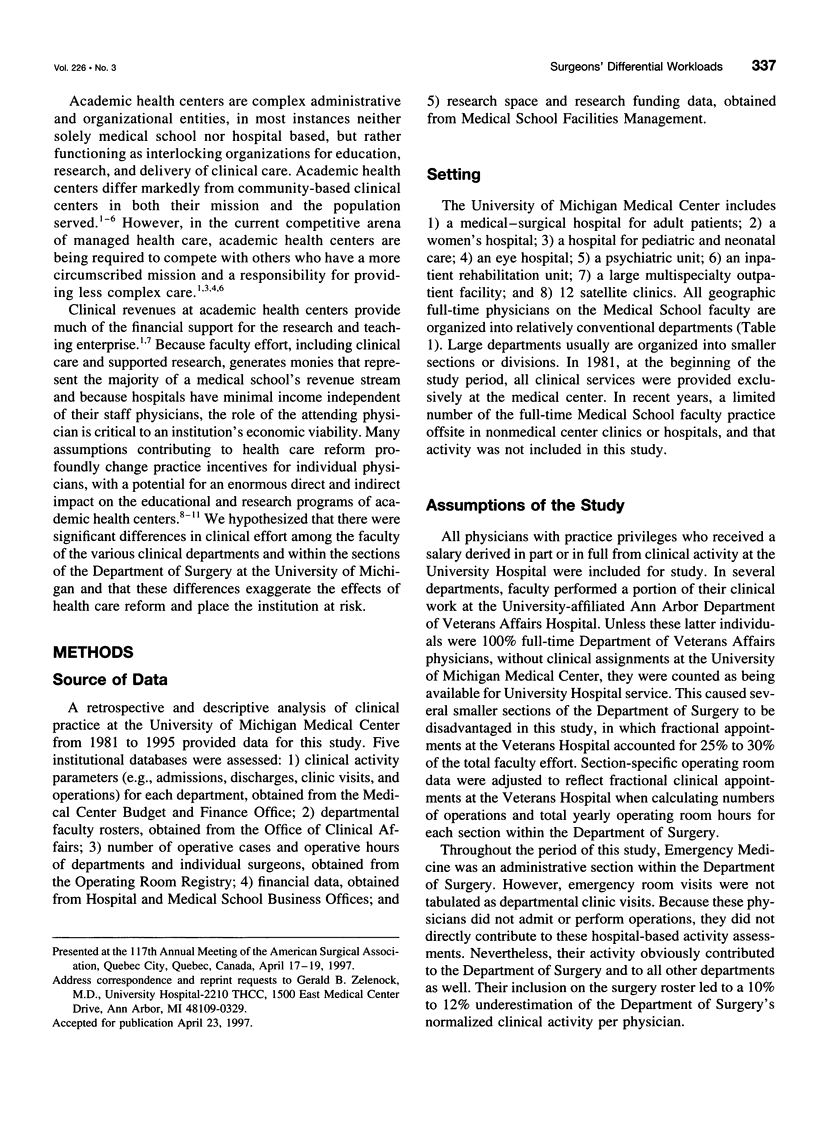
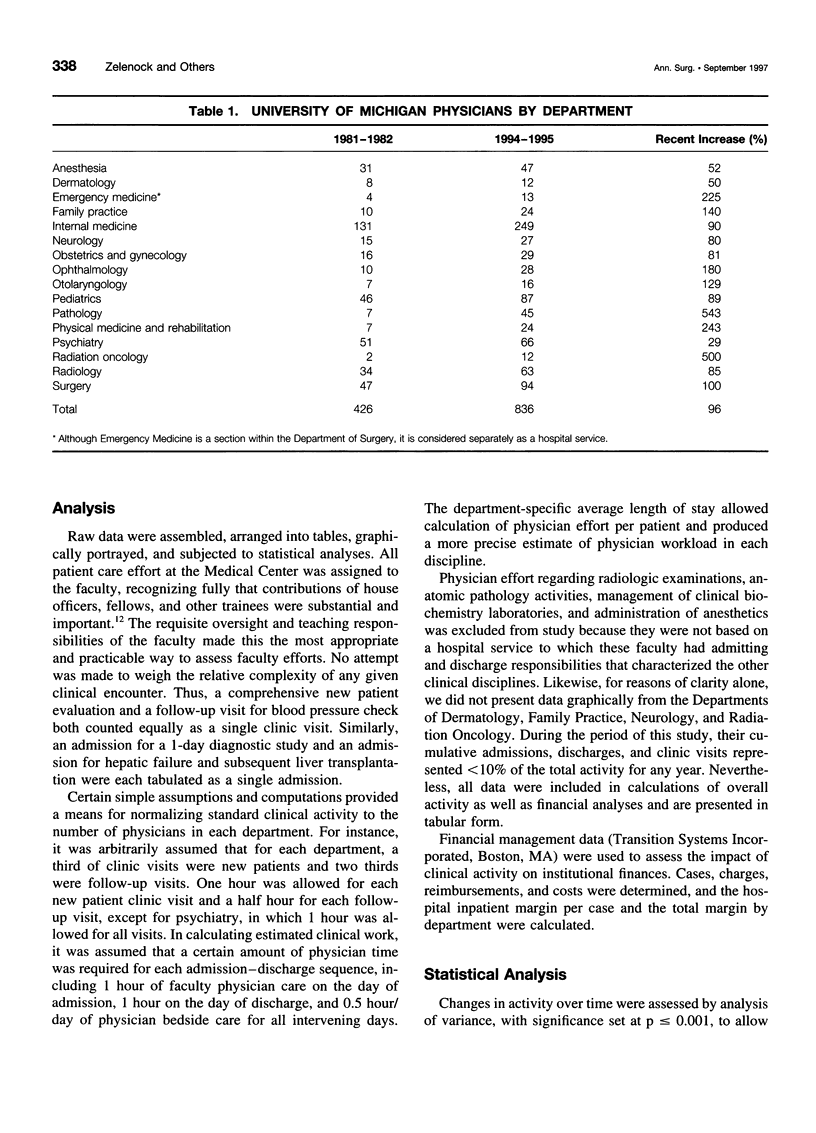
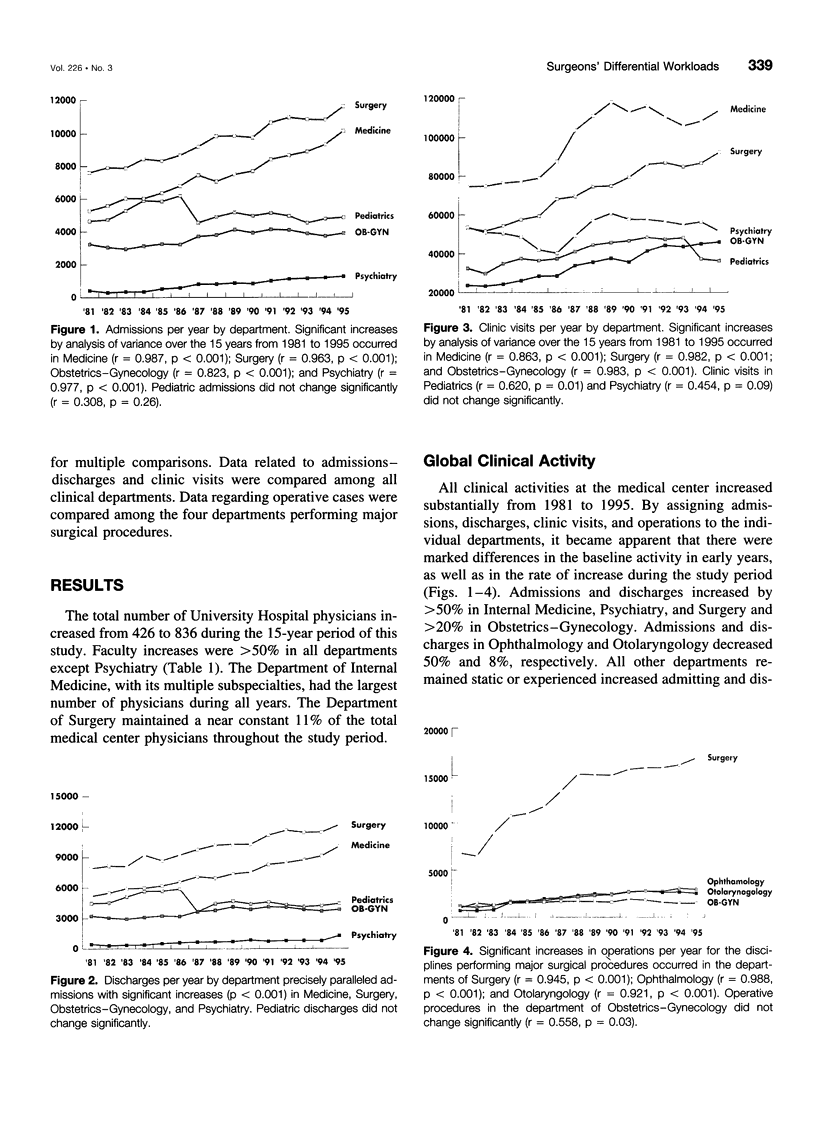
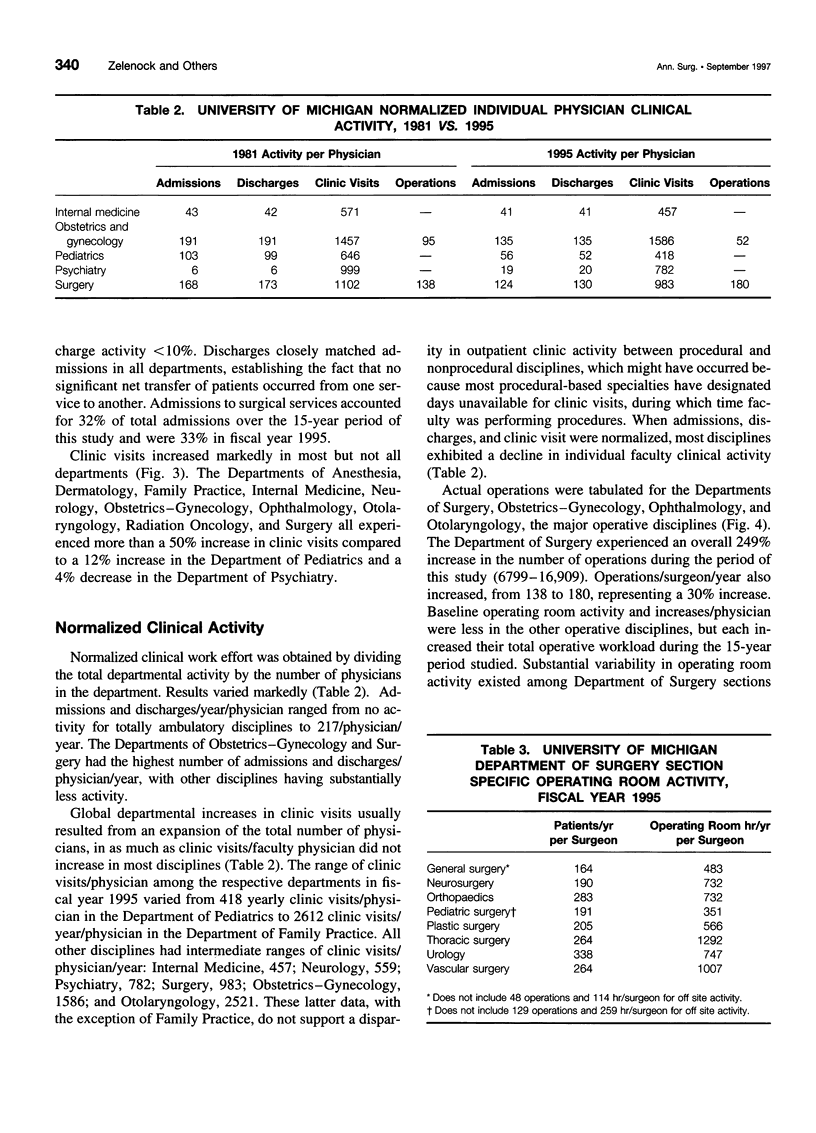
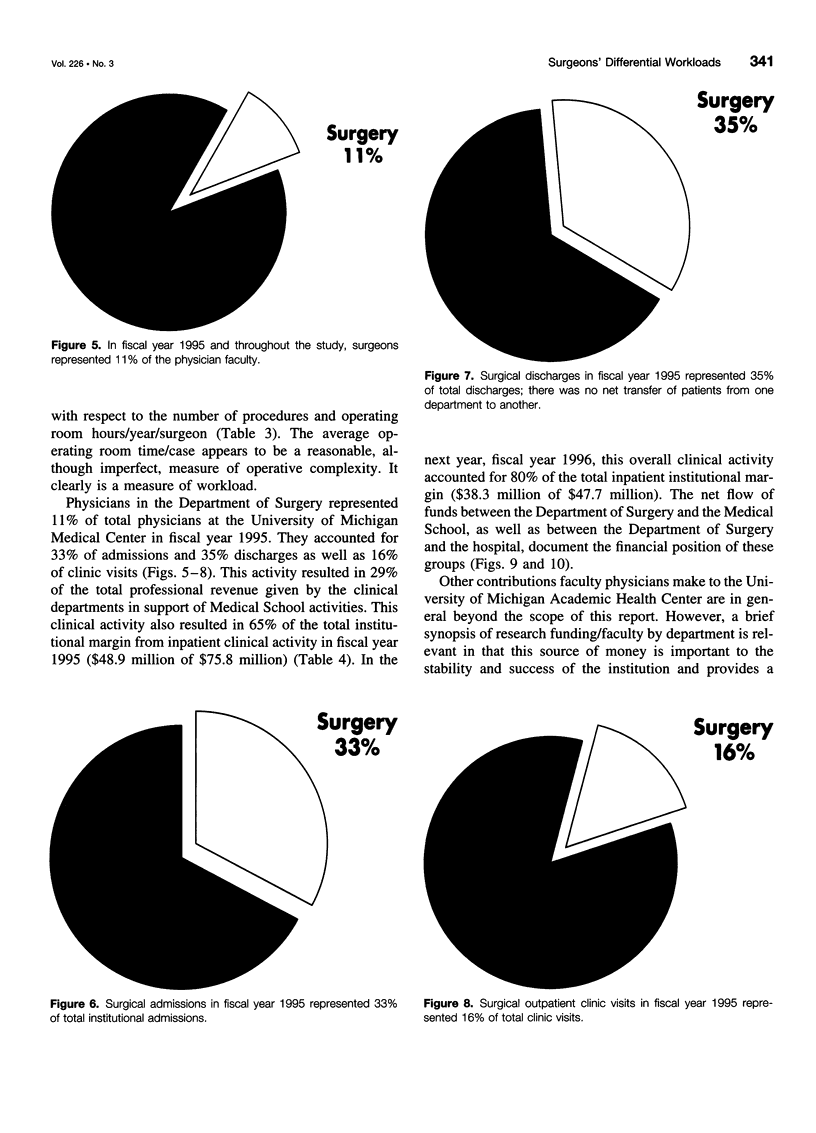
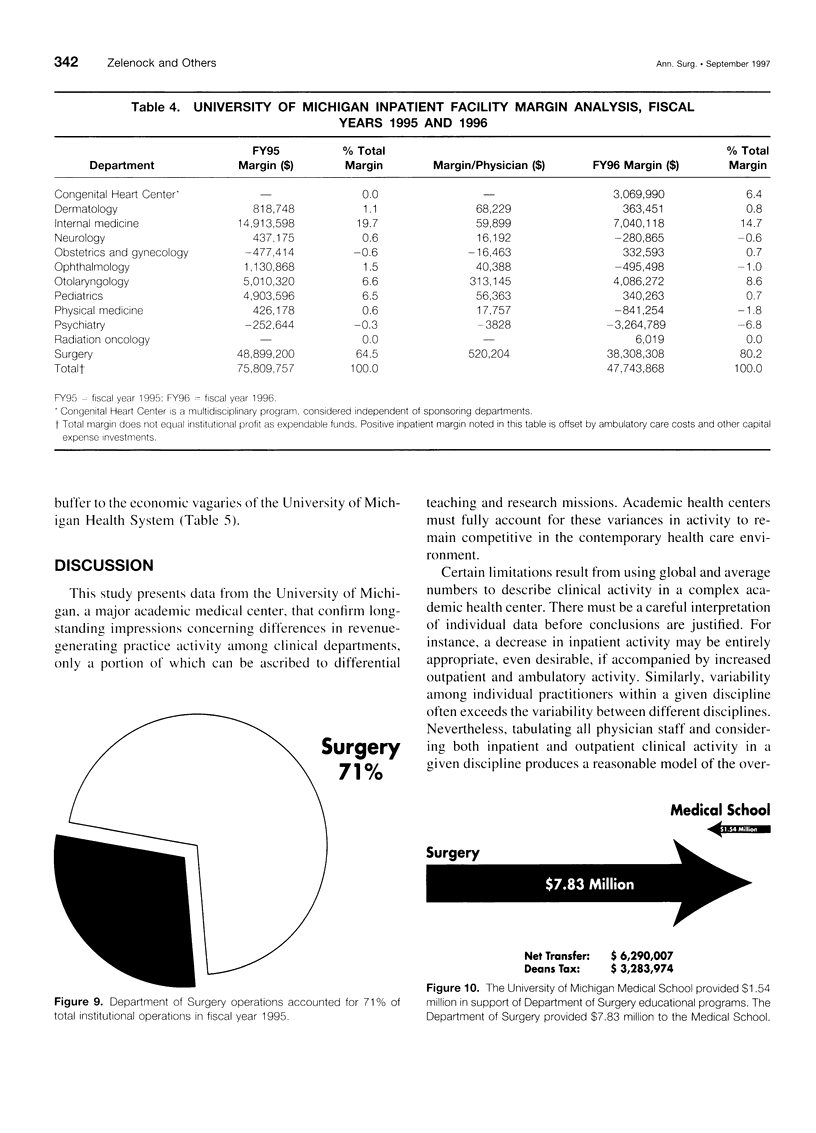
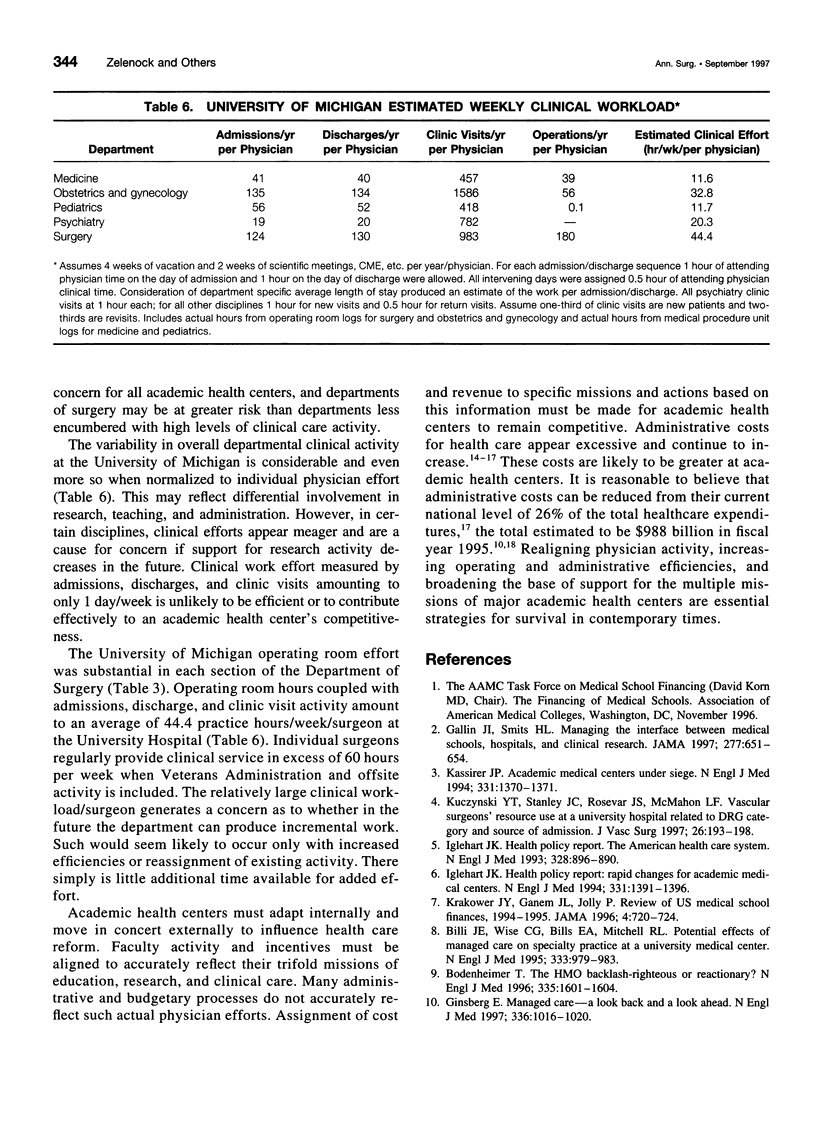
OBJECTIVE: The authors analyzed patient care (1981-1995) and financial data (1991-1996) to determine if differential workloads existed at a major academic health center. SUMMARY BACKGROUND DATA: Academic health centers differ markedly from community-based medical centers, but they are required to compete with others who have a more circumscribed mission and a responsibility for providing less complex care. Changes in health care systems may lessen incentives to generate clinical revenue and may adversely affect educational and research programs. METHODS: Patient care data at the University of Michigan Health System were analyzed by discipline for level of activity from 1981 to 1995 and were compared to professional and institutional financial data from 1991 to 1995. RESULTS: Surgeons represented 11% of the total full-time physicians throughout the period of the study (94 of the 836 Medical Center physicians, 1995). They accounted for 33% of hospital admissions (11,616 of 35,101) and 16% of outpatient visits (92,364 of 568,738). Since 1981, surgeons experienced a 249% increase in total operative workload (6799-16,909 procedures), representing a 30% increase in operations/surgeon (138-180 operations). Surgical efforts in 1995 accounted for 29% of the total professional fee revenue and $240 million of the $512-million University of Michigan Hospital revenue. CONCLUSIONS: Surgeons had a greater collective and individual responsibility than did nonsurgeons for clinical activity and the financial viability of the academic health centers studied. Many proposals for financing health care delivery systems have the potential to exacerbate this differential. Restructuring of academic health centers must address this fact, lest their academic mission and scholarly activity be compromised.
Full text
PDF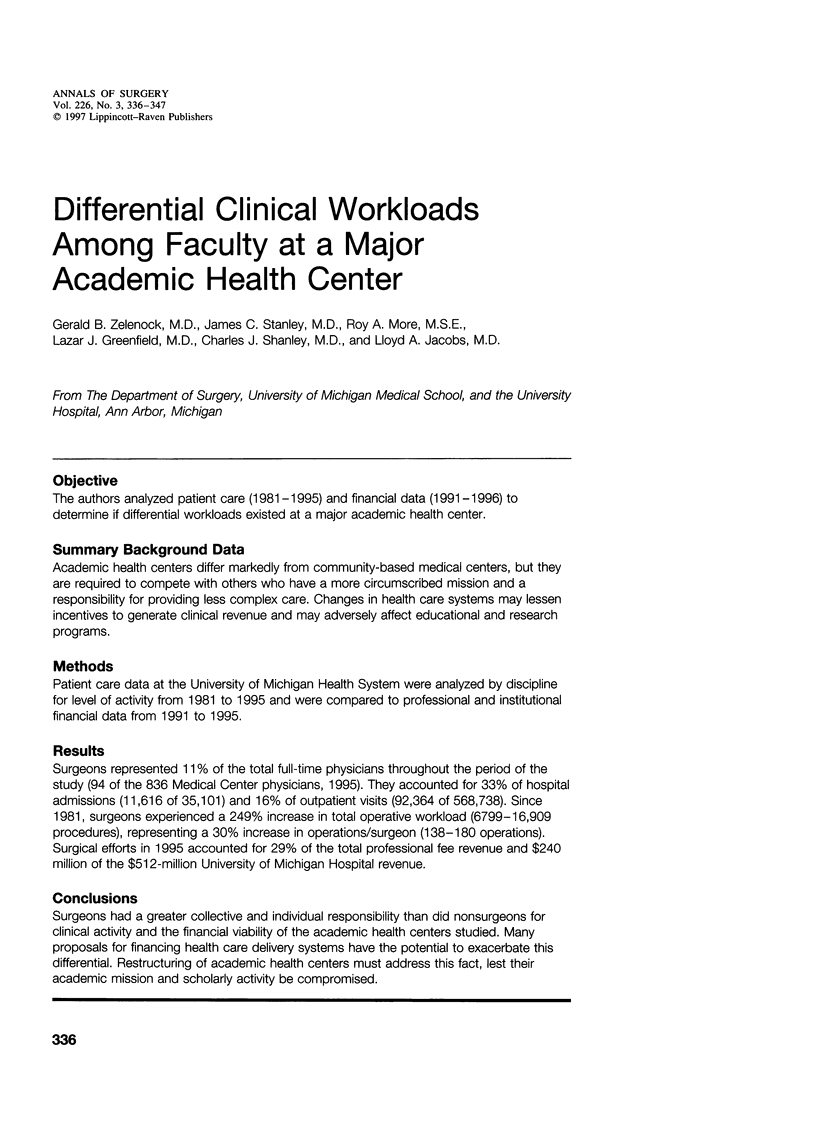

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Billi J. E., Wise C. G., Bills E. A., Mitchell R. L. Potential effects of managed care on specialty practice at a university medical center. N Engl J Med. 1995 Oct 12;333(15):979–983. doi: 10.1056/NEJM199510123331507. [DOI] [PubMed] [Google Scholar]
- Bodenheimer T. The HMO backlash--righteous or reactionary? N Engl J Med. 1996 Nov 21;335(21):1601–1604. doi: 10.1056/NEJM199611213352112. [DOI] [PubMed] [Google Scholar]
- Gallin J. I., Smits H. L. Managing the interface between medical schools, hospitals, and clinical research. JAMA. 1997 Feb 26;277(8):651–654. [PubMed] [Google Scholar]
- Gold M. R., Hurley R., Lake T., Ensor T., Berenson R. A national survey of the arrangements managed-care plans make with physicians. N Engl J Med. 1995 Dec 21;333(25):1678–1683. doi: 10.1056/NEJM199512213332505. [DOI] [PubMed] [Google Scholar]
- Iglehart J. K. Rapid changes for academic medical centers. 1. N Engl J Med. 1994 Nov 17;331(20):1391–1395. doi: 10.1056/NEJM199411173312025. [DOI] [PubMed] [Google Scholar]
- Iglehart J. K. The American health care system--Medicaid. N Engl J Med. 1993 Mar 25;328(12):896–900. doi: 10.1056/NEJM199303253281226. [DOI] [PubMed] [Google Scholar]
- Kassirer J. P. Academic medical centers under siege. N Engl J Med. 1994 Nov 17;331(20):1370–1371. doi: 10.1056/NEJM199411173312010. [DOI] [PubMed] [Google Scholar]
- Krakower J. Y., Ganem J. L., Jolly P. Review of US medical school finances, 1994-1995. JAMA. 1996 Sep 4;276(9):720–724. [PubMed] [Google Scholar]
- Kuczynski Y. T., Stanley J. C., Rosevear J. S., McMahon L. F., Jr Vascular surgeons' resource use at a university hospital related to diagnostic-related group and source of admission. J Vasc Surg. 1997 Aug;26(2):193–198. doi: 10.1016/s0741-5214(97)70179-4. [DOI] [PubMed] [Google Scholar]
- Minsky B. D. Adjuvant therapy for rectal cancer--a good first step. N Engl J Med. 1997 Apr 3;336(14):1016–1017. doi: 10.1056/NEJM199704033361410. [DOI] [PubMed] [Google Scholar]
- Redelmeier D. A., Fuchs V. R. Hospital expenditures in the United States and Canada. N Engl J Med. 1993 Mar 18;328(11):772–778. doi: 10.1056/NEJM199303183281107. [DOI] [PubMed] [Google Scholar]
- Shea S., Nickerson K. G., Tenenbaum J., Morris T. Q., Rabinowitz D., O'Donnell K., Perez E., Weisfeldt M. L. Compensation to a department of medicine and its faculty members for the teaching of medical students and house staff. N Engl J Med. 1996 Jan 18;334(3):162–167. doi: 10.1056/NEJM199601183340307. [DOI] [PubMed] [Google Scholar]
- Woolhandler S., Himmelstein D. U. Costs of care and administration at for-profit and other hospitals in the United States. N Engl J Med. 1997 Mar 13;336(11):769–774. doi: 10.1056/NEJM199703133361106. [DOI] [PubMed] [Google Scholar]
- Woolhandler S., Himmelstein D. U., Lewontin J. P. Administrative costs in U.S. hospitals. N Engl J Med. 1993 Aug 5;329(6):400–403. doi: 10.1056/NEJM199308053290606. [DOI] [PubMed] [Google Scholar]
- Woolhandler S., Himmelstein D. U. The deteriorating administrative efficiency of the U.S. health care system. N Engl J Med. 1991 May 2;324(18):1253–1258. doi: 10.1056/NEJM199105023241805. [DOI] [PubMed] [Google Scholar]
- Zelenock G. B., Holmes M. M., Campbell D. A., Jr, Stanley J. C., Greenfield L. J. Quantitative increases in surgical house officer clinical activity as the basis for increased work loads in a university hospital. Surgery. 1992 Aug;112(2):235–243. [PubMed] [Google Scholar]


